Professional Documents
Culture Documents
Communicable Diseases CETRA
Communicable Diseases CETRA
Uploaded by
ACERET, IVAN LAURENTINE G.Copyright:
Available Formats
You might also like
- 1.a HIV Treatment Hub (Assessment Checklist)Document15 pages1.a HIV Treatment Hub (Assessment Checklist)RMON IAN100% (2)
- Idoc - Pub Nursing Care Plan For Seizure NCPDocument2 pagesIdoc - Pub Nursing Care Plan For Seizure NCPACERET, IVAN LAURENTINE G.No ratings yet
- TetanusDocument32 pagesTetanusVinotheran MichaelNo ratings yet
- Common Communicable DiseasesDocument13 pagesCommon Communicable DiseasesSanthosh.S.U100% (1)
- FlipchartDocument24 pagesFlipchartSamantha Ishi LimNo ratings yet
- Diphtheria JellyDocument23 pagesDiphtheria JellyRexaurus EncarriosusNo ratings yet
- Communicable and Non Communicable DiseasesDocument24 pagesCommunicable and Non Communicable DiseasesACERET, IVAN LAURENTINE G.No ratings yet
- School PrerequistesDocument65 pagesSchool Prerequistesmanaribrahim309No ratings yet
- Name: Carlo M. Yao Bachelor of Science in NursingDocument33 pagesName: Carlo M. Yao Bachelor of Science in Nursingcarlo24_briggsNo ratings yet
- DengueDocument4 pagesDengueAdrian Jake LiuNo ratings yet
- Communicable Diseases HandoutsDocument15 pagesCommunicable Diseases HandoutsLloyd LozanoNo ratings yet
- CHAPTER Three CommunicableDocument25 pagesCHAPTER Three CommunicableAyro Business CenterNo ratings yet
- Case 3Document27 pagesCase 3Eduard GarchitorenaNo ratings yet
- ImpetigoDocument7 pagesImpetigoBenjamin VanlaltlansangaNo ratings yet
- ImpetigoDocument66 pagesImpetigozbestgurlNo ratings yet
- Communicable DiseasesDocument164 pagesCommunicable DiseasesJasmin Jacob33% (3)
- Chicken Pox (Varicella) - Acute MUMPS (Epidemic Parotitis) - An AcuteDocument7 pagesChicken Pox (Varicella) - Acute MUMPS (Epidemic Parotitis) - An AcutejunlynNo ratings yet
- Sexually Transmitted Infections and PregnancyDocument19 pagesSexually Transmitted Infections and PregnancyBeyins TiuNo ratings yet
- Bacillary DysenteryDocument8 pagesBacillary DysenteryRijane Tabonoc OmlangNo ratings yet
- Diphtheria HandoutsDocument8 pagesDiphtheria HandoutsRachelle Mae DimayugaNo ratings yet
- Communicable DiseasesDocument6 pagesCommunicable DiseasesLory LynNo ratings yet
- Chicken PoxDocument26 pagesChicken PoxKrishna GandhiNo ratings yet
- MEASLES Case DiscussionDocument21 pagesMEASLES Case DiscussionjuiceNo ratings yet
- RabiesDocument45 pagesRabiesVivienne MiguelNo ratings yet
- Brucellosis in NepalDocument22 pagesBrucellosis in NepalBinayaNo ratings yet
- DPT Hib 2015Document42 pagesDPT Hib 2015Hannan AliNo ratings yet
- Lerelyn Case Reading4Document53 pagesLerelyn Case Reading4Ma Lerelyn DatinguinooNo ratings yet
- Lec 8 Ulcerative Vesicular & Bullous LesionsDocument6 pagesLec 8 Ulcerative Vesicular & Bullous LesionsAbd 9961No ratings yet
- Derma 2Document40 pagesDerma 2tyleree3No ratings yet
- Inflammatory & Immunologic Diseases IIIDocument252 pagesInflammatory & Immunologic Diseases IIIiamaldrinoNo ratings yet
- NCM109 - Reviewer-Lp-1-To-Lp-4Document54 pagesNCM109 - Reviewer-Lp-1-To-Lp-4princessNo ratings yet
- Definition:: Pelvic Inflammatory Disease (Pid)Document20 pagesDefinition:: Pelvic Inflammatory Disease (Pid)Malueth AnguiNo ratings yet
- Diphtheria and MeaslesDocument35 pagesDiphtheria and MeaslesMurugesanNo ratings yet
- If Maglalagay Kayo Info. Separate Niyo Narin Yung Ilalagay Sa PPT Na Mga Keywords para Di Na Mahirapan MamayaDocument11 pagesIf Maglalagay Kayo Info. Separate Niyo Narin Yung Ilalagay Sa PPT Na Mga Keywords para Di Na Mahirapan MamayaJhay-r BaldoNo ratings yet
- UNIT I Disorders Spread by Droplet InfectionsDocument20 pagesUNIT I Disorders Spread by Droplet InfectionsAmmar BhattiNo ratings yet
- Diagnosis and Management of Monkeypox in Primary Care - PDFDocument50 pagesDiagnosis and Management of Monkeypox in Primary Care - PDFGardnerNo ratings yet
- Communicable DiseasesDocument7 pagesCommunicable DiseasesRaisa Robelle Quicho100% (1)
- Diptheria Converted 200726175940Document44 pagesDiptheria Converted 2007261759407dbnf4stjyNo ratings yet
- Monkey PoxDocument29 pagesMonkey PoxMalavika A GNo ratings yet
- Eruptive Fever DiseaseDocument61 pagesEruptive Fever DiseasePearl DiBerardino100% (2)
- Locally Endemic DiseasesDocument23 pagesLocally Endemic DiseasesERMIAS, ZENDY I.No ratings yet
- Pulmonary Tuberculosis (PTB)Document6 pagesPulmonary Tuberculosis (PTB)carls burg a. resurreccion100% (2)
- MumpsDocument11 pagesMumpsamirahaliNo ratings yet
- RabiesDocument28 pagesRabiesrouhanbinrashidNo ratings yet
- Nursing Therapeutics Specifically For Children and Adolescents With Infectious DiseasesDocument86 pagesNursing Therapeutics Specifically For Children and Adolescents With Infectious Diseasesgladz25No ratings yet
- Childhood Infectious DiseasesDocument17 pagesChildhood Infectious DiseasesRNStudent1No ratings yet
