Professional Documents
Culture Documents
Dental Care During The Coronavirus Disease
Dental Care During The Coronavirus Disease
Uploaded by
clinicOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dental Care During The Coronavirus Disease
Dental Care During The Coronavirus Disease
Uploaded by
clinicCopyright:
Available Formats
GENERAL DENTISTRY
Dental care during the coronavirus disease 2019 (COVID-19)
outbreak: operatory considerations and clinical aspects
Itzhak Abramovitz, DMD/Aaron Palmon, DMD, PhD/David Levy, DMD, MS/Bekir Karabucak, DMD, MS/Nurit
Kot-Limon, DMD/Boaz Shay, DMD, PhD/Antonia Kolokythas, DDS, MSc/Galit Almoznino, DMD, MSc, MHA
Objectives: This paper is aimed at addressing the urgent need for a hospital setting and includes considerations related to
to develop a protocol that will address the operatory and clin- dental treatment in both healthy subjects and those suspected
ical aspects of dental care during the Coronavirus disease 2019 or diagnosed with COVID-19. The first part of this review dis-
(COVID-19) outbreak. Data sources: The epidemiology, clinical cusses operatory considerations; the second part discusses
signs and symptoms, and modes of transmission of COVID-19 general dental clinical aspects; the third part discusses end-
are presented. This protocol was established as an international odontic considerations; and the fourth part discusses surgical
collaboration of three dental universities: Hadassah School of aspects. This protocol may be applicable to other future similar
Dental Medicine, Israel; University of Rochester Medical Center, pandemics. Conclusion: Logistic and clinical steps are required
USA; and the University of Pennsylvania, USA. This protocol is to provide dental care during the COVID-19 outbreak while
based on a detailed review of the existing English language preventing cross-contamination and protecting the dental
literature as well on the logistic and clinical experience of each team during the provision of care. (Quintessence Int 2020;51:
facility and the opinion of the authors. The protocol is designed 418–429; doi: 10.3290/j.qi.a44392)
Key words: coronavirus, COVID-19, dental, endodontics, infection control, pulpitis
A novel disease emerged in Wuhan, China, in late 2019.1,2 The ■ Dental emergencies are potentially life-threatening and
disease was designated by the World Health Organization require immediate treatment to stop ongoing tissue bleed-
(WHO) on 12 February 2020, as Coronavirus disease 2019 ing or to alleviate severe pain or infection.
(COVID-19).3 The disease is caused by Severe Acute Respiratory ■ Urgent dental care are conditions that require immediate
Syndrome Coronavirus-2 (SARS-CoV-2) virus.2 The virus expo- attention to relieve severe pain and/or risk of infection.
nentially spread in countries around the world,4 as can be seen
in real-time visualization of the globally confirmed cases.5,6 The The ADA recommends specifically that dental practitioners
exponential increase eventually led the WHO to declare should use their professional judgment to determine the need
COVID-19 a pandemic.7 Subsequently, on 16 March 2020, the for urgent or emergency care.10
American Dental Association (ADA) recommended that dental This paper is aimed at addressing the urgent need to de-
practitioners nationwide postpone elective procedures for the velop a protocol that includes guidelines for dental care during
following three weeks,8 leading to the Israeli Ministry of Health the COVID-19 outbreak. This protocol was established for a
(MOH) recommendation to postpone elective dental proced- hospital setting and includes considerations related to dental
ures.9 The ADA proposed guidance on what conditions to con- treatment in both healthy subjects and those suspected or di-
sider as dental emergencies and nonemergency dental care.10 agnosed with COVID-19. Operatory and clinical considerations
Within a dental emergency, the ADA guidelines defined the are discussed, with particular focus on endodontic and surgi-
following10: cal care. The endodontic treatment presents unique chal-
418 QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020
Abramovitz et al
lenges, is complex, requires a longer time compared to other depending on the type of surface, the temperature, and the
dental procedures, and involves special equipment, such as humidity of the environment.24
microscopes and ultrasonic devices. Long-term assessment of
treatment outcomes is usually required. The logistic and clin-
Operatory considerations in the dental
ical steps required for the treatment of common urgent dental
set-up during the COVID-19 outbreak
care procedures, mostly endodontic urgencies, including pulp
and periapical diagnoses according to the American Associ-
Screening procedure to identify a suspected case
ation of Endodontists (AAE) Consensus Conference Recom-
of COVID-19
mended Diagnostic Terminology11 will be discussed. The goal
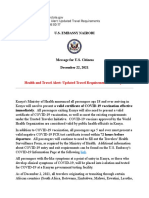
is to provide emergency and urgent dental care to patients, to Figure 1 presents a flowchart for urgent dental care during the
prevent cross-contamination, and to protect dental care pro- COVID-19 outbreak. Presenting patients, persons accompany-
viders during the provision of care. ing them, and staff can be asymptomatic. Therefore, all patients
and accompanying persons to the dental clinic during the out-
break of COVID-19 should be screened to identify asymptom-
Clinical presentation
atic and suspected cases of COVID-19.
Common symptoms of COVID-19 include fever, dry cough, dys-
pnea, sputum production, fatigue, anorexia, myalgia, and diar-
Triage protocol and patient flow
rhea.7,12,13 While the majority of patients will present with mild
symptoms, severe symptoms including high fever, pneumonia, Telehealth
acute respiratory distress syndrome (ARDS), and kidney failure Strategies to minimize face-to-face contact for initial screening
can eventually cause death.12,13 While most infected people can be accomplished via telephone or synchronous telehealth
show mild-to-moderate respiratory symptoms, 5% to 10% of encounters to identify patients suspected of COVID-19.29 When
the infected individuals show the full and severe COVID-19 re- a patient calls a dental facility to make an appointment, the
spiratory syndrome.14 According to a statement of the Ameri- phone conversation should include the main questions that
can Academy of Otolaryngology-Head and Neck Surgery (AAO- will be described below. If there is a positive (ie, “yes”) answer
HNS), anosmia, hyposmia, and dysgeusia in the absence of to any of the questions, a pharmacologic pain and/or infection
another respiratory disease should alert physicians to the pos- control-management prescription should be provided, if
sibility of coronavirus (SARS-CoV-2) infection and warrant seri- appropriate.
ous consideration for self-isolation and testing of these individ- Every practice should develop a triage protocol, based on
uals.15 The incubation period for COVID-19 is between 1 and 14 the degree of patient and community outbreak.30 This protocol
days,16-19 and the virus is shed by asymptomatic infected peo- should be kept dynamic, and adapted to changes in the local
ple.20,21 The mortality rate of COVID-19 ranges from 0.2% in circumstances. For example, as the number of COVID-19 cases
young healthy people, increasing with age and comorbidities.22 rose to a pandemic, the disease became relevant to people far
Laboratory findings include leukopenia, leukocytosis, and from Wuhan city and its surrounding areas.
lymphopenia.12,13 Radiographic findings in chest computed Triage screening procedures can be performed by dentists,
tomography (CT) scans demonstrate ground-glass opacifica- hygienists, dental assistants, and dental aids as long as per-
tion with or without consolidative abnormalities, consistent sonal protective equipment (PPE) is used. The PPE should in-
with viral pneumonia.23 clude a long-sleeved disposable gown, disposable cap, surgical
face masks, and protective eyewear.
