Professional Documents
Culture Documents
AUBF - Chapter 1
AUBF - Chapter 1
Uploaded by
Kristin Soquillo0 ratings0% found this document useful (0 votes)
66 views7 pagesThis document discusses infection control procedures in healthcare facilities. It outlines the chain of infection which requires an infectious agent, reservoir, means of transmission, portal of entry, and susceptible host. Common infectious agents include bacteria, fungi, parasites, and viruses. The document then discusses various types of safety hazards including biologic, sharps, chemical, radioactive, electrical, fire/explosive, and physical hazards. It provides guidelines for standard precautions to prevent infection transmission including hand hygiene, use of gloves and gowns, patient care equipment handling, and environmental control. The document also discusses OSHA regulations for protecting workers from exposure to bloodborne pathogens.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document discusses infection control procedures in healthcare facilities. It outlines the chain of infection which requires an infectious agent, reservoir, means of transmission, portal of entry, and susceptible host. Common infectious agents include bacteria, fungi, parasites, and viruses. The document then discusses various types of safety hazards including biologic, sharps, chemical, radioactive, electrical, fire/explosive, and physical hazards. It provides guidelines for standard precautions to prevent infection transmission including hand hygiene, use of gloves and gowns, patient care equipment handling, and environmental control. The document also discusses OSHA regulations for protecting workers from exposure to bloodborne pathogens.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
66 views7 pagesAUBF - Chapter 1
AUBF - Chapter 1
Uploaded by
Kristin SoquilloThis document discusses infection control procedures in healthcare facilities. It outlines the chain of infection which requires an infectious agent, reservoir, means of transmission, portal of entry, and susceptible host. Common infectious agents include bacteria, fungi, parasites, and viruses. The document then discusses various types of safety hazards including biologic, sharps, chemical, radioactive, electrical, fire/explosive, and physical hazards. It provides guidelines for standard precautions to prevent infection transmission including hand hygiene, use of gloves and gowns, patient care equipment handling, and environmental control. The document also discusses OSHA regulations for protecting workers from exposure to bloodborne pathogens.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 7
Chapter 1
Susceptible host - can be another patient during
Biologic Hazards invasive procedures, visitors, and health-care
personnel when exposed to infectious specimen or
Infection control - All health-care facilities have needlestick injuries.
developed procedures to control and monitor Susceptible host:
infectious occurring within their facilities. Immunocompromised patients
The chain of infection requires a continuous link
Newborns and infants
between an infectious agent, a reservoir, a portal
of exit, a means of transmission, a portal of entry, Elderly
and a susceptible host.
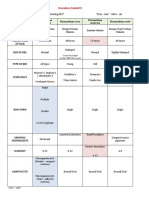
Table 1-1 TYPES OF SAFETY HAZARDS
Infectious agents:
Bacteria TYPE SOURCE POSSIBLE INJURY
Fungi
Parasites Biologic Infectious Bacterial, fungal,
Viruses agents viral, or parasitic
Reservoir - is the location of potentially harmful infections
microorganisms, such as a contaminated clinical
specimen or an infected patient Sharps Needles, Cuts, punctures, or
Fomites - equipment and other soiled inanimate lancets, blood-borne
objects. broken glass pathogen exposure
- They will serve as reservoirs, particularly if
Chemical Preservatives Exposure to toxic,
they contain blood, urine, or other body and reagents carcinogenic, or
fluids. caustic agents
The infectious agents must have a way to exit the
reservoir to continue the chain of infection. This Radioactive Equipment Radiation exposure
can be through the mucous membrane of the and
radioisotopes
nose, mout, eyes, and in blood, or other body
fluids. Electrical Ungrounded Burns or shock
Once the infectious agent has left the reservoir, it or wet
must have a way to reach a susceptible host. equipment;
Means of transmission include: frayed cords
1. Direct contact: the unprotected host
Fire/ explosive Open flames, Burns or
touches the patient specimen, or a organic dismemberment
contaminated subject (reservoir) chemicals
2. Airborne: inhalation of dried aerosol
particles circulating on air currents or Physical Wet floors, Falls, sprains, or
attached to dust particles heavy boxes, strains
patients
3. Droplets: the host inhales material from
the reservoir (e.g., aerosol droplets from a
patient or an uncapped centrifuge tube,
or when specimen are aliquoted or
spilled)
4. Vehicle: ingestion of a contaminated
substance (e.g., food, water, specimen)
5. Vector: from an animal or insect bite
Portal of entry - can be the same as portal of exit,
which includes the mucous membrane of the nose,
mouth, and eyes, breaks in the skin, and open
wounds.
