Professional Documents
Culture Documents
Nursing Procedures
Nursing Procedures
Uploaded by
Irene Grace BalcuevaCopyright:
Available Formats
You might also like
- Manual of Operations For Drug Testing LaboratoriesDocument24 pagesManual of Operations For Drug Testing LaboratoriesSarah Jane V. Denia100% (6)
- Rodak Questions CompilationDocument40 pagesRodak Questions CompilationGertrudeshane IletoNo ratings yet
- CSF SopDocument19 pagesCSF SopdeblackaNo ratings yet
- Questionnaire (HTMLE)Document16 pagesQuestionnaire (HTMLE)Angelo Mercede100% (1)
- MT113BL Analysis of Urine and Other Body Fluids ManualDocument28 pagesMT113BL Analysis of Urine and Other Body Fluids ManualAsxe Cee100% (1)
- PCP Obe-Cbtp Dops Rtp-Acc Form#7Document6 pagesPCP Obe-Cbtp Dops Rtp-Acc Form#7Ko HakuNo ratings yet
- CLINICAL PRACTICUM Activity Book Revised 2014Document17 pagesCLINICAL PRACTICUM Activity Book Revised 2014helpNo ratings yet
- Learning Activity No. 7Document15 pagesLearning Activity No. 7Gabrielle SerenoNo ratings yet
- 2016 ACHE Healthcare Executie Competencies Assessment ToolDocument28 pages2016 ACHE Healthcare Executie Competencies Assessment ToolragcajunNo ratings yet
- BS en 13478 Fire Prevention and ProtectionDocument30 pagesBS en 13478 Fire Prevention and Protectiontoalok4723No ratings yet
- Checklist On Vital Signs - Blood Oxygenation Using Pulse OxymeterDocument2 pagesChecklist On Vital Signs - Blood Oxygenation Using Pulse Oxymeteraliyah2 sanchezNo ratings yet
- Immunohema Lab ActivitiesDocument46 pagesImmunohema Lab ActivitiesMushu MunuNo ratings yet
- Course Syllabus PLAB 1223 - Phlebotomy: WWW - Panola.eduDocument12 pagesCourse Syllabus PLAB 1223 - Phlebotomy: WWW - Panola.edukisserie licyayoNo ratings yet
- Nursingbullets: Respiratory System - Diagnostic ProceduresDocument41 pagesNursingbullets: Respiratory System - Diagnostic ProceduresErmadutz Sumampong FernandezNo ratings yet
- Respiratory Diagnostic ProceduresDocument41 pagesRespiratory Diagnostic Proceduresseigelystic100% (23)
- Respiratory System Diagnostic Procedures: Marjorie V. Aguinaldo RN, MANDocument32 pagesRespiratory System Diagnostic Procedures: Marjorie V. Aguinaldo RN, MANKun KandaNo ratings yet
- Blood Pressure ChecklistDocument2 pagesBlood Pressure ChecklistKatherine bundalianNo ratings yet
- Tugas Kelompok 2 BHS Inggris SopDocument17 pagesTugas Kelompok 2 BHS Inggris Sopmoms naraNo ratings yet
- Oxygen Saturation ChecklistDocument2 pagesOxygen Saturation ChecklistPatrick SantosNo ratings yet
- CHECKLIST Performing Clinical Electrocardiography ECGDocument3 pagesCHECKLIST Performing Clinical Electrocardiography ECGTriciaNo ratings yet
- Surgical Skin Prep PDFDocument12 pagesSurgical Skin Prep PDFDrrjdrjd MemeNo ratings yet
- Kashi PanchakamDocument2 pagesKashi PanchakamAnandNo ratings yet
- Is Lab. Activity 1 ETSDocument6 pagesIs Lab. Activity 1 ETSJuren LasagaNo ratings yet
- SL Evaluation Sheet Vital SignsDocument5 pagesSL Evaluation Sheet Vital SignsJoycee BoNo ratings yet
- Clinical Skill Manual of Gastrointestinal System 1819Document24 pagesClinical Skill Manual of Gastrointestinal System 1819SalmaNo ratings yet
- NCM 109 B Checklist of Procedures 1Document26 pagesNCM 109 B Checklist of Procedures 1manolbatindaan13No ratings yet
- 3obtaining Vital SignsDocument5 pages3obtaining Vital Signscharlotejeanbalanon1No ratings yet
- FTC SCRIPT O2 ADDocument2 pagesFTC SCRIPT O2 ADJUSTIN ALZATENo ratings yet
- Model Answer of Formative Written OSCADocument6 pagesModel Answer of Formative Written OSCAAhmed SamahaNo ratings yet
- Module 5 SuctioningDocument2 pagesModule 5 SuctioningDcimasaNo ratings yet
- Intubation ProcedureDocument6 pagesIntubation ProceduresinasinaaiNo ratings yet
- NCM 116b Checklist of ProceduresDocument44 pagesNCM 116b Checklist of ProceduresRhu PastranaNo ratings yet
- Sample QuestionsDocument15 pagesSample QuestionsAnonymous MtKJkerbpUNo ratings yet
- CC2433 Skill Performance Checklist Lab 2 2009Document5 pagesCC2433 Skill Performance Checklist Lab 2 2009twy113No ratings yet
- 6 ETS VenipunctureDocument7 pages6 ETS VenipunctureMyedelle SeacorNo ratings yet
- Or ExamDocument21 pagesOr Examlouie roderosNo ratings yet
- 100Document48 pages100Jerome JucutanNo ratings yet
- Emt BLS SkillsDocument45 pagesEmt BLS SkillsCHEN GAONo ratings yet
- 2007 NleDocument18 pages2007 NlealexisalvioNo ratings yet
- Equ10-04 Micro QC - Eqpt Maint SOPDocument7 pagesEqu10-04 Micro QC - Eqpt Maint SOPpokhara144No ratings yet
- Outlines: Arterial Blood GasesDocument9 pagesOutlines: Arterial Blood GasesToka HessenNo ratings yet
- O2 Therapy ChecklistDocument3 pagesO2 Therapy ChecklistKathlyn PactorananNo ratings yet
- PerioperativeDocument37 pagesPerioperativemj CanilangNo ratings yet
- Name: Section: Date PerformedDocument2 pagesName: Section: Date PerformedMaelyn Avanceña DujaleNo ratings yet
- AVOX July2011Document6 pagesAVOX July2011Kriss JonesNo ratings yet
- Lab Manual CSI103Document30 pagesLab Manual CSI103Nurul AinNo ratings yet
- Soal Perioperative Eng VersionDocument22 pagesSoal Perioperative Eng VersionZulaikah Nur IstiqomahNo ratings yet
- Arterial Line Placement (Adult)Document5 pagesArterial Line Placement (Adult)Sayan ChattopadhyayNo ratings yet
- Medical-Surgical Nusing Checklist: Conams Wesleyan University Philippines 2020-2021Document3 pagesMedical-Surgical Nusing Checklist: Conams Wesleyan University Philippines 2020-2021Kobe ManuelNo ratings yet
- Chapter 4 Vital SignsDocument11 pagesChapter 4 Vital SignsNila ManguerraNo ratings yet
