Professional Documents
Culture Documents
Mental Health in Zambia - Challenges and Way Forwa
Mental Health in Zambia - Challenges and Way Forwa
Uploaded by
Josephine Chirwa0 ratings0% found this document useful (0 votes)
62 views2 pagesZambia faces significant challenges in providing adequate mental healthcare to its population of 12 million. It has only 3 psychiatrists and relies heavily on clinical officers to treat patients. Infrastructure is also lacking, with only one psychiatric hospital and small annexes. There is no graduate training for psychiatrists within Zambia, and the few who study abroad rarely return due to lack of incentives. Significant stigma exists around mental illness. To improve the system, Zambia needs to prioritize mental health in policy, increase trained professionals, expand infrastructure like adding beds in district hospitals, and implement public awareness campaigns to reduce stigma.
Original Description:
Original Title
Mental_health_in_Zambia_-_challenges_and_way_forwa
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentZambia faces significant challenges in providing adequate mental healthcare to its population of 12 million. It has only 3 psychiatrists and relies heavily on clinical officers to treat patients. Infrastructure is also lacking, with only one psychiatric hospital and small annexes. There is no graduate training for psychiatrists within Zambia, and the few who study abroad rarely return due to lack of incentives. Significant stigma exists around mental illness. To improve the system, Zambia needs to prioritize mental health in policy, increase trained professionals, expand infrastructure like adding beds in district hospitals, and implement public awareness campaigns to reduce stigma.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
62 views2 pagesMental Health in Zambia - Challenges and Way Forwa
Mental Health in Zambia - Challenges and Way Forwa
Uploaded by
Josephine ChirwaZambia faces significant challenges in providing adequate mental healthcare to its population of 12 million. It has only 3 psychiatrists and relies heavily on clinical officers to treat patients. Infrastructure is also lacking, with only one psychiatric hospital and small annexes. There is no graduate training for psychiatrists within Zambia, and the few who study abroad rarely return due to lack of incentives. Significant stigma exists around mental illness. To improve the system, Zambia needs to prioritize mental health in policy, increase trained professionals, expand infrastructure like adding beds in district hospitals, and implement public awareness campaigns to reduce stigma.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 2
39
Co u n t r y p r o file
Mental health in Zambia – challenges and
way forward
Jedrin Ngungu1 and Julian Beezhold2
1
Specialist Registrar, Norfolk and Waveney Mental Health Foundation Trust, email ngunguj@yahoo.com
(former Acting Medical Director for a year at Chainama Hills Hospital, Zambia)
2
Consultant Psychiatrist, Norfolk and Waveney Mental Health Foundation Trust
Z ambia, previously called Northern Rhodesia, was
a colony of Great Britain until 1964, when it gained
independence and changed its name. It is a landlocked
sychologists, occupational therapists or mental health social
p
workers. The bulk of the work in mental health is carried out
by clinical officers, who are specially trained medical assist-
country located in southern Africa and shares its borders ants (see below).
with Zimbabwe, Namibia, Botswana, Mozambique,
Malawi, Tanzania, Congo and Angola. It has an area of
752 612 km2, about three times the size of Britain, but a Infrastructure and services
population of only 12 million.
The country is divided into nine provinces for admin Zambia has only one psychiatric hospital, Chainama Hills
istrative purposes, each with a provincial headquarters. Hospital, which is based in the capital city of Lusaka. It was
Although there are 72 languages spoken in Zambia, there opened in 1962 as a national referral centre. It has a capacity
are seven main ones: Nyanja, Bemba, Lunda, Luvale, of 500 beds, divided into 380 general adult and 120 forensic.
Kaonde, Lozi and Tonga. The official language is English, It is modelled after the asylums that characterised English
which is spoken by most citizens. Zambia is largely a mental healthcare more than 50 years ago. The wards are
youthful country, with 90% of its population less than 45 large halls with many patients in each. The beds are usually
years old; only 2% are over 65. just mattresses placed on the floor.
