Professional Documents
Culture Documents
Joung2007-BM Mononuclear Cells - MI
Joung2007-BM Mononuclear Cells - MI
Uploaded by
iulia andreeaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Joung2007-BM Mononuclear Cells - MI
Joung2007-BM Mononuclear Cells - MI
Uploaded by
iulia andreeaCopyright:
Available Formats
Yonsei Med J 48(5):754 - 764, 2007
DOI 10.3349/ymj.2007.48.5.754
Bone Marrow Mononuclear Stem Cells Transplanted in Rat
Infarct Myocardium Improved the Electrical Conduction
without Evidence of Proarrhythmic Effects
1 1 1 2 1
Boyoung Joung, * Il-kwon Kim, * Moon-Hyoung Lee, Kyung-Jong Yoo, and Sung-Soon Kim
1
Division of Cardiology and 2Department of Cardiovascular Surgery, Yonsei Cardiovascular Center and Research Institute,
Yonsei University College of Medicine, Seoul, Korea.
Purpose: The arrhythmogenic effect of stem cells trans- an increasing proportion of patients with acute
plantation (SCT) in an infarct myocardium is still unknown. myocardial infarctions (AMIs) surviving with
We investigated arrhythmogenicity of SCT in rat cryo-infarct
significant impairment of the systolic function of
model. Materials and Methods: In rat cryo-infarct model,
bone marrow mononuclear stem cells (MNSC, 1 × 107 cells) their left ventricles (LVs). On the basis of experi-
were transplanted into the infarct border zone (BZ) of the LV mental studies that have suggested that the
epicardium. We compared the optical mapping and induci- cardiac transfer of unfractionated bone marrow
bility of ventricular tachycardia/fibrillation (VT/VF) among cells (BMCs) or bone marrow-derived stem and
normal (n = 5), cryo-infarct (n = 6), and SCT rats (n = 6). progenitor cells can promote functional improve-
Results: The VT/VF inducibility was higher in the cryo-
infarct (47.2%, p = 0.001) and SCT groups (34.6%, p = 0.01)
ments after an AMI,1-4 several clinical trials have
than in the normal group (12.8%). The induced VT/VF explored the hypothesis that intracoronary
episodes persisted for more than 2 minutes in 4.3%, 26.4% infusion of autologous BMCs may enhance the
and 17.3% in the normal, cryo-infarct and SCT group, recovery of the LV systolic function after an
respectively. In the SCT group, the action potential duration AMI.5-8 However, the arrhythmogenicity of stem
at 70% was shorter at the SCT site than the BZ during SR
cell transplantations (SCTs) still is unknown. Early
(75.2 ± 8.1 vs. 145.6 ± 4.4 ms, p = 0.001) and VT (78.2 ±
13.0 vs. 125.7 ± 21.0 ms, p = 0.001). Conduction block was studies by Smits et al.9 and Menasche et al.10,11
observed at the SCT site and BZ during VT. However, no suggested there were proarrhythmic effects after
reentry or ectopic foci were observed around the SCT sites. stem cell therapy. In order for cell therapy to
Conclusion: The electrical conduction was improved by SCT become widely applicable clinically, it has to be
without evidence of augmentation of arrhythmia in the rat compatible both mechanically and electrically
cryo-infarct model.
with the host myocardium. Although, it remains
Key Words: Arrhythmogenicity, stem cell, optical mapping possible that these arrhythmias reflect the natural
history of a myocardial infarction rather than the
introduction of the new cells, it seems clear that
Modern reperfusion strategies and advances in we must consider the potential mechanisms of the
the pharmacological management have resulted in arrhythmias and strategies to control or eliminate
them.
Received November 6, 2006
In the present study, we investigated the electrical
Accepted March 12, 2007 conduction of bone marrow mononuclear stem
This work was supported in part by MIC IITA through IT cells (MNSC) transplanted into the infarct border
Leading R D Support Project. zone of rat LVs. We also evaluated the effect of
*These two authors contributed equally to this article. transplanted MNSC on the inducibility of
Reprint address: requests to Dr. Moon-Hyoung Lee, Division of ventricular arrhythmias and whether or not they
Cardiology, Yonsei University College of Medicine, 250 Seongsanno,
can be used as part of the reentry circuit or
Seodaemun-gu, Seoul 120-752, Korea. Tel: 82-2-2228-8460~1, Fax:
82-2-393-2041, E-mail: mhlee@yuhs.ac ectopic focus for arrhythmias.
Yonsei Med J Vol. 48, No. 5, 2007
Arrhythmogenicity of Stem Cells
MATERIALS AND METHODS were labeled with a fluorescent cell tracker [5-(and
6)-carboxyfluoresceindiacetate-succinimidyl-ester,
All procedures were approved by the Institu- CFDA, Molecular Probes, Eugene, OR] for Tro-
tional Animal Care and Use Committee and ponin I staining. Twenty mL of Saline (cryo-
performed in accordance with the "Guidance for infarction group, n = 6) or the MNSCs with 20 mL
the Care and Use of Laboratory Animals" of of saline {stem cell transplantation (SCT) group,
Yonsei University College of Medicine. n = 6}, which contained about 1 × 107 cells, were
injected directly into the border zone of the infarc-
Bone marrow mononuclear stem cell harvesting tion with a 28-gauge needle attached to a 1 mL
tuberculin syringe. Only one injection was per-
Thirty adult Sprague-Dawley rats (weight 250 formed at the left edge of cryo-infarcted area.
to 300 g) were used in this study as stem cell When we exposed heart for MNSCs injection, we
donors. The MNSCs were isolated from the could clearly see the infarcted zone and easily
femoral and tibial bones of donor rats. Extracted identify the border zone. We counted bone
MNSCs from the donor rats were mixed with PBS marrow MNSCs for the each injection. A succes-
(Dulbecco's Phosphate Buffered Saline, Gibco). sful injection was typified by the formation of a
The mixed solutions were centrifuged at 2000 rpm bleb covering the infarct zone. Several rats without
for 20 minutes and the buffy coat layer was a cyo-infarct were used as a normal group (n = 5)
extracted. This buffy coat was diluted with PBS to evaluate the normal electrical conduction and
and centrifuged at 1500 rpm for 5 minutes. After inducibility of ventricular tachycardia (VT) or
two centrifugations, the bone marrow MNSCs fibrillation (VF).
were extracted.
