Professional Documents
Culture Documents
Zegen Tablet
Zegen Tablet
Uploaded by
Ellain CaballeroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Zegen Tablet
Zegen Tablet
Uploaded by
Ellain CaballeroCopyright:
Available Formats
CLINICAL PHARMACOLOGY
PHARMACODYNAMICS
Cefuroxime, a semi-synthetic second generation cephalosporin which exerts its bactericidal activity by interfering with the bacterial cell wall
synthesis. It binds to specific penicillin-binding proteins responsible for the synthesis of peptidoglycan, a heteropolymeric structure that gives
the cell wall its mechanical stability. The final stage of the peptidoglycan synthesis involves the completion of the cross-linking of the terminal
glycine residue of the pentaglycine bridge to the fourth residue of the pentapeptide. The transpeptidase that catalyzes this step is inhibited
by cephalosporins. As a result, the bacterial cell wall is weakened, the cell swells and then ruptures.
ANTIMICROBIAL SPECTRUM OF ACTIVITY
The in vivo bactericidal activity of cefuroxime axetil is due to the parent compound cefuroxime.
Cefuroxime has demonstrated activity against most strains of the following microorganisms both in vitro and in clinical infections:
Anaerobic
Listeria monocytogenes and certain strains of enterococci, e.g., Enterococcus faecalis (formerly Streptococcus faecalis), are resistant to
cefuroxime. Methicillin-resistant staphylococci are resistant to cefuroxime.
Pseudomonas spp., Campylobacter spp., Acinetobacter calcoaceticus, Legionella spp., and most strains of Serratia spp. and Proteus
vulgaris are resistant to most first- and second-generation cephalosporins. Some strains of Morganella morganii, Enterobacter cloacae, and
Citrobacter spp. have been shown by in vitro tests to be resistant to cefuroxime and other cephalosporins.
Most strains of Clostridium difficile and Bacteroides fragilis are resistant to cefuroxime.
PHARMACOKINETICS
Cefuroxime's apparent volume of distribution in healthy adults ranges from 9.3 to 15.8 L per 1.73 m2. Cefuroxime is widely distributed in the
body including pleural fluid, sputum, bone, synovial fluid, and aqueous humor, but only achieves therapeutic concentrations in the
cerebrospinal fluid when the meninges are inflamed. Cefuroxime is 33-50% protein-bound.
Cefuroxime readily crosses the placenta and can also be detected in human milk.
In adults, the serum or plasma half-life (t½) after oral administration of cefuroxime axetil ranges from 1.2 to 1.6 hours and about 50% of an
administered dose is recovered in the urine within 12 hours.
Following oral administration of cefuroxime axetil, the drug undergoes rapid hydrolysis by nonspecific esterases in the intestinal mucosa
and blood to yield the active parent drug cefuroxime, which is released into the systemic circulation.
The axetil moiety of the drug is metabolized to acetaldehyde and acetic acid. Cefuroxime itself is not metabolized and its serum level is
much closer to the minimum inhibitory concentration (MIC) of important pathogens than cefuroxime axetil.
Cefuroxime is excreted unchanged primarily in the urine by both glomerular filtration and tubular secretion.
In patients with renal impairment, the serum t½ of the drug is prolonged and generally ranges from 1.9-16.1 hours depending on the degree
of renal impairment.
Cefuroxime is removed by hemodialysis and by peritoneal dialysis.
