Professional Documents
Culture Documents
9 Hema Extrinsic RBC Defects
9 Hema Extrinsic RBC Defects
Uploaded by
Gwen Kirsten AtayanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
9 Hema Extrinsic RBC Defects
9 Hema Extrinsic RBC Defects
Uploaded by
Gwen Kirsten AtayanCopyright:
Available Formats
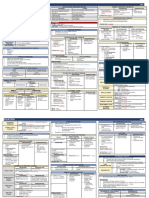
EXTRINSIC DEFECTS
EXTRINSIC RBC DEFECTS HEMOLYTIC ANEMIA Special tests - YES
- B2 came from B1
LABORATORY TESTS Thalassemia minor – microcytic - Are they equal? = NO
Basic test Thalassemia major – hemolytic anemia
Can be counted manually
RBC – *low levels, patient has anemia Carrier protein of B1 – Albumin
Hgb DECREASED or NORMAL RETIC COUNT = Bone marrow problem B2 – will go to the intestines for further breakdown
CBC Hct INCREASED RETIC COUNT = hemolytic anemia Will be converted into urobilinogen
WBC – *anemia is not a diagnosis, but a syndrome Urine urobilinogenuria
MPV
RDW
*Retic count Biliribinuria – problem with liver, biliary obstruction habang
MCV lumalabas yung B2
MCH
MCHC
INTRINSIC – problem in the RBC
ü Cytometric method – classify anemia (microcytic anemia, B1 – cannot exit; non-soluble - Kernicterus
EXTRINSIC – outside the RBC
macrocytic anemia, normocytic, normochromic) B2 – has exit; water soluble
May be a problem in plasma, blood vessel wall (endothelial lining)
ü Normocytic & Normochromic – where hemolytic anemia falls
RBC is normal
RBCI ü Reticulocyte count – index of hematopoiesis
o Compensate to red blood cell in peripheral blood Significance of Hemoglobinuria
ü Hemolytic anemia – destruction of RBC Intravascular Hemolysis
o Spleen – graveyard of cells Hemoglobinopathies are classified as hemolytic anemia
o Loss of RBC, Bone marrow will compensate
RPI – destruction of RBC due to bone marrow Bilirubinuria = biliary obstruction
Electrophoresis – diagnosing hemoglobinopathies and thalassemia Antibody immunoglobulin bind to normal RBC = forming immune complex
Immune complex activated complement system attack RBC RBC lyse Hemosidenuria = intravascular hemolysis
Spherocyte - Hallmark poikilocytes of hemolytic anemia Urobilinogenuria = extravascular hemolysis
Sign of hemolysis
Hemolysis:
PBS Schistocytes – fragmented red blood cells Extravascular lysis – graveyard (spleen); left side of abdominal cavity
INTRAVASCULAR Ab-mediated hemolysis – phagocytosis or complement-
OR mediated destruction
HEMOLYTIC ANEMIA EXTRAVASCULAR
BMA & BMB – to validate Destruction of RBC before their normal 120-day life span with anemia
Serum Fe
Serum Ferritin
IRON STUDIES TIBC CAUSES: separate mechanism and diverse entities whose common clinical feature is
No role in diagnosing hemolytic anemia hemolysis ETIOLOGIES OF HEMOLYSIS
Applied in differentiating micro hypo chromic anemia INTRINSIC EXTRINSIC
HEMOLYSIS Basic routine test for hemolysis
Inherited protein deficits Immune-mediated hemolytic anemia
TB B1:B2 CLINICAL SIGNIFICANCE: - Lead to increased destruction in - Abs + RBCs = IC
o If patient is undergoing hemolysis Spectrum from chronic to life-threatening membranopathies - Phagocytosis ADCC
o Particularly B1 Always considered in patients with unexplained normocytic or macrocytic anemia - Complement mediated lysis
o B2 – opposite bilirubin
o Elevated B1 Enzymopathies
o Manifestation: PATHOPHYSIOLOGY: - Hemolysis due to overwhelming Non-immune – walang antibody
Hyperbilirubinemia - jaundice Intravascularly oxidative stress or decreased - Microangiopathic hemolytic anemia
Urobilinogen – by product of conjugated bilirubin Extravascularly energy production (MAHA)
