Professional Documents
Culture Documents
Diabetic Foot
Diabetic Foot
Uploaded by
Azi Mohamed AminOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetic Foot
Diabetic Foot
Uploaded by
Azi Mohamed AminCopyright:
Available Formats
Diabetic Foot
Examination 1. Exposure - until the upper knee - examine both feet 2. Inspection a) Examination of the surrounding tissue redness, pale, bluish and congested oedema scar hard corns(hyperkeratosis over the bony prominence, caused by pressure against the shoe) soft corns(marcerated hyperkeratosis lesion between the toes not a/w pressure or friction) callosity fissure cellulitis(raised, erythematous, edematous, painful and warm) abscess scaly trophic changes(hair loss, brittle nails, skin shiny, dry, loss of tissue turgor) gangrenous changes veno-varicosity deformity i) fore foot: claw toe ii) mid foot: cavus foot, pes cavus iii) hind foot: valgus heel space between the toes: any fungal infection b) Examination of the ulcer - single/multiple - site - size - shape - surrounding skin/tissue: redness, swelling - margin regular/irregular well/ill-defined - edge slopping: healing punched out: non-healing undermined: chronic process(pyogenic, TB, amaebic) rolled: basal cell carcinoma - floor pale, pink or red healthy looking? granulation tissue(sign of recovery/healing) sloughed(pale, yellowish or greenish necrosed tissue) discharge(serous, seropurulent, purulent) exposed structures(bone, joint, tendon, neurovascular bundle) - depth 3. Palpation - temperature - tenderness(of the ulcer and surrounding skin) - consistency of surrounding skn
fixation
base - soft/firm/indurated(induration indicates fibrotic tissue underlying) - smooth/irregular - fluctuant(abscess, pus) - contact bleeding - press at edge(milk for pus) 4. Movement - toes - ankle 5. Neurovascular a) motor - tone - power - reflex(knee and ankle jerks) b) sensory - light touch - pain - vibration(first sensation to loss) - proprioception * look for grove and stocking distribution of sensory loss c) vascular - pulses(popliteal, posterior tibialis and dorsalis pedis arteries) - capillary refilling Approach and Assessment 1. determine the cause - neuropathy - ischaemic - combination Neuropathic ulcer 1. dependant and pressure area: metatarsal head, heel and ball of the foot 2. 3. 4. 5. 6. 7. 8. deformity(e.g.claw foot) pink surrounding skin distended vein callosities and fissures painless foot is warm ulcer base: bleeds easily
9. palpable pulses 10. complications: - painless ulceration - infected ulcer - callosities - digital gangrene - Charcoats joint - Neuropathic oedema
Ischaemic ulcer 1. distal part: medial surface of 1st metatarsal head, lateral surface of 5th metatarsal head, tips of toes 2. gangrenous digits 3. pale surrounding skin 4. trophic changes 5. skinny 6. painful to touch 7. cold foot 8. ulcer base: dull fibrotic and no bleed easily 9. weak or absent pulses 10. complications: - painful ulceration - claudication - digital gangrene
* venous ulcer bloated, edematous; usually at medial malleolus 2. determine the stage(by Meggit-Wagner Classification)