Transmission
Accompanying persons
Human-to-human transmission has been described mainly During the COVID-19 outbreak, accompanying persons are not
through respiratory droplets and contaminated hands or sur- allowed to enter many dental facilities. However, one guardian
faces.24-26 The virus remained viable in aerosols under experi- of a patient who is a minor or a patient with an intellectual or
mental conditions for at least 3 hours27 and has been detected developmental disability is allowed.
also in blood and stool specimens.28 Coronavirus can persist on
inanimate surfaces like metal, glass, or plastic for up to 9 days,
QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020 419
GENERAL DENTISTRY
Triage will be referred for medical consultation and will not be allowed
The triage procedure should include the following records: to enter the dental facility. Necessary emergency dental care
Questionnaire A self-administered questionnaire should be should be performed in properly equipped designated hospi-
completed by the patient or his/her guardian, and include the tals.31 These hospitals should identify a negative pressure
name, identity number, and signature. This information is of room(s) for the dental treatment of suspected/confirmed cases
particular importance in cases of tracing or an epidemiologic of COVID-19 within the area treating these patients.31 In addi-
investigation. tion to being negatively pressurized, the room should include
a dental unit and radiographic equipment similar to rooms
The questionnaire should include questions regarding: where general anesthesia is utilized. Suspected/confirmed
■ A history of contact with a person suspected for or diag- patients who need emergency or urgent dental care should
nosed with COVID-19 within the previous 14 days. transfer to the emergency room in a medical center for exam-
■ Experiencing flu-like symptoms including fever, respiratory ination by an oral and maxillofacial surgeon or an attending
problems such as dry cough or difficulty in breathing within dental practitioner. Pharmacologic or noninvasive measures
the past 14 days, or being in contact with another person are recommended. However, invasive procedures should be
with these symptoms. performed by the relevant dental expert in a negatively pres-
■ Experiencing loss/change of smell or taste.* surized and appropriately equipped room, as described in
(*Based on the addition of these symptoms to the list of screening tools for possible detail below (see section “Clinical guidelines for emergency
COVID-19 infection, proposed by the AAO-HNS.15
and urgent general dental care”).
Temperature Record the temperature of patients and the
accompanying person using a contact-free forehead thermo-
Safety considerations for staff during the
meter.25,31
COVID-19 outbreak
Visible signs and symptoms of respiratory problems The US Occupational Safety and Health Administration (OSHA)
Patients and the accompanying person should be instructed to developed planning guidance to prepare workplaces for the
remove their face masks (if any) to evaluate signs of respiratory COVID-19 outbreak.29 According to the recommendations,
problems such as cough and shortness of breath. workers should be encouraged to self-assess daily for symp-
In Israel, the Ministry of Health has launched HAMAGEN, a toms of COVID-19 as described above and stay home if they are
phone application that identifies contacts between diagnosed sick.29 Staff should be screened upon entering a facility to iden-
patients and people who came in contact with them in the 14 tify suspected cases of COVID-19, as previously described.
days before the patient’s diagnosis of the disease.32 Such appli- The individual risk factors of the staff including older age,
cations, if available in other countries, may also assist the triage medical comorbidities, and presence of chronic systemic illness
process and identify suspected patients. should be assessed.29 Increased risk factors include immuno-
compromising conditions, pregnancy, as well as nonoccupa-
Treatment of patients who are found “negative” in the tional risk factors at home and in community settings.29 If
triage procedure absenteeism increases, dental teams should cross-train staff for
Emergency/urgent care can be performed within the dental all essential office and medical/dental functions.30
facility if all the questions are answered “no,” there are no visible
signs and symptoms of respiratory problems, and if the body
Infection prevention and control recommenda-
temperature is below 38°C (100.4°F).33 In Hadassah hospital,
tions during the COVID-19 outbreak
37.5°C (99.5°F) is considered the deciding temperature. The
patients and an accompanying person who are allowed to Infection control measures should address modes of transmis-
enter the facility wear a bracelet with an identity number, sion and persistence of the virus in the air and on surfaces. The
enabling them to move within the building. general rule is compliance with standard precautions, assuming
that every patient may be potentially infected or colonized with
Treatment of patients who are “positive” in the triage/ a pathogen.30 The US Centers for Disease Control and Preven-
screening procedure tion (CDC) published interim infection prevention and control
Patients who are positive to any of the triage/screening steps recommendations for patients with suspected or confirmed
420 QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020
Abramovitz et al
COVID-19 in healthcare settings.34 The recommendations are General measures required in all dental care include the fol-
modifications and additions to the 2003 CDC guidelines35 and lowing.
the 2016 CDC summary.36 Proper disinfectants should be used
against SARS-CoV-2, as published by the US Environmental Pro-
Medical history and consultation
tection Agency (EPA).37 The adequate time between patient
appointments must be taken to prepare the treatment room Before the initiation of emergency/urgent dental care, the den-
properly, allow for time-sensitive, appropriate disinfection, and tal practitioner should review the medical history of the patient
environmental cleaning. Proper hand hygiene,38 thorough dis- and consider consulting a physician, as needed. The dental
infection of all clinical and administrative surfaces within the practitioner should record the current medical diagnoses, med-
dental clinic in addition to the treatment room, proper steriliza- ication, allergies/sensitivities, and other pertinent information.
tion processes using chemical indicators, and appropriate
waste disposal should be routine and reinforced.35,36
Patients without COVID-19 symptoms/diagnosis
Waiting areas Emergency/urgent dental treatment should be performed
Patients in the waiting area should be separated by 2 m. Hand within a typical dental facility.
sanitizers with at least 70% alcohol should be provided in all
waiting and patient care areas. Signs showing proper hand-
Patients with suspected COVID-19
washing technique should be placed close to soap dispens-
ers.30 Shared items such as toys, pens, and magazines, should When there is a negative triage result, and yet the medical
not be placed in waiting areas.30 Waiting time should be as evaluation reveals suspicion for COVID-19 disease, the patient
short as possible to minimize the number of people present. should be referred for proper medical evaluation. Emergency/
urgent dental treatment should be performed within the neg-
Personal protective equipment (PPE) ative pressure room in a properly equipped hospital.
Access to PPE for health providers is a key concern in most af-
f
fected facilities as there are PPE shortages, including reports
Patients with COVID-19 diagnosis
that some supplies and equipment might not meet require-
ments.39 Unfortunately, as the pandemic accelerates, COVID-19 Patients diagnosed with COVID-19 should be treated in a neg-
has spread to health providers.39 PPE should include a long- ative pressure room in a properly equipped hospital. Emphasis
sleeved disposable gown, a disposable cap, a surgical face mask, should be on the current medical status, symptoms, and com-
and a face shield as well as protective eyewear and gloves. All plications related to the COVID-19 infection, particularly those
eyes should be covered by using eyewear with upper, lower, and related to respiratory disease, its severity, and level of control.
side shields. All aerosol generation procedures should be per-
formed wearing an N-95 mask.31 Guidelines for donning and
COVID-19 diagnosis with unstable respiratory
doffing PPE40 and respirators,41 as well as guidance for extended
disease
use and limited reuse of N95 mask,42 should be followed. The
staff should discard all PPE within the treatment room and not Before performing emergency dental treatment of hospitalized
leave the room with any of the disposable items. patients with unstable respiratory symptoms (eg, shortness of
breath at rest, and oxygen saturation level < 91%), consult the
physician and, if possible, defer invasive treatment until the
General dental considerations:
patient’s condition stabilizes. Use alternatives such as pharma-
Clinical guidelines for emergency and
cologic agents.43
urgent general dental care
Emergency and urgent dental care treatments should be
COVID-19 diagnosis with stable respiratory disease
treated as minimally invasively as possible in a well-ventilated
and, if available, negative pressure room.10 Only the doctor and If breathing and oxygenation is adequate, emergency dental
an assistant should be present during treatment to minimize care procedures should be minimally invasive and be per-
exposure to other individuals. formed in a designated room. Depression of respiration or re-
QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020 421
GENERAL DENTISTRY
duction in oxygenation should be avoided by treating the pa- standard regimen to prevent endocarditis is recommended
tient in a semi-supine or upright chair position, using a pulse (http://www.heart.org) unless another regimen is advised by
oximeter, providing oxygen supplementation, and avoiding the general physician.
respiratory depressing medications.43 Treatment of these pa-
tients should be definitive on a single occasion, anticipating
Prophylactic mouth rinse
the possibility that the respiratory status may deteriorate, obvi-
ating any further treatment. Use a prophylactic mouth rinse, such as 1% hydrogen peroxide
or 0.2% povidone, before dental procedures.25,31 For children
under the age of 6 years, the application of the mouth rinse can
Management of dental anxiety
be done using a gauze pad. It is also recommended to apply the
Dental practitioners recognize that dental and surgical proced- mouth rinse on endodontically treated teeth after rubber dam
ures are potential stress- and anxiety-inducing44 as a result of is placed and the access opening is established. Patients should
physiologic (eg, pain) or psychologic (anxiety, fear) factors.45 be encouraged to keep good oral hygiene during the outbreak.