o Urine and stool specimen More common - Infections
Haptoglobin – carrier of free-hemoglobin - Direct trauma
o Main carrier of free hemoglobin Hemoglobinopathies - Drug-induced hemolysis
o Decreased level in plasma - Lead to splenic destruction SCD
Inside the bloodstream
o There is a limit and normal value - Likely multiple mechanism of
Direct cellular destruction – toxins, trauma or lysis
o Not being produced forever destruction
Fragmentation hemolysis – extrinsic factors produce shearing
o Hemoglobin cannot be excreted in the urine and rupture of RBCs
o Excess free hemoglobin – hold in free iron Oxidative hemolysis – protective mechanism of cells are CLINICAL PRESENTATION IF HEMOLYSIS IS SUSPECTED
o Transferrin – normal carrier protein of iron overwhelmed Jaundice
INTRAVASCULAR ACUTE
Hemopexin – carrier protein of free-iron in the blood Hemoglobinuria in the presence of anemia
(extrinsic)
LAD
What are the intravascular measures? HSM
CHRONIC
If you have hemolytic anemia, what will happen to hemopexin levels? It - Haemoglobinaemia Cholestasis
will DECREASE - Methaemalbuminaemia Choledocholithiasis
- Haemoglobinuria Fatigue
- haemosidenuria OTHER
Dyspnea
** Haptoglobin and hemopexin = decrease in times of hemolysis PRIMARY NONSPECIFIC
Outside the bloodstream; spleen – major organ Hypotension
EXTRAVASCULAR SYMPTOMS
Sequestration and phagocytosis – due to poor RBC Tachycardia
deformability Medical diagnosis
Methemoglobin – ferric is changed, ferric is oxidized (3+) o Inability to change shape enough to pass through HISTORY INCLUDE
Medications
the spleen KNOWN
Personal or family history of hemolytic anemia
PHYSICAL Identify associated condition
If you have hemolytic anemia, what will happen to meth heme albumin EXAMINATION Infections or malignancies
levels? It will INCREASE Heme oxygenase – enzyme inside spleen converted to biliverdin Complete Review Systems
(green pigment)
HEMATURIA – intact RBC, seen in microscopic analysis, cloudy
HEMOGLOBINURIA – lysed RBC, clear urine INITIAL WORK UP
CBC (anemia) Normo-Normo or Macrocytic
Biliverdin reductase – convert to bilirubin B1
Reticulocyte count
B1; LDH – not common
Methemalbumin
Haptoglobin
Hemoglobinuria – tested by reagent strip test If you have hemolysis, do you have hyperbilirubinemia? UA
Hemosiderinuria – presence of hemosiderin in urine - YES LDH Intracellular, and levels increase when RBC rupture
o Hemosiderin from hemoglobin - Secondary to B1 elevation
HAPTOGLOBIN Binds to free hemoglobin, and levels decrease in hemolysis
o Form of iron in the urine - Because in the liver it becomes conjugated
B1 Levels rise as its production exceeds elimination capability
RETIULOCYTOSIS Unless significant IDA or marrow suppression is present
CAUSING
In hemolysis, do you expect elevated B2?
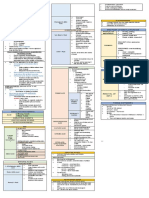
EXTRINSIC DEFECTS
MACROCYTOSIS
Hemoglobinuria
UA
Absence of these findings should prompt a search for other causes CLINICAL FEATURES: similar to other MAHA syndromes
SUPPORTIVE
Initiated after hemolysis is confirmed
CARE
For abnormal RBCs TREATMENT: discontinuing the offending agent, providing supportive care, plasma exchange
Spherocytes is not beneficial
PBS
Schistocytes
Bite or blister cells MICROANGIOPATHIC HEMOLYTIC ANEMIA (MAHA)
Caused by membrane deficits or repeated small membrane MECHANISM: RBC fragment schistocytes due to trauma from an endovascular device or
removals by macrophages microthrombi
SPHETOCYTES
SPHEROCYTOSIS – not a diagnostic for hemolytic anemia because CAUSES:
