Professional Documents
Culture Documents
Calcium, Phosphate and Magnesium Metabolism (Self-Note)
Calcium, Phosphate and Magnesium Metabolism (Self-Note)
Uploaded by
Raja RuzannaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Calcium, Phosphate and Magnesium Metabolism (Self-Note)
Calcium, Phosphate and Magnesium Metabolism (Self-Note)
Uploaded by
Raja RuzannaCopyright:
Available Formats
Calcium
Most abundant mineral
Total= 1kg (22 500mmol)
99% in the bone
0.1% in ECF = 22.5mmol
= 9 mmol in plasma + 16 mmol in intracellular
In bone:
Calcium moves between bone and ECF
~500 mmol/24 hours
In kidneys:
Filtered in kidney = 240mmol/24h
Reabsorbed in the tubules = 234 mmol/24h
Excretion in urine = 6 mmol/24h
In GIT:
Calcium in food: 25mmol/25h
Calcium in GIT secretion: 6mmol/24h
Calcium excretion in faeces: 19mmol/24 hours
GIT reabsorb calcium in secretion + food
Calcium loss:
0.3mmol (skin) + 19mmol (faeces) + 6 mmol (urine) = 25mmol
Calcium requirement: 12.5mmol/24 hours
Function of calcium
Structural
• Bone
• Teeth
Neuromuscular
• Control of excitability
• Release of neurotransmitter
• Initiate muscle contraction
Enzymic
• Co-factor for coagulation factors
Signalling
• Intracellular second messenger
Bone
• Osteoid (collagenous matrix) + calcium salt ( hydroxyapatite)
• Remodelling = Resorption (osteoclast) + Formation (osteoblast)
• Formation = Osteoid synthesis + calcium + phosphate (hydroxyapatite)
• Phosphate: released from pyrophosphate
• Mediated by alkaline phosphatase
• Alkaline phosphatase released by osteoblast
• Bone is a reservoir: calcium, phosphate, magnesium, sodium
Plasma calcium
Distribution of calcium in plasma
Total calcium: 2.25-2.6 mmol/L
= diffusible 54% + non diffusible 46%
= (free 47% + complexed 7%) + non diffusible 46%
Non diffusible: protein bound
Free: physiologically active
maintained by homeostatic mechanism
Complexed: with citrate and phosphate, bicarbonate, lactate
Alkalosis: Increased calcium binding to albumin
Increased calcium complex
-> reduced physiologically active calcium (total calcium still normal)
-> clinical sign of hypocalcaemia
Acidosis : Calcium has to compete with H+ for albumin
Reduced calcium binding to albumin
Reduced calcium complex
-> increased physiologically active calcium
-> signs of hypercalcaemia
Plasma albumin:
Affect total calcium concentration (regardless ionized calcium concentration)
Corrected calcium corrected for hypoalbuminaemia
= Total calcium (measured) + (Normal albumin , assumed to be 4.4 which is normal - Patient's albumin) x 0.8
Analytical technique:
• Total calcium
• Measurement include protein bound and ionized calcium
• Easier to measure
• Affected by albumin level
• Although calcium binds to other protein, only albumin is clinically significant
• Thus, eg; hypogammaglobulinemia unlikely to alter total calcium level
• Ionized calcium can be measure too
Method for total calcium measurement:
• Colorimetric analysis with metallochromic indicator
◦Metallochromic indicator or dyes bind calcium and forms color complex
◦Ca ions are released when exposed to acids
◦Released ion binds to chelating agent eg: arsenzo III
◦Measure absorbance at 650nm
◦Concentration of Ca-dye complex determined from Beer's Law
• Atomic absorption spectrometry (AAS)
◦reference method
• Indirect potentiometry
◦ISE method
◦Add acid to Ca to release from albumin
◦Total calcium measured voltametrically
◦Ionized calcium: direct measurement (no need acid treatment)
Calcium-Regulating Hormones
• Parathyroid hormone
• Calcitriol
• Calcitonin (minimal)
Parathyroid hormone
• Polypeptide hormone
• Synthesised from larger precursor (inactive)
• Forms active PTH in the plasma
• Synthesised in the Parathyroid glands chief cells
• Half-life: 3-4 min
• Metabolised in the liver and kidneys
Stimulation of PTH release
