Professional Documents
Culture Documents
Wong 2016
Wong 2016
Uploaded by
Agnieszka SmagaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Wong 2016
Wong 2016
Uploaded by
Agnieszka SmagaCopyright:
Available Formats
Orthopedic Research and Reviews Dovepress
open access to scientific and medical research
Open Access Full Text Article REVIEW
3D-printed patient-specific applications
in orthopedics
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
This article was published in the following Dove Press journal:
Orthopedic Research and Reviews
14 October 2016
Number of times this article has been viewed
Kwok Chuen Wong Abstract: With advances in both medical imaging and computer programming, two-dimen-
Department of Orthopedics and
sional axial images can be processed into other reformatted views (sagittal and coronal) and
Traumatology, Prince of Wales three-dimensional (3D) virtual models that represent a patients’ own anatomy. This processed
Hospital, The Chinese University of digital information can be analyzed in detail by orthopedic surgeons to perform patient-specific
Hong Kong, Shatin, Hong Kong
For personal use only.
orthopedic procedures. The use of 3D printing is rising and has become more prevalent in medi-
cal applications over the last decade as surgeons and researchers are increasingly utilizing the
technology’s flexibility in manufacturing objects. 3D printing is a type of manufacturing process
in which materials such as plastic or metal are deposited in layers to create a 3D object from a
digital model. This additive manufacturing method has the advantage of fabricating objects with
complex freeform geometry, which is impossible using traditional subtractive manufacturing
Video abstract methods. Specifically in surgical applications, the 3D printing techniques can not only generate
models that give a better understanding of the complex anatomy and pathology of the patients
and aid in education and surgical training, but can also produce patient-specific surgical guides or
even custom implants that are tailor-made to the surgical requirements. As the clinical workflow
of the 3D printing technology continues to evolve, orthopedic surgeons should embrace the latest
knowledge of the technology and incorporate it into their clinical practice for patient-specific
orthopedic applications. This paper is written to help orthopedic surgeons stay up-to-date on
the emerging 3D technology, starting from the acquisition of clinical imaging to 3D printing
for patient-specific applications in orthopedics. It 1) presents the necessary steps to prepare
the medical images that are required for 3D printing, 2) reviews the current applications of 3D
printing in patient-specific orthopedic procedures, 3) discusses the potential advantages and
Point your SmartPhone at the code above. If you have a limitations of 3D-printed custom orthopedic implants, and 4) suggests the directions for future
QR code reader the video abstract will appear. Or use:
http://youtu.be/ORIOihXhHVs
development. The 3D printing technology has been reported to be beneficial in patient-specific
orthopedics, such as in the creation of anatomic models for surgical planning, education and
surgical training, patient-specific instruments, and 3D-printed custom implants. Besides being
anatomically conformed to a patient’s surgical requirement, 3D-printed implants can be fab-
ricated with scaffold lattices that may facilitate osteointegration and reduce implant stiffness.
However, limitations including high cost of the implants, the lead time in manufacturing, and
lack of intraoperative flexibility need to be addressed. New biomimetic materials have been
investigated for use in 3D printing. To increase utilization of 3D printing technology in ortho-
Correspondence: Kwok Chuen Wong
Department of Orthopedics and pedics, an all-in-one computer platform should be developed for easy planning and seamless
Traumatology, Prince of Wales Hospital, communications among different care providers. Further studies are needed to investigate the
The Chinese University of Hong Kong,
real clinical efficacy of 3D printings in orthopedic applications.
Shatin, Hong Kong
Tel +852 2632 3947 Keywords: 3D printing, patient-specific orthopedics, custom implants, patient-specific instru-
Fax +852 2637 7889 ment, image processing
Email skcwong@ort.cuhk.edu.hk
submit your manuscript | www.dovepress.com Orthopedic Research and Reviews 2016:8 57–66 57
Dovepress © 2016 Wong. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.
http://dx.doi.org/10.2147/ORR.S99614
php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the work
you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For
permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Powered by TCPDF (www.tcpdf.org)
Wong Dovepress
Introduction Patient-specific orthopedics
Orthopedics is a surgical discipline that is commonly tied to In traditional orthopedic procedures, surgeons have to
biomedical engineering, which has been applied to various mentally integrate all preoperative two-dimensional (2D)
orthopedic disciplines, ranging from trauma surgery, joint images and formulate a 3D surgical plan. This preoperative
arthroplasty, and tumor surgery to deformity correction. planning is particularly difficult in areas that have complex
One of the reasons for the success of these applications is anatomy and severe deformity or in cases of bone tumor
the contemporary medical imaging technologies that have surgery. With the advent of volumetric medical imaging and
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
allowed for detailed analysis of the individual’s musculo- computing technology, 2D axial images can be processed
skeletal system. With advances in both medical imaging and into other reformatted views (sagittal and coronal), and 3D
computing programming, virtual models that are representa- virtual models with patient-specific anatomy can be created.
tive of patients’ own anatomy can be generated for planning With improved visualization, surgeons can then analyze this
patient-specific orthopedic procedures. processed information to make more detailed diagnosis, plan-
From preoperative planning to training and education ning, and surgical intervention on a patient-specific basis.
to implant designing, the use of three-dimensional (3D) Although frequently used, the term “patient-specific” has
printing is rising and has become more prevalent in medical not been clearly defined. An orthopedic surgeon may intui-
applications over last decade as surgeons and researchers tively refer to it as the unique bone geometry or density that
are increasingly utilizing the technology’s flexibility in is assessed using the patient’s medical images. Other factors
manufacturing objects. 3D printing is a type of manufac- like material properties, design of orthopedic implants, or
For personal use only.
turing process in which materials such as plastic or metal force acting on an individual patient may be incorporated
are deposited in layers to create a 3D object from a digital qualitatively in the decision of “patient-specific” orthopedic
model.1 The process is distinct from traditional manufactur- treatment. On the other hand, the outcome for a particular
ing methods in that it is an additive rather than a subtractive treatment is based on the results of clinical trials that are
process. Specifically in surgical applications, the 3D printing only average estimates of different patients within the trials.
techniques can not only generate models that give a better These average results might not apply directly to individual
understanding of the complex anatomy and pathology of the patients for whom surgeons care.17 In biomedical engineer-
patients,2 but can also produce patient-specific instruments ing, patient-specific modeling (PSM) is the development of
(PSIs)3–11 or even custom implants12,13 that are tailor-made computational models of human pathophysiology that are
to the surgical requirements. personalized to patient-specific data.18 PSM is gaining more
Only a few papers have recently reviewed the 3D print- attention because of its potential to optimize an individual’s
ing technology and its medical applications.2,14–16 However, treatment by predicting outcomes of surgical interventions.
they were reported mainly from the perspectives of radiolo- It has been utilized in optimizing the preoperative planning
gists, surgeons, and engineers. Although relevant studies of periacetabular osteotomies in hip dysplasia19,20 and in
and clinical data on 3D printing in orthopedics are limited, predicting the outcome of corrective surgery in scoliosis21,22
its potential in personalized treatment in orthopedics is and bony reconstruction with a custom implant after complex
huge. As the clinical applications of 3D printing continue pelvic tumor resection.23 Although PSM is beyond the scope
to evolve, orthopedic surgeons should embrace the latest of discussion of this paper, the combination of PSM and 3D
knowledge of the technology and incorporate it into their printing technology has been increasingly used in patient-
clinical practice for possible benefits to patients. This paper specific orthopedic applications such as for the creation of
is written to help orthopedic surgeons stay up-to-date on the anatomic models for surgical planning, education and train-
emerging 3D technology, starting from the acquisition of ing, PSIs, and custom implants (Figure 1).
