Professional Documents
Culture Documents
JCM 02589-20
JCM 02589-20
Uploaded by
NorellaCopyright:
Available Formats
You might also like
- Tracheostomy Care Checklist 1Document2 pagesTracheostomy Care Checklist 1Nicholas Tagle100% (2)
- WHO Skin NTDs Working GroupsDocument5 pagesWHO Skin NTDs Working GroupsAkinlolu AdediranNo ratings yet
- PIIS1198743X20306972Document4 pagesPIIS1198743X20306972KARLA PATRICIA DIAZ LOPEZNo ratings yet
- Jurnal 20Document5 pagesJurnal 20Ahmad Fari Arief LopaNo ratings yet
- JurnalDocument6 pagesJurnalDaffa AthaNo ratings yet
- 1 s2.0 S1386653220302420 MainDocument4 pages1 s2.0 S1386653220302420 MainZahira SafouanNo ratings yet
- Multiplex Detection and Dynamics of IgG Antibodies To SARS-CoV2 and The Highly Pathogenic Human Coronaviruses SARS-CoV and MERS-CoVDocument7 pagesMultiplex Detection and Dynamics of IgG Antibodies To SARS-CoV2 and The Highly Pathogenic Human Coronaviruses SARS-CoV and MERS-CoVamyNo ratings yet
- International Journal of Infectious DiseasesDocument3 pagesInternational Journal of Infectious DiseasesDetti FahmiasyariNo ratings yet
- Mm695152a3 HDocument6 pagesMm695152a3 HKinja NinjaNo ratings yet
- Journal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFDocument33 pagesJournal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFDwi Ratna KarimNo ratings yet
- Id Now NP Rna VLDocument5 pagesId Now NP Rna VLluis achaNo ratings yet
- Usefulness of High-Resolution Computed Tomography in Early Diagnosis of Patients With Suspected COVID-19Document7 pagesUsefulness of High-Resolution Computed Tomography in Early Diagnosis of Patients With Suspected COVID-19Israel Parra-OrtegaNo ratings yet
- Diagnostic Performance of A Sars-Cov-2 Igg/Igm Lateral Flow Immunochromatography Assay in Symptomatic Patients Presenting To The Emergency DepartmentDocument3 pagesDiagnostic Performance of A Sars-Cov-2 Igg/Igm Lateral Flow Immunochromatography Assay in Symptomatic Patients Presenting To The Emergency DepartmentWilmer UcedaNo ratings yet
- Jurnal MPIDocument4 pagesJurnal MPIMarini TaslimaNo ratings yet
- Title: Improved Molecular Diagnosis of COVID-19 by The Novel, Highly Sensitive and SpecificDocument33 pagesTitle: Improved Molecular Diagnosis of COVID-19 by The Novel, Highly Sensitive and SpecificCristina GuţuNo ratings yet
- International Journal of Infectious Diseases: SciencedirectDocument7 pagesInternational Journal of Infectious Diseases: SciencedirectKinja NinjaNo ratings yet
- Pooling of Samples For Testing Sars Cov 2 in Asymptomatic PatientsDocument2 pagesPooling of Samples For Testing Sars Cov 2 in Asymptomatic Patientsm.ihsan anggiNo ratings yet
- Journal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFDocument33 pagesJournal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFdavid zhangNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesmikhaelyosiaNo ratings yet
- Artemisin PiperaquineDocument8 pagesArtemisin PiperaquineIrma Rahayu LatarissaNo ratings yet
- Comparación de Pruebas Rápidas de Antígenos para COVID-19Document9 pagesComparación de Pruebas Rápidas de Antígenos para COVID-19Cristal Jewels DiamondNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesArum Rahmawatie VirgieNo ratings yet
- Oral, Nasal and Saliva SensitivityDocument6 pagesOral, Nasal and Saliva SensitivitySnow wanNo ratings yet
- JCM 01438-20Document9 pagesJCM 01438-20043 Ni Putu Anna NatasyaNo ratings yet
- Assessment of Diagnostic and Prognostic Laboratory Biomarkers in Severe COVID-19Document22 pagesAssessment of Diagnostic and Prognostic Laboratory Biomarkers in Severe COVID-19Reda RamzyNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesmeNo ratings yet
- Different Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsDocument5 pagesDifferent Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsagboxNo ratings yet
- 1 s2.0 S0033350620301141 MainDocument3 pages1 s2.0 S0033350620301141 MainFedrik Monte Kristo LimbongNo ratings yet
- International Journal of Infectious Diseases: A A A A A B A B A B A C A BDocument4 pagesInternational Journal of Infectious Diseases: A A A A A B A B A B A C A BAhmad Afianto MuttolibNo ratings yet
- Dynamics and Correlation Among Viral Positivity, Seroconversion, and Disease Severity in COVID-19Document15 pagesDynamics and Correlation Among Viral Positivity, Seroconversion, and Disease Severity in COVID-19yanuarizkaNo ratings yet