- NCM 112 Lesson5Document6 pagesNCM 112 Lesson5Trisha LopezNo ratings yet
- Kewenangan Klinis KMB PK IIIDocument11 pagesKewenangan Klinis KMB PK IIImiraNo ratings yet
- Transfusion SpecimenCollectionDocument5 pagesTransfusion SpecimenCollectionDominic EmerencianaNo ratings yet
- I. Desired Learning OutcomesDocument7 pagesI. Desired Learning OutcomesMaelyn Avanceña DujaleNo ratings yet
- SuturingDocument3 pagesSuturingKiran RamloganNo ratings yet
- RPSGT Exam BlueprintDocument2 pagesRPSGT Exam BlueprintKarloveyNo ratings yet
- PCCN BipapDocument15 pagesPCCN Bipapkarthikayini3590No ratings yet
- Surg SGD Topics PrelimsDocument2 pagesSurg SGD Topics PrelimsMariana B.No ratings yet
- Collecyion SpecimenDocument52 pagesCollecyion Specimenرافت العواضيNo ratings yet
- Files of Accreditation 2016 2017 2Document309 pagesFiles of Accreditation 2016 2017 2Lovelie Grace GalarpeNo ratings yet
- LABORATORY MANUAL FOR A MINI PROJECT: MSCB 1113 BIOCHEMISTRY & MICROBIAL PHYSIOLOGYFrom EverandLABORATORY MANUAL FOR A MINI PROJECT: MSCB 1113 BIOCHEMISTRY & MICROBIAL PHYSIOLOGYNo ratings yet
- Que NCPDocument6 pagesQue NCPIrene Grace BalcuevaNo ratings yet
- Seizure ReadyDocument8 pagesSeizure ReadyIrene Grace BalcuevaNo ratings yet
- NCP 1Document2 pagesNCP 1Irene Grace BalcuevaNo ratings yet
- DS 4 5Document4 pagesDS 4 5Irene Grace BalcuevaNo ratings yet
- Cabasa Drugstudy 12 14Document4 pagesCabasa Drugstudy 12 14Irene Grace BalcuevaNo ratings yet
- NCPDocument6 pagesNCPIrene Grace BalcuevaNo ratings yet
- The Literature of Visayas "Bonsai" by Edith TiempoDocument20 pagesThe Literature of Visayas "Bonsai" by Edith TiempoIrene Grace Balcueva100% (1)
- Fellows PowerShred C-320CDocument36 pagesFellows PowerShred C-320CByron BrainardNo ratings yet
- The Hole Problem in Knit GoodsDocument13 pagesThe Hole Problem in Knit GoodsKathirrveluSubramainanNo ratings yet
- Serie-6-Ttv Brochure enDocument16 pagesSerie-6-Ttv Brochure envaneaNo ratings yet
- Hbo Chapter 4Document13 pagesHbo Chapter 4132345usdfghjNo ratings yet
- RRLDocument5 pagesRRLAyen Alecksandra CadaNo ratings yet
- Apxvdgll26exd 43-C-I20 PreDocument4 pagesApxvdgll26exd 43-C-I20 Precmsd01No ratings yet
- University of Cambridge International Examinations General Certifi Cate of Education Advanced LevelDocument8 pagesUniversity of Cambridge International Examinations General Certifi Cate of Education Advanced LevelKazi Ahnaf SaadNo ratings yet
- Power Plant Project ReportDocument66 pagesPower Plant Project ReportPoojit PopliNo ratings yet
- ISA RP60 1 1990 Control Center FacilitiesDocument22 pagesISA RP60 1 1990 Control Center FacilitiesDaniel Arrieta DarrásNo ratings yet
- Sankya Theory Number Wise.Document23 pagesSankya Theory Number Wise.Suresh Lakshmi NarasimhanNo ratings yet
- Flavouring and SavouringDocument4 pagesFlavouring and SavouringVaishaly MA Psych sem1No ratings yet
- Drug and Alcohol Testing in The WorkplaceDocument16 pagesDrug and Alcohol Testing in The WorkplaceYasmin KayeNo ratings yet
- Acu in HorsesDocument72 pagesAcu in Horsespeter911xNo ratings yet
- Print Ko BukasDocument3 pagesPrint Ko BukasKatrina CaveNo ratings yet
- Rachana 2nd Issue FinalDocument20 pagesRachana 2nd Issue Finalpacesoft321No ratings yet
- AS350B3 Flight-ManualDocument376 pagesAS350B3 Flight-ManualBruno Alonso Pacheco100% (2)
- Inspection Checklist - HDPE Butt Fusion WeldingDocument1 pageInspection Checklist - HDPE Butt Fusion WeldingQasim Saeed KhanNo ratings yet
- Solutions ACC415Document46 pagesSolutions ACC415gloriyaNo ratings yet
- (Tham Khảo) Tài Liệu Ngoại Ngữ Y2Document55 pages(Tham Khảo) Tài Liệu Ngoại Ngữ Y2Nam TruongNo ratings yet
- CHRA 1st Reprint 2018 PDFDocument149 pagesCHRA 1st Reprint 2018 PDFMohd Jamalil Azam MustafaNo ratings yet
- Gingival Biotype - A ReviewDocument6 pagesGingival Biotype - A ReviewAna Maria Montoya GomezNo ratings yet
- Johnson OE (2012) - Therapeutic Exercises in The Management of Non-Specific Low Back PainDocument23 pagesJohnson OE (2012) - Therapeutic Exercises in The Management of Non-Specific Low Back PainApollwn100% (1)
- Anesthetics and Analgesics SheepDocument1 pageAnesthetics and Analgesics Sheepari putraNo ratings yet
- Molecular PolarityDocument13 pagesMolecular PolarityDanielle KaplanNo ratings yet
- Present Tense Exercise 18Document1 pagePresent Tense Exercise 18Adrijan AlispahićNo ratings yet
- LoveDocument3 pagesLoveAntonio CarmeloNo ratings yet
- LIT Equipment - Catalogue A4 en VLRDocument56 pagesLIT Equipment - Catalogue A4 en VLREkaluck JongprasithpornNo ratings yet
- Approval Document ASSET DOC LOC 537Document4 pagesApproval Document ASSET DOC LOC 537aNo ratings yet
Nursing Procedures
Nursing Procedures
Uploaded by
Irene Grace BalcuevaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Procedures
Nursing Procedures
Uploaded by
Irene Grace BalcuevaCopyright:
Available Formats
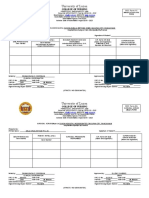
CEBU TECHNO LO GICAL U NIVERS ITY
In c ons or t i um w i t h
CEBU CITY MEDICAL CE NTER - CO LLEGE O F NU RSING
N. Bacalso Ave. cor Panganiban St., 6000 Cebu City, Cebu, Philippines
ATTACHING PULSE OXIMETRY
Name: Nicole Dominique B. Tinapay Level: 3-B
Date materials checked:
Instructor in Charge: Date performed:
I. Learning Objectives:
a. Define the terminologies related to this procedure.
b. Identify the indications and contraindications following this procedure.
c. Familiarize the different parts of a pulse oximeter.
d. Recognize the abnormal and abnormal parameters based on the findings
at the end of the procedure.
