Professional Documents
Culture Documents
Orthostatic Hypotension (Postural Hypotension) - Symptoms and Causes - Mayo Clinic
Orthostatic Hypotension (Postural Hypotension) - Symptoms and Causes - Mayo Clinic
Uploaded by
ruba al hammadiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Orthostatic Hypotension (Postural Hypotension) - Symptoms and Causes - Mayo Clinic
Orthostatic Hypotension (Postural Hypotension) - Symptoms and Causes - Mayo Clinic
Uploaded by
ruba al hammadiCopyright:
Available Formats
Find out about COVID-19, COVID-19
vaccines, and Mayo Clinic patient and
visitor updates.
English
MENU SEARCH
Request an Appointment
Patient Care & Health Information Diseases & Conditions
Orthostatic hypotension
(postural hypotension)
SECTIONS
Overview
Orthostatic hypotension — also called postural
hypotension — is a form of low blood pressure that
happens when standing after sitting or lying down.
Orthostatic hypotension can cause dizziness or
lightheadedness and possibly fainting.
Orthostatic hypotension can be mild. Episodes might
be brief. However, long-lasting orthostatic hypotension
can signal more-serious problems. It's important to see
a health care provider if you frequently feel lightheaded
when standing up.
Advertisement
Mayo Clinic does not endorse companies or products.
Advertising revenue supports our not-for-profit mission.
Advertising & Sponsorship
Policy Opportunities Ad Choices
Occasional orthostatic hypotension is usually caused
by something obvious, such as dehydration or lengthy
bed rest. The condition is easily treated. Chronic
orthostatic hypotension is usually a sign of another
health problem, so treatment depends on the cause.
Products & Services
Book: Mayo Clinic Family Health Book, 5th
Edition
Show more products from Mayo Clinic
Symptoms
The most common symptom of orthostatic hypotension
is lightheadedness or dizziness when standing after
sitting or lying down. Symptoms usually last less than
a few minutes.
Orthostatic hypotension signs and symptoms include:
Lightheadedness or dizziness upon standing
Blurry vision
Weakness
Fainting (syncope)
Confusion
When to see a doctor
Occasional dizziness or lightheadedness can be minor
— triggered by mild dehydration, low blood sugar or
overheating. Dizziness or lightheadedness can also
result from standing after sitting for a long time. If
these symptoms happen only occasionally, there's
likely no cause for concern.
It's important to see a health care provider for frequent
symptoms of orthostatic hypotension. Losing
consciousness, even for just a few seconds, is serious.
It requires seeing a provider right away.
Keep a record of your symptoms, when they occurred,
how long they lasted and what you were doing at the
time. Tell your care provider if symptoms occur at
times that could be dangerous, such as while driving.
Request an Appointment at Mayo Clinic
From Mayo Clinic to your
inbox
Sign up for free, and stay up to date on
research advancements, health tips and
current health topics, like COVID-19, plus
expertise on managing health.
Enter your email
Learn more about Mayo Clinic’s use of data.
Subscribe!
Causes
When standing from a sitting or lying position, gravity
causes blood to collect in the legs and belly. Blood
pressure drops because there's less blood flowing
back to the heart.
Usually, special cells (baroreceptors) near the heart
and neck arteries sense this lower blood pressure. The
baroreceptors send signals to the brain. This tells the
heart to beat faster and pump more blood, which
evens out blood pressure. These cells also narrow the
blood vessels and increase blood pressure.
Orthostatic hypotension occurs when something
interrupts the body's process of dealing with the low
blood pressure. Many conditions can cause orthostatic
hypotension, including:
Dehydration. Fever, vomiting, not drinking
enough fluids, severe diarrhea and strenuous
exercise with a lot of sweating can all lead to
dehydration. Dehydration decreases blood
volume. Mild dehydration can cause symptoms of
orthostatic hypotension, such as weakness,
dizziness and fatigue.
Heart problems. Some heart conditions that can
lead to low blood pressure include extremely low
heart rate (bradycardia), heart valve problems,
heart attack and heart failure. These conditions
prevent the body from quickly pumping more
blood when standing up.
Endocrine problems. Thyroid conditions,
adrenal insufficiency (Addison's disease) and low
blood sugar (hypoglycemia) can cause orthostatic
hypotension. So can diabetes, which can damage
the nerves that help send signals that control
blood pressure.
Nervous system disorders. Some nervous
system disorders, such as Parkinson's disease,
multiple system atrophy, Lewy body dementia,
pure autonomic failure and amyloidosis, can
disrupt the body's ability to control blood
pressure.
Eating meals. Some people have low blood
pressure after eating meals (postprandial
hypotension). This condition is more common in
older adults.
