Professional Documents
Culture Documents
A Bronchoalveolar Lavage-Driven Antimicrobial Treatment Improves Survival in Hematologic Malignancy Patients With Detected Lung Infiltrates A Prospective Multicenter Study of The SEIFEM Group
A Bronchoalveolar Lavage-Driven Antimicrobial Treatment Improves Survival in Hematologic Malignancy Patients With Detected Lung Infiltrates A Prospective Multicenter Study of The SEIFEM Group
Uploaded by
Xaralyn XaviereOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A Bronchoalveolar Lavage-Driven Antimicrobial Treatment Improves Survival in Hematologic Malignancy Patients With Detected Lung Infiltrates A Prospective Multicenter Study of The SEIFEM Group
A Bronchoalveolar Lavage-Driven Antimicrobial Treatment Improves Survival in Hematologic Malignancy Patients With Detected Lung Infiltrates A Prospective Multicenter Study of The SEIFEM Group
Uploaded by
Xaralyn XaviereCopyright:
Available Formats
A bronchoalveolar lavage-driven antimicrobial treatment improves survival in hematologic
malignancy patients with lung infiltrates detection: a prospective multicenter study of the
SEIFEM group
Francesco Marchesi,1 Chiara Cattaneo,2 Marianna Criscuolo,3 Mario Delia,4 Michelina Dargenio,5
Maria Ilaria Del Principe,6 Antonio Spadea,1 Nicola Stefano Fracchiolla,7 Lorella Melillo,8 Katia
Perruccio,9 Caterina Alati,10 Domenico Russo,11 Mariagrazia Garzia,12 Marco Brociner,13
Mariagiovanna Cefalo,14 Daniele Armiento,15 Simone Cesaro,16 Nunzia Decembrino,17 Andrea
Mengarelli,1 Mario Tumbarello,3,18 Alessandro Busca,19 and Livio Pagano3,20 on behalf of the
Sorveglianza Epidemiologica Infezioni nelle Emopatie (SEIFEM) Group
1
Hematology and Stem Cell Transplant Unit, IRCCS Regina Elena National Cancer Institute (Rome, Italy)
2
Hematology Division, ASST-Spedali Civili di Brescia (Brescia, Italy);
3
Fondazione Policlinico Universitario Agostino Gemelli - IRCCS (Roma, Italy);
4
Hematology and Bone Marrow Transplantation Unit, Department of Emergency and Organ Transplantation,
University of Bari (Bari, Italy);
5
Hematology and Stem Cell Transplantation Unit, 'Vito Fazzi' Hospital (Lecce, Italy);
6
Hematology, Department of Biomedicine e Prevention, Tor Vergata University (Rome, Italy);
7
Hematology Unit, Foundation IRCCS Ca' Granda Ospedale Maggiore Policlinico (Milan, Italy);
8
UO of Hematology, Fondazione IRCSS Casa Sollievo della Sofferenza (San Giovanni Rotondo, Italy);
9
Pediatric Hematology Oncology, Azienda Ospedaliera Universitaria, Ospedale Santa Maria della Misericordia
(Perugia, Italy);
10
Hematology Unit, Bianchi-Melacrino-Morelli Hospital (Reggio Calabria, Italy);
11
Bone Marrow Transplant Unit, University of Brescia and ASST-Spedali Civili (Brescia, Italy);
12
Hematology, San Camillo-Forlanini Hospital (Rome, Italy);
13
Division of Hematology, Foundation IRCCS Policlinico San Matteo, University of Pavia (Pavia, Italy);
14
Hematology, San Eugenio Hospital (Rome, Italy);
15
Hematology and Stem Cell Transplantation Unit, University Campus Bio-Medico (Rome, Italy);
16
Pediatric Hematology Oncology, Azienda Ospedaliera Universitaria Integrata (Verona, Italy);
17
Pediatric Hematology Oncology, IRCCS Policlinico San Matteo, University of Pavia (Pavia, Italy);
This article has been accepted for publication and undergone full peer review but has not been
through the copyediting, typesetting, pagination and proofreading process which may lead to
differences between this version and the Version of Record. Please cite this article as doi:
10.1002/ajh.25585
This article is protected by copyright. All rights reserved.
18
Istituto di Malattie Infettive, Università Cattolica del Sacro Cuore (Roma, Italy);
19
Stem Cell Transplant Center, AOU Citta' della Salute e Della Scienza (Turin, Italy);
20
Istituto di Ematologia, Università Cattolica del Sacro Cuore (Roma, Italy)
Running title: BAL in hematologic malignancies
Keywords: bronchoalveolar lavage fluid (BAL), lung infiltrate, hematologic malignancies,
antimicrobial treatment, invasive fungal disease
Corresponding author:
Francesco Marchesi, MD
Hematology and Stem Cell Transplant Unit
IRCCS Regina Elena National Cancer Institute
Via E. Chianesi, 53 00144 - Rome (Italy)
Email: francesco.marchesi@ifo.gov.it
Phone: +39 06-52665022
Fax: +39 06-52662849
This article is protected by copyright. All rights reserved.
ABSTRACT
Bronchoalveolar lavage (BAL) is recommended for diagnosing lung infiltrates (LI) in patients with
hematologic malignancy (HM). Prospective data on the impact of BAL on survival are still lacking.
We conducted a prospective observational study on patients who performed BAL for LI among
3.055 HM patients hospitalized from January to September 2018. BAL was performed in 145 out of
434 patients who developed LI at a median time of 4 days from LI detection. The median age was
60 (1-83). Most patients had an acute myeloid leukaemia/myelodisplastic syndrome (81), followed
by lymphoma (41), acute lymphoblastic leukaemia (27), and other types of HM (36). A putative
causal agent was detected in 111 cases (76%) and in 89 cases (61%) where the BAL results allowed
to guide antimicrobial treatment. We observed a significantly improved outcome of LI at day +30 in
patients who could receive a BAL-driven antimicrobial treatment (improvement/resolution rate:
71% vs 55%; P=0,04). Moreover, we observed a significantly improved outcome in 120d-OS (78%
vs 59%; P=0,009) and 120d-AM (11% vs 30%; P=0,003) for patients who could receive a BAL-
driven treatment. The multivariate analysis showed that BAL-driven antimicrobial treatment was
significantly associated with better 120d-OS and lower 120d-AM. We did not observe any severe
adverse events. In conclusion BAL allows to detect a putative agent of LI in about 75% of cases, it
resulted feasible and well tolerated in most cases, demonstrating that a BAL-driven antimicrobial
treatment allows to improve clinical outcome and survival.
This article is protected by copyright. All rights reserved.
INTRODUCTION
Detection of lung infiltrates (LI) is a relevant concern in patients with hematologic malignancy
(HM), occurring in about 12-15% of severely neutropenic patients1 and significantly affecting
survival.2-4 Moreover, infectious and less frequently non-infectious LI occur in up to 70% and 25%
of patients undergoing allogeneic hematopoietic stem cell transplant (alloSCT) and autologous
hematopoietic stem cell transplant (ASCT), respectively. Despite advances in the diagnostic yield, a
putative microbiological agent of LI remains undetected because of the low sensibility of available
non-invasive diagnostic assays. Moreover, microbiologically undiagnosed LI may reflect a deferred
diagnostic approach where clinicians prefer to adopt an empirical treatment strategy and use more
invasive approaches only in cases of persistence of fever and when there is an appearance or
worsening of respiratory distress.2 In case of LI of undefined etiology, bronchoscopy coupled with
bronchoalveolar lavage (BAL) are used to diagnose putative microbiological agents in order to
perform guided-antimicrobial therapy. This procedure is associated with a significantly lower
complication rate compared with trans-bronchial or transthoracic needle aspirate.5 In HM or allo-
SCT patients, the yield of BAL was of 15-67% before the advent of non-culture-based methods.