- 1.2 Leptospirosis Dengue Fever Malaria Filariais EncephalitisDocument95 pages1.2 Leptospirosis Dengue Fever Malaria Filariais Encephalitisesbercinio8528valNo ratings yet
- SGD Case Presentation 8Document34 pagesSGD Case Presentation 8Karen C. Del Rosario100% (1)
- Brucellosis: Kapil Puri Gaurav ShresthaDocument22 pagesBrucellosis: Kapil Puri Gaurav ShresthaBinayaNo ratings yet
- 4 - 5798623977551169101 ExportDocument3 pages4 - 5798623977551169101 Exportجميل قطيهNo ratings yet
- Infectious Diseases 2Document12 pagesInfectious Diseases 2Jean GolezNo ratings yet
- Clinical Management Protocol PDFDocument7 pagesClinical Management Protocol PDFAJEET KUMAR PANDEYNo ratings yet
- Catarrhal Stage: 1-2 Weeks Coryza, FeverDocument45 pagesCatarrhal Stage: 1-2 Weeks Coryza, FeverAbigail BrillantesNo ratings yet
- Viral InfectionsDocument34 pagesViral InfectionsAlaa MadmoujNo ratings yet
- HIV InfectionDocument13 pagesHIV Infectionsun shineNo ratings yet
- Bacterial Infection Magazine 2Document6 pagesBacterial Infection Magazine 2Cindy Mae de la TorreNo ratings yet
- Agent Source/Mot IP POC S/S Therapeutic MGMT Complications Nurisng ConsiderationsDocument13 pagesAgent Source/Mot IP POC S/S Therapeutic MGMT Complications Nurisng ConsiderationsKuennie SabalNo ratings yet
- A. Infectious ProcessDocument22 pagesA. Infectious ProcessKyla Malapit GarvidaNo ratings yet
- LeprosyDocument10 pagesLeprosyRizweta DestinNo ratings yet
- Case Discussion ImpetigoDocument3 pagesCase Discussion ImpetigolouisNo ratings yet
- Skin Lichen Planus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSkin Lichen Planus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Parental 1Document11 pagesParental 1ACERET, IVAN LAURENTINE G.No ratings yet
- Quizlet Personality DisordersDocument27 pagesQuizlet Personality DisordersACERET, IVAN LAURENTINE G.No ratings yet
- Perioperative Nursing PDFDocument10 pagesPerioperative Nursing PDFACERET, IVAN LAURENTINE G.No ratings yet
- TPN and EtDocument11 pagesTPN and EtACERET, IVAN LAURENTINE G.No ratings yet
- Ass Device PDFDocument14 pagesAss Device PDFACERET, IVAN LAURENTINE G.No ratings yet
- TPNDocument6 pagesTPNACERET, IVAN LAURENTINE G.100% (2)
- ASSSSDocument21 pagesASSSSACERET, IVAN LAURENTINE G.No ratings yet
- Suctioning 3Document2 pagesSuctioning 3ACERET, IVAN LAURENTINE G.No ratings yet
- Parental 2Document8 pagesParental 2ACERET, IVAN LAURENTINE G.No ratings yet
- Fluid and ElectrolytesDocument8 pagesFluid and ElectrolytesACERET, IVAN LAURENTINE G.No ratings yet
- Therapeutic Communication With Older AdultsDocument4 pagesTherapeutic Communication With Older AdultsACERET, IVAN LAURENTINE G.No ratings yet
- Adult CareDocument44 pagesAdult CareACERET, IVAN LAURENTINE G.No ratings yet
- Care of Patients With Problems of The Hematologic SystemDocument12 pagesCare of Patients With Problems of The Hematologic SystemACERET, IVAN LAURENTINE G.No ratings yet
- Assessment MememeDocument2 pagesAssessment MememeACERET, IVAN LAURENTINE G.No ratings yet
- Health StatisticsDocument2 pagesHealth StatisticsACERET, IVAN LAURENTINE G.No ratings yet
- Activity or Developmental Task TheoryDocument15 pagesActivity or Developmental Task TheoryACERET, IVAN LAURENTINE G.No ratings yet
- 1 - CoparDocument30 pages1 - CoparACERET, IVAN LAURENTINE G.No ratings yet
- Med Surg CV SystemDocument9 pagesMed Surg CV SystemACERET, IVAN LAURENTINE G.No ratings yet
- Chapter 2Document16 pagesChapter 2ACERET, IVAN LAURENTINE G.No ratings yet
- nURSING ASESSEMENTDocument82 pagesnURSING ASESSEMENTACERET, IVAN LAURENTINE G.No ratings yet
- NCM 107 Rle Individual and Group Case Study NCM 107 InstructorsDocument35 pagesNCM 107 Rle Individual and Group Case Study NCM 107 InstructorsACERET, IVAN LAURENTINE G.No ratings yet
- Paeds AssessmentDocument29 pagesPaeds AssessmentACERET, IVAN LAURENTINE G.No ratings yet
- Concept of CHNDocument34 pagesConcept of CHNACERET, IVAN LAURENTINE G.No ratings yet
- Communicable and Non Communicable DiseasesDocument24 pagesCommunicable and Non Communicable DiseasesACERET, IVAN LAURENTINE G.No ratings yet
- Vi. Course of Visit Home Visit: 1st Day - Establish RapportDocument5 pagesVi. Course of Visit Home Visit: 1st Day - Establish RapportACERET, IVAN LAURENTINE G.No ratings yet
- Home Visit - 3rd DayDocument2 pagesHome Visit - 3rd DayACERET, IVAN LAURENTINE G.No ratings yet
- HOME VISIT - 1st Day Establish RapportDocument2 pagesHOME VISIT - 1st Day Establish RapportACERET, IVAN LAURENTINE G.No ratings yet
- Phenol MSDSDocument1 pagePhenol MSDSGermán Cárdenas AlvarezNo ratings yet
- Final Research Essay DropboxDocument12 pagesFinal Research Essay Dropboxapi-584319388No ratings yet
- Origin of The Pantaneiro Horse in Brazil: Additional Keywords Palabras Clave AdicionalesDocument11 pagesOrigin of The Pantaneiro Horse in Brazil: Additional Keywords Palabras Clave AdicionalesmmbasquesNo ratings yet