Apart from Chainama, there are smaller units, called
annexes, in seven provincial headquarters: Ndola, Mansa,
Policy and legislation Kasama, Kabwe, Chipata, Mongu and Livingstone. These
provide a few extra beds and are staffed by clinical officers
Since 1992, the country has had five national develop- and psychiatric nurses.
ment plans; the latest was the Fifth National Development In Zambia, therapy almost exclusively comprises the use of
Plan (FNDP) in 2006. In the first four plans, there was no psychotropics; talking therapies are non-existent. However,
mention of mental health. There is only a casual mention this is not as problematic as it might be, given that almost all
in the FNDP, in which the health agenda is dominated by admissions are for psychotic illness (mostly acute psychotic
infectious diseases (HIV, tuberculosis, malaria and diarrhoeal episode, followed by schizophrenia and bipolar disorders).
diseases) followed by child health and reproductive health. It is rare to see patients with depression unless they have
The strategy for mental health is less than coherent. psychotic symptoms as well. The country has no specific
Zambia still uses the 1951 Mental Disorders Act in which forensic, drug and alcohol or children’s services.
patients are referred to as idiots, imbeciles and invalids.
Since the early 2000s, there has been some effort to reform
the Act and this reached the stage of a parliamentary draft Education and training
bill in 2006. However, the draft bill is far from perfect as it
is not based on the United Nations human rights charter, The University of Zambia’s School of Medicine is the country’s
which is the bedrock of most current mental health legisla- only medical school. It produces 40 graduates every year,
tion. The limited availability of mental health professionals half of whom never practise locally but leave the country.
to spearhead this agenda has contributed to the lack of Whereas there is postgraduate training in surgery, medicine,
progress. It has to be said, however, that there is almost paediatrics and obstetrics and gynaecology, there is no such
no recourse to the Act in clinical practice, as most people training in psychiatry. To become a psychiatrist, one has to
are too ignorant to challenge their detention for treatment go abroad and herein lies one of Zambia’s problems: the few
against their will. who go for such training rarely return. (There are at least six
Zambian psychiatrists working abroad.)
Similarly, there is no graduate training for psychologists,
Personnel social workers or occupational therapists. What is available
is training for psychiatry clinical officers and nurses. This is
Zambia has only three psychiatrists for a population of based at Chainama Hills College of Health Sciences, which is
12 million. Two of these are not in clinical practice but located in Lusaka just adjacent to Chainama Hospital. Clinical
are attached to the local university. There are no graduate officers are the mainstay of mental health services in Zambia.
International Psychiatry Volume 6 Number 2 April 2009
40
These are medical assistants who spend 3 years studying Infrastructure
medicine before graduating to work in general medicine. There is a need to have mental health beds in every district.
After about a year, some of the clinical officers return to Every district has a general hospital and, to keep costs down,
Chainama College for an extra year, to become psychiatry some of these could be allocated to psychiatry.
clinical officers.
Stigma
High levels of stigma exist not only against those who are
Challenges and way forward mentally ill but also against their families and those working
in the mental health services. Many patients are disowned by
Government policy and legislation their families. Most long-stay patients in Chainama Hospital
While some progress has been made in putting forward the have no contact with their family members. The ‘out of sight
mental health agenda for government policy, much remains out of mind’ mentality is prevalent.
to be done to convince not only government but also parlia- Public awareness campaigns are needed. These could be
ment of the importance of a robust mental health policy and targeted at schools, colleges, workplaces and other public
infrastructure. Successful lobbying cannot be achieved by areas. One or two charities are trying but, with limited
locals alone but requires the help of international partners capacity, little is being achieved. The government may decide
such as the World Health Organization and the World Psychi- to make this one of the priorities for mental health. It is cer-
atric Association. tainly an achievable goal which, unlike the above, does not
require massive funding.
Human resources
There is a serious deficit of trained personnel in the medical
field. This is even more pronounced in mental health. Zambia Sources
needs more psychiatrists just to help build capacity in the Haworth, A. (1988) Psychiatry in Zambia. Bulletin of the Royal College of
mental health services, let alone to run such services. There is Psychiatrists, 12, 127–129.
also a need for other mental health professionals, including Mayeya, J., Chazulwa, R., Mayeya, P. N., et al (2004) Zambia mental
psychologists and occupational therapists. To address this health country profile. International Review of Psychiatry, 16, 63–72.