The yield was significantly higher when the BAL was performed early after LI detection (up to 87%
of positive results), allowing to change the on-going empirical antimicrobial treatment in about 50-
65% of patients.6-13 Nevertheless, several issues are still under debate and investigation, these
include: the diagnostic yield of BAL, the gold-standard used to properly evaluate the positive and
negative predictive value of BAL, as well as the impact of using a BAL-guided antimicrobial
strategy on clinical outcome and survival.1,14-15 Based on these considerations, we designed a
prospective multicenter study in 18 hematology institutes participating in the Sorveglianza
Epidemiologica Infezioni nelle Emopatie (SEIFEM) Group on adult and pediatric HM patients with
LI detection in order to evaluate the efficacy and the safety of BAL as well as the impact on clinical
outcome and survival of a BAL-guided antimicrobial strategy.
METHODS
Study design
This article is protected by copyright. All rights reserved.
This is a prospective observational multicenter study that was carried out in 18 hematology centers
from January 1 to September 30, 2018. Adult and pediatric severely immunocompromised patients
with HM at any phase of treatment were enrolled according to the following criteria: 1) the presence
of a host risk factor for invasive fungal disease (IFD) according to the EORTC/MSG 2008
criteria;16 2) the absence of any microbiological documentation at standard non-invasive diagnostic
work-up; 3) any fever or respiratory distress not responding to broad-spectrum antimicrobial
therapy; 4) LI detection at computed tomography (CT) scan. According to the investigators, the
patients fulfilling these criteria underwent a bronchoscopy with BAL.
The study was approved by the Ethical Committee of the coordinating center (IRCCS Regina Elena
National Cancer Institute, prot. R.S. 976/17) and by each participating institute. The study was
conducted in accordance with the Helsinki declaration and all patients signed a written informed
consent before study enrolment.
End-points
The primary study end-point was to evaluate the efficacy of BAL in identifying a putative
microbiological agent. The secondary endpoints were to evaluate the folowing: 1) the clinical
response to a BAL-driven antimicrobial treatment at day +30 from LI detection; 2) the overall
survival (OS) and attributable mortality (AM) at day +120 from LI detection; 3) the frequency of
BAL positivity for GM in patients with LI radiologically atypical for IFD; 4) the safety of BAL.
Procedures and definition
Patients experiencing a fever of unknown origin underwent empiric broad-spectrum antibiotic
treatment, according the international guidelines17-18 and the local policy. A standard diagnostic
work-up including serial blood and urine cultures, nasopharyngeal swab for respiratory viruses,
serum GM (three consecutive checks), 1,3-beta-D-glucan and CT scan was performed in those
patients who did not respond to empiric broad-spectrum antibiotic treatment and/or who presented
respiratory distress in the subsequent 48-72 hours from the onset of fever. Patients with LI were
classified according to the standard glossary of CT imaging and to the EORTC/MSG 2008 criteria,
dividing them into typical and atypical criteria.16,19 Patients experiencing fever or respiratory
distress who did not respond to broad-spectrum antibiotics and those who did not have any
This article is protected by copyright. All rights reserved.
microbiological and/or serological documentation at diagnostic work-up were eligible candidates to
perform BAL, ideally within 3-4 days from LI detection.
Demographic, hematological and microbiological data were registered in an electronic form. All
patients were evaluated for severity of their illness by the APACHE II scoring system.20 Response
to antimicrobial treatment at day +30 from LI detection was evaluated by CT scan. Resolution was
defined as the complete disappearance of radiological features in the presence of a significant
clinical improvement, whereas improvement was defined as a decrease in size of previous described
radiological features without complete disappearance. Finally, a worsening of LI was defined as an
increase in size of previously described radiological features or the appearance of new lesions,
associated with the deterioration of clinical conditions. OS was defined as the time from LI
detection to death due to any causes, whereas AM was defined as the time from LI detection to
death directly caused by lung infection. The observation time was of 120 days from LI detection.
Bronchoscopy with BAL was performed according to the standard procedures published by the MD
Anderson Cancer Center group.11 The recommended diagnostic panel on BAL included: a) bacterial
and fungal growth; b) cytologic exam; c) GM; d) multiplex PCR for respiratory bacteria (S.
pneumoniae, L. pneumophila, C. pneumoniae, M. pneumoniae, B. pertussis, B. parapertussis, H.
influenziae); e) PCR for respiratory viruses (including Cytomegalovirus); f) PCR for P. jiroveci,
adding evaluation of immunofluorescence in case of PCR-positivity to confirm diagnosis;21 g) PCR
for M. tuberculosis complex; h) PCR for Aspergillus spp. Available commercial kits were used
according to the manufacturer's instructions, with the only exception of PCR for Aspergillus spp
(homemade). A positive BAL-GM was defined as an optical density index > 0,5.22-25 CMV findings
were interpreted according to the current published guidelines.26 Acceptable adherence to the
recommended diagnostic panel was reached if the single test was performed in at least 75% of
enrolled patients.
Invasive pulmonary aspergillosis (IPA) was defined according to the EORTC/MSG 2008 criteria.16
Post-procedure adverse effects were defined and graded according to the Common Toxicity Criteria
(version 4.02).
Statistical analysis
This article is protected by copyright. All rights reserved.
The estimated sample size was approximately 150 patients and was calculated on the basis of a
previous study in which the efficacy of BAL identifying a putative agent of LI was of 65% with a
confidence interval (CI) of 58-73%.13 Even if we consider a drop-out rate of 10%, this CI would
have remained the same whether 150 patients had been enrolled into the study. Data were analyzed
by the Statistical Package of Social Sciences software (version 20, Chicago, IL, USA). Continuous
variables were compared with Student’s t-test (for normally distributed variables) or the Mann–
Whitney U-test (for non-normally distributed variables). Categorical variables were evaluated with
the two tailed Fisher’s exact test. Results are expressed as median (continuous variables) or as
percentages of the group from which they were derived (categorical variables). The two-tailed tests
were used to determine statistical significance. The OS and AM was estimated with Kaplan-Meier
method and was compared to the two-sided log-rank test. The multivariate analysis was used in
order to identify independent risk factors for survival and mortality. For this analysis, Cox
proportional hazard models were built and variables found to be significant in univariate testing
were incorporated by using a stepwise approach. The related estimates were reported as hazard
ratios (HR) and 95% CI. P-values ≤ 0,05 were considered statistically significant.
RESULTS
Epidemiological data
During the study period, a total of 3.055 patients were hospitalized in participating centers. The
underlying disease was as follows: lymphoma 861, acute myeloid leukaemia (AML) 742, myeloma
567, acute lymphoblastic leukaemia (ALL 383 patients with), chronic lymphocytic leukaemia
(CLL) 92, other HM 410 patients. CT-confirmed LI were diagnosed in 434 out of 3.055 patients
(14%). A LI was detected after a median time of 3 days after fever onset. Baseline demographic
characteristics and flow-chart of enrolled patients is shown in Table 1 and Figure 1 (panel A),
respectively. Among 434 patients with LI, 145 out of 177 (82%) patients matching the study
criteria performed BAL whereas 32 patients (18%) did not undergo the procedure for the following
reasons: clinical instability n=11, severe thrombocytopenia n=8, local clinical decision n=7, patient
refusal n=6). At the time of BAL, 58 patients (33%) were receiving glucocorticoids at the time of
This article is protected by copyright. All rights reserved.
enrolment (> 0,3 mg/Kg/day for at least 3 weeks or higher doses for less long time) with a median
administration time of 10 days. Median absolute neutrophil count (ANC) was of 0,46 x 10/9L, and
106 patients (60%) had experienced prolonged and severe neutropenia (ANC < 0,1 x 10/9L for a
median of 12 days); median platelets (PLT) count was of 40 x 109/L. Twenty-nine patients (16%)
presented severe respiratory failure (p02 < 60 mmHg) and the median APACHE II score was 16
(range: 5-27). The adherence of clinicians to the recommended diagnostic panel on BAL was
acceptable (≥ 75%) for all tests with the only exception of Aspergillus PCR, that was performed in
less than 50% of patients.