- A 1 CDocument8 pagesA 1 CRajiv Ranjan100% (1)
- Case Report 3 MukokelDocument3 pagesCase Report 3 MukokelWidychii GadiestchhetyaNo ratings yet
- Management of Sleep Disorders in ElderlyDocument20 pagesManagement of Sleep Disorders in ElderlyRiyaSinghNo ratings yet
- (Livestock Health Ii (Livestock Parasites)Document5 pages(Livestock Health Ii (Livestock Parasites)Brian BrianNo ratings yet
- AmpkDocument9 pagesAmpkEgieAprianNo ratings yet
- Chap# 9 / IGCSE Biology/ 0610 Animal TransportDocument6 pagesChap# 9 / IGCSE Biology/ 0610 Animal TransportAtif MohammadNo ratings yet
- HBS-Distance Learning - Heart Diagram LabelingDocument4 pagesHBS-Distance Learning - Heart Diagram LabelingCin CinNo ratings yet
- 33 MCQs On Renal Physiology USMLE Step 1 ForumDocument23 pages33 MCQs On Renal Physiology USMLE Step 1 ForumAisha YolaNo ratings yet
- SNV Emo Demos Case Study - January 2019Document8 pagesSNV Emo Demos Case Study - January 2019zvitaNo ratings yet
- History and Literary Works of Alexander PopeDocument9 pagesHistory and Literary Works of Alexander PopeYang MarañoNo ratings yet
- Cervical Cancer in PregnancyDocument21 pagesCervical Cancer in Pregnancymineresearch100% (1)
- Molecular-Docking Study of Malaria DrugDocument14 pagesMolecular-Docking Study of Malaria DrugJubairNo ratings yet
- Differential Diagnosis: Giant Cystic Abdominal Masses in Children and Adolescents: UltrasonicDocument5 pagesDifferential Diagnosis: Giant Cystic Abdominal Masses in Children and Adolescents: UltrasonicGoran MaliNo ratings yet
- Chronic Myeloid LeukemiaDocument26 pagesChronic Myeloid LeukemiaasaleemnaNo ratings yet
- IDLife ID Nutrition FAQDocument7 pagesIDLife ID Nutrition FAQIdlife SupplementsNo ratings yet
- Dar ProspectusDocument280 pagesDar ProspectusAntony Obanda100% (1)
- LLENAS - DLL Sci 9 - Sept 5 9 KMLDocument6 pagesLLENAS - DLL Sci 9 - Sept 5 9 KMLNicole Eve Pelaez-AbarrientosNo ratings yet
- Whooping Cough Letter Shahala Middle SchoolDocument2 pagesWhooping Cough Letter Shahala Middle SchoolKGW NewsNo ratings yet
- Managment of Trauma Patient in ERDocument46 pagesManagment of Trauma Patient in ERtofanNo ratings yet
- Hollow Organ InjuryDocument47 pagesHollow Organ InjuryreginaNo ratings yet
- Angelman Syndrome: Genetic ProfileDocument4 pagesAngelman Syndrome: Genetic ProfileChelseaNo ratings yet
- Reading For Journal WritingDocument4 pagesReading For Journal WritingRAPIDAH BINTI OMAR KPM-GuruNo ratings yet
- Assignment of Pathology 401: Submitted byDocument5 pagesAssignment of Pathology 401: Submitted byaymen gulzarNo ratings yet
- Medical Reimbursement AptranscoDocument13 pagesMedical Reimbursement AptranscopenusilaNo ratings yet
- Dermatology System - Answer KeysDocument5 pagesDermatology System - Answer KeysF6imNo ratings yet
- 5096 s07 Ms 2Document7 pages5096 s07 Ms 2mstudy1234560% (1)
Communicable Diseases CETRA
Communicable Diseases CETRA
Uploaded by
ACERET, IVAN LAURENTINE G.Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Communicable Diseases CETRA
Communicable Diseases CETRA
Uploaded by
ACERET, IVAN LAURENTINE G.Copyright:
Available Formats
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Cetra, Bridgette Charise T. September 28, 2022
BSN 3B NCM 113 RLE (5320)
COMMUNICABLE DISEASES
I. DISEASES AFFECTING INTEGUMENTARY SYSTEM
Bacterial
Leprosy
- It is also known as Hansen’s Disease, it is chronic infectious disease that mostly affects the skin,
peripheral nerves, upper respiratory tract mucosa, and the eyes. Leprosy is treatable, and early
treatment can avoid disability.
Causative Agent: Mycobacterium Leprae (closely associated with M. tuberculosis)
Mode of transmission: It is transmitted via droplets, from the nose and mouth, during close and
frequent contact with untreated cases.
Incubation period: It usually takes about 3 to 5 years for symptoms to appear after coming into contact
with the bacteria that causes leprosy. Some people do not develop symptoms until 20 years later.
Clinical manifestations:
✓ Discolored patches of skin, usually flat, that may be numb and look faded (lighter than the
skin around)
✓ Growths (nodules) on the skin
✓ Thick, stiff or dry skin
✓ Painless ulcers on the soles of feet
✓ Painless swelling or lumps on the face or earlobes
✓ Loss of eyebrows or eyelashes
Pathognomonic Sign/s:
Peripheral Nerve Enlargement
Loss of sensation
(+) skin smear test for M. leprae
Medical management/s:
Diagnostic tests: Skin Smear Test, Skin Lesion Biopsy, Lepromin Test, and Wassermann Reaction
Test
Multiple Drug Therapy is done.
- Prevent drug resistance (esp. Dapsone – mainstay drug)
- Hasten recovery
- Lessen period of communicability (1-2 weeks)
Paucibacillary Multibacillary
Rifampicin – once/month Rifampicin – once/month
Dapsone – OD Dapsone – OD
Duration: 6-9 mos. Lamphen – OD (SE: hyperpigmentation of skin)
Duration: 12-18 mos.