Mwanza, J., Sikwese, A., Banda, M., et al (2008) Phase 1 Country
deficit, local training must be developed. Training people
Report. Mental Health Policy Development and Implementation in
overseas, as has been proved over the years, is not a viable Zambia: A Situation Analysis. WHO. Available at http://www.who.
option. The establishment of training facilities will be expen- int/mental_health/policy/development/Zambia%20Country%20report.
sive, nonetheless. pdf (last accessed January 2009).
O r i g i n a l pape r
Correlates of lifetime alcohol abuse
and dependence among older community
residents in Brazil
Gerda G. Fillenbaum,1 Sergio Luís Blay,2 Sergio Baxter Andreoli2 and
Fabio Leite Gastal3
1
Center for the Study of Aging and Human Development, Duke University Medical Center, and Geriatric Research, Education and
Clinical Center, Veterans Administration Medical Center, Durham, NC, USA, email ggf@geri.duke.edu
2
Department of Psychiatry, Federal University of São Paulo, Brazil (Escola Paulista de Medicina – UNIFESP)
3
Invited Professor, Medical University of Minas Gerais/UFMG, Brazil
M isinterpretation in major surveys of alcohol use
disorder as described by DSM–IV (Hasin et al,
2007) has raised serious questions regarding the extent
and combined associations with demographic, social and
health characteristics in a representative community-
resident sample aged 60 years and over. We hypothesised
of alcohol use disorder, and the relationship between that, while for each of the three groups (those with alcohol
alcohol abuse and alcohol dependence. While the adverse abuse, those with alcohol dependence, and those with
social, physical and mental effects of alcohol misuse are both) there would be associated demographic character-
well known (Council on Scientific Affairs, 1996), there istics, abuse would be more closely associated with social
is little information on the determinants of alcohol characteristics, dependence with health characteristics,
abuse (societal impact) and alcohol dependence (physio and the combined presence of abuse and dependence
logical impact). We therefore examined their separate with both social and health characteristics.
International Psychiatry Volume 6 Number 2 April 2009
You might also like
- Hygiene (NCLEX) Flashcards - QuizletDocument5 pagesHygiene (NCLEX) Flashcards - QuizletA.No ratings yet
- Kozier Chapter 17 Health Wellness Well BeingDocument10 pagesKozier Chapter 17 Health Wellness Well BeingpauchanmnlNo ratings yet
- Zambian Syllabus For Civic Education Grade 10Document7 pagesZambian Syllabus For Civic Education Grade 10Makwebo Kamema0% (1)
- Zambias Challenges at IndependenceDocument7 pagesZambias Challenges at Independencemuna moono100% (2)
- Nursing As An Art: CaringDocument58 pagesNursing As An Art: CaringZeus CabungcalNo ratings yet
- Checklist Topical ApplicationDocument5 pagesChecklist Topical Applicationpramod kumawatNo ratings yet
- Ethics in PediatricsDocument20 pagesEthics in PediatricsCruz YrNo ratings yet
- Measles BrochureDocument2 pagesMeasles Brochureapi-340763234No ratings yet
- Community Health Nursing I (Individual and Family) : Prepared By: Mrs. Lavinia T. Malabuyoc, MAN, R.NDocument48 pagesCommunity Health Nursing I (Individual and Family) : Prepared By: Mrs. Lavinia T. Malabuyoc, MAN, R.NLerma Pagcaliwangan100% (1)