clinical imaging to 3D printing for patient-specific applica-
tions in orthopedics. The paper 1) presents the necessary Image acquisition to generation of 3D
steps to prepare the medical images that are required for 3D objects
printing, 2) reviews the current applications of 3D printing For patient-specific analysis in orthopedic applications, accu-
in patient-specific orthopedic procedures, 3) discusses the rate medical imaging data must be obtained to represent an
potential advantages and limitations of 3D-printed custom individual patient. The modern multirow detector computer
orthopedic implants, and 4) suggests the directions for tomography (MDCT) and magnetic resonance imaging
future development. (MRI) provide fast and accurate 3D image data with high
58 submit your manuscript | www.dovepress.com Orthopedic Research and Reviews 2016:8
Dovepress
Powered by TCPDF (www.tcpdf.org)
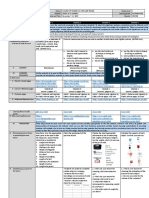
Dovepress 3D printing for patient-specific orthopedics
A B
Medical images
Surgeons (CT ± MR)
Image processing
Patient
specific
modeling C D
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
Surgical planning
FEA
Engineers evaluation
Patient-specific Figure 2 Axial CT images were acquired in a patient with low-grade osteosarcoma
Anatomical instruments Custom
involving the sacrum (red arrows).
models implants Notes: The CT images in DICOM format were imported into a CAD engineering
3D printing program. As the sacrum was at a tilted position during CT scanning, the image
data set could be resliced to allow better visualization of sacrum in its anatomical
alignment. The extent of the tumor could also be segmented manually from the
Patient-specific images. The reformatted axial (A), coronal (B), and sagittal (C) views, and the
orthopaedics 3D bone-tumor model (D) enabled surgeons to analyze the patient’s anatomy and
pathology accurately for customized surgical planning.
Abbreviations: CT, computer tomography; CAD, computer-aided design;
Figure 1 This image summarizes the clinical workflow of patient-specific
For personal use only.
DICOM, digital imaging and communications in medicine.
orthopedics from image acquisition to 3D-printed models and implants.
Notes: The workflow requires close collaboration between surgeons and engineers
to achieve the surgery that is customized to the patient’s anatomy and surgical
requirement.
image postprocessing as the image quality of the MRI can be
Abbreviations: CT, computer tomography; MR, magnetic resonance; FEA, finite
element analysis. adversely affected by movement artifacts generated during
the long scanning times.25 Therefore, image postprocessing
resolution. With image postprocessing tools, it is possible to in orthopedic applications is mainly based on CT images
produce multiplanar reformatted 2D images and 3D views and supplemented with tissue information from MRI. All
of the patient’s anatomy. The technique of converting digital the acquired medical images are saved in digital imaging and
medical images into a 3D physical object has been described communications in medicine (DICOM), which is a standard
in detail in a previously published review article.14 The con- data format to store, exchange, and transmit medical images.
version consists of three steps: 1) image acquisition, 2) image
postprocessing, and 3) 3D printing. Image postprocessing
Image postprocessing software extracts DICOM images
Image acquisition for data reconstruction. Thin-section axial images are used
High-quality medical images must be acquired first as the to create nonaxial 2D images by means of multiplanar ref-
resolution of 3D objects generated from medical images is ormation.24 The additional reformatted coronal or sagittal
dependent on the resolution of the medical images them- images can then be visualized for better clinical interpretation
selves. The quality of the 3D object cannot outreach the (Figure 2). This technique is particularly useful for examin-
quality of its raw 2D imaging data. Both MDCT and MRI ing skeletal structures as some information like fractures or
are commonly used imaging modalities. Because of high joint alignment may not be readily apparent on axial sections.
contrast in CT, it is the imaging modality of choice in ortho- Other 3D visualization tools such as volume rendering gener-
pedics when bones are the region of interest for an imaging ate 3D representations of the data set. Image segmentation is
study. MDCT can produce thin-section axial image with usually required to select regions of interest within the image
slice thickness of less than 1 mm and isotropic voxel. These data. Thresholding voxel intensity value is a technique that
high-resolution CT images are ideal to facilitate the image is commonly applied in segmenting regions that uniformly
postprocessing for 3D applications.24 MRI has the advan- differ in intensity from their surrounding tissue, such as bone.
tage of no radiation exposure during image acquisition. It 3D objects can be generated from the segmented regions of
is superior to CT in delineating soft tissue anatomy, such as interest. Computer-aided design (CAD) software transforms
that of articular cartilage in joint disease and intramedullary the contour of a 3D model into a series of polygons, usu-
or extraossoeus extension in orthopedic tumors. However, it ally triangles, the number of which directly correlates with
is more difficult to obtain thin 1–2 mm thick MR slices for resolution.26 The CAD information is then converted into a
Orthopedic Research and Reviews 2016:8 submit your manuscript | www.dovepress.com
59
Dovepress
Powered by TCPDF (www.tcpdf.org)
Wong Dovepress
common 3D file format, STereoLithography (STL). Further by one layer thickness after scanning of each cross section. A
editing of the STL files like optimization of triangular meshes new layer of material is then applied on top, and the process
or modification of object geometries can be performed before is repeated until the fabrication is completed. In contrast with
the CAD data are sent to a 3D printing machine for object other 3D printing technology such as SLA and FDM, which
fabrication (Figure 3). Therefore, DICOM images are the requires special supporting structures to fabricate overhanging
key link between 3D printing technology and patient-specific designs, SLS or EBM does not require supporters because the
medical imaging data in orthopedics.26 model being constructed is surrounded by unsintered powder
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
at all times. This allows fabrication of objects with previously
3D printing impossible complex geometries.
CAD software analyzes the STL file that represents the 3D
model to be fabricated and “slices” the model into a series of Applications of 3D printing in
cross-sectional layers. A 3D printing machine then fabricates patient-specific orthopedics
the 3D physical model by adding successive layers of material In the last decades, 3D printing has undergone tremendous
to recreate the virtual cross sections. The 3D printing technol- development and now has important applications in various
ogy used in medicine can be classified according to the tech- fields of medicine. However, reports on orthopedic applica-
nique of manufacturing. It mainly includes stereolithography tions are limited and mainly consist of case reports or small
apparatus (SLA), fused deposition modeling (FDM), selective series. They include anatomic models for surgical planning,
laser sintering (SLS), or electron beam melting (EBM).14,15 education and training, PSI for assisting surgical procedures,
For personal use only.
The liquid-based 3D printing technology of SLA makes suc- and fabrication of complex custom metal implants.
cessive layers by using photosensitive resin that is cured by an
ultraviolet laser. The solid-based 3D printing technology of Anatomic models for surgical planning
FDM works by the extrusion of small beads of melted thermo- In traditional preoperative planning, orthopedic surgeons
plastic materials, from a small nozzle, that harden afterward utilized 2D plain X-ray and CT images to assess the bony
to form layers. The powder-based 3D printing technology of anatomy and pathology of the patient. As more advanced
SLS or EBM involves the use of a focused laser or electron image postprocessing software can generate 3D nonaxial
beam to selectively fuse small particles of plastic or metal on reformatted images and 3D images, patient-specific treatment
the surface of a powder bed. The focused energy scans each choice(s) can be selected by studying all the digital images.
layer according to the cross section generated from the STL Despite these advances in image processing technology,
file of the fabricated 3D object. The powder bed is reduced the 3D anatomy is still being viewed as a flat, 3D image.