- Diagnostic Accuracy of A Rapid Diagnostic Test For The Early Detection of COVID 19Document4 pagesDiagnostic Accuracy of A Rapid Diagnostic Test For The Early Detection of COVID 19Franklin SierraNo ratings yet
- 1 s2.0 S1807593222004495 MainDocument9 pages1 s2.0 S1807593222004495 MainandressanrliraNo ratings yet
- Correspondence: Pandemic Peak Sars-Cov-2 Infection and Seroconversion Rates in London Frontline Health-Care WorkersDocument2 pagesCorrespondence: Pandemic Peak Sars-Cov-2 Infection and Seroconversion Rates in London Frontline Health-Care WorkersJimmy A. Camones ObregonNo ratings yet
- ArchitechDocument5 pagesArchitechERIE YUWITA SARINo ratings yet
- Rapid AntibodiDocument5 pagesRapid AntibodiDzulRizkaNo ratings yet
- XmdffaDocument5 pagesXmdffaIndira LarasatiNo ratings yet
- Jurnal 1Document5 pagesJurnal 1Jojo McalisterNo ratings yet
- JMV 9999 NaDocument10 pagesJMV 9999 NaNurul AzizahNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument14 pagesJournal Pre-Proof: International Journal of Infectious DiseasesMohammed Shuaib AhmedNo ratings yet
- Highly Accurate and Sensitive Diagnostic Detection of Sars-Cov-2 by Digital PCRDocument23 pagesHighly Accurate and Sensitive Diagnostic Detection of Sars-Cov-2 by Digital PCRJosé ManriqueNo ratings yet
- Comparison of Rapid Antigen TestsDocument8 pagesComparison of Rapid Antigen TestsshofidhiaaaNo ratings yet
- Journal Pre-Proof: Journal of Clinical VirologyDocument14 pagesJournal Pre-Proof: Journal of Clinical VirologyMajlinda HalitiNo ratings yet
- Anosmia and Dysgeusia Associated With Sars-Cov-2 Infection: An Age-Matched Case Control StudyDocument6 pagesAnosmia and Dysgeusia Associated With Sars-Cov-2 Infection: An Age-Matched Case Control StudyCarolina ValenzuelaNo ratings yet
- Clinical Microbiology and Infection: D. Hornuss, B. Lange, N. SCHR Oter, S. Rieg, W.V. Kern, D. WagnerDocument2 pagesClinical Microbiology and Infection: D. Hornuss, B. Lange, N. SCHR Oter, S. Rieg, W.V. Kern, D. Wagnerayuines lassyaniNo ratings yet
- Recurrence of Positive Sars Cov 2 Rna in Covid 19 A Case Report Dabiao Chen Download 2024 Full ChapterDocument25 pagesRecurrence of Positive Sars Cov 2 Rna in Covid 19 A Case Report Dabiao Chen Download 2024 Full Chapterrichard.byrd946100% (11)
- Sensitive On-Site Detection of SARS-CoV-2 by ID NOW COVID-19Document12 pagesSensitive On-Site Detection of SARS-CoV-2 by ID NOW COVID-19luis.achaNo ratings yet
- Article Andre AdiantoDocument7 pagesArticle Andre AdiantoAndre AdiantoNo ratings yet
- Anti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsDocument6 pagesAnti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsdhairyasheelNo ratings yet
- Correspondence To: Professor Changxin Shen Department of Blood TransfusionDocument13 pagesCorrespondence To: Professor Changxin Shen Department of Blood TransfusionAlfa RidziNo ratings yet
- Journal of InfectionDocument4 pagesJournal of InfectionLorena Ek MaciasNo ratings yet
- Evaluation of A COVID 19 IgM and IgG Rapid Test An Efficient Tool For Assessment of Past Exposure To SARS CoV 2Document6 pagesEvaluation of A COVID 19 IgM and IgG Rapid Test An Efficient Tool For Assessment of Past Exposure To SARS CoV 2Alma MutiaraniNo ratings yet
- Clinical Applications of Detecting IgG, IgM or IgADocument9 pagesClinical Applications of Detecting IgG, IgM or IgAreginabrizolaraNo ratings yet
- Idcm 2021 0059Document8 pagesIdcm 2021 0059Elaine SantiagoNo ratings yet
- Diagnostic Aspect of COVIDDocument8 pagesDiagnostic Aspect of COVIDYanMardianNo ratings yet
- Réponse Immun Covid19Document8 pagesRéponse Immun Covid19Tidiane SibyNo ratings yet
- Chest CT CovidDocument6 pagesChest CT CovidShinta FrennandaNo ratings yet
- Genoamp® Real-Time PCR Tests For Detection of Covid-19: Mahtas Covid-19 Rapid Evidence UpdatesDocument5 pagesGenoamp® Real-Time PCR Tests For Detection of Covid-19: Mahtas Covid-19 Rapid Evidence UpdatesDesmond KhorNo ratings yet
- The Application of Sample Pooling For Mass Screening of Sars-Cov-2 in An Outbreak of Covid-19 in VietnamDocument4 pagesThe Application of Sample Pooling For Mass Screening of Sars-Cov-2 in An Outbreak of Covid-19 in VietnamMedtech ChuongNo ratings yet
- Main 1Document4 pagesMain 1Raya KurniawanNo ratings yet
- Donders Et Al. - 2021 - Sperm Quality and Absence of SARS-CoV-2 RNA in SemDocument9 pagesDonders Et Al. - 2021 - Sperm Quality and Absence of SARS-CoV-2 RNA in SemC. MohrNo ratings yet