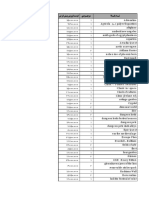
R e c o m m e n d e d D o se
(T o b e ta k e n o ra lly a fte r m e a ls ) D u ra tio n
In fe c tio n s C h ild re n 7 to 12 A d u lts a n d of
y e a rs o ld A d o le s c e n ts (1 3 T re a tm e n t
(W h o c a n s w a llo w y e a rs a n d o ld e r) (d a y s )
ta b le t w h o le )
250 m g 2 5 0 m g o r 50 0 m g
A cu te sin u sitis 10
e ve ry 1 2 h o u rs e ve ry 1 2 h ou rs
250 m g 500 m g
A cu te o titis m e d ia 10
e ve ry 1 2 h ou rs e ve ry 1 2 h ou rs
250 m g 2 5 0 m g o r 50 0 m g
A cu te to n sillop h a ryn g itis 10
e ve ry 1 2 h o u rs e ve ry 1 2 h ou rs
250 m g 2 5 0 m g o r 50 0 m g
A cu te b a cte ria l e xa ce rb a tion s o f ch ro n ic b ro n ch itis 10*
e ve ry 1 2 h o u rs e ve ry 1 2 h ou rs
250 m g 2 5 0 m g o r 50 0 m g
S e co nd a ry b a cte ria l in fe ction s o f a cu te b ron ch itis 5 -1 0
e ve ry 1 2 h ou rs e ve ry 1 2 h ou rs
250 m g 2 5 0 m g o r 50 0 m g
U n co m p lica te d skin a n d skin stru ctu re in fe ctio n s 10
e ve ry 1 2 h ou rs e ve ry 1 2 h ou rs
250 m g 2 5 0 m g o r 50 0 m g
U n co m p lica te d u rin a ry tra ct in fe ction s 7 -1 0
e ve ry 1 2 h o u rs e ve ry 1 2 h ou rs
U n co m p lica te d go n o rrhe a (-) 1 ,0 00 m g o n ce S in g le D o se
250 m g 500 m g
E a rly L ym e D ise a se 20
e ve ry 1 2 h ou rs e ve ry 1 2 h ou rs
O r, a s p re scribe d b y a p h ysicia n
Known hypersensitivity to cefuroxime, cephalosphorins, penicillins, or any component of the product.
·Careful inquiry should be made prior to cefuroxime therapy to determine whether the patient has had previous hypersensitivity
reactions to cefuroxime, other cephalosporins, penicillins, or other drugs. Use with caution in penicillin-sensitive patients since
cross-sensitivity among beta-lactam antibiotics has been clearly documented and may occur in patients with a history
of allergy to penicillin. In case of an allergic reaction to cefuroxime, the drug should be discontinued.
Serious acute hypersensitivity reactions may require treatment with epinephrine and other emergency measures including oxygen,
intravenous fluids, corticosteroids, pressor amines, and airway management, as clinically indicated.
·Clostridium difficile-associated diarrhea (CDAD) and colitis have been reported with the use of nearly all antibacterial agents, including
cefuroxime, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters the normal flora of the
colon leading to overgrowth of C. difficile.
C. difficile produces toxins A and B which contribute to the development of CDAD. Hypertoxin-producing strains of C. difficile cause
increased morbidity and mortality, as these infections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be
considered in all patients who present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been
reported to occur over two months after the administration of antibacterial agents.
If CDAD is suspected or confirmed, ongoing antibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and
electrolyte management, protein supplementation, antibiotic treatment of C. difficile, and surgical evaluation should be instituted as clinically
indicated.
·Cefuroxime should not be used in patients with a history of cephalosphorin-associated hemolytic anemia since the recurrence of
hemolysis is much more severe.
If a patient develops anemia anytime during, or within 2 to 3 weeks subsequent to the administration of cefuroxime, the diagnosis of
cephalosphorin-associated anemia should be considered and the drug discontinued until the etiology is determined.
Periodic monitoring for signs and symptoms of hemolytic anemia, including measurement of hematological parameters of drug-induced
antibody testing is recommended in patients treated with cefuroxime.
·As with other broad-spectrum antibacterial agents, cefuroxime should be used with caution in patients with a history of gastrointestinal
disease, particularly colitis.
·Cephalosporins, including cefuroxime, have been associated with the development of seizures, particularly in patients with renal impairment,
in whom dosage of the drug was not reduced. If seizures due to cefuroxime develop, the drug should be discontinued and treatment with an
anticonvulsant be given as clinically indicated.
·Cephalosporins may be associated with a fall in prothrombin activity. Patients who are at risk are those with renal or hepatic impairment or
poor nutritional state, as well as patients receiving a protracted course of antimicrobial therapy, and patients previously stabilized on
anticoagulant therapy. Prothrombin time should be monitored in patients at risk and exogenous Vitamin K administered as indicated.
·The patient's renal function should be carefully monitored when cefuroxime is given concurrently with aminoglycosides and/or diuretics
because adverse renal effects may occur [see Interactions with Other Medicaments].
·The Jarisch-Herxheimer reaction, a transient immunological reaction lasting 1 to 2 days, has been observed following cefuroxime treatment
of Lyme disease. Patients should be reassured that this is a common and usually a self-limiting consequence of antibiotic treatment of Lyme
disease.
·Cefuroxime has been used safely in a few patients with porphyria although data are insufficient and experimental evidence of
porphyrinogenicity are conflicting.