A B C
Image acquisition Image postprocessing 3D printing
CT/MR images Volume rendering (3D visualization) Physical models
Axial images in DICOM 3D CAD models with 3D-printed custom
surgical simulation implants
Figure 3 Summary of the steps in patient-specific orthopedics in a patient with low-grade chondrosarcoma involving the anterior acetabulum of pelvis and a partial acetabular
tumor resection and reconstruction with a 3D-printed custom implant was planned.
Notes: The steps consist of image acquisition (A), image postprocessing (B), and 3D printing (C).
Abbreviations: DICOM, digital imaging and communications in medicine; CAD, computer-aided design; CT, computer tomography; MR, magnetic resonance; 3D, three-
dimensional.
60 submit your manuscript | www.dovepress.com Orthopedic Research and Reviews 2016:8
Dovepress
Powered by TCPDF (www.tcpdf.org)
Dovepress 3D printing for patient-specific orthopedics
Patient-specific physical bone models can be recreated from Education and surgical training
patients’ CT image data by 3D printing. The models not only Patient-specific 3D-printed models can be used for education
allow surgeons to have tactile and visual understanding of and preoperative discussions about surgical strategies and
the patient-specific anatomy and pathology, but also antici- options among care providers across different disciplines.
pate the operative challenges that will aid in the planning of The use of the models has been reported in various pedi-
orthopedic procedures. atric orthopedic disorders, such as Perthe’s disease, Blount
3D physical models have been reported to be helpful in disease, physeal bars, or coalitions.33 These models could
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
surgical treatment of complex acetabular27–29 and clavicle assist surgeons, therapists, and patients to understand bet-
fractures.30 The models aided in better understanding of ter the patients’ musculoskeletal pathology. Patient-specific
acetabular fractures and significantly reduced the degree fracture models have also been used to improve the consent
of interobserver variation in the classification of these frac- process in patients with complex acetabular fractures. It may
tures.31 The metal plates could also be placed to the fracture increase the patient satisfaction as patients and their families
bone model and bent to match the reduced bone fracture can now easily understand their medical conditions with real
surface prior to the actual surgery.28,30 The precontoured plates physical models.29 Postoperatively, these physical models and
could then be used to assess and assist in fracture reduction, their electronic CAD files could be kept to build a library of
and these have even facilitated minimally invasive plating various types of fracture so that the models can be 3D-printed
in comminuted clavicle fractures.30 In a prospective obser- again when necessary. Such a collection of fracture models
vational study of the surgeons’ perceptions of 3D printed are useful educational tools for surgeons, other physicians,
For personal use only.
models to assist with complex surgical cases in pediatric spine and medical students.29
and pelvis with anomalies, significant benefits were rated in Although the use of 3D-printed models has not been
designing a surgical plan, selecting implant type or external reported in surgical training in orthopedics, the potential
fixator, intraoperative reference of patients’ anatomy, preci- benefits are obvious. Majority of the surgeons just train in the
sion of osteotomies, and communication with patients.32 The operating theater. This may place patients at risk when sur-
operative time may even be reduced in cases of congenital geons are trying to master certain surgical skills at the initial
spinal deformity due to improvement in 3D understanding learning curve. With tangible solid models, senior surgeons
of the condition and surgical planning.32 In the author’s can convey their surgical experience to residents much more
experience, patient-specific 3D-printed models can also be easily. In addition, as complex or rare cases such as deformity
sterilized so that the surgeon can manipulate the model on correction, fracture fixation, or bone tumor resection may
the operative field while performing the procedure. It may not be normally seen during resident training, 3D-printed
help confirm surgical anatomy and guide resection in bone models of the cases can provide residents or junior surgeons
tumor surgery (Figure 4A). unique opportunities for authentic simulation-based surgical
training. Besides enhancing surgeons’ understanding of the
A B
orthopedic conditions, surgical practice on prototypes created
by 3D printing enables surgeons to be more familiar with
the patient-specific scenarios before they actually perform
similar procedures in real clinical setting. It may improve
patients’ safety.
Patient-specific instruments
PSI is customized on the basis of the 3D surface model of
bony anatomy, which is generated by image segmentation of
a patient’s imaging data. The design is then fabricated by 3D
printing technology for orthopedic applications (Figure 4B).
Figure 4 (A) This image shows surgical exposure in a patient with humeral shaft This customized tool is used with an intention of easily repli-
bone sarcoma undergoing intercalary tumor resection. The 3D-printed PSM with cating surgical plans that involve guiding a saw and/or drill in
planned resections (red arrows) could be used for easy intraoperative reference of
the surgical plan. 3D-printed PSIs and bone models (B) were fabricated preoperatively a specific planned direction. PSI has been reported in pedicle
for a joint-saving tumor resection in a 9-year-old patient with femur osteosarcoma.
screw insertion for spinal surgery in the cervical4 or thoracic
Abbreviations: 3D, three-dimensional; PSM, patient-specific model; PSI, patient-
specific instrument. region,3 for performing difficult osteotomies in deformity
Orthopedic Research and Reviews 2016:8 submit your manuscript | www.dovepress.com
61
Dovepress
Powered by TCPDF (www.tcpdf.org)
Wong Dovepress
correction of fracture malunion,6,10 and for guiding accurate a custom implant is a perfect match for the unique anatomy
implant placement in total knee and hip arthroplasty.5,7,9 The of that patient as it is based on the patient’s own medical
use of PSI has also recently been described in bone tumor images. Custom implants may be indicated when 1) patients’
surgery. It might help improve the bone resection accuracy bony geometries fall outside the range of standard implants
for oncological clearance11 and the matching of a customized with respect to implant size- or disease-specific requirements,
tumor implant to the bone defect after tumor resection.8,23 and 2) improved surgical results are anticipated due to a
In contrast to computer navigation-assisted techniques better fit between implants and patients’ anatomical needs.14
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
that require bulky navigation facilities and a machine opera-
tor, PSI technique has the theoretical benefit of improving Potential advantages and limitations
surgical accuracy by using simple personalized instruments of 3D-printed custom implants
with minimal operative setup and without distraction from The nature of additive layer manufacturing in 3D printing
the surgical field. However, two recent meta-analyses did not allows fabrication of custom implants with any complex
support the routine use of PSI in total knee arthroplasty as shape or geometric feature; this is impossible using tradi-
it was not shown to provide superior accuracy to using con- tional subtractive manufacturing techniques. In addition
ventional manual instrumentation.31,34 One of the limitations to the advantage of being anatomically conformed to an
in PSI technique is incorrect placement of a PSI on the bone individual patient, a 3D-printed implant can be generated
surface determined during PSI design per the CAD software. with a complex free-form surface such as scaffold lattice in a
The accurate fit between a PSI and its predetermined bone metal monoblock (Figure 5). This interconnected pore surface
For personal use only.