Risk factors
The risk factors for orthostatic hypotension include:
Age. Orthostatic hypotension is common in those
who are age 65 and older. Special cells
(baroreceptors) near the heart and neck arteries
that control blood pressure can slow as you age.
It also can be harder for an aging heart to speed
up to make up for drops in blood pressure.
Medications. These include medications used to
treat high blood pressure or heart disease, such
as diuretics, alpha blockers, beta blockers,
calcium channel blockers, angiotensin-converting
enzyme (ACE) inhibitors and nitrates.
Other medications that can increase the risk of
orthostatic hypotension include medications used
to treat Parkinson's disease, certain
antidepressants, certain antipsychotics, muscle
relaxants, medications to treat erectile
dysfunction and narcotics.
Certain diseases. Diseases that can increase
the risk of low blood pressure include some heart
conditions, such as heart valve problems, heart
attack and heart failure. They also include certain
nervous system disorders, such as Parkinson's
disease. And they include diseases that cause
nerve damage (neuropathy), such as diabetes.
Heat exposure. Being in a hot environment can
cause heavy sweating and possibly dehydration,
which can lower blood pressure and trigger
orthostatic hypotension.
Bed rest. Staying in bed for a long time because
of an illness or injury can cause weakness. This
can lead to orthostatic hypotension.
Alcohol. Drinking alcohol can increase the risk of
orthostatic hypotension.
Complications
Persistent orthostatic hypotension can cause serious
complications, especially in older adults. These
include:
Falls. Falling as a result of fainting is a common
complication in people with orthostatic
hypotension.
Stroke. The swings in blood pressure from
standing and sitting as a result of orthostatic
hypotension can be a risk factor for stroke due to
the reduced blood supply to the brain.
Cardiovascular diseases. Orthostatic
hypotension can be a risk factor for
cardiovascular diseases and complications, such
as chest pain, heart failure or heart rhythm
problems.
By Mayo Clinic Staff
Request an Appointment at Mayo Clinic
Diagnosis & treatment
May 26, 2022
Advertisement
Mayo Clinic does not endorse companies or products.
Advertising revenue supports our not-for-profit mission.
Advertising & Sponsorship
Policy Opportunities Ad Choices
Share on: Facebook Twitter
Show references
Related
Associated Procedures
Blood pressure test
Echocardiogram
Electrocardiogram (ECG or EKG)
Show more associated procedures
Products & Services
Book: Mayo Clinic Family Health Book, 5th Edition
Show more products and services from Mayo Clinic
Orthostatic hypotension (postural
hypotension)
Symptoms & causes
Diagnosis & treatment
Doctors & departments
Advertisement
Mayo Clinic Press
Check out these best-sellers and special offers on books
and newsletters from Mayo Clinic Press.
NEW – Man Overboard!
NEW – The Essential Diabetes Book
NEW – Mayo Clinic on Hearing and Balance
FREE Mayo Clinic Diet Assessment
Mayo Clinic Health Letter - FREE book
CON-20303971
Patient Care & Health Information
Diseases & Conditions
Orthostatic hypotension (postural hypotension)
Request Appointment
Symptom Checker
Contact Us
About Mayo Clinic
Employees
Find a Job
Site Map
About This Site
Twitter
Facebook
PinterestYouTube
Mayo Clinic is a not-for-profit organization. Make a donation.
Any use of this site constitutes your agreement to the Terms and
Conditions and Privacy Policy linked below.
Terms and Conditions
Privacy Policy
Notice of Privacy Practices
Notice of Nondiscrimination
Manage Cookies
A single copy of these materials may be reprinted for
noncommercial personal use only. "Mayo," "Mayo Clinic,"
"MayoClinic.org," "Mayo Clinic Healthy Living," and the triple-shield
Mayo Clinic logo are trademarks of Mayo Foundation for Medical
Education and Research.
This site complies with the
HONcode standard for trustworthy health
information:
verify here.
© 1998-2022 Mayo Foundation for Medical Education and
Research (MFMER). All rights reserved.