Langendorff preparation
Model of the cryo-infarction and injection of the
MNSCs Adult rat hearts (weight 250 to 300 g) were
excised under general anesthesia at 4 weeks after
The rats were anesthetized with ketamine (75 the saline or stem cell injection. The ascending
mg/kg IP) and xylazine (5 mg/kg IP). After endo- aorta was immediately cannulated and perfused
tracheal intubation and mechanical ventilation at 15 to 20 mL/min with oxygenated Tyrode's
(room air, rate 60 cycles/min, tidal volume 1 mL solution (NaCl, 125.0; KCl, 4.5; MgCl2, 0.5; CaCl2
per 100 g of body weight, Harvard Apparatus 0.54; NaH2PO4, 1.2; NaHCO3 24.0; glucose, 5.5;
Rodent Ventilator, model 683), the heart was ex- albumin 50 mg/L, pH 7.4, 36.5 ). The heart was
posed through a mid thoracotomy. The cryo-in- both perfused and superfused in a tissue bath
jury was created on the epicardial side of the LV made with transparent glass.
of the rats. The first cryo-injury was made with
a 1 cm cryo-injury rode (homemade) for 20 Study of the inducibility of ventricular arrhy-
seconds and 4 additional cryo-injuries were then thmias
made for 60 seconds. The rats were allowed to
12
recover under care. We paced the right ventricular epicardium of
We started this study with 20 rats. Two rats the Langendorff perfused hearts with a stimulus
died right after applying cryo-injury. And one rat using a 2-ms pulse width and at twice the
died under normal raising facility 10 days after diastolic threshold current, using a programmed
cryo-injury. So survival ratio was 85% for making stimulator (Intermedics, Austin, TX, USA). VF was
this infarction model. Four weeks after the cryo- induced by burst pacing (PCL 75 ms, 5-ms pulse
injury, the rats were reanesthetized and the chest duration and 5-mA current for 5 seconds). The
was reopened for the injection of the MNSCs or inducibility of the VT/VF was determined by the
saline and the infarcted region was visually ratio of the successful VT/VF inductions to the
identified by a mottled and pale appearance. Prior number of burst pacing attempts (maximum 10).
to cell transplantation, the bone marrow MNSCs Once induced, VF was continuously monitored by
Yonsei Med J Vol. 48, No. 5, 2007
Boyoung Joung, et al.
a bipolar recording. Optical recordings were secondary antibodies (Jackson ImmunoResearch
recorded immediately and every 2 minutes there- Laboratories, West Grove, PA, USA). The immu-
after. If VF persisted for more than 5 minutes, it nofluorescently stained sections were analyzed
was terminated by defibrillation using 1 to 2 using a confocal microscope (LSM510, Carl Zeiss,
Joules. We compared the inducibility of the Oberkochen, Germany).
VT/VF and optical mapping among the normal
(n = 5), cyo-infarction (n = 6), and SCT (n = 6) Data analysis
groups.
The inducibility of VT/VF after stimulation was
Optical mapping compared with a Chi-squire test between the three
groups. Optical mapping data were processed
13,14
The optical mapping system has been described through several image processing algorithms.
previously.13,14 The hearts were stained with di-4- After the data processing, pixels from the normal
ANEPPS (Molecular Probes, Inc,. Eugene, OR, myocardium, border zone, STC site, and infarct
USA). They were then excited with quasi-mono- site were chosen for optical signal analysis and
chromatic light (500 ± 30 nm) from two green LED APD determinations. The comparison of the APD
lamps (LL-50R30-G25, Optronix, Seoul, Korea). duration between sinus rhythm and VT was made
Fluorescent and scattered light was collected by using the unpaired Student t-test. Differences with
an image-intensified charge-coupled device camera a value of p < 0.05 were considered statistically
(CCD camera, Dalsa Inc., Waterloo, Canada). The significant.
data were gathered at 3.75-ms sampling intervals,
acquiring from 100 × 100 sites simultaneously over
a 35 × 35-mm2 area with a pixel size of 0.27 mm. RESULTS
The mapped area included parts of the right and
left ventricular free walls. For detailed mapping of We used 180 ± 10 mg rat initially. The body
the anterior wall of the LV including the SCT site, weight was 235 ± 30, 240 ± 35, 238 ± 40 mg in
we magnified the field to a 10 × 10-mm2 area. To normal, cryo-infarction, and SCT groups, respec-
decrease the motion related artifact, diacetyl tively. The experiments lasted an average of 95 ±
monoxime (DAM) was used with an infusion rate 25 minutes. After the excised hearts were perfused
of 8 mmol/l.13 with Tyrode's solution and di-4-ANEPPS, a
VT/VF induction study was performed 3 to 10
Assessment of the survival and differentiation of times in all hearts. Optical mapping was per-
the MNSCs in a myocardial infarction formed in all hearts after adequate staining with
di-4-ANEPPS.
The heart specimens were obtained from all
rats. The specimens were fixed in 10% (v/v) The results of optical the mapping
buffered formaldehyde, dehydrated with a graded
ethanol series, embedded in paraffin, and cut into In the normal group, the depolarization during
4-μm-thick sections. The distribution of the cells sinus rhythm was initiated from the mid-LV and
was evaluated with a Hematoxyline & Eosin stain. spread to the rest of the ventricle without any
The degree of fibrosis was evaluated with a conduction disturbances. The analysis of optical
Masson's trichrome stain. The slides were first signals also revealed that the initiation of the
examined at a 100 × magnification to identify the depolarization was from the mid-LV (site 2) and
infarcted area, and then evaluated at a 400 × then propagated in both directions (sites 1 and 2)
magnification. (Figs. 2A, B and D). Multiple wavefronts meandered
For the detection of the CFDA-labeled cells and over the entire during VF with amorphorous
cardiac troponin I-positive cells, the tissue sections optical signals (Figs. 2C and E).
were stained immunofluorescently for cardiac In the cryo-infarction group, the depolarization
troponin I using cyanine-conjugated anti-goat IgG during sinus rhythm was initiated from the mid-
Yonsei Med J Vol. 48, No. 5, 2007
Arrhythmogenicity of Stem Cells
LV. However, the depolarization became delayed or VF, conduction block was observed at the
at the border zone, and almost disappeared at the border zone and infarct zone. Reentry around the
cryo-infraction zone (Figs. 3A, B and D). During entire infarction site was observed (Figs. 4C and
VF, multiple wavefronts appeared throughout the E). However, no reentry or ectopic beats around
heart except for at the cryo-infarction zone (Figs. the SCT site were observed. Conduction block was
3C and E). Conduction block was observed at the observed at the border and infarct zone.
border zone and cryo-infarction zone (Fig. 3E).