surface requires that the chosen bone contact surface or structure has the potential to facilitate osteointegration and
footprint should have sufficient registration features for stable therefore the possibility to reduce the stiffness mismatch at
positioning of PSI. A footprint with more contoured bone bone–implant junctions.38,39 The stress-shielding problem
surface may improve the fit. In addition, accurate bone seg- may be further minimized as the porosity and pore size in
mentation from the preoperative image data set (CT or MRI) the implants can be modified40 and the elastic modulus of
is important to depict the real bony anatomy for PSI design. porous titanium can be tailored to be comparable to that
In patients with osteoarthritis undergoing PSI-assisted joint of the patient’s bone with the use of modern 3D printing
arthroplasty, the depiction of osteophytes in CT images can techniques.41 Therefore, the modern design of a 3D-printed
be unreliable and can possibly result in errors in determining custom implant not only has the structural geometry that can
PSI footprint, which should exactly match the bone surface match the surgical requirements of an individual patient, but
with osteophytes.35 Unlike the navigation-assisted technique, also allows biomechanical evaluation under patient-specific
the PSI technique does not have the intraoperative visual loading conditions for design modification prior to the actual
feedback of preoperative images that can reveal errors.36,37 implant fabrication.23,42
Inaccurate placement of a PSI and the subsequent incorrect The use of 3D-printed custom implants has recently
guided procedure may be undetected intraoperatively and been reported in difficult revision hip arthroplasty with
may result in deviation error from the planned procedures. severe acetabular bone loss.12 Sixteen patients with large
Currently, accurate intraoperative PSI placement relies acetabular defects underwent revision hip arthroplasty
mainly on the subjective feeling of the fit by surgeons. Stud- using 3D-printed custom trabecular titanium implants. The
ies are needed to investigate how much footprint at the bone implants were designed from a detailed analysis of patients’
contact is sufficient for consistent positioning of a PSI.8 In CT images with special reference to the bone quality and
addition, possible intraoperative methods to quantitatively the bone geometry of deficient acetabulum. The implant
verify the correct positioning of the PSI should be determined consisted of a porous augment and cage that recreated the
as they might help minimize registration errors of the PSI.35 artificial acetabulum. Flanges were added to the design for
optimum screw fixation to the remaining pelvic bone. Patient-
3D-printed custom implants specific aids and instruments such as 3D-printed physical
Off-the-shelf, standard-sized bone implants are mainly fab- models of the hemipelvis, trial implants, and drill guides
ricated using traditional subtractive manufacturing method. were provided for preoperative rehearsal and intraoperative
They are readily available to meet the surgical requirement for reference and guidance. However, difficulty was reported in
most patients. In contrast to an off-the-shelf implant in that placing the custom implants accurately as planned in 7 out
the patient’s anatomy may need to be modified for a proper fit, of 16 implants, which were found to be malpositioned in
62 submit your manuscript | www.dovepress.com Orthopedic Research and Reviews 2016:8
Dovepress
Powered by TCPDF (www.tcpdf.org)
Dovepress 3D printing for patient-specific orthopedics
A arthroplasty in patients with osteoarthritis. On the basis of
the patient’s CT images, the implant is customized to match
to each patient’s knee with unique shape and contour, thus
optimizing bone preservation. A disposable set of person-
C alized instrumentation is also provided with each implant
to replicate the planned bone cuts. It may reduce implant
inventory for the hospital when compared with the traditional
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
off-the-shelf knee implants. However, it remains to be seen
B whether the potential benefit of this patient-specific implants
can actually translate into a better clinical outcome.
Although the potential clinical performance of 3D printed
custom implants can be outstanding owing to their ability
to address reconstructive challenges that are beyond the
scope of off-the-shelf implants, limitations of this emerging
technology should be noted. The concerns include the high
Figure 5 (A) and (B) The figures show a 3D-printed custom implant for acetabular cost of the implants, the lead time required in designing
reconstruction in the patient with low-grade chondrosarcoma. The implant has a and manufacturing to meet the surgical deadlines, the lack
solid plate, flanges, and an acetabular cup with screw holes for fixation. The scaffold
lattice (C) contains an interconnected network of pores with an average porosity of intraoperative flexibility, and the difficulty of achieving
For personal use only.
of 70%.
accurate implant placement.16 The initial cost of custom
Notes: The pores have an average size of 720 µm and the thickness of the solid
struts is about 350 µm. The porous construct can facilitate the bone ingrowth at the implants may be higher than off-the-shelf implants. However,
bone–implant interface for better implant longevity. In addition, it is highly resistant
to mechanical compression, while its elastic modulus is similar to that of bone to
3D printing can generate custom implants with structural
minimize the stress-shielding problem around the implant. geometry that would be impossible using traditional subtrac-
Abbreviation: 3D, three-dimensional.
tive technique irrespective of costs. Therefore, it is better to
one or more parameters of measurement. This was the only evaluate with reference to the total procedural costs from the
study that addressed the accuracy of placement of custom preoperative planning, the implant design and manufacturing,
acetabular implants by comparing the preoperative CT plan- the implementation of surgical procedures, and the long-
ning with CT data on the postoperative position. Further term clinical outcomes. The potential excellent long-term
follow-up is needed to evaluate the clinical outcome of this performance of the custom implants may reduce the costly
new 3D-printed custom implant. revision surgeries due to implant-related failures and result in
Bone tumor resection creates a bone defect that needs lower overall lifetime costs.16 With the advances in computer
reconstruction to restore skeletal stability and function. design software and 3D printing technology, biomedical
3D-printed tumor implants may be the ideal reconstructive engineers and implant manufacturers can integrate the whole
solutions as they can be customized to match various shapes planning process from 3D image data processing to complex
of the bone defects after tumor resection. Early reports have custom implant fabrication via the close collaboration with
suggested that the custom implants were useful for recon- surgeons. Therefore, the turnaround time of the implant fab-
struction in clavicular, scapular, or pelvic bone tumors, which rication may be further reduced and the 3D-printed custom
have unique bony geometry and no available off-the-shelf implants can be a suitable adjunct for most patients in the
prosthesis.13,23 In addition, prefabricated custom implants future. In addition, post 3D printing steps, such as surface
and 3D models allowed surgeons to evaluate and better finishing and cleaning of metal powders in scaffold lattice,
understand the surgical procedures prior to the actual surgery. are essential to provide suitable and flawless 3D-printed
To achieve a good fit of the custom implants, surgeons may objects to surgeons. Sterilization of physical models with
require guiding tools such as PSI23 or computer navigation43 to materials not resistant to high temperature may raise a
replicate the same resection planes as planned per the design critical issue for intraoperative use. Implant-related infection
software. This patient-specific tumor implants may gain may be a concern as the lattice structure may increase the
more attention and popularity in bone tumor surgery when hospitable surface for microbial adherence that is difficult
the digital and manufacturing technology further advances. to eradicate. Finally, some regulatory considerations in the
A custom patient-specific knee implant (ConforMIS, design and manufacturing of 3D-printed custom implants
Bedford, MA, USA) is commercially available for knee remain challenging for hospitals as there are currently
Orthopedic Research and Reviews 2016:8 submit your manuscript | www.dovepress.com
63
Dovepress
Powered by TCPDF (www.tcpdf.org)
Wong Dovepress
limited regulatory standards that monitor the safety of these The current workflow from clinical imaging to 3D
3D-printed custom products.26 Overall, although the clini- printing of physical models requires multiple separate
cal data to support the routine use of the 3D-printed custom software that are designed for use mainly by biomedical
implants are currently limited, the integration of advanced engineers. Surgeons might not easily master the steps
3D design and 3D printing technology with PSI or computer in the working process such as image postprocessing,
navigation-assisted implant placement is very promising as creating 3D images that highlight of regions of interest,
it may further enhance the performance of custom implants planning the surgery with various reconstructive options,
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
in patient-specific orthopedics. and even preoperative biomechanical evaluation of the
implant design or a reconstructive method. To increase
Directions for potential future the popularity of 3D printing technology among orthope-
developments dic surgeons, an integrated all-in-one computer platform
A few years ago, only plastics could be 3D-printed into should be developed to allow for easy planning and
anatomic models and PSIs. Then, metal powders, such as seamless communication among different care providers
titanium or cobalt-chrome, were used to fabricate custom like radiologists, orthopedic surgeons, engineers, and
implants by 3D printing. The advances in biomimetic mate- implant companies. All the digital orthopedic data can
rials for 3D printing will be one major direction for future be integrated to facilitate customized patient treatments.
development in 3D printing technology in patient-specific Surgeons may then choose which 3D-printed products are
orthopedics. The material should be biocompatible and steril- most appropriate for their patients.