- Journal Pre-Proof: Journal of Clinical VirologyDocument12 pagesJournal Pre-Proof: Journal of Clinical VirologymiNo ratings yet
- A 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerDocument9 pagesA 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerNur SanaaniNo ratings yet
- Mortons NeuromaDocument12 pagesMortons NeuromaJunben DelacruzNo ratings yet
- Genograms: Practical Tools PhysiciansDocument6 pagesGenograms: Practical Tools PhysiciansThariq Mubaraq DrcNo ratings yet
- Managing Medicine SelectionDocument25 pagesManaging Medicine SelectionShoaib BiradarNo ratings yet
- Breast, Imaging, Reporting and Data System (BI RADS) - StatPearls - NCBI Bookshelf PDFDocument3 pagesBreast, Imaging, Reporting and Data System (BI RADS) - StatPearls - NCBI Bookshelf PDFnn hijo de alguienNo ratings yet
- 7 PsccauticurrentDocument22 pages7 PsccauticurrentLuz Glenny CastroNo ratings yet
- Asthma Action Plan Budesonide FormoterolDocument2 pagesAsthma Action Plan Budesonide Formoterolabob619No ratings yet
- FmasDocument30 pagesFmashaneefmdfNo ratings yet
- Zen ShiatsuDocument90 pagesZen ShiatsuLuz Violeta Platino100% (1)
- Classification System For Complete EdentulismDocument33 pagesClassification System For Complete EdentulismSahana RangarajanNo ratings yet
- Aravind Eye Care PDFDocument10 pagesAravind Eye Care PDFJe RomeNo ratings yet
- Laboratory Trainer TheoryDocument478 pagesLaboratory Trainer Theoryمحمد الغامدي100% (1)
- AOP Form 3Document4 pagesAOP Form 3Ferzada SajiranNo ratings yet
- CPG Intrapartum and Immediate Postpartum Care PDFDocument52 pagesCPG Intrapartum and Immediate Postpartum Care PDFAngela SaldajenoNo ratings yet
- Anesthesia For Tracheal Surgery - Specific Procedures - UpToDateDocument29 pagesAnesthesia For Tracheal Surgery - Specific Procedures - UpToDateMaría Augusta Robayo UvilluzNo ratings yet
- Forensic Med. CertificateDocument9 pagesForensic Med. Certificatedeeksha100% (2)
- OxyContin (Oxycodone) MundipharmaDocument15 pagesOxyContin (Oxycodone) MundipharmaRayzal AdamNo ratings yet
- PC Metabolic AcidosisDocument4 pagesPC Metabolic AcidosisErine Emmanuelle Cawaling Hetrosa50% (2)
- Hyperprolactinemia: A Systematic Review of Diagnosis and ManagementDocument12 pagesHyperprolactinemia: A Systematic Review of Diagnosis and ManagementJaveria RphNo ratings yet
- Miocarditis Por Clozapina Ronaldson2017 Revisión SistematicaDocument19 pagesMiocarditis Por Clozapina Ronaldson2017 Revisión SistematicaAlejandro PiscitelliNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Sle PaperDocument73 pagesSle PaperRight VentricleNo ratings yet
- Reaction PaperDocument2 pagesReaction PaperLinzie CariquetanNo ratings yet
- Newborn CareDocument30 pagesNewborn CareAlexandria P. OrcajadaNo ratings yet
- May 2022 NP 5 CmuDocument7 pagesMay 2022 NP 5 Cmujptorresrn09No ratings yet
- Acupuncture - MeniereDocument4 pagesAcupuncture - MeniereTinnitus Man IndonesiaNo ratings yet
- 5440 15044 1 PBDocument10 pages5440 15044 1 PBDelfia Tanjung SariNo ratings yet
- Dr. Pharmacist: Mawahib Abdelfatah MohamedDocument1 pageDr. Pharmacist: Mawahib Abdelfatah Mohamedmtariq60No ratings yet
JCM 02589-20
JCM 02589-20
Uploaded by
NorellaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
JCM 02589-20
JCM 02589-20
Uploaded by
NorellaCopyright:
Available Formats
LETTER TO THE EDITOR
crossm
Evaluation of the Panbio COVID-19 Rapid Antigen Detection
Test Device for the Screening of Patients with COVID-19
Florence Fenollar,a,b Amar Bouam,a Mehdi Ballouche,a Léa Fuster,a,c Elsa Prudent,a Philippe Colson,a,b
Hervé Tissot-Dupont,a,b Matthieu Million,a,b Michel Drancourt,a,b Didier Raoult,a,b Pierre-Edouard Fourniera,c
a Institut Hospitalo-universitaire Méditerranée Infection, Marseille, France
b UMR MEPHI, Aix-Marseille Université, IRD, Assistance Publique-Hôpitaux de Marseille, Institut Hospitalo-Universitaire Méditerranée-Infection, Marseille, France
c
UMR VITROME, Aix-Marseille Université, IRD, Service de Santé des Armées, Assistance Publique-Hôpitaux de Marseille, Institut Hospitalo-Universitaire Méditerranée-
Infection, Marseille, France
KEYWORDS COVID-19, SARS-CoV-2, diagnosis, antigen assay, rapid diagnosis,
RT-PCR, rapid antigenic device, sensitivity
C oronavirus disease 2019 (COVID-19), declared a pandemic by the WHO on 11 March
2020 (1), requires an early diagnosis to optimize patient management and limit