II. Definitions:
a. Pulse Oximetry – is the noninvasive measurement of estimated saturation of
arterial Hb with oxygen.
b. Oxygen Saturation – is a measure of the amount of hemoglobin that is bound to
molecular oxygen at a given time point. It is an important parameter for managing
patients in a clinical setup.
III. Purpose:
Allows for continuous monitoring of SpO2 in the critically ill patient.
It can be used to monitor the patient’s response to exercise and activity in
hospital and community settings.
It can also be used to make treatment decisions (e.g. the need for oxygen
therapy, ensuring safety / effectiveness of interventions (e.g. position change)
IV. Materials and Supplies needed: (to be checked days prior to return
demonstration)
a. Replica of pulse oximeter - 1 per group
b. Alcohol swab - 2 pcs.
c. Replica sensor -
d. Nail polish remover -
V. Procedure and Rationale
PROCEDURE RATIONALE
Assessment:
1. Assess the client’s hemoglobin le9svel.
2. Assess the client’s color.
3. Assess the client’s mental status.
4. Assess the client’s pulse rate.
5. Assess the area where the sensors will be
placed.
6. Remove the nail polish or acrylic nails.
Procedure:
1. Wash hands.
2. Select an appropriate sensor.
3. Select an appropriate site for the sensor.
4. Assess for capillary refill and proximal
pulse.
5. Clean the site with an alcohol swab.
Remove artificial nails or nail polish. Clean
the site with any adhesive tape, with soap
and water.
6. Apply the sensor, making sure the photon
detectors are aligned on opposite sides of
the selected site.
7. Connect the sensor to the oximeter with
sensor cable.
8. Turn on the machine. Initially, a tone can
be heard, followed by an arterial wave
form fluctuation with each arterial pulse.
9. Adjust the alarm limits for high and low O2
saturation levels. (including pulse rate
limits).
10. If taking the reading, note the results.
If the oximeter is being used for constant
monitoring, move the site of spring
sensors every 2 hours and adhesive
sensors every 4 hours.
11. Cover the sensor with a sheet or towel.
12. Notify the physician for abnormal results.
13. Record the result of oxygen saturation
according to the health care providers
order or protocol. Include in the
documentation the type of sensor used,
the site of application, the hemoglobin
level, and the assessment of the client’s
skin at the sensor site.
CEBU TECHNO LO GICAL U NIVERS ITY
In c ons or t i um w i t h
CEBU CITY MEDICAL CE NTER - CO LLEGE O F N U RSING
N. Bacalso Ave. cor Panganiban St., 6000 Cebu City, Cebu, Philippines
ATTACHING CARDIAC MONITOR
Name: Level:
Date materials checked:
Instructor in Charge: Date performed:
I. Learning Objectives:
a. Define the terminologies related to this procedure.
b. Identify the indications and contraindications following this procedure.
c. Familiarize the different parts of cardiac monitor.
d. Recognize the abnormal and abnormal parameters based on the findings at the end
of the procedure.
II. Definitions:
a. Cardiac monitor –
a. Electrocardiogram –
III. Purposes:
IV. Materials and Supplies needed: (to be checked days prior to return demonstration)
a. Replica of cardiac monitor (pls see model/picture provided) - 1 per group
b. Alcohol swab - 2 pcs.
b. Washcloth, soap and towel -
c. Dry gauze pads or ECG prep pads -
V. Procedure and Rationale
PROCEDURE RATIONALE
Preparation:
1. Explain the reason for ECG monitoring.
2. Reassure client that changes in heart
rhythm can be noted and immediately
treated if necessary.
3. Explain that loose or disconnected lead
wires, poor electrode contact, excessive
movement, electrical interference, or
equipment malfunction may trigger alarms
and alert the staff.
4. Reassure that movement allowed, within
activity restrictions, while on the monitor.
5. Explain skin preparation procedure.
6. Provide privacy and drape appropriately.
Procedure:
1. Wash hands.
2. Check equipment for damage. Connect
lead wires to cable, and secure
connections.
3. Select electrode sites on the chest wall.
Avoiding areas of excessive movement,
joints, skin creases, scar tissue or other
lesions.
4. Clean the sites with soap and water and
dry thoroughly. Alcohol may be used to
remove skin oils; allow the skin to dry for
60 seconds after use.
5. Gently rub the site with a dry gauze pad or
ECG prep pad.
6. Open the electrode package; peel the
backing from the electrode and check to
ensure that the center of the pad is moist
with conductive gel.
7. Apply electrode pads, pressing firmly to
ensure contact.
8. Attach leads and position cables with
sufficient slack for comfort. Place the
telemetry unit (if used) in gown pouch or
pocket.
9. Assess ECG tracing on the monitor,
adjusting settings as needed.
10. Set monitor alarm limits at 20BPM higher
and lower than the client’s baseline rate.
11. Turn the alarms on, and leave on at all
times. Assess immediately if alarm is
triggered.
12. Time and date pads with every change.
13. Monitor periodically for comfort. Assess
electrode and lead wire connections as
needed.
14. Remove and apply new pads every 24 –
48 hours or whenever the pads becomes
dislodged or non-adherent.
15. Clean gel residue from previous site, and
document skin condition under the pads.
Choose alternative site if the skin
appears irritated or blistered.
16. Document ECG strips, cardiac rhythm or
the client’s condition changes. Record
the date, time, client identification,
monitor lead, duration of PR and QT
intervals, and rhythm interpretation on
each ECG strip.
CEBU TECHNO LO GICAL U NIVERS ITY
In c ons or t i um w i t h
CEBU CITY MEDICAL CE NTER - CO LLEGE O F NU RS ING
N. Bacalso Ave. cor Panganiban St., 6000 Cebu City, Cebu, Philippines
PREPARING THE CHEST DRAINAGE SYSTEM
Name: Level:
Date materials checked:
Instructor in Charge: Date performed:
I. Learning Objectives:
a. Define the terminologies related to this procedure.
b. Identify the indications that necessitate the need for chest thoracostomy insertion.
c. Distinguish the expected/therapeutic outcomes of CTT insertion.
d. Enumerate the necessary client’s teachings essential for this procedure.
e. Ascertain the essential nursing interventions prior, during and post CTT insertion.
II. Definitions:
a. Thoracostomy –
b. Pneumothorax –
c. Hemothorax –
d. Pyothorax –
e. Hydrothorax –
III. Purposes:
IV. Materials and Supplies needed:
a. Improvised sterile pack which consist of: - 2 packs/group
3 empty bottles with removed
(e.g. mayonnaise, Gatorade)
Drinking straws cut to its appropriate length
b. Any type of venoclysis - 1 per group
c. Sterile gloves - 1 pair
d. Face mask - 1 pc.
V. Procedure and Rationale:
PROCEDURE RATIONALE
Assessment:
1. Check the physician’s order.
2. Assess for the available equipment.
3. Assess the client’s environment.
4. Render the appropriate client’s education.
Procedure:
1. Gather equipment in a clean area or at the
client’s bedside table.
