Professional Documents
Culture Documents
1 s2.0 S0735109716308580 Main
1 s2.0 S0735109716308580 Main
Uploaded by
Muhammad LutfiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1 s2.0 S0735109716308580 Main
1 s2.0 S0735109716308580 Main
Uploaded by
Muhammad LutfiCopyright:
Available Formats
857
JACC April 5, 2016
Volume 67, Issue 13
Arrhythmias and Clinical EP
IMPLANTABLE DEFIBRILATOR MANAGEMENT NEAR THE END OF LIFE: DO PATIENTS KNOW
ENOUGHT TO DECIDE?
Poster Contributions
Poster Area, South Hall A1
Monday, April 04, 2016, 9:45 a.m.-10:30 a.m.
Session Title: Clinical Care of Patients With Implanted Devices
Abstract Category: 18. Arrhythmias and Clinical EP: Devices
Presentation Number: 1266-324
Authors: Silvia del Castillo, Miguel Angel Arias, Roger Villuendas, Marta Pachon, Alberto Puchol, Damia Pereferrer, Alejandro Curcio,
Hospital Universitario de Fuenlabrada, Madrid, Spain
Background: Management of ICD therapies in terminal patients or patients with a bad quality of life is complex. About 33% of the patients
with an ICD implanted can receive painful and stressing shocks in the last day of life if those therapies are not deactivated. Patient
autonomy is a bioethics imperative. In order to respect it, patients should be informed of the possibility and have a complete understanding
of the consequences of deactivation.
Methods: We carried out a survey among 243 consecutive adult patients (21% female) in the outpatient clinic of 3 University Hospitals.
Questions were organized in 3 fields: Motivation of the implant, Basic ICD function and shocks and, end-of-life management. Age, sex and
educational background were also registered.
Results: Patients had a high level of knowledge of the reason of the implant and a basic knowledge of their functioning (91% described
correctly the reason for implant, 86% could name the device, 66% knew that an ICD does not cure their illness and 74% that they can
have a cardiac death after the implant). Their knowledge about shocks was very variable: 64% knew shocks are painful, 78% knew that an
ICD can be programmed but 68% think that shocks are inevitable in the presence of a ventricular tachycardia. Patients were remarkably
unaware of their right to decide in end-of-life questions regarding their ICD (just 38% think they can decide to deactivate after consulting
with their doctors), and were confused about what ICD deactivation means (21% think that deactivation leads to immediate heart arrest).
Just 37% knew that ICD deactivation is ethically appropriate and recommended by the scientific societies. Surprisingly a higher level of
education did not imply a better knowledge of the patients’ rights or an understanding of the bioethical questions regarding their device
management.
Conclusions: Knowledge of ICD functions and possibility of reprogramming, especially concerning end-of-life decisions among ICD
patients must be improved in order to respect their right to autonomous decisions.
You might also like
- Critical Care Nursing A Holistic Approach 11th Edition Morton Fontaine Test Bank PDFDocument335 pagesCritical Care Nursing A Holistic Approach 11th Edition Morton Fontaine Test Bank PDFSami Atawi100% (1)
- Data Interpretation in Anesthesia 2017Document450 pagesData Interpretation in Anesthesia 2017Noni Frista Al Azhari100% (2)
- Guia de Buena Practica Autismo With Cover Page v2Document13 pagesGuia de Buena Practica Autismo With Cover Page v2Micaela Astudillo ParedesNo ratings yet
- HRT Treatment Options V9a Minor UpdateDocument2 pagesHRT Treatment Options V9a Minor Updatekarthime86No ratings yet
- Ischemic StrokeDocument103 pagesIschemic Strokebogdasus100% (1)
- 12 Strokes: A Case-based Guide to Acute Ischemic Stroke ManagementFrom Everand12 Strokes: A Case-based Guide to Acute Ischemic Stroke ManagementFerdinand K. HuiNo ratings yet