·Prescribing cefuroxime in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide
benefit to the patient and increases the risk of antibiotic resistance.
·As with other antibacterial agents, long term or repeated use may result in overgrowth of non-susceptible organisms, including fungi.
Carcinogenesis, Mutagenesis, Impairment of Fertility:
The carcinogenic potential of cefuroxime has not been evaluated in long-term animal studies.
No evidence of mutagenicity was observed with cefuroxime in various in vitro and in vivo test systems, including the mouse lymphoma
assay, micronucleus test, and bacterial mutation tests. Cefuroxime produced positive results in the in vitro chromosome aberration assay.
There are no adequate and controlled studies using cefuroxime in pregnant women. Cefuroxime axetil has not been studied for use during
labor and delivery. Since cefuroxime is distributed into milk, cefuroxime axetil should be used with caution in breastfeeding women.
Effects on Ability to Drive and Use Machines: Since cefuroxime may cause dizziness, patients should be advised to avoid performing
tasks which require complete mental alertness such as driving and operating machinery.
·A false-positive reaction for glucose in the urine may occur with copper reduction tests (Benedict's or Fehling's solution or with Clinitest®
Tablets), but not with enzyme-based tests for glycosuria (e.g., Clinistix , Tes-Tape ).
® ®
·As a false-negative result may occur in the ferricyanide test, it is recommended that either the glucose oxidase or hexokinase method be
used to determine blood/plasma glucose levels in patients receiving cefuroxime.
·The presence of cefuroxime does not interfere with the assay of serum and urine creatinine by the alkaline picrate method.
·Positive direct antiglobulin (Coombs') test results have also been reported in a few patients receiving oral cefuroxime; however, it is not
clear whether the mechanism of this reaction is immunologic in nature. This phenomenon can interfere with cross matching of blood.
STATEMENT ON USAGE FOR HIGH RISK GROUPS
Pregnancy: (Pregnancy Category B) - Since there are no adequate and well controlled studies to date using cefuroxime in pregnant
women, use in pregnancy only if the potential benefit justifies the potential risk to the fetus.
Lactation: Cefuroxime is distributed into human milk and should be used with caution in breastfeeding women.
Children: The safety and efficacy of cefuroxime axetil in children younger than 3 months old have not been established.
Elderly: There are no apparent differences in efficacy and safety of cefuroxime between the elderly and younger adults. However, since
elderly patients have increased risk of renal impairment, dose adjustment and renal function monitoring may be necessary.
Renal Impairment: The safety and efficacy of oral cefuroxime axetil in patients with renal impairment have not been established. Since
cefuroxime is renally eliminated, its half-life will be prolonged in patients with reduced renal function.
The following adverse events have been reported with the use of cefuroxime, although in many instances the causal relationship to the
drug has not been established:
Dermatologic / Hypersensitivity Reaction: Rash (e.g., morbilliform), hives, erythema, pruritus, urticaria, drug fever, anaphylaxis (very
rarely), angioedema, serum sickness-like reaction, erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis
(exanthemic necrolysis), shortness of breath and severe bronchospasm
Gastrointestinal (GI): Diarrhea or loose stools, nausea, vomiting, abdominal pain/cramps, gagging, epigastric burning, epigastric pain/