Major importance in the laboratory environments. Ensure that single-use
Proper hand hygiene items are discarded properly.
Correct disposal of contaminated 6. Environmental control: ensure that the
materials hospital has adequate procedures for the
Wearing personal protective equipment routine care, cleaning, and disinfection of
(PPE) environmental surfaces, beds, bed rails,
The modification of UP for body substance bedside equipment, and other frequently
isolation (BSI) helped to alleviate this concern. touched surfaces.
BSI guidelines are not limited to blood borne 7. Linen: prevents skin and mucous
pathogens; they consider all body fluids and moist membrane exposures and clothing
body substance to be potentially infectious. contamination and avoids the transfer of
A major disadvantage of BSI guidelines is that they microorganisms to other patients and
do not recommend hand washing after removing environments.
gloves unless visual contaminants are present. 8. Occupational health and blood-borne
In 1996, the CDC and the Healthcare Infection pathogens: use self-sheathing needles or
Control Practices Advisory Committee (HIPAC) a mechanical device to conceal the
combined the major features of UP and BSi needle.
guidelines and called the new guidelines Standard 9. Patient placement
Precautions. 10. Respiratory hygiene/cough etiquette
Standard Precautions are as follows: The Occupational Exposure to Blood-Borne
1. Hand hygiene: includes both hand Pathogens Standard is a law monitored and
washing and the use of alcohol-based enforced by OSHA. Specific requirements of this
antiseptic cleaners. Sanitizing hands may OSHA standards include the following:
be necessary between tasks and ● Engineering controls
procedures on the same patient to a. Providing sharps disposal
prevent cross-contamination of different containers and needles with
body sites. safety devices.
2. Gloves: wear gloves (clean, non sterile b. Requiring discarding of needings
gloves are adequate) when touching the with the safety device activated
blood, bloody fluids, secretions, and the holder attached
excretions, and contaminated items. c. Labeling all biohazardous
3. Mouth, nose, and eye protection: A materials and containers.
specially fitted respirator (N95) must be ● Work practice controls
used during patient care activities related a. Requiring all employees to
to suspected mycobacterium exposure. practice Standard Precautions
4. Gown: wear a gown (a clean, non sterile and documenting training on an
gown is adequate) to protect skin and annual basis.
prevent soiling of clothing during b. Prohibiting eating, drinking,
procedures and patient care activities that smoking, and applying cosmetics
are likely to generate splashes or sprays of in the work area.
blood, body fluids, secretions, or c. Establishing a daily work surface
excretions. disinfection protocol.
5. Patient care equipment: handle used ● Personal protective equipment
patient care equipment soiled with blood, a. Providing laboratory coats,
body fluids, secretions and excretions in a gowns, face shields, and gloves
manner that prevents skin mucous to employees and laundry
membrane exposure, clothing facilities for non disposable
contamination, and transfer of protective clothing.
microorganisms to other patients or
● Medical Hand Hygiene
a. Providing immunization for the
hepatitis B virus free of charge. Hand contact is the primary method of infection
b. Providing medical follow-up to transmission. Alcohol-based cleaners can be used
employees who have been when hands are not visibly contaminated. They are
accidentally exposed to not recommended after contact with
blood-borne pathogens. spore-forming bacteria, including Clostridium
● Documentation difficile and Bacillus spp.
a. Documenting annual training of Hand washing procedure
employees in safety standards Equipment:
b. Documenting evaluations and Antimaicrobial soap
implementation of safer needle Paper towels
devices. Running water
Any accidental exposure to a possible blood-borne Waste container
pathogen must be immediately reported to a Procedure
supervisor. Evaluation of the incident must begin 1. Wet hands with warm water. Do not allow
right away to ensure appropriate postexposure parts of body to touch the sink
prophylaxis (PEP). 2. Apply soap, preferably antimicrobial
3. Rub to form a lather, create friction, and
Personal Protective Equipment loosen debris.