2. Wash hands.
3. Open the pre-packaged disposable chest
tube system using aseptic technique.
4. Don sterile gloves.
One Bottle Water Seal
1. Insert a long glass tube through one hole
of a two hole rubber stopper. Insert a short
glass tube through the other hole in the
stopper.
2. Pour sterile saline or sterile water into the
glass, filling it to a depth for at least 4cm.
3. Be careful not to contaminate the inside of
the rubber stopper or the portion of the
glass tubes that will be inside the bottle,
put the rubber stopper onto the bottle.
4. Be sure the end of the long glass tube is
submerged 2 cm into the water in the
bottle. If the tube does not extend deeply
enough add more water to the bottle. Do
not fill the bottle more than one third full.
5. Attach rubber tubing to the outside end of
the long glass tube for drainage from the
client’s chest tube.
6. Place measuring guide on the side of the
bottle, marking the water level before
connection to the client.
Two Bottle Drainage and Water Seal
1. Insert two short glass tubes into a two
hole rubber stopper. Place this rubber
stopper onto the drainage bottle.
2. Insert one long glass tube and one short
glass tube into a second two hole rubber
stopper.
3. Pour sterile water or sterile saline into the
water seal bottle to a depth of about 4cm.
Do not fill the bottle more than one third
full.
4. Place the rubber stopper with the long
glass tube onto the water seal, being
careful not to contaminate the inside of the
bottle or the glass tubes.
5. Be sure the end of the long glass tubes is
submerged 2cm into the water in the
bottle. If the tube does not extend deeply
enough add more water to the bottle. Do
not fill the bottle more than one third full.
6. Place a length of rubber tubing between
the outer end of the short glass tubes on
the drainage bottle & the outer end of the
long glass tube on the water seal bottle.
7. Place a length of rubber tubing on the
outer end of the second short glass tubes
on the drainage. This tube is for
connecting to the client for drainage.
8. Place measuring guide on the side of the
bottle, marking the water level before
connection to the client.
Two Bottle Drainage and Suction Control
1. Insert a long glass tube through one hole
of a two hole rubber stopper.
Insert a short glass tube through the other
hole in the rubber stopper.
2. Pour sterile water or sterile saline into the
water seal or drainage bottle filling it to a
depth of at least 4 cm.
3. Pour sterile water or sterile saline into the
suction control bottle to the ordered depth
of usually 20 cm of water.
4. Place the two hole rubber stopper with the
long glass tube onto the water seal or
drainage bottle, being careful not to
contaminate the inside of the bottle or the
glass tubes.
5. Be sure the end of the long glass tubes is
submerged 2cm into the water in the
bottle. If the tube does not extend deeply
enough, add more water to the bottle. Do
not fill the bottle more than one third full.
6. Place the three hole rubber stopper with
the long glass tube and two short glass
tubes onto the suction control bottle, being
careful not to contaminate the inside of the
bottle or the glass tubes.
7. Be sure the long glass tubes extends well
into the water but does not touch the
bottom of the bottle.
8. Attach a length of rubber tubing to the
outside end of the short glass tube in the
water seal or drainage bottle and connect
it to the outer end of one of the short glass
tubes in the suction control bottle.
9. Attach the suction tubing to the outer end
of the second short glass tubes in the
suction control bottle.
10. Do not attach any tubing to the outer end
of the long glass tube in the suction
control bottle.
11. Attach the drainage tubing from the client
to the outer end of the long glass tube in
the water seal or drainage bottle.
12. Turn the suction source up until a gentle
bubbling noted in the suction control
bottle.
a. To increase the suction, add more
water to the suction control bottle.
b. To decrease the suction, remove
water from the suction control bottle.
13. Place measuring guide on the side of the
bottle, marking the water level before
connection to the client.
Three Bottle Drainage, Water Seal and
Suction
1. Insert a short glass tubes through the
holes in one of the two hole rubber
stopper.
2. Insert a long glass tube through one hole
of a two hole rubber stopper. Insert a short
glass tube through the other hole in the
stopper.
3. Insert a long glass tube through the
middle hole of a three hole rubber stopper
and short glass tubes through the other
two holes in the three hole stopper.
4. Pour sterile water or sterile saline into the
water seal bottle, filling it to a depth of at
least 4 cm.
5. Pour sterile water or sterile saline into the
suction control bottle to the ordered depth
of usually 20 cm of water.
6. Be careful not to contaminate the inside of
the rubber stopper or the portion of the
glass tubes that will be inside the bottle.
Put the rubber stopper onto the bottle with
the two short glass tubes onto the
drainage collection tube.
7. Place the two hole rubber stopper with the
long glass tube onto the water seal bottle,
being careful not to contaminate the inside
of the bottle or the glass tube.
8. Be sure the end of the long glass tube is
submerged 2 cm into the water in the
bottle. If the tube does not extend deeply
enough, add more water to the bottle. Do
not fill the bottle more than one third full.
9. Place the three hole rubber stopper with
the long glass tube and two short glass
tubes onto the suction control bottle, being
careful not to contaminate the inside of the
bottle or the glass tubes.
10. Be sure the long glass tubes extends
well into the water but does not touch the
bottom of the bottle.
11. Attach the rubber tubing to the outside
end of one of the short glass tubes
extending from the drainage collection
bottle, to attach to the client’s chest tube.
12. Attach a length of rubber tubing from the
short glass tube in drainage collection
bottle, to the long glass tube in the water
seal bottle.
13. Attach a length of rubber tubing from the
short glass tube in the water seal bottle,
to one of the short glass tubes in the
suction control bottle.
14. Attach the suction tubing to the second
short glass tubes in the suction control
bottle and to the suction source.
15. Do not attach any tubing to the outer end
of the long glass tube in the suction
control bottle.
16. Turn the suction source up until a gentle
bubbling noted in the suction control
bottle.
a. To increase the suction, add more
water to the suction control bottle.
b. To decrease the suction, remove
water from the suction control bottle.
17. Place measuring guide on the side of the
bottle, marking the water level before
connection to the client.
18. Tape all connections.
19. Dispose wastes to their appropriate
receptacle. Do after care.
20. Document relevant data.
CEBU TECHNO LO GICAL U NIVERS ITY
In c ons or t i um w i t h
CEBU CITY MEDICAL CE NTER - CO LLEGE O F NU RSING
N. Bacalso Ave. cor Panganiban St., 6000 Cebu City, Cebu, Philippines
IRRIGATING THE BLADDER USING A CLOSED SYSTEM CATHETER
Name: Level:
Date materials checked:
Instructor in Charge: Date performed:
I. Learning Objectives:
a. Define the terminologies related to this procedure.
b. Identify the indications that necessitate the need for continuous bladder irrigation.
c. Distinguish the expected/therapeutic outcomes of continuous bladder irrigation.
d. Ascertain the essential nursing interventions prior, during and post continuous
bladder irrigation.
II. Definitions:
a. Cystoclysis –
b. Bladder training –
III. Purposes:
IV. Materials and Supplies needed:
a. Standard retention catheter - 2 pcs/group
b. Y adapter for bladder irrigation (stopcock) - 2 pcs/group
c. Closed irrigation tubing - 2 pcs/group
d. Any types of venoclysis - 4 bots/group
e. Sterile gloves - 1 pair
f. Face mask - 1 pc.
g. Alcoholized swabs - 5 pcs.