- Imaging Predictors of Procedural and Clinical OutcDocument13 pagesImaging Predictors of Procedural and Clinical OutcYusuf BrilliantNo ratings yet
- Thrombectomy Within 8 Hours After Symptom Onset in Ischemic StrokeDocument11 pagesThrombectomy Within 8 Hours After Symptom Onset in Ischemic StrokefontzzNo ratings yet
- REQUITE A Prospective Multicentre Cohort Study ofDocument9 pagesREQUITE A Prospective Multicentre Cohort Study ofAhmad ShamyNo ratings yet
- Acp 027Document13 pagesAcp 027otakualafugaNo ratings yet
- Acw 018Document11 pagesAcw 018otakualafugaNo ratings yet
- Validacion de Action Research Arm Test ARAT en PacDocument8 pagesValidacion de Action Research Arm Test ARAT en PacMauro PogliacomiNo ratings yet
- Symbol Digit NeuronormaDocument21 pagesSymbol Digit NeuronormaMarta Milián TeixidóNo ratings yet
- 2016 AoCN One-Year References RCI Sanchez-BenavidesDocument11 pages2016 AoCN One-Year References RCI Sanchez-BenavidesneuromiguelNo ratings yet
- 1-IsRS Technical Guidelines For StereotacticDocument12 pages1-IsRS Technical Guidelines For Stereotactictaharount.amel20No ratings yet
- Knowledge Regarding Role of Anaesthesia Technologists among Patients Undergoing Elective Surgery in Multispeciality Hospitals of Aurangabad MaharashtraDocument7 pagesKnowledge Regarding Role of Anaesthesia Technologists among Patients Undergoing Elective Surgery in Multispeciality Hospitals of Aurangabad MaharashtraEditor IJTSRDNo ratings yet
- Vagus Nerve Stimulation .2024Document219 pagesVagus Nerve Stimulation .2024ANTONIO ROMERONo ratings yet
- Neuronorma Digit Corsi LyN TMT SDMT Más de 50Document21 pagesNeuronorma Digit Corsi LyN TMT SDMT Más de 50julsNo ratings yet
- Stroke Nursing DissertationDocument4 pagesStroke Nursing DissertationBestCollegePaperWritingServiceCanada100% (1)
- UntitledDocument21 pagesUntitledxxxNo ratings yet
- Igrt ThesisDocument8 pagesIgrt Thesislisanetkowiczerie100% (1)
- Guía de Buena Práctica para El Diagnóstico de Los Trastornos Del Espectro AutistaDocument12 pagesGuía de Buena Práctica para El Diagnóstico de Los Trastornos Del Espectro AutistaEquipo de Orientación Liceo CastillaNo ratings yet
- Test Barcelona ArticuloDocument14 pagesTest Barcelona Articulomadalena limaNo ratings yet
- Utilizationof PCSin SwedishhospitalsDocument10 pagesUtilizationof PCSin SwedishhospitalsAlberto Jr. AndresNo ratings yet
- Dissertation Topics For MD AnaesthesiaDocument4 pagesDissertation Topics For MD AnaesthesiaWhitePaperWritingServicesCanada100% (1)
- Experimental Neurosurgery in Animal ModelsDocument261 pagesExperimental Neurosurgery in Animal ModelsgpuruenamNo ratings yet
- jamainternal_sanchis_2023_oi_230003_1681506441.53919Document9 pagesjamainternal_sanchis_2023_oi_230003_1681506441.53919Eileen AmaroNo ratings yet
- Dry Needling StrokeDocument10 pagesDry Needling StrokerizkazahratiNo ratings yet
- Basic StatisticsDocument113 pagesBasic Statisticsrajsalgyan100% (1)
- NEURONORMA ADULTOS 50 A 92 AÑOS Spans-LNS-TMT-SDMTDocument22 pagesNEURONORMA ADULTOS 50 A 92 AÑOS Spans-LNS-TMT-SDMTmaría del pinoNo ratings yet
- Acp038v1 Spans LNS TMT SDMT PDFDocument21 pagesAcp038v1 Spans LNS TMT SDMT PDFRocío G IzqNo ratings yet
- Feasibility and Efficacy of Nurse-Driven Acute Stroke CareDocument5 pagesFeasibility and Efficacy of Nurse-Driven Acute Stroke Careyenni fajriaNo ratings yet
- Asincronia en VM y MortalidadDocument9 pagesAsincronia en VM y MortalidadFreddy EcheverryNo ratings yet
- Textbook Atlas of Postsurgical Neuroradiology Imaging of The Brain Spine Head and Neck 2Nd Edition Daniel Thomas Ginat Ebook All Chapter PDFDocument63 pagesTextbook Atlas of Postsurgical Neuroradiology Imaging of The Brain Spine Head and Neck 2Nd Edition Daniel Thomas Ginat Ebook All Chapter PDFdonna.riebel227100% (19)
- Neuronorma ViejosDocument11 pagesNeuronorma ViejosDavidNo ratings yet