Pain assessment using a 0 to 10 numeric pain scale is recom-
mended. Stress for people and communities may be exacer-
Local anesthesia
bated by public health emergencies such as COVID-19.46,47
Moreover, anxiety regarding COVID-19 disease can lead to social The proper use of sharps is crucial, with special emphasis on
stigma.46 Resources on handling stress during a pandemic, such recapping needles using a one-handed scoop technique. The sys-
as published by the ADA, are recommended.48 Stress reduction temic condition of the patient should be evaluated in the selec-
protocols are recommended during treatment,45,49 including the tion of the local anesthetic. The use of a vasoconstrictor may be
use of premedication, psychosedation during therapy, and ade- limited or contraindicated in many patients infected with COVID-
quate pain control during therapy and postoperatively. 19 due to advanced age and comorbidities. Local anesthesia may
Nitrous oxide (N2O) inhalation sedation should not be not be needed in cases of previously endodontically treated teeth
administered to patients suspected as coronavirus carriers, or and teeth with pulp necrosis. However, local anesthesia may be
sick with COVID-19, or showing any other upper respiratory considered necessary in cases of previously initiated endodontic
tract infection (URTI). N2O inhalation sedation should be only therapy, and mandatory in symptomatic irreversible pulpitis.
be performed in settings that can provide proper infection con-
trol measures of the equipment used, including autoclaving of
Isolation with rubber dam and extra high-volume
face masks and using disposable components.
suction
Both rubber dam isolation and high-volume suction should be
Dental radiography
used whenever possible to minimize contact with saliva and
Extraoral dental radiography methods (eg, panoramic radiog- reduce contaminated aerosol or spatter.25,31
raphy and cone beam CT) are preferable during the outbreak
of COVID-19.31 Intraoral sensors should be protected with a dis-
Anti-retraction handpieces
posable barrier, cleaned, and disinfected. Cone extension par-
alleling instruments should be heat-sterilized and placed in The frequency of aerosol-generating procedures should be
sealed packages after use. minimized and when necessary high-speed dental handpieces
with anti-retraction valves are recommended to avoid aspira-
tion of debris and fluids which can later be expelled.25
Antibiotic prophylaxis
A dental practitioner treating a patient with active COVID-19
Postoperative antibiotics
infection should consult the general physician regarding the
need for antibiotic prophylaxis to prevent systemic infection Postoperative antibiotics should be considered in a patient
from invasive dental procedures. Since many COVID-19 patients with active COVID-19 infection, when in addition to endodon-
are older with comorbidities, there might be other indications tic emergency the patient presents with systemic involvement,
for antibiotic prophylaxis. The American Heart Association’s localized fluctuant swellings, elevated body temperature above
422 QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020
Abramovitz et al
38°C, malaise, lymphadenopathy, or trismus.50 The systemic dental clearance before heart transplantation and allogeneic
antibiotics should be added to the treatment plan for each hematopoietic stem cell transplantation.53 The current proto-
endodontic pathology, as described below. The choice of anti- cols in the treatment for each AAE diagnostic category were
biotic should be confirmed with the patient’s physician. reviewed and appropriate modifications were recommended to
develop new protocols during the COVID-19 outbreak. In gen-
eral, if the tooth is is nonrestorable, extraction is recommended.
Postoperative analgesics
The protocol for emergency endodontic treatment includes
Postoperative analgesics should be considered in all patients. the measures outlined below.
The choice of analgesics should be confirmed with the patient’s
physician. Although news reports previously stated that the
Endodontic equipment
use of nonsteroidal anti-inflammatory drugs (NSAIDs) could
worsen COVID-19,51 the US Food and Drug Administration The use of endodontic microscopes and endodontic loops
(FDA) published a statement declaring the FDA is not aware of should be minimized. Since the emphasis during treatment is
scientific evidence connecting the use of NSAIDs with worsen- to utilize simple and minimally invasive procedures, the use of
ing COVID-19 symptoms but will be further investigating this these devices in a specially equipped operating room for
issue.52 Considering this controversial issue, treatment options COVID-19 patients may be contraindicated. Moreover, micro-
other than NSAIDs should be preferred for a patient who suffers scopes may be incompatible with PPE, due to the increased
from COVID-19. distance from the lenses created by the PPE. The increased dis-
tance may lead to an inability to achieve adequate and useful
views. Loops may be used as long as there is side coverage, a
Endodontic considerations during the
face shield, and an appropriate mask. There is an urgent need
COVID-19 outbreak
to develop techniques and microscopes compatible with full
PPE protection.
Urgent endodontic treatment
Endodontic procedures require modifications to the previously
Endodontic procedures
discussed recommendations pertaining to general emergency/
urgent dental care. The ADA definitions of dental emergency Prophylactic mouth rinses should be used as described above.
include the management of relevant conditions, many of which As mentioned, rubber dam should be placed before the estab-
are endodontic, including pulpal inflammation, abscess, local- lishment of an access cavity. The use of high-speed handpieces
ized bacterial infection, tooth fracture, dental trauma with avul- should be limited to minimize the generation of aerosol. If pos-
sion/luxation, dental treatment required before critical medical sible, use low-speed devices to remove caries and access pulp
procedures, and replacement of temporary restorations on chambers and root canals. High-power, high-volume suction
endodontic access openings.10 In this section, the ADA recom- should be used for all procedures.
mendations have been modified, using the currently accepted
classification of the AAE Consensus Conference Recommended
Irrigants
Diagnostic Terminology.11 During this crisis, the general princi-
ple that emergency and urgent dental care treatment should be Standard practice in endodontic treatment is the use of a disinfec-
minimally invasive applies also to endodontic procedures. Spe- tant irrigant such as sodium hypochlorite (NaOCl), chlorhexidine
cial considerations include the possibility of complications fol- gluconate, or a mixture of tetracycline, citric acid, and a detergent
lowing an endodontic intervention (eg, flare-ups), occurring as (MTAD). NaOCl is the preferred irrigant due to reports that chlor-
COVID-19 worsens, leading to an unstable respiratory condi- hexidine gluconate may be ineffective in killing coronavirus.25,54
tion. Moreover, as the patient’s immune system is challenged by
the infection, endodontic healing might be compromised. A
Temporary restoration
general guideline is to perform not only minimally invasive pro-
cedures but also to limit the treatment intervention to a single At this time, the calcium sulfate base is not recommended due
episode. The model for treating patients who may become to low compressive strength, solubility, and expansion.55 These
hemodynamic and immunologically unstable already exists for characteristics may impact the integrity of the seal, leading to
QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020 423
GENERAL DENTISTRY
Pharmacologic Screening via Emergency/
pain/infection phone/ urgent dental care
control- Telehealth
management
Screening:
– Questionnaire
– Temperature
– Visible signs
Positive screening Negative screening
Refer for urgent dental care Urgent dental treatment in the
in hospital setting dental facility
COVID-19 diagnosis
Unstable Stable
Pharmacologic – IPC considerations
pain/infection – Manage dental anxiety
control- – Systemic evaluation
management – Prophylactic mouth rinse
– Analgesics AB consideration
– Rubber dam if possible
– Anti-retraction headpiece
– Specific clinical algorithm – see Fig 2
Treatment of stable COVID-19
patients should be performed in
a negatively pressurized room
1
Fig 1 Urgent dental care flowchart during the COVID-19 outbreak.
a cracked tooth,56 resulting in further discomfort, and a need outbreak, urgent treatment is focused on providing relief of the
for additional emergency dental care. In all cases where a tem- patient’s chief complaint as quickly as possible to reduce virus
porary restoration is placed, an occlusal reduction is mandatory exposure risk, as well as to reduce the need for further visits.
for patients with COVID-19 infection. Removal of a temporary The protocol includes the following treatment modalities
restoration should be performed at low speed, if possible. for the treatment of urgent endodontic care.
