Professional Documents
Culture Documents
2013, Treatment of Severe Metabolic Alkalosis in Patients With CHF
2013, Treatment of Severe Metabolic Alkalosis in Patients With CHF
Uploaded by
Angelin GozaliCopyright:
Available Formats
You might also like
- Updated List of All PLAB 2 StationsDocument9 pagesUpdated List of All PLAB 2 StationsDr-Arif Rehman100% (1)
- Acute Renal Failure Complicated by Multiple Bee Stings: A Case Report and Literature ReviewDocument3 pagesAcute Renal Failure Complicated by Multiple Bee Stings: A Case Report and Literature ReviewHafizah FzNo ratings yet
- AcuteLiverFailureUpdate201journalformat1 PDFDocument26 pagesAcuteLiverFailureUpdate201journalformat1 PDFDewanggaWahyuPrajaNo ratings yet
- AcuteLiverFailureUpdate201journalformat1 2 PDFDocument26 pagesAcuteLiverFailureUpdate201journalformat1 2 PDFHuy HuynhNo ratings yet
- Hypokalemic Periodic Paralysis A Case ReportDocument2 pagesHypokalemic Periodic Paralysis A Case ReportEditor IJTSRDNo ratings yet
- Fígado Acute Liver FailureDocument6 pagesFígado Acute Liver FailureEdson MarquesNo ratings yet
- A Physiologic-Based Approach To The Treatment of A Patient With HypokalemiaDocument6 pagesA Physiologic-Based Approach To The Treatment of A Patient With HypokalemiaPablo IgnacioNo ratings yet
- Hypokalaemia Periodic Paralysis: Liam J StapletonDocument4 pagesHypokalaemia Periodic Paralysis: Liam J StapletonJL DeomampoNo ratings yet
- Overview of Management of Acute Renal Failure andDocument6 pagesOverview of Management of Acute Renal Failure andParhimpunan NasutionNo ratings yet
- Approach To Treatment of Hypophosphatemia: Acid-Base and Electrolyte Teaching CaseDocument7 pagesApproach To Treatment of Hypophosphatemia: Acid-Base and Electrolyte Teaching CasemasranraisaNo ratings yet
- Hypokalemic Paralysis PDFDocument7 pagesHypokalemic Paralysis PDFFanny SimaNo ratings yet
- Furosemide in The Long-Term Management of Heart Failure: The Good, The Bad, and The UncertainDocument3 pagesFurosemide in The Long-Term Management of Heart Failure: The Good, The Bad, and The UncertainFauzan AprnNo ratings yet
- A Case Report of An Unusual Complication of Amanita Phalloides PoisoningDocument3 pagesA Case Report of An Unusual Complication of Amanita Phalloides PoisoningArmando BetancourthNo ratings yet
- Lectura Recomendada HiperkalemiaDocument7 pagesLectura Recomendada HiperkalemianeomaosNo ratings yet
- Hyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDocument8 pagesHyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDaniel HeSaNo ratings yet
- Hiperkalemia en ERDocument8 pagesHiperkalemia en ERmjbb1310No ratings yet
- Weissbach 2010Document2 pagesWeissbach 2010VALERIA VARGAS LOZANONo ratings yet
- Acute Liver FailureDocument46 pagesAcute Liver FailureDoc On CallNo ratings yet
- Hepatic Encephalopathy: Diagnosis and Management: Piero AmodioDocument10 pagesHepatic Encephalopathy: Diagnosis and Management: Piero AmodioMarcel DocNo ratings yet
- Ala 2019Document4 pagesAla 2019Timea SzuszerNo ratings yet
- Acute Liver Failure: Concise ReviewDocument8 pagesAcute Liver Failure: Concise ReviewJoseph Stans KasiryeNo ratings yet
- 10 1 1 622 7158 PDFDocument8 pages10 1 1 622 7158 PDFz31nNo ratings yet
- Conundrum in An Asthma Exacerbation: BMJ Case Reports May 2016Document5 pagesConundrum in An Asthma Exacerbation: BMJ Case Reports May 2016Jamaica Malunes ManuelNo ratings yet
- 469 FullDocument7 pages469 FullCristina Adriana PopaNo ratings yet
- Neuro4Nurses: Syndrome of Inappropriate Release of Antidiuretic HormoneDocument2 pagesNeuro4Nurses: Syndrome of Inappropriate Release of Antidiuretic HormoneM Zainun IrsyadNo ratings yet
- Weakness Following Diarrhea: 1/4: 1. What Can Be The Cause of Her Condition?Document4 pagesWeakness Following Diarrhea: 1/4: 1. What Can Be The Cause of Her Condition?ZauzaNo ratings yet
- Tebak AjaDocument3 pagesTebak AjaSanti P TambunanNo ratings yet
- Management of Acute Liver Failure: A. Initial Evaluation and TriageDocument3 pagesManagement of Acute Liver Failure: A. Initial Evaluation and TriagePande Indra PremanaNo ratings yet
- Falla HepaticaDocument24 pagesFalla HepaticaCbrera ValentinaNo ratings yet
- How Dangerous Is Hyperkalemia?Document11 pagesHow Dangerous Is Hyperkalemia?Erika SalazarNo ratings yet
- 13no2 3Document5 pages13no2 3Wisnu WardanaNo ratings yet
- Arritmias X HipercalemiaDocument9 pagesArritmias X Hipercalemiafh2301lrNo ratings yet
- Acute Liver Injury and FailureDocument14 pagesAcute Liver Injury and FailureWeslei ChaconNo ratings yet
- Anuria Oliguria: A Review RatesDocument7 pagesAnuria Oliguria: A Review Ratessurya rajNo ratings yet
- Criticallyillpatientswith End-Stageliverdisease: Sara CragerDocument17 pagesCriticallyillpatientswith End-Stageliverdisease: Sara CragerHima OmerNo ratings yet
- Case ScenarioDocument9 pagesCase ScenarioKM DelantarNo ratings yet
- Extracorporeal Liver Assist Device To Exchange Albumin and Remove Endotoxin in Acute Liver Failure: Results of A Pivotal Pre-Clinical StudyDocument9 pagesExtracorporeal Liver Assist Device To Exchange Albumin and Remove Endotoxin in Acute Liver Failure: Results of A Pivotal Pre-Clinical StudyIwan Budianto HadiNo ratings yet
- I Am Sharing 'Case Study NCM 118' With YouDocument6 pagesI Am Sharing 'Case Study NCM 118' With YouQusai BassamNo ratings yet
- 9 Case Report-HyponatremiaDocument2 pages9 Case Report-HyponatremiaKamal Kumar Kamal KumarNo ratings yet
- Management of Acute Liver Failure in The Intensive Care Unit SettingDocument6 pagesManagement of Acute Liver Failure in The Intensive Care Unit SettingCristian CollazosNo ratings yet
- Article - Liver Dysfunction in SepsisDocument6 pagesArticle - Liver Dysfunction in Sepsisthys2000No ratings yet
- Case Report Hyperthyroid-Acute LiverDocument5 pagesCase Report Hyperthyroid-Acute Liverpratiwi saputriNo ratings yet
- Anti Hepatic FailureDocument4 pagesAnti Hepatic Failuregoyabeb59No ratings yet
- GH 05 647Document10 pagesGH 05 647Ema Emanuela SarcaNo ratings yet
- Shah 2019Document2 pagesShah 2019khadidja BOUTOUILNo ratings yet
- R Falla Hepatica 16 GuiasDocument35 pagesR Falla Hepatica 16 GuiasRICARDO BOSSANo ratings yet
- Asidosis Laktat 2Document10 pagesAsidosis Laktat 2MizanMaulanaNo ratings yet
- Dysnatremia in The ICU: Milap Pokaharel and Clay A. BlockDocument13 pagesDysnatremia in The ICU: Milap Pokaharel and Clay A. BlockJonathan Gustavo MenaNo ratings yet