further transmission. Currently, the gold standard and most commonly used diagnostic
method in clinical microbiology laboratories is real-time PCR (RT-PCR) detecting the
viral RNA in nasopharyngeal specimens (2). However, RT-PCR requires specialized
instruments and personnel. In contrast, rapid antigen (Ag) detection (RAD) tests,
which are widely used to diagnose viral diseases other than COVID-19, not only are
rapid (15 to 30 min) but are less laborious and require only a comparatively short
training period. However, to date, several commercialized RAD tests have been
evaluated and most have demonstrated a lack of sensitivity (see Table S1 in the
supplemental material).
In the present study, we evaluated the performance of the Panbio COVID-19 Ag
rapid test device assay (Abbott) in comparison to that of the VitaPCR severe acute
Downloaded from https://journals.asm.org/journal/jcm on 28 October 2022 by 61.6.230.46.
respiratory syndrome coronavirus 2 (SARS-CoV-2) assay (Credo Diagnostics, Singapore)
on nasopharyngeal specimens. Both systems provide results within 20 min. The former
is an immunochromatographic assay detecting the SARS-CoV-2 nucleocapsid protein
and requiring no specialized instruments. This device is distributed worldwide except
in the United States, where its equivalent, the BinaxNOW COVID-19 Ag card (Abbott),
is FDA approved. Using 10-fold dilutions of a quantified suspension of Vero E6 cell-
cultured SARS-CoV-2 (IHUMI3 strain), as previously described (3), from 780 ⫻ 106 cop-
ies/ml at a dilution of 10⫺1 to 1,484 copies/ml at a dilution of 10⫺6, we found that the
Citation Fenollar F, Bouam A, Ballouche M,
RT-PCR assay was positive for all tested virus dilutions, with cycle threshold (CT) values
Fuster L, Prudent E, Colson P, Tissot-Dupont H,
of 16 and 34 for the most concentrated (10⫺1) and most dilute (10⫺6) solutions, Million M, Drancourt M, Raoult D, Fournier P-E.
respectively. In contrast, the RAD test was positive for all dilutions except 10⫺5 and 2021. Evaluation of the Panbio COVID-19 rapid
antigen detection test device for the screening
10⫺6. Two further replicates of this evaluation confirmed these results for both assays.
of patients with COVID-19. J Clin Microbiol
Then, we tested prospectively, from 21 September to 2 October 2020, nasopharyngeal 59:e02589-20. https://doi.org/10.1128/JCM
samples from 341 patients and subjects who presented at our institute for COVID-19 .02589-20.
testing using the two methods. Of these, 182 were symptomatic patients and 159 were Editor Angela M. Caliendo, Rhode Island
Hospital
asymptomatic subjects who had had contact with patients. For each patient, two
Copyright © 2021 American Society for
nasopharyngeal samples were collected, from one nostril each, with a specific swab Microbiology. All Rights Reserved.
according to the assay used. All tests were performed within 1 h after specimen Address correspondence to Pierre-Edouard
collection. All of the 182 symptomatic patients but only 22 of the 159 asymptomatic Fournier, pierre-edouard.fournier@univ-amu.fr.
patients were PCR positive (median CT values, 25 and 30.5, respectively, P ⬍ 10⫺2, Table Accepted manuscript posted online 2
November 2020
1), for a total of 204 PCR positives (Table S2). The Panbio COVID-19 Ag rapid test Published 21 January 2021
detected 154 of the 204 PCR-positive samples (sensitivity, 75.5%; 95% confidence
February 2021 Volume 59 Issue 2 e02589-20 Journal of Clinical Microbiology jcm.asm.org 1
Letter to the Editor Journal of Clinical Microbiology
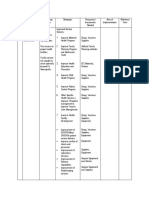
TABLE 1 Sensitivity of the Panbio COVID-19 Ag rapid test (Abbott) according to the CT
values
Sensitivity of the Panbio COVID-19 Ag rapid test in the present
study
CT range No. of positive patients % of positive patients
⬍10 1 100
10–15 19 95
16–20 38 100
21–25 49 94.2
26–30 39 73.6
31–34 8 20
interval [95% CI], 69.5 to 81.5), including 144/182 symptomatic patients (79.1%), but
only 10/22 asymptomatic patients (45.4%). However, the test result was positive in 7 of
the 137 PCR-negative samples, all of which had been collected from asymptomatic
patients (specificity, 94.9%; 95% CI, 91.2 to 98.6). Among the individuals diagnosed
(n ⫽ 204) or not diagnosed (n ⫽ 137) with COVID-19, positive and negative predictive
values were 95.6% (154/161) and 72.2% (130/180), respectively.