• Reduced ionised Ca
• Mild hypomagnesemia
• Low calcitriol
Inhibition of PTH release
• Hypercalcaemia
• Severe hypomagnesemia
• Increased calcitriol
PTH not affected by phosphate concentration
In the absence of adequate calcitriol, there is resistance to the calcium mobilizing effect of PTH
Action of PTH
• Increase Ca, reduce phosphate
• Bone
◦Mobilize calcium from bone
◦Osteoclast cause bone resorption
• Kidneys
◦Increase reabsorption of filtered calcium
‣ Increase bone resorption causing increased ca
‣ Despite increased reabsorption, may still cause hypercalciuria
◦Decreasing reabsorption of phosphate
‣ Causing phosphaturia, reduced plasma phosphate
◦Decrease reabsorption of bicarbonate
‣ Causing acidosis
◦Stimulate formation of calcitriol
‣ Increase calcium and phosphate absorption from the gut
‣ Increase ostoclastic resorption (in high concentration)
‣ Promotes bone mineralization (in low concentration)
Analytical technique
• Sandwich Immunoassay, detection via IRMA (radioactive-labelled) or CMIA (chemiluminescent-labelled)
• Cons: lack of specificity, may detect inactive fragments
Calcitriol
• Is a vitamin D, steroid hormone
• 7 dehydrocholesterol in skin + sunlight -> precalciferol
• Precalciferol to liver and hydroxylated (25-hydroxylation) to cholecalciferol
• Cholecalciferol to kidney and hydroxylated (1α-hydroxylation) to 1,25-
dihydrocalciferol
Stimulation of calcitriol synthesis
• high PTH
• Low phosphate
• Low calcium
• Calcitonin
• Oestrogen
• Cytokines
• Interferon
Inhibition of calcitriol synthesis
• low PTH
• High phosphate
• High FGF32
• High calcitriol
• Leptin
• Ascorbic acids
When Calcitriol synthsis is inhibited, Cholecalciferol will be hydroxylated into
• 24,25-dihydrocalciferol
• 1,24,25-dihydrocalciferol
These are inactive form of calcitriol
Action of calcitriol
• Synthesise calbindin D (Ca carrier protein) to increase GIT calcium and phosphate absorption
• Bind to osteoblast to release ALP (ALP release phosphate from pyrophosphate for bone mineralization)
• Stimulate osteoblast to release osteocalcin to increase bone mineralization
• Increase bone resorption (at high level)
• Enhance effect of PTH in renal tubules (for reabsorption of Ca)
• Others: Reduce osteoporosis, anti-tumour growth activity
Analytical methods
• HUKM: detect 25-hydrocalciferol via sandwich immunoassay (RIA or CMIA)
◦Longer half-life (2-3 weeks)
◦Reduced fluctuation with sunlight and dietary intake
◦Larger concentration
◦Easier to measure
• Reference method: Dual mass spectometry
Calcitonin
• Peptide hormone
• Produced from C-cell of the thyroid
Action
• Inhibit bone resorption
• Increase calcium uptake from the gut
-> increase calcium without loss of mineral from bone
Analytical method
• Sandwich Immunoassay, detection via IRMA (radioactive-labelled) or CMIA (chemiluminescent-labelled)
Fibroblast growth factor 23 (FGF23)
• Produced by osteocytes
• Causes increase phosphate loss
Stimulation of FGF23 synthesis
• High calcitriol
• High phosphate
Action
• inhibit Na-Po4 cotransporter -> reduced reabsorption of Na and PO4
• Inhibit 1α-hydoxylase -> reduced calcitriol -> reduced GIT absorption of calcium and phosphate
FGF23 Mutation
• Hypophosphatemia + osteomalacia
Calcium Homeostasis
Low Calcium stimulates PTH secretion
Increase bone resorption
Increase calcitriol ️ increase gut reabsorption of calcium and phosphate
️increase bone mineralization
Increase reabsorption of calcium from kidney ️ hypercalciuria
Decrease phosphate reabsorption in kidney ️phosphaturia
Phosphate homeostasis
Hypophosphatemia
increase calcitriol release ️ stimulate calcium absorption from the gut ️ excess calcium excreted in urine
️ ️stimulate phosphate absorption from the gut
inhibit FGF23 release
loss of inhibition of Na-Po4 cotransporter in the kidneys
increase PO4 reabsorption