dyspepsia, flatulence, indigestion, GI bleeding, mouth ulcers, swollen tongue, dislike of taste, stomach cramps, anorexia, thirst, GI infection,
ptyalism, pseudomembranous colitis
Genitourinary: Urethral pain or bleeding, kidney pain, urinary tract infection, dysuria, acute renal failure/dysfunction, interstitial nephritis,
transient increases in blood urea nitrogen (BUN) and serum creatinine concentrations; decreased creatinine clearance; bilateral renal
cortical necrosis, vaginitis, vaginal candidiasis, vulvovaginal pruritus, vaginal discharge or irritation, menstrual irregularities
Hematologic: Eosinophilia, neutropenia, hemolytic anemia, leukopenia, pancytopenia, thrombocytopenia, thrombocytosis, lymphocytosis;
increased prothrombin time; increased erythrocyte sedimentation rate, decreased hemoglobin and/or hematocrit, positive Coombs' test
Hepatic: Transient elevations in aspartate aminotransferase (AST), alanine aminotransferase (ALT), γ-glutamyl transferase, alkaline
phosphatase, lactate dehydrogenase (LDH), and bilirubin; jaundice, hepatic impairment including hepatitis and cholestasis, decreased
serum albumin and/or total protein
Musculoskeletal: Muscle spasm of the neck, muscle cramps or stiffness, arthralgia/joint pain or swelling
Nervous System: Headache, dizziness, somnolence/ sleepiness, irritable behavior, seizures, myoclonic jerks, generalized
hyperexcitability/hyperactivity
Respiratory: Pleural effusion, pulmonary infiltrate, dyspnea or respiratory distress, upper respiratory infection, rhinitis, sinusitis, cough
Cardiovascular: Chest pain or tightness, tachycardia
Other Adverse Effects: Jarisch-Herxheimer reaction in patients treated for Lyme disease, candidiasis/candida overgrowth, mild to severe
hearing loss, increased or decreased serum glucose concentration, lockjaw-type reaction, viral illness
Cefuroxime (Zegen) 250 mg tablet box of 100’s (in alu-alu foil blister x 4’s): DR-XY38616
Cefuroxime (Zegen) 500 mg tablet box of 60’s (in alu-alu foil blister x 4’s): DR-XY38617
For suspected adverse drug reaction, seek medical attention immediately and
report to the FDA at www.fda.gov.ph AND Unilab at (+632) 858-1000 or
productsafety@unilab.com.ph. By reporting undesirable effects, you can help
provide more information on the safety of this medicine.
Manufactured by NECTAR LIFESCIENCES LIMITED
Unit-VI, Village: Bhatolikalan, adjoining Jharmajri, E.P.I.P.
Post Office: Barotiwala, Tehsil: Nalagarh, District: Solan
Himachal Pradesh - 173205, India
Imported and Distributed by UNILAB, Inc.
No. 66 United Street, Mandaluyong City, Metro Manila, Philippines
Date of Revision: 07/2018
Reg. IPOPHIL
Date of First Authorization: Zegen 250 mg Tab: 10/2010 UA153571IN03
Zegen 500 mg Tab: 10/2010
You might also like
- Aqa A Level Biology p1 QPDocument36 pagesAqa A Level Biology p1 QPJaden MistryNo ratings yet
- (Cambridge Manuals in Archaeology) R Lee Lyman-Vertebrate Taphonomy-Cambridge University Press (1994)Document549 pages(Cambridge Manuals in Archaeology) R Lee Lyman-Vertebrate Taphonomy-Cambridge University Press (1994)Danny Florest100% (3)
- CArolina S. AGRAvanteDocument37 pagesCArolina S. AGRAvanteEllain CaballeroNo ratings yet
- Physics: FlashbackDocument2 pagesPhysics: FlashbackWonderlapseNo ratings yet
- امتحانات الكترونيه PDFDocument10 pagesامتحانات الكترونيه PDFAli AhmedNo ratings yet
- Barracuda SantosDocument238 pagesBarracuda Santoscasadosparafusos.jsNo ratings yet
- 39760Document4 pages39760RUMBIDZAI MARAWANo ratings yet
- Turunkan Kolesterol Anda: Disarikan Dari Sumber Di Internet AWM ForeverDocument24 pagesTurunkan Kolesterol Anda: Disarikan Dari Sumber Di Internet AWM ForeverGias Maheyssa AmarullahNo ratings yet