We acknowledge the fact that our study population may not be representative of
the general population of Marseille as symptomatic patients also came from other cities
from southern France and were thus overrepresented. However, our study showed that
the Panbio COVID-19 Ag rapid test had a good specificity for SARS-CoV-2 detection in
nasopharynx swab samples but a good sensitivity only for samples with CT values lower
than 25 (corresponding to viral loads higher than 106 copies/ml, which has been
proposed as threshold of transmissibility [4, 5]). In our study, all 10 asymptomatic
patients, as well as 57/144 symptomatic patients, exhibited CT values of ⱖ25 (Table S2).
In this population, the Panbio COVID-19 Ag rapid test may miss about 40% of diag-
noses. However, as the clinical performance of RAD tests largely depends on the setting
in which they are used, we believe that the Panbio COVID-19 Ag rapid test may be a
useful mass screening test when RT-PCR assays are not or are insufficiently available, in
particular, in symptomatic patients.
The patients gave informed consent for this study.
SUPPLEMENTAL MATERIAL
Downloaded from https://journals.asm.org/journal/jcm on 28 October 2022 by 61.6.230.46.
Supplemental material is available online only.
SUPPLEMENTAL FILE 1, PDF file, 0.1 MB.
ACKNOWLEDGMENTS
This study was supported by the Méditerranée-Infection Foundation and the French
Agence Nationale de la Recherche under reference Investissements d’Avenir Méditer-
ranée Infection 10-IAHU-03 and Région Provence-Alpes-Côte d’Azur and European
funding FEDER IHUBIOTK.
D.R. and M.D. are cofounders of the Pocrame startup, which develops diagnostic
devices for infectious diseases. We certify that we have no other conflict of interest to
declare in relation to this research.
Our contributions were as follows: conceptualization, D.R. and P.-E.F.; formal anal-
ysis, F.F., D.R., and P.-E.F.; investigation, A.B., M.B., L.F., E.P., H.T.-D., and M.M.; resources,
D.R. and P.-E.F.; data curation, P.C.; writing— original draft preparation, F.F. and P.-E.F.;
writing—review and editing, F.F., M.D., D.R., and P.-E.F. All of us have read and agreed
to the published version of the manuscript.
REFERENCES
1. WHO. 11 March 2020. Coronavirus disease (COVID-19) situation report – 51. T, Brunink S, Schneider J, Schmidt ML, Mulders DG, Haagmans BL, van der
https://www.who.int/docs/default-source/coronaviruse/situation-reports/ Veer B, van den Brink S, Wijsman L, Goderski G, Romette JL, Ellis J,
20200311-sitrep-51-covid-19.pdf?sfvrsn⫽1ba62e57810. Zambon M, Peiris M, Goossens H, Reusken C, Koopmans MP, Drosten C.
2. Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, Bleicker 2020. Detection of 2019 novel coronavirus (2019-nCoV) by real-time
February 2021 Volume 59 Issue 2 e02589-20 jcm.asm.org 2
Letter to the Editor Journal of Clinical Microbiology
RT-PCR. EuroSurveill 25(3): pii⫽2000045. https://www.eurosurveillance relative transmissibility of asymptomatic COVID-19 infections among
.org/content/10.2807/1560-7917.ES.2020.25.3.2000045. close contacts. Int J Infect Dis 94:145–147. https://doi.org/10.1016/j
3. La Scola B, Le Bideau M, Andreani J, Hoang VT, Grimaldier C, Colson P, .ijid.2020.04.034.
Gautret P, Raoult D. 2020. Viral DNA as determined by cell culture as a 5. Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA,
management tool for discharge of SARS-CoV-2 patients from infectious Niemeyer D, Jones TC, Vollmar P, Rothe C, Hoelscher M, Bleicker T, Brünink
disease wards. Eur J Clin Microbiol Infect Dis 39:1059 –1061. https://doi S, Schneider J, Ehmann R, Zwirglmaier K, Drosten C, Wendtner C. 2020.
.org/10.1007/s10096-020-03913-9. Virological assessment of hospitalized patients with COVID-2019. Nature
4. He D, Zhao S, Lin Q, Zhuang Z, Cao P, Wang MH, Yang L. 2020. The 581:465– 469. https://doi.org/10.1038/s41586-020-2196-x.
Downloaded from https://journals.asm.org/journal/jcm on 28 October 2022 by 61.6.230.46.