- Arterial Ammonia and Clinical Risk Factors For Encephalopathy and Intracranial Hypertension in Acute Liver FailureDocument9 pagesArterial Ammonia and Clinical Risk Factors For Encephalopathy and Intracranial Hypertension in Acute Liver FailureChannesya TanNo ratings yet
- Ac 1Document12 pagesAc 1Alamsyah TegarNo ratings yet
- Falla CardiacaDocument6 pagesFalla CardiacaFelipeNo ratings yet
- Systemic AmiloidosisDocument4 pagesSystemic AmiloidosisioannesturrisoricisNo ratings yet
- Seizures, Antiepileptic Drugs, and CKD: in PracticeDocument12 pagesSeizures, Antiepileptic Drugs, and CKD: in Practicefais123No ratings yet
- Seizures, Antiepileptic Drugs, and CKDDocument12 pagesSeizures, Antiepileptic Drugs, and CKDRudeus GreyratNo ratings yet
- Chapter 5: Electrolyte and Acid - Base Disorders in MalignancyDocument7 pagesChapter 5: Electrolyte and Acid - Base Disorders in MalignancyPratita Jati PermatasariNo ratings yet
- Electrolyte Disorders: Camiron L. Pfennig and Corey M. SlovisDocument18 pagesElectrolyte Disorders: Camiron L. Pfennig and Corey M. SlovisMutianbllNo ratings yet
- Case HipotiroidDocument3 pagesCase HipotiroidVivi DeviyanaNo ratings yet
- 403 Bargman FINALDocument5 pages403 Bargman FINALTiago Francisco Meleiro ZubioloNo ratings yet
- ALF 418RLE Group1Document21 pagesALF 418RLE Group1PAOLA LUZ CRUZNo ratings yet
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?From EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?No ratings yet
- 17 - 3510 - DR Batool Butt - DoneDocument6 pages17 - 3510 - DR Batool Butt - DoneUsama Bin ZubairNo ratings yet
- Bacterial MeningitisDocument51 pagesBacterial MeningitiscaseinrenninNo ratings yet
- اخطاء انكسار 4Document4 pagesاخطاء انكسار 4Hassan AljaberiNo ratings yet
- SOME MCQ'S, CLASS OF 2020Document10 pagesSOME MCQ'S, CLASS OF 2020BISMARCK BANAHENE BOAHENENo ratings yet
- Amina Rizvon Finalfamous PersonDocument7 pagesAmina Rizvon Finalfamous Personapi-664229394No ratings yet
- 6 Thrombosis MorphologyDocument20 pages6 Thrombosis MorphologySawera RaheemNo ratings yet
- Controversies in The Management of Functional Constipation in ChildrenDocument8 pagesControversies in The Management of Functional Constipation in ChildrenDaniela Rodríguez MartínezNo ratings yet
- A Case of Fatal Multi-Organ Inflammation Following COVID-19 VaccinationDocument4 pagesA Case of Fatal Multi-Organ Inflammation Following COVID-19 VaccinationAmarpreet Singh MalhanNo ratings yet
- Luttik Et Al-2007-European Journal of Heart FailureDocument7 pagesLuttik Et Al-2007-European Journal of Heart FailureSiti lestarinurhamidahNo ratings yet
- Meropenem - Drug Information - UpToDate-3Document8 pagesMeropenem - Drug Information - UpToDate-3Vh TRNo ratings yet
- Ma 2021 Uveitis 101Document5 pagesMa 2021 Uveitis 101Jenny MaNo ratings yet
- Sign, Sypmtoms and Tretment of PosioningDocument18 pagesSign, Sypmtoms and Tretment of PosioningmaryamNo ratings yet
- Preeclampsia 2022Document16 pagesPreeclampsia 2022Jose DuranNo ratings yet
- A Detailed Lesson Plan in Living ThingsDocument23 pagesA Detailed Lesson Plan in Living ThingsclarisseNo ratings yet
- Bacterionomicon Digital PDFDocument77 pagesBacterionomicon Digital PDFMichelle LindsayNo ratings yet
- Besant Hypnotism and Mesmerism 1935Document86 pagesBesant Hypnotism and Mesmerism 1935Abdul Hakeem100% (1)
- PEDIA 1 The Pediatric History and Physical Exam HandoutDocument16 pagesPEDIA 1 The Pediatric History and Physical Exam HandoutRyan Loyd MarquezNo ratings yet
- Acupuncture Points ChartDocument9 pagesAcupuncture Points ChartAnnaNo ratings yet
- Research Proposal Paper - Ian GraffDocument5 pagesResearch Proposal Paper - Ian Graffapi-614243581No ratings yet
- ADHD Dari KaplanDocument25 pagesADHD Dari KaplanAldo D'vatho MpNo ratings yet
- A-Level Psychology - Mock Test 1 1Document4 pagesA-Level Psychology - Mock Test 1 1Kristen LeNo ratings yet
- Behavioral Variant Frontotemporal DementiaDocument24 pagesBehavioral Variant Frontotemporal DementiaADRIANA MARCELA YARA DUARTENo ratings yet
- IPD A Cardiovascular System Bates and and VideoDocument10 pagesIPD A Cardiovascular System Bates and and Videostar220498No ratings yet
- 2 5406729617908171096 PDFDocument506 pages2 5406729617908171096 PDFKamal Jauoda100% (1)
- Surgical Management of Head and Neck RDDDocument6 pagesSurgical Management of Head and Neck RDDDevy OctaviaNo ratings yet
- Immunity WorksheetDocument4 pagesImmunity WorksheetShahd MohamedNo ratings yet
- Anemia Table283Document2 pagesAnemia Table283Bridget ParkerNo ratings yet
- Nursing Care Plan: FeverDocument1 pageNursing Care Plan: FeverOlive Claire T. ManlambusNo ratings yet
- Woc Acute Pancreatitis EngDocument10 pagesWoc Acute Pancreatitis EngMuhammad Alvin Fuzail IyazNo ratings yet
2013, Treatment of Severe Metabolic Alkalosis in Patients With CHF
2013, Treatment of Severe Metabolic Alkalosis in Patients With CHF
Uploaded by
Angelin GozaliOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2013, Treatment of Severe Metabolic Alkalosis in Patients With CHF
2013, Treatment of Severe Metabolic Alkalosis in Patients With CHF
Uploaded by
Angelin GozaliCopyright:
Available Formats
Acid-Base and Electrolyte Teaching Case
Treatment of Severe Metabolic Alkalosis in a Patient With
Congestive Heart Failure
Aldo J. Peixoto, MD,1,2 and Robert J. Alpern, MD1
Metabolic alkalosis, isolated or in combination with another abnormality, is the most common acid-base
disorder in patients with congestive heart failure. In most cases, it is a result of diuretic therapy, which causes
activation of the renin-angiotensin system, chloride depletion, increased distal sodium delivery, hypokalemia,
and increased urine acidification, all of which contribute to bicarbonate retention. In addition, the disease state
itself results in neurohormonal activation (renin-angiotensin system, sympathetic nervous system, and endothe-
lin) that further amplifies the tendency toward alkalosis. Treatment of metabolic alkalosis is based on the
elimination of generation and maintenance factors, chloride and potassium repletion, enhancement of renal
bicarbonate excretion (such as acetazolamide), direct titration of the base excess (hydrochloric acid), or, if
accompanied by kidney failure, low-bicarbonate dialysis. In congestive heart failure, appropriate management
of circulatory failure and use of an aldosterone antagonist in the diuretic regimen are integral to treatment.
Am J Kidney Dis. 61(5):822-827. Published by Elsevier Inc. on behalf of the National Kidney Foundation, Inc.
This is a US Government Work. There are no restrictions on its use.