Disorder of Calcium, Phosphate and Magnesium Metabolism
Hypercalcaemia
Causes Clinical Features
• most common is
◦Primary hyperthyroidism
◦Malignancy
• usually asymptomatic
Malignant Disease
• usually symptomatic
️Metastatic
️no relationship between bone metastasis with severity/presence of hypercalcaemia
️can be due to humoral factors eg: growth factors, prostaglandins and osteoclast-activating
cytokines
️Non-metastic ️ due to secretion of PTH-related peptide (PTHrP)
Primary hyperparathyrodism
• 1 in 1000
• occur at any age
• most common in postmenopausal women
• Commonly due to
◦Parathyroid adenoma, may be due to MEN
◦Diffuse parathyroid hyperplasia
◦Parathyroid carcinoma, rare
• Complications
◦osteoporosis
◦renal impairment
◦renal calculi
• Diagnosis
◦to localize tumour (adenoma is usually not palpable)
‣ 99mTc-Sestamibi scanning
‣ Measurement of PTH via selective jugular cannulation
◦Measurement of PTH to confirm sucessful resection
◦Lab investigations:
• Treatment:
◦Definitive: surgical removal
◦Indication for surgery
‣ Symptomatic patients
‣ Ca >2.85mmol/L
‣ Evidence of decrease bone density
‣ eGFR <60mL/min/1.73m2
‣ Young patient <50yo
◦Asymptomatic: reassessment of complications, high fluid intake
Secondary Hyperparathyroidism
• Resistance to the metabolic actions of PTH
• Eg: Renal failure, Vitamin D deficiency, pseudohypoparathyroidism
• Renal failure
◦Reduced GFR ️decrease PO4 excreation
◦Reduced calcitriol ️ reduced action of PTH for bone resorption ️ hypocalcaemia
️ reduced GIT absorption of calcium ️ hypocalcaemia
◦Reduced renal excreation of PTH, increased secretion of PTH
increased PTH level
Parathyroid gland hyperplasia (chronic parathyroid stimulation)
initially low calcium, hyperphosphatemia
severe hyperparathyrodism cause hypercalcaemia and hyperphosphatemia
➡ ➡
Tertiary Hyperparathyroidism
• Autonomous hyperparathyroidism
• Due to chronic parathyroid stimulation
• Renal failure causing inability to correct hypocalcaemia ️chronic PTH stimulation ️PTH hyperplasia
️Autonomous PTH secretion
• Transplanted kidney causing normal calcitriol production ️ PTH effect manifested as hypercalcaemia
Thyrotoxicosis
• d/t increased osteoclastic activity ️ osteoporosis and hypercalcaemia
➡
Excessive Vitamin D
▶
• increased GIT absorption of calcium
• Enhanced bone resorption
• Hypercalciuria
▶
• Symptoms: weakness, irritability, nausea, vomiting, diarrhea, soft tissue calcification
• Synptoms may persists for years d/t adipose tissue storage of Vit D
• Dx; measurement of 25(OH)D
• Rx: steroid
Granulomatous disorders
• eg: Sarcoidosis, Tuberculosis, Coccidiodomycosis, silicone-induced granuloma
➡
• Due to:
◦1α-hydroxylation of 25-hydroxycholecalciferol by macrophages in the sarcoid granuloma
◦increased sensitivity to Vit D
Milk-alkali Syndrome
• ingestion of milk/antacid
• Alkali increases calcium reabsorption
• Symptoms: Hypercalcaemia, hypocalciuria, alkalosis, azotemia, soft tissue calcification
Thiazide diuretic
• Increase calcium reabsorption
Lithium therapy
• Increased PTH secretion
Acute Adrenal Failure
• d/t sudden fall in cortisol causing plasma volume contraction
Immobilization
• Bone resorption without bone formation ️ hypercalciuria
Familial Hypocalciuric Hypercalcaemia
• autosomal dominant
• mutation in the CaSR gene ️ increase in PTH
• asymptomatic, benign
• present throughout life
• DX: relative hypocalciuria to the degree of hypercalcaemia
◦Familial Hypocalciuric Hypercalcaemia : Calcium clearance: Creatinine clearance = <0.01
◦Primary Hyperparathyroidism : >0.02
Investigation
HYPOCALCAEMIA
CLINICAL FEATURES
• Behavioural disturbance
• Stupor
• Numbness and paraesthesia
• Carpopedal spasm
• Tetany, convulsion
• Laryngeal spasm
• Respiratory arrest
• Cataracts (chronic hypocalcaemia)
• Basal ganglia calcifications (chronic hypocalcaemia)