February 2021 Volume 59 Issue 2 e02589-20 jcm.asm.org 3
You might also like
- Tracheostomy Care Checklist 1Document2 pagesTracheostomy Care Checklist 1Nicholas Tagle100% (2)
- WHO Skin NTDs Working GroupsDocument5 pagesWHO Skin NTDs Working GroupsAkinlolu AdediranNo ratings yet
- PIIS1198743X20306972Document4 pagesPIIS1198743X20306972KARLA PATRICIA DIAZ LOPEZNo ratings yet
- Jurnal 20Document5 pagesJurnal 20Ahmad Fari Arief LopaNo ratings yet
- JurnalDocument6 pagesJurnalDaffa AthaNo ratings yet
- 1 s2.0 S1386653220302420 MainDocument4 pages1 s2.0 S1386653220302420 MainZahira SafouanNo ratings yet
- Multiplex Detection and Dynamics of IgG Antibodies To SARS-CoV2 and The Highly Pathogenic Human Coronaviruses SARS-CoV and MERS-CoVDocument7 pagesMultiplex Detection and Dynamics of IgG Antibodies To SARS-CoV2 and The Highly Pathogenic Human Coronaviruses SARS-CoV and MERS-CoVamyNo ratings yet
- International Journal of Infectious DiseasesDocument3 pagesInternational Journal of Infectious DiseasesDetti FahmiasyariNo ratings yet
- Mm695152a3 HDocument6 pagesMm695152a3 HKinja NinjaNo ratings yet
- Journal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFDocument33 pagesJournal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFDwi Ratna KarimNo ratings yet
- Id Now NP Rna VLDocument5 pagesId Now NP Rna VLluis achaNo ratings yet
- Usefulness of High-Resolution Computed Tomography in Early Diagnosis of Patients With Suspected COVID-19Document7 pagesUsefulness of High-Resolution Computed Tomography in Early Diagnosis of Patients With Suspected COVID-19Israel Parra-OrtegaNo ratings yet
- Diagnostic Performance of A Sars-Cov-2 Igg/Igm Lateral Flow Immunochromatography Assay in Symptomatic Patients Presenting To The Emergency DepartmentDocument3 pagesDiagnostic Performance of A Sars-Cov-2 Igg/Igm Lateral Flow Immunochromatography Assay in Symptomatic Patients Presenting To The Emergency DepartmentWilmer UcedaNo ratings yet
- Jurnal MPIDocument4 pagesJurnal MPIMarini TaslimaNo ratings yet
- Title: Improved Molecular Diagnosis of COVID-19 by The Novel, Highly Sensitive and SpecificDocument33 pagesTitle: Improved Molecular Diagnosis of COVID-19 by The Novel, Highly Sensitive and SpecificCristina GuţuNo ratings yet
- International Journal of Infectious Diseases: SciencedirectDocument7 pagesInternational Journal of Infectious Diseases: SciencedirectKinja NinjaNo ratings yet
- Pooling of Samples For Testing Sars Cov 2 in Asymptomatic PatientsDocument2 pagesPooling of Samples For Testing Sars Cov 2 in Asymptomatic Patientsm.ihsan anggiNo ratings yet
- Journal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFDocument33 pagesJournal of Clinical Microbiology-2020-Chan-JCM.00310-20.full PDFdavid zhangNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesmikhaelyosiaNo ratings yet
- Artemisin PiperaquineDocument8 pagesArtemisin PiperaquineIrma Rahayu LatarissaNo ratings yet
- Comparación de Pruebas Rápidas de Antígenos para COVID-19Document9 pagesComparación de Pruebas Rápidas de Antígenos para COVID-19Cristal Jewels DiamondNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesArum Rahmawatie VirgieNo ratings yet
- Oral, Nasal and Saliva SensitivityDocument6 pagesOral, Nasal and Saliva SensitivitySnow wanNo ratings yet
- JCM 01438-20Document9 pagesJCM 01438-20043 Ni Putu Anna NatasyaNo ratings yet
- Assessment of Diagnostic and Prognostic Laboratory Biomarkers in Severe COVID-19Document22 pagesAssessment of Diagnostic and Prognostic Laboratory Biomarkers in Severe COVID-19Reda RamzyNo ratings yet
- Predicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesDocument4 pagesPredicting Infectious Severe Acute Respiratory Syndrome Coronavirus 2 From Diagnostic SamplesmeNo ratings yet
- Different Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsDocument5 pagesDifferent Longitudinal Patterns of Nucleic Acid and Serology Testing Results Based On Disease Severity of COVID-19 PatientsagboxNo ratings yet
- 1 s2.0 S0033350620301141 MainDocument3 pages1 s2.0 S0033350620301141 MainFedrik Monte Kristo LimbongNo ratings yet
