Professional Documents
Culture Documents
Jay Davidson - The Essential Guide To Calming Lyme Induced Inflamation
Jay Davidson - The Essential Guide To Calming Lyme Induced Inflamation
Uploaded by
nUno MichaelsCopyright:
Available Formats
You might also like
- Understanding Immune Health Mayo ClinicDocument8 pagesUnderstanding Immune Health Mayo ClinicCarmel HarelNo ratings yet
- Jay Davidson Symptoms of A Parasitic InfectionDocument4 pagesJay Davidson Symptoms of A Parasitic InfectionNaga BalaNo ratings yet
- Biodiversity of Micro-OrganismsDocument32 pagesBiodiversity of Micro-Organismsapi-20234922250% (2)
- The Essential Guide To Calming Lyme-Induced InflammationDocument7 pagesThe Essential Guide To Calming Lyme-Induced InflammationDorian GrayNo ratings yet
- Trovanje HranomDocument14 pagesTrovanje HranomLamija EmricNo ratings yet
- Autoimmune Diseases: Immune SystemDocument11 pagesAutoimmune Diseases: Immune Systemmaria nataliaNo ratings yet
- HKDSE Biology Part 3 Health & DiseasesDocument17 pagesHKDSE Biology Part 3 Health & DiseasesTSZ YAN CHEUNGNo ratings yet
- Reporting ScienceDocument20 pagesReporting ScienceYasuhiro Hinggo EscobilloNo ratings yet
- Ebook Top 26 Shopping List Supermarket Foods 1Document19 pagesEbook Top 26 Shopping List Supermarket Foods 1Dragica BernotNo ratings yet
- Arthritis RheumatoidDocument15 pagesArthritis Rheumatoidputri rahmadaniNo ratings yet
- Lyme Disease: Submitted byDocument6 pagesLyme Disease: Submitted byhsmolenggeNo ratings yet
- Leaky Gut: The Guide To Treating The Source of Allergies, Joint Pain, Digestive Diseases and MoreDocument15 pagesLeaky Gut: The Guide To Treating The Source of Allergies, Joint Pain, Digestive Diseases and Moresurveytryer2No ratings yet
- Toxic Mold It May Be Harming Your Health More Than You Know Eguide 2555Document17 pagesToxic Mold It May Be Harming Your Health More Than You Know Eguide 2555Petite PoubelleNo ratings yet
- Diseases and VaccinesDocument37 pagesDiseases and Vaccinesraghu ramNo ratings yet
- What Makes You Ill: Made By: Amna AmeenDocument7 pagesWhat Makes You Ill: Made By: Amna Ameenamna ameen StudentNo ratings yet
- Introduction To Disease and Vaccines What Is A Disease?Document2 pagesIntroduction To Disease and Vaccines What Is A Disease?Sue Adames de VelascoNo ratings yet
- Disorders of NSDocument4 pagesDisorders of NSThe KhanNo ratings yet
- Fibromyalgia: The complete guide to fibromyalgia, understanding fibromyalgia, and reducing pain and symptoms of fibromyalgia with simple treatment methods!From EverandFibromyalgia: The complete guide to fibromyalgia, understanding fibromyalgia, and reducing pain and symptoms of fibromyalgia with simple treatment methods!Rating: 2 out of 5 stars2/5 (2)
- Final Product 2024-05-01 16 06 36Document12 pagesFinal Product 2024-05-01 16 06 36api-711508569No ratings yet
- Diseases and VaccinesDocument22 pagesDiseases and VaccineslakshNo ratings yet
- 6246bb700cf2ee69840e3596 OriginalDocument24 pages6246bb700cf2ee69840e3596 Originalsoma5koshasNo ratings yet
- Margaret Christensen Got Mold Now What Final EditDocument5 pagesMargaret Christensen Got Mold Now What Final EditMarcelo FernandezNo ratings yet
- Guillain Barré SyndromeDocument20 pagesGuillain Barré Syndromelourdes kusumadiNo ratings yet
- CandidaguideDocument12 pagesCandidaguideNica norNo ratings yet
- Lyme Disease 1Document1 pageLyme Disease 1api-547400638No ratings yet
- Autoimmune Disorders: Description of The DisabilityDocument6 pagesAutoimmune Disorders: Description of The DisabilityCemara Boro SaestiNo ratings yet
- Autoimmune GuidebookDocument20 pagesAutoimmune Guidebookedurodica7No ratings yet
- Nerve Pain and Nerve Damage 2Document17 pagesNerve Pain and Nerve Damage 2Ryan BediNo ratings yet
- Lyme Disease 1Document14 pagesLyme Disease 1api-677928137No ratings yet
- Margaret-Christensen Got Mold Now What UpdatedDocument5 pagesMargaret-Christensen Got Mold Now What UpdatedMirela Olarescu100% (1)
- The Effects of Chronic Stress: Stress Is Your Body's Way of Responding To Any KindDocument3 pagesThe Effects of Chronic Stress: Stress Is Your Body's Way of Responding To Any KindXanthophile ShopeeNo ratings yet