both hereditary spherocytosis and immune etiologies may cause 1. Thrombotic MicroAngiopathies (TMAs)
anemia - Diverse group of clinical entities that share MAHA as a central feature
Fragmented cells that result from intravascular destruction - Thrombotic thrombocytopenic purpura
SCHISTOCYTES
Occurs in MAHA syndromes - Hemolytic uremic syndrome
Result from partial phagocytosis 2. Other microangiopathic hemolytic anemia syndromes
BITE AND
Occur in oxidative causes
BLISTER CELLS
G6PD Deficiency THROMBOTIC MICROANGIOPATHIES (TMAs)
Further differentiates immune causes of hemolytic anemia from Thrombitic thrombocytopenic purpura
DAT
nonimmune causes
IMMUNE HEMOLYTIC ANEMIA DEFECT: reduced or absence of ADAMTS13 enzyme activity
AUTOIMMUNE HEMOLYTIC ANEMIA (AIHA)
Approximately 95% of TTP cases are associated with acquired autoantibodies
MECHANISM: autoantibody-mediated destruction Often without an inciting event or disorder
HALLMARK: positive DAT result TTP – life-threatening and requires timely diagnosis and treatment
CAUSES: HALLMARKS OF TTP:
Idiopathic o Thrombocytopenia
Viral and bacterial infection o Fever
Autoimmune conditions o Renal injury
Connective tissue disorder o MAHA
Lymphoproliferative malignancies o Neurologic dysfunction
Blood transfusion
LABORATORY FINDINGS:
Transplantations
Negative DAT result
AIHA Two primary subgroups based on binding temperatures Normal coagulation testing
WARM AIHA COLD AIHA Assessment of ADAMTS13 enzyme activity is diagnosing for TTP
More common than cold AIHA Cold agglutinin disease Result usually delayed
Making a presumptive diagnosis imperative
MECHANISM: IgG autoantibodies reaction MECHANISM: IgM autoantibodies reaction
with RBC protein antigens with RBC polysaccharide antigens causing PLASMIC SCORE – used to predict severely reduced ADAMTS13 enzyme activity and initiate
lysis on rewarming by complement fixation early treatment
and intravascular hemolysis TREATMENT:
IgG coated RBCs removed by Plasma exchange and glucocorticoids
reticuloendothelial macrophages and Plasma exchange removes affected platelet
sequestered in the spleen, sometimes Associated with infectious or malignant Autoantibodies while replenishing ADAMTS13 enzyme levels
leading to splenomegaly processes
o Mycoplasma pneumonia
o Mononucleosis PLASMA EXCHANGE IS SUPERIOR = FFP infusion is beneficial and should be started if
TREATMENT: TREATMENT: transfer to a plasma exchange-capable center is delayed
o Glucocorticoids o Supportive measures
o Management of the underlying o Avoidance of triggers OTHER MICROANGIOPATHIC HEMOLYTIC ANEMIA SYNDROMES
condition o Underlying disease management
o Blood transfusion
o Supportive care
HEMOLYTIC TRANSFUSION REACTIONS
CAUSE: alloantibodies that reacts with incompatible RBCs
CLINICAL SIGNIFICANCE: Hemolysis can range from acute to delayed, and can be life-
threatening
DRUG-INDUCED IMMUNE HEMOLYTIC ANEMIA
Rare
MECHANISM: drug-induced antibody formation a DAT result is positive in patients with this
condition
TREATMENT: involves removal of the offending agent
DRUG INDICED THROMBOTIC MICROANGIOPATHY (DI-TMA)
MECHANISM: drug induced antibodies formation or direct toxicity causing formation of
placement microthrombi
You might also like
- Ninja Nerd AnemiaDocument13 pagesNinja Nerd AnemiaAndra Bauer100% (4)
- Hematology Cell Morphology ChartDocument2 pagesHematology Cell Morphology ChartMiaoNo ratings yet
- PoikilocytosisDocument3 pagesPoikilocytosisJasonNo ratings yet
- 3 - Advances in The Diagnosis and Treatment of VasculitisDocument378 pages3 - Advances in The Diagnosis and Treatment of VasculitisAnonymous nGhxGKWXJr100% (1)