You might also like
- Functional Concepts and The Interior EnvironmentDocument23 pagesFunctional Concepts and The Interior EnvironmentLouella Mae ClataNo ratings yet
- Mould Change, Storage and Maintenance ProcedureDocument10 pagesMould Change, Storage and Maintenance ProcedureTechnicians SIM100% (1)
- Performing Body MassageDocument60 pagesPerforming Body MassageJoie Boquio50% (2)
- HypotensionDocument7 pagesHypotensionNader Smadi100% (3)
- Orthostatic HypotensionDocument9 pagesOrthostatic HypotensionأحمدالشحاتNo ratings yet
- HypotensionDocument9 pagesHypotensiondanny17ph100% (1)
- Blood Pressure CausesDocument4 pagesBlood Pressure CausesPatrickBulawanNo ratings yet
- Understanding Low Blood Pressure - The BasicsDocument6 pagesUnderstanding Low Blood Pressure - The BasicsRajeev Nechiyil100% (1)
- Low Blood Pressure (Hypotension) Lifestyle Mayo ClinicDocument8 pagesLow Blood Pressure (Hypotension) Lifestyle Mayo ClinicanupamrcNo ratings yet
- Low Blood Pressure MayoDocument10 pagesLow Blood Pressure MayoJairo Estupiñan DuqueNo ratings yet
- BP and Its ReasonDocument8 pagesBP and Its ReasonMuhammad FaisalNo ratings yet
- Low Blood Pressure - Google SearchDocument1 pageLow Blood Pressure - Google SearchLarissa SchuefftanNo ratings yet
- Overview (Intro - Clinical Manifestations, Causes, Risk Factors, Complications, Prevention) Assessment, Diagnosis (Med and Nursing)Document27 pagesOverview (Intro - Clinical Manifestations, Causes, Risk Factors, Complications, Prevention) Assessment, Diagnosis (Med and Nursing)Luayon FrancisNo ratings yet
- Allied Health-Blood Pressure Class AssignmentDocument4 pagesAllied Health-Blood Pressure Class Assignmentapi-385125344No ratings yet
- Berdebar DebarDocument5 pagesBerdebar DebaraghniajolandaNo ratings yet
- Hypertensive Heart DiseaseDocument8 pagesHypertensive Heart DiseaseJames TombocNo ratings yet
- How to Control High Blood Pressure Without MedicationsFrom EverandHow to Control High Blood Pressure Without MedicationsRating: 5 out of 5 stars5/5 (1)
- Heart PalpitationsDocument3 pagesHeart PalpitationsmshahidshaukatNo ratings yet
- CardiomyopathyDocument13 pagesCardiomyopathyRaprnaNo ratings yet
- Hypotension: Causes, Incidence, and Risk FactorsDocument4 pagesHypotension: Causes, Incidence, and Risk Factorsclubsanatate100% (1)
- Addison'Sdisease Symptomsandcauses MayoClinic 1705658561903Document11 pagesAddison'Sdisease Symptomsandcauses MayoClinic 1705658561903Ifeoluwa AdeniyiNo ratings yet
- Group 3 - CHF With BurnsDocument16 pagesGroup 3 - CHF With BurnsHarvey T. Dato-onNo ratings yet
- Management of Common Medical Problems of the Elderly in Plain (Non-Medical) LanguageFrom EverandManagement of Common Medical Problems of the Elderly in Plain (Non-Medical) LanguageNo ratings yet
- Cerebellar StrokeDocument17 pagesCerebellar StrokeAna CotomanNo ratings yet
- 5 CS and 5 RSDocument54 pages5 CS and 5 RSKristine CatariningNo ratings yet
- What's Causing Me To Feel Dizzy When I Bend Over?: Causes Treatment When To See A Doctor TakeawayDocument7 pagesWhat's Causing Me To Feel Dizzy When I Bend Over?: Causes Treatment When To See A Doctor TakeawayalwaysdejavuuNo ratings yet
- Low Blood Preasure BlogDocument9 pagesLow Blood Preasure BlogSheffield PharmaciesNo ratings yet
- High Blood PressureDocument10 pagesHigh Blood PressureKenneth Mark B. TevesNo ratings yet
- What Is HypertensionDocument18 pagesWhat Is HypertensionShahzad ShameemNo ratings yet
- Stroke Script - ABACDocument6 pagesStroke Script - ABACLee AndrewNo ratings yet
- Low Blood PreasureDocument9 pagesLow Blood PreasureNhs VacancyNo ratings yet
- Pubmed Health: Ventricular TachycardiaDocument8 pagesPubmed Health: Ventricular Tachycardiaphysio_shaheenNo ratings yet
