Professional Documents
Culture Documents
1242 4532 1 PB
1242 4532 1 PB
Uploaded by
Adrian Diaz LopezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1242 4532 1 PB
1242 4532 1 PB
Uploaded by
Adrian Diaz LopezCopyright:
Available Formats
International Surgery Journal
Velappan DP et al. Int Surg J. 2017 May;4(5):1773-1776
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: http://dx.doi.org/10.18203/2349-2902.isj20171638
Original Research Article
Clinical study and management of hollow viscus
perforation of abdomen
Dhanapal Pattanam Velappan1*, Selvam Kaveri2
1
Associate Professor, Department of General Surgery, Government Dharmapuri Medical College and Hospital,
Dharmapuri, Tamil Nadu, India
2
Department of Surgery, Government Dharmapuri Medical College and Hospital, Dharmapuri, Tamil Nadu, India
Received: 14 March 2017
Accepted: 04 April 2017
*Correspondence:
Dr. Dhanapal Pattanam Velappan,
E-mail: dhanapal65@gmail.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: Gastrointestinal perforation is a common abdominal emergency having a high morbidity and mortality.
Surgery plays an important role in the management of perforation. Gastrointestinal perforation is a common
abdominal emergency having a high morbidity and mortality.
Methods: 100 cases of hollow viscus perforation of the abdomen have been studied prospectively in detail during the
period from May 2010 to July 2012. Cases were selected randomly from admissions in Government
Mohankumaramangalam Medical College Hospital, Salem, Tamil Nadu, India. Clinical diagnosis of hollow viscus
perforation confirmed by investigations or by laparotomy performed.
Results: The results obtained in the present study were analysed: Among hollow viscus perforation duodenal ulcer
perforation was common (52 out of 100 cases). Next being appendicular perforation. Age group of 20-40 years were
affected mainly. Males are affected more than females. Signs and symptoms of acute abdomen like acute abdominal
pain vomiting fever may present tachycardia, hypotension, abdominal tenderness guarding\rigidity with obliteration
of liver dullness and absence of bowel sounds and absolute constipation were predominant signs.
Conclusions: GI hollow viscus perforations cause significant morbidity and sometimes mortality. Hollow viscus
perforation is the common cause of acute abdomen needing immediate effective surgical attention. A proper early
diagnosis and adequate treatment can prevent complications. Surgical approach depends on the site, size, age of
perforation and number of perforations.
Keywords: Abdominal emergency, Morbidity, Mortality
INTRODUCTION intestine represents a major surgical challenge to the
clinician.3 Since it is a rapidly fatal condition death being
Gastrointestinal perforation is a common abdominal caused by sepsis from peritoneal contamination with
emergency having a high morbidity and mortality.1 various pathogens both aerobic and anaerobic. Main aims
Missed diagnosis and late intervention are frequent of treatment are to control sepsis, to minimise
causes of increased morbidity and mortality especially in contamination and treat the underlying cause.4 Surgery
patients who survive the initial phase of insult.2 Diagnosis plays an important role in the management of perforation.
and treatment of gastrointestinal perforation remains a The structure of the hollow viscera is more fragile than
formidable problem in our country. A great majority of parenchymatous organ and even minor degrees of trauma
perforation of stomach and duodenum are due to can cause serious injury.5 This clinical study was
complications of peptic ulceration. Perforation of large undertaken to find the age and sex incidence and
International Surgery Journal | May 2017 | Vol 4 | Issue 5 Page 1773
Velappan DP et al. Int Surg J. 2017 May;4(5):1773-1776
etiological factors and clinical features of different types RESULTS
of perforations. It also assesses the common type of
perforations and its presentations, complications arising The results obtained in the present study were analyzed
post operatively and finally to analyse the prognosis in as follows.
our setup from the basis of present study.
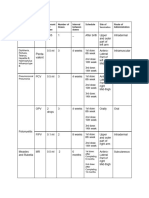
Table 1: Age distribution.
Aim of the study
Age No. of patients Percentages
• To present the problem of hollow viscus perforation <20 14 14%
due to various causes. 21-40 45 45%
• To study the age, sex incidence and clinical features 41-60 31 31%
of hollow viscous perforations. >60 10 10%
• To find the commonest type of perforation in our Total 100 100%
study.
• To review the postoperative complications. Maximum number of patients (45) were in the age group
• To assess the prognosis of each type of hollow of 20 to 40 years.
viscous perforations.