Identification of a putative microbiological agent (primary end-point)
A putative causal agent of LI was detected in 111 out of 145 patients who underwent BAL (76%).
In 41 cases, positive BAL-GM was found, 36 for bacteria, 6 for Pneumocystis and in the remaining
28 cases for respiratory viruses. In 10 cases, a mixed infection was diagnosed; no cases of
tuberculosis were detected. As shown in Figure 1, the results of BAL allowed to guide the ongoing
empiric antimicrobial therapy in 89 cases (61%) (Table 2), whereas in the remaining 56 cases (39%)
BAL did not permit to modify it (no further microbiological data n=43; virus-positive-BAL for
which a specific therapy is not possible to perform n=13). Table 1S (supplementary material) shows
a comparative analysis between patients undergoing or not a BAL-driven antimicrobial treatment:
we did not find any significant differences in terms of clinical features and empiric antimicrobial
strategy between cohort of patients undergoing or not a BAL-driven treatment. In particular, among
89 patients in which a BAL-driven antimicrobial treatment was possible on the basis of BAL
results, 7 patients (8%) were treated with empiric antifungal treatment at the time of LI detection
and in other 36 (40%) an empirical antifungal treatment was started on the basis of radiological
findings. Similar results were obtained in patients in which a BAL-driven antimicrobial treatment
was not possible: 3 patients (5%) were treated with empiric antifungal treatment at the time of LI
detection and in other 21 (37%) empirical antifungal treatment was started in the basis of
radiological findings. Even though GM was positive in 41 cases (28%), a diagnosis of probable IPA
according to the EORTC/MSG 2008 criteria was possible only in 18 cases with "typical"
radiological signs. Alternatively, in 23 cases (56%) a positive BAL-GM in patients with "atypical"
radiological signs was detected. However, in almost all cases in which a GM was positive on BAL
This article is protected by copyright. All rights reserved.
(40/41), these findings allowed clinicians to guide the antimicrobial treatment by starting patients
on specific antifungal therapy and/or modifying the on-going empirical therapy. Cases with
“atypical” radiological signs and with positive BAL-GM but not fulfilling the EORTC/MSG 2008
criteria were more frequently reported in patients with chronic lymphoproliferative diseases
(P=0,039) and with less severe neutropenia evaluated at the time of LI detection (median ANC
0,95 vs 0,17 x 109/L; P<0,001). Interestingly, a BAL driven antimicrobial treatment approach was
possible in a similar amount of patients in both cohorts (96% vs 100%; P=0,965) and clinical
outcome was not significantly different between the two patient cohorts (P=0,878).
Overall survival and attributable mortality (secondary end-points)
We observed a significant better outcome of LI at day +30 from its detection in patients where a
BAL-driven antimicrobial treatment was possible (resolution/improvement rate: 71% vs 55%;
P=0,04). We observed a significantly improved outcome in terms of 120d-OS (78% vs 59%;
P=0,009) and 120d-AM (11 vs 30%; P=0,003) for patients in which a BAL-driven antimicrobial
treatment was possible (Figure 1, panel B and Figure 1S, supplementary material). Finally, the
univariate and multivariate analyses were performed in order to identifying the factors that were
significantly associated with the risk of OS and AM (Table 3). Advanced age (HR 2,33 95%CI:
1,03-5,21; P=0,04) and high value of APACHE II (HR 2,28 95%CI: 1,03-5,05; P=0,04) were found
to be independent factors negatively affecting survival, whereas a BAL-driven antimicrobial
treatment was related to better 120d-OS (HR 0,24 95%CI: 0,11-0,52; P<0,001). Moreover, a BAL-
driven antimicrobial treatment was the only independent factor related to a lower 120d-AM in our
study patient-population (HR 0,35 95%CI: 0,16-0,79; P=0,011).
Safety (secondary end-point)
We did not observe any severe adverse effects, but only 5 cases of grade 1-2 adverse events
occurred after the procedure and were easily managed and resolved (respiratory distress n=2, fever
n=2, epistaxis n=1).
DISCUSSION
This article is protected by copyright. All rights reserved.
Bronchoscopy with BAL is useful in HM patients particularly when performed early, allowing to
guide on-going antimicrobial treatment based on results from 50-60% of cases.6-7 However, most of
these studies were designed as retrospective analyses, but large prospective studies with rigorous
inclusion criteria suggesting the impact of BAL execution on clinical outcome are very few. Lucena
and collaborators14 conducted a prospective single institution study on patients undergoing ASCT
and allo-SCT identifying 73 cases of pulmonary complications among 169 patients in the study.
The diagnostic yield for infectious pulmonary complications was 78%, showing a more frequent
viral (28%) and bacterial (26%) etiology of pneumonia. A fungal infection was diagnosed in about
16% of cases. Interestingly, an early bronchoscopy (≤5 days from LI detection) had significantly
higher diagnostic yield when compared to late bronchoscopy (78 vs 23%; P=0,02). In this study, the
authors reported that data obtained by BAL results allowed to change the empirical antimicrobial
treatment in about half of the patients, demonstrating the utility of this procedure in the transplant
setting, leading to better patient management. Overall, the mortality rate after 1 year follow-up was
22%, with about one third of all deaths due to pulmonary complications, however the clear
correlation between changes of empirical antimicrobial treatment and survival was not shown by
the authors. The strength of our study is the prospective design and the relatively stringent inclusion
criteria (severely immunocompromised HM patients with LI detection at CT assessment without
any non-invasive diagnostic documentation and unresponsive to broad-spectrum antimicrobial
therapy) that allowed us to analyze an homogenous patient population. Moreover, we established
primary and secondary end-points, including clinical outcomes in term of both treatment response
and survival. This was an observational study because the final choice on performing or not
bronchoscopy in eligible patients was up to the local physicians. Our data show that a LI was
detected in about 14% of HM patients admitted to hospital, which is in line with other published
data.1 Out of 177 eligible patients, BAL was feasible in 82% of cases within a median time from LI
detection of 4 days. Our patients were severely immunocompromised, most frequently affected by
acute leukaemia or undergoing allo-SCT, with a median ANC at LI detection of about 0,4 x 10/9L
and most having experienced (60%) a prolonged and severe neutropenia or received steroid therapy
(33%). Moreover, some patients presented severe respiratory failure (16%) and the median value of
APACHE II score was 16, suggesting a “severely ill population”. Despite the multicenter design,
our data appeared quite homogeneous because of how the recommended diagnostic panel was
This article is protected by copyright. All rights reserved.
planned, including culture-based and non-culture-based exams, obtaining an acceptable adherence
rate for all diagnostic assays, except for Aspergillus PCR. Using this recommended panel, the
diagnostic yield was of 76%: in 41 cases positive BAL-GM was found, 36 for bacteria, 5 for
Pneumocystis and the remaining cases for respiratory viruses. In 10 cases, a mixed infection was
diagnosed. Our diagnostic yield seems to be better than the other published data,1-2,6-7,11 but almost
identical to those reported in the few prospective studies with a similar design.13-14 In our study, the
BAL results allowed to guide the on-going empirical treatment in about 60% of cases, according to
the data reported in the literature that are more heterogeneous but reported an overall percentage
between 20 and 70%.2,6-7,13,15,27-31 We showed a significantly better clinical outcome in terms of
response to antimicrobial treatment, 120d-OS (78% vs 59%; P=0,009) and 120d-AM (11% vs 30%;
P=0,003) for patients in which a BAL-driven antimicrobial treatment was possible. However, it is
important to underline that the most relevant weakness of our study is the non-randomized design,
that could negatively affects the reliability of these findings. Nevertheless, our data are very
relevant because only a few studies prospectively evaluated the impact of diagnostic BAL on
survival. Interestingly, we showed that BAL results permitted to adding or modifying antibiotic or
antiviral treatment in about half of patients, avoiding unnecessary prolonged antifungal treatment.