4. Rinse hands in a downward position to
PPE used in laboratories includes gloves, prevent recontamination of hands and
fluid-resistant gowns, eye and face shields, and wrists.
plexiglas countertop shields. When a specimen is 5. Obtain a paper towel from the dispenser.
collected, gloves should be changed between 6. Dry hands with a paper towel.
every patient. A variety of gloves types are 7. Turn off the faucet with a clean paper
available, including sterile and non sterile, towel to prevent contamination.
powdered and unpowdered, and latex and
nonlatex. Biologic Waste Disposal
Reactions to latex include irritant contact
dermatitis, which produces patches of dry, itchy All biological waste, except urine, must be placed
irritation on the hands; delayed hypersensitivity in appropriate containers labeled with the
reactions resembling poison ivy that appear 24 to biohazard symbol.
48 hours after exposure; and rue, immediate The waste is then decontaminated following
hypersensitivity reactions often characterized by institutional policy:
facial flushing and breathing difficulties. Any Incineration
symptoms of latex allergy should be reported to a Autoclaving
supervisor because true latex allergy can be Pick-up by a certified hazardous waste
life-threatening. company
Disposable coats are placed in containers for Disinfection of the sink using a 1:5 or 1:10 dilution
biohazardous waste, and nondisposable coats are of sodium hypochlorite should be performed daily.
placed in designated laundry receptacles. Sodium hypochlorite dilutions stored in plastic
A variety of protective equipment is available: bottles are effective for 1 month if protected from
Mask and goggles light after preparations. The same solution also can
Full-face plastic shields that cover the be used for routinely disinfecting countertops and
front and sides of the face accidental spills. The solution should be allowed to
Mask with attached shield air-dry on the contaminated area.
Plexiglas countertop shields
Absorbent materials used for cleaning countertops Chemical Labeling
and removing spills must be discarded in biohazard
containers. Hazardous chemicals should be labeled with a
description of their particular hazard, such as
Sharp Hazards poisonous, corrosive, flammable, explosive,
teratogenic, or carcinogenic.
Sharp objects in the laboratory, including needles, The National Fire Protection Association (NFPA)
lancets, and broken glassware, present a serious has developed the standard system for the
biologic hazard, particularly for the transmission of Identification of the Fire Hazards of Materials and
blood-borne pathogens. All sharp objects must be NFPA 704.
disposed of in a puncture-resistant, leak-proof This symbol system is used to inform firefighters of
container with the biohazard symbol. the hazards they may encounter with fires in a
Chemical spill kits containing protective apparel, particular area.
nonreactive absorbent material, and bags for The diamond-shaped, color-coded symbol
disposing of contaminated materials should be contains information relating to health,
available for cleaning up spills. flammability, reactivity, and personal
protection/special precautions.
Chemical Handling Each category is graded on a scale of 0 to 4, based
Chemicals should never be mixed together unless on the extent of concern.
specific instructions are followed, and they must
be added in the order specified. Material Safety Data Sheets
Acid should always be added to water to avoid the
possibility of sudden splashing caused by the rapid The OSHA Federal Hazard Communication
generation of heat in some chemical reactions. Standard requires all the employees have a right to
Chemicals should be used from containers that are know about all chemical hazards present in their
of an easily manageable size. workplace.
Pipetting by mouth is unacceptable in the Information contained in an MSDS includes the
laboratory. following:
1. Physical and chemical characteristics
Chemical Hygiene Plan 2. Fire and explosion potential
3. Reactivity potential
OSHA also requires all facilities that use hazardous 4. Health hazards and emergency first aid
chemicals to have a written Chemical hygiene plan procedures
(CHP) available to employees. The purpose of the 5. Methods for safe handling and disposal
plan is to detail the following: 6. Primary routes of entry
1. Appropriate work practices 7. Exposure limits and carcinogenic potential
2. Standard operating procedures
3. PPE Radioactive Hazards
4. Engineering controls, such as fume hoods
and inflammables safety cabinets Radioactivity may be encountered in the clinical
5. Employee training requirements laboratory when procedures using radioisotopes
6. Medical consultation guidelines are performed.
Each facility must appoint a chemical hygiene The amount of radiation exposure is related to a
officer, who is responsible for implementing and combination of time, distance, and shielding.
documenting compliance with the plan. Persons working in a radioactive environment are
required to wear measuring devices to determine
the amount of radiation they are accumulating.