INDEX WORDS: Metabolic alkalosis; treatment; congestive heart failure.
ing the risks and benefits of various treatment strate-
Note from Feature Editor Jeffrey A. Kraut, MD: This article is
part of a series of invited case discussions highlighting either gies.
the diagnosis or treatment of acid-base and electrolyte disor-
ders. The present case discussion is the second of 2 articles CASE REPORT
discussing metabolic alkalosis. In this article, Drs Peixoto
Clinical History and Initial Laboratory Data
and Alpern present their approach to the treatment of meta-
bolic alkalosis; in the first teaching case, Gennari et al1 de- A 68-year-old man was transferred to the intensive care unit due
scribe a physiologic-based approach to its diagnosis and to atrial fibrillation and pulmonary edema requiring intubation. His
evaluation. history was significant for hypertension, coronary artery disease,
CHF with preserved systolic function, obesity, and a recent pulmo-
nary embolus. He had been in the hospital for approximately 3
weeks undergoing treatment for L5-S1 Enterococcus faecalis
osteomyelitis. During this period, he had persistent signs of vol-
ume overload but received only intermittent doses of furosemide
INTRODUCTION due to concerns about his kidney function in the setting of infection
and poor oral intake. Three days prior to transfer, he developed
Metabolic alkalosis is a common complication of more overt signs of CHF, prompting more aggressive use of
congestive heart failure (CHF) and its treatment with furosemide (40-80 mg intravenously [IV] twice daily). Despite
these efforts, he remained volume overloaded and developed
diuretics.2 When severe, the alkalosis can have signifi- pulmonary edema requiring intubation during an episode of rapid
cant adverse effects on cellular function, as shown in atrial fibrillation that could not be controlled promptly.
Table 1, and contribute to increased mortality. There- Medications at the time of intensive care unit admission in-
fore, identifying this acid-base disorder and initiating cluded ampicillin/sulbactam, gentamicin, aspirin, IV heparin, furo-
semide (80 mg IV twice daily), potassium chloride (40 mEq twice
specific treatment is important. In the present teaching
daily), lisinopril (20 mg daily), metoprolol tartrate (150 mg twice
case, we discuss the treatment of a patient with severe daily), transdermal nitroglycerin, simvastatin, morphine, omepra-
metabolic alkalosis with underlying CHF, emphasiz- zole, and tamsulosin.
On examination, the patient was afebrile with blood pressure of
150/64 mm Hg, heart rate of 105 beats/min, and oxygen saturation
1
From the Section of Nephrology, Yale University School of Medi- of 91% on 60% inhaled oxygen. His jugular veins could not be
cine; and 2VA Connecticut Healthcare System, West Haven, CT. assessed adequately. He had bibasilar crackles, heart beat was
Received April 25, 2011. Accepted in revised form October 12, irregular with a third sound, and he had edema (2⫹) of the legs.
2012. Originally published online March 7, 2013.
Address correspondence to Aldo J. Peixoto, MD, Medical Ser- Additional Investigations
vice-111, 950 Campbell Ave, West Haven, CT 06516. E-mail: Relevant laboratory test results are listed in Table 2. A chest film
aldo.peixoto@yale.edu showed pulmonary edema. The electrocardiogram revealed atrial
Published by Elsevier Inc. on behalf of the National Kidney fibrillation and no signs of acute ischemia. An echocardiogram
Foundation, Inc. This is a US Government Work. There are no showed atrial dilatation, moderate aortic insufficiency and mitral
restrictions on its use. regurgitation (with normal valve morphology), left ventricular
0272-6386/$0.00 ejection fraction of 50% with mild posterobasal hypokinesis, and
http://dx.doi.org/10.1053/j.ajkd.2012.10.028 impaired diastolic filling. Right ventricular function was normal.
822 Am J Kidney Dis. 2013;61(5):822-827
Metabolic Alkalosis in CHF
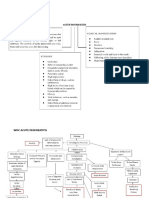
Table 1. Acid-Base Abnormalities in Patients With Congestive acid-base and electrolyte issues were not a problem during the rest
Heart Failure of his hospitalization, although he had, as noted in Table 2,
persistent respiratory alkalosis explained by his long-term ventila-
% of tor dependence, frequent episodes of systemic infection, and
Acid-Base Abnormalities Patients agitated delirium.
Overall prevalence 46 DISCUSSION
Specific disorders: Few studies have systematically evaluated the preva-
Isolated metabolic alkalosis 16
Isolated respiratory alkalosis 11
lence of acid-base disturbances in CHF. We compiled
Combined metabolic and respiratory alkalosis 13 data from 4 studies that reported detailed information
Combined metabolic alkalosis and respiratory 2 for acid-base status and/or reported specific frequen-
acidosis cies of individual disorders in 170 patients with CHF
Isolated metabolic acidosis 4 and no pulmonary disease.3-6 As shown in Table 1, a
Note: Table based on data from 170 patients with heart failure total of 46% had at least one acid-base abnormality,
and no overt pulmonary disease. most commonly metabolic alkalosis, alone or paired
Sources: Elisaf and Siamopoulos,3 Milionis and Elisaf,4 Riggio
and Clemente,5 and Squires et al.6
with respiratory alkalosis. Two other large series con-
firm the trend toward alkalemia of mixed metabolic
The patient underwent diuresis with IV furosemide with gradual
and respiratory origin in unselected patients with
improvement in congestion. However, he developed progressive advanced heart failure.7,8 Alkalemia is more common
alkalemia and severe hypokalemia over the ensuing 5 days. in patients with more advanced CHF (36% in patients
with class IV symptoms compared with 11% of those
Diagnosis with class III symptoms3). In addition, diuretic therapy
CHF; metabolic alkalosis due to heart failure and loop diuretic increases the prevalence of metabolic alkalosis,8 al-
use; hypokalemia due to loop diuretic use and secondary hyperal- though patients who experience significant improve-
dosteronism from decompensated heart failure.
ment in circulatory status with diuretic therapy may
Clinical Follow-up improve their alkalosis.9 Although it is possible that
Table 2 shows the temporal trend of the patient’s fluid balance, alkalemia is associated with worse outcomes in CHF,
potassium level, and acid-base status. The sequential addition of as noted in other populations,10,11 this hypothesis has
spironolactone and later acetazolamide led to improvement in not been formally tested in the literature.
these metabolic derangements while allowing him to remain in The metabolic alkalosis of CHF most commonly is
adequate fluid balance. However, he remained intubated due to a generated by diuretic therapy. The mechanisms in-
complicating pneumonia and deconditioning, requiring tracheos-
tomy and long-term ventilatory support. He had a complicated volved in the alkalosis caused by loop diuretics in-
course and died 2 months later of another ventilator-associated clude chloride loss, decreased effective circulating
pneumonia. He retained stable volume control, and metabolic volume, activation of the renin-angiotensin-aldoste-
Table 2. Clinical Course of Fluid Balance and Relevant Laboratory Tests
Day ⴚ5 Day ⴚ3 Day 0 Day 3 Day 6 Day 10 Day 15
Clinical events Pulmonary Furosemide Intubation for SPRL started, Acetazolamide started, Acetazolamide stopped, Still mechanically
embolus started pulmonary aggressive furosemide held, SPRL continued; ventilated,
edema potassium SPRL continued; furosemide still held often agitated
repletion new pneumonia,
unable to wean from
ventilator
BP (mm Hg)a 120/68 132/60 150/64 147/65 133/54 126/52 108/45
Fluid balance (L)b (reference) ⫹3.4 ⫹1 ⫺2.8 ⫺8.4 ⫺9.5 ⫺8.5
CVP (mm Hg)a NA NA 18 11 8 NA NA
Laboratory tests
Creatinine (mg/dL) 1.7 1.2 1.6 1.6 1.5 1.4 1.5
Sodium (mEq/L)c 142 142 143; 99 (urine) 147; 73 (urine) 141 138 137
Potassium (mEq/L)c 4 3.4 2.8; 53 (urine) 3; 118 (urine) 4 3.8 4
Chloride (mEq/L)c 105 107 102; 65 (urine) 107; 110 (urine) 105 99 100
Bicarbonate (mEq/L) 25 26.5 31.1 38.4 35.8 28.5 21.1
Arterial PCO2 (mm Hg) 36 36 39 54 40 41 31
Arterial pH 7.46 7.49 7.52 7.47 7.57 7.46 7.46
Note: Conversion factor for serum creatinine in mg/dL to mol/L, ⫻88.4.