- CB5 - Revision - Summary Filled inDocument3 pagesCB5 - Revision - Summary Filled inSiaNo ratings yet
- Got Mold? Now What?: Hope For Health and HomeDocument5 pagesGot Mold? Now What?: Hope For Health and HomeFlo BorsNo ratings yet
- ACUTE INFLAMMATION VS CHRONIC INFLAMMATION Assignment #2 (CU-1774-2020)Document17 pagesACUTE INFLAMMATION VS CHRONIC INFLAMMATION Assignment #2 (CU-1774-2020)Ali Aasam KhanNo ratings yet
- Black Neon Green Neon Pink Trendy Illustrative Creative Presentation 2Document21 pagesBlack Neon Green Neon Pink Trendy Illustrative Creative Presentation 2Sherry-Ann TulauanNo ratings yet
- Multiple Sclerosis 1.1. Definition: Immunologic DisorderDocument21 pagesMultiple Sclerosis 1.1. Definition: Immunologic Disordergrazelantonette.calubNo ratings yet
- Guillain-Barré Syndrome Fact Sheet - National Institute of Neurological Disorders and StrokeDocument9 pagesGuillain-Barré Syndrome Fact Sheet - National Institute of Neurological Disorders and StrokeCarl MacCordNo ratings yet
- Iitei: NieieiircDocument1 pageIitei: Nieieiircapi-21190143No ratings yet
- PBL 1 ResultDocument11 pagesPBL 1 ResultNabilla MahdiNo ratings yet
- Parasites and SusceptibilityDocument13 pagesParasites and SusceptibilityCaroline D.No ratings yet
- Chapter 1 DiseasesDocument10 pagesChapter 1 DiseasesQaran PrintingNo ratings yet
- DISEASES FINALDocument29 pagesDISEASES FINALnitishkumarswain2No ratings yet
- RA and FMDocument3 pagesRA and FMSNo ratings yet
- PainDocument5 pagesPainSyamsulAriefNo ratings yet
- Causes and Prevention of DiseasesDocument4 pagesCauses and Prevention of DiseasesSusan Hepzi100% (1)
- 6B-Biology Notes - Diseases and HygieneDocument13 pages6B-Biology Notes - Diseases and HygieneJagrity SinghNo ratings yet
- Depression and CopingDocument18 pagesDepression and CopingAlcesua EalmyelaNo ratings yet
- Tle Lead PoisoningDocument2 pagesTle Lead PoisoningXhaNo ratings yet
- HEALTH 9 QUARTER2 MODULE3 WeeK5-6Document9 pagesHEALTH 9 QUARTER2 MODULE3 WeeK5-6Heidee Basas100% (3)
- University of Northern PhilippinesDocument4 pagesUniversity of Northern PhilippinesCatherine PradoNo ratings yet
- English Final ProjectDocument16 pagesEnglish Final ProjectAry SanucasNo ratings yet
- Yoga 4 Immune SystemDocument33 pagesYoga 4 Immune Systemsukunath100% (1)
- Psy 325 LecturesDocument14 pagesPsy 325 LecturesErika BalaniNo ratings yet
- Virus, Viroids and PrionsDocument29 pagesVirus, Viroids and PrionscatherinejoaquinNo ratings yet
- HEALTH 4TH Q NCD - For Blended LearnersDocument35 pagesHEALTH 4TH Q NCD - For Blended LearnersAlmighty OperyNo ratings yet
- Health Problems Most Common in School Aged ChildrenDocument15 pagesHealth Problems Most Common in School Aged ChildrenAsterlyn ConiendoNo ratings yet
- GR - 9 - Revision Notes - Why We Do Fall IllDocument9 pagesGR - 9 - Revision Notes - Why We Do Fall IllAditi KumariNo ratings yet
- Examples of DrugsDocument29 pagesExamples of DrugsEdwins MaranduNo ratings yet
- Symptoms: What Are The Complications of Insomnia?Document4 pagesSymptoms: What Are The Complications of Insomnia?Mohamad nazrinNo ratings yet
- F&E ExamDocument3 pagesF&E ExamDino PringNo ratings yet
- (Burnett James C.) Tumours of The Breast and TheirDocument78 pages(Burnett James C.) Tumours of The Breast and TheirRajendraNo ratings yet
- Benefit Packages (Private)Document103 pagesBenefit Packages (Private)You Are Not Wasting TIME HereNo ratings yet
- ALU 101 Sample QuestionsDocument4 pagesALU 101 Sample Questionsartlover30No ratings yet
- Case 013: Fever in A Cirrhotic PatientDocument5 pagesCase 013: Fever in A Cirrhotic PatientFitri 1997No ratings yet
- Chaves 2020Document10 pagesChaves 2020Matheus CastroNo ratings yet
- 08-Hand-Arm VibrationDocument35 pages08-Hand-Arm Vibrationjimmy tiarlinaNo ratings yet
- Read Online Textbook Second A Gay Hockey Romance La Storm Book 2 RJ Scott Ebook All Chapter PDFDocument22 pagesRead Online Textbook Second A Gay Hockey Romance La Storm Book 2 RJ Scott Ebook All Chapter PDFrodney.ellison150100% (3)