- @MedicalBooksStore 2017 Emergency PDFDocument103 pages@MedicalBooksStore 2017 Emergency PDFUmmu AtikahNo ratings yet
- Baremos NeuronormaDocument21 pagesBaremos NeuronormaDebbieNo ratings yet
- Norms For The Abbreviated Barcelona TestDocument14 pagesNorms For The Abbreviated Barcelona TestMel MartinNo ratings yet
- Clinical Genetics - 2023 - Saura - Spanish Mental Health Residents Perspectives About Residency Education On The GeneticsDocument8 pagesClinical Genetics - 2023 - Saura - Spanish Mental Health Residents Perspectives About Residency Education On The GeneticsJuanNo ratings yet
- Ryan Et Al 2023 Preventing Depression in Aphasia A Cluster Randomized Control Trial of The Aphasia Action SuccessDocument9 pagesRyan Et Al 2023 Preventing Depression in Aphasia A Cluster Randomized Control Trial of The Aphasia Action Success_maghus_No ratings yet
- Intensive Care To Facilitate Organ Donation. Ont-Semicyuc RecommendationsDocument9 pagesIntensive Care To Facilitate Organ Donation. Ont-Semicyuc Recommendationsjulian zuletaNo ratings yet
- Neuronorma Frontal PDFDocument21 pagesNeuronorma Frontal PDFJose Algomas KnorecuerdoNo ratings yet
- Endovascular Therapy For Ischemic Stroke With Perfusion-Imaging SelectionDocument10 pagesEndovascular Therapy For Ischemic Stroke With Perfusion-Imaging Selectioncitra dewiNo ratings yet
- Dissertation Speckle TrackingDocument4 pagesDissertation Speckle TrackingPaySomeoneToWriteAPaperForMeSingapore100% (1)
- Atlas of Anterior Segment Optical Coherence TomographyFrom EverandAtlas of Anterior Segment Optical Coherence TomographyJorge L. AlióNo ratings yet
- Acute Stroke Intervention: The Heart of The Matter: SciencedirectDocument2 pagesAcute Stroke Intervention: The Heart of The Matter: SciencedirectMarianaPlataNo ratings yet
- Anthony J Furlan MD: For The CLOSURE I Investigators Trial Sponsor: NMT Medical BostonDocument21 pagesAnthony J Furlan MD: For The CLOSURE I Investigators Trial Sponsor: NMT Medical Bostongreg1919No ratings yet
- Baremos TMTDocument21 pagesBaremos TMTAntonio J. LópezNo ratings yet
- Evelyn M. Teasdale, Susan Aitken-Multidetector CT in Neuroimaging - An Atlas and Practical Guide-Clinical Publishing Services (2009) PDFDocument146 pagesEvelyn M. Teasdale, Susan Aitken-Multidetector CT in Neuroimaging - An Atlas and Practical Guide-Clinical Publishing Services (2009) PDFcongkty1No ratings yet
- Does The Artery-First Approach Improve The Rate of R0 Resection in Pancreatoduodenectomy?Document9 pagesDoes The Artery-First Approach Improve The Rate of R0 Resection in Pancreatoduodenectomy?vmdcabanillaNo ratings yet
- Mosoiu Et Al 2023 Core Palliative Care Research Competencies Framework For Palliative Care CliniciansDocument10 pagesMosoiu Et Al 2023 Core Palliative Care Research Competencies Framework For Palliative Care CliniciansAmbaNo ratings yet
- Neurosurgery: A Case-Based Approach Christos M. Tolias Anastasios Giamouriadis Florence Rosie Avila Hogg Prajwal GhimireDocument225 pagesNeurosurgery: A Case-Based Approach Christos M. Tolias Anastasios Giamouriadis Florence Rosie Avila Hogg Prajwal GhimireMystero Rasico100% (2)
- Effects of Motor Imagery After Cerebrovascular AccidentDocument6 pagesEffects of Motor Imagery After Cerebrovascular AccidentNatalia Toledo MasíasNo ratings yet
- Central Nervous System MetastasesFrom EverandCentral Nervous System MetastasesManmeet AhluwaliaNo ratings yet
- 1 Patel2016Document6 pages1 Patel2016Brock StonNo ratings yet
- Protocolo Stars CrashDocument24 pagesProtocolo Stars CrashteranrobleswaltergabrielNo ratings yet
- Jlo and Vosp Over 49Document16 pagesJlo and Vosp Over 49xxxNo ratings yet
- Endovascular Resuscitation and Trauma Management: Bleeding and Haemodynamic ControlFrom EverandEndovascular Resuscitation and Trauma Management: Bleeding and Haemodynamic ControlTal HörerNo ratings yet