Table 2: Sex distribution.
METHODS
Sex No. of patients Percentage
100 cases of hollow viscus perforation of the abdomen Male 77 77%
have been studied prospectively in detail during the Female 13 13%
period from May 2010 to July 2012. Cases were selected Total 100 100%
randomly from admissions in Government
Mohankumarmangalam Medical College Hospital,
In present study there were 77 male patients (73%) and
Salem, Tamil Nadu, India. Clinical diagnosis of hollow
13 female patients (13%).
viscus perforation confirmed by investigations or by
laparotomy performed.
Table 3: Site of perforation.
Investigations done were:
Site No. of cases Percentage
Duodenal ulcer 52 52%
• Urine routine examinations including albumin, sugar
Gastric ulcer 10 10%
deposits.
Appendicular perforation 16 16%
• Blood routine examinations including Hb%, total
count and differential count. Meckel’s diverticulum 4 4%
• X ray abdomen erect view to detect free gas under Typhoid perforation 14 14%
diaphragm. Traumatic
• Widal test was done in suspected enteric perforation. Jejunum 1 1%
Ileum 3 3%
In all cases close monitoring of vital signs and Total 100 100%
preoperative correction of fluid and electrolyte imbalance
was done. Ciprofloxacin and metronidazole were used in Most common site of perforation was duodenal ulcer
all cases. Antibiotics were changed according to culture perforation (52%) next was appendicular perforation
and sensitivity report. Explorative laparotomy was done (16%) with gangrene of ileum (14%). No of patients who
under general anaesthesia in all cases. Right paramedian had traumatic injury of abdomen was 4% -among which
incision, upper midline or lower midline incision was 3 ileal perforation and 1 jejunal perforation. Meckels
made depending on the suspected site of perforation. diverticulum was found in 4 patients. Duodenal ulcer
perforation was in the first part of duodenum and was
Viscera were inspected carefully, the site of perforation common in males. Among the male patients 49 had
located and appropriate surgical procedure was duodenal ulcer perforation, 9 had gastric perforation, 13
performed. Peritoneal toilet with normal saline was done had appendicular perforation and 4 had Meckel’s
and peritoneal cavity was drained. Postoperatively diverticulum perforation (Table 4).
patients were put on continuous naso gastric aspiration
intravenous fluids and antibiotics. Vital signs were Table 4: Relation between sex and site of perforation.
monitored.
Sex Du. Gastric App. Meck Jej. Ileum
Assessment of intake and output was done. Recovery was Male 49 9 13 4 1 10
observed in the patients and any complications which Female 3 1 3 - - 7
occurred during the course were noted. Total 52 10 16 4 1 17
International Surgery Journal | May 2017 | Vol 4 | Issue 5 Page 1774
Velappan DP et al. Int Surg J. 2017 May;4(5):1773-1776
Table 5: Duration. About 90% patients presented within 24 hours and 60 out
of 90 patients presented within 13 to 24 hours of the
Duration No. of patients Percentage onset of symptoms in this study.
0-12 hours 30 30%
13-24 hours 60 60% In duodenal ulcer perforation history of drug intake was
25-48 hours 6 6% the common etiology. Gastric ulcer perforation common
49-72 hours 4 4% etiology was alcohol intake/smoking. Typhoid fever was
Total 100 100% the common etiology in ileal perforation (Table 6).
Table 6: Etiology and site of perforation.
Etiology Duodenal Gastric Ileal Jejunum App.
Nontraumatic
Drug intake 28
Alcohol intake/smoking 20 8
Typhoid 9
TB 5
Meckel’s 4
Idiopathic 4 2 16
Ascaris lumbricoides 1
Traumatic 2 1
Table 7: Sign and symptoms. Hypotension is the main sign. All cases were positive for
gas under the diaphragm and Widal test.
Symptoms and signs No. of patients
Fever 95 Table 8: Diagnosis and surgical procedure.