- Community Health NursingDocument10 pagesCommunity Health NursingAira AcasNo ratings yet
- Energy Field Theories Energy FieldsDocument12 pagesEnergy Field Theories Energy FieldsJames Kurt CruzatNo ratings yet
- The Role of Fiji Nursing AssociationDocument11 pagesThe Role of Fiji Nursing AssociationJSeashark100% (3)
- International NursingDocument18 pagesInternational NursingJennifer DixonNo ratings yet
- The Prehistory of Psychiatry in EthiopiaDocument3 pagesThe Prehistory of Psychiatry in EthiopiaifriqiyahNo ratings yet
- Community Assessment Windshield Survey - EditedDocument8 pagesCommunity Assessment Windshield Survey - EditedGeorge OwuorNo ratings yet
- Adventist University of The Philippines: Urinary Cathetirization P RIS RemarksDocument2 pagesAdventist University of The Philippines: Urinary Cathetirization P RIS RemarksAnnie AlbertoNo ratings yet
- BANDAGING ProcedureDocument6 pagesBANDAGING ProcedureAngelie PantajoNo ratings yet
- Intramuscular Injectoin ChecklistDocument2 pagesIntramuscular Injectoin ChecklistBettina ChuaNo ratings yet
- A Report On Imogene KingDocument17 pagesA Report On Imogene KingRibelyne loise AquisioNo ratings yet
- 5B Assessing Apical Pulse-2Document4 pages5B Assessing Apical Pulse-2Marky RoqueNo ratings yet
- Administering Pulse OxDocument2 pagesAdministering Pulse OxjepoiNo ratings yet
- Foundation of Nursing OBJ QUESTIONSDocument12 pagesFoundation of Nursing OBJ QUESTIONSElla AdogunNo ratings yet
- Availability and Utilization of Health Informatics System Among Health Workers in Niger State, NigeriaDocument8 pagesAvailability and Utilization of Health Informatics System Among Health Workers in Niger State, NigeriaEditor IJTSRDNo ratings yet
- Thesisproposalformat 110311092418 Phpapp01 PDFDocument23 pagesThesisproposalformat 110311092418 Phpapp01 PDFAilee MnrngNo ratings yet
- Patient EducationDocument18 pagesPatient Educationspalte48No ratings yet
- OxygenationDocument12 pagesOxygenationCherry Lou Guanzing100% (1)
- Colostomy CareDocument2 pagesColostomy CareMel RodolfoNo ratings yet
- Pulido, Nathaniel T. (Quiz - Activity 6)Document2 pagesPulido, Nathaniel T. (Quiz - Activity 6)Nathaniel PulidoNo ratings yet
- Group 2 - Telehealth and Older AdultDocument15 pagesGroup 2 - Telehealth and Older AdultErickson V. LibutNo ratings yet
- Stress and AdaptationDocument56 pagesStress and AdaptationKathleen Frugalidad100% (1)
- Manual Blood Pressure Competency ChecklistDocument1 pageManual Blood Pressure Competency Checklistshubham verma100% (1)
- Nursiing Management WR. Whole PackageDocument24 pagesNursiing Management WR. Whole Packageeyna30No ratings yet
- Home Visit and BAG TECHNIQUEDocument18 pagesHome Visit and BAG TECHNIQUESusan Intes RulidaNo ratings yet
- Complete Bed Bath2Document3 pagesComplete Bed Bath2rufino delacruzNo ratings yet
- Nursing 5 1092 PDFDocument4 pagesNursing 5 1092 PDFDared GesangNo ratings yet
- Operational Guidelines For HWCDocument83 pagesOperational Guidelines For HWCharleenNo ratings yet
- Nursing As A Profession-Nurse's Role DR S FarragDocument28 pagesNursing As A Profession-Nurse's Role DR S FarragAmwaj Mohammed100% (1)
- CourseSyllabus - NCM 103 FUNDA OF NSGDocument17 pagesCourseSyllabus - NCM 103 FUNDA OF NSGEmmyNo ratings yet
- Contemporary ImageDocument43 pagesContemporary ImageProf. L100% (1)
- Community As Client PDFDocument2 pagesCommunity As Client PDFNathan0% (1)