Azoulay and collaborators did not find that BAL had any influence on mortality in a prospective
experience on 128 critically ill cancer patients, including transplant recipients, suggesting however
that performing an early BAL (within 4 days from symptoms onset) was significantly associated
with better survival compared with late BAL.15 Similar results were obtained by another interesting
study that failed to show an overall impact on survival, but highlighted that BAL-driven antibiotic
changes within 7 days from LI presentation significantly correlated with a lower mortality.27
However, the results obtained in both these studies are not completely comparable with our data, as
they were carried out several years ago and focused on a more heterogeneous and critical patient
population. To the best of our knowledge, our study is the first prospective study in which a BAL-
driven antimicrobial approach is found to have a positive impact on clinical outcome and mortality.
These results are relevant because they were obtained in the context of a prospective multicenter
study. As for safety, similarly to previously cited studies, we did not observe any grade 3 adverse
events, but only five case of grade 1-2 adverse events that were easily managed, confirming that
BAL execution is safe also in this population of patients. In our study, a positive BAL-GM was
This article is protected by copyright. All rights reserved.
defined as an optical density index > 0,5 according to the recent clinical guidelines of the European
Society for Clinical Microbiology and Infectious Diseases, the European Confederation of Medical
Mycology and the European Respiratory Society Joint .22-25 The optimal cut-off of BAL GM has not
been established yet. Some published studies suggested a higher positive predictive value of
1,0,25,32-33 others instead showed the best diagnostic performance of 0,523 while some reports
highlighted the excellent sensitivity and specificity of 1,5 in the HM setting.27 By using the 0,5 cut-
off, we found 41 positive cases of BAL-GM. In 40 cases, the local investigators considered this
value reliable and modified the on-going antimicrobial treatment accordingly, whereas one case
only was interpreted as a "false positive". Only about half of the cases, were we able to diagnose a
probable IPA according to the EORTC/MSG 2008 criteria, as only these presented "typical"
radiological signs needing formal diagnosis of a probable IPA. Interestingly, by comparing cases
with "typical" and "atypical" radiological signs, we found that positivity of BAL-GM in the absence
of typical radiological lesions of IFD can be detected mostly in patients with chronic
lymphoproliferative disorders and with less severe neutropenia and that clinical outcome and
survival between the two group of patients were similar, probably due to the prompt start of a
specific antifungal treatment. These data are interesting and suggest the need to revise the
EORTC/MSG radiological criteria that seem to be too stringent. The EORTC/MSG criteria were
proposed with the aim to establish a standardized set of criteria that allow to easily compare the
results of clinical trials concerning IFD, but failed to be applied extensively in clinical practice
where the application of these criteria could underestimate these severe complications.34-39 As a
result, the revision of these criteria with the inclusion of a new category of IPA granting a greater
weight on microbiological criteria was proposed by Nucci and collaborators in 2010.38 Based on
these considerations, in our study 40 over 41 cases of BAL-GM positivity were considered, treated
and managed as a probable IPA and the clinical outcome of cases without "typical" radiological
criteria was substantially equivalent to others, suggesting a higher positive predictive value of a
positive BAL-GM irrespective of the presence of typical radiological findings.
In conclusion, in severely immunocompromised HM patients with LI detection at high risk of
invasive fungal disease without any microbiological and/or serological documentation nor fever or
respiratory distress not responding to broad-spectrum antimicrobial therapy we found that: 1) BAL
allows to detect a putative agent of LI in about 75% of cases; 2) BAL is a feasible procedure in
This article is protected by copyright. All rights reserved.
almost all cases; 3) cases with positive BAL-GM without radiological criteria according to
EORTC/MSG show similar features and clinical outcome of probable IPA completely fulfilling
EORTC/MSG criteria; 4) a BAL-driven antimicrobial treatment is feasible in 61% of patients who
underwent BAL and allows to improve clinical outcome and survival. Further randomized studies
are warrant to confirm these results.
This article is protected by copyright. All rights reserved.
ACKNOWLEGMENTS
We thank Federica Falcioni and Elena Papa for the technical support during protocol submission to
Ethical Committee and Diana Giannarelli for the support in statistical study design. We thank
thoracic surgeons, pneumologists and microbiologists for their support during study carrying out.
We thank Tania Merlino (English native speaker, scientific clinical writer) for revising the
manuscript.
FUNDING
None. The study has been carried out as part of our routine work.
CONFLICT OF INTEREST
All authors: none to declare.
AUTHOR CONTRIBUTIONS
FM, CC, MD and LP: conception and design of the study; FM, CC, MC, MD, MD, MIDP, AS,
NSF, LM, KP, CA, DR, MG, MB, MC, DA, SC, ND, AB: patients management and data
collection; FM, CC, AM, LP: data analysis and results interpretation; FM and CC: manuscript
writing; SC, MT, AM and LP: critical manuscript review.
This article is protected by copyright. All rights reserved.
REFERENCES
1. Maschmeyer G, Donnelly JP. How to manage lung infiltrates in adults suffering from
haematological malignancies outside allogeneic haematopoietic stem cell transplantation. Br J
Haematol. 2016; 173: 179-89.
2. Harris B, Geyer AI. Diagnostic evaluation of pulmonary abnormalities in patients with
hematologic malignancies and hematopoietic cell transplant. Clin Chest Med. 2017; 38: 317-31.
3. Garcia JB, Lei X, Wierda W, et al. Pneumonia during remission induction chemotherapy in
patients with acute leukemia. Ann Am Thorac Soc. 2013;10: 432-440.
4. Mayer S, Pastores SM, Riedel E, et al. Short- and long-term outcomes of adult allogeneic
hematopoietic stem cell transplant patients admitted to the intensive care unit in the peritransplant
period. Leuk Lymphoma. 2017; 58: 382-90.
5. Hummel M, Rudert S, Hof H, Hehlmann R, Buchheidt D. Diagnostic yield of bronchoscopy with
bronchoalveolar lavage in febrile patients with hematologic malignancies and pulmonary infiltrates.
Ann Hematol. 2008; 87: 291-297.
6. Wingard JR, Hiemenz JW, Jantz MA. How I manage nodular lesions and nodular infiltrates in
patients with hematologic malignancies or undergoing hematopoietic cell transplantation. Blood.
2012; 120: 1791-1800.
7. Shannon VR, Andersson BS, Lei X, Champlin RE, Kontoyiannis DP. Utility of early versus late
fiberoptic bronchoscopy in the evaluation of new pulmonary infiltrates following hematopoietic
stem cell transplantation. Bone Marrow Transplant. 2010; 45: 647-55.
8. Kontoyiannis DP. Rational approach to pulmonary infiltrates in leukemia and transplantations.
Best Pract Res Clin Haematol. 2013; 26: 301-6.
This article is protected by copyright. All rights reserved.
9. Huaringa AJ, Leyva FJ, Signes-Costa J, et al. Bronchoalveolar lavage in the diagnosis of
pulmonary complications of bone marrow transplant patients. Bone Marrow Transplant. 2000; 25:
975-9.