Nursing responsibilities:
• Psychological Aspect of Care because of low self-esteem and social stigma
• Clean the wounds with saline or nontoxic substances as indicated.
• Apply a sterile bandage to cover the wounds and maintain an aseptic technique.
• Provide/encourage physical exercise
• Provide information to community people that leprosy is an infectious disease but curable
with treatment.
• Provide information to community people that leprosy is an infectious disease but curable
with treatment.
• Provide drug information
- Encourage the affected people to maintain regular medical care with Multidrug therapy
(MTD).
- Monitor any signs of adverse effects regarding medications and take proper action.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Bubonic Plague
- It is also known as Black Death, an illness that is mostly transmitted to people by infected fleas
that travel on rodents. It killed millions of Europeans during the Middle Ages. Prevention does
not entail vaccination, but it does include limiting your exposure to infected mice, rats,
squirrels, and other animals.
Causative Agent: Yersinia pestis
Mode of transmission: It is most often transmitted by the bite of an infected flea. Less common
exposures include handling infected animal tissues (hunters, wildlife personnel), inhalation of infectious
droplets from cats or dogs with plague, and, rarely, contact with a pneumonic plague patient.
Incubation period: It usually takes 1–6 days
Clinical manifestations:
✓ rapid onset of fever
✓ body malaise
✓ chills
✓ seizures
✓ muscle cramps
✓ painful, swollen, and tender lymph nodes, usually inguinal, axillary, or cervical
Pathognomonic Sign/s:
Swollen lymph nodes or buboes which is very painful and hot-to-the-touch and can range from 1-
10cm in length.
Medical management/s:
- Antibiotics such as streptomycin, gentamicin, doxycycline, or ciprofloxacin are used to
treat plague.
- Oxygen, intravenous fluids, and respiratory support are usually also needed.
Nursing responsibilities:
• Begin antibiotic medication immediately as ordered
• When plague is detected, the patient should be hospitalized and isolated as soon as possible.
• Maintain standard safety procedures.
• Obtain a contact history so that persons who have had close contact with the patient can be
checked and treated, if necessary.
Erysipelas
- It is a common bacterial skin infection. It affects the upper dermis and the lymphatic veins
within the skin.
Causative Agent: group A streptococcal bacteria, especially Streptococcus pyogenes
Mode of transmission: They may enter through a wound, an insect bite, or lesions caused by another
condition, such as eczema or scabies.
Incubation period: It usually takes 24 to 48 hours.
Clinical manifestations:
✓ lesion may feel hot and be painful
✓ high fever
✓ chills
✓ headache
✓ nausea
✓ skin in the affected area may resemble the peel of an orange
✓ Infants: may appear on the abdomen due to infection of the umbilical cord.
Pathognomonic Sign/s:
raised, well-defined, tender, and bright red rash
Medical management/s:
- Penicillin administered orally or intramuscularly is sufficient for most cases of classic
erysipelas and should be given for 5 days, but if the infection has not improved, treatment
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
duration should be extended. A first-generation cephalosporin may be used if the patient
has an allergy to penicillin.
• Nursing responsibilities:
• Symptomatic treatment of aches and fever
• Hydration (oral intake if possible)
• Cold compresses
• Elevation and rest of the affected limb: Recommended to reduce local swelling,
inflammation, and pain
• Saline wet dressings: Should be applied to ulcerated and necrotic lesions and changed every
2-12 hours, depending on the severity of the infection
Yaws
- It is a common bacterial skin infection. It affects the upper dermis and the lymphatic veins
within the skin.
Causative Agent: group A streptococcal bacteria, especially Streptococcus pyogenes
Mode of transmission: They may enter through a wound, an insect bite, or lesions caused by another
condition, such as eczema or scabies.
Incubation period: It usually takes 24 to 48 hours.
Clinical manifestations:
✓ lesion may feel hot and be painful
✓ high fever
✓ chills
✓ headache
✓ nausea
✓ skin in the affected area may resemble the peel of an orange
✓ Infants: may appear on the abdomen due to infection of the umbilical cord.
Pathognomonic Sign/s:
raised, well-defined, tender, and bright red rash
Medical management/s:
- Penicillin administered orally or intramuscularly is sufficient for most cases of classic
erysipelas and should be given for 5 days, but if the infection has not improved, treatment
duration should be extended. A first-generation cephalosporin may be used if the patient
has an allergy to penicillin.
Nursing responsibilities:
• Symptomatic treatment of aches and fever
• Hydration (oral intake if possible)
• Cold compresses
• Elevation and rest of the affected limb: Recommended to reduce local swelling, inflammation,
and pain
• Saline wet dressings: Should be applied to ulcerated and necrotic lesions and changed every 2-
12 hours, depending on the severity of the infection
Viral
German Measles
- It is also known as 3-day disease or Rubella, a contagious disease that mostly affects
children.
Causative Agent: Rubella virus (RuV) (Pseudo paramyxovirus/Togavirus)
Mode of transmission: It is spread when someone who is infected coughs or sneezes tiny germ-filled
droplets into the air and onto surfaces (Direct-droplet).
Incubation period: The average incubation period of rubella virus is 17 days, with a range of 12 to 23
days.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Clinical manifestations:
✓ pink or red-spotted rash (first sign of infection) that starts on the face and spreads to the rest
of the body.
✓ Pre-eruptive Stage
- Presence or absence of fever (1 to 2 days)
- Mild cough or mild colds
✓ Eruptive Stage
Maculo-papular rashes
- Pinkish, discreet – smaller/finer rashes
- Cephalocaudal – starts at the face
- 24 hrs entire body
Enlargement of lymph nodes – differentiating factor between measles and German measles
✓ Post-eruptive Stage
- Rashes disappears (3rd day of illness)
- Enlarged lymph node gradually subsides
Pathognomonic Sign/s:
Forchheimer Spots
- Fine red spots/ Petechial spots
- Soft palate
Medical management/s:
- Blood tests and a virus culture to confirm
- No specific medicine to treat rubella or make the disease go away faster
- Reverse-transcription polymerase chain reaction (PCR) evaluation
- Chest radiography
- Vitamin A
- Antivirals
- Vaccines
- Immunoglobulins
Nursing responsibilities:
• Advise the patient or the S/O to drink plenty of fluids.