For personal use only.
izable for intraoperative use. 3D-printed artificial bone should
consist of materials with mechanical properties similar to Conclusion
the native bone, which might help restore bony anatomi- The advent of image processing and 3D printing technology
cal structures and biomechanical function. One example is is opening up many opportunities in patient-specific applica-
polyether ether ketone (PEEK), which has been used as an tions in orthopedics. The modern high-resolution medical
effective biomaterial for implantable medical devices. This imaging data can further be processed to create 3D images
high-performance thermoplastic can now be 3D printed that are essential for 3D printing of physical objects. The
to make durable, lightweight, and geometrically complex 3D printing technology has been reported to be beneficial
objects. Besides offering exceptional strength along with in patient-specific orthopedics, such as for the creation
superior heat and chemical resistance, PEEK has a modulus of anatomic models for surgical planning, education and
of elasticity closer to that of cortical bone, which might help surgical training, PSIs, and 3D-printed custom implants.
minimize stress-shielding effects in orthopedic implants.44,45 Besides being anatomically conformed to a patient’s surgical
PEEK has been used as reconstructive cages in cervical spine requirement, 3D-printed implants can be fabricated with scaf-
surgery.46 It is yet to be demonstrated if 3D-printed PEEK fold lattices that may facilitate osteointegration and reduce
artificial bones or implants are beneficial in patient-specific implant stiffness. Early results in revision hip arthroplasty
orthopedics. and bone tumor surgery have been promising. However,
Drug delivery is the method of administering a pharma- limitations including high cost of the implants, the lead time
ceutical compound to achieve a therapeutic effect in cells in manufacturing, and lack of intraoperative flexibility need
and humans. 3D printing technology has been successfully to be addressed. Materials like PEEK, which are biocompat-
incorporated into drug delivery systems to fabricate 3D ible and have superior strength and heat resistance, have been
scaffolds with biomolecules or pharmaceutical compounds.47 investigated for use in 3D printing. In addition, 3D printing
The combination of 3D printing technology and drug deliv- has been incorporated into drug delivery systems that may
ery systems has been suggested for surgery in tuberculous restore bony anatomy and deliver therapeutic compound
spinal infection. Poly-DL-lactide and nanohydroxyapatite, to the target tissue. To increase utilization of 3D printing
two promising drug delivery systems and materials for bone technology in orthopedics, an all-in-one computer platform
repair, were mixed with antituberculosis drugs to fabricate should be developed for easy planning and seamless com-
a 3D porous scaffold via 3D printing technology.48 The con- munication among different care providers. Further objective
struct may provide sufficient mechanical properties for spinal investigation into the clinical efficacy of the technology is
stabilization, encourage bone growth, and function as drug needed before one can put the technology into routine clinical
delivery platforms for treating tuberculosis. practice in orthopedics.
64 submit your manuscript | www.dovepress.com Orthopedic Research and Reviews 2016:8
Dovepress
Powered by TCPDF (www.tcpdf.org)
Dovepress 3D printing for patient-specific orthopedics
Disclosure 19. Lepisto J, Armand M, Armiger RS. Periacetabular osteotomy in
adult hip dysplasia – developing a computer aided real-time biome-
The Materialise, Mobelife company did not fund or sponsor chanical guiding system (BGS). Suom Ortoped Traumatol. 2008;31:
this research in any way. The author reports no conflicts of 186–190.
20. Armiger RS, Armand M, Tallroth K, Lepisto J, Mears SC. Three-
interest in this work. dimensional mechanical evaluation of joint contact pressure in 12
periacetabular osteotomy patients with 10-year follow-up. Acta Orthop.
2009;80:155–161.
References 21. Lafon Y, Lafage V, Dubousset J, Skalli W. Intraoperative three-dimen-
1. Schubert C, Van Langeveld MC, Donoso LA. Innovations in 3D print- sional correction during rod rotation technique. Spine. 2009;34:512–519.
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
ing: a 3D overview from optics to organs. Br J Ophthalmol. 2014; 22. Wang X, Aubin CE, Labelle H, Crandall D. Biomechanical modelling
98:159–161. of a direct vertebral translation instrumentation system: preliminary
2. Martelli N, Serrano C, van den Brink H, et al. Advantages and disad- results. Stud Health Technol Inform. 2008;140:128–132.
vantages of 3-dimensional printing in surgery: a systematic review. 23. Wong KC, Kumta SM, Geel NV, Demol J. One-step reconstruction with
Surgery. 2016;159(6):1485–1500. a 3D-printed, biomechanically evaluated custom implant after complex
3. Mac-Thiong JM, Labelle H, Rooze M, Feipel V, Aubin CE. Evaluation of pelvic tumor resection. Comput Aided Surg. 2015;20(1):14–23.
a transpedicular drill guide for pedicle screw placement in the thoracic 24. Dalrymple NC, Prasad SR, Freckleton MW, Chintapalli KN. Infor-
spine. Eur Spine J. 2003;12:542–547. matics in radiology (info-RAD): introduction to the language of
4. Lu S, Xu YQ, Lu WW, et al. A novel patient-specific navigational three-dimensional imaging with multidetector CT. Radio-Graphics.
template for cervical pedicle screw placement. Spine. 2009; 2005;25:1409–1428.
34(26):E959–E966. 25. Wong KC, Kumta SM, Antonio GE, Tse LF. Image fusion for
5. Hananouchi T, Saito M, Koyama T, Sugano N, Yoshikawa H. Tailor- computer-assisted bone tumor surgery. Clin Orthop Relat Res.
based surgical guide reduces incidence of outliers of cup placement. 2008;466(10):2533–2541.
Clin Orthop Relat Res. 2010;468:1088–1095. 26. Trace AP, Ortiz D, Deal A, et al. Radiology’s emerging role in 3-D
6. Miyake J, Murase T, Moritomo H, Sugamoto K, Yoshikawa H. Distal printing applications in health care. J Am Coll Radiol. 2016;13(7):
For personal use only.
radius osteotomy with volar locking plates based on computer simula- 856–862.
tion. Clin Orthop Relat Res. 2011;469(6):1766–1773. 27. Brown GA, Milner B, Firoozbakhsh K. Application of computer-gener-
7. Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV Jr. Improved ated stereolithography and interpositioning template in acetabular frac-
accuracy of alignment with patient-specific positioning guides compared tures: a report of eight cases. J Orthop Trauma. 2002;16(5): 347–352.
with manual instrumentation in TKA. Clin Orthop Relat Res. 2012; 28. Hurson C, Tansey A, O’Donnchadha B, Nicholson P, Rice J, McElwain
470(1):99–107. J. Rapid prototyping in the assessment, classification and preoperative
8. Wong KC, Kumta SM, Sze KY, Wong CM. Use of a patient-specific planning of acetabular fractures. Injury. 2007;38(10):1158–1162.
CAD/CAM surgical jig in extremity bone tumor resection and 29. Niikura T, Sugimoto M, Lee SY, et al. Tactile surgical navigation
custom prosthetic reconstruction. Comput Aided Surg. 2012;17(6): system for complex acetabular fracture surgery. Orthopaedics. 2014;
284–293. 37:237.