- Gordon's Health Pattern ChecklistDocument3 pagesGordon's Health Pattern ChecklistNavora, Bryle TrixthaneNo ratings yet
- FWPDocument37 pagesFWPhemaanandhyNo ratings yet
- National Health Mission (NHM) : 2.2.1 AshaDocument14 pagesNational Health Mission (NHM) : 2.2.1 AshaManisha MalikNo ratings yet
- Cultural Factor/ethnicity Such As Regard For Elders, Perception of HealthDocument3 pagesCultural Factor/ethnicity Such As Regard For Elders, Perception of HealthQueency Jane Ursulum100% (1)
- Health EducationDocument2 pagesHealth EducationLara NavarroNo ratings yet
- Alterations in Oxygenation 2Document18 pagesAlterations in Oxygenation 2alejandrino_leoaugustoNo ratings yet
- Aseptic TechniqueDocument7 pagesAseptic TechniqueRochele Buenavista- BuenaventuraNo ratings yet
- NURS 115 Course Syllabus 201910 DMLDocument41 pagesNURS 115 Course Syllabus 201910 DMLJade BouchardNo ratings yet
- Colombo PlanDocument2 pagesColombo PlanDenise LabagnaoNo ratings yet
- INNOVATIONS IN NURSING Final PDFDocument8 pagesINNOVATIONS IN NURSING Final PDFPatel AmeeNo ratings yet
- Fundamental of Nursing: Unit OneDocument13 pagesFundamental of Nursing: Unit OneSumaira NoreenNo ratings yet
- Public Health Nursing Community Health NursingDocument23 pagesPublic Health Nursing Community Health NursingJorge Danielle100% (1)
- Study Guide, Community Health Nursing Science 1Document55 pagesStudy Guide, Community Health Nursing Science 1Enos ErastusNo ratings yet
- Narrative Report-Mam Monsanto2Document3 pagesNarrative Report-Mam Monsanto2Annie Lucrecia Mallari AguinaldoNo ratings yet
- Skin PreparationDocument3 pagesSkin Preparationmckulit_joey100% (2)
- TRIAGE Skills LabDocument8 pagesTRIAGE Skills Labczeremar chanNo ratings yet
- Fundamentals of Nursing Practice LectureDocument19 pagesFundamentals of Nursing Practice LectureMJ ArazasNo ratings yet
- Personal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyDocument12 pagesPersonal Data of Patient: Intensive Nursing Practicum - Pediatric Ward (BMC) CASE STUDY 5: Pediatric OncologyromelynNo ratings yet
- Jean Watson - Philosophy & Caring TheoryDocument12 pagesJean Watson - Philosophy & Caring Theorydorothy kageni100% (1)
- Teaching Plan 2Document10 pagesTeaching Plan 2Terma JamiriNo ratings yet
- Healthcare Reflections, Insights, and Lessons: Proactive/ReactiveFrom EverandHealthcare Reflections, Insights, and Lessons: Proactive/ReactiveNo ratings yet
- Community Health A Complete Guide - 2020 EditionFrom EverandCommunity Health A Complete Guide - 2020 EditionRating: 5 out of 5 stars5/5 (1)
- Baked Banana Ok-WPS OfficeDocument2 pagesBaked Banana Ok-WPS OfficeJosephine ChirwaNo ratings yet
- Creamy Cooked S-WPS OfficeDocument2 pagesCreamy Cooked S-WPS OfficeJosephine ChirwaNo ratings yet
- Estigma and Mental Health A Proposal For Next StepsDocument6 pagesEstigma and Mental Health A Proposal For Next StepsJosephine ChirwaNo ratings yet
- Crossroads To Hope MHSA Sonoma Innovation Project ProposalDocument30 pagesCrossroads To Hope MHSA Sonoma Innovation Project ProposalJosephine ChirwaNo ratings yet
- CEEC2 - Industrial Yard - Application FormDocument8 pagesCEEC2 - Industrial Yard - Application FormJosephine ChirwaNo ratings yet
- Job Advert CEO For IDC 29 August 2022 Print Media FinalDocument2 pagesJob Advert CEO For IDC 29 August 2022 Print Media FinalJosephine ChirwaNo ratings yet