- MILLETSDocument11 pagesMILLETSVeer VijayNo ratings yet
- ACOG Combined List of TitlesDocument13 pagesACOG Combined List of TitlesLaura RojasNo ratings yet
- Reflection AssignmentDocument5 pagesReflection Assignmentapi-659065431No ratings yet
- Transmission Sars Cov-2Document7 pagesTransmission Sars Cov-2Ikmah FauzanNo ratings yet
- Endomaterial Cancer-1Document28 pagesEndomaterial Cancer-1A.H.ANo ratings yet
- Fat-And Water-Soluble VitaminsDocument9 pagesFat-And Water-Soluble VitaminsJessa Mae OhaoNo ratings yet
- Water and ElectrolytesDocument39 pagesWater and ElectrolytesevbptrprnrmNo ratings yet
- Communicable Diseases HandoutDocument7 pagesCommunicable Diseases Handoutariane100% (1)
- Cefuroxime Drug StudyDocument1 pageCefuroxime Drug StudyACOB, Jamil C.No ratings yet
- Lippincotts Antiarrhythmics 5Document1 pageLippincotts Antiarrhythmics 5Wijdan HatemNo ratings yet
- Week 14 - Leukocyte Abnormalities and Non-Malignant Leukocyte DisordersDocument83 pagesWeek 14 - Leukocyte Abnormalities and Non-Malignant Leukocyte DisordersSheine EspinoNo ratings yet
- Nursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationDocument2 pagesNursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationOmar IzzoNo ratings yet
- Basic Encoding ActivityDocument3 pagesBasic Encoding ActivityJHOMER CABANTOGNo ratings yet
- Polycythemia: (Primary & Secondary)Document16 pagesPolycythemia: (Primary & Secondary)Vanessa Camille DomingoNo ratings yet
- PA1 HandoutDocument22 pagesPA1 HandoutIligan, JamaicahNo ratings yet
- 7.2 FTAT Coding Registers Case ScenariosDocument25 pages7.2 FTAT Coding Registers Case ScenariosGosa MohammedNo ratings yet
- 47-Article Text-305-1-10-20220731Document10 pages47-Article Text-305-1-10-20220731alyn30274No ratings yet
- ANT Handbook 2023Document84 pagesANT Handbook 2023latibaleni02No ratings yet
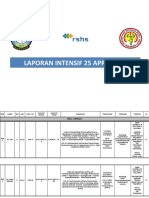
- Laporan Intensif 25 April 2021Document21 pagesLaporan Intensif 25 April 2021bosnia agusNo ratings yet
- Avian Influenza H5N1 VirusDocument27 pagesAvian Influenza H5N1 VirusHarsh Purwar100% (3)
- DGHS IPHS Sub-Dist Hosps 31 To 50Document113 pagesDGHS IPHS Sub-Dist Hosps 31 To 50shanmugapriyasankarNo ratings yet
- WEEK 2 Management of Patients With Chest and Lower Respiratory Tract DisordersDocument9 pagesWEEK 2 Management of Patients With Chest and Lower Respiratory Tract DisordersTin tinNo ratings yet
Jay Davidson - The Essential Guide To Calming Lyme Induced Inflamation
Jay Davidson - The Essential Guide To Calming Lyme Induced Inflamation
Uploaded by
nUno MichaelsOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jay Davidson - The Essential Guide To Calming Lyme Induced Inflamation
Jay Davidson - The Essential Guide To Calming Lyme Induced Inflamation
Uploaded by
nUno MichaelsCopyright:
Available Formats
The Essential
Guide to Calming
Lyme-Induced
Inflammation
People with chronic illnesses, like Lyme disease, usually have a long
list of health problems that have them digging through various
internet sources (hopefully, reputable ones) for answers. Those
seemingly separate issues could boil down to one central source —
chronic Lyme disease.
Indeed, chronic Lyme disease has many vague, erratic, and
concealed symptoms. What’s more, chronic illnesses have so many
symptoms in common and can look a lot like one another. Mapping
out your personal scenario can be challenging, since testing for
Lyme disease may be unreliable.
Chronic Lyme Disease
During the early stages of Lyme disease, it may seem like you have a flu bug. You could
have aches, pains, stiffness, and swollen glands. These symptoms may last a few weeks. If
caught in the early stages, Lyme disease may be easier to diagnose and treat.
Chronic Lyme disease, or “late-stage Lyme,” is much different. Signs of this chronic illness
may arise gradually, over time. Or, they may be ongoing, having never entirely resolved
with earlier treatment. In some cases, physical or emotional stress may have an impact,
and push the disease front and center.