10. Boersma WG, Erjavec Z, van der Werf TS, de Vries-Hosper HG, Gouw AS, Manson WL.
Bronchoscopic diagnosis of pulmonary infiltrates in granulocytopenic patients with hematologic
malignancies: BAL versus PSB and PBAL. Respir Med. 2007; 101: 317-25.
11. Sampsonas F, Kontoyiannis DP, Dickey BF, Evans SE. Performance of a standardized
bronchoalveolar lavage protocol in a comprehensive cancer center: a prospective 2-year study.
Cancer. 2011; 117: 3424-33.
12. Svensson T, Lundström KL, Höglund M, Cherif H. Utility of bronchoalveolar lavage in
diagnosing respiratory tract infections in patients with hematological malignancies: are invasive
diagnostics still needed? Ups J Med Sci. 2017; 122: 56-60.
13. Marchesi F, Spadea A, Pimpinelli F, et al. The predictive value of Aspergillus PCR testing on
bronchoalveolar lavage fluid for early diagnosis of invasive pulmonary aspergillosis in hematologic
patients. Leuk Lymphoma. 2017; 58: 2943-6.
14. Lucena CM, Torres A, Rovira M, et al. Pulmonary complications in hematopoietic SCT: a
prospective study. Bone Marrow Transplant. 2014; 49: 1293-9.
15. Azoulay E, Mokart D, Rabbat A, et al. Diagnostic bronchoscopy in hematology and oncology
patients with acute respiratory failure: prospective multicenter data. Crit Care Med. 2008; 1: 100-7.
16. De Pauw B, Walsh TJ, Donnely JP, et al. Revised definitions of invasive fungal disease from
the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections
This article is protected by copyright. All rights reserved.
Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study
Group (EORTC/MSG) consensus group. Clin Infect Dis. 2008; 46: 1813-21.
17. Averbuch D, Orasch C, Cordonnier C, et al; ECIL4, a joint venture of EBMT, EORTC, ICHS,
ESGICH/ESCMID and ELN. European guidelines for empirical antibacterial therapy
for febrile neutropenic patients in the era of growing resistance: summary of the 2011 4th European
Conference on Infections in Leukemia. Haematologica. 2013; 98: 1826-35.
18. Baden LR, Swaminathan S, Angarone M, et al. Prevention and Treatment of Cancer-
Related Infections, Version 2.2016, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr
Canc Netw. 2016; 14: 882-913.
19. Hansell DM, Bankier AA, MacMahon H, et al. Fleischner Society: glossary of terms for
thoracic imaging. Radiology. 2008; 246: 697-722.
20. Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification
system. Crit Care Med. 1985; 13 :818-829.
21. Alaino A, Hauser PM, Lagrou K, et al. ECIL guidelines for the diagnosis of Pneumocystis
jirovecii pneumonia in patients with haematological malignancies and stem cell transplant
recipients. J Antimicriob Chemotherap. 2016; 71: 2386-2396.
22. Ullmann AJ, Aguado JM, Arikan-Akdagli S, et al. Diagnosis and management of Aspergillus
diseases: executive summary of the 2017 ESCMID-ECMM-ERS guideline. Clin Microbiol Infect.
2018; 24 Suppl 1: e1-e38.
23. Reinwald M, Spiess B, Heinz WJ, et al. Diagnosing pulmonary aspergillosis in patients with
hematological malignancies: a multicenter prospective evaluation of an Aspergillus PCR assay and
a galactomannan elisa in bronchoalveolar lavage sample. Eur J Haematol. 2012; 89: 120-7.
This article is protected by copyright. All rights reserved.
24. Heng SC, Morrissey O, Chen SC, et al. Utility of bronchoalveolar lavage fluid galactomannan
alone or in combination withPCR for the diagnosis of invasive aspergillosis in adult hematology
patients: a systematic review and meta-analysis. Crit Rev Microbiol. 2015; 41: 124-34.
25. Zou M, Tang L, Zhao S, Zhao Z, Chen L, Chen P, et al. Systematic review and meta-analysis of
detecting galactomannan in bronchoalveolar lavage fluid for diagnosing invasive aspergillosis.
PLoSOne. 2012; 7, e43347.
26. Ljungman P, Boeckh M, Hirsch HH, et al. Definitions of cytomegalovirus infection and disease
in transplant patients for use in clinical trials. Clin Infect Dis. 2017; 64: 87-91.
27. Rano A, Agusti C, Jimenez P, et al. Pulmonary infiltrates in non-HIV immunocompromised
patients: a diagnostic approach using a non-invasive and bronchoscopic procedure. Thorax. 2001;
56: 379-87.
28. Kim SW, Rhee CK, Kang HS, et al. Diagnostic value of bronchoscopy in patients with
hematologic malignancy and pulmonary infiltrates. Ann Hematol. 2015; 94: 153-9.
29. Hofmeister CC, Czerlanis C, Forsythe S, et al. Retrospective utility of bronchoscopy after
hematopoietic stem cell transplant. Bone Marrow Transplant. 2006; 38: 693-8.
30. Gilbert CR, Lerner A, Baram M, et al. Utility of flexible bronchoscopy in the evaluation of
pulmonary infiltrates in the hematopoietic stem cell transplant population – a single center fourteen
year experience. Arch Bronconeumol. 2013; 49: 189-95.
31. Gupta S, Sultenfuss M, Romaguera JE, et al. CT-guided percutaneous lung biopsies in patients
with hematologic malignancies and undiagnosed pulmonary lesions. Hematol Oncol. 2010; 28: 75-
81.
This article is protected by copyright. All rights reserved.
32. Taremi M, Kleinberg ME, Wang EW, et al. Galactomannan antigen detection using bronchial
wash and bronchoalveolar lavage in patients with hematologic malignancies. Ann Clin Microbiol
Antimicrob. 2015; 14: 50.
33. Farmakiotis D, Le A, Weiss, et al. False positive bronchoalveolar lavage galactomannan: Effect
of host and cut-off value. Mycoses. 2019; 62: 204-13.
34. Chamilos G, Luna M, Lewis RE, et al. Invasive fungal infections in patients with hematologic
malignancies in a tertiary care cancer center: an autopsy study over a 15-year period (1989-2003).
Haematologica. 2006; 91: 986-9.
35. Hachem R, Sumoza D, Hanna H, et al. Clinical and radiologic predictors of invasive pulmonary
aspergillosis in cancer patients: should the European Organization for Research and Treatment of
Cancer/Mycosis Study Group (EORTC/MSG) criteria be revised? Cancer. 2006; 106:1581-6.
36. Sinkó J, Csomor J, Nikolova R, et al. Invasive fungal disease in allogeneic hematopoietic stem
cell transplant recipients: an autopsy-driven survey. Transpl Infect Dis. 2008; 10: 106-9.
37. Subirà M, Martino R, Rovira M, et al. Clinical applicability of the new EORTC/MSG
classification for invasive pulmonary aspergillosis in patients with hematological malignancies and
autopsy-confirmed invasive aspergillosis. Ann Hematol. 2003; 82: 80-82.
38. Nucci M, Nouér SA, Grazziutti M, et al. Probable invasive aspergillosis without prespecified
radiologic findings: proposal for inclusion of a new category of aspergillosis and implications for
studying novel therapies. Clin Infect Dis. 2010; 51: 1273-80.
39. Girmenia C, Guerrisi P, Frustaci AM, et al. New category of probable invasive pulmonary
aspergillosis in haematological patients. Clin Microbiol Infect. 2012; 18: 990-6.
This article is protected by copyright. All rights reserved.
Figure legends
Figure 1. Flow chart of enrolled patients (panel A); attributable mortality (AM) of 145 patients
undergoing BAL evaluated at 120 days from LI detection (panel B).
This article is protected by copyright. All rights reserved.