• Positive Trosseau sign
• Positive Chvostek sign
• Prolonged QT
• Low voltage T wave (repolarization)
CAUSES OF HYPOCALCAEMIA
Associated with low PTH
• Post surgical removal thyroid/parathyroid
• Low Mg++
• Hypoparathyroidism
• Hungry bone syndrome
• Inherited disorders
Associated with high PTH level
• ESRF
• Vitamin D deficiency
◦Dietary
◦Malabsorption
◦Inadequate exposure to UV light
• Disorder of Vitamin D metabolism
◦ESRF
◦Lithium therapy
◦1α-hydroxylase deficiency
◦Vitamin D resistance
• Pseudohypoparathyroidism
• Acute pancreatitis
• Hyperphosphatemia
• Massive transfusion with citrated blood
• Acute rhabdomyolysis
Artefactual
• Blood collected from EDTA tube
Others
• Critically ill patients with sepsis, burns and acute renal failure
• Drugs: Heparin, glucagon, protamine (transient)
Hypoparathroidism
• Can be
◦Inherited : DiGeorge, thymic aplasia
◦Acquired: idiopathic, autoimmune, surgery, haemochromatosis, infiltrative condition
• low PTH ️ low calcium high phosphate
• usually have low calcitriol too ️ low GIT reabsorption
Pseudohypoparathyroidism (Albright's Osteodystrophy)
• ineffective PTH
• Two types
➡ ➡
◦Type 1: PTH binds to receptor ️ defective activation of adenyl cyclase ️ no cAMP formed
◦Type 2: PTH binds to receptor adenyl cyclase formed ️ cAMP formed ️ response is blocked
➡
• Clinical features
◦Extraosseous calcifications
◦Rounded face
◦Short stature
◦Shortening of 4th and 5th metacarpals/ metatarsals
◦Learning difficulty
◦Extrapyramidal symptoms : choreoathetotic movement, dystonia
◦Increased ICP, papilloedema
◦Lenticular cataracts
• Lab investigations
◦High PTH
➡
◦Low calcium
◦PTH infusion:
‣ Type 1: low cAMP
➡ ➡
‣ Type 2 or normal people : high cAMP
Hypomagnesemia
• causes deficiency of PTH and impaired responsiveness to PTH
Vitamin D Deficiency
• Can be due to inadequate intake, inadequate synthesis (enzyme x cukup, malabsorption
• Causes
◦Adults: Osteomalacia
◦Childrens: Rickets
• Low vit D ️low calcitriol ️ reduced calcium and phosphate absorption from GIT hypocalcaemia
secondary hyperparathyroidism hypophosphatemia increased ALP
• Lab ix:
◦Hypocalcaemia
◦Hypophosphatemia
◦Increased ALP
◦High PTH
Impaired Vitamin D Metabolism
• Phenobarbital treatment, phenytoin
◦Induce hepatic microsomal hydroxylating enzymes alter vitamin D metabolism in the liver
◦Directly inhibit intestinal calcium absorption
• Chronic liver disease, Primary Biliary Cirrhosis
◦Hypocalcaemia, metabolic bone disease
◦Mechanism:
‣ Malabsorption of vit D
‣ Decreased 25-hydroxylation in the liver
‣ Decreased synthesis of vitamin d binding protein
Hungry Bone Syndrome
• Hyperparathyroidism increased bone resorption hypercalcaemia
surgical removal of parathyroid
➡ ➡
️
rapid intake of calcium by the bone
️
⬇
hypocalcaemia (often severe and symptomatic)
• must be anticipated, give calcium and vit D before surgery
HYPERPHOSPHATEMIA
CLINICAL FEATURES
• No direct symptoms
• If chronic, enhanced mineralization
◦Inhibit 1α-hydroxylation in the kidneys
◦Phosphate + Calcium = Ectopic calcifications
• Most common in ESRF supplemented with vitamin D
MECHANISM
• Increased extracellular load due to transcellular shift
eg: acidosis
• Increased tubular reabsorption
eg: hypoparathyroidism, pseudohypoparathyroidism
• Increased extracellular load
Eg: rhabdomyolysis. Intravascular hemolysis, leukaemia,
lymphoma, cytotoxic therapy, tumour lysis syndrome
• secondary to increased vitamin D
Eg: granulomatous disease ie: Sarcoidosis
MANAGEMENT
• Treat underlying cause
• Phosphate binder
◦Usually calcium salt eg: CaCO3
◦Reduce GIT absorption
Phosphate pyramid
HYPOPHOSPHATEMIA
CLINICAL FEATURES
• Symptomatic only in severe cases (<0.3mmol/L)
◦Proximal weakness
◦Anorexia
◦Dizziness
◦Myopathy
◦Dysphagia
◦Ileus
◦Respiratory failure d/t respiratory muscle weakness