Blood tests often fail to diagnose this type of Lyme disease, as the acute phase is past. The
corkscrew-shaped Lyme bacteria are no longer floating in the bloodstream; they have
drilled down into the tissues where they are harder to see. Plus, the infection can confuse
your immune system. It may not create the antibodies required to get a positive test
result.
Thus, the source of your pain and inflammation can be elusive. Yet, Lyme disease
symptoms may be in plain sight. You may develop long-term issues like joint pain, severe
and debilitating fatigue, headaches, and trouble concentrating. These may become more
crippling and devastating over time.
Lyme Disease Contributes to
Immune System Dysfunction
Chronic Lyme disease can cause a substantial amount of inflammation, due in part to
taxing your immune system. The Lyme bacteria provoke your immune cells to produce
small proteins called cytokines. These substances generate inflammation to fight the
infection.[1]
But, another problem may manifest — your immune system’s activity may not return to
normal — even after the infection is knocked back. It may go into a hyperactive state,
continuing to fight just as hard as if it was battling a new threat.
This is partly the case because the bacteria are masters of disguise. They can mutate and
change form. Over and over, the immune cells see them as new threats. The immune cells
search for many invaders, rather than merely the original one. Then, the immune system is
continually in hyperimmune emergency mode, which continues to cause painful
inflammation.
So, the effect of Lyme disease on the immune system is both suppression
(downregulation) and too much stimulation (upregulation). In this scenario, balancing
immune function (immune modulation) is critical.
Lyme Disease Causes
Joint Inflammation
Chronic Lyme disease doesn’t discriminate. You could be the fittest,
healthiest person before you contract it. It will still try to take you down.
This disease damages the joints and can cause excruciating pain. You
might become unable to enjoy your former quality of life.
Borrelia burgdorferi, the bacteria that causes Lyme disease, love to
hang out in the joints and connective tissues, including cartilage,
tendons, and ligaments. The bacteria bind to collagen in these
connective tissues. Then, they break it down and destroy it. If your body
tries to regenerate these tissues, the microbes can disrupt its efforts.[2]
The Lyme disease bacteria are dependent on your body for nutrients.
Since they can’t make specific proteins, they’ll steal them from your
joints. They’re especially fond of a gel-like substance called hyaluronic
acid. Without it, connective tissues can be brittle, and joints can be stiff.
These stealthy bacteria also cause inflammation in your joints.
Fragments of borrelia remain in joints, even after the microbes are
killed off. This is triggered by a specific substance in their cell walls
(peptidoglycan) that is dumped into the surrounding environment. The
borrelia litterbugs cause you to appear to have arthritis, but the real
culprit is chronic Lyme disease.[3]
The peptidoglycan stays in the synovial fluid, which is the thick liquid
that lubricates the joint and allows it to move smoothly. It causes
ongoing inflammation as the immune system continues to respond.[4]
Lyme Disease Causes
Brain Inflammation
Lyme is an inflammatory disease that affects the nervous system adversely, as well. This
fact is both accurate and terrifying since damage to the brain is a dreaded consequence of
illness.
Lyme spirochetes cross the blood-brain barrier, causing inflammation in the central
nervous system. The brains of patients with chronic Lyme disease show chemical changes
and widespread inflammation.[5] Some of those infected with Lyme disease will ONLY
show nervous system symptoms and signs — they don’t have the joint and body pains.
Lyme neuroborreliosis is the scientific name for the effects B. burgdorferi may produce in
both the peripheral and central nervous systems.[6] The disease and its associated
symptoms develop as a result of inflammatory changes in the central nervous system
(brain and spinal cord), spinal nerves, and dorsal root ganglia.