Pain abdomen 98
Vomiting 86 Surgical procedure No. of
Diagnosis
Distension 95 adopted patients
Constipation 7 Closure of perforation
Diarrhoea 7 Duodenal ulcer with omentum and 52
peritoneal lavage
Tenderness
Closure of perforation
Right iliac fossa 20
Gastric with omentum and 10
All quadrants 80
peritoneal lavage
Guarding 100
Excision of 1.5 feet of
Liver 20 Ileal perforation
terminal ileum with ilio
Spleen 3 with gangrene
transverse end to side 2
Obliterated liver dullness 68 of the terminal
anastamosis with
Free fluid 68 ileum
peritoneal lavage
Bowel sound absent 70 Jejunal and ileal Ilio ileal end to end
Air under diaphragm 75 perforation due anastamosis, jejunal
3
Fluid levels 25 to penetrating / proximal end to end
Diagnostic paracentesis +ve 40 blunt injury anastamosis
Blood Widal 9 Meckel’s Diverticulectomy with end
4
diverticulum to end ileal anastamosis
In the present study all the patients with duodenal ulcer App. Appendicectomy with
16
perforation presented with all signs mentioned above. Perforation peritoneal lavage
Gas under the diaphragm were present in 100% and 4
quadrant aspiration were positive in all cases (Table 7). Patients included in this study were managed according
All cases of appendicular perforation presented with to the standard measures. Preoperative resuscitation in
symptoms of abdominal pain, vomiting and fever but cases of shock and correction of electrolyte abnormality
there was no gas under the diaphragm. In ileal perforation were carried out in all patients. After preoperative
due to typhoid, fever was the main symptom. treatment all cases were subjected to laparotomy and the
primary cause was identified and treated accordingly.
International Surgery Journal | May 2017 | Vol 4 | Issue 5 Page 1775
Velappan DP et al. Int Surg J. 2017 May;4(5):1773-1776
Complications • Age group of 20-40 years were affected mainly
• Males are affected more than females
8 cases had wound dehiscence which healed with • Signs and symptoms of acute abdomen like acute
secondary sutures, no major morbidity was noted. abdominal pain vomiting fever may present
tachycardia, hypotension, abdominal tenderness
Mortality guarding\rigidity with obliteration of liver dullness
and absence of bowel sounds and absolute
No mortality noted in present study. constipation were predominant signs
• Hollow viscus perforation is the common cause of
DISCUSSION acute abdomen needing immediate effective surgical
attention.
GI hollow viscus perforation constitute one of the • In this study except for wound dehiscence in 8 cases
important cause of abdominal pain in adults. Duodenal which needed secondary suturing no major morbidity
ulcer perforation was the most common cause.6 Duodenal noted.
ulcer perforation is common in the first part of duodenum • No mortality noted in the present study.
and most common in males. The other causes of GI
hollow viscus perforations were acid peptic disease, Funding: No funding sources
enteric fever, amoebic colitis, appendicular perforation, Conflict of interest: None declared
trauma, malignancy, tuberculosis, iatrogenic injuries Ethical approval: The study was approved by the
which constitute major portion of emergency surgical institutional ethics committee
admissions. Majority of traumatic perforations are caused
by road traffic accidents.7 Early diagnosis and emergency REFERENCES
explorative laparotomy improves outcome. The high
incidence of duodenal ulcer perforation is due to 1. Langell JT, Mulvihill SJ. Gastrointestinal perforation
alcoholism, smoking and incomplete treatment of H. and the acute abdomen. Med Clin N Am. 2008;92:599-
pylori.8 NSAID abuse also plays a major role in duodenal 625.
ulcer perforation. Irrespective of the pathology of 2. Dhikav V, Singh S, Pande S, Chawla A, Anand KS.
perforation the maximum incidence were in males aged Non steroidal drug induced gastrointestinal
between 20-40 years. Enteric fever perforations are toxicity:mechanisms and management. JIACM
common in second week of the disease and are treated by 2003;4:315-22.
simple closure of the defect if the defect is small. 3. Kellog LC. A treatise on peptic perforations. Surgery.
Tubercular perforations involving the ileocaecal junction 1939;6:524-30.
4. Donovan AJ, Berne TV, Donovan JA. Perforated
are treated by right hemicolectomy. For appendicular
duodenal ulcer: An alternative therapeutic plan. Arch
perforation emergency appendicectomy with peritoneal
Surg. 1998;133:1166-71.
lavage is sufficient.9 Nowadays iatrogenic perforations 5. Fontana D, Webster GD, Wier J. Approach to
are common due to minimally invasive or endoscopic management of lesser curvature gastric perforations.
procedures. The incidence of perforation due to upper GI Scott Med J. 1958;3:238-49.
scopy was 1.2%.10 Perforations of the proximal region is 6. Rao DCM, Mathur JC, Ramu D, Anand M.
most common in india and that of distal perforation is Gastrointestinal perforations- a study of 46 cases. Ind J
common in the western countries.11 Surg. 1984;94-6.