- B. Pharm. 1 Year Human Anatomy & Physiology BP-112: Amity Institute of PharmacyDocument37 pagesB. Pharm. 1 Year Human Anatomy & Physiology BP-112: Amity Institute of PharmacyAyush panditNo ratings yet
- Early Warning Signs Your Blood Pressure Is Dangerously HighDocument9 pagesEarly Warning Signs Your Blood Pressure Is Dangerously HighRatnaPrasadNalamNo ratings yet
- Coronary Heart DiseaseDocument7 pagesCoronary Heart DiseaseAnzala KhanNo ratings yet
- Hypertension: Medlineplus TopicsDocument31 pagesHypertension: Medlineplus TopicsMcNover Catlin OsamNo ratings yet
- Emediong SeminarDocument33 pagesEmediong SeminarItoro UdohNo ratings yet
- 7 2015 Not Eng Csse IIDocument2 pages7 2015 Not Eng Csse IIPeer MohamedNo ratings yet
- Hypothyroidism: Causes, Incidence, and Risk FactorsDocument5 pagesHypothyroidism: Causes, Incidence, and Risk FactorsPhineas KangoreNo ratings yet
- Hosp#2Document4 pagesHosp#2tsukiyaNo ratings yet
- Coronary Artery Heart Disease CDDocument28 pagesCoronary Artery Heart Disease CDchristinaNo ratings yet
- Blood PressureDocument5 pagesBlood PressureBreann StanleyNo ratings yet
- Thyroid Disorders and Heart Conditions 3231710Document5 pagesThyroid Disorders and Heart Conditions 3231710Giiszs AlvarezNo ratings yet
- Cardiovasculer Disorders 1Document77 pagesCardiovasculer Disorders 1SaraNo ratings yet
- HypertensionDocument21 pagesHypertensionM RaisNo ratings yet
- Hypertension: High Blood PressureDocument6 pagesHypertension: High Blood PressureAnne BattulayanNo ratings yet
- Hypertension IDocument14 pagesHypertension IHilary PasiliaoNo ratings yet
- Report About HypertensionDocument11 pagesReport About HypertensionZA IDNo ratings yet
- Signs and SymptomsDocument5 pagesSigns and SymptomsMichael Eka PutraNo ratings yet
- Walking Through Pain Combatting Peripheral Arterial DiseaseFrom EverandWalking Through Pain Combatting Peripheral Arterial DiseaseNo ratings yet
- Causes of MyocarditisDocument3 pagesCauses of MyocarditisTeresa CardinozaNo ratings yet
- Strokes: Abdominal Aortic AneurismDocument5 pagesStrokes: Abdominal Aortic AneurismMaja LucasNo ratings yet
- Causes: Sheehan Syndrome, Also Known As Postpartum Hypopituitarism or Postpartum Pituitary NecrosisDocument5 pagesCauses: Sheehan Syndrome, Also Known As Postpartum Hypopituitarism or Postpartum Pituitary NecrosisHyacinth ExmundoNo ratings yet
- This Is ItDocument6 pagesThis Is Itjagipeb439No ratings yet
- Disease of Human Circulatory System: Submitted To: Jordan Aquino Submitted By: Kenta YamamotoDocument31 pagesDisease of Human Circulatory System: Submitted To: Jordan Aquino Submitted By: Kenta YamamotoCarl Maga VlogsNo ratings yet
- A Simple Guide to Hypertension and Heart DiseasesFrom EverandA Simple Guide to Hypertension and Heart DiseasesRating: 5 out of 5 stars5/5 (1)
- Chap 7 High Blood PressureDocument3 pagesChap 7 High Blood PressureSabina MoolyeNo ratings yet
- Beating High Blood Pressure Naturally: Your Complete Guide to Self-Care, Healthy Eating, and Herbal Remedies: Self Care, #1From EverandBeating High Blood Pressure Naturally: Your Complete Guide to Self-Care, Healthy Eating, and Herbal Remedies: Self Care, #1No ratings yet
- Symptoms of StrokeDocument3 pagesSymptoms of StrokeMichael Pert GonzagaNo ratings yet
- Case Study: Congestive Heart Failure By: Daniel Angelo E. ArangoDocument7 pagesCase Study: Congestive Heart Failure By: Daniel Angelo E. ArangoDaniel Angelo ArangoNo ratings yet
- KIdney FailureDocument5 pagesKIdney FailureLillabinNo ratings yet
- ME EngRW 11 Q3 0701 - SG - The Main Idea and Supporting Details in A ParagraphDocument13 pagesME EngRW 11 Q3 0701 - SG - The Main Idea and Supporting Details in A ParagraphROSEMARIE CARONo ratings yet
- Braouonline MSC Psychology Assignments Psychology I Year 2019-20Document8 pagesBraouonline MSC Psychology Assignments Psychology I Year 2019-20Telika RamuNo ratings yet