3. determine whether is the lesion complicated by infection(cellulitis, abscess or osteomyelitis) Characteristics of Diabetic Foot Infection 1. polymicrobial - aerobes: S.aureus, Streptococci, Coliform - anaerobes: Bacteroides spp. 2. very notorious(does not respect tissue plane can involve whole fascia) 3. chronic in nature and relatively resistant to treatment(healing process is abnormal) Meggit-Wagner Classification - based on depth ofulcer, presence osteomyelitis and severity of gangrene Stage 0: No ulcer; present of risk factors(e.g. foot deformities, sensory neuropathy, previous Hx.of foot ulcer, blind/partially sighted) Stage 1: Superficial ulcer, skin deep(full thickness of skin loss) Stage 2: Deep ulcer usually with infection/cellulitis; no bone involvement Stage 3: Infected deep ulcer with osteomyelitis and abscess formation Stage 4: Ulcer with gangrene of hindfoot(digits) Stage 5: Ulcer with gangrene of forefoot Pathophysiology - multifactorial - 3 main causes: A) polyneuropathy a. motor - weakness of the intrinsic muscles imbalance between the flexors and extensors deformities such as cavus foot, claw toes unusual and uneven pressure distribution repeated trauma b. sensory - loss of pain sensation unaware of noxious stimuli and unable to avoid trauma continuous pressure on a particular pressure area(repetitive stress and high pressure injury hard callosities) - loss of proprioception sensation ataxia and prone to fall c. autonomic - reduced sweating dry skin fissures and cracks portal of entry for microorganisms - loss of microcirculation autoregulation loss of normal hyperaemic response needed to fight the infection B) peripheral vascular disease compromised blood supply poor immune mechanism and wound healing ischaemia devitalised tissue prone to infection C) infection high glucose content culture medium for microorganisms high glucose content reduced chemotactic phagocytosis of inflammatory cells Investigations - 4 important investigations: i) wound swab for microbiological examination + culture & sensitivity(if abscess present aspiration) ii) random blood sugar or fasting blood sugar(assess blood sugar control) iii) foot x-ray(look for osteomyelitis and charcots joint) iv) ankle-brachial systolic index(by Doppler u/s probe)
- important esp. for ischaemic cause and serious infection - normal: 1.0 - > 0.45 is necessary for ulcer healing(wound healing will depend directly on the local blood flow) - < 0.5: impending gangrene - < 0.3: amputation may be needed other investigations: - blood culture - FBC - BUSE - screen for other complications of diabetic mellitus
Management - depends on the grading: A) Grade 0 - mainly prophylaxis: a) foot care - foot hygiene - wear sock s or stockings - footwear should be well fitting with soft and pliable uppers - nails should be transversely at the centre - daily inspection of accidental damage to feet - corns and callosities should be treated by a chiropodist - never walk bare-footed b) patient education - diabetic control(diet, compliance and follow-up) - stop smoking( peripheral vascular disease) c) corrective surgery for deformities - to relieve pressure over potential breakdowns areas B) Grade 1, 2 and 3 1. Control the infection a) local - abscess drainage and dressings - removing mechanical forces(neuropathic ulcer can only be healed if the mechanical forces are removed): i. strict bed rest ii. non weight-bearing on crutches iii. total contact cast invaluable for the Mx of plantar ulcer for grade 1 and 2 ulcers not used in ischaemic ulcers(made the condition worse) the ulcer is debrided and excess callus is removed before the cast application below knee plaster cast applied with minimal padding for a bony prominence it provides equal distribution of forces along the plantar surface of the foot a rigid compression dressing to control swelling ans oedema a protective covering to compensate for the lack of sensation - surgical debridement of infected ulcer and necrotic tissue - surgical revascularization(vascular reconstruction) of the ischaemic foot - skin graft(grade 1) - sometimes may need local amputation(grade 3)