◦Impairment of cardiac contractility due to ATP
depletion
◦Metabolic encephalopathy
MECHANISMS
• Shift in PO4 from extracellular fluid into cells
◦acute respiratory alkalosis,
◦salicylate poisoning
◦alcohol withdrawal
◦heatstroke
◦hepatic coma
◦increase insulin during glucose administration
◦recovery from DKA
◦refeeding in malnourished patients
• Increased urinary excretion
◦Usually secondary to hyperparathyroidism
◦Renal tubular defects eg: Fanconi's syndrome, Familial Hypophosphatemia
◦X-linked vitamin D-resistant rickets
◦Aldosteronisms
◦Glucocorticoid and Mineralocorticoid administration
◦Diuretic therapy
• Increase urinary loss
◦Osmotic diuresis
◦Acute volume expansion
◦Malignant neoplasm eg leukaemia and lymphoma
• Decrease intake/absorption
◦Vomiting
◦Diarrhea
◦Phosphate binding antacids
◦Malabsorption
◦Vitamin D deficiency ->reduce calcitriol for absorption
◦Steatorrhea
• Oncogenic hypophosphatemia with osteomalacia
◦Hyperphosphaturia via activation of FGF23
MANAGEMENT
• Give PO4 (enteral or IV)
◦Dont give in oliguric and hypercalcaemic
MAGNESIUM
• Normal: 0.7-1.0 mmol/L
• Daily intake: 8 mmol/24 hours
• Some bind to albumin
ACTION
• Co-factor for enzymes
• Maintenence of ribosome, nucleic acid, proteins
• affect permeability of excitable membranes
HYPERMAGNESEMIA
DEFINITION
• Se Mg2++ >0.9mmol/L
CLINICAL FEATURES
• 2.5-5.0 mmol/L : affect cardiac conduction, bradycardia,
respiratory depression, depressed mental status
• >7.5 mmol/L : Respiratory paralysis and cardiac arrest
• 3.0-4.0 mmol/L: Induced hypermagnesemia in
bronchospasm and eclampsia
CAUSES
• Renal insuffiuciency
• Bowel disorder
MANAGEMENT
• IV Calcium
• Dialysis
HYPOMAGNESEMIA
DEFINITION
• Se Mg <0.5mmol/L
CLINICAL FEATURES
• Usually associated with hypocalcaemia
• Hypomagnesemia causes low PTH ️ hypocalcaemia
◦Neuromuscular excitability: Carpopedal spasm, seizure, muscular weakness
◦Depression, psychosis
◦Metabolic abnormalities: Carbohydrate intolerence, hyperinsulinism
◦Cardiac arrhythmia
MECHANISM
• Loss of Mg fro GIT
◦Diarrhoea
◦Malabsorption
◦Steatorrhea
◦Bowel resection
◦IEM ; primary intestinal hypomagnesemia
• Urinary loss
◦Thiazide and loop diuretics
➡
◦Na resorption in kidneys: via Na-dependent magnesium efflux pathway in kidney
◦Volume expansion
◦Hypercalcemia and hypercalciuria
◦Nephrotoxic drugs
◦Diabetes mellitus: Glycosuria and osmotic diuresis
• Others:
◦Alcoholism
◦Sustained and extensive stress
BIOCHEMICAL MARKERS OF BONE REMODELLING
• Starts with bone resorption by osteoclast ️ formation of new bone by osteoblast
• Resorption > formation = Net bone loss ️ osteoporotic fracture
DIAGNOSTIC PROCEDURE TO MONITOR BONE TURNOVER
• Imaging technique
➡
• Bone biopsy
• Biochemical markers of bone turnover
➡
Imaging technique
Eg: bone density measurement
• Pros:
◦Non-invasive
• Cons:
◦ Difficult to detect early stages/ acute changes
◦Does not define abnormal distribution of bone loss
Bone biopsy
• Pros:
◦Define the distribution of bone mass
• Cons:
◦Invasive
◦Cannot provide ideas of the long and slowly developing process
Biochemical markers
• Conventional markers: less sensitive
◦Osteopotosis: Calcium and PTH will be normal due to minute changes over time
• Bone turnover markers:
◦Pros:
‣ More sensitive to subtle changes
‣ Noninvasive
‣ Can detect and monitor progression
BONE TURNOVER MARKERS
BONE RESORPTION MARKERS
• Bone tissue:
◦Organic matrix (osteoid)
◦Bone mineral
◦Bone cells
• Bone resorption markers
◦quantify:
‣ Constituent of bone matrix : calcium
‣ Collagen degradation products : hydrpoxyproline, pyridinium cross-links, telopeptides
‣ Cellular products from mineralized matrix degradation : TRAP
‣ Others: cathepsin K
‣ Bone metaboplism regulator: RANK, RANKL,osteoprotegerin
◦Has a diurnal rhythm, highest in the morning
BONE FORMATION MARKERS
• ALP