In the SCT group, the depolarization also in- The influence of stem cell transplantation on
itiated from the mid-LV during sinus rhythm. The inducibility of VT or VF
depolarization was delayed at the border zone,
and almost disappeared at the cryo-infraction In the normal group, VT or VF was induced in
zone. However, the depolarization improved at 6 of 47 burst pacing applications (12.8%) as
the SCT sites (Figs. 4A, B and D). During the VT compared with 25 of 53 in the cryo-infarction
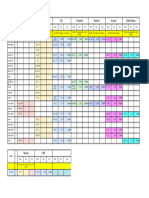
Table 1. Comparison of the Ventricular Tachycardia or Fibrillation (VT/VF) Inducibility between the Control,
Cryo-Injury, and SCT Groups
n (%)
Rat
Stimulation Induced VT/VF Induced VT/VF > 2 min
Control 47 6 (13) 2 (4)
1 10 1 (10) 0
2 10 0 0
3 10 1 (10) 0
4 7 3 (43) 1 (14)
5 10 1 (10) 1 (10)
Cryo-injury group* 53 25 (47) 14 (26)
1 3 1 (33) 1 (33)
2 10 5 (50) 3 (30)
3 10 8 (80) 4 (40)
4 10 1 (10) 0
5 10 4 (40) 2 (20)
6 10 6 (6) 4 (40)
SCT group 52 18 (35) 9 (17)
1 8 3 (36) 2 (25)
2 4 2 (50) 1 (25)
3 10 4 (40) 2 (20)
4 10 1 (10) 1 (10)
5 10 5 (50) 3 (30)
6 10 3 (30) 0
SCT, Stem cell transplantation.
*p = 0.001, Chi-squire test between the control and cryo-injury groups.
p = 0.01, Chi-squire test between the control and SCT groups.
Yonsei Med J Vol. 48, No. 5, 2007
Boyoung Joung, et al.
group (47.2%) and 18 of 52 in the SCT group cryo-infarction and SCT groups, respectively.
(34.6%). Compared with the normal group, the
VT/VF inducibility was higher in the cryo-infarc- The influence of the stem cell transplantation on
tion (p = 0.001) and SCT groups (Table 1, Fig. 1, the action potential duration
p = 0.01). The VT/VF induced persisted for more
than 2 minutes in 2 of 47 (4.3%), 14 of 53 (26.4%) The APD at 70% (ADP70) was analyzed during
and 9 of 52 stimulations (17.3%) in the normal, sinus rhythm and VT in the SCT group. The
APD70 during sinus rhythm was 49.6 ± 2.0 ms,
75.2 ± 8.1 ms, and 145.6 ± 4.4 ms at the normal,
stem cell transplant sites, and border zones,
respectively. The APD70 in the SCT sites was
shorter than that for the border zones (p = 0.001).
The APD70 during VT was 72.7 ± 3.3 ms, 78.2
±13.0 ms, and 125.7 ± 21.0 ms at the normal, stem
cell transplant sites, and border zones, respec-
tively. The APD70 of the SCT sites was also
shorter than that of the border zone (Table 2, p =
0.001).
Histology of rat hearts with stem cell transplants
Fig. 1. Comparison of the ventricular tachycardia or
and a cryo-infarct
fibrillation (VT/VF) inducibility between the control,
cryo-injury, and stem cell transplantation (SCT) groups. The microscopic appearance of a stem cell
SCT indicates stem cell transplantation group. The transplanted rat heart with a cryo-infarct is shown
inducibility of VT/VF was 12.8%, 34.6%, and 47.2% in
control, cryoinjury, and stem cell transplantation group, in Fig. 5. According to H & E staining (Figs. 5A
respectively. Cryoinjury and STC group had higher and B) and Masson Trichrome staining (Figs. 5C
VT/VF inducibility than control (p = 0.01). and D), huge fibrosis was observed in the
A B
Fig. 2. Optical mapping of the control rat
hearts during normal sinus rhythm (B
C and D) and ventricular fibrillation (C and
E). (A) Optical mapping was recorded
from the epicardium of the left ventricle
(box). The numbers 1 to 3 represent the
sites where the optical signals were taken.
(B and C) Pseudo color membrane voltage
maps at certain times are presented. (D
D and E) Optical signals were recorded
from sites 1 to 3. During sinus rhythm,
the depolarization was initiated from the
mid-LV (site 2) and spread to the rest of
the heart (sites 1 and 3). During VF,
multiple wavefronts meandered over the
entire heart during VF with amorphorous
E optical signals recorded from sites 1 to 3.
Yonsei Med J Vol. 48, No. 5, 2007
Arrhythmogenicity of Stem Cells
Fig. 3. Optical mapping of cryo-infarct rat
A B hearts during normal sinus rhythm (B
and D) and ventricular fibrillation (C and
E). (A) Optical mapping was recorded
from the epicardium of the LV (box). The
numbers 1 to 4 represent the sites where
optical signals were taken. Sites 1 and 2
C are normal myocardium, 3 a border zone,
and 4 a cryo-infarct. (B and C) Pseudo
color membrane voltage maps at certain
times are presented. Depolarization was
initiated from the mid-LV (site 2), and
spread to the normal myocardium (site 1,
544 ms) and then to the border zone (site
3,564 ms). (D and E) Optical signals re-
D corded from sites 1 to 4. During sinus
rhythm, depolarization was initiated
from the mid-LV (site 2) and spread to
the rest of the heart (sites 1 and 3). How-
ever, no depolarization was observed in
the cryo-infarct (site 4). During VF, am-
orphorous waves are observed in the
normal myocardium and border zone
(sites 1 to 3) but not in the cryo-infarct
E (site 4).
A B
C
Fig. 4. Optical mapping of a cryo-infarct
in stem cell transplanted rat hearts
during normal sinus rhythm (B and D)
and ventricular fibrillation (C and E). (A)
Optical mapping was recorded on the
anterior LV including the SCT site (Box).
The numbers 1 to 3 represent the sites
D where optical signals were recorded. (B
and C) Pseudo color membrane voltage
maps at certain times are presented. (D
and E) Optical signals were recorded
from sites 1 (normal zone), 2 (stem cell
transplanted site), and 3 (border zone) as
marked in the first sub-panel of panels B
and C (asterisk). The ventricular tachy-
E cardia terminated spontaneously.
Yonsei Med J Vol. 48, No. 5, 2007
Boyoung Joung, et al.