- 234 Proposal GUIDANCE Improving MH and Wellbeing in KenyaDocument30 pages234 Proposal GUIDANCE Improving MH and Wellbeing in KenyaJosephine ChirwaNo ratings yet
- 4 Bedroomed House For Sale With 2 Bedroomed Self-Contained, Tiled, in A Wall Fence, Well Designed, Location: Hills View, Price: K 1.2mDocument18 pages4 Bedroomed House For Sale With 2 Bedroomed Self-Contained, Tiled, in A Wall Fence, Well Designed, Location: Hills View, Price: K 1.2mJosephine ChirwaNo ratings yet
- CEEC1 Agricultural-Mechanisation Application-FormDocument7 pagesCEEC1 Agricultural-Mechanisation Application-FormJosephine ChirwaNo ratings yet
- CEEC1 - Auto Mechanics - Application FormDocument7 pagesCEEC1 - Auto Mechanics - Application FormJosephine ChirwaNo ratings yet
- Msopa Real Estate Update: Proprties On SaleDocument14 pagesMsopa Real Estate Update: Proprties On SaleJosephine ChirwaNo ratings yet
- 5 Lessons That Jacob's Night of Wrestling Teaches Us About PrayerDocument2 pages5 Lessons That Jacob's Night of Wrestling Teaches Us About PrayerJosephine Chirwa100% (1)
- Fact Sheets Forestry Business Proposals: Forestry Investments in Emerging MarketsDocument23 pagesFact Sheets Forestry Business Proposals: Forestry Investments in Emerging MarketsJosephine ChirwaNo ratings yet
- Zambia Urban Housing Sector ProfileDocument205 pagesZambia Urban Housing Sector ProfileJosephine ChirwaNo ratings yet
- Saia RPT 11 Dupreezchevallier 20120806Document77 pagesSaia RPT 11 Dupreezchevallier 20120806Josephine ChirwaNo ratings yet
- RELISA HOUSING CO OPERATIVE SOCIETY LIMITED CHAIRMAN'S REPORT TO THE 20TH ANNUAL GENERAL MEETING TO BE HELD ON THE 27th APRIL 2018Document11 pagesRELISA HOUSING CO OPERATIVE SOCIETY LIMITED CHAIRMAN'S REPORT TO THE 20TH ANNUAL GENERAL MEETING TO BE HELD ON THE 27th APRIL 2018Josephine ChirwaNo ratings yet
- Important Factors Responsible For Making Event Effective and EfficientDocument11 pagesImportant Factors Responsible For Making Event Effective and EfficientJosephine ChirwaNo ratings yet
- OHS Safety & Risk ManagementDocument9 pagesOHS Safety & Risk ManagementJosephine ChirwaNo ratings yet
- Business Management For Small-Scale Agro-Processors: Agsf Working DocumentDocument89 pagesBusiness Management For Small-Scale Agro-Processors: Agsf Working DocumentJosephine ChirwaNo ratings yet
- Memorandum and Articles of Association of Life With Hope TrustDocument36 pagesMemorandum and Articles of Association of Life With Hope TrustJosephine ChirwaNo ratings yet
- Mini-MBA in Food and Agribusiness Management SyllabusDocument12 pagesMini-MBA in Food and Agribusiness Management SyllabusJosephine ChirwaNo ratings yet
- Achievement of Environmental Goals at Visy: Management Accounting 1Document6 pagesAchievement of Environmental Goals at Visy: Management Accounting 1Josephine ChirwaNo ratings yet
- Traditional Land/ General Land AcquisitionDocument3 pagesTraditional Land/ General Land AcquisitionJosephine ChirwaNo ratings yet
- The Role of Foreign Banks in Emerging CountriesDocument32 pagesThe Role of Foreign Banks in Emerging CountriesJosephine ChirwaNo ratings yet
- (Company Name) : Contact: (NAME) (Address) (City, State Zip) Phone XXX-XXX-XXXX Fax XXX-XXX-XXXX (Email) (Website)Document38 pages(Company Name) : Contact: (NAME) (Address) (City, State Zip) Phone XXX-XXX-XXXX Fax XXX-XXX-XXXX (Email) (Website)Josephine ChirwaNo ratings yet