V. Procedure and Rationale
PROCEDURE RATIONALE
Assessment:
1. Assess the client for bladder distention or
complaints of fullness or discomfort.
2. Assess the drainage system for equal or
large amounts of drainage versus infused
irrigant.
3. Assess the color, consistency, and clarity
of the bladder drainage as well as noting
any clots or debris present.
Intermittent Bladder Irrigation using a
Standard Retention Catheter and a Y
Adapter
1. Gather equipment in a clean area or at the
client’s bedside table.
2. Wash hands.
3. Provide privacy or close curtain door.
4. Hang the prescribed irrigation solution in
an IV pole.
5. Insert the clamped irrigation tubing into the
bottle or irrigant, & prime tubing with fluid,
expelling all air & re-clamping the tube.
6. Don sterile gloves.
7. Clamp the urinary catheter.
8. Unhook the drainage bag from the
retention catheter.
9. While holding the drainage tubing and the
drainage port of the catheter in your non-
dominant hand, cleanse both the tubing
and the port with antiseptic swabs.
10. Connect one port of the Y adapter to the
drainage tubing and the bag.
11. Attach the third port of the Y adapter to
the irrigant tubing and bag.
12. Unclamp the urinary catheter and
establish that urine is draining through
the catheter into the drainage bag.
13. To irrigate the catheter and bladder,
clamp the drainage tubing distal to the Y
adapter.
14. Instill the prescribed amount of irrigant.
15. Clamp the irrigant tubing.
16. If the physician has ordered that the
irrigant to remain in the bladder for a
measured length of time, wait the
prescribed length of time.
17. Unclamp the drainage tubing and monitor
the drainage as it flows into the drainage
bag.
18. Appropriate care after the procedure.
19. Document relevant data.
CEBU TECHNO LO GICAL U NIVERS ITY
In c ons or t i um w i t h
CEBU CITY MEDICAL CE NTER - CO LLEGE O F NU RSING
N. Bacalso Ave. cor Panganiban St., 6000 Cebu City, Cebu, Philippines
INFUSION, DRIPS, AND HEPARIN LOCK INSERTION
Name: Level:
Date materials checked:
Instructor in Charge: Date performed:
I. Learning Objectives:
a. Define the terminologies related to this procedure.
b. Identify the indications that necessitate the need for heparin lock insertion.
c. Distinguish the expected/therapeutic outcomes of medications given through
infusion/drip.
d. Ascertain the essential nursing interventions prior, during and post infusion.
e. Maintain and observe the rights of medication administration.
II. Definitions:
a. Formula for drug computation:
b. Formula for computing intravenous rate:
c. Heparin Lock –
III. Purposes:
IV. Materials and Supplies needed:
a. Volume control infusion device (e.g. Soluset) - 2 pcs/group
b. Any type/king of venoclysis - 2 bots/group
c. IV cannula - 2 pcs/group
d. Heparin lock - 2 pcs/group
e. 3 cc syringe (with 25 gauge needle) - 8 pcs/group
f. Clean gloves - 1 pair
g. Empty vial (e.g. distilled water bottle) - 6 bots/group
h. Medication tray - 1 pc.
i. Alcohol swab - 2 pcs.
j. Plaster - 1 pc.
k. IVF tag - 1 sheet
V. Procedure and Rationale:
PROCEDURE RATIONALE
Assessment:
1. Assess the rights in drug administration.
2. Check the physician’s order for the client,
medication, dosage, frequency, time and
route of administration.
3. Review information regarding the drug,
including action, purpose, side effects,
normal dose, peak onset, and nursing
implications.
A. DRUG COMPUTATION
Able to arrive Solution Time Attempt
at the correct
answer
B. IVF RATE COMPUTATION
Able to arrive Solution Time Attempt
at the correct
answer
C. ADDING MEDICATIONS TO AN IV SOLUTION via VOLUME CONTROL SET
1. Check the physician’s order for the IV
solution and additives ordered.
2. Determine whether the ordered additives
are compatible with the IV solution and
with each other.
3. Wash hands and don clean gloves.
4. Prepare the medication for one client at a
time.
5. Assemble equipment and supplies
needed.
6. Prepare new bag by removing protective
cover from the bag.
7. Inspect the bag for leaks or tears.
8. Inspect for clarity, particulate matter and
color. Check expiry date.
9. Close clamps and open air vent on
chamber.
10. Connect the primary IV bag to the
volume control set. Then connect the IV
tubing to the volume control set.
11. Open the upper clamp and let the IV
solution partially fill the chamber. Close
the clamp.
12. Open the lower clamp, squeeze the drip
chamber and close the lower clamp at
the same time. Allow the fluid to fill the
drip chamber and then open it and allow
the solution to flow down to fill the tubing.
13. Prepare the medication for delivery.
Draw up the medication into a syringe.
14. Check the client’s armband before
administering the medication.
15. Add the medication to IV solution. Wipe
off port or site with alcohol swab, then
inject the needle into the chamber and
gently mix.
16. Open upper clamp and add additional IV
solution to bring the volume of
medication and diluent to the prescribed
amount. Close clamp.
17. Adjust the flow rate. (as computed
above)
18. Label the chamber with medication
information, date, time and nurse’s
signature.
19. Observe the client for side effects or
adverse reactions.
20. When the volume in the chamber has
been infused, close the air vent and reset
the flow rate to the prescribed IV infusion
rate.
D. DISCONTINUING THE IV and CHANGING TO A SALINE/HEPARIN LOCK
Assessment:
1. Check the physician’s order to discontinue
IV and insert a saline lock.
2. For existing IV’s, assess the skin and
patency of the IV.
3. Assess the client’s understanding of the
purpose of the saline lock.
4. Wash hands and don clean gloves.
5. Check client’s identification bracelet.
6. Explain the procedure and the reason for
discontinuing IV solution.
7. Prepare supplies at bedside.
a. Syringe with saline
b. Syringe with heparin
c. Saline lock
8. Stop the IV solution.
a. For IV tubing, roll clamp to close IV
tubing.
b. For infusion pump, turn switch to off.
9. Loosen IV tubing then remove.
10. Screw the saline lock into the hub of
tubing.
11. Check for patency:
a. Clean heparin lock with alcohol swab.
b. Insert syringe with 25 gauge needle
into center of diaphragm.
c.Pull back gently on syringe and watch
for blood return.
d. Inject saline slowly into lock.
e. Assess client’s pain at site.
12. Keep lock patent with heparin or normal
saline, every 8 hours.
13. Assess the site for any signs of leakage,
irritation, or infiltration.
14. Remove gloves and dispose with all used
materials.
15. Wash hands.
CEBU TECHNO LO GICAL U NIVERS ITY
In c ons or t i um w i t h
CEBU CITY MEDICAL CE NTER - CO LLEGE O F NU RSING
N. Bacalso Ave. cor Panganiban St., 6000 Cebu City, Cebu, Philippines
TRACHEOSTOMY CARE
Name: Level:
Date materials checked:
Instructor in Charge: Date performed:
I. Learning Objectives:
a. Define terminologies related to the procedure.
b. Properly perform tracheostomy care considering the principles of asepsis.
c. Identify the role of the nurse in the care of client with tracheostomy.