- 9 Hema Extrinsic RBC DefectsDocument2 pages9 Hema Extrinsic RBC DefectsGwen Kirsten AtayanNo ratings yet
- Hematology 4Document21 pagesHematology 4saad samyNo ratings yet
- HEMA 2 - Midterm Topic 1 - ADDITIONAL NOTESDocument6 pagesHEMA 2 - Midterm Topic 1 - ADDITIONAL NOTESLowenstein JenzenNo ratings yet
- RBC DisordersDocument8 pagesRBC DisordersDavid JohnNo ratings yet
- Diseases of The Newborn Part2Document6 pagesDiseases of The Newborn Part2sarguss14100% (1)
- Anemia DX TXDocument2 pagesAnemia DX TXProsanjit MajumderNo ratings yet
- CP RBC DisorderDocument15 pagesCP RBC DisorderDETECTIVE CONANNo ratings yet
- Anemia: Signs and SymptomsDocument6 pagesAnemia: Signs and SymptomsHarisree SNo ratings yet
- Approach To Anemia: - Reticulocyte Count Is Most Important TestDocument15 pagesApproach To Anemia: - Reticulocyte Count Is Most Important TestJanella SuerteNo ratings yet
- Hematology Trans 10Document6 pagesHematology Trans 10Claire GonoNo ratings yet
- 112 Lecture MidtermsDocument18 pages112 Lecture MidtermsRose Ann CammagayNo ratings yet
- 112 Lecture MidtermsDocument8 pages112 Lecture MidtermsRose Ann CammagayNo ratings yet
- Super Simplified Pathology Hematology - Dr. Priyanka SachdevDocument500 pagesSuper Simplified Pathology Hematology - Dr. Priyanka SachdevMohd SaquibNo ratings yet
- Amboss Hemolytic AnemiaDocument16 pagesAmboss Hemolytic AnemiaAhmed Ali100% (2)
- CBC (Complete Blood Count)Document38 pagesCBC (Complete Blood Count)yeshitla amsaluNo ratings yet
- Anemia SDocument8 pagesAnemia SCarlo SantosNo ratings yet
- RBC PathologyDocument7 pagesRBC PathologyKent CruzNo ratings yet
- Shanz - Clinpath Le1Document7 pagesShanz - Clinpath Le1Petrina XuNo ratings yet
- Hema 9th WeekDocument2 pagesHema 9th WeekGwen Kirsten AtayanNo ratings yet
- (PATHO) LEC 013 RBC-and-Bleeding-DisordersDocument20 pages(PATHO) LEC 013 RBC-and-Bleeding-DisordersEzhilNo ratings yet
- Hematology 101: Interpreting Lab Results - Patterns and PitfallsDocument55 pagesHematology 101: Interpreting Lab Results - Patterns and PitfallsAmorrita Puspita Ratu100% (1)
- RBC AnomaliesDocument5 pagesRBC AnomaliesThe16LoverrNo ratings yet
- Anemia - AMBOSSDocument2 pagesAnemia - AMBOSStgayuNo ratings yet
- Physiology Lab V2Document14 pagesPhysiology Lab V2Mohammed EljackNo ratings yet
- RED CELL MORPHOLOGY Tabulation SummaryDocument6 pagesRED CELL MORPHOLOGY Tabulation SummaryStephen YorNo ratings yet
- Chapter 1: An Overview of Clinical LaboratoryDocument13 pagesChapter 1: An Overview of Clinical LaboratoryAshley Tañamor100% (2)
- Anemia Workup - Approach Considerations, Investigation For Pathogenesis, Evaluation For Blood LossDocument14 pagesAnemia Workup - Approach Considerations, Investigation For Pathogenesis, Evaluation For Blood LossRahul SahadevanNo ratings yet
- Hemolytic Anemia: Song Qiaoqiao Hubei University of Science and Technology Internal Medicine DepartmentDocument66 pagesHemolytic Anemia: Song Qiaoqiao Hubei University of Science and Technology Internal Medicine DepartmentMEDS easyNo ratings yet
- Anemias: RBC Morphology & Approach To Diagnosis: Physiologic AdaptationsDocument5 pagesAnemias: RBC Morphology & Approach To Diagnosis: Physiologic AdaptationsASHLEY ALEXIS GUEVARRANo ratings yet
- Hematology Oncology - Anemia ApproachDocument1 pageHematology Oncology - Anemia ApproachEugen MNo ratings yet
- Anemia ApproachDocument1 pageAnemia ApproachLanaNo ratings yet
- Degenevie - HematologyDocument71 pagesDegenevie - Hematologykkq7fhkwvkNo ratings yet