• Educate that getting plenty of rest will help the body to heal.
• Avoid contact with people who have never had rubella and who have not been immunized.
• Advise the patient to try not to scratch the rash. Put wet and cold cloths on the rash to reduce itching.
• Instruct patient to take an over-the-counter pain medicine, such as acetaminophen (Tylenol),
• ibuprofen (Advil, Motrin), or naproxen (Aleve), to reduce fever and discomfort.
Measles
- It is also known as rubeola, one of the most contagious infectious diseases, with at least a 90%
secondary infection rate in susceptible domestic contacts. It can affect all ages.
• Causative Agent: Morbillivirus
• Mode of transmission: The virus is transmitted by direct contact with infectious droplets or by
airborne spread when an infected person breathes, coughs, or sneezes.
• Incubation period: The incubation period of measles from exposure to prodrome averages 11 to 12
days. The time from exposure to rash onset averages 14 days, with a range of 7 to 21 days. The
prodrome lasts 2 to 4 days, with a range of 1 to 7 days.
• Clinical manifestations:
✓ Pre-eruptive Stage
o High grade fever (3 to 4 days)
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
o 3 C’s
- Cough
- Colds/ coryza
- Conjunctivitis
o Eyes are red, excessive lacrimal discharges
o Photosensitivity
✓ Eruptive Stage
o Maculo-papular rashes
o Reddish, blotchy
o Cephalocaudal – 1st appears behind the ears, face, neck, extremities
o Appears 3rd day of illness (2 to 3 days entire body)
✓ Post-eruptive Stage
o Fine branny
o Desquamation
o If the spots start to peel off – on the road to recovery
• Pathognomonic Sign/s:
Koplick Spots
- Fine red spots with bluish or grayish white spot at the center
- Within the inner cheek
• Medical management/s:
- Blood tests and a virus culture to confirm
- No specific medicine to treat rubella or make the disease go away faster
- Reverse-transcription polymerase chain reaction (PCR) evaluation
- Chest radiography
- Vitamin A
- Antivirals
- Vaccines
- Immunoglobulins
• Nursing responsibilities:
• Patients will need to be on isolation precautions to decrease transmission within the
community; emphasize the need for immediate isolation when early catarrhal symptoms
appear.
• Measles causes extreme pruritus; nursing interventions include keeping the patient’s nails
short, encourage long pants and sleeves to prevent scratching, keeping skin moist with health
care provider recommended lotions, and avoiding sunlight and heat.
• Treat conjunctivitis with warm saline when removing eye secretions and encourage patient not
to rub eyes; protect the eyes from the glare of strong light.
• Encourage oral hydration; medical literature encourages the use of oral rehydration solution.
• Antipyretics should be administered to the patient as ordered for a temperature greater than
100.4 Fahrenheit unless directed elsewise by a healthcare provider; be sure to remind parents
not to administer aspirin due to the risk of Reye’s syndrome.
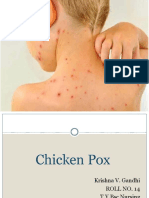
Chicken pox
- It is a highly contagious disease that causes an itchy rash with small, fluid-filled blisters.
• Causative Agent: Varicella-zoster virus
• Mode of transmission: The virus can be spread from person to person by direct contact, inhalation
of aerosols from vesicular fluid of skin lesions of acute varicella or zoster, and possibly through
infected respiratory secretions that also may be aerosolized.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
• Incubation period: The average incubation period for varicella is 14 to 16 days after exposure to a
varicella or a herpes zoster rash, with a range of 10 to 21 days
• Clinical manifestations:
✓ Pre-eruptive Stage – 24 to 48 hours
- Presence of absence of low-grade fever
- Headache
- body malaise
- muscle pain
✓ Eruptive Stage
- Vesiculo-papular/ pustular rashes
- Macule → Papule → Vesicle →Vesiculopapular
- Itchy – Pock Marks
✓ Post-eruptive Stage
- Rashes start to dry
- Crusts (dry), falls off (peels off)
• Pathognomonic Sign/s:
Rash that turns into itchy, fluid-filled blisters that eventually turn into scabs
• Medical management/s:
- Use Acetaminophen (Tylenol) for Pain and Fever
- Antiviral therapy
- Varicella zoster immune globulin
- Antibiotic therapy.
• Nursing responsibilities:
• Educate parents about the importance and safety of the Varicella Zoster vaccine.
• Manage pruritus in patients with varicella with cool compresses and regular bathing; warm
soaks and oatmeal or cornstarch baths may reduce itching and provide comfort.
• Trimming the child’s fingernails and having the child wear mittens while sleeping may reduce
scratching.
• Advise parents to provide a full and unrestricted diet to the child
Herpes Zoster
- It is also known as shingles, is caused by the reactivation of the varicella-zoster virus (VZV), the
same virus that causes varicella (chickenpox).
• Causative Agent: Varicella-zoster virus
• Mode of transmission: The virus is spread through direct contact with the rash or through
• breathing in virus particles that get mixed in the air.
• Incubation period: The average incubation period for varicella is 14 to 16 days after exposure or a
herpes zoster rash with a range of 10 to 21 days.
• Clinical manifestations:
✓ Enlarged lymph nodes
✓ Fever, chills, and headache
✓ Itching
✓ Raised dots on your skin and redness in that area
✓ Stabbing or shooting pain
✓ Tingling or burning feeling in or under your skin
✓ Upset stomach
• Pathognomonic Sign/s:
rash and sometimes even before the rash appears patients have typical pain in a dermatomal
distribution.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
• Medical management/s:
- Symptomatic treatment
- Antivirals (acyclovir, famciclovir, valacyclovir), especially for immunocompromised patients
• Nursing responsibilities:
• Assess the client’s description of pain or discomfort: severity, location, quality, duration,
precipitating or relieving factors.