II. Definitions:
a. Tracheostomy –
b. Tracheostomy care –
III. Purposes:
IV. Materials and Supplies needed:
V. Procedure and Rationale:
PROCEDURE RATIONALE
Preparation:
1. Assess:
a. Respiratory status, including ease of
breathing, rate, rhythm, depth and lung
sounds.
b. Pulse rate
c. Character and amount of secretions from
tracheostomy site
d. Presence of drainage on tracheostomy
dressings or ties.
e. Appearance of incision.
2. Assemble equipment and supplies:
a. Sterile disposable tracheostomy
cleaning kit or supplies.
b. Towel or drape to protect bed linens.
c. Sterile suction catheter kit
d. Hydrogen peroxide and sterile normal
saline
e. 2 pairs sterile gloves
f. Clean gloves
g. Moisture-proof bag
h. Sterile tracheostomy dressings or sterile
4” x 4” gauze dressings.
i. Cotton twill ties
j. Clean pair of scissors
Procedure:
1. Explain the procedure.
Provide for a means of communication,
such as eye blinking or raising of hand to
indicate pain or distress.
2. Wash hands and observe appropriate
infection control procedures.
3. Provide client’s privacy.
4. Prepare the client and the equipment:
a. Assist the client to a Semi-Fowler’s or
Fowler’s position.
b. Open tracheostomy kit or sterile basins.
Pour hydrogen peroxide and sterile
normal saline into separate containers.
c. Establish sterile field.
5. Suction the tracheostomy tube:
a. Don a clean glove on your non-dominant
hand and a sterile glove on your
dominant hand (or don sterile gloves)
b. Suction the full length of the
tracheostomy tube to remove secretions
and ensure a patent airway.
c. Rinse the suction catheter and wrap the
catheter around your hand, and peel the
glove off so that it turns inside out over
the catheter.
d. Using the gloved hand, unlock the inner
cannula (if present) and remove it gently
by pulling it out toward you in line with
its curvature. Place the inner cannula in
the hydrogen peroxide solution.
e. Remove the soiled tracheostomy
dressings, and discard the gloves and
the dressings.
f. Don sterile gloves. Keep your dominant
hand sterile during the procedure.
6. Clean the inner cannula.
a. Remove the inner cannula from the
soaking solution.
b. Clean the lumen and entire inner
cannula thoroughly, using the brush or
pipe cleaners moistened with sterile
normal saline. Inspect the cannula for
cleanliness by holding it at eye level and
looking through it into the light.
c. Rinse the inner cannula thoroughly in the
sterile normal saline.
d. After rinsing, gently tap the cannula
against the inside edge of the sterile
saline container. Use a pipe cleaner
folded in half to dry only the inside of the
cannula. Do not dry the outside of the
cannula.
e. Using sterile technique, suction the
outside of the cannula.
7. Replace the inner cannula, securing it into
place.
a. Insert the inner cannula by grasping the
outer flange and inserting the cannula in
the direction of its curvature.
b. Lock the cannula in place by turning the
lock (if present) into position to secure
the flange of the inner cannula to the
outer cannula.
8. Clean the incision site and tube flange.
a. Using sterile applicators or gauze
dressings moistened with normal saline,
clean the incision site. Handle the sterile
supplies with your dominant hand, and
use each applicator or gauze dressing
only once and then discard.
b. Hydrogen peroxide maybe used to
remove crusty secretions. Thoroughly
rinse the cleaned area, using gauze
squares moistened with sterile normal
saline.
c. Clean the flange of the tube in the same
manner.
d. Thoroughly dry the client’s skin & tube
flanges with dry gauze squares.
9. Apply sterile dressings.
a. Using commercially prepared
tracheostomy dressing of non-raveling
material, or open and refold a 4” x 4”
gauze dressing into a “V” shape.
b. Place the dressing under the flange of
the tracheostomy tube.
c. While applying the dressing, ensure that
the tracheostomy tube is securely
supported.
10. Change the tracheostomy ties:
a. Two-Strip Method
Cut two unequal strips of twill tape,
one approximately 25 cm (10 in)
long and the other about 50 cm
(20 in) long.
Cut a 1 cm lengthwise slit 2.5 cm
from one end of each strip. To do
this, fold the end of the tape back
onto itself about 2.5 cm, then cut a
slit in the middle of the tape from
its folded end.
Leaving the old ties in place,
thread the slit end of one clean
tape through the eye of the
tracheostomy flange from the
bottom side, then thread the long
end of the tape through the slit
pulling it tight until it is securely
fastened to the flange.
If the old ties are very soiled, or if it
is difficult to thread new ties onto
the tracheostomy flange with the
old ties in place, have an assistant
to put on a sterile glove and hold
the tracheostomy in place while
you replace the ties.
Repeat the process with the
second ties.
Ask the client to flex his neck, then
slip the longer tape under the
client’s neck, place two fingers
between the tape and the client’s
neck and tie the tapes together at
the side of the neck.
Tie the ends of the tapes, using
square knots. Cut off any long
ends, leaving approximately 1 – 2
cm.
Once the clean ties are secured,
remove the soiled ties and discard.
b. One-Strip Method
Cut a length of twill tape 2.5 cm
times the length needed to go
around the client’s neck from one
tube flange to the other.
Thread one end of the tape into
the slot on one side of the flange.
Bring both ends of the tape
together and tape them around the
client’s neck, keeping them flat
and untwisted.
Thread the end of the tape next to
the client’s neck through the slot
from the back to the front.
Have the client flex his neck. Tie
the loose ends with square knot at
the side of the client’s neck allow
for slack by placing two fingers
under the ties, as with the two-strip
method. Cut off longs ends.
11. Tape and pad the tie knot.
a. Place a folded 4” x 4” gauze square
under the tie knot, and apply tape over
the knot.
12. Check the tightness of the ties.
a. Frequently check the tightness of the
tracheostomy ties and position of the
tracheostomy tube.
13. Document all relevant information.
CEBU TECHNO LO GICAL U NIVERS ITY
In c ons or t i um w i t h
CEBU CITY MEDICAL CE NTER - CO LLEGE O F NU RSING
N. Bacalso Ave. cor Panganiban St., 6000 Cebu City, Cebu, Philippines
ADMINISTERING EYE MEDICATIONS
Name: Level:
Date materials checked:
Instructor in Charge: Date performed:
I. Learning Objectives:
a. Define the terminologies related to the procedure.
b. Identify the indications that necessitate the need for eye medication.
c. Enumerate the necessary client teachings essential for this procedure.
II. Definition:
a. Ophthalmologic medications –
III. Purposes:
IV. Materials and Supplies needed:
V. Procedure and Rationale:
PROCEDURE RATIONALE
Preparation:
1. Check the client and the chart for any
known allergies or medication conditions
that would contraindicate use of the drug.
2. Gather the necessary equipment and
supplies.
3. Follow the different rights of drug
administration.