9. Buller L, Smith T, Bryan J, Klika A, Barsoum W, Innotti JP. The use of 30. Kim HN, Liu XN, Noh KC. Use of a real-size 3D-printed model as
patient-specific instrumentation improves the accuracy of acetabular a preoperative and intraoperative tool for minimally invasive plating
component placement. J Arthroplasty. 2013;28:631–636. of comminuted midshaft clavicle fractures. J Orthop Surg Res. 2015;
10. Takeyasu Y, Oka K, Miyake J, Kataoka T, Moritomo H, Murase T. 10:91.
Preoperative, computer simulation-based, three-dimensional corrective 31. Voleti PB, Hamula MJ, Baldwin KD, Lee GC. Current data do not
osteotomy for cubitus varus deformity with use of a custom-designed support routine use of patient-specific instrumentation in total knee
surgical device. J Bone Joint Surg Am. 2013 20;95(22):e173. arthroplasty. J Arthroplasty. 2014;29(9):1709–1712.
11. Gouin F, Paul L, Odri GA, Cartiaux O. Computer-assisted planning and 32. Guarino J, Tennyson S, McCain G, Bond L, Shea K, King H. Rapid
patient-specific instruments for bone tumor resection within the pelvis: prototyping technology for surgeries of the pediatric spine and pelvis:
a series of 11 patients. Sarcoma. 2014;Article ID 842709:9. benefits analysis. J Pediatr Orthop. 2007;27(8):955–960.
12. Baauw M, van Hellemondt GG, van Hooff ML, Spruit M. The accuracy 33. Starosolski ZA, Kan JH, Rosenfeld SD, Krishnamurthy R, Annapragada
of positioning of a custom-made implant within a large acetabular A. Application of 3-D printing (rapid prototyping) for creating physi-
defect at revision arthroplasty of the hip. Bone Joint J. 2015;97-B(6): cal models of pediatric orthopedic disorders. Pediatr Radiol. 2014;
780–785. 44:216.
13. Fan H, Fu J, Li X, et al. Implantation of customized 3-D printed tita- 34. Cavaignac E, Pailhé R, Laumond G, et al. Evaluation of the accuracy
nium prosthesis in limb salvage surgery: a case series and review of of patient-specific cutting blocks for total knee arthroplasty: a meta-
the literature. World J Surg Oncol. 2015;13:308. analysis. Int Orthop. 2015;39(8):1541–1552.
14. Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing 35. Kunz M, Balaketheeswaran S, Ellis RE, Rudan JF. The influence of
based on imaging data: review of medical applications. Int J Comput osteophyte depiction in CT for patient-specific guided hip resurfacing
Assist Radiol Surg. 2010;5:335–341. procedures. Int J Comput Assist Radiol Surg. 2015;10(6):717–726.
15. Kim GB, Lee S, Kim H, et al. Three-dimensional printing: basic prin- 36. Leeuwen JA, Grøgaard B, Nordsletten L, Röhrl SM. Comparison of
ciples and applications in medicine and radiology. Korean J Radiol. planned and achieved implant position in total knee arthroplasty with
2016;17(2):182–197. patient-specific positioning guides. Acta Orthop. 2014;11:1–6.
16. Unwin PS, Eshraghi A. Custom implants. In: Ritacco LE, Milano 37. Wong KC, Sze KY, Wong IO, Wong CM, Kumta SM. Patient-specific
FE, Chao E, editors. Computer-Assisted Musculoskeletal Sur- instrument can achieve same accuracy with less resection time than
gery: Thinking and Executing in 3D. Switzerland: Springer; 2016; navigation assistance in periacetabular pelvic tumor surgery: a cadaveric
181–198. study. Int J Comput Assist Radiol Surg. 2016;11(2):307–316.
17. Kent DM, Hayward RA. Limitations of applying summary results of 38. Ryan G, Pandit A, Apatsidis DP. Fabrication methods of porous metals
clinical trials to individual patients: the need for risk stratification. for use in orthopaedic applications. Biomaterials. 2006;27:2651–2670.
JAMA. 2007;298:1209–1212. 39. Lopez-Heredia MA, Goyenvalle E, Aguado E, et al. Bone growth in
18. Neal ML, Kerckhoffs R. Current progress in patient-specific modeling. rapid prototyped porous titanium implants. J Biomed Mater Res A.
Brief Bioinform. 2010; 11(1):111–126. 2008;85(3):664–673.
Orthopedic Research and Reviews 2016:8 submit your manuscript | www.dovepress.com
65
Dovepress
Powered by TCPDF (www.tcpdf.org)
Wong Dovepress
40. Harrysson OLA, Cansizoglu O, Marcellin-Little DJ, Cormier DR, West 44. Kostecki K. PEEK usage climbs for devices. Med Des. 2011. Available
HA II. Direct metal fabrication of titanium implants with tailored materi- from: http://medicaldesign.com/materials/peek-usage-climbs-devices.
als and mechanical properties using electron beam melting technology. Accessed on September 4, 2016.
Mater Sci Eng C. 2008;28:366–373. 45. Li CS, Vannabouathong C, Sprague S, Bhandari M. The use of carbon-
41. Hein P, Müller L, Körner C, Singer RF, Müller FA. Cellular Ti–6Al– fiber-reinforced (CFR) PEEK material in orthopedic implants: a
4V structures with interconnected macro porosity for bone implants systematic review. Clin Med Insights Arthritis Musculoskelet Disord.
fabricated by selective electron beam melting, Acta Biomater. 2015;8:33–45.
2008;4:1536–1544. 46. Kersten RF, van Gaalen SM, de Gast A, Öner FC. Polyetheretherketone
42. Harrysson O, Hosni Y, Nayfeh J. Custom-designed orthopedic implants (PEEK) cages in cervical applications: a systematic review. Spine J.
evaluated using finite element analysis of patient-specific computed 2015;15(6):1446–1460.
Orthopedic Research and Reviews downloaded from https://www.dovepress.com/ by 5.188.217.61 on 29-Jul-2018
tomography data: femoral component case study. BMC Musculoskelet 47. Lee JW, Cho DW. 3D Printing technology over a drug delivery for tissue
Disord. 2007;8:91. engineering. Curr Pharm Des. 2015;21(12):1606–1617.
43. Wong KC, Kumta SM, Chiu KH, et al. Computer assisted pelvic 48. Dong J, Zhang S, Liu H, Li X, Liu Y, Du Y. Novel alternative therapy
tumor resection and reconstruction with a custom-made prosthesis for spinal tuberculosis during surgery: reconstructing with anti-
using an innovative adaptation and its validation. Comput Aided Surg. tuberculosis bioactivity implants. Expert Opin Drug Deliv. 2014;
2007;12(4):225–232. 11:299.
For personal use only.