Electrical Hazards 2. Aim at the base of the fire
3. Squeeze handles
Equipment should not operated with wet hands. 4. Sweep nozzle side to side
Designated hospital personnel minitor electrical
equipment closely; however, laboratory personnel Quality Assessment
should continually observe for any dangerous
conditions such as frayed cords and overloaded The term Quality Assessment (QA) refers to the
circuits, and report them to the supervisor. overall process of guaranteeing quality patient care
and is regulated throughout the total testing
Fire/Explosive hazards system.
Quality system refers to all of the laboratory’s
The joint commission (JC) requires that all policies, processes, procedures, and resources
health-care institutions post evacuation routes and needed to achieve quality testing.
detailed plans to follow in the event of a fire. In clinical laboratory, a quality assessment program
When a fire is discovered, all employees are includes not only testing controls, referred to as
expected to take actions in the acronym RACE: quality control (QC), but also encompasses
Rescue - rescue anyone in immediate Pre examination variables (e.g., specimen
danger collecting, handling,and storage)
Alarm - activate the institutional fire Examination variables (e.g., reagent and test
alarm system performance, instrument calibration and
maintenance, personnel requirements, and
Contain - close all doors to potentially
technical competence)
affected areas
Postexamination variables (e.g., reporting of
Extinguish/evacuate - attempt to
results and interpretation), and documentation
extinguish the fire, if possible or evacuate,
that the program is being meticulously followed.
closing the door
QA program
Procedure manual
Internal quality control
External quality control
Electronic quality control
Calibration or calibration verification
Standardization
Proficiency testing (PT) more formally
known as External Quality Assessment
(EQA)
QA is the continual monitoring of the entire test
process from test ordering and specimen collection
through reporting and interpreting results.
Table 1-2 Types of Fires and Fire Extinguisher
Fire Type Extinguishing Type/Comp Extinguisher
Material osition of
Fire
Class A Wood, paper, Class A Water
The acronym PASS can be used to remember the clothing
steps in the operation:
1. Pull pin Class B Flammable Class B Dry
organic chemicals, Nonmatching labels and requisition forms
chemicals carbon Contaminated specimens with feces or toilet
dioxide, paper
foam, or Containers with contaminated exteriors
halon Insufficient volume of urine
Improperly transported or preserved specimens
Class C Electrical Class C Dry Delay between time of collection and receipt in
chemicals, the laboratory
carbon
Examination variables are the processes that
dioxide, or
halon directly affect the testing of specimens. They
include reagents, instrumentation and equipment,
Class D Combustible None Sand or dry testing procedure, QC, preventive maintenance
metals powder (PM), access to procedure manuals, and
competency of personnel performing the tests.
Class ABC Dry
chemicals External Quality Control - used to verify the
accuracy (ability to obtain the expected result) and
Class K Grease, oils, Class K Liquid precision (ability to obtain the same result on the
fats designed to same specimen) of a test and are exposed to the
prevent same conditions as the patient samples.
splashing
Food and Drug Administration (FDA) standards
and cool in
the fire require that the control material test negative for
HIV and hepatitis virus.
Standard mean is the average of all data points
Preexamination variables occur before the actual
Standard deviation is a measurement statistic that
testing of the specimen and include test requests,
describes the average distance each data point in a
patient preparation, timing, specimen collection,
normal distribution is from the mean.
handling, and storage.