4. Take the medication in the client’s room
and place on a clean surface.
5. Check the client’s identification arm band.
6. Explain the procedure to the client. Inquire
the client wants to instill medication. If so
assess the client’s ability to do so.
7. Wash hands. Don clean gloves if needed.
8. Place client in a supine position with the
head slightly hyperextended.
Instilling Eye Drops:
1. Remove cap from the eye medication
bottle and place cap on its side.
2. Squeeze the prescribe amount of
medication into the eye dropper.
3. Place a tissue below the lower lid.
4. With a dominant hand, hold the eye
dropper one half to one third inch above
the eyeball, rest hand on client’s forehead
to stabilize.
5. Place hand on cheekbone and expose
lower conjunctival sac by pulling down on
the check.
6. Instruct client to look up and drop
prescribed number of drops into center of
conjunctival sac.
7. Instruct client to gently close and move
eyes. Briefly place fingers on either side of
the client’s nose to close the tear ducts
and prevent the medication from draining
out of the eye.
8. Remove gloves and wash hands.
9. Record on the MAR the route, site and
time administered.
You might also like
- Manual of Operations For Drug Testing LaboratoriesDocument24 pagesManual of Operations For Drug Testing LaboratoriesSarah Jane V. Denia100% (6)
- Rodak Questions CompilationDocument40 pagesRodak Questions CompilationGertrudeshane IletoNo ratings yet
- CSF SopDocument19 pagesCSF SopdeblackaNo ratings yet
- Questionnaire (HTMLE)Document16 pagesQuestionnaire (HTMLE)Angelo Mercede100% (1)
- MT113BL Analysis of Urine and Other Body Fluids ManualDocument28 pagesMT113BL Analysis of Urine and Other Body Fluids ManualAsxe Cee100% (1)
- PCP Obe-Cbtp Dops Rtp-Acc Form#7Document6 pagesPCP Obe-Cbtp Dops Rtp-Acc Form#7Ko HakuNo ratings yet
- CLINICAL PRACTICUM Activity Book Revised 2014Document17 pagesCLINICAL PRACTICUM Activity Book Revised 2014helpNo ratings yet
- Learning Activity No. 7Document15 pagesLearning Activity No. 7Gabrielle SerenoNo ratings yet
- 2016 ACHE Healthcare Executie Competencies Assessment ToolDocument28 pages2016 ACHE Healthcare Executie Competencies Assessment ToolragcajunNo ratings yet
- BS en 13478 Fire Prevention and ProtectionDocument30 pagesBS en 13478 Fire Prevention and Protectiontoalok4723No ratings yet
- Checklist On Vital Signs - Blood Oxygenation Using Pulse OxymeterDocument2 pagesChecklist On Vital Signs - Blood Oxygenation Using Pulse Oxymeteraliyah2 sanchezNo ratings yet
- Immunohema Lab ActivitiesDocument46 pagesImmunohema Lab ActivitiesMushu MunuNo ratings yet
- Course Syllabus PLAB 1223 - Phlebotomy: WWW - Panola.eduDocument12 pagesCourse Syllabus PLAB 1223 - Phlebotomy: WWW - Panola.edukisserie licyayoNo ratings yet
- Nursingbullets: Respiratory System - Diagnostic ProceduresDocument41 pagesNursingbullets: Respiratory System - Diagnostic ProceduresErmadutz Sumampong FernandezNo ratings yet
- Respiratory Diagnostic ProceduresDocument41 pagesRespiratory Diagnostic Proceduresseigelystic100% (23)
- Respiratory System Diagnostic Procedures: Marjorie V. Aguinaldo RN, MANDocument32 pagesRespiratory System Diagnostic Procedures: Marjorie V. Aguinaldo RN, MANKun KandaNo ratings yet
- Blood Pressure ChecklistDocument2 pagesBlood Pressure ChecklistKatherine bundalianNo ratings yet
- Tugas Kelompok 2 BHS Inggris SopDocument17 pagesTugas Kelompok 2 BHS Inggris Sopmoms naraNo ratings yet
- Oxygen Saturation ChecklistDocument2 pagesOxygen Saturation ChecklistPatrick SantosNo ratings yet
- CHECKLIST Performing Clinical Electrocardiography ECGDocument3 pagesCHECKLIST Performing Clinical Electrocardiography ECGTriciaNo ratings yet
- Surgical Skin Prep PDFDocument12 pagesSurgical Skin Prep PDFDrrjdrjd MemeNo ratings yet
- Kashi PanchakamDocument2 pagesKashi PanchakamAnandNo ratings yet
- Is Lab. Activity 1 ETSDocument6 pagesIs Lab. Activity 1 ETSJuren LasagaNo ratings yet
- SL Evaluation Sheet Vital SignsDocument5 pagesSL Evaluation Sheet Vital SignsJoycee BoNo ratings yet
- Clinical Skill Manual of Gastrointestinal System 1819Document24 pagesClinical Skill Manual of Gastrointestinal System 1819SalmaNo ratings yet
- NCM 109 B Checklist of Procedures 1Document26 pagesNCM 109 B Checklist of Procedures 1manolbatindaan13No ratings yet
- 3obtaining Vital SignsDocument5 pages3obtaining Vital Signscharlotejeanbalanon1No ratings yet
- FTC SCRIPT O2 ADDocument2 pagesFTC SCRIPT O2 ADJUSTIN ALZATENo ratings yet
- Model Answer of Formative Written OSCADocument6 pagesModel Answer of Formative Written OSCAAhmed SamahaNo ratings yet
- Module 5 SuctioningDocument2 pagesModule 5 SuctioningDcimasaNo ratings yet
- Intubation ProcedureDocument6 pagesIntubation ProceduresinasinaaiNo ratings yet
- NCM 116b Checklist of ProceduresDocument44 pagesNCM 116b Checklist of ProceduresRhu PastranaNo ratings yet
- Sample QuestionsDocument15 pagesSample QuestionsAnonymous MtKJkerbpUNo ratings yet
- CC2433 Skill Performance Checklist Lab 2 2009Document5 pagesCC2433 Skill Performance Checklist Lab 2 2009twy113No ratings yet
- 6 ETS VenipunctureDocument7 pages6 ETS VenipunctureMyedelle SeacorNo ratings yet
- Or ExamDocument21 pagesOr Examlouie roderosNo ratings yet
- 100Document48 pages100Jerome JucutanNo ratings yet
- Emt BLS SkillsDocument45 pagesEmt BLS SkillsCHEN GAONo ratings yet
- 2007 NleDocument18 pages2007 NlealexisalvioNo ratings yet
- Equ10-04 Micro QC - Eqpt Maint SOPDocument7 pagesEqu10-04 Micro QC - Eqpt Maint SOPpokhara144No ratings yet
- Outlines: Arterial Blood GasesDocument9 pagesOutlines: Arterial Blood GasesToka HessenNo ratings yet