Table 2. Comparison of the APD at 70% During Sinus Rhythm and Ventricular Tachycardia which was
Presented in Figs. 4B and D, Respectively
APD70 Normal Stem cell site Border zone p value (between SCTZ and BZ)
During SR (ms) 49.6 ± 2.0 75.2 ± 8.1 145.6 ± 4.4 0.001
During VT (ms) 72.7 ± 3.3 78.2 ± 13.0 125.7 ± 21.0 0.001
A B
C D
Fig. 5. Microscopic appearance of a cryo-infarct in a stem cell transplanted rat heart (Fig. 4). (A) H & E staining revealed
cells in the mononuclear stem cell implant site. (B) Magnified view of the box in A. The stem cell transplant site had
a higher density of cells (arrow). (C) With Masson Trichrome staining, a huge amount of fibrosis was observed from 1
to 6 o'clock along the left ventricle after the cryo-infarction (blue color). The stem cell transplant site had a brown color
(box). (D) Magnified view of the box in C. The stem cell transplant site had less fibrosis (brown color, arrow).
cryo-infarct sites from 1 to 6 o'clock in the LV, and people in the United States, with 550,000 new
15
the SCT sites exhibited less fibrosis with some cases reported annually. Despite major improve-
cells (Figs. 5C and D). MNSCs transplanted in ments in medical therapy, a significant proportion
infarct border zone showed positive with troponin of patients remain symptomatic. The disease pro-
I staining (Fig. 6). cesses leading to myocardial contractile dysfunc-
tion all, to a greater or lesser extent, occur in a
patchy or regional pattern and, along with cor-
DISCUSSION respondingly heterogeneous electrical remodeling,
create this nonuniformity associated with arrhy-
Heart failure affects an estimated 4.9 million thmogenesis. Emerging strategies of cell trans-
Yonsei Med J Vol. 48, No. 5, 2007
Arrhythmogenicity of Stem Cells
A B
C D
Fig. 6. Differentiation of transplanted MNSCs into cardiomyocytes. MNSCs transplanted in infarct border zone showed
rich viable cells (blue color in A). Transplanted MNSCs were engrafted in the myocardium and stained for cardiac troponin
I. Troponin I positive cells are presented with red color in B, green color in C, and yellow color in D.
plantation to restore myocardial function in the mias after open chest autologous skeletal myoblast
failing heart are focusing largely on the com- transplantation. Proarrhythmia after stem cell
pelling goal of improving contractile function or therapy might be attributed to one or more of the
promoting angiogenesis, with little attention given following reasons: 1) Heterogeneity of action
initially to how arrhythmic risk may be modified. potentials between the native and the transplanted
One important question that this raises is whether stem cells; 2) intrinsic arrhythmic potential of
this approach will suppress an arrhythmic ten- injected cells; 3) increased nerve sprouting
dency, by restoring greater uniformity of healthy induced by stem cell injection; and 4) local injury
tissue architecture and function, or whether it will or edema induced by intramyocardial injection.17
further add to the heterogeneity, thereby en-
hancing any arrhythmic tendency.16,17 Model of the cryo-infarction and injection of the
In the study by Smits et al.1 one of the five MNSCs
patients had sustained episodes of ventricular
tachycardia and required implantable cardioverter- Four weeks after cryo-injury, infarction sites
defibrillator (ICD) placement. The investigators were easily identified because it showed white
also describe a subsequent unpublished experience color compared normal tissue. For appropriate
of two sudden deaths and three serious ven- tracking of MNSCs injection site, only one
tricular arrhythmias in eight additional patients. injection was performed at the left edge of cryo-
These data seem to correspond to the Menasche infarcted area. In our experience, MNSC injection
et al.2,3 experience in which 4 of 10 patients site showed revascularization with reddish color
rezuired ICD implantation for ventricular arrhyth- after 4 weeks. Electrical conduction between cells
Yonsei Med J Vol. 48, No. 5, 2007
Boyoung Joung, et al.
was not evaluated in this study. This study According to Zhang, et al.24 stem cells showed
evaluated so called electrical conduction between conduction disturbances in vitro patch-clamp
tissues with high resolution optical mapping studies. However, the border zone already ex-
system. hibited a severe conduction disturbance and the
transplanted MNSCs showed differentiation to
The influence of MNSCs on electrical conduction troponin I positive cells and improved the elec-
trical conduction in this study. The repolarization
In the rat cryo-infarct model, the infarct lesion phase of the APD was significantly prolonged at
exhibited almost no electrical activity. The border the border zone. This prolonged APD may pro-
zone exhibited a delayed depolarization and mote arrhythmias. The transplanted MNSCs also
broad APD as compared to the normal myocar- shorten the APD at the border zone. However, the
dium. In this study, we could find that MNSCs limited method used in this study could not
transplanted at the border zone of a cryo-infarc- explain whether the improvement in the electrical
tion improved the electrical conduction. conduction was caused by the regeneration of the
The data about the influence of a cryo-infarct on myocardium or only by neovascularization.
the electrical conduction is limited in the rat
cryo-infarct model. However, data obtained from The influence of MNSCs on induciblity of
4- to 5-day-old canine infarcts showed that the ventricular arrhythmia and mechanism
healing infarct undergoes structural and func-
tional changes. The surviving epicardial cells The MNSCs transplantation did not effect the
overlying the infarct have abnormal action inducibility or duration of the VT/VF. The result
potentials with diminished upstrokes with the loss was in concordance with the improved electrical
of the plateau and a shorter action potential conduction, especially for the repolarization by
duration. The density and kinetics of a number of the MNSC transplantation. When we were con-
ion channel become altered, and the sodium ion sidering the proarrhythmic effects of the MNSCs
and calcium ion currents become reduced, as do transplantation, the mechanism was thought to be
the transient outward potassium ion currents and possibly due to reentry caused by an electrical
delayed and inward rectifying potassium ion heterogeneity, or ectopic focus with automaticity
currents.18 During this stage, reentrant VT in the or triggered activity. However, we could not find
so-called epicardial border zone (the layer of any evidence that the MNSC transplanted sites
surviving cells overlying the infarct) can easily be served as a part of a reentry circuit or ectopic
induced by premature stimuli. Both the cellular focus. The severe prolongation of the repolariza-
abnormalities, as well as a redistribution of the tion and heterogeneity which were observed at
intercellular gap junction, play a role in deter- the border zones, improved at the stem cell trans-
mining the reentry.19 These VTs may degenerate plantation sites. That improvement may have
into VF, especially in the presence of a high attenuated the arrhythmogeneity of this border
sympathetic tone,20 but this is uncommon. zone.
Over the next few weeks, transmembrane action In conclusion, the electrical conduction was
potentials of the surviving cells gradually return improved more by the MNSCs transplantation.
to normal, as most of the ion channels recover, The MNSCs transplantation in the rat cryo-in-
and by 2 months, the action potential configura- farction model did not increase the inducibility of
tion in both canine and human infarcts is the VT/VF. There was no evidence of augmenta-
completely normal.21,22 It is difficult to be certain tion of the arrhythmia from the MNSCs in the
when the healing phase of a myocardial infarction cryo-infarct rat model.
is over and when the fully healed phase begins.