- 6 RX 6 Rs 6 SRDocument4 pages6 RX 6 Rs 6 SRMark J AbarracosoNo ratings yet
- Introduction HandoutDocument3 pagesIntroduction Handoutathenalavega100% (1)
- Anatomic Sciences EDITDocument214 pagesAnatomic Sciences EDITreviewer.email001No ratings yet
- Fizika M 2015Document19 pagesFizika M 2015Dachi VartagavaNo ratings yet
- List ContactsDocument9 pagesList ContactsrobertthomaswhiteNo ratings yet
- Manual TsoDocument33 pagesManual TsoFrancisco de Assis Domingos PenhaNo ratings yet
- BS 4659 1989 Specification For Tool and Die SteelsDocument22 pagesBS 4659 1989 Specification For Tool and Die SteelsLeon MarcoNo ratings yet
- Pasal Time Table MPV Banner 2023Document1 pagePasal Time Table MPV Banner 20233MANANo ratings yet
- Produktdatenblatt BIKUTEC V60Document1 pageProduktdatenblatt BIKUTEC V60stebeb800No ratings yet
- Intuitionistic Logic Constructive LogicDocument13 pagesIntuitionistic Logic Constructive Logic'Prasada WedatamaNo ratings yet
- 24 Z Pan PDFDocument7 pages24 Z Pan PDFhimamahanNo ratings yet
- قانون ضریبة الدخلDocument58 pagesقانون ضریبة الدخلJCPAJONo ratings yet
- T T T T: Scanned by CamscannerDocument24 pagesT T T T: Scanned by CamscannerTriveniTammuNo ratings yet
- Productivity RatesDocument2 pagesProductivity RatesAnonymous M6O8URiNo ratings yet
- Alsun Floordeck FD-1000Document4 pagesAlsun Floordeck FD-1000Teknik produksi wikonNo ratings yet
- and 55011 Conducted EmissionsDocument21 pagesand 55011 Conducted EmissionssnfulNo ratings yet
- قانون الضریبة العامة علی المبیعاتDocument88 pagesقانون الضریبة العامة علی المبیعاتJCPAJONo ratings yet
- Brosur Mini BankerDocument2 pagesBrosur Mini BankerRama Asmara TariganNo ratings yet
- PDF New Makalah Krisis Hipertensi CompressDocument22 pagesPDF New Makalah Krisis Hipertensi CompressLionel IboyNo ratings yet
- Compare Mineral WaterDocument1 pageCompare Mineral WaterDanang NCONo ratings yet
- Rotated 61000-4-11 Immunity To Ac Supply Dips Dropouts InterruptionsDocument13 pagesRotated 61000-4-11 Immunity To Ac Supply Dips Dropouts InterruptionsShawn DeolNo ratings yet
- Analysis of Molybdenite Bioleaching by Thiobacillus Ferrooxidans in The Absence of Iron (Ii)Document6 pagesAnalysis of Molybdenite Bioleaching by Thiobacillus Ferrooxidans in The Absence of Iron (Ii)kmirjaliliNo ratings yet
- MenuDocument1 pageMenudwi mutiaNo ratings yet
- Reactor: UDC 621.039.534.44:620.193o23Document5 pagesReactor: UDC 621.039.534.44:620.193o23sum74316No ratings yet
- Lao Phrasebook PDFDocument159 pagesLao Phrasebook PDFAmido Hernan Rios OvalleNo ratings yet
- The REG Procedure Model: MODEL1 Dependent Variable: y The REG Procedure Model: MODEL1 Dependent Variable: yDocument4 pagesThe REG Procedure Model: MODEL1 Dependent Variable: y The REG Procedure Model: MODEL1 Dependent Variable: yveechowNo ratings yet
- MAS P Math1 March2545Document10 pagesMAS P Math1 March2545rtafa qaNo ratings yet
- Aniı Isis PDocument42 pagesAniı Isis PNubia Alejandro HernandezNo ratings yet
- Control SystemsDocument39 pagesControl SystemsKrushnasamy SuramaniyanNo ratings yet
- Contribution Breakdown Graduation and JSDocument5 pagesContribution Breakdown Graduation and JSRussell SanicoNo ratings yet
- Labour Productivity and Rate AnalysisDocument6 pagesLabour Productivity and Rate AnalysisGanesh Un100% (1)
- A Practical Guide For EN 61000-3-3 and EN 61000-3-11 - Electromagnetic CompatibilityDocument15 pagesA Practical Guide For EN 61000-3-3 and EN 61000-3-11 - Electromagnetic CompatibilityanilNo ratings yet
- 3GS BrochureDocument3 pages3GS BrochureIsaac Joshua EscañoNo ratings yet
- Jeep WJ 2000Document220 pagesJeep WJ 2000djgibus0% (1)