- AnemiaDocument88 pagesAnemiaMans FansNo ratings yet
- Blood Cell AnomaliesDocument4 pagesBlood Cell AnomaliesCiullaeNo ratings yet
- Basic HematologyDocument69 pagesBasic HematologyDimas Bayu FirdausNo ratings yet
- RBC Morphology and InclusionsDocument3 pagesRBC Morphology and InclusionsDeomicah SolanoNo ratings yet
- Anemia TutoringDocument28 pagesAnemia TutoringngNo ratings yet
- Strategi Diagnosis AnemiaDocument49 pagesStrategi Diagnosis Anemianiniek yusidaNo ratings yet
- Anemia Hndout FR SeniorsDocument18 pagesAnemia Hndout FR Seniorschris andrieNo ratings yet
- An Approach To Anemia: Brad Lewis Director Hematology San Francisco General HospitalDocument47 pagesAn Approach To Anemia: Brad Lewis Director Hematology San Francisco General HospitalyapponNo ratings yet
- AnemiaDocument8 pagesAnemiasibanah menor100% (1)
- Clinical Haematology-Lecture SlidesDocument55 pagesClinical Haematology-Lecture SlidesShiv Sookun100% (1)
- Anemia, Polycythemia and Jaundice PDFDocument5 pagesAnemia, Polycythemia and Jaundice PDFAnshumaan PatraNo ratings yet
- AnemiaDocument16 pagesAnemiaAaron GarciaNo ratings yet
- Generalities of Blood and Its ElementsDocument3 pagesGeneralities of Blood and Its ElementsRem AlfelorNo ratings yet
- RBC ANOMALIES AND INCLUSIONS With Their Associated DiseasesDocument2 pagesRBC ANOMALIES AND INCLUSIONS With Their Associated DiseasesCamella Beatrice Lujan ValleNo ratings yet
- Intravascular Extravascular: Fe Storage Tibc SerumDocument2 pagesIntravascular Extravascular: Fe Storage Tibc Serumazhar hussinNo ratings yet
- RBC anomalies-ANEMIADocument19 pagesRBC anomalies-ANEMIAJeremiahNo ratings yet
- Reticulocyte Count: Esr: RBC Count: Reticulocyte Count: Low For Reticulocyte Count: Platelet Count: Packed Reticulocyte CountDocument3 pagesReticulocyte Count: Esr: RBC Count: Reticulocyte Count: Low For Reticulocyte Count: Platelet Count: Packed Reticulocyte CountVarshaa BharathiNo ratings yet
- (Trans) Chapter 16: Anemias - Red Blood Cell Morphology and Approach To DiagnosisDocument4 pages(Trans) Chapter 16: Anemias - Red Blood Cell Morphology and Approach To Diagnosisgotvelvet world dominationNo ratings yet
- Haematology: MAP 6.1 AnaemiaDocument12 pagesHaematology: MAP 6.1 AnaemiaGrecia BocuNo ratings yet
- Hematologi ModulDocument67 pagesHematologi ModulSyifa Mahmud Syukran Akbar100% (1)
- Hematology: Hemoglobinopathies TableDocument3 pagesHematology: Hemoglobinopathies TableMeevie Toledo0% (1)
- AnemiaDocument11 pagesAnemiaNada AmjadNo ratings yet
- CLINPATH 02.erythrocyte DisordersDocument13 pagesCLINPATH 02.erythrocyte DisordersCharisse Angelica MacedaNo ratings yet
- 9 Hema Extrinsic RBC DefectsDocument2 pages9 Hema Extrinsic RBC DefectsGwen Kirsten AtayanNo ratings yet
- 7.3 Hema Lab Diagnosis HemaDocument1 page7.3 Hema Lab Diagnosis HemaGwen Kirsten AtayanNo ratings yet
- 7.4 Hema Megaloblastic AnemiaDocument2 pages7.4 Hema Megaloblastic AnemiaGwen Kirsten AtayanNo ratings yet
- Hema 9th WeekDocument2 pagesHema 9th WeekGwen Kirsten AtayanNo ratings yet
- 7 HCT FixationDocument2 pages7 HCT FixationGwen Kirsten AtayanNo ratings yet
- 8 HCT Clearing, EmbeddingDocument1 page8 HCT Clearing, EmbeddingGwen Kirsten AtayanNo ratings yet
- 7 HCT FixationDocument3 pages7 HCT FixationGwen Kirsten AtayanNo ratings yet
- 7.2 HCT DecalcificationDocument1 page7.2 HCT DecalcificationGwen Kirsten AtayanNo ratings yet
- Project in Mapeh: Alexander Jake A. Diaz 6 EarthDocument12 pagesProject in Mapeh: Alexander Jake A. Diaz 6 EarthGwen Kirsten AtayanNo ratings yet