Common neurocognitive problems include:[7]
Brain fog Sleep disorders
Poor memory Dyslexic-like errors when writing or
Slower thinking speed speaking
Difficulty retrieving words Spatial disorientation
Attention and focus issues Confusion
Irritability, sometimes extreme Emotional responses that are irregular or
out of proportion to the situation at hand
(mood lability)
Neurological system impairments may include:[8]
Numbness Bell's palsy (paralysis of the facial muscles)
Pain Meningitis symptoms such as severe
Fatigue headache, fever, and stiff neck
Weakness Nerve damage in the arms and legs
Increased sensitivity to specific Visual disturbances
frequencies and volume ranges of sound Impaired fine motor control
(auditory hyperacusis)
Around 40% of individuals with chronic Lyme develop neurological issues. Lyme disease
can also affect the neurotransmitters, manifesting as anxiety, depression, bipolar disorder,
anorexia, obsessive-compulsive disorder, or schizophrenia. Major depression develops in
many chronic Lyme patients, which contributes to thoughts of suicide. Panic attacks and
aggression are a sign of the spirochete’s attack on the central nervous system, as well.[9,10]
Address Inflammation
with Dietary Adjustments
It’s plain to see that calming inflammation in the body could provide some much-needed
relief for people with Lyme disease. Eating an anti-inflammatory diet is helpful. Some foods
and beverages are associated with an increased risk of inflammation. Consider reducing or
cutting out:
Sugar and sugary beverages Processed snack foods
Refined carbs Processed seed and vegetable oils (like corn,
Gluten canola, and soybean)
Wheat and corn (due to pesticide residues, Foods with partially hydrogenated (trans-
mold, fungus) fat) ingredients
Pre-packaged and fast foods Genetically modified foods
Processed meats Alcohol
You can also ADD anti-inflammatory foods, including:
Vegetables (particularly cruciferous veggies) Wild-caught fatty fish, including salmon,
Low-sugar fruits sardines, herring, anchovies, and mackerel
High-fat fruits, including avocados and Dark chocolate (in moderation)
olives Spices, including turmeric, ginger, garlic,
Healthy fats, including olive oil, avocado oil, cinnamon, clove, and cayenne
and coconut oil Green tea
Nuts Red wine (in moderation)
Remember to “eat the rainbow” of fruits and vegetables. Also, eat organic, wild-caught,
and pasture-raised produce and meats whenever possible.
Address Inflammation
with Anti-Inflammatory
Herbs and Supplements
Nature offers many plant-based solutions to help calm
inflammation. These may be especially potent when taken as
extracts and used in combination. Collectively, the following
may be more powerful together, rather than individually:
Broccoli sprouts
Mulberry
Artichoke leaf
Blueberry
Wheatgrass
Acai
Pineapple bromelain
Olive leaf
Citrulline (a non-essential amino acid)
Pomegranate
Astaxanthin (a naturally-occurring carotenoid)
General Recommendations for
Lyme-Associated Inflammation
Chronic, low-grade systemic inflammation is a significant contributor to chronic
diseases. Besides the above recommendations, here are a few more to take to
heart:
Get exercise. Physical activity can decrease inflammatory markers, reducing
your risk of Lyme symptoms and chronic disease.[11]
Sleep well.
Both quality and quantity of sleep are extremely critical. Manage
inflammation by focusing on healthy sleep habits.[12]
Obesity
Manage your weight. causes chronic, low-grade inflammation.[13]
Balance
your
blood
sugar
level.
Blood sugar imbalances play a role in
inflammation, increasing the likelihood of insulin resistance, metabolic
syndrome, and diabetes.[14]
Clear environmental toxins.
Daily exposure to toxins, such as chemicals,
pesticides, heavy metals, mycotoxins (from mold), radioactive metals, toxins
released by pathogens, and much more, contribute to inflammation. Reduce
your exposure to these when possible, and detoxify your body to clear them.
As you can see, no matter what you are experiencing health-wise, inflammation
is a likely factor. Since inflammation is involved in so many health conditions, and
the world presents inflammatory environmental challenges daily, keeping
inflammation in check is vital to staying healthy and aging well. Even individuals
who have no health challenges may want to consider keeping tabs on
inflammation.
Lyme disease patients may develop persistent, painful inflammatory issues. If
you’ve been treated for Lyme disease and still feel unwell, your immune system’s
inflammatory response may be out of whack. See your functional medicine
provider or natural health expert to discuss personalized options for managing
your symptoms.
Powered by:
For more information, visit www.MicrobeFormulas.com. At Microbe Formulas, we
live by a simple standard. Creating supplements that work is what we do. Restoring
hope and health is who we are. We’ll help you create Your Roadmap to Health. If
you're chronically ill and looking for solutions, an effective roadmap is critical to your
success. We'd love to help guide you on your path to healing and recovery!
Source:
. Strle, Klemen, et al. “T-Helper 17 Cell Cytokine Responses in Lyme
Disease Correlate With Borrelia burgdorferi Antibodies During Early
Infection and With Autoantibodies Late in the Illness in Patients
With Antibiotic-Refractory Lyme Arthritis.” Clinical Infectious
Diseases, vol. 64, no. 7, 1 April 2017.
. Zambrano, Maria C, et al. “Borrelia Burgdorferi Binds to, Invades, and
Colonizes Native Type I Collagen Lattices.” Infection and Immunity,
American Society for Microbiology, vol. 72, no. 6, June 2004.
. Ross, John. “Chronic Lyme Arthritis: A Mystery Solved?” Harvard
Health Blog, 7 Oct. 2019.
. “Lyme Disease's Arthritis Inflammation Trigger Identified.” GEN, 18
June 2019.
. “New Scan Technique Reveals Brain Inflammation Associated with
Post-Treatment Lyme Disease Syndrome.” Johns Hopkins Medicine
Newsroom, 5 Feb 2019.
. Ramesh, Geeta et al. “Inflammation in the pathogenesis of lyme
neuroborreliosis.” The American Journal of Pathology, vol 185, no. 5,
May 2015.
. Westervelt, Holly James and McCaffrey, Robert J.