systemic antibiotics: cloxacillin metronidazole(Flagyl) gentamicin 2. Control the blood sugar diet control oral hypoglycaemic agents(OHA) insulin(may shift from OHA to insulin to have proper blood sugar control) C) Grade 4 and 5 - grade 4: a) local amputation - if ABI >0.45 and gangrene is dry and limited to distal portion of toe b) ray amputation - if gangrene is wet and progressive c) below-knee, through-knee or above-knee amputation - if ABI has not been high enough for distal amputation - grade 5: local pocedures not adequate below-knee, through-knee and even above-knee amputation as indicated by vascular status -
b)
You might also like
- Turgeon - Hematology Study QuestionsDocument65 pagesTurgeon - Hematology Study QuestionsGertrudeshane IletoNo ratings yet
- NCP - DMDocument4 pagesNCP - DMMonica Garcia88% (8)
- Skin Care PowerpointDocument52 pagesSkin Care Powerpointisapatrick812667% (3)
- Fs - Evilla, E. (Vertam Farms Opc) 2020Document44 pagesFs - Evilla, E. (Vertam Farms Opc) 2020Ma Teresa B. Cerezo100% (2)
- Diabetic Foot Ulcer and Soft Tissue Infections (NF) : Prepared By: Che Wan Nur Hajar Binti Saimi Supervised By: MR NaikDocument31 pagesDiabetic Foot Ulcer and Soft Tissue Infections (NF) : Prepared By: Che Wan Nur Hajar Binti Saimi Supervised By: MR NaikMujahid Zurich Takaful Johor-GanuNo ratings yet
- Diabetic Foot Ulcer: By: FauzanadliDocument43 pagesDiabetic Foot Ulcer: By: FauzanadliWan RahimahNo ratings yet
- Diabetic FoootDocument34 pagesDiabetic Foootsiakonihmat433No ratings yet
- Diabetic Foot UlcerDocument44 pagesDiabetic Foot UlcerCandy Lee100% (1)
- Diabetic Foot 1Document23 pagesDiabetic Foot 1DR AAMNo ratings yet
- Diabetic FootDocument6 pagesDiabetic FootproudofskyNo ratings yet
- Diabetic Foot Ulcer: DR Surein PrasadDocument43 pagesDiabetic Foot Ulcer: DR Surein PrasadNinaNo ratings yet
- CME - Diabetic Foot UlcerDocument38 pagesCME - Diabetic Foot UlcerChuah Su WenNo ratings yet
- Managemen Kaki Diabetika Edit DesDocument44 pagesManagemen Kaki Diabetika Edit DesAsmawatiNo ratings yet
- Diabetic FootDocument4 pagesDiabetic FootSyurahbil Abdul Halim100% (1)
- Diabetic Foot UlcerDocument14 pagesDiabetic Foot UlcerRhomizal MazaliNo ratings yet
- Mohd Afiq Izzuddin Bin Rossli (1001336000) (Soft Tissue Swelling) 543. 15-16Document23 pagesMohd Afiq Izzuddin Bin Rossli (1001336000) (Soft Tissue Swelling) 543. 15-16Star CruiseNo ratings yet
- Knee ExaminationDocument54 pagesKnee ExaminationZed HarrisNo ratings yet
- IPT 12 Venous UlcersDocument41 pagesIPT 12 Venous UlcersLAL DIME 1No ratings yet
- Topic Confernce: Int Nontapat PaesarochDocument19 pagesTopic Confernce: Int Nontapat Paesarochnontapat paesarochNo ratings yet
- Bacterial Infection 2Document3 pagesBacterial Infection 2jihanNo ratings yet
- Ulceration and Ulcers: Ulceration - Is The Cellular Death of Superficial Tissue Leading ToDocument4 pagesUlceration and Ulcers: Ulceration - Is The Cellular Death of Superficial Tissue Leading ToAshref BelhajNo ratings yet
- Acute Purulent Diseases of Fingers and HandDocument9 pagesAcute Purulent Diseases of Fingers and Handvem_nikhil4uNo ratings yet
- SKINDocument12 pagesSKINJaleah Gwyneth Fernandez EdullantesNo ratings yet
- OsteoarthritisDocument25 pagesOsteoarthritisRaymund Christopher Dela PeñaNo ratings yet
- Hand ExamDocument49 pagesHand Examياسر نعيم الربيعيNo ratings yet
- Knee PainDocument34 pagesKnee Painmanoj ramlal kandoi100% (1)
- The Diabetic Foot: by Dr. Myrna Rita, SPRM Instalasi Rehabilitasi Medik Rsud A.W.Sjahranie, SamarindaDocument16 pagesThe Diabetic Foot: by Dr. Myrna Rita, SPRM Instalasi Rehabilitasi Medik Rsud A.W.Sjahranie, SamarindaDessy Vinoricka AndriyanaNo ratings yet