7. Espinoza R, Rodríguez A. Traumatic and nontraumatic
CONCLUSION perforation of hollow viscera. Surg Clin North Am.
1997;77(6):1291-304.
This is a prospective randomized study consisting of 100 8. Torpy JM, Lynm C, Golub RM. Peptic ulcer disease.
cases of hollow viscus perforation of abdomen selected JAMA. 2012;307(12):1329-.
from surgical units of Government 9. Drake FT, Mottey NE, Farrokhi ET, Florence MG,
Mohankumarmangalam Medical College Hospital, Johnson MG, Mock C, et al. Time to appendectomy
Salem, Tamil Nadu, India from May 2010 to July 2012. and risk of perforation in acute appendicitis. JAMA
All case of this study group were subjected to pre Surg. 2014;149(8):837-44.
10. Chung IK, Lee JH, Lee SH, Kim SJ, Cho JY, Cho WY,
operative standard investigations and after pre operative
et al. Therapeutic outcome in 1000 cases of endoscopic
resuscitative measures exploratory laparotomy were
submucosal dissection for early gastric neoplasms:
performed and after identifying site of perforation Korean ESD Study Group multicenter study.
suitable standard surgical procedures adopted. The results Gastrointest Endosc. 2009;69:1228-35.
obtained in the present study were analyzed: 11. Nitecki W. Colonoscopic injuries. Asian J Surg.
1997;20:283-6.
• Among hollow viscus perforation duodenal ulcer
perforation was common (52 out of 100 cases). Next Cite this article as: Velappan DP, Kaveri S. Clinical
being appendicular perforation study and management of hollow viscus perforation
of abdomen. Int Surg J 2017;4:1773-6.
International Surgery Journal | May 2017 | Vol 4 | Issue 5 Page 1776
You might also like
- Kuchera - Osteopathic Considerations in Somatic DysfunctionDocument296 pagesKuchera - Osteopathic Considerations in Somatic DysfunctionWhiteLightning11100% (9)
- Periodontology III MCQ For The FinalDocument55 pagesPeriodontology III MCQ For The FinalLolita A. Hicks67% (3)
- Bio AssDocument10 pagesBio AsseliasNo ratings yet
- Absence Liver DullnessDocument8 pagesAbsence Liver DullnessqweqweqwNo ratings yet
- Clinical Study and Management of Gastric Perforation: Original ResearchDocument4 pagesClinical Study and Management of Gastric Perforation: Original ResearchEvi NainggolanNo ratings yet
- Clinical Study and Management of Gastric Perforation: Original ResearchDocument4 pagesClinical Study and Management of Gastric Perforation: Original Researchpeekaboo oooNo ratings yet
- Medip, ISJ-2223 ODocument5 pagesMedip, ISJ-2223 Odasarirevanth2002No ratings yet
- Original Article: Clinical Study of Perforations of Small BowelDocument7 pagesOriginal Article: Clinical Study of Perforations of Small BowelGarry WidjajaNo ratings yet
- Typhoid Perforation NepalDocument3 pagesTyphoid Perforation NepalMagdalena PranataNo ratings yet
- A Prospective Study of Predictors For Post Laparotomy Abdominal Wound DehiscenceDocument4 pagesA Prospective Study of Predictors For Post Laparotomy Abdominal Wound DehiscencemelisaberlianNo ratings yet
- 6665 PDFDocument4 pages6665 PDFerindah puspowatiNo ratings yet
- Clinical Study: Adhesive Intestinal Obstruction in Infants and Children: The Place of Conservative TreatmentDocument5 pagesClinical Study: Adhesive Intestinal Obstruction in Infants and Children: The Place of Conservative TreatmentOdiet RevenderNo ratings yet
- 20waqar PDFDocument4 pages20waqar PDFMelisa ClaireNo ratings yet
- Israr - Frequency of Abdominal Dehisence in Patient LaparotomyDocument3 pagesIsrar - Frequency of Abdominal Dehisence in Patient Laparotomyrhyzik reeNo ratings yet