“Neuropsychological Functioning in Chronic Lyme Disease.”
Neuropsychology Review, U.S. National Library of Medicine, vol. 12,
no. 3, Sept 2002.
. “Neurological Complications of Lyme Disease Information Page.”
National Institute of Neurological Disorders and Stroke, U.S.
Department of Health and Human Services, n.d.
. Fallon, B A and Nields, J A. “Lyme Disease: a Neuropsychiatric
Illness.” The American Journal of Psychiatry, U.S. National Library of
Medicine, vol. 151, no. 11, Nov 1994,
. Bransfield, Robert C. “Suicide and Lyme and associated diseases.”
Neuropsychiatric Disease and Treatment, vol. 13, 16 Jun 2017
. Pedersen, Bente Klarlund. “The Anti-Inflammatory Effect of Exercise:
Its Role in Diabetes and Cardiovascular Disease Control.” Essays in
Biochemistry, U.S. National Library of Medicine, vol. 42, 2006.
. Mullington, Janet M et al. “Sleep Loss and Inflammation.” Best
Practice & Research. Clinical Endocrinology & Metabolism, U.S.
National Library of Medicine, vol. 24, no. 5, Oct 2010.
. Vandanmagsar, Bolormaa et al. “The NLRP3 Inflammasome
Instigates Obesity-Induced Inflammation and Insulin Resistance.”
Nature Medicine, vol. 17, no. 2, Feb 2011.
. Romeo, Giulio R et al. “Metabolic Syndrome, Insulin Resistance, and
Roles of Inflammation--Mechanisms and Therapeutic Targets.”
Arteriosclerosis, Thrombosis, and Vascular Biology, vol. 32, no. 8, Aug
2012.
You might also like
- Understanding Immune Health Mayo ClinicDocument8 pagesUnderstanding Immune Health Mayo ClinicCarmel HarelNo ratings yet
- Jay Davidson Symptoms of A Parasitic InfectionDocument4 pagesJay Davidson Symptoms of A Parasitic InfectionNaga BalaNo ratings yet
- Biodiversity of Micro-OrganismsDocument32 pagesBiodiversity of Micro-Organismsapi-20234922250% (2)
- The Essential Guide To Calming Lyme-Induced InflammationDocument7 pagesThe Essential Guide To Calming Lyme-Induced InflammationDorian GrayNo ratings yet
- Trovanje HranomDocument14 pagesTrovanje HranomLamija EmricNo ratings yet
- Autoimmune Diseases: Immune SystemDocument11 pagesAutoimmune Diseases: Immune Systemmaria nataliaNo ratings yet
- HKDSE Biology Part 3 Health & DiseasesDocument17 pagesHKDSE Biology Part 3 Health & DiseasesTSZ YAN CHEUNGNo ratings yet
- Reporting ScienceDocument20 pagesReporting ScienceYasuhiro Hinggo EscobilloNo ratings yet
- Ebook Top 26 Shopping List Supermarket Foods 1Document19 pagesEbook Top 26 Shopping List Supermarket Foods 1Dragica BernotNo ratings yet
- Arthritis RheumatoidDocument15 pagesArthritis Rheumatoidputri rahmadaniNo ratings yet
- Lyme Disease: Submitted byDocument6 pagesLyme Disease: Submitted byhsmolenggeNo ratings yet
- Leaky Gut: The Guide To Treating The Source of Allergies, Joint Pain, Digestive Diseases and MoreDocument15 pagesLeaky Gut: The Guide To Treating The Source of Allergies, Joint Pain, Digestive Diseases and Moresurveytryer2No ratings yet
- Toxic Mold It May Be Harming Your Health More Than You Know Eguide 2555Document17 pagesToxic Mold It May Be Harming Your Health More Than You Know Eguide 2555Petite PoubelleNo ratings yet
- Diseases and VaccinesDocument37 pagesDiseases and Vaccinesraghu ramNo ratings yet
- What Makes You Ill: Made By: Amna AmeenDocument7 pagesWhat Makes You Ill: Made By: Amna Ameenamna ameen StudentNo ratings yet
- Introduction To Disease and Vaccines What Is A Disease?Document2 pagesIntroduction To Disease and Vaccines What Is A Disease?Sue Adames de VelascoNo ratings yet
- Disorders of NSDocument4 pagesDisorders of NSThe KhanNo ratings yet
- Fibromyalgia: The complete guide to fibromyalgia, understanding fibromyalgia, and reducing pain and symptoms of fibromyalgia with simple treatment methods!From EverandFibromyalgia: The complete guide to fibromyalgia, understanding fibromyalgia, and reducing pain and symptoms of fibromyalgia with simple treatment methods!Rating: 2 out of 5 stars2/5 (2)