• Products of bone matrix synthesis
◦Osteocalcin
◦Procollagen Type 1 N-terminal and C-Terminal peptides
You might also like
- Invention and Evolution Design in Nature and EngineeringDocument387 pagesInvention and Evolution Design in Nature and Engineeringphucborso1100% (1)
- Calcium, Phosphate and MagnesiumDocument46 pagesCalcium, Phosphate and Magnesiumkiedd_04100% (3)
- Calcium and PhosphateDocument49 pagesCalcium and Phosphatehaidernadhem57No ratings yet
- What Is The Most Abundant Mineral in The Body?Document33 pagesWhat Is The Most Abundant Mineral in The Body?Niño Española BenedictoNo ratings yet
- Calcium and PhosphateDocument35 pagesCalcium and PhosphateSULEIMAN OMARNo ratings yet
- Endo Lect - ParathyroidDocument25 pagesEndo Lect - ParathyroiddoctorrfarrukhNo ratings yet
- Calcium and Phosphate Metabolism 1Document14 pagesCalcium and Phosphate Metabolism 1samueltoluwabori360No ratings yet
- Parathyroid: Calcium and Vitamin DDocument135 pagesParathyroid: Calcium and Vitamin DPhysiology by Dr Raghuveer100% (1)
- Calcium HomeostasisDocument38 pagesCalcium Homeostasiskelvinmaina9993No ratings yet
- Drugs Affecting Calcium Balance: Harsh Vinayak Roll No. 39 Mbbs 2 Yr Student BATCH 2019 Rdasmc, AyodhyaDocument24 pagesDrugs Affecting Calcium Balance: Harsh Vinayak Roll No. 39 Mbbs 2 Yr Student BATCH 2019 Rdasmc, AyodhyaA2Z GyanNo ratings yet
- 27 - Hypo and Hypernatremia - and Hypo and Hyperkalieama PDFDocument48 pages27 - Hypo and Hypernatremia - and Hypo and Hyperkalieama PDFEITHAR OmarNo ratings yet
- Calcium MetabolismDocument19 pagesCalcium MetabolismShabariNath R NairNo ratings yet
- Lect 9 Parathyroid Gland-1Document30 pagesLect 9 Parathyroid Gland-1warda farooqNo ratings yet
- Learning Objectives Biochemistry of BonesDocument7 pagesLearning Objectives Biochemistry of BonesRaissa GabriellaNo ratings yet
- Calcium MetabolismDocument51 pagesCalcium MetabolismAlan ThomasNo ratings yet
- Regulation of Calcium Parathyroid, Vitamin D & CalcitoninDocument29 pagesRegulation of Calcium Parathyroid, Vitamin D & CalcitoninJessica StewartNo ratings yet
- Calcium, Phos, MGDocument27 pagesCalcium, Phos, MGRiya AktarNo ratings yet
- Renal & Electrolyted Physiology FinalDocument21 pagesRenal & Electrolyted Physiology FinalVondNo ratings yet
- Calcium Phosphorus Metabolic DisordersDocument102 pagesCalcium Phosphorus Metabolic DisordersAME DENTAL COLLEGE RAICHUR, KARNATAKANo ratings yet
- Parathyroid HormonesDocument104 pagesParathyroid Hormonesc96gtf8hkkNo ratings yet
- Calcium HomeostasisDocument37 pagesCalcium Homeostasispolog.jm610No ratings yet
- Calcium Metabolism and Disorders (Hanan)Document169 pagesCalcium Metabolism and Disorders (Hanan)drhananfathyNo ratings yet
- Calcium Balance I 2020Document35 pagesCalcium Balance I 2020Nadun MethwadaneNo ratings yet
- Calcium Metabolism: Presented By-Dr. Chinansha Arya Second Year Postgraduate Department of Conservative and EndodonticsDocument103 pagesCalcium Metabolism: Presented By-Dr. Chinansha Arya Second Year Postgraduate Department of Conservative and EndodonticsmeghaNo ratings yet
- Chapter X - Mechanism of Protein MetabolismDocument30 pagesChapter X - Mechanism of Protein MetabolismAngelo AngelesNo ratings yet
- Calcium and PhosporusDocument29 pagesCalcium and PhosporusJoe AjibadeNo ratings yet
- Carbohydrate MetabolismDocument30 pagesCarbohydrate MetabolismDipak YogiNo ratings yet
- Calcium and Phosphate MetabolismDocument27 pagesCalcium and Phosphate MetabolismIshaq100% (1)
- Study Guide For Calcium and Phosphate MetabolismDocument74 pagesStudy Guide For Calcium and Phosphate MetabolismMohammad MamunuzzamanNo ratings yet
- Mineral 2Document60 pagesMineral 2yixecix709No ratings yet
- Disorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1Document62 pagesDisorders of Calcium, Inorganic Phosphate and Magnesium Metabolism 1IiiNo ratings yet