- Indore Presentation - 23.02.15Document48 pagesIndore Presentation - 23.02.15arthiarulNo ratings yet
- Et Al. Macaca Fascicularis: 0 1 O0 200 3 O0 I I I 30Document1 pageEt Al. Macaca Fascicularis: 0 1 O0 200 3 O0 I I I 30AkicaNo ratings yet
- Labour OutputDocument9 pagesLabour Outputanand_parchureNo ratings yet
- TUGAS DATA MINING NadyaDocument7 pagesTUGAS DATA MINING Nadyahanny davNo ratings yet
- 1 EstrellitaDocument2 pages1 EstrellitaAgustín GonzálezNo ratings yet
- Bey A2 VocabEx Wsh2Document1 pageBey A2 VocabEx Wsh2Wayra BANo ratings yet
- Modifiwd Zoology MSC Vsu SyllabusDocument30 pagesModifiwd Zoology MSC Vsu SyllabusNarasimha MurthyNo ratings yet
- موجودی بازی خارجی 29 خردادDocument4 pagesموجودی بازی خارجی 29 خردادfardad shirinichNo ratings yet
- T 3 H M M K 7: TT T T T T T TDocument4 pagesT 3 H M M K 7: TT T T T T T Tmohdwajid2009No ratings yet
- Chapter 4 - Water Quality: ElectronDocument14 pagesChapter 4 - Water Quality: ElectronshrutiNo ratings yet
- Science Paper MT 1Document4 pagesScience Paper MT 1Rashmi MAAM 748No ratings yet
- Windsurfing: 1 Look, Find and Circle. Then Look and Find Other English Words You KnowDocument17 pagesWindsurfing: 1 Look, Find and Circle. Then Look and Find Other English Words You KnowJesús Box Soler100% (1)
- Machine DesignDocument463 pagesMachine DesignReymart Ebora100% (4)
- T" Ii M', N, I I Tlilltll: Isothermal Treatment OF AlloyDocument3 pagesT" Ii M', N, I I Tlilltll: Isothermal Treatment OF AlloySinhro018No ratings yet
- Redspot Physics 1000 MCQsDocument258 pagesRedspot Physics 1000 MCQsAndrew NyanhowoNo ratings yet
- Jadavp Ur Univ Ersit Y Dec Ent Ralized V Acant S E at Mat Rix (Se at S Offered According T O Wbjee-2 019 Rank)Document1 pageJadavp Ur Univ Ersit Y Dec Ent Ralized V Acant S E at Mat Rix (Se at S Offered According T O Wbjee-2 019 Rank)Lakkhi ShawNo ratings yet
- AndDocument1 pageAndzyrussiNo ratings yet
- 2024 - 03 - 00 Globa LaviatorDocument78 pages2024 - 03 - 00 Globa Laviator9g694mq27fNo ratings yet
- Problem Set in Boyle: 1 L G WHDocument1 pageProblem Set in Boyle: 1 L G WHKENT 45No ratings yet
- LESSON 01 ANSWER SHEET - Caballero, Ellain C.Document2 pagesLESSON 01 ANSWER SHEET - Caballero, Ellain C.Ellain CaballeroNo ratings yet
- Peste KaDocument1 pagePeste KaEllain CaballeroNo ratings yet
- Lesson 01 Answer SheetDocument2 pagesLesson 01 Answer SheetEllain CaballeroNo ratings yet
- HeragestDocument1 pageHeragestEllain CaballeroNo ratings yet
- PravazDocument1 pagePravazEllain CaballeroNo ratings yet
- ZeptrigenDocument1 pageZeptrigenEllain CaballeroNo ratings yet
- FunxionDocument1 pageFunxionEllain CaballeroNo ratings yet
- ZoldemDocument1 pageZoldemEllain CaballeroNo ratings yet
- Solmux Adult Suspension PILDocument1 pageSolmux Adult Suspension PILEllain CaballeroNo ratings yet
- SoniphenDocument1 pageSoniphenEllain CaballeroNo ratings yet
- Plogrel 799Document1 pagePlogrel 799Ellain CaballeroNo ratings yet
- LovorinDocument1 pageLovorinEllain CaballeroNo ratings yet
- Rythma IVDocument1 pageRythma IVEllain CaballeroNo ratings yet
- Montra 966Document1 pageMontra 966Ellain CaballeroNo ratings yet
- Bill of RightsDocument37 pagesBill of RightsEllain CaballeroNo ratings yet
- Zenith TabletDocument1 pageZenith TabletEllain CaballeroNo ratings yet
- MeropDocument1 pageMeropEllain CaballeroNo ratings yet
- Zyra Front PageDocument3 pagesZyra Front PageEllain CaballeroNo ratings yet
- Lesson 1 Elements and Principles of Visual Arts PDFDocument14 pagesLesson 1 Elements and Principles of Visual Arts PDFEllain CaballeroNo ratings yet
- Ginisang Sitaw at Kalabasa - 45: Kaldereta - 50Document1 pageGinisang Sitaw at Kalabasa - 45: Kaldereta - 50Ellain CaballeroNo ratings yet