- Final Product 2024-05-01 16 06 36Document12 pagesFinal Product 2024-05-01 16 06 36api-711508569No ratings yet
- Diseases and VaccinesDocument22 pagesDiseases and VaccineslakshNo ratings yet
- 6246bb700cf2ee69840e3596 OriginalDocument24 pages6246bb700cf2ee69840e3596 Originalsoma5koshasNo ratings yet
- Margaret Christensen Got Mold Now What Final EditDocument5 pagesMargaret Christensen Got Mold Now What Final EditMarcelo FernandezNo ratings yet
- Guillain Barré SyndromeDocument20 pagesGuillain Barré Syndromelourdes kusumadiNo ratings yet
- CandidaguideDocument12 pagesCandidaguideNica norNo ratings yet
- Lyme Disease 1Document1 pageLyme Disease 1api-547400638No ratings yet
- Autoimmune Disorders: Description of The DisabilityDocument6 pagesAutoimmune Disorders: Description of The DisabilityCemara Boro SaestiNo ratings yet
- Autoimmune GuidebookDocument20 pagesAutoimmune Guidebookedurodica7No ratings yet
- Nerve Pain and Nerve Damage 2Document17 pagesNerve Pain and Nerve Damage 2Ryan BediNo ratings yet
- Lyme Disease 1Document14 pagesLyme Disease 1api-677928137No ratings yet
- Margaret-Christensen Got Mold Now What UpdatedDocument5 pagesMargaret-Christensen Got Mold Now What UpdatedMirela Olarescu100% (1)
- The Effects of Chronic Stress: Stress Is Your Body's Way of Responding To Any KindDocument3 pagesThe Effects of Chronic Stress: Stress Is Your Body's Way of Responding To Any KindXanthophile ShopeeNo ratings yet
- CB5 - Revision - Summary Filled inDocument3 pagesCB5 - Revision - Summary Filled inSiaNo ratings yet
- Got Mold? Now What?: Hope For Health and HomeDocument5 pagesGot Mold? Now What?: Hope For Health and HomeFlo BorsNo ratings yet
- ACUTE INFLAMMATION VS CHRONIC INFLAMMATION Assignment #2 (CU-1774-2020)Document17 pagesACUTE INFLAMMATION VS CHRONIC INFLAMMATION Assignment #2 (CU-1774-2020)Ali Aasam KhanNo ratings yet
- Black Neon Green Neon Pink Trendy Illustrative Creative Presentation 2Document21 pagesBlack Neon Green Neon Pink Trendy Illustrative Creative Presentation 2Sherry-Ann TulauanNo ratings yet
- Multiple Sclerosis 1.1. Definition: Immunologic DisorderDocument21 pagesMultiple Sclerosis 1.1. Definition: Immunologic Disordergrazelantonette.calubNo ratings yet
- Guillain-Barré Syndrome Fact Sheet - National Institute of Neurological Disorders and StrokeDocument9 pagesGuillain-Barré Syndrome Fact Sheet - National Institute of Neurological Disorders and StrokeCarl MacCordNo ratings yet
- Iitei: NieieiircDocument1 pageIitei: Nieieiircapi-21190143No ratings yet
- PBL 1 ResultDocument11 pagesPBL 1 ResultNabilla MahdiNo ratings yet
- Parasites and SusceptibilityDocument13 pagesParasites and SusceptibilityCaroline D.No ratings yet
- Chapter 1 DiseasesDocument10 pagesChapter 1 DiseasesQaran PrintingNo ratings yet
- DISEASES FINALDocument29 pagesDISEASES FINALnitishkumarswain2No ratings yet
- RA and FMDocument3 pagesRA and FMSNo ratings yet
- PainDocument5 pagesPainSyamsulAriefNo ratings yet
- Causes and Prevention of DiseasesDocument4 pagesCauses and Prevention of DiseasesSusan Hepzi100% (1)
- 6B-Biology Notes - Diseases and HygieneDocument13 pages6B-Biology Notes - Diseases and HygieneJagrity SinghNo ratings yet
- Depression and CopingDocument18 pagesDepression and CopingAlcesua EalmyelaNo ratings yet
- Tle Lead PoisoningDocument2 pagesTle Lead PoisoningXhaNo ratings yet
- HEALTH 9 QUARTER2 MODULE3 WeeK5-6Document9 pagesHEALTH 9 QUARTER2 MODULE3 WeeK5-6Heidee Basas100% (3)
- University of Northern PhilippinesDocument4 pagesUniversity of Northern PhilippinesCatherine PradoNo ratings yet
- English Final ProjectDocument16 pagesEnglish Final ProjectAry SanucasNo ratings yet
- Yoga 4 Immune SystemDocument33 pagesYoga 4 Immune Systemsukunath100% (1)
- Psy 325 LecturesDocument14 pagesPsy 325 LecturesErika BalaniNo ratings yet
- Virus, Viroids and PrionsDocument29 pagesVirus, Viroids and PrionscatherinejoaquinNo ratings yet