It is likely that the electrophysiological substrate Study limitations
for VT gradually develops over several weeks and
remains stable from several months to 15 to 20 The type of infarct model used in this study
years.23 was a cryo-infarction model. Coronary artery
Yonsei Med J Vol. 48, No. 5, 2007
Arrhythmogenicity of Stem Cells
ligation model is more popular for the evaluation 9. Smits PC, van Geuns RJ, Poldermans D, Bountioukos
of infarct model. Actually we also studied with M, Onderwater EE, Lee CH, et al. Catheter-based
intramyocardial injection of autologous skeletal myo-
ligation model initially. Compared to ligation
blasts as a primary treatment of ischemic heart failure:
model, the cryo-infarction model is known to clinical experience with six-month follow-up. J Am Coll
have less arrhythmias and ventricular aneurysms. Cardiol 2003;42:2063-9.
However, the optical mapping in the LAD ligation 10. Menasché P, Hagège AA, Scorsin M, Pouzet B, Desnos
model was not appropriate because of an unclear M, Duboc D, et al. Myoblast transplantation for heart
failure. Lancet 2001;357:279-80.
infarct border. In this study, only MNSCs were
11. Menasché P, Hagège AA, Vilquin JT, Desnos M,
used for the stem cell transplantation. Therefore, Abergel E, Pouzet B, et al. Autologous skeletal myo-
further studies are needed to apply this result to blast transplantation for severe postinfarction left ven-
other cell types. If we could have monitored rats tricular dysfunction. J Am Coll Cardiol 2003;41:1078-
ambulatory ECG, it would have been better for 83.
evaluation of arrhythmia. 12. Ryu JH, Kim IK, Cho SW, Cho MC, Hwang KK, Piao
H, et al. Implantation of bone marrow mononuclear
cells using injectable fibrin matrix enhances neovascu-
larization in infarcted myocardium. Biomaterials 2005;
REFERENCES 26:319-26.
13. Lee MH, Lin SF, Ohara T, Omichi C, Okuyama Y,
1. Orlic D, Kajstura J, Chimenti S, Jakoniuk I, Anderson Chudin E, et al. Effects of diacetyl monoxime and
SM, Li B, et al. Bone marrow cells regenerate infarcted cytochalasin D on ventricular fibrillation in swine right
myocardium. Nature 2001;410:701-5. ventricles. Am J Physiol Heart Circ Physiol 2001;280:
2. Kamihata H, Matsubara H, Nishiue T, Fujiyama S, H2689-96.
Tsutsumi Y, Ozono R, et al. Implantation of bone 14. Garfinkel A, Kim YH, Voroshilovsky O, Qu Z, Kil JR,
marrow mononuclear cells into ischemic myocardium Lee MH, et al. Preventing ventricular fibrillation by
enhances collateral perfusion and regional function via flattening cardiac restitution. Proc Natl Acad Sci U S
side supply of angioblasts, angiogenic ligands, and A 2000;97:6061-6.
cytokines. Circulation 2001;104:1046-52. 15. Hunt SA, Baker DW, Chin MH, Cinquegrani MP,
3. Balsam LB, Wagers AJ, Christensen JL, Kofidis T, Feldman AM, Francis GS, et al. ACC/AHA guidelines
Weissman IL, Robbins RC, et al. Haematopoietic stem for the evaluation and management of chronic heart
cells adopt mature haematopoietic fates in ischaemic failure in the adult: executive summary: A Report of
myocardium. Nature 2004;428:668-73. the American College of Cardiology/American Heart
4. Yoon YS, Wecker A, Heyd L, Park JS, Tkebuchava T, Association Task Force on Practice Guidelines (Com-
Kusano K, et al. Clonally expanded novel multipotent mittee to Revise the 1995 Guidelines for the Evaluation
stem cells from human bone marrow regenerate and Management of Heart Failure): developed in col-
myocardium after myocardial infarction. J Clin Invest laboration with the International Society for Heart and
2005;115:326-38. Lung Transplantation; endorsed by the Heart Failure
5. Strauer BE, Brehm M, Zeus T, Köstering M, Hernandez Society of America. Circulation 2001;104:2996-3007.
A, Sorg RV, et al. Repair of infarcted myocardium by 16. Peters NS. Arrhythmias after cell transplantation for
autologous intracoronary mononuclear bone marrow myocardial regeneration: natural history or result of the
cell transplantation in humans. Circulation 2002;106: intervention? J Cardiovasc Electrophysiol 2005;16:1255-
1913-8. 7.
6. Assmus B, Schächinger V, Teupe C, Britten M, 17. Makkar RR, Lill M, Chen PS. Stem cell therapy for
Lehmann R, Döbert N, et al. Transplantation of Pro- myocardial repair: is it arrhythmogenic? J Am Coll
genitor Cells and Regeneration Enhancement in Acute Cardiol 2003:42:2070-2.
Myocardial Infarction (TOPCARE-AMI). Circulation 18. Pinto JM, Boyden PA. Electrical remodeling in ischemia
2002;106:3009-17. and infarction. Cardiovasc Res 1999;42:284-97.
7. Fernández-Avilés F, San Román JA, García-Frade J, 19. Peters NS, Coromilas J, Severs NJ, Wit AL. Disturbed
Fernández ME, Peñarrubia MJ, de la Fuente L, et al. connexin 43 gap junction distribution correlates with
Experimental and clinical regenerative capability of the location of reentrant circuits in the epicardial bor-
human bone marrow cells after myocardial infarction. der zone of healing canine infarcts that cause ventri-
Circ Res 2004;95:742-8. cular tachycardia. Circulation 1997;95:988-96.
8. Wollert KC, Meyer GP, Lotz J, Ringes-Lichtenberg S, 20. Wit AL, Janse MJ. The ventricular arrhythmias of
Lippolt P, Breidenbach C, et al. Intracoronary auto- ischemia and infarction. Electrophysiological mech-
logous bone-marrow cell transfer after myocardial anisms. Mount Kisco, NY: Futura Publishing; 1993.
infarction: the BOOST randomised controlled clinical 21. Ursell PC, Gardner PI, Albala A, Fenoglio JJ Jr, Wit AL.
trial. Lancet 2004;364:141-8. Structural and electrophysiological changes in the
Yonsei Med J Vol. 48, No. 5, 2007
Boyoung Joung, et al.
epicardial border zone of canine myocardial infarcts associated with coronary artery disease. In; Zipes DP,
during infarct healing. Circ Res 1985;56:436-51. Jalife J, editors. Cardiac electrophysiology: From cell to
22. de Bakker JM, van Capelle FJ, Janse MJ, Wilde AA, Bedside, 2nd ed. Philadelphia: WB Saunders; 1995.
Coronel R, Becker AE, et al. Reentry as a cause of ven- p.732-43.
tricular tachycardia in patients with chronic ischemic 24. Zhang YM, Hartzell C, Narlow M, Dudley SC Jr. Stem
heart disease: electrophysiologic and anatomic correla- cell-derived cardiomyocytes demonstrate arrhythmic
tion. Circulation 1988;77:589-606. potential. Circulation 2002;106:1294-9.