• Assess for nonverbal signs of pain or discomfort.
• Educate the client about the following measures:
• Wear loose, nonrestrictive clothing made of cotton.
• Apply cool, moist dressings to pruritic lesions with or without Burrow’s solution several times a
day. Discontinue once the lesions have dried.
• Avoid temperature extremes, in both the air and bathwater.
• Avoid rubbing or scratching the skin or lesion.
• Use topical steroids (anti-inflammatory effect), anti-histamines (anti-itching effect, particularly
useful at bedtime), and analgesics.
• Use topical steroids (anti-inflammatory effect), anti-histamines (anti-itching effect, particularly
useful at bedtime), and analgesics.
II. DISEASES AFFECTING THE GASTROINTESTINAL TRACT
Bacterial
Bacillary dysentery
- It is also known as shigellosis, a gastrointestinal disease caused by bacterial infection.
Causative Agent: Shigella
Mode of transmission: The virus is spread through direct contact with the rash or through breathing
in virus particles that get mixed in the air.
Incubation period: The incubation period is usually 1 - 3 days, but can be up to 7 days.
Clinical manifestations:
✓ Diarrhea containing blood or mucus.
✓ High fever.
✓ Painful stomach cramps.
✓ Nausea and vomiting
Pathognomonic Sign/s:
Stool may contain blood and mucus.
Medical management/s:
- Stool Examination
- Rectal Swab
- Antibiotic (Ciprofloxacin)
- Oral rehydration Therapy
Nursing responsibilities:
- Rehydrate patient with oral or IV fluid and antibiotics
- Monitor signs and symptoms of dehydration and teach the patient to finish medication
- Warn patient to avoid antimotility medications which delay excretion of microorganisms
- Assess for vital signs, sudden increase in pulse rate, extreme pallor, and prostration may
indicate impending shock or intestinal perforation.
- Educate patient and/or S/O about the 5 keys to food safety in handling food: Choose (Choose
safe raw materials); Clean (Keep hands and utensils clean); Separate (Separate raw and
cooked food); Cook (Cook thoroughly); and Safe Temperature (Keep food at safe
temperature) to prevent foodborne diseases
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Cholera
Causative Agent: Vibrio Cholerae
Mode of transmission: A person can get cholera by drinking water or eating food contaminated with
cholera bacteria. In an epidemic, the source of the contamination is usually the feces of an infected
person that contaminates water or food. The disease can spread rapidly in areas with inadequate
treatment of sewage and drinking water.
Incubation period: The incubation period of cholera is between 2 hours and 5 days.
Clinical manifestations:
✓ profuse watery diarrhea
✓ vomiting
✓ thirst
✓ leg cramps
✓ restlessness or irritability
Pathognomonic Sign/s:
Rice-watery stools
Medical management/s:
- Stool Examination
- Rectal Swab
- Antibiotic (Tetracycline)
- IV Therapy
Nursing responsibilities:
- Assess the status of dehydration (skin color, temperature, skin turgor, mucous membranes, eyes,
crown, body temperature, pulse, respiration, behavior, weight loss).
- Observe for a sudden attack of diarrhea, fever, anorexia, vomiting, nausea, abdominal cramps,
increased bowel sounds, and bowel movements more than 3 times a day, with liquid stool
consistency, with or without mucus or blood.
- Assess for the knowledge of diarrhea at home, dietary knowledge, and knowledge about the
prevention of recurrent diarrhea.
- Drink plenty of fluids to avoid dehydration. Oral Rehydration Salt (ORS) is used to prevent
dehydration.
- Daily weight is an indicator of overall fluid and nutritional status.
- Maintain hydration. Replace ongoing fluid losses until diarrhea stops.
- Administer medications as indicated. Give an oral antibiotic to the patient with severe
dehydration as prescribed.
Food poisoning (has types: protein & carbohydrates)
- It is also known as food-borne illness which is the result of eating contaminated, spoiled, or toxic
food.
Protein poisoning is when the body takes in too much protein with not enough fat and
carbohydrate for a long period of time. It is also known as “rabbit starvation” or “mal de
caribou.” These terms came about to describe only consuming very lean proteins, such as
rabbit, without consuming other nutrients.
Carbohydrates poisoning is an excessive intake of different types of carbohydrates ranging
from digestible polysaccharides to refined sugars that collectively mediate noxious effects on
human health, a phenomenon that we refer to as ''carbotoxicity.
Causative Agent: Norovirus, Salmonella, Clostridium perfringens, Campylobacter, Staphylococcus
aureus (Staph, listeria
Campylobacter Meat and poultry. Contamination occurs during processing if animal
feces contact meat surfaces. Other sources include unpasteurized milk
and contaminated water.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Clostridium perfringens Meats, stews and gravies. Commonly spread when serving dishes don't
keep food hot enough or food is chilled too slowly.
Noroviruses Raw, ready-to-eat produce and shellfish from contaminated water. Can
be spread by an infected food handler.
Staphylococcus aureus Meats and prepared salads, cream sauces, and cream-filled pastries. Can
be spread by hand contact, coughing and sneezing.
Salmonella Raw or contaminated meat, poultry, milk, or egg yolks. Survives
inadequate cooking. Can be spread by knives, cutting surfaces or an
infected food handler.
Listeria Queso fresco and other soft cheeses, raw sprouts, melons, hot dogs,
pâtés, deli meats, smoked seafood, and raw (unpasteurized) milk
Mode of transmission: It is usually caused by the consumption of contaminated food or water
containing bacteria, viruses, parasites, biotoxins or chemicals. Places where such agents are commonly
found: Widely distributed in domestic and wild animals.
Incubation period: It usually begins 6 to 24 hours after exposure
Clinical manifestations:
✓ Upset stomach
✓ Stomach cramps
✓ Nausea
✓ Vomiting
✓ Diarrhea
✓ Fever
Pathognomonic Sign/s:
puffy cheeks and swollen jaw
Medical management/s:
- Replacement of lost fluids. Fluids and electrolytes — minerals such as sodium, potassium and
calcium that maintain the balance of fluids in your body — lost to persistent diarrhea need to be
replaced
- Hydration formulas such as Pedialyte™ can be helpful
- Doctor may prescribe antibiotics if you have a certain kind of bacterial food poisoning and your
symptoms are severe. Food poisoning caused by listeria needs to be treated with intravenous
antibiotics during hospitalization
Nursing responsibilities:
- Assess the condition of patient.