Symptomatic irreversible pulpitis with normal apical tissues
Suggested treatment plan for urgent endodontic
This entity is categorized as “severe dental pain from pulpal in-
treatment protocol during the COVID-19 outbreak
flammation” in the ADA guideline on dental emergency and
Figure 2 summarizes the treatment protocol for specific pulp and nonemergency procedures.10 Pulpotomy should be performed
periapical diagnoses based on the AAE Consensus Conference as an emergency procedure for temporary relief of symptoms.57
Recommended Diagnostic Terminology.11 During the COVID-19 Calcium hydroxide- or bioceramic-based material may be used as
424 QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020
Abramovitz et al
Extraction Questionable/
Poor prognosis
Urgent endodontic care Asymptomatic
Symptomatic Postponed treatment
SIP/SAP/AAA VRF/ Endodontic-periodontal Dental trauma
Cracked tooth lesion
SIP SAP/AAA VRF Cracked tooth Primary Primary Tooth fracture Avulsion/
endodontic periodontal involving the luxation
lesion lesion with pulp
secondary
Pulpotomy Debridement, Extraction
endodontic
Irrigation, Reposition
involvement
Dressing and splinting
1 probing pocket Probing pocket Debridement, Debridement,
depth ≥ 5 mm depth < 5 mm Irrigation, Irrigation,
Dressing Dressing
Pulpotomy if tooth is Vital pulp
Extraction Pulp necrosis
vital; Debridement,
Irrigation, Dressing if
tooth is nonvital
Debridement,
Pulpotomy
Irrigation, 2
Dressing
Fig 2 Urgent endodontic treatment flowchart during COVID-19 outbreak. AAA, acute periapical abscess; SAP, symptomatic apical periodonti-
tis; SIP, symptomatic irreversible pulpitis; VRF, vertical root fracture.
a dressing material according to the standard of care of the Amer- dressing.62 These procedures should be followed with a tem-
ican Board of Endodontics.58 Alternatively, pulpotomy with bio- porary restoration and occlusal reduction, to prevent pain from
ceramic material may be used.59 Both options should be followed the apical origin and to protect the remaining tooth structure.63
by a temporary restoration and occlusal reduction. However, if In cases of pulp necrosis with an acute apical abscess and con-
irreversible pulpitis is associated with a poor prognosis due to tinuous inflammatory exudate, consider endodontic drainage
periodontal or restorative reasons that may require subsequent directly through the tooth or soft tissue incision and drainage
urgent care treatment, extraction is recommended (Fig 2).60 (I&D) and consider systemic antibiotics.50
Pulp necrosis with symptomatic apical involvement Previously treated teeth
Symptomatic apical periodontitis or acute apical abscesses Previously treated teeth may present with symptomatic apical
may be the sequellae of an infected root canal (pulp necrosis or periodontitis or an acute apical abscess. In both cases, if removal
previously initiated treatment) or infected root canal filling of the previous root canal filling is uncomplicated and achieved,
(previously treated teeth).61 In cases of pulp necrosis or previ- treatment should be provided as described for pulp necrosis. If
ously initiated treatment, the recommendation is to perform the removal of root canal filling cannot be achieved, occlusal
root canal debridement, irrigation, and calcium hydroxide reduction and a prescription for antibiotics are recommended.50
QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020 425
GENERAL DENTISTRY
If the tooth presents with an unfavorable prognosis, ex- calcium hydroxide dressing68 and glass-ionomer restoration. If
traction should be performed.60 I&D should be considered in the pulp is necrotic, it should be treated according to the
cases of a previously treated tooth with an acute apical abscess above-mentioned protocol for pulp necrosis. Emphasis should
and favorable prognosis. be made to remove sharp edges and to protect the soft tissue.
Avulsion/luxation Tooth repositioning and flexible splinting
Previously initiated therapy may be performed in healthy subjects and subjects with mild
In the situation where endodontic treatment was previously disease without respiratory symptoms.69 However, for hospital-
initiated, continuing treatment of a tooth with normal apical ized patients with respiratory symptoms, reimplantation,
tissue is considered elective and not an urgent dental problem. repositioning, and splinting are not recommended due to risks of
Treatment can be postponed until elective treatments resume aspiration, and the need for ongoing treatment and follow-ups.
in the future.
Oral and maxillofacial surgery procedures
Cracked tooth and vertical root fracture (VRF)
during the COVID-19 outbreak
Teeth with signs and symptoms of VRF should be extracted.60
Meng et al31 reported on the treatment of a patient presenting For the safety of all involved in the care of patients during the
with a caries-free cracked tooth. The patient was scheduled for COVID-19 outbreak, it is advisable to defer all elective aero-
the last appointment of the day and a high-speed handpiece was sol-producing procedures due to the extreme risk of spreading
used to prepare the cavity. If a visible crack is seen directly with- the virus. Procedures such as incision and drainage of neck fas-
out the use of visual augmentation, extraction is recommended. cia space abscess, head and neck cancer, and maxillofacial
However, if there is a concern that the full extent of a crack can trauma, although aerosol-producing, are urgent or emergency
be revealed only with the aid of a microscope and the patient is procedures handled in the hospital and the operating room set-
confirmed for COVID-19, the dental practitioner should rely on tings. As such, the specific protocols set in place by the leader-
basic endodontic examination to diagnose a cracked tooth. A ship in each hospital regarding personnel and patient manage-
cracked tooth should be suspected when there is pain perceived ment on the use of PPE and place of care should be followed.
on sudden release of pressure in a bite stick test and sensitivity in Per general surgery guidelines, “Essential surgery is an (opera-
cold/heat tests.64,65 Krell and Caplan66 showed that cracked teeth tive) procedure that is considered to be vitally necessary for treat-
with one probing pocket depth ≥ 5 mm had a poor prognosis, ing a disease or injury. Postponing or deciding against an essential
and in this case extraction is recommended (see Fig 2). procedure may result in a patient’s death or permanent impair-
ment.”70 Extractions, especially those requiring a high-speed hand-
Endodontic-periodontal lesion piece, generate aerosol and ideally should be postponed unless
A vitality test for the tooth is required for a suspected endodon- deemed essential, urgent, or emergency. Appropriate PPE when
tic-periodontal lesion. For a vital tooth suggestive of a primary performing extractions during the COVID-19 outbreak includes
periodontal lesion, consultation with a periodontist is recom- the use of an N-95 mask or a higher level respirator and face shield
mended. If a periodontal consultation is not possible and the since regular surgical masks do not offer adequate protection.
tooth is symptomatic, consider extraction.60 When possible, the use of a high-speed handpiece to perform the
A tooth with a primary endodontic lesion and secondary extraction(s) should be avoided. Additionally, the procedures
periodontal involvement should be treated according to the should be performed by the most experienced providers available,
above-mentioned protocol for pulp necrosis if there was no to maximize efficiency and minimize the time of the operation.
previous endodontic treatment. A tooth with previous end-
odontic treatment should be treated according to the protocol
Conclusion
for previously treated teeth.
Cases with unfavorable/questionable prognosis (periodon- The new COVID-19 outbreak challenges current treatment pro-
tal or endodontic) should be extracted.60 tocols. Each dental discipline should establish the necessary
modifications in logistics and treatment protocols. This updated
Dental trauma protocol will assist dental practitioners to treat their patients
Tooth fracture involving the pulp Cases of vital pulp should during the COVID-19 outbreak. This protocol may be applicable
be managed with a pulpotomy, using bioceramic material67 or to other future similar pandemics.
426 QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020
Abramovitz et al
Declarations
The authors have no conflicts of interest to declare.
References
1. Li ZY, Meng LY. [The prevention and con- 11. American Association of Endodontists. 21. Zhang W, Du RH, Li B, et al. Molecular
trol of a new coronavirus infection in depart- Guide to clinical endodontics. 6th ed. http:// and serological investigation of 2019-nCoV
ment of stomatology]. Zhonghua Kou Qiang dental.id/wp-content/uploads/2016/08/aae_ infected patients: implication of multiple
Yi Xue Za Zhi 2020;55:E001. guidetoclinicalendodontics6.pdf. Accessed 1 shedding routes. Emerg Microbes Infect
2. Zhu N, Zhang D, Wang W, et al. A novel April 2020. 2020;9:386–389.
coronavirus from patients with pneumonia 12. Chen N, Zhou M, Dong X, et al. Epide- 22. [The epidemiological characteristics
in China, 2019. N Engl J Med 2020;382:727– miological and clinical characteristics of 99
of an outbreak of 2019 novel coronavirus
733. cases of 2019 novel coronavirus pneumonia
diseases (COVID-19) in China]. Zhonghua Liu
in Wuhan, China: a descriptive study. Lancet
3. World Health Organization. Director- Xing Bing Xue Za Zhi 2020;41:145–151.
2020;395:507–513.