Accepted Article
This article is protected by copyright. All rights reserved.
Table 1. Demographic characteristics of 145 patients undergoing BAL.
Demographic characteristics at enrollment N (%)
Median age (range) 61 (1-83)
Sex
M 85 (59%)
F 60 (41%)
Diagnosis
Accepted Article
AML/MDS 67 (46%)
Lymphoma 34 (24%)
ALL 19 (13%)
Myeloma 14 (10%)
CLL 5 (3%)
Other* 6 (4%)
Disease status
Newly diagnosed 48 (33%)
CR 41 (28%)
PR 41 (28%)
R/R 15 (11%)
Last treatment received
Induction 53 (36%)
Salvage 37 (25%)
AlloSCT 27 (19%)
Cytoreduction/pre-phase 11 (8%)
Consolidation 10 (7%)
ASCT 7 (5%)
Radiologic features of LI **
Not well circumscribed or diffuse consolidations 66 (45%)
Dense, well circumscribed lesions with or without halo sign 46 (32%)
Ground glass opacity 20 (14%)
Micronodules 4 (3%)
Interstitial lung abnormalities 3 (2%)
Cavity 3 (2%)
Tree in bud 3 (2%)
AML: acute myeloid leukemia; MDS: myelodysplastic syndrome; ALL: acute lymphoblastic leukemia;
CLL: chronic lymphocytic leukemia; CR: complete response; PR: partial response; R/R: relapsed/refractory;
alloSCT: allogeneic hematopoietic stem cell transplant; ASCT: autologous hematopoietic stem cell transplant.
*
Other: aplastic anemia (n=2), hairy cell leukemia (n=2), idiopathic myelofibrosis (n=1), POEMS syndrome (n=1).
**
Radiologic feature of LI: the prevalent aspect at thoracic computed tomography assessment has been reported.
This article is protected by copyright. All rights reserved.
Table 2. Detailed report of pathogens detected by BAL in 89 patients undergoing a BAL-
driven antimicrobial treatment.
Isolation (*) No. cases Percentage
Galactomannan 40 45%
Without fungal growth 35
Aspergillus fumigatus 3
Aspergillus terreus 1
Aspergillus niger 1
Bacteria 32 36%
Klebsiella pneumoniae 6
Accepted Article
Stenotrophomonas maltophilia 5
Pseudomonas aeruginosa 5
VRE 4
Staphylococcus aureus 3
Acinetobacter baumanii 2
Escherichia coli 2
Other gram positive (**) 2
Haemophilus influenziae 1
Legionella pneumophila 1
Clamydia pneumoniae 1
Viruses 11 12%
Cytomegalovirus 7
Influenza A (H1N1) 4 (3)
Pneumocystiis jirovecii 6 7%
(*) in 10 cases we detected mixed infections
(**) Streptococcus pneumoniae (1); Rothia mucillaginosa pneumonia diagnosed and confirmed by MALDI (2).
VRE: vancomycin-resistant Enterococci
This article is protected by copyright. All rights reserved.
Table 3. Univariate and multivariate analysis for 120d-OS and 120d-AM in patients undergoing BAL (n=145).
Variable (120d-OS) Univariate Multivariate
P HR (95%CI) P
Accepted Article
Age < vs ≥ median (60 years) 0,009 2,33 (1,03-5,21) 0,04
Diagnosis (AML vs ALL vs lymphoma vs myeloma vs other) 0,905 - -
Treatment (induction vs alloSCT vs salvage vs other) 0,169 - -
Disease status (CR/PR vs newly diagnosed vs R/R) 0,124 2,67 (0,33-21,6) 0,122
APACHE II score < vs ≥ median (16) 0,042 2,28 (1,03-5,05) 0,04
BAL-driven antimicrobial treatment (yes vs no) 0,009 0,24 (0,11-0,52) < 0,001
Variable (120d-AM) Univariate Multivariate
P HR (95%CI) P
Age < vs ≥ median (60 years) 0,046 2,18 (0,94-5,07) 0,068
Diagnosis (AML vs ALL vs lymphoma vs myeloma vs other) 0,982 - -
Treatment (induction vs alloSCT vs salvage vs other) 0,098 - -
Disease status (newly diagnosed vs R/R vs CR/PR) 0,494 - -
APACHE II score < vs ≥ median (16) 0,249 - -
BAL-driven antimicrobial treatment (yes vs no) 0,003 0,35 (0,16-0,79) 0,011
120d-OS: overall survival after 120 days from lung infiltrate detection; HR: hazard ratio; CI: confidence interval;
AML: acute myeloid leukemia; ALL: acute lymphoblastic leukemia; R/R: relapsed/refractory; CR: complete remission;
PR: partial remission.
This article is protected by copyright. All rights reserved.
You might also like
- The OCD Workbook - Your Guide To Breaking Free From Obsessive-Compulsive Disorder (PDFDrive)Document378 pagesThe OCD Workbook - Your Guide To Breaking Free From Obsessive-Compulsive Disorder (PDFDrive)MrRamm100% (12)
- Panss PDFDocument10 pagesPanss PDFJana Chihai50% (2)
- Medicolegal Reporting in Orthopaedic Trauma PDFDocument543 pagesMedicolegal Reporting in Orthopaedic Trauma PDFRajiv Tanwar100% (1)
- Abus A User GuideDocument304 pagesAbus A User Guidemaria astrianiNo ratings yet
- Nordic Questionnaire For Low Back PainDocument5 pagesNordic Questionnaire For Low Back Painbubbly_bea86% (7)
- Caselli 2014Document5 pagesCaselli 2014AdrianaGallardoTapiaNo ratings yet
- Isrn Oncology2012-652682Document7 pagesIsrn Oncology2012-652682Igoh Est Part IINo ratings yet
- Clinical OncologyDocument8 pagesClinical OncologyHector VillaseñorNo ratings yet
- Thelancethaematology D 18 00319R2Document154 pagesThelancethaematology D 18 00319R2anabejarano530No ratings yet
- Invasive Fungal Infections in Pediatric Oncology: MD MD MD MD MD MDDocument6 pagesInvasive Fungal Infections in Pediatric Oncology: MD MD MD MD MD MDerickmattosNo ratings yet
- Complicated Parapneumonic Effusion and Empyema Thoracis: Microbiology and Predictors of Adverse OutcomesDocument9 pagesComplicated Parapneumonic Effusion and Empyema Thoracis: Microbiology and Predictors of Adverse OutcomesabhikanjeNo ratings yet
- ArticleDocument16 pagesArticleobbyNo ratings yet
- Validation of The Meet URO Score in Patients WithDocument9 pagesValidation of The Meet URO Score in Patients Withveaceslav coscodanNo ratings yet
- Pi Is 1201971213002142Document5 pagesPi Is 1201971213002142melisaberlianNo ratings yet
- Vivia BiotechDocument10 pagesVivia Biotech11 11No ratings yet
- Epstein-Barr Virus-Related Post-Transplant Lymphoproliferative Disorder in Solid Organ Transplant RecipientsDocument10 pagesEpstein-Barr Virus-Related Post-Transplant Lymphoproliferative Disorder in Solid Organ Transplant Recipients19112281s3785No ratings yet
- 2018 Article 2099Document10 pages2018 Article 2099igariok06No ratings yet
- Antibiotics 02 00001Document10 pagesAntibiotics 02 00001Jenny AlmagroNo ratings yet
- Reference - 04Document9 pagesReference - 04Omar García HernándezNo ratings yet
- WJH 3 130bacteremiaDocument7 pagesWJH 3 130bacteremiaLasiaf AlaskaNo ratings yet
- Carraro 2013 RSBMTV 46 N 2 P 161Document5 pagesCarraro 2013 RSBMTV 46 N 2 P 161Emerson CarraroNo ratings yet
- tmp8B97 TMPDocument11 pagestmp8B97 TMPFrontiersNo ratings yet