Abbreviations: BP, blood pressure; CVP, central venous pressure; NA, not available; SPRL, spironolactone.
a
Representative average value at each time.
b
Fluid balance: all measurements are listed in comparison to day ⫺5. Weights were not consistently available for this patient.
c
Serum measurements except as indicated.
Am J Kidney Dis. 2013;61(5):822-827 823
Peixoto and Alpern
Box 1. Adverse Clinical and Physiologic Effects of Alkalemia Unadjusted analyses indicate that patients who have
That Justify Therapy metabolic alkalosis have increased hospital mortality,
● Vasoconstriction (hypertension, myocardial ischemia, cere- which is noticeable at pH ⬎7.50 (43%) and is most
bral ischemia) significant when pH is ⬎7.60 (61%).10,11 Addition-
● Seizures
● Delirium ally, it appears that most of this risk is related to
● Cardiac arrhythmias (mostly due to associated hypokalemia) metabolic, not respiratory, alkalosis,11 thus separating
● Hypoventilation leading to hypercapnia and hypoxia the impact of pH itself from that of the underlying
● Hypokalemia mechanisms. To date, no well-designed observational
● Hypocalcemia
● Hypomagnesemia
studies have been published to confirm or refute these
● Hypophosphatemia (primarily in respiratory alkalosis) observations. Therefore, the decision to treat meta-
Sources: Adrogué and Madias19 and Galla.20
bolic alkalosis is based on opinion: we believe that
patients with pH ⬎7.50 should have the process
addressed “semiurgently” (ie, correction within days),
rone system, increased sodium delivery to the distal and if pH is ⬎7.60, immediate measures to correct the
nephron, and hypokalemia.12 Additionally, sympa- alkalemia (within hours) should be used.
thetic overactivity is common in decompensated CHF, The first step in the general management of meta-
and increased renal adrenergic tone results in activa- bolic alkalosis is the correction of generation and
tion of the sodium/hydrogen ion exchanger in the maintenance factors (see Box 2 for a summary of
proximal tubule.13,14 available treatment options). In patients with de-
Several factors maintain metabolic alkalosis in CHF. creased effective circulating volume, appropriate re-
First, neurohormonal activation and chloride deple- placement of sodium, chloride, and potassium losses
tion maintain a state of bicarbonate avidity. Second, typically is sufficient to correct the alkalosis. In pa-
impairment of the circulation due to poor cardiac tients with CHF, who typically have expansion of
function and/or overdiuresis leads to further activa-
tion of these neurohormonal pathways and decreases
glomerular filtration rate, which limits the ability to Box 2. Summary of Available Treatment Options for
excrete bicarbonate. Third, the potassium depletion Metabolic Alkalosis
that often accompanies diuretic therapy further adds ● Correction of underlying precipitating and maintaining factors
to the maintenance of alkalosis through stimulation of (ie, “general measures”)
〫 Replace sodium, chloride, potassium deficits
hydrogen ion/potassium exchange through the respon-
〫 Normalize extracellular fluid volume (isotonic fluids if
sible adenosine triphosphatase pump (H⫹/K⫹- volume depleted, management of circulatory failure if
ATPase), resulting in increased proton secretion.14 congestive heart failure)
Last, there may be a role for endothelin 1, an impor- ● Acetazolamide
tant regulator of proton excretion during acid loading, 〫 Use in euvolemic or hypervolemic patients who did not
respond to general measures
of which levels are increased by about 4-fold in 〫 Effective within 18-24 h
patients with CHF, leading to a net increase in urine 〫 Caution with hypokalemia, hypophosphatemia
acidification and bicarbonate retention.15-18 ● Aldosterone antagonists (spironolactone, eplerenone)
Evaluation of alkalemic patients with CHF focuses 〫 Use in volume-overloaded patients
on the degree of volume overload. Urine chloride, 〫 Slow acting (3-7 d)
〫 Survival benefit in patients with impaired left ventricular
often used as a diagnostic test in metabolic alkalo- function
sis,14 is useful to establish the status of effective 〫 Caution with hyperkalemia and overdiuresis
circulating volume. However, it has limited value to ● Hydrochloric acid
distinguish the specific cause of metabolic alkalosis in 〫 Use if life-threatening alkalemia (pH ⬎7.6)
patients with CHF for two reasons. First, it can be low 〫 Rapid effect (8-12 h); allows close titration
〫 Requires central venous access; caution with hyperkale-
in both volume-depleted and volume-overloaded pa- mia
tients because both groups are characterized by de- 〫 Lack of immediate availability may limit its utility
creased effective circulating volume and decreased ● Renal replacement therapy (standard hemodialysis or con-
kidney perfusion. Second, if a diuretic dose was tinuous venovenous renal replacement modalities)
administered recently, urine chloride excretion could 〫 Alternative for severe alkalemia
〫 Action is quick (4-12 h depending on modality); precise
be high despite contraction of the effective circulating titration
volume. 〫 Standard hemodialysis is limited by need to maintain
Metabolic alkalosis merits therapy due to its asso- dialysate bicarbonate levels ⬃20-24 mEq/L in dialysis
ciation with a series of potential complications (Box machines
1).19,20 Unfortunately, the strength of the clinical 〫 Typically restricted to patients with another indication for
renal replacement
evidence to support targets for intervention is low.
824 Am J Kidney Dis. 2013;61(5):822-827
Metabolic Alkalosis in CHF
extracellular fluid volume, other measures may be calculated according to the estimated target bicarbon-
necessary. ate level to be reached, using 50% of body weight as
Sodium repletion in the form of isotonic saline the presumed bicarbonate space. Thus, if one desires
solution is important because it expands extracellular to see a decrease in serum bicarbonate level of 10
volume, shuts down renin and aldosterone production, mEq/L (eg, from 50 to 40 mEq/L) in a 70-kg patient,
increases glomerular filtration rate, and replaces the the estimated bicarbonate excess to be titrated is 350
chloride deficit. Chloride repletion can correct alkal- mEq (70 kg ⫻ 0.5 ⫻ 10 mEq).19 The infusion should
emia even in the absence of restoration of extracellu- not be faster than 0.2 mEq of hydrogen per 1 kg of
lar fluid volume.21 Moreover, repletion of extracellu- body weight per hour; thus, most infusions will be
lar fluid volume without correction of the chloride designed to correct the process over 8-24 hours.