The CV indicates whether the distribution of values
TAT is defined as the amount of time required from
about the mean is in a narrow versus broad range
the point at which a test is ordered by the
and should be less than 5%.
health-care provider until the results are reported
Control ranges are determined by setting
to the health-care provider.
confidence limits that are within +-2 SD or +-3 SD
The form should include space for recording:
of the mean, which indicates that 95.5% to 99.7%
1. The actual date and time of specimen
of the values are expected to be within that range.
collection
Trend that is a gradual changing in the mean in
2. Whether the specimen was refrigerated
one direction
before transporting
Shift is an abrupt change in the mean.
3. The time the specimen was received in
Internal Quality Control consists of internal
the laboratory and the time the test was
monitoring systems built into the test system and
performed
are called internal or procedural controls.
4. Test are quested
External Quality Control uses a mechanical or
5. An area for specific instructions that
electrical device in place of a liquid QC specimen.
might affect the results of the analysis
EQC verifies the functional ability of testing
6. Patient identification information
devices, but it does not verify the integrity of the
All urine specimens should be examined within 2
testing supplies.
hours
PT or EQA is the testing of unknown samples
received from an outside agency, and provides
Table 1-4 Criteria for Urine Specimen Rejection unbiased validation of the quality of patient test
results.
Unlabeled containers
The Clinical Laboratory Improvement 3. During laboratory accreditation
Amendments (CLIA) mandates comparison testing inspections, procedure manuals are
for laboratory accreditation. examined for the presence of: critical
Postexamination variables are processes that values, procedure reference and
affect the reporting of results and correct procedure for specimen preservation
interpretation of data. 4. As supervisor of the urinalysis laboratory,
Electronic transmission is now the most common you have just adopted a new procedure.
method for reporting results. You should: Put a complete, referenced
procedure in teh manual
5. Indicate whether each of the following
Summary 1-1 Quality Assessment
would be considered 1.) preexamination,
Preexamination 2) examination, 3) postexamination factor
Patient misidentification by placing the appropriate number in the
Wrong test ordered blank:
Incorrect urine specimen type a. Reagent examination date - 2
collected b. Rejecting a contaminated
Insufficient urine volume specimen - 1
Delayed transport of urine to the c. Constructing a Levy-Jennings
laboratory chart - 2
Incorrect storage or preservation of d. Telephoning a positive Clinitest
urine
result on a newborn - 3
Examination e. Calibrating the centrifuge - 2
Sample misidentification f. Collecting a timed specimen - 1
Erroneous instrument calibration 6. The testing of sample from an outside
Reagent deterioration agency and the comparison of results
Poor testing technique with participating laboratories is called:
Instrument malfunction Proficiency testing
Interfering substances present 7. A color change that indicates that a
Misinterpretation of quality control sufficient amount of patient’s specimen or
data reagent is added correctly to the test
system would be an example of: Internal
Postexamination QC
Patient misidentification 8. What steps are taken when the results of
Poor handwriting reagent strip QC are outside of the stated
Transcription error confidence limits? : check the expiration