- Hepatitis C Virus in Non-Hodgkin's Lymphoma. A Reappraisal After A Prospective Case-Control Study of 300 PatientsDocument6 pagesHepatitis C Virus in Non-Hodgkin's Lymphoma. A Reappraisal After A Prospective Case-Control Study of 300 PatientsAraceli EnríquezNo ratings yet
- UNICEF Annual ReportDocument15 pagesUNICEF Annual ReportraissametasariNo ratings yet
- Cytometry Part B Clinical - 2017 - Dworzak - AIEOP BFM Consensus Guidelines 2016 For Flow Cytometric Immunophenotyping ofDocument12 pagesCytometry Part B Clinical - 2017 - Dworzak - AIEOP BFM Consensus Guidelines 2016 For Flow Cytometric Immunophenotyping ofdworzakNo ratings yet
- Eli SpotDocument20 pagesEli SpotAdel HamadaNo ratings yet
- Cytopenias in Patients With CLLDocument11 pagesCytopenias in Patients With CLLLuana MNo ratings yet
- Mortality & Recurrent Seizure Risk After New-Onset Seizure in HIV-positive Zambian AdultsDocument10 pagesMortality & Recurrent Seizure Risk After New-Onset Seizure in HIV-positive Zambian AdultsAdam PrabataNo ratings yet
- First Diagnosis of Systemic Lupus Erythematosus in HospitalizedDocument35 pagesFirst Diagnosis of Systemic Lupus Erythematosus in HospitalizedFranco PacelloNo ratings yet
- Loglio 2020Document2 pagesLoglio 2020AvianitaNo ratings yet
- Diagnostic Accuracy of 3 Urine Lipoarabinomannan TuberculosisDocument10 pagesDiagnostic Accuracy of 3 Urine Lipoarabinomannan TuberculosisvanialibNo ratings yet
- Cyto B 21518 PDFDocument12 pagesCyto B 21518 PDFNurul Huda KowitaNo ratings yet
- Cancers 12 02747Document15 pagesCancers 12 02747Hematología INSNSBNo ratings yet
- Research Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology FindingsDocument9 pagesResearch Article: Neutropenic Sepsis in The ICU: Outcome Predictors in A Two-Phase Model and Microbiology Findings28121998No ratings yet
- A Study Oncytopenias and The Factors Associated With Cytopenias Among Hiv Infected Patients Admitted at A Tertiary Care HospitalDocument8 pagesA Study Oncytopenias and The Factors Associated With Cytopenias Among Hiv Infected Patients Admitted at A Tertiary Care HospitalIJAR JOURNALNo ratings yet
- 2953 Hbsag SkriningDocument4 pages2953 Hbsag Skriningursula 002No ratings yet
- Heparin-Binding Protein: A Diagnostic Biomarker of Urinary Tract Infection in AdultsDocument9 pagesHeparin-Binding Protein: A Diagnostic Biomarker of Urinary Tract Infection in AdultsFitria NurulfathNo ratings yet
- R Codox M Linfoma BurkittDocument8 pagesR Codox M Linfoma BurkittALEXANDER AVILANo ratings yet
- Applicability of Serum Interleukin-6 As A Screening Tool For Nasopharyngeal CarcinomaDocument8 pagesApplicability of Serum Interleukin-6 As A Screening Tool For Nasopharyngeal Carcinomarimelda aquinasNo ratings yet
- Teori Eosinopenia DewasaDocument7 pagesTeori Eosinopenia DewasaNurlyanti RustamNo ratings yet
- Pathogen Inctivation in Donated BloodDocument30 pagesPathogen Inctivation in Donated BloodNader AlharbiNo ratings yet
- Use of F-FDG PET To Predict Response To First-Line Tuberculostatics in HIV-Associated TuberculosisDocument6 pagesUse of F-FDG PET To Predict Response To First-Line Tuberculostatics in HIV-Associated TuberculosisdhaniNo ratings yet
- Immature Platelet Fraction Predicts Early Marrow Recovery in Febrile NeutropeniaDocument13 pagesImmature Platelet Fraction Predicts Early Marrow Recovery in Febrile NeutropeniasulvitaNo ratings yet
- Cas 111 1739Document11 pagesCas 111 1739Nathur IdrisNo ratings yet
- ManuscriptDocument13 pagesManuscriptMegbaruNo ratings yet
- Pediatric Blood Cancer - 2023 - Abstracts From The 39th Annual Meeting of The Histiocyte SocietyDocument64 pagesPediatric Blood Cancer - 2023 - Abstracts From The 39th Annual Meeting of The Histiocyte SocietySeham GoharNo ratings yet
- JMP 02 00022Document19 pagesJMP 02 00022Peterpan NguyenNo ratings yet
- Cancers 14 00826Document14 pagesCancers 14 00826ZakiyahulfahdwNo ratings yet
- Jurnal Interna 123456Document9 pagesJurnal Interna 123456vonnyandira28No ratings yet
- Outcome and Clinical Characteristics in Pleural Empyema: A Retrospective StudyDocument7 pagesOutcome and Clinical Characteristics in Pleural Empyema: A Retrospective StudylestarisurabayaNo ratings yet
- Antifungal Treatment Duration in Hematology Patients With Invasive Mold Infections A Real-Life UpdateDocument9 pagesAntifungal Treatment Duration in Hematology Patients With Invasive Mold Infections A Real-Life UpdateNelly Mabel Quiroz HernandezNo ratings yet
- Management of Urinary Tract Infections in Female General Practice PatientsDocument7 pagesManagement of Urinary Tract Infections in Female General Practice PatientsCosmin CalanciaNo ratings yet
- Management of Urinary Tract Infections in Female General Practice PatientsDocument7 pagesManagement of Urinary Tract Infections in Female General Practice PatientsGede ArianaNo ratings yet
- CANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan TangDocument7 pagesCANCER UPDATE Clinical Stem Cell Document - Alex Mou & Ryan Tangalexmou2008No ratings yet
- Sensitive Electrochemiluminescence (ECL) Immunoassays For Detecting Lipoarabinomannan (LAM) and ESAT-6 in Urine and Serum From Tuberculosis PatientsDocument19 pagesSensitive Electrochemiluminescence (ECL) Immunoassays For Detecting Lipoarabinomannan (LAM) and ESAT-6 in Urine and Serum From Tuberculosis PatientsMohamed ChedlyNo ratings yet
- Conter 2010 ALL Risk SratificationDocument10 pagesConter 2010 ALL Risk SratificationjenyardenNo ratings yet
- Research Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal SepsisDocument7 pagesResearch Article: The Analysis of Etiology and Risk Factors For 192 Cases of Neonatal Sepsisflorentina lulutNo ratings yet
- I J M R P S: Ndian Ournal of Edical Esearch and Harmaceutical CiencesDocument7 pagesI J M R P S: Ndian Ournal of Edical Esearch and Harmaceutical CiencesidiNo ratings yet
- 2 +Hardi+and+Soeroharjo +analysis+of+hematologicalDocument6 pages2 +Hardi+and+Soeroharjo +analysis+of+hematologicalInnayah KhnisaNo ratings yet
- CML IM Drug-Free Ross Haematologica 2012Document3 pagesCML IM Drug-Free Ross Haematologica 2012JuniaNo ratings yet
- Association Between Immune-Related Adverse Event TDocument8 pagesAssociation Between Immune-Related Adverse Event TAndrew FincoNo ratings yet
- Parik H 2016Document35 pagesParik H 2016Jose Angel AbadíaNo ratings yet