- Perianal AbsesDocument4 pagesPerianal AbsesRizki SatriaNo ratings yet
- JCDR 8 80aDocument4 pagesJCDR 8 80adr.deyshieNo ratings yet
- Management of Perforated Appendicitis in Children: A Decade of Aggressive TreatmentDocument5 pagesManagement of Perforated Appendicitis in Children: A Decade of Aggressive Treatmentapi-308365861No ratings yet
- A Retrospective Clinical Study of Perforation Peritonitis in Rural Area in Andhra Pradesh November 2022 9921131660 120 PDFDocument9 pagesA Retrospective Clinical Study of Perforation Peritonitis in Rural Area in Andhra Pradesh November 2022 9921131660 120 PDFVijay KumarNo ratings yet
- Jurnal Bedah BaruuuuDocument17 pagesJurnal Bedah BaruuuuLalu Rizki Andri SaputraNo ratings yet
- 20 WaqarDocument4 pages20 WaqarmelisaberlianNo ratings yet
- Surgical Interventions in Abdominal Tuberculosis: A Clinico-Pathological StudyDocument5 pagesSurgical Interventions in Abdominal Tuberculosis: A Clinico-Pathological StudySatwinder KaurNo ratings yet
- Clinical Study and Management of Pseudocyst of Pancreas: Original Research ArticleDocument5 pagesClinical Study and Management of Pseudocyst of Pancreas: Original Research Articleneel patelNo ratings yet
- Exploratory Laparotomy For Acute Intestinal Conditions in Children: A Review of 10 Years of Experience With 334 CasesDocument9 pagesExploratory Laparotomy For Acute Intestinal Conditions in Children: A Review of 10 Years of Experience With 334 CasesuqbaNo ratings yet
- Spectrum of Perforation Peritonitis in Delhi: 77 Cases ExperienceDocument5 pagesSpectrum of Perforation Peritonitis in Delhi: 77 Cases ExperienceAhmad Rahmat Ramadhan TantuNo ratings yet
- VVF RepairDocument4 pagesVVF RepairAdil KhurshidNo ratings yet
- Removal of Foreign Body (Denture) in Esophagus With Rigid EsophagoscopeDocument6 pagesRemoval of Foreign Body (Denture) in Esophagus With Rigid EsophagoscopetaagrettaaNo ratings yet
- 30 Retained Surgical SpongesDocument8 pages30 Retained Surgical SpongesErickNo ratings yet
- PerforasiDocument3 pagesPerforasiEinz Nur Amalyah IdrusNo ratings yet
- A Clinical Study of Abdominal Wound DehiscenceDocument25 pagesA Clinical Study of Abdominal Wound DehiscenceKarthikeyan RNo ratings yet
- The Outcome of Surgery For Perforated Peptic Ulcer in Modern TimesDocument6 pagesThe Outcome of Surgery For Perforated Peptic Ulcer in Modern TimesFarizka Dwinda HNo ratings yet
- Journal of Pediatric SurgeryDocument6 pagesJournal of Pediatric SurgeryEkaNo ratings yet
- Moberg 2007Document5 pagesMoberg 2007Julio Adan Campos BadilloNo ratings yet
- Fistula in AnoDocument5 pagesFistula in AnoIoannis ValioulisNo ratings yet
- Peritonitis Following Prepyloric Ulcer Perforation A Case ReportDocument2 pagesPeritonitis Following Prepyloric Ulcer Perforation A Case ReportraysellaNo ratings yet
- 984 Pediatric Hernias and Hydrocele Pediatric SurgeryDocument27 pages984 Pediatric Hernias and Hydrocele Pediatric SurgeryVijay KumarNo ratings yet
- Complicated AppendicitisDocument4 pagesComplicated AppendicitisMedardo ApoloNo ratings yet
- Ca SekumDocument7 pagesCa SekumNely M. RosyidiNo ratings yet
- A Study On Groin Hernias Presenting As Acute Surgical Emergencies in AdultsDocument7 pagesA Study On Groin Hernias Presenting As Acute Surgical Emergencies in AdultsNi Nyoman SidiasihNo ratings yet
- Perforated Gastric and Duodenal Ulcers: Treatment Options: International Physical Medicine & Rehabilitation JournalDocument4 pagesPerforated Gastric and Duodenal Ulcers: Treatment Options: International Physical Medicine & Rehabilitation JournalNazila HanaNo ratings yet