Poor quality of instrument printer date of the reagent strip, run a new
Failure to send report
control, open a new reagent strips
Failure to call critical values
container.
Inability to identify interfering
9. When a new bottle of QC material is
substances
opened, what information is placed on
the label?: The data and the laboratory
Study questions: worker’s initials
10. When a control is run, what information is
1. The current routine infection control documented? : The lot number,
policy developed by CDC and followed in expiration date of the control and the
all health-care settings is: Standard test results
Precautions
2. Quality assessment refers to: Quality of
specimens and patient care
You might also like
- Histopath Transes 1Document9 pagesHistopath Transes 1Nico LokoNo ratings yet
- AD GT700P User Guide en Rev.2.01Document23 pagesAD GT700P User Guide en Rev.2.01Mohamed AlkharashyNo ratings yet
- AUBF Notes 1Document9 pagesAUBF Notes 1ChiNo ratings yet
- Compiled Quizes AubfDocument39 pagesCompiled Quizes AubfCharmaine BoloNo ratings yet
- Aubf Lec - Serous FluidDocument12 pagesAubf Lec - Serous FluidColene MoresNo ratings yet
- Environment, Health and Safety PDFDocument253 pagesEnvironment, Health and Safety PDFRishabh Rastogi100% (1)
- Histopath Lec (Module 1) : Iintroduction To PathologyDocument17 pagesHistopath Lec (Module 1) : Iintroduction To PathologyAngela ReyesNo ratings yet
- IS LessonDocument30 pagesIS Lessonjohn dale duranoNo ratings yet
- Antigen and Its PropertiesDocument20 pagesAntigen and Its Propertiestusharpremin92% (12)
- Aubf LabDocument99 pagesAubf Labhinata shoyoNo ratings yet
- M6 Histopath ImpregantionAndEmbeddingDocument4 pagesM6 Histopath ImpregantionAndEmbeddingninaNo ratings yet
- Impregnation and EmbeddingDocument5 pagesImpregnation and EmbeddingOsannah Irish InsongNo ratings yet
- 1 Antigens and AntibodiesDocument31 pages1 Antigens and AntibodiesJohn Louis RanetNo ratings yet
- Leptospires General Characteristics:: Bacteriology: SpirochetesDocument5 pagesLeptospires General Characteristics:: Bacteriology: SpirochetesJaellah MatawaNo ratings yet
- Klebsiella Shigella Yersinia: Have Little Value in IDDocument6 pagesKlebsiella Shigella Yersinia: Have Little Value in IDKenneth Jake Batiduan100% (1)
- Analysis of Urine and Other Body Fluids - , RMT Sputum & Bronchoalveolar Lavage (Bal)Document11 pagesAnalysis of Urine and Other Body Fluids - , RMT Sputum & Bronchoalveolar Lavage (Bal)jeffreyNo ratings yet
- L E CellDocument59 pagesL E CellAvi VermaNo ratings yet
- TREMATODESDocument31 pagesTREMATODESKen Mark ConcepcionNo ratings yet
- Microscopy TransDocument2 pagesMicroscopy TransMarco TolentinoNo ratings yet
- Clinical MicrosDocument26 pagesClinical MicrosDarla YsavelNo ratings yet
- Medical Technology Laws AND Bioethics: Imelda A. de Leon, RMT, Mpa ProfessorDocument42 pagesMedical Technology Laws AND Bioethics: Imelda A. de Leon, RMT, Mpa ProfessorMaria ClaraNo ratings yet
- Lesson 16: Adhesives and Mounting MediaDocument3 pagesLesson 16: Adhesives and Mounting MediaZairah PascuaNo ratings yet
- Mycology 1 PrelimDocument4 pagesMycology 1 PrelimKaye Angel VillonNo ratings yet
- Joshua Ty Cayetano 3DMT #15: A B C A B B B A ADocument4 pagesJoshua Ty Cayetano 3DMT #15: A B C A B B B A AJoshua Ty CayetanoNo ratings yet
- Gram Positive CocciDocument34 pagesGram Positive CocciMaria Cecilia Flores50% (2)
- Bacteriology PDFDocument49 pagesBacteriology PDFKat JornadalNo ratings yet
- Lecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterDocument4 pagesLecture 10 Vibrio, Aeromonas, Campylobacter and HelicobacterRazmine RicardoNo ratings yet