- Assess the type of poisoning
- Oral rehydration is achieved by administering clear liquids and sodium-containing and glucose-
containing solutions. A simple ORS may be composed of 1 level teaspoon of salt and 4 heaping
teaspoons of sugar added to 1 liter of water.
Viral
Mumps
- It is a viral infection that primarily affects saliva-producing (salivary) glands that are located near
your ears.
Causative Agent: Paramyxovirus, a member of the Rubulavirus family.
Mode of transmission: It is transmitted person to person through direct contact with saliva or
respiratory droplets of a person infected with mumps.
Incubation period: The average incubation period for mumps is 16 to 18 days, with a range of 12 to 25
days
Clinical manifestations:
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
✓ Fever
✓ Headache
✓ Muscle aches
✓ Tiredness
✓ Loss of appetite
Pathognomonic Sign/s:
puffy cheeks and tender, swollen jaw
Medical management/s:
- Antipyretics (acetaminophen) to reduce fever.
- Analgesics – NSAID
- Antiviral regimens
Nursing responsibilities:
- Educate patient about mumps
- Encourage hydration and rest
- Educate about hand washing
- Tell patient to keep away from school or work until symptoms subside
- Educate caregiver on vaccination
- Take acetaminophen for pain
- Evaluate patient for other complications like pancreatitis, orchitis, aseptic meningitis,
weakness, etc.
Parasite
Protozoa
- A type of gastroenteritis brought on by a parasite
Causative Agent: Giardia and Cryptosporidium
Mode of transmission: It is transmitted by consumption of contaminated water and food. Exposure to
an infected person through his/her blood.
Incubation period: It usually takes 10-15 days
Clinical manifestations:
✓ Diarrhea
✓ Stomach cramps
✓ Fatigue
✓ Loss of appetite
✓ Low blood pressure
✓ Low grade fever
Medical management/s:
- Anthelminthics
Nursing responsibilities:
- Encourage the patient to drink plenty of fluids
- Monitor patient for signs of dehydration.
- Remind patient to wash hands after using the bathroom and before eating or handling food.
Flukes
- Liver flukes are parasites that can infect humans and infect the liver, gallbladder, and bile duct in
humans.
Causative Agent: Opisthorchiidae (Clonorchis and Opisthorchis) and Fasciolidae (Fasciola)
Mode of transmission: Humans can get by eating raw or undercooked fish, crabs, or crayfish from
areas where the parasite is found.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Incubation period: The infection is patent about 10-12 weeks after the metacercariae are ingested.
The whole cycle takes 18-20 weeks. The hatching of fluke eggs and the multiplication of snails depend
on adequate moisture and temperatures greater than 10ºC.
Clinical manifestations:
✓ fever
✓ chills
✓ abdominal pain
✓ liver enlargement
✓ nausea
✓ vomiting
✓ hives
Medical management/s:
- Triclabendazole
- Praziquantel
Nursing responsibilities:
- Increase the electrolyte and fluid balance.
- Monitor fluid intake and output and look out for dehydration symptoms
- Reduce pain and discomfort.
• Determine the kind and severity of the pain
• Determine the kind and severity of the pain
• Provide a warm compress to the abdomen
• Teach a distraction technique to lessen discomfort
• Choose a comfortable position that helps lessen pain.
- Improve nutrition. Give a balanced diet, daily body weight measurements, emphasize the need of
proper nutrition and practice excellent oral hygiene.
III. DISEASES AFFECTING THE RESPIRATORY SYSTEM
Bacterial
Diphtheria
- It is a serious bacterial infection that usually affects the mucous membranes of the nose and
throat.
Causative Agent: Corynabacterium diphtheriae (Klebs – loeffler bacilli)
Mode of transmission: It is spread from person to person, usually through respiratory droplets, like
from coughing or sneezing. People can also get sick from touching infected open sores or ulcers.
Incubation period: It usually takes 2-6 days
Clinical manifestations:
✓ a thick grey-white coating that may cover the back of your throat, nose and tongue.
✓ a high temperature (fever)
✓ sore throat.
✓ swollen glands in your neck.
✓ difficulty breathing and swallowing.
Pathognomonic Sign/s:
swollen glands (enlarged lymph nodes) in the neck
Medical management/s:
- Nose and throat culture
- Schick’s test – intradermal injection of toxin, will show (+) without immunity, 1-3 cm
- Moloney test – intradermal injection of toxoid, if positive there is erythema within 24 hrs
(hypersensitivity to Diphtheria toxoid)
- Penicillin G Sodium
- Supportive: Oxygen inhalation
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
- Tracheostomy
- Suction secretions
Nursing responsibilities:
- Strict Isolation
- Complete bed rest
- Concurrent disinfection
- Proper disposal of nasopharyngeal secretions
- Complete bed rest
- Liquid to soft diet
- Small frequent feedings
- Increase fluid intake
Pertussis
- It is also known as whooping cough which is a highly contagious respiratory disease
Causative Agent: Bordetella pertussis
Mode of transmission: It is spread easily from person to person through the air. When a person who
has whooping cough sneezes or coughs, they can release small particles with the bacteria in them.
Other people then breathe in the bacteria.
Incubation period: It usually takes 7-10 days, while disease takes 6 weeks
Clinical manifestations:
✓ Catarrhal Stage
- nasal catarrhal, frequent sneezing, teary-eyed
- cough
✓ Paroxysmal Stage
- cough worsens: becomes rapid, successive, paroxysmal, ends in inspiratory whoop,
followed by vomiting
- force of coughing may cause involuntary micturition/defecation, bulging of eyes,
intracerebral hemorrhage, abdominal hernia
- vomiting signals end attack
✓ Convalescent Stage
- Episodes of coughing become less frequent and not as severe
- Slow recovery begins during this phase of the disease.