- Exploratorylaparotomyinthe EmergencyroomDocument5 pagesExploratorylaparotomyinthe EmergencyroomBalaji MallaNo ratings yet
- A Study of Inguinal Hernia in ChildrenDocument5 pagesA Study of Inguinal Hernia in ChildrenrhmathidayatNo ratings yet
- 1 Salim TahirhvDocument4 pages1 Salim TahirhvTajudin SuryaNo ratings yet
- Surgical Outcome of Genito Urinary Fistula - RayazDocument3 pagesSurgical Outcome of Genito Urinary Fistula - RayazRiaz Ahmed ChaudhryNo ratings yet
- A Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesDocument4 pagesA Non-Operative Treatment of Perforated Peptic Ulcer: A Prospective Study With 50 CasesSake Cinema21No ratings yet
- EsofagusDocument7 pagesEsofagusWillie VanegasNo ratings yet
- Gallbladder Perforation: Experience of 35 Cases at A Tertiary Care HospitalDocument6 pagesGallbladder Perforation: Experience of 35 Cases at A Tertiary Care HospitalIJAR JOURNALNo ratings yet
- Perforacion ColonosDocument5 pagesPerforacion ColonosKeyla barriosNo ratings yet
- Laproscopic Vagotony PaperDocument4 pagesLaproscopic Vagotony Paperpeter_mrNo ratings yet
- Large Bowel Perforation: Morbidity and Mortality: K. Bielecki P. Kami M. KlukowskiDocument6 pagesLarge Bowel Perforation: Morbidity and Mortality: K. Bielecki P. Kami M. KlukowskiDiana AdămescuNo ratings yet
- Wound DehiscenceDocument3 pagesWound DehiscencesmileyginaaNo ratings yet
- Typhoid PerforationDocument3 pagesTyphoid PerforationSaryia JavedNo ratings yet
- Prevalence and Risk Factors of Inguinal Hernia Study in A Semi-Urban Area in Rayalaseema, Andhra PradeshDocument4 pagesPrevalence and Risk Factors of Inguinal Hernia Study in A Semi-Urban Area in Rayalaseema, Andhra Pradeshsamsara vrindaNo ratings yet
- GJMS Vol-7-1 PDFDocument4 pagesGJMS Vol-7-1 PDFgraceflowerNo ratings yet
- Ileal Peritonites Epidemiological, Clinical and Therapeutic Aspects in The Vision Surgery Department of The Donka National HopitalDocument4 pagesIleal Peritonites Epidemiological, Clinical and Therapeutic Aspects in The Vision Surgery Department of The Donka National HopitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 404 398 1 SMDocument4 pages404 398 1 SMfak youNo ratings yet
- (Final Edit) Ventral Onlay Buccal Graft For Urethrorectal FistulaDocument13 pages(Final Edit) Ventral Onlay Buccal Graft For Urethrorectal FistulaNadia Rezky ElizaNo ratings yet
- Prevalence and Risk Factors of Hemorrhoids: A Study in A Semi-Urban CentreDocument4 pagesPrevalence and Risk Factors of Hemorrhoids: A Study in A Semi-Urban CentreNaily Nuzulur RohmahNo ratings yet
- Peritonsillar Abscess: Pattern and Treatment Intervention in A Tertiary Health Institution in Sokoto MetropolisDocument4 pagesPeritonsillar Abscess: Pattern and Treatment Intervention in A Tertiary Health Institution in Sokoto Metropolismuhammad hasan fuadyNo ratings yet
- Ann Punjab Med Coll 2009 3 1 27 31Document5 pagesAnn Punjab Med Coll 2009 3 1 27 31eka henny suryaniNo ratings yet
- Etiological Pattern and Outcome of Non-Variceal Upper G.I. BleedingDocument5 pagesEtiological Pattern and Outcome of Non-Variceal Upper G.I. BleedingJawad ZafarNo ratings yet
- 433-Article Text-896-1-10-20170620Document7 pages433-Article Text-896-1-10-20170620Tri AdityaNo ratings yet
- Applied Peritoneal Dialysis: Improving Patient OutcomesFrom EverandApplied Peritoneal Dialysis: Improving Patient OutcomesAnjay RastogiNo ratings yet
- Mastery of IBD SurgeryFrom EverandMastery of IBD SurgeryNeil HymanNo ratings yet