- O2 Therapy ChecklistDocument3 pagesO2 Therapy ChecklistKathlyn PactorananNo ratings yet
- PerioperativeDocument37 pagesPerioperativemj CanilangNo ratings yet
- Name: Section: Date PerformedDocument2 pagesName: Section: Date PerformedMaelyn Avanceña DujaleNo ratings yet
- AVOX July2011Document6 pagesAVOX July2011Kriss JonesNo ratings yet
- Lab Manual CSI103Document30 pagesLab Manual CSI103Nurul AinNo ratings yet
- Soal Perioperative Eng VersionDocument22 pagesSoal Perioperative Eng VersionZulaikah Nur IstiqomahNo ratings yet
- Arterial Line Placement (Adult)Document5 pagesArterial Line Placement (Adult)Sayan ChattopadhyayNo ratings yet
- Medical-Surgical Nusing Checklist: Conams Wesleyan University Philippines 2020-2021Document3 pagesMedical-Surgical Nusing Checklist: Conams Wesleyan University Philippines 2020-2021Kobe ManuelNo ratings yet
- Chapter 4 Vital SignsDocument11 pagesChapter 4 Vital SignsNila ManguerraNo ratings yet
- NCM 112 Lesson5Document6 pagesNCM 112 Lesson5Trisha LopezNo ratings yet
- Kewenangan Klinis KMB PK IIIDocument11 pagesKewenangan Klinis KMB PK IIImiraNo ratings yet
- Transfusion SpecimenCollectionDocument5 pagesTransfusion SpecimenCollectionDominic EmerencianaNo ratings yet
- I. Desired Learning OutcomesDocument7 pagesI. Desired Learning OutcomesMaelyn Avanceña DujaleNo ratings yet
- SuturingDocument3 pagesSuturingKiran RamloganNo ratings yet
- RPSGT Exam BlueprintDocument2 pagesRPSGT Exam BlueprintKarloveyNo ratings yet
- PCCN BipapDocument15 pagesPCCN Bipapkarthikayini3590No ratings yet
- Surg SGD Topics PrelimsDocument2 pagesSurg SGD Topics PrelimsMariana B.No ratings yet
- Collecyion SpecimenDocument52 pagesCollecyion Specimenرافت العواضيNo ratings yet
- Files of Accreditation 2016 2017 2Document309 pagesFiles of Accreditation 2016 2017 2Lovelie Grace GalarpeNo ratings yet
- LABORATORY MANUAL FOR A MINI PROJECT: MSCB 1113 BIOCHEMISTRY & MICROBIAL PHYSIOLOGYFrom EverandLABORATORY MANUAL FOR A MINI PROJECT: MSCB 1113 BIOCHEMISTRY & MICROBIAL PHYSIOLOGYNo ratings yet
- Que NCPDocument6 pagesQue NCPIrene Grace BalcuevaNo ratings yet
- Seizure ReadyDocument8 pagesSeizure ReadyIrene Grace BalcuevaNo ratings yet
- NCP 1Document2 pagesNCP 1Irene Grace BalcuevaNo ratings yet
- DS 4 5Document4 pagesDS 4 5Irene Grace BalcuevaNo ratings yet
- Cabasa Drugstudy 12 14Document4 pagesCabasa Drugstudy 12 14Irene Grace BalcuevaNo ratings yet
- NCPDocument6 pagesNCPIrene Grace BalcuevaNo ratings yet
- The Literature of Visayas "Bonsai" by Edith TiempoDocument20 pagesThe Literature of Visayas "Bonsai" by Edith TiempoIrene Grace Balcueva100% (1)
- Fellows PowerShred C-320CDocument36 pagesFellows PowerShred C-320CByron BrainardNo ratings yet
- The Hole Problem in Knit GoodsDocument13 pagesThe Hole Problem in Knit GoodsKathirrveluSubramainanNo ratings yet
- Serie-6-Ttv Brochure enDocument16 pagesSerie-6-Ttv Brochure envaneaNo ratings yet
- Hbo Chapter 4Document13 pagesHbo Chapter 4132345usdfghjNo ratings yet
- RRLDocument5 pagesRRLAyen Alecksandra CadaNo ratings yet
- Apxvdgll26exd 43-C-I20 PreDocument4 pagesApxvdgll26exd 43-C-I20 Precmsd01No ratings yet
- University of Cambridge International Examinations General Certifi Cate of Education Advanced LevelDocument8 pagesUniversity of Cambridge International Examinations General Certifi Cate of Education Advanced LevelKazi Ahnaf SaadNo ratings yet
- Power Plant Project ReportDocument66 pagesPower Plant Project ReportPoojit PopliNo ratings yet
- ISA RP60 1 1990 Control Center FacilitiesDocument22 pagesISA RP60 1 1990 Control Center FacilitiesDaniel Arrieta DarrásNo ratings yet
- Sankya Theory Number Wise.Document23 pagesSankya Theory Number Wise.Suresh Lakshmi NarasimhanNo ratings yet
- Flavouring and SavouringDocument4 pagesFlavouring and SavouringVaishaly MA Psych sem1No ratings yet
- Drug and Alcohol Testing in The WorkplaceDocument16 pagesDrug and Alcohol Testing in The WorkplaceYasmin KayeNo ratings yet
- Acu in HorsesDocument72 pagesAcu in Horsespeter911xNo ratings yet
- Print Ko BukasDocument3 pagesPrint Ko BukasKatrina CaveNo ratings yet
- Rachana 2nd Issue FinalDocument20 pagesRachana 2nd Issue Finalpacesoft321No ratings yet
- AS350B3 Flight-ManualDocument376 pagesAS350B3 Flight-ManualBruno Alonso Pacheco100% (2)
- Inspection Checklist - HDPE Butt Fusion WeldingDocument1 pageInspection Checklist - HDPE Butt Fusion WeldingQasim Saeed KhanNo ratings yet
- Solutions ACC415Document46 pagesSolutions ACC415gloriyaNo ratings yet
- (Tham Khảo) Tài Liệu Ngoại Ngữ Y2Document55 pages(Tham Khảo) Tài Liệu Ngoại Ngữ Y2Nam TruongNo ratings yet
- CHRA 1st Reprint 2018 PDFDocument149 pagesCHRA 1st Reprint 2018 PDFMohd Jamalil Azam MustafaNo ratings yet
- Gingival Biotype - A ReviewDocument6 pagesGingival Biotype - A ReviewAna Maria Montoya GomezNo ratings yet
- Johnson OE (2012) - Therapeutic Exercises in The Management of Non-Specific Low Back PainDocument23 pagesJohnson OE (2012) - Therapeutic Exercises in The Management of Non-Specific Low Back PainApollwn100% (1)
- Anesthetics and Analgesics SheepDocument1 pageAnesthetics and Analgesics Sheepari putraNo ratings yet
- Molecular PolarityDocument13 pagesMolecular PolarityDanielle KaplanNo ratings yet
- Present Tense Exercise 18Document1 pagePresent Tense Exercise 18Adrijan AlispahićNo ratings yet
- LoveDocument3 pagesLoveAntonio CarmeloNo ratings yet
- LIT Equipment - Catalogue A4 en VLRDocument56 pagesLIT Equipment - Catalogue A4 en VLREkaluck JongprasithpornNo ratings yet
- Approval Document ASSET DOC LOC 537Document4 pagesApproval Document ASSET DOC LOC 537aNo ratings yet