- Touch For Socioemotional and Physical Well-BeingDocument17 pagesTouch For Socioemotional and Physical Well-BeingcarlyNo ratings yet
- The Human Breathing System Part2Document23 pagesThe Human Breathing System Part2Delfin Jr UrbanoNo ratings yet
- TCE Safety Pocket Manual-11 PDFDocument41 pagesTCE Safety Pocket Manual-11 PDFqamar sayed100% (1)
- Fissura Ani Dr. Adi Rizka, SPBDocument8 pagesFissura Ani Dr. Adi Rizka, SPBErwin SyahNo ratings yet
- Business PlanDocument3 pagesBusiness PlanMony SilvaNo ratings yet
- Teacher Evaluation Report 2: March 23, 2022 Shannon Scott Temporary Iron Ridge Elementary Campus Grade 3Document12 pagesTeacher Evaluation Report 2: March 23, 2022 Shannon Scott Temporary Iron Ridge Elementary Campus Grade 3api-331862751No ratings yet
- Pengaruh Murattal Alquran Terhadap Tingkat Stres Mahasiswa Muslim Di YogyakartaDocument12 pagesPengaruh Murattal Alquran Terhadap Tingkat Stres Mahasiswa Muslim Di YogyakartaMayang AfriolaNo ratings yet
- Envirotrends Regulatory Update#105 of 2020 - PESOs Circular Regarding Safety Precautions Under Petroleum Rules 2002Document2 pagesEnvirotrends Regulatory Update#105 of 2020 - PESOs Circular Regarding Safety Precautions Under Petroleum Rules 2002Rohit ShuklaNo ratings yet
- HS-Series Instruction Manual 4HS / 6HS: Reciprocating CompressorDocument151 pagesHS-Series Instruction Manual 4HS / 6HS: Reciprocating CompressornavNo ratings yet
- 7 Signs YouDocument3 pages7 Signs Youbevs syNo ratings yet
- Consensus Statement On The Early Management of Crush Injury and Prevention of Crush SyndromeDocument8 pagesConsensus Statement On The Early Management of Crush Injury and Prevention of Crush SyndromeHaris SahirulNo ratings yet
- Las Week 7 Peh12Document6 pagesLas Week 7 Peh12Rheena-Ann Dupale PadillaNo ratings yet
- 2019年6月英语四级考试真题试卷 (完整版 第1套)Document12 pages2019年6月英语四级考试真题试卷 (完整版 第1套)jiaxuNo ratings yet
- Sphygmomanometer HM-HS-20A HM-HS-50C: AneroidDocument7 pagesSphygmomanometer HM-HS-20A HM-HS-50C: AneroidalexanderNo ratings yet
- The Effect of Overbite and Overjet On Clinical Par PDFDocument6 pagesThe Effect of Overbite and Overjet On Clinical Par PDFfennilubisNo ratings yet
- Application Form Linindo Pacific International (Group of Companies)Document3 pagesApplication Form Linindo Pacific International (Group of Companies)Yehezkiel BayuNo ratings yet
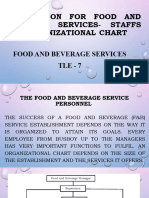
- Preparation For Food and Beverage Services - Staffs andDocument17 pagesPreparation For Food and Beverage Services - Staffs andALODIE ASUNCIONNo ratings yet
- EC Certificate - Full Quality Assurance System EC Certificate - Full Quality Assurance SystemDocument11 pagesEC Certificate - Full Quality Assurance System EC Certificate - Full Quality Assurance SystemWalid DougaishNo ratings yet
- B HCG PlusDocument4 pagesB HCG PlusSanjay DhimanNo ratings yet
- Public Health Internship: Environmental Health and Safety Intern at Berry Global Summer ScottDocument17 pagesPublic Health Internship: Environmental Health and Safety Intern at Berry Global Summer Scottapi-677941383No ratings yet
- SM 048 Surgi Max Ultra Brochure Rev ADocument2 pagesSM 048 Surgi Max Ultra Brochure Rev ACleyton NascimentoNo ratings yet
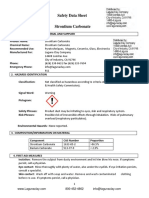
- Strontium CarbonateDocument7 pagesStrontium Carbonatetrishala shahiNo ratings yet
- Addiction From The Harmful Dysfunction Perspective - How There Can Be A Mental Disorder in A Normal Brain PDFDocument9 pagesAddiction From The Harmful Dysfunction Perspective - How There Can Be A Mental Disorder in A Normal Brain PDFAndreia AlmeidaNo ratings yet
- Accucheck Inform Ii Quick Reference Card: Tips and Tricks On Patient UseDocument2 pagesAccucheck Inform Ii Quick Reference Card: Tips and Tricks On Patient UseEmily HollandNo ratings yet
- Questions 1 - 6Document2 pagesQuestions 1 - 6Kim Oanh DinhNo ratings yet