- International Journal of Infectious Diseases: A A A A A B A B A B A C A BDocument4 pagesInternational Journal of Infectious Diseases: A A A A A B A B A B A C A BAhmad Afianto MuttolibNo ratings yet
- Dynamics and Correlation Among Viral Positivity, Seroconversion, and Disease Severity in COVID-19Document15 pagesDynamics and Correlation Among Viral Positivity, Seroconversion, and Disease Severity in COVID-19yanuarizkaNo ratings yet
- Diagnostic Accuracy of A Rapid Diagnostic Test For The Early Detection of COVID 19Document4 pagesDiagnostic Accuracy of A Rapid Diagnostic Test For The Early Detection of COVID 19Franklin SierraNo ratings yet
- 1 s2.0 S1807593222004495 MainDocument9 pages1 s2.0 S1807593222004495 MainandressanrliraNo ratings yet
- Correspondence: Pandemic Peak Sars-Cov-2 Infection and Seroconversion Rates in London Frontline Health-Care WorkersDocument2 pagesCorrespondence: Pandemic Peak Sars-Cov-2 Infection and Seroconversion Rates in London Frontline Health-Care WorkersJimmy A. Camones ObregonNo ratings yet
- ArchitechDocument5 pagesArchitechERIE YUWITA SARINo ratings yet
- Rapid AntibodiDocument5 pagesRapid AntibodiDzulRizkaNo ratings yet
- XmdffaDocument5 pagesXmdffaIndira LarasatiNo ratings yet
- Jurnal 1Document5 pagesJurnal 1Jojo McalisterNo ratings yet
- JMV 9999 NaDocument10 pagesJMV 9999 NaNurul AzizahNo ratings yet
- Journal Pre-Proof: International Journal of Infectious DiseasesDocument14 pagesJournal Pre-Proof: International Journal of Infectious DiseasesMohammed Shuaib AhmedNo ratings yet
- Highly Accurate and Sensitive Diagnostic Detection of Sars-Cov-2 by Digital PCRDocument23 pagesHighly Accurate and Sensitive Diagnostic Detection of Sars-Cov-2 by Digital PCRJosé ManriqueNo ratings yet
- Comparison of Rapid Antigen TestsDocument8 pagesComparison of Rapid Antigen TestsshofidhiaaaNo ratings yet
- Journal Pre-Proof: Journal of Clinical VirologyDocument14 pagesJournal Pre-Proof: Journal of Clinical VirologyMajlinda HalitiNo ratings yet
- Anosmia and Dysgeusia Associated With Sars-Cov-2 Infection: An Age-Matched Case Control StudyDocument6 pagesAnosmia and Dysgeusia Associated With Sars-Cov-2 Infection: An Age-Matched Case Control StudyCarolina ValenzuelaNo ratings yet
- Clinical Microbiology and Infection: D. Hornuss, B. Lange, N. SCHR Oter, S. Rieg, W.V. Kern, D. WagnerDocument2 pagesClinical Microbiology and Infection: D. Hornuss, B. Lange, N. SCHR Oter, S. Rieg, W.V. Kern, D. Wagnerayuines lassyaniNo ratings yet
- Recurrence of Positive Sars Cov 2 Rna in Covid 19 A Case Report Dabiao Chen Download 2024 Full ChapterDocument25 pagesRecurrence of Positive Sars Cov 2 Rna in Covid 19 A Case Report Dabiao Chen Download 2024 Full Chapterrichard.byrd946100% (11)
- Sensitive On-Site Detection of SARS-CoV-2 by ID NOW COVID-19Document12 pagesSensitive On-Site Detection of SARS-CoV-2 by ID NOW COVID-19luis.achaNo ratings yet
- Article Andre AdiantoDocument7 pagesArticle Andre AdiantoAndre AdiantoNo ratings yet
- Anti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsDocument6 pagesAnti-SARS-CoV-2 IgG Antibody Response Among Indian COVID-19 PatientsdhairyasheelNo ratings yet
- Correspondence To: Professor Changxin Shen Department of Blood TransfusionDocument13 pagesCorrespondence To: Professor Changxin Shen Department of Blood TransfusionAlfa RidziNo ratings yet
- Journal of InfectionDocument4 pagesJournal of InfectionLorena Ek MaciasNo ratings yet
- Evaluation of A COVID 19 IgM and IgG Rapid Test An Efficient Tool For Assessment of Past Exposure To SARS CoV 2Document6 pagesEvaluation of A COVID 19 IgM and IgG Rapid Test An Efficient Tool For Assessment of Past Exposure To SARS CoV 2Alma MutiaraniNo ratings yet
- Clinical Applications of Detecting IgG, IgM or IgADocument9 pagesClinical Applications of Detecting IgG, IgM or IgAreginabrizolaraNo ratings yet
- Idcm 2021 0059Document8 pagesIdcm 2021 0059Elaine SantiagoNo ratings yet
- Diagnostic Aspect of COVIDDocument8 pagesDiagnostic Aspect of COVIDYanMardianNo ratings yet