General’s remarks at the media briefing on
13. Wang D, Hu B, Hu C, et al. Clinical char- 23. Shi H, Han X, Jiang N, et al. Radiological
2019-nCoV on 11 February 2020. https://
www.who.int/dg/speeches/detail/who-di- acteristics of 138 hospitalized patients with findings from 81 patients with COVID-19
rector-general-s-remarks-at-the-media-brief- 2019 novel coronavirus-infected pneumonia pneumonia in Wuhan, China: a descriptive
ing-on-2019-ncov-on-11-february-2020. in Wuhan, China (epub ahead of print 7 Feb study (epub 24 Feb 2020). Lancet Infect Dis
Accessed 12 February 2020. 2020). JAMA doi: 10.1001/jama.2020.1585. doi: 10.1016/S1473-3099(20)30086-4.
4. Phelan AL, Katz R, Gostin LO. The novel 14. Yang X, Yu Y, Xu J, et al. Clinical course 24. Kampf G, Todt D, Pfaender S, Steinmann
coronavirus originating in Wuhan, China: and outcomes of critically ill patients with E. Persistence of coronaviruses on inanimate
challenges for global health governance SARS-CoV-2 pneumonia in Wuhan, China: a surfaces and their inactivation with biocidal
(epub ahead of print 30 Jan 2020). JAMA doi: single-centered, retrospective, observational agents. J Hosp Infect 2020;104:246–251.
10.1001/jama.2020.1097. study (epub ahead of print 24 Feb 2020).
Lancet Respir Med doi: 10.1016/S2213- 25. Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren
5. Dong E, Du H, Gardner L. An interactive 2600(20)30079-5. B. Transmission routes of 2019-nCoV and
web-based dashboard to track COVID-19 in controls in dental practice. Int J Oral Sci
real time (epub ahead of print 19 Feb 2020). 15. AAO-HNS AAoOHaNS. Anosmia, Hy-
posmia, and Dysgeusia Symptoms of Coro- 2020;12:9.
Lancet Infect Dis doi: 10.1016/S1473–3099
navirus Disease, 22 March 2020. https:// 26. World Health Organization. Modes of
(20)30120-1.
www.entnet.org/content/aao-hns-anosmia- transmission of virus causing COVID-19:
6. John Hopkins University: Coronavirus hyposmia-and-dysgeusia-symptoms-corona- implications for IPC precaution recommen-
Resource Center. Coronavirus COVID-19 virus-disease. Accessed 30 March 2020. dations. https://www.who.int/news-room/
global cases by the Center for Systems
16. Leung C. The difference in the incuba- commentaries/detail/modes-of-
Science and Engineering (CSSE) at Johns
tion period of 2019 novel coronavirus (SARS- transmission-of-virus-causing-covid-19-
Hopkins 2020. https://coronavirus.jhu.edu/
CoV-2) infection between travelers to Hubei implications-for-ipc-precaution-recommen-
map.html. Accessed 30 March 2020. and non-travelers: The need of a longer dations. Accessed 1 April 2020.
7. World Health Organization. Coronavirus quarantine period (epub ahead of print 18
disease (COVID-2019) situation Report – 51. March 2020). Infect Control Hosp Epidemiol 27. van Doremalen N, Bushmaker T, Morris
Geneva: World Health Organization, 2020. doi: 10.1017/ice.2020.81. DH, et al. Aerosol and surface stability of
https://www.who.int/docs/default-source/ SARS-CoV-2 as compared with SARS-CoV-1
17. Linton NM, Kobayashi T, Yang Y, et al.
coronaviruse/situation-reports/20200311- Incubation period and other epidemiologi- (epub ahead of print 17 March 2020). N Engl
sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10. cal characteristics of 2019 novel coronavirus J Med doi: 10.1056/NEJMc2004973.
Accessed 30 March 2020. infections with right truncation: a statistical 28. Tang A, Tong ZD, Wang HL, et al. Detec-
8. American Dental Association. ADA analysis of publicly available case data. J Clin tion of novel coronavirus by RT-PCR in stool
recommending dentists postpone elective Med 2020;9:E538. specimen from asymptomatic child, China
procedures. 16 March 2020. https://www. 18. Backer JA, Klinkenberg D, Wallinga J. (epub ahead of print 9 March 2020). Emerg
ada.org/en/publications/ada-news/2020-ar- Incubation period of 2019 novel coronavirus Infect Dis 2020;26 doi: 10.3201/
chive/march/ada-recommending-den- (2019-nCoV) infections among travellers eid2606.200301.
tists-postpone-elective-procedures. from Wuhan, China, 20-28 January 2020.
29. U.S. Department of Labor. Occupa-
9. State of Israel: Ministry of Health. Guide- Euro Surveill 2020;25:2000062.
tional Safety and Health Administration.
lines for Dental Clinics on the Coronavirus. 19. Guan WJ, Ni ZY, Hu Y, et al. Clinical char- Guidance on Preparing Workplaces for
https://www.health.gov.il/hozer/dent_2020- acteristics of coronavirus disease 2019 in
158357020.pdf. Accessed 1 April 2020. COVID-19. US Department of Labor: OSHA
China (epub 28 Feb 2020). N Engl J Med
3990-03 2020.
10. Solana K, American Dental Association. doi.10.1056/NEJMoa2002032.
ADA develops guidance on dental emer- 20. Lai CC, Shih TP, Ko WC, Tang HJ, Hsueh 30. American Academy of Family Physi-
gency, nonemergency care. 18 March 2020. PR. Severe acute respiratory syndrome coro- cians. Checklist to Prepare Physician Offices
https://www.ada.org/en/publications/ada- navirus 2 (SARS-CoV-2) and coronavirus dis- for COVID-19. https://www.aafp.org/dam/
news/2020-archive/march/ada-devel- ease-2019 (COVID-19): The epidemic and the AAFP/documents/patient_care/public_
ops-guidance-on-dental-emergency-none- challenges. Int J Antimicrob Agents health/COVID-19%20Office%20Prep%20
mergency-care. Accessed 30 March 2020. 2020;55:105924. Checklist.pdf. Accessed 30 March 2020.
QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020 427
GENERAL DENTISTRY
31. Meng L, Hua F, Bian Z. Coronavirus Dis- 43. Little J, Miller C, Rhodus N. Little and 56. Tennert C, Eismann M, Goetz F, Woelber
ease 2019 (COVID-19): Emerging and future Falace’s Dental Management of the Medically JP, Hellwig E, Polydorou O. A temporary filling
challenges for dental and oral medicine (epub Compromised Patient, 9th edition. St Louis: material used for coronal sealing during end-
ahead of print 12 March 2020). J Dent Res doi: Mosby, 2017. odontic treatment may cause tooth fractures
10.1177/0022034520914246. 44. Corah NL, Gale EN, Illig SJ. Assessment in large Class II cavities in vitro. Int Endod J
32. Israel Ministry of Health. The Ministry of of a dental anxiety scale. J Am Dent Assoc 2015;48:84–88.
Health launches “HAMAGEN” – an app to pre- 1978;97:816–819. 57. American Association of Endodontists.
vent the spread of coronavirus. https://www. 45. Malamed SF. Knowing your patients. Guide to Clinical Endodontics. 6th ed. Chicago:
gov.il/en/departments/news/ 22032020_04. J Am Dent Assoc 2010;141(Suppl 1):3S–7S. American Association of Endodontists, 2016.
Accessed 30 March 2020. 46. Centers for Disease Control and Preven- 58. Lee M, Winkler J, Hartwell G, Stewart J,
33. Huang C, Wang Y, Li X, et al. Clinical tion. Coronavirus Disease 2019 (COVID-19): Caine R. Current trends in endodontic prac-
features of patients infected with 2019 novel Reducing Stigma. https://www.cdc.gov/ tice: emergency treatments and technological
coronavirus in Wuhan, China. Lancet coronavirus/2019-ncov/daily-life-coping/re- armamentarium. J Endod 2009;35:35–39.
2020;395:497–506. ducing-stigma.html. Accessed 30 March 2020. 59. Duncan HF, Galler KM, Tomson PL, et al.