- Acute Viral Gastroenteritis in Adults - UpToDateDocument14 pagesAcute Viral Gastroenteritis in Adults - UpToDatedaniso12No ratings yet
- Healthcare Associated InfectionDocument11 pagesHealthcare Associated InfectionPankajNo ratings yet
- eMRCS Microbiology 19 QuestionsDocument7 pageseMRCS Microbiology 19 QuestionsSaad KhanNo ratings yet
- Complete Bacteriology Notes From Levinson by Medical Study CenterDocument13 pagesComplete Bacteriology Notes From Levinson by Medical Study CenterUsama HameedNo ratings yet
- Infection Prevention and Control Prsactices 1570477491 PDFDocument29 pagesInfection Prevention and Control Prsactices 1570477491 PDFLarr SumalpongNo ratings yet
- Collection and Transportation of Microbiology SpecimensDocument4 pagesCollection and Transportation of Microbiology SpecimensanupreetNo ratings yet
- Etiology: 1.urinary RetentionDocument38 pagesEtiology: 1.urinary RetentionAbdurre YNo ratings yet
- Management of Acute Chemotherapy-Related Diarrhea - UpToDateDocument19 pagesManagement of Acute Chemotherapy-Related Diarrhea - UpToDateMarius PapuricaNo ratings yet
- Esomeprazole Tablets GranulesDocument57 pagesEsomeprazole Tablets GranulesMohammed shamiul ShahidNo ratings yet
- Micro - Systemic Bacteriology Questions PDFDocument79 pagesMicro - Systemic Bacteriology Questions PDFShashipriya AgressNo ratings yet
- NMC CBT Mock Test 2Document13 pagesNMC CBT Mock Test 2Charles Osiako100% (3)
- PDF Share Prescribing Information: Mechanism of ActionDocument3 pagesPDF Share Prescribing Information: Mechanism of Actionmehul da aviatorNo ratings yet
- Mtap-Bacte-Ratio-11-19-22 2Document9 pagesMtap-Bacte-Ratio-11-19-22 2lansangan.regine.coeliNo ratings yet
- 2013 AAFP Acute Diarrhea PDFDocument11 pages2013 AAFP Acute Diarrhea PDFJoseph AndradeNo ratings yet
- Xenex Effectiveness Summary Studies PDFDocument4 pagesXenex Effectiveness Summary Studies PDFREDENLAKE LTDNo ratings yet
- Pharmacological and Parenteral TherapiesDocument99 pagesPharmacological and Parenteral TherapieslNo ratings yet
- Assessing With EliminationDocument79 pagesAssessing With EliminationhalayehiahNo ratings yet
- Clindamycin 1Document21 pagesClindamycin 1ksachchuNo ratings yet
- Nutrition Pathway For Clostridium Difficile Infection (CDI) Colitis in Long-Term CareDocument4 pagesNutrition Pathway For Clostridium Difficile Infection (CDI) Colitis in Long-Term CareDavide CezarNo ratings yet
- Gastroenteritis: Saima Alam AfridiDocument23 pagesGastroenteritis: Saima Alam AfridiMahnoor ParvezNo ratings yet
- History of Hospital-Acquired InfectionsDocument16 pagesHistory of Hospital-Acquired InfectionsRasha MuhammadNo ratings yet
- Lec4 TransDocument23 pagesLec4 TransErika PatarayNo ratings yet
- Chapter 43 - Miscellaneous Bacterial Infections of GITDocument52 pagesChapter 43 - Miscellaneous Bacterial Infections of GITpooja pandeyNo ratings yet
- Symptoms of ColitisDocument5 pagesSymptoms of ColitisChatrina TandiloloNo ratings yet
- Ciprofloxacin TAB MonographDocument56 pagesCiprofloxacin TAB MonographSelvi RahmatiaNo ratings yet
- UW Infectious Diseases + Microbiology Educational Objectives PDFDocument75 pagesUW Infectious Diseases + Microbiology Educational Objectives PDFDrbee10No ratings yet
- The Gram-Positive Bacilli of Medical Importance: Group 5Document148 pagesThe Gram-Positive Bacilli of Medical Importance: Group 5Tolentino, Ma. LykaNo ratings yet
- Jase Medical Antibiotic GuideDocument33 pagesJase Medical Antibiotic GuideelectronicoscaldasNo ratings yet
- Ranicef Tablets Cefdinir Tablets 300MG FidsonDocument13 pagesRanicef Tablets Cefdinir Tablets 300MG FidsonWright JohnNo ratings yet