23. Callans DJ, Josephson ME. Ventricular tachycardia
Yonsei Med J Vol. 48, No. 5, 2007
You might also like
- Virtual Cardiologist LabDocument2 pagesVirtual Cardiologist LabVinsmoke SanjiNo ratings yet
- Mitral StenosisDocument29 pagesMitral Stenosisrameshbmc100% (7)
- Acls Algorithms 2021 ChecklistDocument1 pageAcls Algorithms 2021 ChecklistpepNo ratings yet
- Cardiac/Cardiogenic Shock: Clinical Practice GuidelinesDocument3 pagesCardiac/Cardiogenic Shock: Clinical Practice GuidelinesAnonymous Yo0mStNo ratings yet
- CV Karman TandonDocument3 pagesCV Karman TandonkarmantandonNo ratings yet
- Hypertonic Saline Attenuates Cord Swelling and Edema in Experimental Cord Injury - Experimental (2009) PDFDocument7 pagesHypertonic Saline Attenuates Cord Swelling and Edema in Experimental Cord Injury - Experimental (2009) PDFCoal CoalyNo ratings yet
- Echo 2Document16 pagesEcho 2Indera VyasNo ratings yet
- Mesenchymal Stem Cell Implantation in A Swine Myocardial Infarct Model: Engraftment and Functional EffectsDocument8 pagesMesenchymal Stem Cell Implantation in A Swine Myocardial Infarct Model: Engraftment and Functional EffectsAndrés AlvaradoNo ratings yet
- Fitzpatrick 2016Document13 pagesFitzpatrick 2016smansa123No ratings yet
- Jurnal 12Document10 pagesJurnal 12Zella ZakyaNo ratings yet
- Stem Cell Transplantation: The Lung Barrier: Cite This PaperDocument5 pagesStem Cell Transplantation: The Lung Barrier: Cite This Paper190384205058 Cilsa Nabila Hilal MandalikoNo ratings yet
- Physical Exercise Reduces Transplant Arteriosclerosis in A Mouse Aorta Transplantation ModelDocument8 pagesPhysical Exercise Reduces Transplant Arteriosclerosis in A Mouse Aorta Transplantation ModelNicoleta Popa-FoteaNo ratings yet
- 475 929 2 PBDocument6 pages475 929 2 PBErfaniNo ratings yet
- Evaluation of Morphological Changes in Experimental Models of Myocardial Infarction: Electron and Light Microscopical EvidenceDocument11 pagesEvaluation of Morphological Changes in Experimental Models of Myocardial Infarction: Electron and Light Microscopical EvidenceRania QhalisyaNo ratings yet
- Borenstein 05Document9 pagesBorenstein 05emmanuel le bretNo ratings yet
- JCTVS Myxo Ring Clinical Trial 2008Document9 pagesJCTVS Myxo Ring Clinical Trial 2008Nalini RajamannanNo ratings yet
- Comparizon of K-X and IsofluraneDocument24 pagesComparizon of K-X and IsofluraneIgnacio BarbieriNo ratings yet
- Volatile Anaesthetic Myocardial Protection: A Review of The Current LiteratureDocument5 pagesVolatile Anaesthetic Myocardial Protection: A Review of The Current Literatureserena7205No ratings yet
- Ischemic Preconditioning Does Not Acutely Improve Load-Insensitive Parameters of Contractility in in Vivo Stunned Porcine MyocardiumDocument8 pagesIschemic Preconditioning Does Not Acutely Improve Load-Insensitive Parameters of Contractility in in Vivo Stunned Porcine MyocardiumSol SolNo ratings yet
- Epidermoid Cysts TNEDocument10 pagesEpidermoid Cysts TNEbello_england_209552No ratings yet
- NeuralRegenRes9184-8563115 234711Document8 pagesNeuralRegenRes9184-8563115 234711JouleAlSBNo ratings yet
- Original Article: Transforming Growth Factor Beta-1 (Document8 pagesOriginal Article: Transforming Growth Factor Beta-1 (Lussiana Folleco InsuastyNo ratings yet
- Analysis and Results of Prolonged Resuscitation in Cardiac Arrest Patients Rescued by Extracorporeal Membrane OxygenationDocument7 pagesAnalysis and Results of Prolonged Resuscitation in Cardiac Arrest Patients Rescued by Extracorporeal Membrane OxygenationMuhammad RizqiNo ratings yet
- Determinants of Delayed Preconditioning Against Myocardial PDFDocument19 pagesDeterminants of Delayed Preconditioning Against Myocardial PDFSol SolNo ratings yet
- The Early Response To Major Trauma and Intramedullary Nailing PDFDocument5 pagesThe Early Response To Major Trauma and Intramedullary Nailing PDFantonio dengNo ratings yet
- Clinical Research: Heart Failure/cardiomyopathyDocument8 pagesClinical Research: Heart Failure/cardiomyopathyNoel Saúl Argüello SánchezNo ratings yet
- Sel Mesenkim 4Document10 pagesSel Mesenkim 4Ida Ifan YulianaNo ratings yet
- Acute Coronary Syndrome in Two Patients With Mechanical Valve ProsthesesDocument5 pagesAcute Coronary Syndrome in Two Patients With Mechanical Valve ProsthesesgalalNo ratings yet
- Cardio ResusiDocument9 pagesCardio ResusiDanarFauzanAdiPrayitnoNo ratings yet
- AJP Heart and Circulatory Physiology Volume 287 Issue 2 2004 (Doi 10.1152 - Ajpheart.01247.2003) Hodgson, D. M. - Stable Benefit of EmbryonDocument10 pagesAJP Heart and Circulatory Physiology Volume 287 Issue 2 2004 (Doi 10.1152 - Ajpheart.01247.2003) Hodgson, D. M. - Stable Benefit of EmbryonArini Dwi NastitiNo ratings yet
- Endovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterDocument5 pagesEndovascular Treatment of Intracranial Aneurysms: Initial Experience in A Low-Volume CenterAswin ChristantoNo ratings yet
- Circulation Research-2015 - E81-94Document40 pagesCirculation Research-2015 - E81-94acNo ratings yet
- Final Histological Assessment of Spinal Cord Injury - RevisedDocument18 pagesFinal Histological Assessment of Spinal Cord Injury - Revisedapi-308976551No ratings yet
- Rodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsDocument9 pagesRodriguez2005-Cognitive Dysfunction After Total Knee Arthroplasty - Effects of Intraoperative Cerebral Embolization and Postoperative ComplicationsSyahpikal SahanaNo ratings yet