- Delta Neutrophil Index As An Early MDocument9 pagesDelta Neutrophil Index As An Early MFariz NurNo ratings yet
- Imaging of the Liver and Intra-hepatic Biliary Tract: Volume 2: Tumoral PathologiesFrom EverandImaging of the Liver and Intra-hepatic Biliary Tract: Volume 2: Tumoral PathologiesNo ratings yet
- Application of Bioelectrical Impedance Analysis (BIA) To Assess Carcass Composition and Nutrient Retention in Rabbits From 25 To 77 Days of AgeDocument15 pagesApplication of Bioelectrical Impedance Analysis (BIA) To Assess Carcass Composition and Nutrient Retention in Rabbits From 25 To 77 Days of AgeXaralyn XaviereNo ratings yet
- Application of Bioelectrical Impedance Analysis To Assess Rabbit's Body Composition From 25 To 77 Days of AgeDocument12 pagesApplication of Bioelectrical Impedance Analysis To Assess Rabbit's Body Composition From 25 To 77 Days of AgeXaralyn XaviereNo ratings yet
- Arya - Usefulness and Safety of Transbronchial Biopsy With Large Forceps During Flexible BronchosDocument5 pagesArya - Usefulness and Safety of Transbronchial Biopsy With Large Forceps During Flexible BronchosXaralyn XaviereNo ratings yet
- Boonsarngsuk - Factors Affecting The Diagnostic Yield of Flexible Bronchoscopy Without Guidance in Pulmonary Nodules or MassesDocument6 pagesBoonsarngsuk - Factors Affecting The Diagnostic Yield of Flexible Bronchoscopy Without Guidance in Pulmonary Nodules or MassesXaralyn XaviereNo ratings yet
- Antonelli - Fiberoptic Bronchoscopy During Noninvasive Positive Pressure Ventilation Delivered by HelmetDocument4 pagesAntonelli - Fiberoptic Bronchoscopy During Noninvasive Positive Pressure Ventilation Delivered by HelmetXaralyn XaviereNo ratings yet
- Agarwal - Bronchoscopic Lung Biopsy Using Noninvasive Ventilatory Support Case Series and Review of Literature of NIV-assisted BronchosDocument10 pagesAgarwal - Bronchoscopic Lung Biopsy Using Noninvasive Ventilatory Support Case Series and Review of Literature of NIV-assisted BronchosXaralyn XaviereNo ratings yet
- Akoun - Bronchoalveolar Lavage Cell Data in Amiodarone-Associated Pneumonitis Evaluation in 22 PatientsDocument6 pagesAkoun - Bronchoalveolar Lavage Cell Data in Amiodarone-Associated Pneumonitis Evaluation in 22 PatientsXaralyn XaviereNo ratings yet
- Adewole - Flexible Fiberoptic Bronchoscopy in Respiratory Care Diagnostic Yield, Complications, and Challenges in A Nigerian Tertiary CenterDocument5 pagesAdewole - Flexible Fiberoptic Bronchoscopy in Respiratory Care Diagnostic Yield, Complications, and Challenges in A Nigerian Tertiary CenterXaralyn XaviereNo ratings yet
- Ackart - Fiberoptic Bronchoscopy in Outpatient Facilities, 1982Document2 pagesAckart - Fiberoptic Bronchoscopy in Outpatient Facilities, 1982Xaralyn XaviereNo ratings yet
- Glasgow Coma Scale - Pediatric - Pediatric Glasgow Coma ScaleDocument3 pagesGlasgow Coma Scale - Pediatric - Pediatric Glasgow Coma Scalepang_accounts_ni_pauline_perez1060No ratings yet
- Ang Mga Pananaw at Opinyon NG Pag-Uulat NG Mag-Uulat Sa Programang Ito Ay Hindi Ang Pangunahing Posisyon O Pahayag NG Organisasyon ItoDocument16 pagesAng Mga Pananaw at Opinyon NG Pag-Uulat NG Mag-Uulat Sa Programang Ito Ay Hindi Ang Pangunahing Posisyon O Pahayag NG Organisasyon ItoRoilan MarlangNo ratings yet
- Advanced Clinical Problem Solving Transition Into Nursing PracticeDocument55 pagesAdvanced Clinical Problem Solving Transition Into Nursing PracticeZarida ArabainNo ratings yet
- ADHD Screening in AdultsDocument3 pagesADHD Screening in AdultsPanduRespatiNo ratings yet
- Neurodevelopmental DisordersDocument59 pagesNeurodevelopmental DisordersHoorya Hashmi100% (1)
- Glu KosaDocument6 pagesGlu Kosajulianprist777No ratings yet
- Teaching Resource Mental Status ExaminationDocument3 pagesTeaching Resource Mental Status ExaminationKevin Leo Lucero AragonesNo ratings yet
- SKD Death Claim English Ver. 01Document1 pageSKD Death Claim English Ver. 01velandoNo ratings yet
- TMJ Manual 792Document19 pagesTMJ Manual 792Ellery FarrellNo ratings yet
- Rapid Cycling Bipolar Disorder in Adults - Treatment of Major Depression PDFDocument10 pagesRapid Cycling Bipolar Disorder in Adults - Treatment of Major Depression PDFdreaming100% (1)
- 356 Mastering Psychiatry Term-Paper PDFDocument356 pages356 Mastering Psychiatry Term-Paper PDFdragutinpetricNo ratings yet
- ADHD Documentation FormDocument3 pagesADHD Documentation FormKyle SmithNo ratings yet
- Thyroid Testing: What Is A Normal TSH Level?: Implications For PatientsDocument1 pageThyroid Testing: What Is A Normal TSH Level?: Implications For PatientskaterinaNo ratings yet
- Attention Deficit Hyperactivity DisorderDocument14 pagesAttention Deficit Hyperactivity DisorderAlexander GoldfarbNo ratings yet
- Nutrition and Vascular DementiaDocument6 pagesNutrition and Vascular Dementiaapi-150223943No ratings yet
- Medical Image Analysis - Overview - NewDocument11 pagesMedical Image Analysis - Overview - Newedi pNo ratings yet
- Research in Autism Spectrum Disorders: Efrosini KalyvaDocument5 pagesResearch in Autism Spectrum Disorders: Efrosini KalyvakarlyNo ratings yet
- Combination PsychotherapyDocument37 pagesCombination PsychotherapyElija MansonNo ratings yet
- Childhood Disorders Lesson PlanDocument8 pagesChildhood Disorders Lesson Planapi-284104206No ratings yet
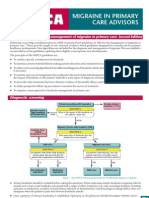
- National Guidelines - MigraineDocument4 pagesNational Guidelines - MigraineSean CardozoNo ratings yet
- DR .Marghoob H YaasDocument3 pagesDR .Marghoob H Yaasمحمد سعد طهNo ratings yet
- Int Endodontic J - 2022 - Azim - Diagnosis Consensus Among Endodontic Specialists and General Practitioners AnDocument10 pagesInt Endodontic J - 2022 - Azim - Diagnosis Consensus Among Endodontic Specialists and General Practitioners AnRazvan UngureanuNo ratings yet
- PSYCHIATRY (Edited by Prof. Gavenko V.L.)Document388 pagesPSYCHIATRY (Edited by Prof. Gavenko V.L.)NIDHIL SYAMNo ratings yet
- Do Mood Instability Symptoms in Epilepsy Represent Formal Bipolar Disorder?Document4 pagesDo Mood Instability Symptoms in Epilepsy Represent Formal Bipolar Disorder?Daiana PiacenzaNo ratings yet
- Clinical Features and Diagnosis of Dementia With Lewy Bodies - FarlowDocument12 pagesClinical Features and Diagnosis of Dementia With Lewy Bodies - FarlowRafael Aramburú Umbert100% (1)