- MT Laws and Lab ManDocument8 pagesMT Laws and Lab ManGene Narune GaronitaNo ratings yet
- Par201 S1lab4 Midterm Phamids Aphasmids PDFDocument27 pagesPar201 S1lab4 Midterm Phamids Aphasmids PDFHanna Alyssa Grace DimarananNo ratings yet
- Student Notes: HPCT: Davao Doctors College Medical Laboratory Science DepartmentDocument3 pagesStudent Notes: HPCT: Davao Doctors College Medical Laboratory Science DepartmentMelody Jane Pardillo100% (1)
- Mtle Bacte Revised 1Document35 pagesMtle Bacte Revised 1melvinsalonga2999No ratings yet
- Immunology & Serology Week 1Document2 pagesImmunology & Serology Week 1Romie SolacitoNo ratings yet
- The Intestinal NematodesDocument9 pagesThe Intestinal NematodesdhaineyNo ratings yet
- AUBF - Chapter 2Document5 pagesAUBF - Chapter 2Kristin SoquilloNo ratings yet
- Lesson 1 History of Medical Technology or The Clinical Laboratory Science ProfessionDocument4 pagesLesson 1 History of Medical Technology or The Clinical Laboratory Science ProfessionGianneCarloGomedNo ratings yet
- Clinical Parasitology LaboratoryDocument4 pagesClinical Parasitology LaboratoryLyka ReyesNo ratings yet
- Viruses PDFDocument54 pagesViruses PDFluz camargoNo ratings yet
- Group 4 - General Pathology, Logic and Cytologic TechniquesDocument11 pagesGroup 4 - General Pathology, Logic and Cytologic Techniquesjulo_05No ratings yet
- My CologyDocument25 pagesMy CologyPlasma CarwashNo ratings yet
- 3 SEMR421 Bacteriology Part 3Document14 pages3 SEMR421 Bacteriology Part 3Micah Daniel TapiaNo ratings yet
- ISBB Aaaaa PDFDocument55 pagesISBB Aaaaa PDFSelena de LimaNo ratings yet
- (Para) Introduction To Parasitology and Protozoology-Dr. Dela Rosa (Tiglao)Document7 pages(Para) Introduction To Parasitology and Protozoology-Dr. Dela Rosa (Tiglao)Arlene DaroNo ratings yet
- HISTOPATH FIXATIONdocx PDFDocument8 pagesHISTOPATH FIXATIONdocx PDFmaricel duque100% (1)
- Fresh Tissue ExaminationDocument23 pagesFresh Tissue ExaminationMarissa CordovaNo ratings yet
- Immunohema SlidesDocument508 pagesImmunohema SlidesBerihunNo ratings yet
- Histopath Lec - Week 2 - Topic 2Document3 pagesHistopath Lec - Week 2 - Topic 2Juren LasagaNo ratings yet
- Malarial ParasitesDocument5 pagesMalarial ParasitesZette ArañaNo ratings yet
- 1.entamoeba Histolytica - Is The Major Pathogen in This GroupDocument14 pages1.entamoeba Histolytica - Is The Major Pathogen in This GroupJoseph De JoyaNo ratings yet
- Analysis of Urine and Other Body FluidsDocument52 pagesAnalysis of Urine and Other Body FluidsJoseph VillamorNo ratings yet
- AUBF Finals Vaginal SecretionsDocument37 pagesAUBF Finals Vaginal SecretionsLyra Dennise LlidoNo ratings yet
- Stool Exam - Routine, Conc. Method - Students'Document27 pagesStool Exam - Routine, Conc. Method - Students'AnastasiaNo ratings yet
- Molecular Biology and Diagnostic Intro To CytogeneticsDocument6 pagesMolecular Biology and Diagnostic Intro To Cytogeneticselijah montefalcoNo ratings yet
- Protozoa: Guanling Wu, Prof. in Dept. Pathogen Biology, Nanjing Medical University, Najing, Jiangsu, ChinaDocument73 pagesProtozoa: Guanling Wu, Prof. in Dept. Pathogen Biology, Nanjing Medical University, Najing, Jiangsu, ChinaUmer RasheedNo ratings yet
- Urine Specimen Collection: Ms. Sneha SehrawatDocument36 pagesUrine Specimen Collection: Ms. Sneha SehrawatRajaNo ratings yet
- Immuno Sero CompleteDocument33 pagesImmuno Sero CompleteAngela ReyesNo ratings yet
- Diagnostic Microbiology - : University of Santo Tomas - Medical TechnologyDocument6 pagesDiagnostic Microbiology - : University of Santo Tomas - Medical TechnologyWynlor AbarcaNo ratings yet