- Disseccao Tipo b2Document6 pagesDisseccao Tipo b2coopervascba.diradmNo ratings yet
- EJVES VF Watanabe April 2020Document4 pagesEJVES VF Watanabe April 2020Francisco Álvarez MarcosNo ratings yet
- Barsheshet 2007Document7 pagesBarsheshet 2007Bambang DwiputraNo ratings yet
- Craneoplastia y Regulacion FSC Germany 00Document9 pagesCraneoplastia y Regulacion FSC Germany 00djcafNo ratings yet
- Intracardiac Echocardiography2Document12 pagesIntracardiac Echocardiography2Salah AttaNo ratings yet
- Etm 14 4 3563 PDFDocument6 pagesEtm 14 4 3563 PDFUlfahNo ratings yet
- Xin 2013Document5 pagesXin 2013Maximiliano PfannlNo ratings yet
- Tissue EngineeringDocument12 pagesTissue EngineeringcerebruzNo ratings yet
- Article - Sequential Bypass Grafting On The Beating Heart - Blood Flow CharacteristicsDocument4 pagesArticle - Sequential Bypass Grafting On The Beating Heart - Blood Flow Characteristicsfluid_man_brazilNo ratings yet
- Cerebral Monitoring During Carotid Endarterectomy by Transcranial Doppler UltrasonographyDocument5 pagesCerebral Monitoring During Carotid Endarterectomy by Transcranial Doppler UltrasonographyAmira DayoubNo ratings yet
- Ross OtoHNS2005 ArterialCouplingDocument5 pagesRoss OtoHNS2005 ArterialCouplingSungjin SongNo ratings yet
- Recombinant Human Vascular Endothelial Growth Factor Enhances Bone Healing in An Experimental Nonunion ModelDocument9 pagesRecombinant Human Vascular Endothelial Growth Factor Enhances Bone Healing in An Experimental Nonunion ModelAnton NopiarNo ratings yet
- Transplantation of Human Placenta-Derived Mesenchymal StemDocument17 pagesTransplantation of Human Placenta-Derived Mesenchymal Stemvirginia.mirandaNo ratings yet
- JHLT Abstract 2019-2Document1 pageJHLT Abstract 2019-2G WNo ratings yet
- Advances in Acute Stroke Treatment 2020Document6 pagesAdvances in Acute Stroke Treatment 2020ayman shomanNo ratings yet
- Apoptosis Post Microwave Ablation of The Liver: Does It Change With Power?Document6 pagesApoptosis Post Microwave Ablation of The Liver: Does It Change With Power?asclepiuspdfsNo ratings yet
- Intervesnsi Stroke 1Document9 pagesIntervesnsi Stroke 1Zilbran BerontaxNo ratings yet
- A Simple and Fast Experimental Model: Laboratory InvestigationDocument4 pagesA Simple and Fast Experimental Model: Laboratory InvestigationAjay PeddiNo ratings yet
- Crocin Attenuates Oxidative Stress and Myocardial Infarction Injury in RatsDocument7 pagesCrocin Attenuates Oxidative Stress and Myocardial Infarction Injury in RatsAdrian BratuNo ratings yet
- JurnalDocument9 pagesJurnalSiscaNo ratings yet
- Midterm Results of Mitral Valve Repair With Homemade Annuloplasty RingsDocument4 pagesMidterm Results of Mitral Valve Repair With Homemade Annuloplasty Ringsadel husseinNo ratings yet
- Chiu 2006Document8 pagesChiu 2006r esspNo ratings yet
- Arrhythmogenic Right Ventricular Cardiomyopathy in A WeimaranerDocument5 pagesArrhythmogenic Right Ventricular Cardiomyopathy in A WeimaranerEmilia AmmariNo ratings yet
- Ehx493 P5438Document1 pageEhx493 P5438Anonymous NeRC5JYiSNo ratings yet
- Veterinary Medicine Today ECG of The MonthDocument4 pagesVeterinary Medicine Today ECG of The Monthabc defNo ratings yet
- Tenecteplase in StrokeDocument10 pagesTenecteplase in StrokeJorge BarriosNo ratings yet
- Tendinitis Crónica Articulo en InglesDocument6 pagesTendinitis Crónica Articulo en IngleskarolndNo ratings yet
- Effect of Pneumatic Tubing System Transport On Platelet Apheresis UnitsDocument13 pagesEffect of Pneumatic Tubing System Transport On Platelet Apheresis Unitsrizka widyanaNo ratings yet
- Conclusion: Long-Term Follow-Up ForDocument31 pagesConclusion: Long-Term Follow-Up ForHima HuNo ratings yet
- Araszkiewicz Et Al. - 2014 - Postconditioning Reduces Enzymatic Infarct Size and Improves Microvascular Reperfusion in Patients With STDocument8 pagesAraszkiewicz Et Al. - 2014 - Postconditioning Reduces Enzymatic Infarct Size and Improves Microvascular Reperfusion in Patients With STscribd mendeleyNo ratings yet
- Clinical Handbook of Cardiac ElectrophysiologyFrom EverandClinical Handbook of Cardiac ElectrophysiologyBenedict M. GloverNo ratings yet
- Fast Two-Photon in Vivo Imaging With Three-Dimensional Random-Access Scanning in Large Tissue VolumesDocument11 pagesFast Two-Photon in Vivo Imaging With Three-Dimensional Random-Access Scanning in Large Tissue Volumesiulia andreeaNo ratings yet
- Eliasmith2012-Large-Scale Model of The Brain-SupplDocument38 pagesEliasmith2012-Large-Scale Model of The Brain-Suppliulia andreeaNo ratings yet
- Sylwestrak2012 Elfn1Document6 pagesSylwestrak2012 Elfn1iulia andreeaNo ratings yet
- Science 2012 Machens Building The Human BrainDocument3 pagesScience 2012 Machens Building The Human Brainiulia andreeaNo ratings yet
- Miller2012 Braqin TeasersDocument1 pageMiller2012 Braqin Teasersiulia andreeaNo ratings yet
- Transcriptome and Epigenome Landscape of Human Cortical Development Modeled in OrganoidsDocument11 pagesTranscriptome and Epigenome Landscape of Human Cortical Development Modeled in Organoidsiulia andreeaNo ratings yet
- Miller2012-Why Is Mental Ilness So Hard To TreatDocument2 pagesMiller2012-Why Is Mental Ilness So Hard To Treatiulia andreeaNo ratings yet
- McBain2012-Decoding The Neuronal Tower of BabelDocument3 pagesMcBain2012-Decoding The Neuronal Tower of Babeliulia andreeaNo ratings yet