- Acp 041Document23 pagesAcp 041Sabri Lozada MonfortNo ratings yet
- CyberKnife NeuroRadiosurgery: A practical GuideFrom EverandCyberKnife NeuroRadiosurgery: A practical GuideAlfredo ContiNo ratings yet
- Atlas of Multiparametric Prostate MRI: With PI-RADS Approach and Anatomic-MRI-Pathological CorrelationFrom EverandAtlas of Multiparametric Prostate MRI: With PI-RADS Approach and Anatomic-MRI-Pathological CorrelationNo ratings yet
- The Healthy Talk b1Document4 pagesThe Healthy Talk b1Ліна КрольNo ratings yet
- Basic Education Learning Continuity Plan in The Time of COVID-19Document65 pagesBasic Education Learning Continuity Plan in The Time of COVID-19Earls jr Computer100% (1)
- 23-Staff NurseDocument40 pages23-Staff NurseVenkatesh prasadNo ratings yet
- Disability Inclusion: Topic GuideDocument54 pagesDisability Inclusion: Topic GuidesineNo ratings yet
- Assigment MicrobiologyDocument7 pagesAssigment MicrobiologyFu'e AbdumalikNo ratings yet
- Endocrown in Digital: Literature ReviewDocument6 pagesEndocrown in Digital: Literature ReviewIJAERS JOURNALNo ratings yet
- Presentation Electri in TrichologyDocument69 pagesPresentation Electri in TrichologycarmenNo ratings yet
- Hydroseeding WorkDocument26 pagesHydroseeding WorkSamsiah TolaNo ratings yet
- Checklist Male GenitaliaDocument3 pagesChecklist Male GenitaliaJessoliver GalvezNo ratings yet
- The Outcome of Ultrasound Guided Percutaneous Drainage of Liver AbscessDocument6 pagesThe Outcome of Ultrasound Guided Percutaneous Drainage of Liver AbscessIJAR JOURNALNo ratings yet
- Grade 11biology: Science of YourselfDocument60 pagesGrade 11biology: Science of YourselfDanielNo ratings yet
- Identify Hazards and Risks: By: Rosemel C. Rempillo TLE Teacher, Balogo HSDocument28 pagesIdentify Hazards and Risks: By: Rosemel C. Rempillo TLE Teacher, Balogo HSMhel Abbyzj100% (1)
- I Have Nothing - Brass - Sax TenorDocument1 pageI Have Nothing - Brass - Sax TenorMiguel Rodrigo Estrada GutierrezNo ratings yet
- Terjemahan GTDocument11 pagesTerjemahan GTALYVIA RISVIANTI PUTRI -No ratings yet
- Late Life Psychiatric DisordersDocument2 pagesLate Life Psychiatric DisordersWaheedullah AhmadiNo ratings yet
- Nanda 2021 2023Document6 pagesNanda 2021 2023Khimberly UmbaoNo ratings yet
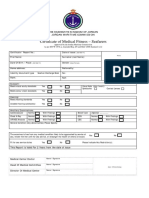
- Medical Fitness Report New For JordanDocument1 pageMedical Fitness Report New For Jordanahmad abdullahNo ratings yet
- Ijomi 15 415Document4 pagesIjomi 15 415Bagis Emre GulNo ratings yet
- M-Mode Echocardiography in DogsDocument10 pagesM-Mode Echocardiography in DogsTactvisNo ratings yet
- Lite Ls04naDocument104 pagesLite Ls04naAdrián Zigo DresingNo ratings yet
- Long ReportDocument11 pagesLong Reportapi-668179157No ratings yet
- Anatomy and Physiology: University of San Agustin Review Center Iloilo City, PhilippinesDocument74 pagesAnatomy and Physiology: University of San Agustin Review Center Iloilo City, PhilippinesChristine Joy MolinaNo ratings yet
- (D Doctor, P Patient) : Chapter 1: Molecular BiologyDocument13 pages(D Doctor, P Patient) : Chapter 1: Molecular BiologyVõ ĐứcNo ratings yet
- Unforgettable Quarantine StoryDocument1 pageUnforgettable Quarantine StoryChad Broski100% (1)
- Generic Name Indication Classification Pharmacokinetics Nursing ConsiderationDocument5 pagesGeneric Name Indication Classification Pharmacokinetics Nursing Considerationjoy rachel tabernillaNo ratings yet
- Altered Elimination LecDocument7 pagesAltered Elimination LecJean Rynne Barrameda BongaisNo ratings yet
- Test Bank For Essentials of Pediatric Nursing 2nd Edition Theresa KyleDocument37 pagesTest Bank For Essentials of Pediatric Nursing 2nd Edition Theresa Kylebiscuitunwist20bsg4100% (24)
- Week 7 - Lecture Midterm Test RevisionDocument5 pagesWeek 7 - Lecture Midterm Test RevisionhxNo ratings yet