34. Centers for Disease Control and Preven- 47. Centers for Disease Control and Preven- European Society of Endodontology position
tion. Interim Infection Prevention and Control tion. Coronavirus Disease 2019 (COVID-19)- statement: Management of deep caries and the
Recommendations for Patients with Sus- Stress and Coping. https://www.cdc.gov/ exposed pulp. Int Endod J 2019;52:923–934.
pected or Confirmed Coronavirus Disease coronavirus/2019-ncov/daily-life-coping/ 60. American Association of Endodontists.
2019 (COVID-19) in Healthcare Settings. managing-stress-anxiety.html. Accessed 30 Scope of Endodontics: Extraction of Teeth.
https://www.cdc.gov/coronavirus/2019-ncov/ March 2020. Chicago: American Association of Endodon-
infection-control/control-recommendations. 48. American Dental Association. Association tists, 2017.
html. Accessed 30 March 2020. offers resources on handling stress during a 61. American Association of Endodontists.
35. Kohn WG, Collins AS, Cleveland JL, Harte pandemic. https://www.ada.org/en/publica- AAE Consensus Conference Recommended
JA, Eklund KJ, Malvitz DM. Guidelines for In- tions/ada-news/2020-archive/march/associa- Diagnostic Terminology. J Endod
fection Control in Dental Health-Care Settings tion-offers-resources-on-handling-stress- 2009;12:1634.
- 2003. MMWR Recomm Rep 2003;52 during-a-pandemic. Accessed 30 March 2020. 62. Mohammadi Z, Dummer PM. Properties
(RR-17):1–61. 49. McCarthy FM, Malamed SF. Physical and applications of calcium hydroxide in end-
36. Centers for Disease Control and Preven- evaluation system to determine medical risk odontics and dental traumatology. Int Endod
tion. Summary of Infection Prevention Prac- and indicated dental therapy modifications. J 2011;44:697–730.
tices in Dental Settings: Basic Expectations for J Am Dent Assoc 1979;99:181–184. 63. Gatewood RS, Himel VT, Dorn SO. Treat-
Safe Care. Atlanta: Centers for Disease Control 50. Lockhart PB, Tampi MP, Abt E, et al. ment of the endodontic emergency: a decade
and Prevention, US Dept of Health and Evidence-based clinical practice guideline on later. J Endod 1990;16:284–291.
Human Services; October 2016. antibiotic use for the urgent management of 64. Cameron CE. The cracked tooth syn-
37. United States Environmental Protection pulpal- and periapical-related dental pain and drome: additional findings. J Am Dent Assoc
Agency. List N: Disinfectants for Use Against intraoral swelling: A report from the American 1976;93:971–975.
SARS-CoV-2. https://www.epa.gov/pesticide- Dental Association. J Am Dent Assoc
registration/list-n-disinfectants-use-against- 65. Cameron CE. Cracked-tooth syndrome.
2019;150:906–921.e912. J Am Dent Assoc 1964;68:405–411.
sars-cov-2. Accessed 30 March 2020. 51. Fang L, Karakiulakis G, Roth M. Are pa-
38. American Dental Association. Hand 66. Krell KV, Caplan DJ. 12-month success
tients with hypertension and diabetes melli- of cracked teeth treated with orthograde root
Hygiene for the Dental Team [Video]. tus at increased risk for COVID-19 infection?
https://success.ada.org/en/practice-manage- canal treatment. J Endod 2018;44:543–548.
(epub ahead of print 11 March 2020). Lancet
ment/staff/hand-hygiene-for-the-dental- Respir Med doi: 10.1016/S2213- 67. Parirokh M, Torabinejad M, Dummer
team. Accessed 30 March 2020. 2600(20)30116-8. PMH. Mineral trioxide aggregate and other
39. The Lancet. COVID-19: protecting bioactive endodontic cements: an updated
52. US Food and Drug Administration. FDA overview - part I: vital pulp therapy. Int Endod
health-care workers. Lancet 2020;395:922. advises patients on use of non-steroidal anti- J 2018;51:177–205.
40. Centers for Disease Control and Preven- inflammatory drugs (NSAIDs) for COVID-19,
tion. Sequence for putting on personal pro- 19 March 2020. https://www.fda.gov/drugs/ 68. Cvek M. A clinical report on partial pul-
tective equipment (PPE). Atlanta: Centers for drug-safety-and-availability/fda-advises- potomy and capping with calcium hydroxide
Disease Control and Prevention, US Dept of patients-use-non-steroidal-anti-inflammatory- in permanent incisors with complicated
Health and Human Services; CS250672-E. drugs-nsaids-covid-19. Accessed 30 March crown fracture. J Endod 1978;4:232–237.
41. Centers for Disease Control and Preven- 2020. 69. Diangelis AJ, Andreasen JO, Ebeleseder
tion; Department of Health and Human 53. Elad S, Thierer T, Bitan M, Shapira MY, KA, et al. Guidelines for the management of
Services; National Institute for Occupational Meyerowitz C. A decision analysis: the dental traumatic dental injuries: 1. Fractures and
Safety and Health. How to Properly Put on management of patients prior to hematology luxations of permanent teeth. Pediatr Dent
and Take off a Disposable Respirator. cytotoxic therapy or hematopoietic stem cell 2017;39:401–411.
CS 207843; DHHS (NIOSH) Publication transplantation. Oral Oncol 2008;44:37–42. 70. Encyclopedia of Surgery. Definition:
No. 2010-133. 54. Chinese National Health Commission. Essential surgery. https://www.surgeryency-
42. Centers for Disease Control and Preven- Guideline for the Diagnosis and Treatment of clopedia.com/Ce-Fi/Essential-Surgery.html.
tion. Recommended Guidance for Extended Novel Coronavirus Pneumonia Accessed 30 March 2020.
Use and Limited Reuse of N95 Filtering (the 5th edition), 2020. [http://www.nhc.gov.
Facepiece Respirators in Healthcare Settings. cn/yzygj/s7653p/202002/3b09b894
https://www.cdc.gov/niosh/topics/hcwcon- ac9b4204a79db5b8912d4440.shtml].
trols/recommendedguidanceextuse.html. Accessed 30 March 2020.
Accessed 30 March 2020. 55. Widerman FH, Eames WB, Serene TP. The
physical and biologic properties of Cavit. J Am
Dent Assoc 1971;82:378–382.
428 QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020
Abramovitz et al
Itzhak Abramovitz Nurit Kot-Limon Member,r Department of Endodontics, Faculty
of Dental Medicine, Hebrew University-Hadassah School of Dental
Medicine, Jerusalem, Israel
Boaz Shay Clinic Manager,r Department of Endodontics, Faculty
of Dental Medicine, Hebrew University-Hadassah School of Dental
Medicine, Jerusalem, Israel
Antonia Kolokythas Chair, Oral and Maxillofacial Surgery, East-
man Institute for Oral Health, University of Rochester, Rochester,
NY, USA
Itzhak Abramovitz Chair, Department of Endodontics, Faculty
of Dental Medicine, Hebrew University-Hadassah School of Dental Galit Almoznino Senior Lecturer in Oral Medicine, Head, Big Bio-
Medicine, Jerusalem, Israel medical Data Research Laboratory, Hebrew University-Hadassah
School of Dental Medicine, Jerusalem, Israel; Head, Infection Pre-
Aaron Palmon Dean, Faculty of Dental Medicine, Hebrew Uni- vention and Control Committee, Hebrew University-Hadassah
versity-Hadassah School of Dental Medicine, Jerusalem, Israel School of Dental Medicine, Jerusalem, Israel; Consultant, Depart-
David Levy Medical Director and Quality Officer, Eastman Insti- ment of Endodontics, Faculty of Dental Medicine, Hebrew Univer-
tute for Oral Health, University of Rochester, Rochester, NY, USA sity-Hadassah School of Dental Medicine; Head, Orofacial Sensory,
Taste and Smell Clinic, Department of Oral Medicine Sedation &
Bekir Karabucak Chair, Department of Endodontics, School of Maxillofacial Imaging, Hebrew University-Hadassah School of Den-
Dental Medicine, University of Pennsylvania, PA, USA tal Medicine, Jerusalem, Israel.