- HEALTH 4TH Q NCD - For Blended LearnersDocument35 pagesHEALTH 4TH Q NCD - For Blended LearnersAlmighty OperyNo ratings yet
- Health Problems Most Common in School Aged ChildrenDocument15 pagesHealth Problems Most Common in School Aged ChildrenAsterlyn ConiendoNo ratings yet
- GR - 9 - Revision Notes - Why We Do Fall IllDocument9 pagesGR - 9 - Revision Notes - Why We Do Fall IllAditi KumariNo ratings yet
- Examples of DrugsDocument29 pagesExamples of DrugsEdwins MaranduNo ratings yet
- Symptoms: What Are The Complications of Insomnia?Document4 pagesSymptoms: What Are The Complications of Insomnia?Mohamad nazrinNo ratings yet
- F&E ExamDocument3 pagesF&E ExamDino PringNo ratings yet
- (Burnett James C.) Tumours of The Breast and TheirDocument78 pages(Burnett James C.) Tumours of The Breast and TheirRajendraNo ratings yet
- Benefit Packages (Private)Document103 pagesBenefit Packages (Private)You Are Not Wasting TIME HereNo ratings yet
- ALU 101 Sample QuestionsDocument4 pagesALU 101 Sample Questionsartlover30No ratings yet
- Case 013: Fever in A Cirrhotic PatientDocument5 pagesCase 013: Fever in A Cirrhotic PatientFitri 1997No ratings yet
- Chaves 2020Document10 pagesChaves 2020Matheus CastroNo ratings yet
- 08-Hand-Arm VibrationDocument35 pages08-Hand-Arm Vibrationjimmy tiarlinaNo ratings yet
- Read Online Textbook Second A Gay Hockey Romance La Storm Book 2 RJ Scott Ebook All Chapter PDFDocument22 pagesRead Online Textbook Second A Gay Hockey Romance La Storm Book 2 RJ Scott Ebook All Chapter PDFrodney.ellison150100% (3)
- MILLETSDocument11 pagesMILLETSVeer VijayNo ratings yet
- ACOG Combined List of TitlesDocument13 pagesACOG Combined List of TitlesLaura RojasNo ratings yet
- Reflection AssignmentDocument5 pagesReflection Assignmentapi-659065431No ratings yet
- Transmission Sars Cov-2Document7 pagesTransmission Sars Cov-2Ikmah FauzanNo ratings yet
- Endomaterial Cancer-1Document28 pagesEndomaterial Cancer-1A.H.ANo ratings yet
- Fat-And Water-Soluble VitaminsDocument9 pagesFat-And Water-Soluble VitaminsJessa Mae OhaoNo ratings yet
- Water and ElectrolytesDocument39 pagesWater and ElectrolytesevbptrprnrmNo ratings yet
- Communicable Diseases HandoutDocument7 pagesCommunicable Diseases Handoutariane100% (1)
- Cefuroxime Drug StudyDocument1 pageCefuroxime Drug StudyACOB, Jamil C.No ratings yet
- Lippincotts Antiarrhythmics 5Document1 pageLippincotts Antiarrhythmics 5Wijdan HatemNo ratings yet
- Week 14 - Leukocyte Abnormalities and Non-Malignant Leukocyte DisordersDocument83 pagesWeek 14 - Leukocyte Abnormalities and Non-Malignant Leukocyte DisordersSheine EspinoNo ratings yet
- Nursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationDocument2 pagesNursing Responsibilities Adverse Effect Indication / Contraindication Mechanism of Action Drug Name IndicationOmar IzzoNo ratings yet
- Basic Encoding ActivityDocument3 pagesBasic Encoding ActivityJHOMER CABANTOGNo ratings yet
- Polycythemia: (Primary & Secondary)Document16 pagesPolycythemia: (Primary & Secondary)Vanessa Camille DomingoNo ratings yet
- PA1 HandoutDocument22 pagesPA1 HandoutIligan, JamaicahNo ratings yet
- 7.2 FTAT Coding Registers Case ScenariosDocument25 pages7.2 FTAT Coding Registers Case ScenariosGosa MohammedNo ratings yet
- 47-Article Text-305-1-10-20220731Document10 pages47-Article Text-305-1-10-20220731alyn30274No ratings yet
- ANT Handbook 2023Document84 pagesANT Handbook 2023latibaleni02No ratings yet
- Laporan Intensif 25 April 2021Document21 pagesLaporan Intensif 25 April 2021bosnia agusNo ratings yet
- Avian Influenza H5N1 VirusDocument27 pagesAvian Influenza H5N1 VirusHarsh Purwar100% (3)
- DGHS IPHS Sub-Dist Hosps 31 To 50Document113 pagesDGHS IPHS Sub-Dist Hosps 31 To 50shanmugapriyasankarNo ratings yet
- WEEK 2 Management of Patients With Chest and Lower Respiratory Tract DisordersDocument9 pagesWEEK 2 Management of Patients With Chest and Lower Respiratory Tract DisordersTin tinNo ratings yet