deficit is not always enough to resolve metabolic Serum chemistry test and arterial blood gas analysis
alkalosis.22-24 Recent evidence links chloride reple- results should be monitored every 1-2 hours because
tion with bicarbonate secretion by B-type intercalated the initial calculation provides only a general target,
cells in the cortical collecting duct, an effect that is but can be adjusted according to the observed changes
mediated by increased activity of pendrin, a chloride- during close follow-up. Although treatment with hy-
bicarbonate exchanger.25 drochloric acid is reported as safe in most case se-
Potassium repletion also is essential, especially ries,27-29 the risk related to its corrosive properties
because it is a frequent accompaniment in metabolic still exists, and we are reminded of severe conse-
alkalosis, a factor in its maintenance, and, when quences, such as nonhealing wounds that sometimes
severe, an important mediator of the adverse conse- are fatal.30 Because of these risks and because hydro-
quences of metabolic alkalosis. However, similar to chloric acid seldom is needed, many hospitals no
volume expansion, potassium repletion needs to be longer carry it in their pharmacy cache. Potassium
accompanied by chloride repletion, as in potassium levels should be monitored closely because hyperkale-
chloride salts, to effectively correct the alkalosis.23 mia may result from changes in pH when hydrochlo-
In patients who remain alkalemic despite correction ric acid is infused. Ammonium chloride, a precursor
of underlying factors, other treatments may be re- of hydrochloric acid, seldom is used now given the
quired. Further intervention is indicated in patients risks of hyperkalemia in patients with decreased kid-
who have severe alkalemia (arbitrarily, pH ⬎7.55); ney function or encephalopathy in those with liver
those with extensive comorbid conditions, including disease.19
heart disease or organic brain disease (stroke and An alternative approach for rapid correction of
dementia) who may not be able to tolerate the effects alkalemia is dialysis with low (or zero) bicarbonate
of alkalemia; those in whom rapid correction of alkal- bath.31,32 However, given the limitation of most con-
emia is required, such as patients undergoing mechani- ventional dialysis machines to reduce dialysate bicar-
cal ventilation who remain agitated with large minute bonate concentration to a minimum of 20-25 mEq/L,
volumes leading to mixed metabolic and respiratory this often is insufficient to correct patients with severe
alkalosis; or patients already showing some of the alkalemia, although dialysate bicarbonate concentra-
manifestations listed in Box 1, such as arrhythmias, tions as high as 30 mEq/L may suffice in some
myocardial ischemia, or seizures. In these patients, patients.33 Therefore, continuous renal replacement
the carbonic anhydrase inhibitor acetazolamide is the therapy (CRRT; continuous venovenous hemofiltra-
first choice of most clinicians. IV acetazolamide (250 tion, hemodialysis, or hemodiafiltration) with fluid
mg every 6 hours for 24 hours or as a single dose of replacement without bicarbonate often is necessary.
500 mg) effectively decreases serum bicarbonate lev- We are anecdotally aware of the use of CRRT for the
els within 12-24 hours in critically ill alkalemic pa- treatment of metabolic alkalosis, but were unable to
tients.26 However, hypokalemia is a major concern find reports in the literature. Alternatively, we know
that needs to be monitored closely. Patients who are that metabolic alkalosis is well documented as a
hypokalemic before its use should be corrected pre- complication of continuous replacement modalities
emptively. when citrate is used for anticoagulation.34 Experience
If immediate correction of alkalemia is required, in this setting shows that decreased blood flow (lower
the most predictable and effective therapy is hydrochlo- clearance) or decreased bicarbonate content of the
ric acid infusion (0.1N or 0.2N hydrochloric acid, ie, replacement fluid can correct the alkalosis.34,35 There-
100-200 mEq of hydrogen per liter of solution).19 fore, it is plausible to use CRRT to treat metabolic
Hydrochloric acid can be diluted in saline solution or alkalosis, but given the need for catheter insertion and
5% dextrose solution and should be administered specialized dialysis care, it is our opinion that dialysis
through a central venous catheter to avoid local caus- primarily is suited for patients in whom metabolic
tic complications. Its infusion volume and rate are alkalosis occurs in the setting of severe decreased
Am J Kidney Dis. 2013;61(5):822-827 825
Peixoto and Alpern
kidney function (acute or chronic) or possibly patients Box 3. Teaching Points: Treatment of Metabolic Alkalosis
with refractory volume overload due to CHF. 1. Metabolic alkalosis is a common complication in patients
As it pertains to alkalemic patients with CHF, manage- with congestive heart failure receiving diuretics
ment starts with correction of volume overload by effec- 2. This acid-base disturbance when severe can cause adverse
effects on cellular function and contribute to increased
tive diuresis, with or without the concomitant use of mortality
afterload-reducing and/or inotropic agents. These thera- 3. Treatment to normalize acid-base abnormalities is indicated
pies may have implications for metabolic alkalosis. In 4. Correction of chloride depletion and normalization of extra-
the long-term management of CHF accompanied by cellular fluid volume are essential to the correction of
impaired systolic function, use of renin-angiotensin metabolic alkalosis
5. Acetazolamide and aldosterone antagonists are useful to
blockade, -blockers, and/or aldosterone antagonists is correct metabolic alkalosis in volume-overloaded patients
essential as a means of improving overall prognosis.36 6. In patients with severe metabolic alkalosis, hydrochloric acid
These drugs result in decreased proton secretion,37,38 or dialysis may be necessary for rapid correction of alkalemia
therefore exerting potentially salutary effects on acid-
base balance, although these have not been demon-
of a method that includes dialysis (either CRRT or
strated in patients with metabolic alkalosis. Although the
standard hemodialysis) may be indicated because it
role of endothelin 1 on acid handling is clear, its rel-
will help correct the alkalosis through bicarbonate
evance to therapy of CHF is not yet defined and cannot
removal. Evidence for or against the merit of this
be advocated at this time.39-41
approach has not appeared in the literature.
Loop diuretics are required in most patients with
In summary, mixed respiratory and metabolic alka-
CHF. As discussed, these drugs are associated with
losis is a common complication of CHF. The meta-
metabolic alkalosis, a risk that is enhanced further
bolic component is rooted primarily on the use of
when a thiazide-type diuretic is used to enhance
diuretics and amplified by activation of neurohor-
natriuresis in patients who remain volume overloaded
monal systems (renin-angiotensin-aldosterone sys-
after use of a loop diuretic. A more effective approach
tem, catecholamines, and endothelin). Treatment of
in such patients is to add a potassium-sparing diuretic,
the alkalosis includes the appropriate management of
particularly an aldosterone antagonist (spironolactone
circulatory failure and the judicious combination of a
or eplerenone). This approach has two benefits: first,
loop diuretic with an aldosterone antagonist. Key
aldosterone antagonists result in decreased risk of
teaching points are listed in Box 3.
death and hospitalization in patients with CHF and
impaired systolic function,42-44 and second, they an- ACKNOWLEDGEMENTS
tagonize the effects of aldosterone in the distal nephron
Support: This work was supported with resources and use of
and thereby allow potassium to be retained and bicar- facilities at the VA Connecticut Health Care System, West Haven,
bonate to be excreted,37,38 two factors that contribute CT (Dr Peixoto).
to the resolution of alkalosis. Amiloride or triamterene Financial Disclosure: The authors declare that they have no
also may be effective with similar acid-base effects,45 relevant financial interests.
but because their impact on outcomes in CHF has not
REFERENCES
been formally demonstrated, they should be used as
1. Gennari FJ, Hussain-Khan S, Segal A. An unusual case of
second-line choices in patients with impaired systolic
metabolic alkalosis: a window into the pathophysiology and diag-
function. Hyperkalemia is obviously a concern with nosis of this common acid-base disturbance. Am J Kidney Dis.
the use of aldosterone antagonists and eNaC (epithe- 2010;55(6):1130-1135.
lial Na⫹ channel)-blockers; thus, close monitoring is 2. Frangiosa A, De Santo LS, Anastasio P, De Santo NG. Acid-
necessary during therapy. base balance in heart failure. J Nephrol. 2006;19(suppl 9):S115-S120.
3. Elisaf MS, Siamopoulos KC. Acid-base and electrolyte abnor-
In patients who remain volume overloaded and mailties in patients with congestive heart failure. Exp Clin Cardiol.
alkalemic despite the mentioned approach, one can 1997;2:140-144.
resort to acetazolamide,46 hydrochloric acid, or dialy- 4. Milionis HJ, Elisaf MS. Metabolic alkalosis in patients with
sis, as discussed. Additionally, ultrafiltration (without renal failure. Nephrol Dial Transplant. 2004;19(7):1932; author
dialysis) has been used to treat acute decompensated reply 1932-1933.