- Case Scenario - Nursing Care Plan (DR - Magsingal)Document1 pageCase Scenario - Nursing Care Plan (DR - Magsingal)Cristyl Shine BariaoNo ratings yet
- Incident Reporting SystemDocument5 pagesIncident Reporting SystemAhmed IbrahimNo ratings yet
- PNLE II For Community Health Nursing and Care of The Mother and ChildDocument14 pagesPNLE II For Community Health Nursing and Care of The Mother and Childkrystelle jade labineNo ratings yet
- Consent LcarnitineDocument2 pagesConsent LcarnitineZen AlkaffNo ratings yet
- EPI Schedule-1Document2 pagesEPI Schedule-1sabbir.boss7333No ratings yet
- Surgery Case Report - AppendicitisDocument18 pagesSurgery Case Report - Appendicitissuperpickle87No ratings yet
- ELECTRIC PULP TESTING - OldDocument7 pagesELECTRIC PULP TESTING - OldShubham EdlaNo ratings yet
- SUMAN Guideline 2020 Web VersionDocument84 pagesSUMAN Guideline 2020 Web VersionJasoners22333No ratings yet
- EpidemiologyDocument10 pagesEpidemiologyMUTHUKUMARANNo ratings yet
- Unit-I. Epidemiology IntroductionDocument60 pagesUnit-I. Epidemiology IntroductionAny OneNo ratings yet
- 1gastrointestinal System Disorders NCLEX Practice QuizDocument8 pages1gastrointestinal System Disorders NCLEX Practice QuizmyNo ratings yet
- Aspirin in Episodic Tension-Type Headache: Placebo-Controlled Dose-Ranging Comparison With ParacetamolDocument9 pagesAspirin in Episodic Tension-Type Headache: Placebo-Controlled Dose-Ranging Comparison With ParacetamolErwin Aritama IsmailNo ratings yet
- Form-2 (Enlistment of Importer)Document2 pagesForm-2 (Enlistment of Importer)Farhan aliNo ratings yet
- HLTH 5465 3.0, Winter 2014: We Will Begin OurDocument12 pagesHLTH 5465 3.0, Winter 2014: We Will Begin Ourመሰረት ሀብቴNo ratings yet
- Efficacy of Terlipressin in Upper Gi Bleeding Due To Liver CirrhosisDocument3 pagesEfficacy of Terlipressin in Upper Gi Bleeding Due To Liver CirrhosisM AbhiNo ratings yet
- Module In: Business Ethics and Social Responsibility LAS 6-7Document2 pagesModule In: Business Ethics and Social Responsibility LAS 6-7Shaina AgravanteNo ratings yet
- Medical Secrets 6Th Edition Mary P Harward Download PDF ChapterDocument38 pagesMedical Secrets 6Th Edition Mary P Harward Download PDF Chaptervicki.krause300100% (20)
- Ears DisordersDocument112 pagesEars DisordersRenie Serrano100% (1)
- Thyroidinum CasesDocument2 pagesThyroidinum CasesAgaNo ratings yet
- Neoadjuvant Treatment Strategies For HER2 Positive Breast Cancer: Cost Effectiveness and Quality of Life OutcomesDocument9 pagesNeoadjuvant Treatment Strategies For HER2 Positive Breast Cancer: Cost Effectiveness and Quality of Life Outcomesfaris nagibNo ratings yet
- Medicine, Coptic.: Chronological Table of Ostraca and Papyri Dealing With MedicineDocument7 pagesMedicine, Coptic.: Chronological Table of Ostraca and Papyri Dealing With MedicinePaula VeigaNo ratings yet
- ETT SUCTION DEWASA ACI14 - Suction - 2-2 PDFDocument46 pagesETT SUCTION DEWASA ACI14 - Suction - 2-2 PDFAde Rahmah YuliaNo ratings yet
- Oxford Malaria VaccineDocument2 pagesOxford Malaria Vaccinegiorgi popiashviliNo ratings yet
- Global Stem Cell Therapy Market IHealthcareAnalyst, IncDocument2 pagesGlobal Stem Cell Therapy Market IHealthcareAnalyst, InciHealthcareAnalyst, Inc.No ratings yet
- Say Cheese With These Top 10 Dentists in Los Angeles, California!.20121204.043541Document2 pagesSay Cheese With These Top 10 Dentists in Los Angeles, California!.20121204.043541anon_734894635No ratings yet
- CHN FinaleDocument163 pagesCHN FinaleJessa Kris RialubinNo ratings yet
- TATHLGP21248V022021Document16 pagesTATHLGP21248V022021vsharma0091No ratings yet