- Collagen Stimulants in Facial Rejuvenation A Systematic Review - Millar-Hume, 2020Document4 pagesCollagen Stimulants in Facial Rejuvenation A Systematic Review - Millar-Hume, 2020Rafael Autran Cavalcante AraújoNo ratings yet
- Rheumatoid ArthritisDocument25 pagesRheumatoid ArthritisGandung PrakosoNo ratings yet
- Quality IndicatorsDocument15 pagesQuality IndicatorsSanjay Rajpal60% (5)
- First Aid Scenario CardsDocument2 pagesFirst Aid Scenario CardsIlaha DamirovaNo ratings yet
- Drug Study and LaboratoryDocument13 pagesDrug Study and LaboratoryGEOMHAI CATBAGANNo ratings yet
- Pucat Dan Anemia Pada AnakDocument21 pagesPucat Dan Anemia Pada AnakHerry WaraNo ratings yet
- Newborn Bathing ...Document3 pagesNewborn Bathing ...alloushi100% (3)
- Concept MapDocument1 pageConcept MapKatrineNo ratings yet
- Neurovascular Interactions in Dental PulpDocument6 pagesNeurovascular Interactions in Dental PulpSaraMAminNo ratings yet
- Application & Medical Forms Cir 2Document2 pagesApplication & Medical Forms Cir 2Ivan FrancisNo ratings yet
- What Are The Different Ways in Which A Genetic Condition Can Be Inherited?Document4 pagesWhat Are The Different Ways in Which A Genetic Condition Can Be Inherited?Chad ParasNo ratings yet
- Nervous System ProformaDocument10 pagesNervous System ProformaEBNo ratings yet
- NP 4Document4 pagesNP 4Hamad RayhanNo ratings yet
- Introduction To MicrobiologyDocument51 pagesIntroduction To MicrobiologyGabz GabbyNo ratings yet
- Kidney Stone Detection Using Image Processing and Convolutional Neural NetworksDocument5 pagesKidney Stone Detection Using Image Processing and Convolutional Neural NetworksInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Mouthwash From Ethanol Leaf Extract Of: Jurnal Ilmiah Farmako BahariDocument11 pagesMouthwash From Ethanol Leaf Extract Of: Jurnal Ilmiah Farmako BahariJr SparkNo ratings yet
- Q3 S10 Week 1 Lecture or NotesDocument5 pagesQ3 S10 Week 1 Lecture or NotesJuben OdalNo ratings yet
- 1NUR8 ABRIO Summative AssessmentDocument3 pages1NUR8 ABRIO Summative AssessmentKYRA CHEYENNE NICHOLLE ABRIO100% (1)
- Eight Types of DementiaDocument4 pagesEight Types of DementiaShradha AlkaNo ratings yet
- Jurnal Internasional 55 PDFDocument5 pagesJurnal Internasional 55 PDFPutri UtamiNo ratings yet
- Chapter 5 Crystalline Lens - Abdelmonem Hamed EditionDocument16 pagesChapter 5 Crystalline Lens - Abdelmonem Hamed EditionAbdelmonem HamedNo ratings yet
- Non Medical Prescribing Using The British National Formulary PDFDocument6 pagesNon Medical Prescribing Using The British National Formulary PDFRyan MwNo ratings yet
- Hamilton Depression Rating Scale (HDRS)Document2 pagesHamilton Depression Rating Scale (HDRS)Rian Candra Ibrahim100% (1)
- Side Effect Information: Post Vaccine Dose #2 of Moderna VaccineDocument1 pageSide Effect Information: Post Vaccine Dose #2 of Moderna VaccineLiza PreissNo ratings yet
- Advanced Mechanical VentilationDocument96 pagesAdvanced Mechanical VentilationMukhtar KhanNo ratings yet
- Safety Blood Bank By-Dr - Mohamed Barouni 222Document31 pagesSafety Blood Bank By-Dr - Mohamed Barouni 222Hannan AliNo ratings yet
- The "50-50 Criteria" On Postoperative Day 5: An Accurate Predictor of Liver Failure and Death After HepatectomyDocument6 pagesThe "50-50 Criteria" On Postoperative Day 5: An Accurate Predictor of Liver Failure and Death After HepatectomyMarcio Apodaca-RuedaNo ratings yet
- NP IiiDocument13 pagesNP IiiVia LatrasNo ratings yet
- Abdominal PainDocument3 pagesAbdominal PainReiciel Joy Gombio100% (2)