- Réponse Immun Covid19Document8 pagesRéponse Immun Covid19Tidiane SibyNo ratings yet
- Chest CT CovidDocument6 pagesChest CT CovidShinta FrennandaNo ratings yet
- Genoamp® Real-Time PCR Tests For Detection of Covid-19: Mahtas Covid-19 Rapid Evidence UpdatesDocument5 pagesGenoamp® Real-Time PCR Tests For Detection of Covid-19: Mahtas Covid-19 Rapid Evidence UpdatesDesmond KhorNo ratings yet
- The Application of Sample Pooling For Mass Screening of Sars-Cov-2 in An Outbreak of Covid-19 in VietnamDocument4 pagesThe Application of Sample Pooling For Mass Screening of Sars-Cov-2 in An Outbreak of Covid-19 in VietnamMedtech ChuongNo ratings yet
- Main 1Document4 pagesMain 1Raya KurniawanNo ratings yet
- Donders Et Al. - 2021 - Sperm Quality and Absence of SARS-CoV-2 RNA in SemDocument9 pagesDonders Et Al. - 2021 - Sperm Quality and Absence of SARS-CoV-2 RNA in SemC. MohrNo ratings yet
- Journal Pre-Proof: Journal of Clinical VirologyDocument12 pagesJournal Pre-Proof: Journal of Clinical VirologymiNo ratings yet
- A 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerDocument9 pagesA 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerNur SanaaniNo ratings yet
- Mortons NeuromaDocument12 pagesMortons NeuromaJunben DelacruzNo ratings yet
- Genograms: Practical Tools PhysiciansDocument6 pagesGenograms: Practical Tools PhysiciansThariq Mubaraq DrcNo ratings yet
- Managing Medicine SelectionDocument25 pagesManaging Medicine SelectionShoaib BiradarNo ratings yet
- Breast, Imaging, Reporting and Data System (BI RADS) - StatPearls - NCBI Bookshelf PDFDocument3 pagesBreast, Imaging, Reporting and Data System (BI RADS) - StatPearls - NCBI Bookshelf PDFnn hijo de alguienNo ratings yet
- 7 PsccauticurrentDocument22 pages7 PsccauticurrentLuz Glenny CastroNo ratings yet
- Asthma Action Plan Budesonide FormoterolDocument2 pagesAsthma Action Plan Budesonide Formoterolabob619No ratings yet
- FmasDocument30 pagesFmashaneefmdfNo ratings yet
- Zen ShiatsuDocument90 pagesZen ShiatsuLuz Violeta Platino100% (1)
- Classification System For Complete EdentulismDocument33 pagesClassification System For Complete EdentulismSahana RangarajanNo ratings yet
- Aravind Eye Care PDFDocument10 pagesAravind Eye Care PDFJe RomeNo ratings yet
- Laboratory Trainer TheoryDocument478 pagesLaboratory Trainer Theoryمحمد الغامدي100% (1)
- AOP Form 3Document4 pagesAOP Form 3Ferzada SajiranNo ratings yet
- CPG Intrapartum and Immediate Postpartum Care PDFDocument52 pagesCPG Intrapartum and Immediate Postpartum Care PDFAngela SaldajenoNo ratings yet
- Anesthesia For Tracheal Surgery - Specific Procedures - UpToDateDocument29 pagesAnesthesia For Tracheal Surgery - Specific Procedures - UpToDateMaría Augusta Robayo UvilluzNo ratings yet
- Forensic Med. CertificateDocument9 pagesForensic Med. Certificatedeeksha100% (2)
- OxyContin (Oxycodone) MundipharmaDocument15 pagesOxyContin (Oxycodone) MundipharmaRayzal AdamNo ratings yet
- PC Metabolic AcidosisDocument4 pagesPC Metabolic AcidosisErine Emmanuelle Cawaling Hetrosa50% (2)
- Hyperprolactinemia: A Systematic Review of Diagnosis and ManagementDocument12 pagesHyperprolactinemia: A Systematic Review of Diagnosis and ManagementJaveria RphNo ratings yet
- Miocarditis Por Clozapina Ronaldson2017 Revisión SistematicaDocument19 pagesMiocarditis Por Clozapina Ronaldson2017 Revisión SistematicaAlejandro PiscitelliNo ratings yet
- NCP-Case Presentation (CHF)Document4 pagesNCP-Case Presentation (CHF)Jessamine EnriquezNo ratings yet
- Sle PaperDocument73 pagesSle PaperRight VentricleNo ratings yet
- Reaction PaperDocument2 pagesReaction PaperLinzie CariquetanNo ratings yet
- Newborn CareDocument30 pagesNewborn CareAlexandria P. OrcajadaNo ratings yet
- May 2022 NP 5 CmuDocument7 pagesMay 2022 NP 5 Cmujptorresrn09No ratings yet
- Acupuncture - MeniereDocument4 pagesAcupuncture - MeniereTinnitus Man IndonesiaNo ratings yet
- 5440 15044 1 PBDocument10 pages5440 15044 1 PBDelfia Tanjung SariNo ratings yet
- Dr. Pharmacist: Mawahib Abdelfatah MohamedDocument1 pageDr. Pharmacist: Mawahib Abdelfatah Mohamedmtariq60No ratings yet