Correspondence: Dr Galit Almoznino, Senior Clinical Lecturer, Specialist in Oral Medicine; Head, Big Biomedical Data Research Laboratory;
Head, Infection Prevention and Control Committee; Consultant, Department of Endodontics; Head, Orofacial Sensory, Taste and Smell
Clinic, Department of Oral Medicine Sedation & Maxillofacial Imaging, Hebrew University-Hadassah School of Dental Medicine, PO Box
12272, Jerusalem 91120, Israel. Email: galit@almoznino.com
QUINTESSENCE INTERNATIONAL | volume 51 • number 5 • May 2020 429
Copyright of Quintessence International is the property of Quintessence Publishing Company
Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv
without the copyright holder's express written permission. However, users may print,
download, or email articles for individual use.
You might also like
- Clinical Endodontic Management During The COVID-19 Pandemic: A Literature Review and Clinical RecommendationsDocument11 pagesClinical Endodontic Management During The COVID-19 Pandemic: A Literature Review and Clinical Recommendationsangel gudiyaNo ratings yet
- Apexa NO 8Document5 pagesApexa NO 8Apexa YadavNo ratings yet
- Running Title: Biosafety at The Dental Office After COVID-19Document16 pagesRunning Title: Biosafety at The Dental Office After COVID-19Karen IzquierdoNo ratings yet
- Impact of COVID 19 On Dentistry - by Group 9 HSDocument41 pagesImpact of COVID 19 On Dentistry - by Group 9 HSmilahelan999No ratings yet
- .Clinical Experience, Knowledge, Attitudes and Practice of Turkish Pediatric Dentists During The COVID-19 PandemicDocument23 pages.Clinical Experience, Knowledge, Attitudes and Practice of Turkish Pediatric Dentists During The COVID-19 PandemicMichael PomaNo ratings yet
- A Review of COVID-19 and The Implications For Orthodontic Provision in EnglandDocument8 pagesA Review of COVID-19 and The Implications For Orthodontic Provision in Englanddruzair007No ratings yet
- COVID-19: Present and Future Challenges For Dental Practice: Environmental Research and Public HealthDocument10 pagesCOVID-19: Present and Future Challenges For Dental Practice: Environmental Research and Public HealthFirda IzzatiNo ratings yet
- BulletinDocument16 pagesBulletindean qpNo ratings yet
- COVID-19 Int Guidance Summary PDFDocument2 pagesCOVID-19 Int Guidance Summary PDFShazeena QaiserNo ratings yet
- COVID-19 Int Guidance Summary PDFDocument2 pagesCOVID-19 Int Guidance Summary PDFJavier NicolaldeNo ratings yet
- Emergency Management in A Dental Clinic During TheDocument8 pagesEmergency Management in A Dental Clinic During TheAriska AndriyaniNo ratings yet
- Being A Dentist in The PandemicDocument2 pagesBeing A Dentist in The PandemicLarissa CostaNo ratings yet
- COVID-19 PublicationDocument8 pagesCOVID-19 PublicationMariam TariqNo ratings yet
- COVID-19's Impact On Private Practice and Academic Dentistry in North AmericaDocument4 pagesCOVID-19's Impact On Private Practice and Academic Dentistry in North AmericaJoDaNo ratings yet
- The Novel Coronavirus Pandemic: Challenges & Coping Strategies For Dental PractitionersDocument13 pagesThe Novel Coronavirus Pandemic: Challenges & Coping Strategies For Dental PractitionersHindol DasNo ratings yet
- 10 1017@dmp 2020 409Document13 pages10 1017@dmp 2020 409Manahil MaqboolNo ratings yet
- Could COVID-19 Change The Way We Manage Caries in Primary Teeth? Current Implications On Paediatric DentistryDocument3 pagesCould COVID-19 Change The Way We Manage Caries in Primary Teeth? Current Implications On Paediatric DentistryRatu Sarisyamsiah NurhaniNo ratings yet
- Chen-2020-Preventive and Control Measures ForDocument6 pagesChen-2020-Preventive and Control Measures ForJaime GonzalezNo ratings yet
- Resume LeafletDocument10 pagesResume LeafletYAALINY YKNo ratings yet
- DownloadDocument4 pagesDownloadSkAliHassanNo ratings yet
- Guidelines On The Prevention and Control of Disease in Dental Practice During The Coronavirus OutbreakDocument6 pagesGuidelines On The Prevention and Control of Disease in Dental Practice During The Coronavirus OutbreakrosminiNo ratings yet
- IFEA IES Endodontic and Dental Practice During COVID-19Document24 pagesIFEA IES Endodontic and Dental Practice During COVID-19Mohammed TarekNo ratings yet
- Approaches To The Management of Patients in Oral and Maxillofacial Surgery During COVID-19 PandemicDocument21 pagesApproaches To The Management of Patients in Oral and Maxillofacial Surgery During COVID-19 PandemicYahul MazfarNo ratings yet
- How Has Covid 19 Affected The Sector and Dental Health?Document5 pagesHow Has Covid 19 Affected The Sector and Dental Health?api-643791617No ratings yet
- 1 s2.0 S1991790220302890 MainDocument9 pages1 s2.0 S1991790220302890 MainBianca DimofteNo ratings yet
- Preventive Measures For Covid 19 in Dental TreatmentsDocument5 pagesPreventive Measures For Covid 19 in Dental Treatmentsbotak berjamaahNo ratings yet
- Covid and Dental Care UpdatedDocument49 pagesCovid and Dental Care UpdatedShubham PatelNo ratings yet
- Pediatric Oral Health During and After The COVID-19 PandemicDocument18 pagesPediatric Oral Health During and After The COVID-19 PandemicRatu Sarisyamsiah NurhaniNo ratings yet
- Seba Saqer - 20180482 Puplic HealthDocument10 pagesSeba Saqer - 20180482 Puplic HealthSaba SaqerNo ratings yet
- Üstün2021 Article InfluenceOfCOVID-19PandemicOnP - Pedo MakalesiDocument7 pagesÜstün2021 Article InfluenceOfCOVID-19PandemicOnP - Pedo MakalesiDerya İçözNo ratings yet
- Redefining Dental Practice During and Post-COVID-19 Era: A ReviewDocument9 pagesRedefining Dental Practice During and Post-COVID-19 Era: A Reviewapridey parinding08No ratings yet
- Review Article: COVID-19 Pandemic and Dental PracticeDocument5 pagesReview Article: COVID-19 Pandemic and Dental PracticeArevamadeline AegesfiNo ratings yet
- Sustainable Practice of Ophthalmology During COVID-19: Challenges and SolutionsDocument10 pagesSustainable Practice of Ophthalmology During COVID-19: Challenges and SolutionsAdhilSharmaNo ratings yet
- Dental Care and Personal Protective Measures For Dentists and Non-Dental Health Care WorkersDocument5 pagesDental Care and Personal Protective Measures For Dentists and Non-Dental Health Care WorkersKalpanaNo ratings yet
- ADA Interim Guidance For Minimizing Risk of COVID-19 TransmissionDocument8 pagesADA Interim Guidance For Minimizing Risk of COVID-19 TransmissionOTNo ratings yet
- ADA Interim Guidance For Minimizing Risk of COVID-19 TransmissionDocument8 pagesADA Interim Guidance For Minimizing Risk of COVID-19 TransmissionMaria Paula Vanegas ForeroNo ratings yet
- ADA COVID Int Guidance Treat Pts PDFDocument8 pagesADA COVID Int Guidance Treat Pts PDFJavier NicolaldeNo ratings yet
- ADA COVID Int Guidance Treat Pts PDFDocument8 pagesADA COVID Int Guidance Treat Pts PDFFavio LunaNo ratings yet
- ADA Interim Guidance For Minimizing Risk of COVID-19 TransmissionDocument8 pagesADA Interim Guidance For Minimizing Risk of COVID-19 TransmissionprasaddenNo ratings yet