5. Riggio G, Clemente R. Modificazioni dell’equilibrio acido-
CHF, with preliminary results indicating fewer epi- base nello scompenso cardiovascolare. Miner Cardioangiol. 1969;
sodes of rehospitalization during follow-up compared 17:591-595.
with aggressive diuretic therapy.47,48 It currently is 6. Squires RD, Singer RB, Moffitt GR Jr, Elkinton JR. The
recommended for patients who are refractory to di- distribution of body fluids in congestive heart failure. II. Abnormali-
uretic therapy.48 The comparative effects on acid-base ties in serum electrolyte concentration and in acid-base equilib-
rium. Circulation. 1951;4(5):697-705.
status have not been reported to our knowledge. Many 7. Frangiosa A, De Santo LS, De Santo NG, et al. Acid-base
clinicians believe that in alkalemic patients with CHF state in patients after cardiac transplantation. Am J Nephrol.
who need ultrafiltration for volume management, use 2002;22(4):332-337.
826 Am J Kidney Dis. 2013;61(5):822-827
Metabolic Alkalosis in CHF
8. Awamura M. Clinical studies on the acid-base balance distur- 31. Leblanc M, Farah A. Severe metabolic alkalosis corrected
bance in congestive heart failure. Jpn Circ J. 1969;33(3):275-291. by hemodialysis. Clin Nephrol. 1997;48(1):65.
9. Kratky V, Bartonova J, Hrdina R. Nektere metabolicke a 32. Gerhardt RE, Koethe JD, Glickman JD, Ntoso KA, Hugo
acidobazicke zmeny pri intenzvini diureticke lecbe srdecni sla- JP, Wolf CJ. Acid dialysate correction of metabolic alkalosis in
bosti. Vnitr Lek. 1990;36(4):330-341. renal failure. Am J Kidney Dis. 1995;25(2):343-345.
10. Wilson RF, Gibson D, Percinel AK, et al. Severe alkalosis 33. Huber L, Gennari FJ. Severe metabolic alkalosis in a
in critically ill surgical patients. Arch Surg. 1972;105(2):197-203. hemodialysis patient. Am J Kidney Dis. 2011;58(1):144-149.
11. Anderson LE, Henrich WL. Alkalemia-associated morbid- 34. Kindgen-Milles D, Amman J, Kleinekofort W, Morgera S.
ity and mortality in medical and surgical patients. South Med J. Treatment of metabolic alkalosis during continuous renal replace-
1987;80(6):729-733. ment therapy with regional citrate anticoagulation. Int J Artif
12. Chan YL. Adrenergic control of bicarbonate absorption in Organs. 2008;31(4):363-366.
the proximal convoluted tubule of the rat kidney. Pflugers Arch. 35. Fall P, Szerlip HM. Continuous renal replacement therapy:
1980;388(2):159-164. cause and treatment of electrolyte complications. Semin Dial.
13. Nord EP, Howard MJ, Hafezi A, Moradeshagi P, Vaystub S, Insel
2010;23(6):581-585.
PA.Alpha 2 adrenergic agonists stimulate Na⫹-H⫹ antiport activity in the
36. Jessup M, Abraham WT, Casey DE, et al. 2009 Focused
rabbit renal proximal tubule. J Clin Invest. 1987;80(6):1755-1762.
update: ACCF/AHA Guidelines for the Diagnosis and Manage-
14. Laski ME, Sabatini S. Metabolic alkalosis, bedside and
ment of Heart Failure in Adults: a report of the American College
bench. Semin Nephrol. 2006;26(6):404-421.
of Cardiology Foundation/American Heart Association Task Force
15. Braunwald E. Biomarkers in heart failure. N Engl J Med.
2008;358(20):2148-2159. on Practice Guidelines: developed in collaboration with the Inter-
16. Nohria A, Creager MA. The peripheral circulation in heart failure. national Society for Heart and Lung Transplantation. Circulation.
In: Hosenpud JD, Greenberg BH, eds. Congestive Heart Failure. 3rd ed. 2009;119(14):1977-2016.
Philadephia, PA: Lippincott Williams & Wilkins; 2007:226-242. 37. Hulter HN, Bonner EL Jr, Glynn RD, Sebastian A. Renal
17. Parker JD, Thiessen JJ. Increased endothelin-1 production and systemic acid-base effects of chronic spironolactone adminis-
in patients with chronic heart failure. Am J Physiol Heart Circ tration. Am J Physiol. 1981;240(5):F381-F387.
Physiol. 2004;286(3):H1141-H1145. 38. Henger A, Tutt P, Riesen WF, Hulter HN, Krapf R. Acid-
18. Wesson DE. Regulation of kidney acid excretion by endo- base and endocrine effects of aldosterone and angiotensin II
thelins. Kidney Int. 2006;70(12):2066-2073. inhibition in metabolic acidosis in human patients. J Lab Clin Med.
19. Adrogue HJ, Madias NE. Management of life-threatening 2000;136(5):379-389.
acid-base disorders. Second of two parts. N Engl J Med. 1998; 39. McMurray JJ, Teerlink JR, Cotter G, et al. Effects of
338(2):107-111. tezosentan on symptoms and clinical outcomes in patients with
20. Galla JH. Metabolic alkalosis. In: DuBose TG, Hamm LL, acute heart failure: the VERITAS randomized controlled trials.
eds. Acid-Base and Electrolyte Disorders. Philadelphia, PA: Saun- JAMA. 2007;298(17):2009-2019.
ders; 2002:109-128. 40. Rehsia NS, Dhalla NS. Potential of endothelin-1 and vaso-
21. Galla JH, Bonduris DN, Luke RG. Correction of acute pressin antagonists for the treatment of congestive heart failure.
chloride-depletion alkalosis in the rat without volume expansion. Heart Fail Rev. 2010;15(1):85-101.
Am J Physiol. 1983;244(2):F217-F221. 41. Anand I, McMurray J, Cohn JN, et al. Long-term effects of
22. Galla JH, Bonduris DN, Luke RG. Effects of chloride and darusentan on left-ventricular remodelling and clinical outcomes
extracellular fluid volume on bicarbonate reabsorption along the in the EndothelinA Receptor Antagonist Trial in Heart Failure
nephron in metabolic alkalosis in the rat. Reassessment of the (EARTH): randomised, double-blind, placebo-controlled trial. Lan-
classical hypothesis of the pathogenesis of metabolic alkalosis. cet. 2004;364(9431):347-354.
J Clin Invest. 1987;80(1):41-50. 42. Zannad F, McMurray JJ, Krum H, et al. Eplerenone in
23. Rosen RA, Julian BA, Dubovsky EV, Galla JH, Luke RG. patients with systolic heart failure and mild symptoms. N Engl
On the mechanism by which chloride corrects metabolic alkalosis J Med. 2011;364(1):11-21.
in man. Am J Med. 1988;84(3, pt 1):449-458. 43. Pitt B, Remme W, Zannad F, et al. Eplerenone, a selective
24. Warms PC, Michelis MF, Singh H, Fusco RD, Eichenholz aldosterone blocker, in patients with left ventricular dysfunction after
A, Davis BB. Effect of hyperoncotic solutions on electrolyte
myocardial infarction. N Engl J Med. 2003;348(14):1309-1321.
excretion in metabolic alkalosis. Metabolism. 1974;23(5):417-423.
44. Pitt B, Zannad F, Remme WJ, et al. The effect of spironolac-
25. Luke RG, Galla JH. It is chloride depletion alkalosis, not
tone on morbidity and mortality in patients with severe heart
contraction alkalosis. J Am Soc Nephrol. 2012;23(2):204-207.
failure. Randomized Aldactone Evaluation Study Investigators.
26. Mazur JE, Devlin JW, Peters MJ, Jankowski MA, Iannuzzi
N Engl J Med. 1999;341(10):709-717.