- Final Application Form-Ethanol Business Loan Mongu IYDocument8 pagesFinal Application Form-Ethanol Business Loan Mongu IYJosephine ChirwaNo ratings yet
- Call For Occupation - LusakaMansa&KitweDocument3 pagesCall For Occupation - LusakaMansa&KitweJosephine ChirwaNo ratings yet
- Annexure H Detailed Cvs of Esia Project TeamDocument111 pagesAnnexure H Detailed Cvs of Esia Project TeamEzzadin BabanNo ratings yet
- National ICT PolicyDocument65 pagesNational ICT PolicySechwayo NzimaNo ratings yet
- Deez Logs Business PlanDocument42 pagesDeez Logs Business PlanMundiya Muyunda KwalombotaNo ratings yet
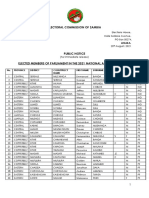
- Electoral Commission of Zambia: Elections House, Haile Selassie Avenue, PO Box 50274, 20 August, 2021Document4 pagesElectoral Commission of Zambia: Elections House, Haile Selassie Avenue, PO Box 50274, 20 August, 2021joseph katongoNo ratings yet
- Zambia Diaspora Submission To The Diaspora DeskDocument6 pagesZambia Diaspora Submission To The Diaspora DeskChola MukangaNo ratings yet
- Hope Development Institute Cover Letter For Open Pit Mine PimDocument1 pageHope Development Institute Cover Letter For Open Pit Mine Pimnorman kachambaNo ratings yet
- Group 1 Final Presentation-1Document16 pagesGroup 1 Final Presentation-1maureen chandaNo ratings yet
- ZEO Zambezi Environment OutlookDocument324 pagesZEO Zambezi Environment OutlookJosh Sam Rindai MhlangaNo ratings yet
- DAILY NATION Monday July 27, 2020 PDFDocument20 pagesDAILY NATION Monday July 27, 2020 PDFDixie CheeloNo ratings yet
- Zambian Traveller 83Document27 pagesZambian Traveller 83Clare Nkwanga-JollyNo ratings yet
- Civic Educations Rev Pamphlate-1Document68 pagesCivic Educations Rev Pamphlate-1Døps Maløne100% (11)
- ZRDC FormsDocument10 pagesZRDC FormsEustersia bwalya0% (1)
- Rhodesiana - Volume1Document35 pagesRhodesiana - Volume1remigeousNo ratings yet
- Null 5Document12 pagesNull 5Mansur BalaNo ratings yet
- Case Study - GIZ - Water KiosksDocument12 pagesCase Study - GIZ - Water KiosksDeniz KoseNo ratings yet
- Geography Part NotesDocument5 pagesGeography Part NotesDavid Ndumba100% (1)
- Kelvin Esiasa's CVDocument4 pagesKelvin Esiasa's CVapi-258191050No ratings yet
- Zambia Diaspora E-Conference 2008Document1 pageZambia Diaspora E-Conference 2008Chola MukangaNo ratings yet
- 2008 Zambia Diaspora Econference ReportDocument50 pages2008 Zambia Diaspora Econference ReportChola MukangaNo ratings yet
- 2019 Zambia Insurance Industry ReportDocument40 pages2019 Zambia Insurance Industry ReportWakari MastaNo ratings yet
- Relief of Zambia Grade 8 M Geog NotesDocument9 pagesRelief of Zambia Grade 8 M Geog NotesErnest100% (1)
- Natasha Mwansa PR Assignment 1Document15 pagesNatasha Mwansa PR Assignment 1Natasha Wang MwansaNo ratings yet
- 2015-2016 Annual ReportDocument51 pages2015-2016 Annual ReportMd. Mamunur RashidNo ratings yet
- The Zambian Peoples PACTDocument2 pagesThe Zambian Peoples PACTChola MukangaNo ratings yet
- BrochureDocument39 pagesBrochurePushparaj AlphonseNo ratings yet
- Choppies AR 2016Document104 pagesChoppies AR 2016Tefo MoggzNo ratings yet
- Grade 9 English - Article WritingDocument3 pagesGrade 9 English - Article WritingtestichilliesNo ratings yet
- CV +++Document5 pagesCV +++Andrew NkhuwaNo ratings yet