- CCCTM FEN HO Rev T199285Document41 pagesCCCTM FEN HO Rev T199285Malte BreitlowNo ratings yet
- Parathyroid-Hormone Calcium HomeostasisDocument58 pagesParathyroid-Hormone Calcium HomeostasisSudhakar LakavathNo ratings yet
- Share Market Report 6Document13 pagesShare Market Report 6Nithish DevadigaNo ratings yet
- Biochemistry: Dr. Dra. Trini Suryowati, MsDocument49 pagesBiochemistry: Dr. Dra. Trini Suryowati, MsDaud ParluhutanNo ratings yet
- Calcium Homeostasis 23,2,14Document51 pagesCalcium Homeostasis 23,2,14Dr ratna kumariNo ratings yet
- Parathormone, CalcitoninDocument14 pagesParathormone, CalcitoninIbrahimNo ratings yet
- 5 Minute Biochemistry PresentationDocument23 pages5 Minute Biochemistry PresentationPITAGAN, Galda Boy 1-FNo ratings yet
- Mineral Metabolism.Document26 pagesMineral Metabolism.Shivanand MaliNo ratings yet
- 4651226Document20 pages4651226bibisupergirlNo ratings yet
- Calcemic Hormones: Leonard Waite, PHD Dept. of Pharmacology and ToxicologyDocument51 pagesCalcemic Hormones: Leonard Waite, PHD Dept. of Pharmacology and ToxicologyPritesh KuNo ratings yet
- Calcium & Phosphorus DentalDocument48 pagesCalcium & Phosphorus Dentalfathimatezil123No ratings yet
- Bone Mineral HomeostasisDocument22 pagesBone Mineral HomeostasisNur Aisyah ZakiNo ratings yet
- Hyper para Thyroid Is MDocument27 pagesHyper para Thyroid Is MIbrahimWagesNo ratings yet
- Calcium, Phosphate, MagnesiumDocument55 pagesCalcium, Phosphate, MagnesiumUdochukwu EnebeNo ratings yet
- CA and Phosphate Metabolism - PDFXDocument25 pagesCA and Phosphate Metabolism - PDFXObsa AhmedNo ratings yet
- Medical Surgical Nursing Module 7Document18 pagesMedical Surgical Nursing Module 7weissNo ratings yet
- Dyskal em Ia: Rs Hana CharitasDocument11 pagesDyskal em Ia: Rs Hana Charitasdwi nugroho prastowoNo ratings yet
- Calcium Metabolism: DR - Ammar Jawad MBCHB, MPHDocument54 pagesCalcium Metabolism: DR - Ammar Jawad MBCHB, MPHMurali ManiNo ratings yet
- 4 - Parathyroid HormoneDocument20 pages4 - Parathyroid HormonedhenaharcaNo ratings yet
- Vitamin D Calcium and PhosphateDocument26 pagesVitamin D Calcium and Phosphatel,Me & MyselfNo ratings yet
- Medical Surgical Nursing Module 8Document9 pagesMedical Surgical Nursing Module 8weissNo ratings yet
- Carbohydrate Metabolism: Sylvia Rianissa PutriDocument47 pagesCarbohydrate Metabolism: Sylvia Rianissa PutriMeilia AndiniNo ratings yet
- Lecture 3 Urea Cycle DisordersDocument27 pagesLecture 3 Urea Cycle Disordersamjadm2002No ratings yet
- Minerals: Role of Minerals in The BodyDocument12 pagesMinerals: Role of Minerals in The BodyZA IDNo ratings yet
- Substances Affecting Bone Mineral HomeostasisDocument33 pagesSubstances Affecting Bone Mineral Homeostasisanaya khan StudentNo ratings yet
- Parathyroid Hormone, Calcitonin, Calcium andDocument61 pagesParathyroid Hormone, Calcitonin, Calcium andchayChay gapolNo ratings yet
- Calcium and PhosphateDocument26 pagesCalcium and Phosphatekhushichunmun gargNo ratings yet
- Endocrine Physiology: Dale Buchanan Hales, PHD Department of Physiology & BiophysicsDocument74 pagesEndocrine Physiology: Dale Buchanan Hales, PHD Department of Physiology & BiophysicsOngen AchillesNo ratings yet
- A Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesFrom EverandA Simple Guide to Hyperparathyroidism, Treatment and Related DiseasesNo ratings yet
- 2022 Intensive Course. MM - Viral Hepatitis & HIV - AP Datin DR Noor ZettiDocument65 pages2022 Intensive Course. MM - Viral Hepatitis & HIV - AP Datin DR Noor ZettiRaja RuzannaNo ratings yet
- GIT InfectionDocument43 pagesGIT InfectionRaja RuzannaNo ratings yet
- HIV&HepatitisDocument46 pagesHIV&HepatitisRaja RuzannaNo ratings yet
- Cassy's MPATH MMB Guide v1.0 (2022)Document104 pagesCassy's MPATH MMB Guide v1.0 (2022)Raja RuzannaNo ratings yet