Orthopedic Research and Reviews Dovepress
Publish your work in this journal
Orthopedic Research and Reviews is an international, peer-reviewed, welcome. The manuscript management system is completely online
open access journal that focusing on the patho-physiology of the and includes a very quick and fair peer-review system, which is all
musculoskeletal system, trauma, surgery and other corrective interven- easy to use. Visit http://www.dovepress.com/testimonials.php to read
tions to restore mobility and function. Advances in new technologies, real quotes from published authors.
materials, techniques and pharmacological agents are particularly
Submit your manuscript here: https://www.dovepress.com/orthopedic-research-and-reviews-journal
66 submit your manuscript | www.dovepress.com Orthopedic Research and Reviews 2016:8
Dovepress
Powered by TCPDF (www.tcpdf.org)
You might also like
- The History of Urban PlanningDocument2 pagesThe History of Urban PlanningJay Mark Balbosa75% (4)
- Seismic Earth Pressures On Cantilever Retaining Structures 2010Document10 pagesSeismic Earth Pressures On Cantilever Retaining Structures 2010myplaxisNo ratings yet
- Worldwide Engineering Standards: Neutral Salt Spray (NSS) TestDocument4 pagesWorldwide Engineering Standards: Neutral Salt Spray (NSS) Testjorgesalg100% (2)
- 3d-Printed Patient-Specific Applications in Orthopedics: Orthopedic Research and Reviews DoveDocument10 pages3d-Printed Patient-Specific Applications in Orthopedics: Orthopedic Research and Reviews DoveOstazNo ratings yet
- MainDocument8 pagesMainOstazNo ratings yet
- From The Printer: Potential of Three-Dimensional Printing For Orthopaedic ApplicationsDocument8 pagesFrom The Printer: Potential of Three-Dimensional Printing For Orthopaedic Applicationssleiter boikaNo ratings yet
- 3D Printing Advancements in Medical Sciences: Department of Mechanical Engineering Wright State UniversityDocument12 pages3D Printing Advancements in Medical Sciences: Department of Mechanical Engineering Wright State UniversityAbhishek UdataneniNo ratings yet
- Applications of 3D Imaging in Orthodontics: Part 1Document10 pagesApplications of 3D Imaging in Orthodontics: Part 1Yassin SalahNo ratings yet
- PIIS2405844023049265Document27 pagesPIIS2405844023049265Arpita rathoreNo ratings yet
- 3D Printing Techniques in A Medical Setting: A Systematic Literature ReviewDocument21 pages3D Printing Techniques in A Medical Setting: A Systematic Literature ReviewIsabella GallardoNo ratings yet
- Applications of 3D Imaging in Orthodontics: Part 1Document10 pagesApplications of 3D Imaging in Orthodontics: Part 1Aly OsmanNo ratings yet
- 3D Printed Materials DentistryDocument150 pages3D Printed Materials DentistrySaimul HossainNo ratings yet
- Bioimpresssao, 2016Document8 pagesBioimpresssao, 2016KarolineNo ratings yet
- Title: Three-Dimensional Printing in HealthcareDocument2 pagesTitle: Three-Dimensional Printing in HealthcareUlloaNo ratings yet
- Advanced Science - 2021 - Jin - 3D Printing of Physical Organ Models Recent Developments and ChallengesDocument27 pagesAdvanced Science - 2021 - Jin - 3D Printing of Physical Organ Models Recent Developments and ChallengesAndres Ricardo Mejia SarmientoNo ratings yet
- 1 s2.0 S2666964122000376 MainDocument5 pages1 s2.0 S2666964122000376 MainMady Deka ApriliyaNo ratings yet
- 1 s2.0 S2214031X22000213 MainDocument20 pages1 s2.0 S2214031X22000213 MainThanh Tùng NguyễnNo ratings yet
- 3D Priting EyeDocument3 pages3D Priting EyeDaisy Arora KhuranaNo ratings yet
- 3d Printing Literature ReviewDocument5 pages3d Printing Literature Reviewea9k5d7j100% (1)
- Virtual Reality and Augmented Reality in Plastic SDocument10 pagesVirtual Reality and Augmented Reality in Plastic Spaseg78960No ratings yet
- The Low Cost Design and 3d Printing of Structural Knee Orthotics For Athletic Knee Injury PatientsDocument7 pagesThe Low Cost Design and 3d Printing of Structural Knee Orthotics For Athletic Knee Injury PatientsİTYNo ratings yet
- JCM 09 02238 v2Document21 pagesJCM 09 02238 v2andres castroNo ratings yet
- E016891 FullDocument11 pagesE016891 FullDr. Aysha SadafNo ratings yet
- 3D Scanning Applications in Medical Field: A Literature-Based ReviewDocument13 pages3D Scanning Applications in Medical Field: A Literature-Based ReviewPraveen VundrajavarapuNo ratings yet
- 3 D PrintingDocument17 pages3 D PrintingJyoti santosh HiremathNo ratings yet
- JBM A 36979Document13 pagesJBM A 36979AJ BoonNo ratings yet
- Three-Dimensional Imaging and Scanning - Current and Future Applications For PathologyDocument18 pagesThree-Dimensional Imaging and Scanning - Current and Future Applications For PathologyHilman HazmiNo ratings yet
- Ijms 23 01045Document27 pagesIjms 23 01045luis miguel ballesteros ospinaNo ratings yet
- 3D PrintingDocument7 pages3D PrintingPankaj VatsaNo ratings yet
- Cad & Cae in Bio-Medical Field: Nternational Ournal of Nnovative Esearch in Cience, Ngineering and EchnologyDocument6 pagesCad & Cae in Bio-Medical Field: Nternational Ournal of Nnovative Esearch in Cience, Ngineering and EchnologyManoj DhageNo ratings yet
- Sensors 24 01373 v2Document19 pagesSensors 24 01373 v2WAHYU DWI LESTARINo ratings yet
- 3D Printing Metal Implants in Orthopedic Surgery Methods, ApplicationsDocument19 pages3D Printing Metal Implants in Orthopedic Surgery Methods, Applicationsnur aisyahNo ratings yet
- 1 s2.0 S0378517322006482 MainDocument8 pages1 s2.0 S0378517322006482 MainMady Deka ApriliyaNo ratings yet
- Manual and Digital Orthodontic Model Analysisintra-Observer Reliability and Agreement ofDocument6 pagesManual and Digital Orthodontic Model Analysisintra-Observer Reliability and Agreement ofLindeny MartinezNo ratings yet
- Introducing The Journal of 3D Printing In: MedicineDocument2 pagesIntroducing The Journal of 3D Printing In: MedicineCanggih WahyunantaNo ratings yet
- Materials 16 06132 v2Document20 pagesMaterials 16 06132 v2vNo ratings yet
- Three Dimensional Printing Basic PrinciplesDocument16 pagesThree Dimensional Printing Basic PrinciplesAndre Antonio Tamayo FernandeNo ratings yet
- 3 - 3d-Printed Upper Limb Prostheses A Review - 2017Document16 pages3 - 3d-Printed Upper Limb Prostheses A Review - 2017Fernando PessoaNo ratings yet
- Anatomical-Models ENDocument14 pagesAnatomical-Models ENfabian hernandez medinaNo ratings yet
- 3D Printing in MedicalDocument4 pages3D Printing in MedicalAadil KakarNo ratings yet
- Graham 3 DPrinting TechnologyDocument12 pagesGraham 3 DPrinting TechnologyBattle SagaNo ratings yet
- Heart Disease Prediction Based On Machine Learning and Web DevelopmentDocument11 pagesHeart Disease Prediction Based On Machine Learning and Web DevelopmentSamar FathimaNo ratings yet