- Vogel2012-Can We Make Our Brains More PlasticDocument3 pagesVogel2012-Can We Make Our Brains More Plasticiulia andreeaNo ratings yet
- Balter2012-Why Are Our Brains So BigDocument2 pagesBalter2012-Why Are Our Brains So Bigiulia andreeaNo ratings yet
- Leathers&Olson2012-LIP Neurons Encode Cue SalienceDocument5 pagesLeathers&Olson2012-LIP Neurons Encode Cue Salienceiulia andreeaNo ratings yet
- Eisch&Petrik2012-Depression and Hippocampal NeurogenesisDocument5 pagesEisch&Petrik2012-Depression and Hippocampal Neurogenesisiulia andreeaNo ratings yet
- Stern2012-Defeating The DementorsDocument1 pageStern2012-Defeating The Dementorsiulia andreeaNo ratings yet
- Scheer2006 Caspase InhibitorsDocument6 pagesScheer2006 Caspase Inhibitorsiulia andreeaNo ratings yet
- Wedeen2012-Grid Structure of Brain Pathways-SOMDocument25 pagesWedeen2012-Grid Structure of Brain Pathways-SOMiulia andreeaNo ratings yet
- Karlsson2012-Network Resets in Prefrontal CortexDocument6 pagesKarlsson2012-Network Resets in Prefrontal Cortexiulia andreeaNo ratings yet
- Gerstner2012-Theory and Simulation in NeuroscienceDocument7 pagesGerstner2012-Theory and Simulation in Neuroscienceiulia andreeaNo ratings yet
- Koo2012-BDNF Negative Regulator of Morphin ActionDocument6 pagesKoo2012-BDNF Negative Regulator of Morphin Actioniulia andreeaNo ratings yet
- Tiwari-Woodruff2007-estrogen Recs&ms ModelDocument6 pagesTiwari-Woodruff2007-estrogen Recs&ms Modeliulia andreeaNo ratings yet
- Wang2008-Diploid Genome Sequence of An Asian IndividualDocument7 pagesWang2008-Diploid Genome Sequence of An Asian Individualiulia andreeaNo ratings yet
- Pastalkova2008 SupplDocument28 pagesPastalkova2008 Suppliulia andreeaNo ratings yet
- Baratta2002-Somatostatin LTP Dentate GyrusDocument9 pagesBaratta2002-Somatostatin LTP Dentate Gyrusiulia andreeaNo ratings yet
- Altshuler2008-Genetic Mapping in Human DiseaseDocument9 pagesAltshuler2008-Genetic Mapping in Human Diseaseiulia andreeaNo ratings yet
- BlissDocument7 pagesBlissiulia andreeaNo ratings yet
- Liu2007 Sox17Document7 pagesLiu2007 Sox17iulia andreeaNo ratings yet
- Wang2007 Icaritin NeuroprotectionDocument12 pagesWang2007 Icaritin Neuroprotectioniulia andreeaNo ratings yet
- Knowles2007-Kinetics and Thermodynamics of Amyloid AggregationDocument7 pagesKnowles2007-Kinetics and Thermodynamics of Amyloid Aggregationiulia andreeaNo ratings yet
- Oakes-Mitochondria Ca Immune SynapseDocument2 pagesOakes-Mitochondria Ca Immune Synapseiulia andreeaNo ratings yet
- Schridde2006 IhDocument13 pagesSchridde2006 Ihiulia andreeaNo ratings yet
- Jan1998-Ion Channels & Neurologic DiseaseDocument8 pagesJan1998-Ion Channels & Neurologic Diseaseiulia andreeaNo ratings yet
- 0298-W1403570 NT Dg3002ih Ang 03 03Document299 pages0298-W1403570 NT Dg3002ih Ang 03 03JORGE NAVARRONo ratings yet
- Brugada Syndrome ECGDocument34 pagesBrugada Syndrome ECGMohammad Irfan100% (1)
- ACS LectureDocument55 pagesACS LectureAyunda AlmiradaniNo ratings yet
- Physical Examination of Cardiovascular SystDocument13 pagesPhysical Examination of Cardiovascular Systgamal attamNo ratings yet
- Cardiac Surgery - Postoperative ArrhythmiasDocument9 pagesCardiac Surgery - Postoperative ArrhythmiaswanariaNo ratings yet
- Đề số 29Document5 pagesĐề số 29Mëssënġër Việt NamNo ratings yet
- NN Drip ObatDocument7 pagesNN Drip ObatDioniivanNo ratings yet
- DapusDocument4 pagesDapusAtika DalilaaNo ratings yet
- 2 Anaesthesia TriadDocument2 pages2 Anaesthesia TriadFarrukh Ali KhanNo ratings yet
- Heart AnatomyDocument178 pagesHeart AnatomysubbuNo ratings yet
- Risk of Arrhythmia and Sudden Death - M. Malik (BMJ, 2001) WWDocument429 pagesRisk of Arrhythmia and Sudden Death - M. Malik (BMJ, 2001) WWRohan Upadhyay UpadhyayNo ratings yet
- Beating Heart Tech Brochure 200701512c - ENDocument6 pagesBeating Heart Tech Brochure 200701512c - ENWinta Sari AprilianaNo ratings yet
- Mending Broken Hearts: by Jennifer Kahn Photograph by Robert ClarkDocument3 pagesMending Broken Hearts: by Jennifer Kahn Photograph by Robert Clarkmonalall0% (1)
- CardiomyopathyDocument9 pagesCardiomyopathyMinh Nguyễn Phương HồngNo ratings yet
- Soca CHF LuhurDocument5 pagesSoca CHF LuhurPradana Nur OviyantiNo ratings yet
- Autopulse Ems Brochure UkDocument5 pagesAutopulse Ems Brochure UkForum PompieriiNo ratings yet
- Angina PectorisDocument4 pagesAngina PectorisJohiarra Madanglog TabigneNo ratings yet
- Stoelting Anasthesia and Co Existing Disease PDFDocument28 pagesStoelting Anasthesia and Co Existing Disease PDFEgidia SetyaNo ratings yet
- Nikaidoh Procedure: A Perspective: EditorialDocument5 pagesNikaidoh Procedure: A Perspective: Editorialmihalcea alinNo ratings yet
- Pathologt of The HeartDocument40 pagesPathologt of The HeartJudithNo ratings yet
- Ic Guía Esc 2021-99-128Document30 pagesIc Guía Esc 2021-99-128aassNo ratings yet
- Step by Step Echocardiography in Congenital Heart DiseasesDocument224 pagesStep by Step Echocardiography in Congenital Heart DiseasesEbookStore.DocNo ratings yet
- Time Table Cardiology: Da y Date Topic Learning Situation English Class Regular Class PICDocument5 pagesTime Table Cardiology: Da y Date Topic Learning Situation English Class Regular Class PICSheryl ElitaNo ratings yet
- Or-DR Tally FinalDocument1 pageOr-DR Tally FinalMarvinNo ratings yet
- Left Ventricular FailureDocument17 pagesLeft Ventricular Failurenisha24100% (1)