MC, Zarowitz BJ. Single versus multiple doses of acetazolamide
for metabolic alkalosis in critically ill medical patients: a random- 45. Schlueter W, Keilani T, Hizon M, Kaplan B, Batlle DC. On
ized, double-blind trial. Crit Care Med. 1999;27(7):1257-1261. the mechanism of impaired distal acidification in hyperkalemic
27. Wagner CW, Nesbit RR Jr, Mansberger AR Jr. Treatment of renal tubular acidosis: evaluation with amiloride and bumetanide.
metabolic alkalosis with intravenous hydrochloric acid. South Med J Am Soc Nephrol. 1992;3(4):953-964.
J. 1979;72(10):1241-1245. 46. Knauf H, Mutschler E. Sequential nephron blockade breaks
28. Kwun KB, Boucherit T, Wong J, Richards Y, Bryan-Brown resistance to diuretics in edematous states. J Cardiovasc Pharma-
CW. Treatment of metabolic alkalosis with intravenous infusion of col. 1997;29(3):367-372.
concentrated hydrochloric acid. Am J Surg. 1983;146(3):328-330. 47. Costanzo MR, Guglin ME, Saltzberg MT, et al. Ultrafiltra-
29. Brimioulle S, Berre J, Dufaye P, Vincent JL, Degaute JP, Kahn RJ. tion versus intravenous diuretics for patients hospitalized for acute
Hydrochloric acid infusion for treatment of metabolic alkalosis associated decompensated heart failure. J Am Coll Cardiol. 2007;49(6):675-
with respiratory acidosis. Crit Care Med. 1989;17(3):232-236. 683.
30. Buchanan IB, Campbell BT, Peck MD, Cairns BA. Chest 48. Costanzo MR, Cozzolino M, Aspromonte N, Mistrorigo F,
wall necrosis and death secondary to hydrochloric acid infusion for Valle R, Ronco C. Extracorporeal ultrafiltration in heart failure and
metabolic alkalosis. South Med J. 2005;98(8):822-824. cardio-renal syndromes. Semin Nephrol. 2012;32(1):100-111.
Am J Kidney Dis. 2013;61(5):822-827 827
You might also like
- Updated List of All PLAB 2 StationsDocument9 pagesUpdated List of All PLAB 2 StationsDr-Arif Rehman100% (1)
- Acute Renal Failure Complicated by Multiple Bee Stings: A Case Report and Literature ReviewDocument3 pagesAcute Renal Failure Complicated by Multiple Bee Stings: A Case Report and Literature ReviewHafizah FzNo ratings yet
- AcuteLiverFailureUpdate201journalformat1 PDFDocument26 pagesAcuteLiverFailureUpdate201journalformat1 PDFDewanggaWahyuPrajaNo ratings yet
- AcuteLiverFailureUpdate201journalformat1 2 PDFDocument26 pagesAcuteLiverFailureUpdate201journalformat1 2 PDFHuy HuynhNo ratings yet
- Hypokalemic Periodic Paralysis A Case ReportDocument2 pagesHypokalemic Periodic Paralysis A Case ReportEditor IJTSRDNo ratings yet
- Fígado Acute Liver FailureDocument6 pagesFígado Acute Liver FailureEdson MarquesNo ratings yet
- A Physiologic-Based Approach To The Treatment of A Patient With HypokalemiaDocument6 pagesA Physiologic-Based Approach To The Treatment of A Patient With HypokalemiaPablo IgnacioNo ratings yet
- Hypokalaemia Periodic Paralysis: Liam J StapletonDocument4 pagesHypokalaemia Periodic Paralysis: Liam J StapletonJL DeomampoNo ratings yet
- Overview of Management of Acute Renal Failure andDocument6 pagesOverview of Management of Acute Renal Failure andParhimpunan NasutionNo ratings yet
- Approach To Treatment of Hypophosphatemia: Acid-Base and Electrolyte Teaching CaseDocument7 pagesApproach To Treatment of Hypophosphatemia: Acid-Base and Electrolyte Teaching CasemasranraisaNo ratings yet
- Hypokalemic Paralysis PDFDocument7 pagesHypokalemic Paralysis PDFFanny SimaNo ratings yet
- Furosemide in The Long-Term Management of Heart Failure: The Good, The Bad, and The UncertainDocument3 pagesFurosemide in The Long-Term Management of Heart Failure: The Good, The Bad, and The UncertainFauzan AprnNo ratings yet
- A Case Report of An Unusual Complication of Amanita Phalloides PoisoningDocument3 pagesA Case Report of An Unusual Complication of Amanita Phalloides PoisoningArmando BetancourthNo ratings yet
- Lectura Recomendada HiperkalemiaDocument7 pagesLectura Recomendada HiperkalemianeomaosNo ratings yet
- Hyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDocument8 pagesHyperkalemia Management in The Emergency Department: An Expert Panel ConsensusDaniel HeSaNo ratings yet
- Hiperkalemia en ERDocument8 pagesHiperkalemia en ERmjbb1310No ratings yet
- Weissbach 2010Document2 pagesWeissbach 2010VALERIA VARGAS LOZANONo ratings yet
- Acute Liver FailureDocument46 pagesAcute Liver FailureDoc On CallNo ratings yet
- Hepatic Encephalopathy: Diagnosis and Management: Piero AmodioDocument10 pagesHepatic Encephalopathy: Diagnosis and Management: Piero AmodioMarcel DocNo ratings yet
- Ala 2019Document4 pagesAla 2019Timea SzuszerNo ratings yet
- Acute Liver Failure: Concise ReviewDocument8 pagesAcute Liver Failure: Concise ReviewJoseph Stans KasiryeNo ratings yet
- 10 1 1 622 7158 PDFDocument8 pages10 1 1 622 7158 PDFz31nNo ratings yet
- Conundrum in An Asthma Exacerbation: BMJ Case Reports May 2016Document5 pagesConundrum in An Asthma Exacerbation: BMJ Case Reports May 2016Jamaica Malunes ManuelNo ratings yet
- 469 FullDocument7 pages469 FullCristina Adriana PopaNo ratings yet
- Neuro4Nurses: Syndrome of Inappropriate Release of Antidiuretic HormoneDocument2 pagesNeuro4Nurses: Syndrome of Inappropriate Release of Antidiuretic HormoneM Zainun IrsyadNo ratings yet
- Weakness Following Diarrhea: 1/4: 1. What Can Be The Cause of Her Condition?Document4 pagesWeakness Following Diarrhea: 1/4: 1. What Can Be The Cause of Her Condition?ZauzaNo ratings yet
- Tebak AjaDocument3 pagesTebak AjaSanti P TambunanNo ratings yet
- Management of Acute Liver Failure: A. Initial Evaluation and TriageDocument3 pagesManagement of Acute Liver Failure: A. Initial Evaluation and TriagePande Indra PremanaNo ratings yet
- Falla HepaticaDocument24 pagesFalla HepaticaCbrera ValentinaNo ratings yet
- How Dangerous Is Hyperkalemia?Document11 pagesHow Dangerous Is Hyperkalemia?Erika SalazarNo ratings yet
- 13no2 3Document5 pages13no2 3Wisnu WardanaNo ratings yet
- Arritmias X HipercalemiaDocument9 pagesArritmias X Hipercalemiafh2301lrNo ratings yet
- Acute Liver Injury and FailureDocument14 pagesAcute Liver Injury and FailureWeslei ChaconNo ratings yet
- Anuria Oliguria: A Review RatesDocument7 pagesAnuria Oliguria: A Review Ratessurya rajNo ratings yet
- Criticallyillpatientswith End-Stageliverdisease: Sara CragerDocument17 pagesCriticallyillpatientswith End-Stageliverdisease: Sara CragerHima OmerNo ratings yet