- C19 2 Hemopoiesis Eythropoiesis LeukopoiesisDocument11 pagesC19 2 Hemopoiesis Eythropoiesis Leukopoiesisnurul azisyah auraNo ratings yet
- Trematodes: Blood FlukesDocument3 pagesTrematodes: Blood FlukesFrance Louie JutizNo ratings yet
- Laboratory Safety in The Clinical Microscopy SectionDocument6 pagesLaboratory Safety in The Clinical Microscopy SectionFarida WongNo ratings yet
- Urinalysis and Other Body FluidsDocument64 pagesUrinalysis and Other Body FluidsJahre Mark ToledoNo ratings yet
- 4 Safety and Infection ControlDocument3 pages4 Safety and Infection ControlRossiene AirosNo ratings yet
- Clinical Bacteriology Lab (W01)Document7 pagesClinical Bacteriology Lab (W01)nicholehernandez05No ratings yet
- Ism Code 1993 - BooksDocument10 pagesIsm Code 1993 - Bookseboy14No ratings yet
- Thorium AA Standard MSDS: Section 1: Chemical Product and Company IdentificationDocument6 pagesThorium AA Standard MSDS: Section 1: Chemical Product and Company IdentificationAlfauziNo ratings yet
- Pressure Sensitive Safety Edge System ManualDocument24 pagesPressure Sensitive Safety Edge System ManualJehiel AlvarezNo ratings yet
- Management MCQs WordDocument42 pagesManagement MCQs WordMadhulika WNo ratings yet
- Design and Management Guidelines For A Safer CityDocument46 pagesDesign and Management Guidelines For A Safer CitySandu Lica0% (1)
- Assessment 1Document5 pagesAssessment 1Agus BudionoNo ratings yet
- MSDS 1147Document4 pagesMSDS 1147Nguyên NguyễnNo ratings yet
- Nigeria Gas Sector ReportDocument138 pagesNigeria Gas Sector ReportvalentineNo ratings yet
- Jsa Grinding W Angle GrinderDocument2 pagesJsa Grinding W Angle GrinderMichael Angelo SanteNo ratings yet
- Bayer Cropscience: Movento®Document11 pagesBayer Cropscience: Movento®EugeniaNo ratings yet
- Risk Assessment LiftingDocument2 pagesRisk Assessment Liftingmohamed ghalyNo ratings yet
- SegwayDocument2 pagesSegwaysharafat hussainNo ratings yet
- Photovoltaic Inverter Testing and Certification Solutions: Tüv SüdDocument2 pagesPhotovoltaic Inverter Testing and Certification Solutions: Tüv SüdlocthaiquocNo ratings yet
- Baby Crib Safety StandardsDocument5 pagesBaby Crib Safety Standardssamar fatimaNo ratings yet
- Maaden MSHEM Safety Documents 8Document143 pagesMaaden MSHEM Safety Documents 8ShadifNo ratings yet
- UC94 - Installations & BrugermanualDocument24 pagesUC94 - Installations & BrugermanualFabio BerréNo ratings yet
- Msds NEXTARD SDocument5 pagesMsds NEXTARD SRyan setiawanNo ratings yet
- Nfpa 1201 2004Document31 pagesNfpa 1201 2004Antonio GutierrezNo ratings yet
- 3 772Document61 pages3 772D MNCNo ratings yet
- 951 180 061 en PDFDocument36 pages951 180 061 en PDFВиталий КозловскийNo ratings yet
- AFManualCOMANDOSKILL20 1059TNPlay125x170Document28 pagesAFManualCOMANDOSKILL20 1059TNPlay125x170testis.pernanaiNo ratings yet
- What Is Environmental AuditingDocument25 pagesWhat Is Environmental AuditingSakshi ChhabraNo ratings yet
- Potable Water Stabiliser Liq.25 LTRDocument9 pagesPotable Water Stabiliser Liq.25 LTRVictor S.No ratings yet
- Commercial Dedication A Manufacturer's PerspectiveDocument8 pagesCommercial Dedication A Manufacturer's Perspectivealien686No ratings yet
- Contoh User ManualDocument74 pagesContoh User Manualaziz abdulNo ratings yet
- BS EN746!3!1997 Industrial Thermoprocessing EquipmentDocument34 pagesBS EN746!3!1997 Industrial Thermoprocessing EquipmentThaiminh Vo100% (1)
- P 4 (1 05) PSI Plant Safety Inspection (35) Jul.2012Document35 pagesP 4 (1 05) PSI Plant Safety Inspection (35) Jul.2012Vaibhav Vithoba Naik100% (9)
- Ansi Isa 84 00 01 2004 Iec 61511 ModDocument84 pagesAnsi Isa 84 00 01 2004 Iec 61511 ModMOZAMMIL MAHBOOBNo ratings yet