- Hepatitis VirusesDocument35 pagesHepatitis VirusesRaja RuzannaNo ratings yet
- HIV&HepatitisDocument100 pagesHIV&HepatitisRaja RuzannaNo ratings yet
- Donor Demographics 2015Document13 pagesDonor Demographics 2015Raja RuzannaNo ratings yet
- Recommended TextbooksDocument8 pagesRecommended TextbooksShi Lin Lau0% (1)
- Full Download Holes Human Anatomy and Physiology 15th Edition Shier Solutions ManualDocument35 pagesFull Download Holes Human Anatomy and Physiology 15th Edition Shier Solutions Manualbarovert.o87w100% (33)
- Stan DigestiveDocument3 pagesStan Digestivejoanna carrenNo ratings yet
- Homeostasis Activity - MARY SHESHIRADocument3 pagesHomeostasis Activity - MARY SHESHIRASheshira Reddy YeruvaNo ratings yet
- MODULE-4 Understanding Harmony in The Nature and Existence - WholeDocument9 pagesMODULE-4 Understanding Harmony in The Nature and Existence - WholeTECHNO YASHNo ratings yet
- Mold and Mildew QA Understanding Mold in Your HousevnoznDocument3 pagesMold and Mildew QA Understanding Mold in Your Housevnoznliftvision70No ratings yet
- EcoCRM A Recombinant CRM197 Carrier ProteinDocument1 pageEcoCRM A Recombinant CRM197 Carrier ProteinRamakrishnaNo ratings yet
- The Plant CellDocument30 pagesThe Plant CellMichael GentilesNo ratings yet
- GCLP Guidelines 2020 FinalDocument78 pagesGCLP Guidelines 2020 FinalGyanuNo ratings yet
- Epigenetic Age Clock Test Sample ReportDocument78 pagesEpigenetic Age Clock Test Sample ReportHIMMAT SINGHNo ratings yet
- Bio-FIT Book EN PDFDocument256 pagesBio-FIT Book EN PDFCesar Augusto Colorado RamirezNo ratings yet
- Genei Affinity Chromatography Teaching Kit ManualDocument9 pagesGenei Affinity Chromatography Teaching Kit ManualHemant Kawalkar100% (1)
- Anti Bacterial and Biofilm Inhibitory Activities of Aegle Marmelos Methanol Leaf ExtractDocument9 pagesAnti Bacterial and Biofilm Inhibitory Activities of Aegle Marmelos Methanol Leaf ExtractIJAR JOURNALNo ratings yet
- Biology Photosynthesis CourseworkDocument7 pagesBiology Photosynthesis Courseworkbdg72wjj100% (2)
- Jeffrey Moss, DDS, CNS, DACBN Jeffrey Moss, DDS, CNS, DACBN 413 413 - 530 530 - 0858 (Cell) 0858 (Cell)Document31 pagesJeffrey Moss, DDS, CNS, DACBN Jeffrey Moss, DDS, CNS, DACBN 413 413 - 530 530 - 0858 (Cell) 0858 (Cell)LukasNo ratings yet
- Tenebrio MolitorDocument9 pagesTenebrio Molitorじょしら フィアンナNo ratings yet
- Experiment 12 (Synthesis of Acetylsalicylic Acid)Document8 pagesExperiment 12 (Synthesis of Acetylsalicylic Acid)Cheng Bauzon100% (1)
- Histogenesis of Salivary Gland NeoplasmsDocument18 pagesHistogenesis of Salivary Gland Neoplasmsporkodi sudhaNo ratings yet
- Life Process - Biology MCQDocument3 pagesLife Process - Biology MCQJASMINE VIDHYANo ratings yet
- Psychic DevelopmentDocument13 pagesPsychic DevelopmentCult of Amon Ra100% (2)
- General Biology - Chapter IDocument10 pagesGeneral Biology - Chapter IG.k. Vinnan Rao100% (2)
- 2014 MBAA Chris White Yeast ManagementDocument30 pages2014 MBAA Chris White Yeast ManagementAdrián LampazziNo ratings yet
- The Evolution of Synthetic Thought: Takshashila EssayDocument42 pagesThe Evolution of Synthetic Thought: Takshashila EssayLINDYLL PONO100% (1)
- Food Chemistry: SciencedirectDocument11 pagesFood Chemistry: Sciencedirectratri nurNo ratings yet
- EMBL-EBI Train OnlineDocument19 pagesEMBL-EBI Train OnlineThyagoNo ratings yet
- WDR-Weaver Dice RulebookDocument29 pagesWDR-Weaver Dice RulebookAzazelNo ratings yet
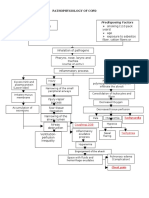
- Streptococcus Pneumonae: Pathophysiology of CopdDocument1 pageStreptococcus Pneumonae: Pathophysiology of CopdDimpal ChoudharyNo ratings yet
- B 10 VRV 2042Document36 pagesB 10 VRV 2042api-283593849No ratings yet
- Caplan Deron 201808 PHD CannabisDocument158 pagesCaplan Deron 201808 PHD CannabisMihai SimionNo ratings yet