- 11 Diabetic FootDocument37 pages11 Diabetic Footkim suhoNo ratings yet
- Diabetic Foot Ulcers: Rapid ResponsesDocument5 pagesDiabetic Foot Ulcers: Rapid ResponsesLuis GarciaNo ratings yet
- NOTES of Management of Pressure UlcersDocument4 pagesNOTES of Management of Pressure UlcersD Dimpy ThakurNo ratings yet
- Diabetic Foot: Renaldi Rizky Mokh. AbdullahDocument17 pagesDiabetic Foot: Renaldi Rizky Mokh. AbdullahRenaldi RizkyNo ratings yet
- Approach To The Differential Diagnosis of Leg Ulcers - UpToDateDocument44 pagesApproach To The Differential Diagnosis of Leg Ulcers - UpToDatePriscillaNo ratings yet
- General OrthopaedicsDocument50 pagesGeneral Orthopaedicsضبيان فرحانNo ratings yet
- 6.dabetic FootDocument81 pages6.dabetic FootArleen MatincaNo ratings yet
- Rheumatoid Arthritis: Prevalence: Cause: Peak AgeDocument7 pagesRheumatoid Arthritis: Prevalence: Cause: Peak AgeAhmad ShaltoutNo ratings yet
- Decubitus UlcerDocument8 pagesDecubitus UlcerDanilo EspinoNo ratings yet
- Diabetic Foot CmeDocument29 pagesDiabetic Foot CmeAli emillyNo ratings yet
- Management of Open Fractures Prof A Sárváry Septic and Non Septic Complications in Traumatology Fractures of The Tibia and FibulaDocument52 pagesManagement of Open Fractures Prof A Sárváry Septic and Non Septic Complications in Traumatology Fractures of The Tibia and FibulaHurulaeniNo ratings yet
- Primary Oral UlcerationDocument41 pagesPrimary Oral Ulcerationاحمد العزكيNo ratings yet
- Diabetic FootDocument68 pagesDiabetic FootEndro Ri WibowoNo ratings yet
- Diabetic Foot, Diabetic Foot Ulcer & Diabetic Foot Care: Prepared by Munirah Supervised by DR NaqibDocument49 pagesDiabetic Foot, Diabetic Foot Ulcer & Diabetic Foot Care: Prepared by Munirah Supervised by DR NaqibAfifah SelamatNo ratings yet
- Chapter 14: The ArthropathiesDocument18 pagesChapter 14: The ArthropathiespoddataNo ratings yet
- Diabetic Foot History AND ExaminationDocument46 pagesDiabetic Foot History AND ExaminationRiaNo ratings yet
- Examination of Limb IschemiaDocument9 pagesExamination of Limb Ischemiaahmed ebrahimNo ratings yet
- NNNNNDocument11 pagesNNNNNAnonymous kdBDppigENo ratings yet
- Diabeticfootulcer Surgicalwounds 190908030737Document22 pagesDiabeticfootulcer Surgicalwounds 190908030737Jeevan VelanNo ratings yet
- Pyogenic Flexor Tenosynovitis PDFDocument6 pagesPyogenic Flexor Tenosynovitis PDFshiromiNo ratings yet
- FW2A AssignemntsDocument7 pagesFW2A Assignemntsekalvino1610No ratings yet
- Notes On AmputationsDocument3 pagesNotes On AmputationsShaileeNo ratings yet
- Diabetic Foot UlcerDocument22 pagesDiabetic Foot UlcerBaihaqi ReadsNo ratings yet
- DR Harikrishna - Management of Diabetic FootDocument89 pagesDR Harikrishna - Management of Diabetic FootAdrian Lim100% (3)
- 06 Skin Care, Aseptic Technique and Prevention For The Pressure UlcersDocument7 pages06 Skin Care, Aseptic Technique and Prevention For The Pressure Ulcers楊畯凱No ratings yet
- Newtem Name: Nursing Practice General SurgeryDocument19 pagesNewtem Name: Nursing Practice General SurgeryRitesh PalNo ratings yet
- Open FracturesDocument51 pagesOpen FracturesStar Cruise100% (1)
- Diabetic Foot Ulcer: Muhammad Mohsein Bin Kamarul BahrinDocument33 pagesDiabetic Foot Ulcer: Muhammad Mohsein Bin Kamarul BahrinNurul Nabilah AzraNo ratings yet
- Diabetic Foot: N. Craig Stone April 17, 2003Document47 pagesDiabetic Foot: N. Craig Stone April 17, 2003Gabriel KlemensNo ratings yet
- Fractures of FemurDocument25 pagesFractures of FemurJared NyakambaNo ratings yet
- 3 Essay OrthoDocument11 pages3 Essay Orthogamal attamNo ratings yet
- Management of Diabetic Foot Ulcers: Pandji MulyonoDocument51 pagesManagement of Diabetic Foot Ulcers: Pandji MulyonoJeffrey Dyer100% (1)