- 2017 A Nwe Data Structure and Workfolw For Using 3d Anthropometry in The Design of Wearable ProductDocument10 pages2017 A Nwe Data Structure and Workfolw For Using 3d Anthropometry in The Design of Wearable ProductVivian LiNo ratings yet
- The Future of Biomedical 3D PrintingDocument10 pagesThe Future of Biomedical 3D PrintingAyush GoplaniNo ratings yet
- 5182-Article Text-34951-2-10-20220126Document6 pages5182-Article Text-34951-2-10-20220126hishamkhan002No ratings yet
- Hospital Future Augmented - Reality - in - SurgeryDocument10 pagesHospital Future Augmented - Reality - in - Surgeryroupen sulahianNo ratings yet
- Implications of 3-Dimensional Printed Spinal Implants On The Outcomes in Spine SurgeryDocument10 pagesImplications of 3-Dimensional Printed Spinal Implants On The Outcomes in Spine SurgeryOstazNo ratings yet
- DR - Ram Kumar Reddy (Prof. & Unit Chief) DR - Prasad Reddy (Assistant Prof.) DR - Prakash (Assistant Prof.)Document42 pagesDR - Ram Kumar Reddy (Prof. & Unit Chief) DR - Prasad Reddy (Assistant Prof.) DR - Prakash (Assistant Prof.)Vignesh WaranNo ratings yet
- Contribution of 3D Printing For The Surgical Management of Jaws Cysts and Benign Tumors: A Systematic Review of The LiteratureDocument9 pagesContribution of 3D Printing For The Surgical Management of Jaws Cysts and Benign Tumors: A Systematic Review of The LiteratureEsteban FernandezNo ratings yet
- JETIRDQ06048Document5 pagesJETIRDQ06048Vikram SwainNo ratings yet
- Andy Christensen, Maintaing Safety and Efficacy For 3D Printign in MedicineDocument10 pagesAndy Christensen, Maintaing Safety and Efficacy For 3D Printign in Medicineyuvanshi jainNo ratings yet
- Semi-Automated Fabrication of Customized Ocular PRDocument9 pagesSemi-Automated Fabrication of Customized Ocular PRnurqumirfanNo ratings yet
- 3D PrintingDocument7 pages3D PrintingMiru BorcanNo ratings yet
- 3d News ReportDocument2 pages3d News Reportstream accountNo ratings yet
- Sicotj 3 16Document10 pagesSicotj 3 16OstazNo ratings yet
- Review Medical ApplicationsDocument12 pagesReview Medical Applicationscain.s.timeNo ratings yet
- 1 s2.0 S2666964121000011 MainDocument7 pages1 s2.0 S2666964121000011 Mainfadia nauraNo ratings yet
- 3D Printing and Amputation: A Scoping Review: Disability and Rehabilitation: Assistive TechnologyDocument21 pages3D Printing and Amputation: A Scoping Review: Disability and Rehabilitation: Assistive TechnologyUI KipediaNo ratings yet
- 2D and 3D Anatomical Analyses of Hand Dimensions For Custom-Made GlovesDocument13 pages2D and 3D Anatomical Analyses of Hand Dimensions For Custom-Made GlovesZiyaNo ratings yet
- 3D Printing ScriptDocument2 pages3D Printing Scriptahmet çelikNo ratings yet
- Jud2020 Article ApplicabilityOfAugmentedRealitDocument13 pagesJud2020 Article ApplicabilityOfAugmentedRealitmohadeseNo ratings yet
- Meo 20 29847Document3 pagesMeo 20 29847AJ BoonNo ratings yet
- Stereopsis and HygieneFrom EverandStereopsis and HygieneHiroki TakadaNo ratings yet
- Szymczyk 2020Document15 pagesSzymczyk 2020Agnieszka SmagaNo ratings yet
- Patel 2018Document5 pagesPatel 2018Agnieszka SmagaNo ratings yet
- CR Onskar 2013Document9 pagesCR Onskar 2013Agnieszka SmagaNo ratings yet
- Castel An 2014Document10 pagesCastel An 2014Agnieszka SmagaNo ratings yet
- Experiment: WE - 1 Title: Infiltration Rate and Double-Ring Infiltrometer Test Duration: 2 Hours: 1 0F 7Document6 pagesExperiment: WE - 1 Title: Infiltration Rate and Double-Ring Infiltrometer Test Duration: 2 Hours: 1 0F 7asadNo ratings yet
- TP - PPST 2023Document4 pagesTP - PPST 2023NI KoLsNo ratings yet
- Chapter 10 - Limits and ContinuityDocument20 pagesChapter 10 - Limits and ContinuityAnkit PokhrelNo ratings yet
- A Review of Mixed Methods, Pragmatism and Abduction TechniquesDocument14 pagesA Review of Mixed Methods, Pragmatism and Abduction TechniquesDeep ShiNo ratings yet
- Diversity in The Plant KingdomDocument14 pagesDiversity in The Plant KingdomJimmy Serendip100% (1)
- Castillo2020 Bayesian Predictive Optimization of Multiple and Profile Responses Systems in IndustryDocument18 pagesCastillo2020 Bayesian Predictive Optimization of Multiple and Profile Responses Systems in IndustryAngel GarciaNo ratings yet
- Dlfiles401109814401att 1134439v1reyrolle 7PG15 Catalog Edition 3.pdfdownload TrueDocument30 pagesDlfiles401109814401att 1134439v1reyrolle 7PG15 Catalog Edition 3.pdfdownload TrueredaNo ratings yet
- Fermentation: Bio Lab ManualDocument11 pagesFermentation: Bio Lab Manualthegp12No ratings yet
- Stellar EvolutionDocument5 pagesStellar EvolutionMayar AzzamNo ratings yet
- Algorithms For Diophantine Equations - B.M.M. de WegerDocument220 pagesAlgorithms For Diophantine Equations - B.M.M. de Wegermontesdoc.trabajo Mont&DocNo ratings yet
- MTH302 Probability and StatisticsDocument7 pagesMTH302 Probability and StatisticsLakhanKadamNo ratings yet
- Manual PDFDocument149 pagesManual PDFCoria AndresNo ratings yet
- TECHNICAL CATALOGUE - VSF - IEC - ATEX - EN - Rev1 - 2017 PDFDocument172 pagesTECHNICAL CATALOGUE - VSF - IEC - ATEX - EN - Rev1 - 2017 PDFLASCARZAMFIRESCUNo ratings yet
- Product Data Guide MalarkeyDocument18 pagesProduct Data Guide MalarkeyHoeNo ratings yet
- Scientists Show That Water Has MemoryDocument2 pagesScientists Show That Water Has MemoryFatiyaNo ratings yet
- Discourses of Psychological Trauma Nikki Kiyimba Full ChapterDocument67 pagesDiscourses of Psychological Trauma Nikki Kiyimba Full Chapterronald.allison470100% (18)
- Admmodule s11 12ps Iiib 12Document11 pagesAdmmodule s11 12ps Iiib 12Lebz RicaramNo ratings yet
- Seal of Good Local GovernanceDocument46 pagesSeal of Good Local GovernanceKyza Mae AlcontinNo ratings yet
- Scour Calculation - Hydropower PDFDocument44 pagesScour Calculation - Hydropower PDFathot789No ratings yet
- Jan-March Exam Time TableDocument12 pagesJan-March Exam Time TableIita FestusNo ratings yet
- Math7 Q2W2Document6 pagesMath7 Q2W2Meryl Fe P. GumeraNo ratings yet
- EVS AssignmentDocument2 pagesEVS AssignmentCharu GautamNo ratings yet
- Unit 10 - JobsDocument5 pagesUnit 10 - JobsFabiola MamaniNo ratings yet
- Cultural Anthropology 16th Edition Conrad Test BankDocument20 pagesCultural Anthropology 16th Edition Conrad Test Bankjonathanwelchjrcizmsdty100% (29)
- Cement Rotary Kiln Questions & AnswersDocument37 pagesCement Rotary Kiln Questions & AnswersNael95% (19)
- Cementing Design - FinalDocument27 pagesCementing Design - FinalBIGBOAZ XX100% (1)
- I'm Learning About Numbers WorksheetsDocument22 pagesI'm Learning About Numbers WorksheetsJozel M. ManuelNo ratings yet