- Case ScenarioDocument9 pagesCase ScenarioKM DelantarNo ratings yet
- Extracorporeal Liver Assist Device To Exchange Albumin and Remove Endotoxin in Acute Liver Failure: Results of A Pivotal Pre-Clinical StudyDocument9 pagesExtracorporeal Liver Assist Device To Exchange Albumin and Remove Endotoxin in Acute Liver Failure: Results of A Pivotal Pre-Clinical StudyIwan Budianto HadiNo ratings yet
- I Am Sharing 'Case Study NCM 118' With YouDocument6 pagesI Am Sharing 'Case Study NCM 118' With YouQusai BassamNo ratings yet
- 9 Case Report-HyponatremiaDocument2 pages9 Case Report-HyponatremiaKamal Kumar Kamal KumarNo ratings yet
- Management of Acute Liver Failure in The Intensive Care Unit SettingDocument6 pagesManagement of Acute Liver Failure in The Intensive Care Unit SettingCristian CollazosNo ratings yet
- Article - Liver Dysfunction in SepsisDocument6 pagesArticle - Liver Dysfunction in Sepsisthys2000No ratings yet
- Case Report Hyperthyroid-Acute LiverDocument5 pagesCase Report Hyperthyroid-Acute Liverpratiwi saputriNo ratings yet
- Anti Hepatic FailureDocument4 pagesAnti Hepatic Failuregoyabeb59No ratings yet
- GH 05 647Document10 pagesGH 05 647Ema Emanuela SarcaNo ratings yet
- Shah 2019Document2 pagesShah 2019khadidja BOUTOUILNo ratings yet
- R Falla Hepatica 16 GuiasDocument35 pagesR Falla Hepatica 16 GuiasRICARDO BOSSANo ratings yet
- Asidosis Laktat 2Document10 pagesAsidosis Laktat 2MizanMaulanaNo ratings yet
- Dysnatremia in The ICU: Milap Pokaharel and Clay A. BlockDocument13 pagesDysnatremia in The ICU: Milap Pokaharel and Clay A. BlockJonathan Gustavo MenaNo ratings yet
- Arterial Ammonia and Clinical Risk Factors For Encephalopathy and Intracranial Hypertension in Acute Liver FailureDocument9 pagesArterial Ammonia and Clinical Risk Factors For Encephalopathy and Intracranial Hypertension in Acute Liver FailureChannesya TanNo ratings yet
- Ac 1Document12 pagesAc 1Alamsyah TegarNo ratings yet
- Falla CardiacaDocument6 pagesFalla CardiacaFelipeNo ratings yet
- Systemic AmiloidosisDocument4 pagesSystemic AmiloidosisioannesturrisoricisNo ratings yet
- Seizures, Antiepileptic Drugs, and CKD: in PracticeDocument12 pagesSeizures, Antiepileptic Drugs, and CKD: in Practicefais123No ratings yet
- Seizures, Antiepileptic Drugs, and CKDDocument12 pagesSeizures, Antiepileptic Drugs, and CKDRudeus GreyratNo ratings yet
- Chapter 5: Electrolyte and Acid - Base Disorders in MalignancyDocument7 pagesChapter 5: Electrolyte and Acid - Base Disorders in MalignancyPratita Jati PermatasariNo ratings yet
- Electrolyte Disorders: Camiron L. Pfennig and Corey M. SlovisDocument18 pagesElectrolyte Disorders: Camiron L. Pfennig and Corey M. SlovisMutianbllNo ratings yet
- Case HipotiroidDocument3 pagesCase HipotiroidVivi DeviyanaNo ratings yet
- 403 Bargman FINALDocument5 pages403 Bargman FINALTiago Francisco Meleiro ZubioloNo ratings yet
- ALF 418RLE Group1Document21 pagesALF 418RLE Group1PAOLA LUZ CRUZNo ratings yet
- The Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?From EverandThe Spectrum of Amniotic Fluid Embolism: Is Intralipid the solution ?No ratings yet
- 17 - 3510 - DR Batool Butt - DoneDocument6 pages17 - 3510 - DR Batool Butt - DoneUsama Bin ZubairNo ratings yet
- Bacterial MeningitisDocument51 pagesBacterial MeningitiscaseinrenninNo ratings yet
- اخطاء انكسار 4Document4 pagesاخطاء انكسار 4Hassan AljaberiNo ratings yet
- SOME MCQ'S, CLASS OF 2020Document10 pagesSOME MCQ'S, CLASS OF 2020BISMARCK BANAHENE BOAHENENo ratings yet
- Amina Rizvon Finalfamous PersonDocument7 pagesAmina Rizvon Finalfamous Personapi-664229394No ratings yet
- 6 Thrombosis MorphologyDocument20 pages6 Thrombosis MorphologySawera RaheemNo ratings yet
- Controversies in The Management of Functional Constipation in ChildrenDocument8 pagesControversies in The Management of Functional Constipation in ChildrenDaniela Rodríguez MartínezNo ratings yet
- A Case of Fatal Multi-Organ Inflammation Following COVID-19 VaccinationDocument4 pagesA Case of Fatal Multi-Organ Inflammation Following COVID-19 VaccinationAmarpreet Singh MalhanNo ratings yet
- Luttik Et Al-2007-European Journal of Heart FailureDocument7 pagesLuttik Et Al-2007-European Journal of Heart FailureSiti lestarinurhamidahNo ratings yet
- Meropenem - Drug Information - UpToDate-3Document8 pagesMeropenem - Drug Information - UpToDate-3Vh TRNo ratings yet
- Ma 2021 Uveitis 101Document5 pagesMa 2021 Uveitis 101Jenny MaNo ratings yet
- Sign, Sypmtoms and Tretment of PosioningDocument18 pagesSign, Sypmtoms and Tretment of PosioningmaryamNo ratings yet
- Preeclampsia 2022Document16 pagesPreeclampsia 2022Jose DuranNo ratings yet
- A Detailed Lesson Plan in Living ThingsDocument23 pagesA Detailed Lesson Plan in Living ThingsclarisseNo ratings yet
- Bacterionomicon Digital PDFDocument77 pagesBacterionomicon Digital PDFMichelle LindsayNo ratings yet
- Besant Hypnotism and Mesmerism 1935Document86 pagesBesant Hypnotism and Mesmerism 1935Abdul Hakeem100% (1)
- PEDIA 1 The Pediatric History and Physical Exam HandoutDocument16 pagesPEDIA 1 The Pediatric History and Physical Exam HandoutRyan Loyd MarquezNo ratings yet
- Acupuncture Points ChartDocument9 pagesAcupuncture Points ChartAnnaNo ratings yet
- Research Proposal Paper - Ian GraffDocument5 pagesResearch Proposal Paper - Ian Graffapi-614243581No ratings yet
- ADHD Dari KaplanDocument25 pagesADHD Dari KaplanAldo D'vatho MpNo ratings yet
- A-Level Psychology - Mock Test 1 1Document4 pagesA-Level Psychology - Mock Test 1 1Kristen LeNo ratings yet
- Behavioral Variant Frontotemporal DementiaDocument24 pagesBehavioral Variant Frontotemporal DementiaADRIANA MARCELA YARA DUARTENo ratings yet
- IPD A Cardiovascular System Bates and and VideoDocument10 pagesIPD A Cardiovascular System Bates and and Videostar220498No ratings yet
- 2 5406729617908171096 PDFDocument506 pages2 5406729617908171096 PDFKamal Jauoda100% (1)
- Surgical Management of Head and Neck RDDDocument6 pagesSurgical Management of Head and Neck RDDDevy OctaviaNo ratings yet
- Immunity WorksheetDocument4 pagesImmunity WorksheetShahd MohamedNo ratings yet
- Anemia Table283Document2 pagesAnemia Table283Bridget ParkerNo ratings yet
- Nursing Care Plan: FeverDocument1 pageNursing Care Plan: FeverOlive Claire T. ManlambusNo ratings yet
- Woc Acute Pancreatitis EngDocument10 pagesWoc Acute Pancreatitis EngMuhammad Alvin Fuzail IyazNo ratings yet