- A Simple Guide to Skin Fungal Infections, (Updated 2023) Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Skin Fungal Infections, (Updated 2023) Diagnosis, Treatment and Related ConditionsRating: 5 out of 5 stars5/5 (2)
- Atlas of Small Animal Wound Management and Reconstructive SurgeryFrom EverandAtlas of Small Animal Wound Management and Reconstructive SurgeryNo ratings yet
- Torque Spiral Wound GSKT TableDocument2 pagesTorque Spiral Wound GSKT TableCarlos Roberto Tamariz100% (1)
- CT Commercial Investment PropertiesDocument25 pagesCT Commercial Investment PropertiesbritalbNo ratings yet
- Unit-3 - Garden Design (Pages-32)Document25 pagesUnit-3 - Garden Design (Pages-32)siva ramanNo ratings yet
- Chapter 01 - Introduction To EaDocument18 pagesChapter 01 - Introduction To EaMrz RostanNo ratings yet
- Chapter 4 ProblemsDocument4 pagesChapter 4 ProblemsSteve DiazNo ratings yet
- FSC International StandardDocument15 pagesFSC International StandardEMINANo ratings yet
- CE PROJECT MidtermDocument5 pagesCE PROJECT MidtermAndrea A. IgupNo ratings yet
- Pattern, Price and Time - Using Gann TheoryDocument29 pagesPattern, Price and Time - Using Gann TheoryRohitOhri44% (9)
- A Call For A Temporary Moratorium On "The DAO"Document13 pagesA Call For A Temporary Moratorium On "The DAO"SoftpediaNo ratings yet
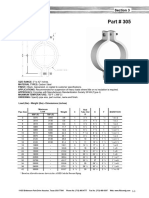
- Part 305 Heavy Pipe ClampDocument1 pagePart 305 Heavy Pipe ClampezhiljananiNo ratings yet
- ANT332 Answer Key 6Document3 pagesANT332 Answer Key 6mariefmuntheNo ratings yet
- AK Khan Telecom Limited: Orientation ScheduleDocument2 pagesAK Khan Telecom Limited: Orientation Schedulemozammel80No ratings yet
- General Biology 1: TEST II. Modified True or False. Indicate Whether The Statement Is True or False. If False, Change TheDocument2 pagesGeneral Biology 1: TEST II. Modified True or False. Indicate Whether The Statement Is True or False. If False, Change TheMA. HAZEL TEOLOGONo ratings yet
- Applied Economics ReportDocument16 pagesApplied Economics ReportJoyce Ann Agdippa Barcelona100% (1)
- Shreya Dikshit ISSNDocument16 pagesShreya Dikshit ISSNPratikNo ratings yet
- FCP Notes RevisedDocument34 pagesFCP Notes Revisedpavana.sNo ratings yet
- 0068 NehaDocument1 page0068 Nehang.neha8990No ratings yet
- Barangay Health Worker Registration FormDocument1 pageBarangay Health Worker Registration FormJairah Marie100% (2)
- CH 2 - Guide To Physics PracticalsDocument20 pagesCH 2 - Guide To Physics PracticalsNong Hm100% (2)
- Behavioral Modeling of A Comparator Using Verilig-AMSDocument88 pagesBehavioral Modeling of A Comparator Using Verilig-AMSPriNo ratings yet
- SPAR International Annual Report 2018 PDFDocument56 pagesSPAR International Annual Report 2018 PDFCristian Cucos CucosNo ratings yet
- Hands On 3.1 ActDocument7 pagesHands On 3.1 Actmarkkyle collantesNo ratings yet
- LAZUDAN ZEKRELLAH I. BSMT 2 BD WATCH 1 Semi Final Exam 1Document8 pagesLAZUDAN ZEKRELLAH I. BSMT 2 BD WATCH 1 Semi Final Exam 1Macxie Baldonado QuibuyenNo ratings yet
- 1-s2.0-S0079670005000122-main.pdf 二氧化碳開環聚合回顧文獻Document33 pages1-s2.0-S0079670005000122-main.pdf 二氧化碳開環聚合回顧文獻hungNo ratings yet
- 27 RevatiDocument4 pages27 RevatiOzy CanNo ratings yet
- Semantic Segmentation Data Labelling: Classes and InstructionsDocument9 pagesSemantic Segmentation Data Labelling: Classes and InstructionsMar FieldsNo ratings yet
- CIR v. Ace Saatch & Saatchi Advertising, Inc. (2017) PDFDocument36 pagesCIR v. Ace Saatch & Saatchi Advertising, Inc. (2017) PDFKriszan ManiponNo ratings yet
- Wa0009.Document2 pagesWa0009.Purahar sathyaNo ratings yet