- ADA COVID Int Guidance Treat Pts 2 PDFDocument8 pagesADA COVID Int Guidance Treat Pts 2 PDFAnil SukumaranNo ratings yet
- The Impact of COVID-19 On Oral and Maxillofacial Surgery Patient Presentations To The Emergency Department - A West of Ireland ExperienceDocument5 pagesThe Impact of COVID-19 On Oral and Maxillofacial Surgery Patient Presentations To The Emergency Department - A West of Ireland ExperienceYuzketNo ratings yet
- Dentistry and Coronavirus (COVID-19) - Moral Decision-MakingDocument3 pagesDentistry and Coronavirus (COVID-19) - Moral Decision-MakingOTNo ratings yet
- Jurnal Ortho 4Document5 pagesJurnal Ortho 4Santika IndahsariNo ratings yet
- Kwak 2020Document4 pagesKwak 2020alyssaNo ratings yet
- 2020 Article 1361-2Document3 pages2020 Article 1361-2Maria Alejandra AconchaNo ratings yet
- Infection Control Measures in Pediatric Dental Practice During Covid - 19 - A Review ArticleDocument5 pagesInfection Control Measures in Pediatric Dental Practice During Covid - 19 - A Review ArticleInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jurnal 3Document8 pagesJurnal 3Febri YolandaNo ratings yet
- 10 1111@ipd 12690Document7 pages10 1111@ipd 12690Tiara HapkaNo ratings yet
- Dental Settings: Key ConceptsDocument7 pagesDental Settings: Key ConceptsVigneshvar SreekanthNo ratings yet
- Guidance On The Use of Personal Protective Equipment Ppe in Hospitals During The Covid 19 OutbreakDocument9 pagesGuidance On The Use of Personal Protective Equipment Ppe in Hospitals During The Covid 19 OutbreakGerlan Madrid MingoNo ratings yet
- Safety Covid TraquesDocument19 pagesSafety Covid TraquesKenjiNo ratings yet
- Jopr 13261Document14 pagesJopr 13261Vineela ChowdaryNo ratings yet
- COVID 19 Guideline (Draft) of Bangladesh Dental Society: MethodDocument20 pagesCOVID 19 Guideline (Draft) of Bangladesh Dental Society: MethodMax FerNo ratings yet
- Dental Considerations After The Outbreak of 2019 Novel Coronavirus Disease: A Review of LiteratureDocument7 pagesDental Considerations After The Outbreak of 2019 Novel Coronavirus Disease: A Review of Literatureharshita parasharNo ratings yet
- Journal of Prosthodontics - 2020 - Ashtiani - Reducing The Risk of COVID 19 Transmission in Dental Offices A ReviewDocument7 pagesJournal of Prosthodontics - 2020 - Ashtiani - Reducing The Risk of COVID 19 Transmission in Dental Offices A ReviewDanaNo ratings yet
- Pandemic Preparedness of Dentists Against Coronavirus Disease: A Saudi Arabian ExperienceDocument13 pagesPandemic Preparedness of Dentists Against Coronavirus Disease: A Saudi Arabian ExperiencenoviNo ratings yet
- Impact of COVID-19 On Oral Emergency Services: Scientific Research ReportDocument55 pagesImpact of COVID-19 On Oral Emergency Services: Scientific Research ReportgeometrydashyioNo ratings yet
- IntJOralHealthDent 6 2 122 125Document5 pagesIntJOralHealthDent 6 2 122 125Laura Putri TraviraNo ratings yet
- OtorhinolaryngologyDocument8 pagesOtorhinolaryngologydrian pamungkasNo ratings yet
- Pandemic Populism: An Analysis of Populist Leaders' Responses To Covid-19Document16 pagesPandemic Populism: An Analysis of Populist Leaders' Responses To Covid-19john3963No ratings yet
- PPE-Conducted Partnership Appreciation and Other School Based Initiatives NarrativeDocument2 pagesPPE-Conducted Partnership Appreciation and Other School Based Initiatives NarrativeCarlz BrianNo ratings yet
- How COVID Is Reshaping Global Policy and What It Means For Market AccessDocument21 pagesHow COVID Is Reshaping Global Policy and What It Means For Market AccessMarti Aroa FamilyNo ratings yet
- HEALTH-GROUP MEDICLAIM June 2021Document61 pagesHEALTH-GROUP MEDICLAIM June 2021Kishore mohan ManapuramNo ratings yet
- PRESIDENT Magufuli SPEECH IN SADC REVISEDDocument8 pagesPRESIDENT Magufuli SPEECH IN SADC REVISEDPeter Msandae HongoaNo ratings yet
- Julia FuscoDocument6 pagesJulia FuscoNatália FuscoNo ratings yet
- 1628 6995 3 PBDocument32 pages1628 6995 3 PBPelayanan Tahanan Rutan KendariNo ratings yet
- Project ProposalDocument7 pagesProject ProposalAirishDiazNo ratings yet
- Published Benefits of Ivermectin Use in Itajaí, Brazil For COVID-19Document19 pagesPublished Benefits of Ivermectin Use in Itajaí, Brazil For COVID-19Ana Carolina Pecanha Antonio AantonioNo ratings yet
- Town of Smithers 2022-2027 Tourism Strategic Plan - V2-1 PDFDocument28 pagesTown of Smithers 2022-2027 Tourism Strategic Plan - V2-1 PDFSufianNo ratings yet
- Eaesp - Prova Objetiva - Bloco 3 - Ingles - Português + GabaritoDocument20 pagesEaesp - Prova Objetiva - Bloco 3 - Ingles - Português + GabaritojairosabinoNo ratings yet
- Akk Jurnal Internasional 1Document7 pagesAkk Jurnal Internasional 1Onnii SltrNo ratings yet
- Covid-19 in Today's EconomyDocument1 pageCovid-19 in Today's EconomyKılıç KöçeriNo ratings yet
- The Mathematics Instruction in Rural Area During The Pandemic Era: Problems and SolutionsDocument13 pagesThe Mathematics Instruction in Rural Area During The Pandemic Era: Problems and SolutionsJe-Ann LugpitNo ratings yet
- English: Quarter 1 - Module 1 Noting Context CluesDocument19 pagesEnglish: Quarter 1 - Module 1 Noting Context CluesFriah Mae Delgado100% (2)
- Health and Travel Alert Updated Travel RequirementsDocument3 pagesHealth and Travel Alert Updated Travel RequirementsShani Mur.No ratings yet
- Dr. Peter McCullough's COVID-19 and Anti-Vaccine Theories - Detecting DesignDocument48 pagesDr. Peter McCullough's COVID-19 and Anti-Vaccine Theories - Detecting DesignMassimo RiserboNo ratings yet
- Barangay Peacekeeping Action Team On Covid-19 Response An AnalysisDocument8 pagesBarangay Peacekeeping Action Team On Covid-19 Response An AnalysisInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Tutorial 3 Ihs113Document5 pagesTutorial 3 Ihs113Laila RahmatNo ratings yet
- Jasmine Gabiana (Introduction)Document2 pagesJasmine Gabiana (Introduction)Jasmine GabianaNo ratings yet
- ALNAP Paper - Getting Remote M&E RightDocument37 pagesALNAP Paper - Getting Remote M&E RightShahid NadeemNo ratings yet
- Impact of Covid 19 Mental Health SynopsisDocument7 pagesImpact of Covid 19 Mental Health SynopsisNikita ChaubeNo ratings yet
- Hospital and Healthcare Industry AnalysisDocument4 pagesHospital and Healthcare Industry Analysisvinay_814585077No ratings yet
- Group 6 - CristobalDocument17 pagesGroup 6 - CristobalRj JutingoNo ratings yet
- PT Ramzy Cahaya KaryaDocument1 pagePT Ramzy Cahaya KaryaYafieNo ratings yet
- MDLZ HRDD and Modern Slavery Report 2021Document25 pagesMDLZ HRDD and Modern Slavery Report 2021ComunicarSe-ArchivoNo ratings yet
- Assignment ECW 445 (Mar 2020 - July 2020) (CO1-PO7)Document2 pagesAssignment ECW 445 (Mar 2020 - July 2020) (CO1-PO7)muiz azihNo ratings yet
- SocSci 10 - GAYTA - PETER JOSHUA F. - MODULE 1&2Document22 pagesSocSci 10 - GAYTA - PETER JOSHUA F. - MODULE 1&2Peter gaytaNo ratings yet
- Act4 Ucsp Alissa JularbalDocument4 pagesAct4 Ucsp Alissa JularbalAlissa MayNo ratings yet
- COV19 Impact On Hotel ChinaDocument11 pagesCOV19 Impact On Hotel ChinaAmrezaa IskandarNo ratings yet