- Occasionally episodes of coughing may recur for months.
Pathognomonic Sign/s:
Violent coughing followed by a whooping sound made as a person gasp for air
Medical management/s:
- Borde-Gengou Culture nasopharyngeal swab
- Penicillin
Nursing responsibilities:
- Bed rest
- Proper positioning during attacks
- Nutritious diet
- Abdominal binders
- Adequate ventilation
- Close nursing observation during attacks
- Concurrent disinfection
- Avoid precipitating attacks
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Viral
Influenza
- It is also known as flu which is viral infection that attacks your respiratory system — your
nose, throat and lungs.
Causative Agent: Influenza virus
Mode of transmission: It is spread mainly by droplets made when people with flu cough, sneeze, or
talk. These droplets can land in the mouths or noses of people who are nearby (usually within about 6
feet away) or possibly be inhaled into the lungs.
Incubation period: It is usually two days but can range from one to four days.
Clinical manifestations:
✓ fever* or feeling feverish/chills.
✓ cough.
✓ sore throat.
✓ runny or stuffy nose.
✓ muscle or body aches.
✓ headaches.
✓ fatigue (tiredness)
✓ some people may have vomiting and diarrhea, though this is more common in children than
adults.
Medical management/s:
- Oseltamivir (Tamiflu)
- Zanamivir (Relenza)
- Peramivir (Rapivab)
- Baloxavir (Xofluza)
- Rapid diagnostic tests
- Polymerase chain reaction testing
- Direct immunofluorescent tests
- Serologic testing
- Testing for Avian infuenza
- Chest radiography
Nursing responsibilities:
- Assess respiratory status for rate, depth, ease, use of accessory muscles, and work of breathing
- Auscultate the lung fields for the presence of wheezes, crackles (rales), rhonchi, or decreased
breath sounds.
- Administer oxygen as ordered. Monitor oxygen saturation by pulse oximetry, and notify the
physician of readings <90% or as prescribed by the physician.
- Assess patient for pallor or cyanosis, especially to nail beds and around the mouth.
- Monitor patient for cough and production of sputum, noting amount, color, character, and
patient’s ability to expectorate secretions, and the ability to cough
- Position patient in high Fowler’s or semi-Fowler’s position, if possible.
- Turn the patient every 2 hours and as needed
- Administer bronchodilators as ordered
- Perform postural drainage and percussion, as ordered.
- Encourage fluids, up to 3-4 L/day unless contraindicated.
- Encourage deep breathing exercises and coughing exercises every 2 hours
- Instruct patient to avoid excessively hot or cold fluids or environmental temperature extremes
- Teach the patient or significant others regarding splinting abdomen with a pillow during cough
efforts.
- Instruct patient/family to avoid crowds and persons with upper respiratory infections when
possible.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Coryza
- It describes symptoms of cold which is the inflammation of the mucous membranes lining the
nasal cavity which usually gives rise to the symptoms of nasal congestion and loss of smell, among
other symptoms.
Causative Agent: Haemophilus paragallinarum
Mode of transmission: Airborne infection by dust or respiratorydischarge droplets, and contamination
of feed and water.
Incubation period: The incubation period is 1–3 days with a typical disease duration of 2–3 weeks.
Clinical manifestations:
✓ Nasal discharge
✓ Nasal obstruction
✓ Sneezing
✓ Sore throat
✓ General malaise
✓ Cough
✓ Hoarseness
✓ Loss of taste and smell
✓ Mild burning of the eyes
✓ Feeling of pressure in the ears or sinuses, due to obstruction
✓ Mucosal swelling
✓ Fever
Medical management/s:
- Erythromycin
- Oxytetracycline
- Sulfonamides
- Fluoroquinolones
- Macrolides
- Vitamin C
Nursing responsibilities:
- Give warm salt-water gargles to relieve sore throat pain.
- Encourage the patient to have adequate rest and have plenty of fluids.
- Administer analgesics, decongestants, and expectorants as indicated.
IV. DISEASE AFFECTING THE CIRCULATORY SYSTEM
Malaria
- It is a serious and sometimes fatal disease caused by a parasite that commonly infects a certain
type of mosquito which feeds on humans
Causative Agent: Plasmodium
- Vivax –most common
o Falciparum – most common/most fatal
- Ovale
- Malariae
Mode of transmission: Usually, people get malaria by being bitten by an infective female Anopheles
mosquito. Only Anopheles mosquitoes can transmit malaria and they must have been infected through
a previous blood meal taken from an infected person.
Incubation period: The incubation period in most cases varies from 7 to 30 days. The shorter periods
are observed most frequently with P. falciparum and the longer ones with P. malariae.
Clinical manifestations:
✓ Cold Stage (15mins.)
- Chilling sensation (shaking of the body)
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
- Keep patient warm (provide with blanket
- warm drinks
- expose to droplight
- hot water bag as ordered on soles of feet
✓ Hot Stage (2-6 hours)
- High grade fever
- Vomiting
- Abdominal pain
✓ Wet Stage
- Profuse sweating
- Feeling of weakness
Medical management/s:
- Blood smears
- Rapid diagnostic tests.
- Atovaquone-proguanil (Malarone)
- Quinine sulfate (Qualaquin) with doxycycline (Oracea, Vibramycin, others)
- Primaquine phosphate
- Chloroquine phosphate
- Artemisinin-based combination therapies (ACTs)
Nursing responsibilities:
- Improve body temperature. Warm water compress on forehead and both axilla (not more than
15 minutes each time)
- Maintain warm environment by using warm blankets, adequate clothing)
- Improve tissue perfusion. Patient may need supplemental oxygen if condition is severe;
maintain a well-ventilated room, head of the bed at 30º
- Lessen activities that require moderate to high exertion.
- Improve fluid volume. Encourage increase in oral fluid intake and administer parenteral fluids
as ordered.
- Educate the patient and family.
V. DISEASES AFFECTING THE GENITO-URINARY SYSTEM
Bacterial
Gonorrhea
- It is also known as Clap, drip, or ‘tulo’ which is an infection caused by a sexually transmitted
bacterium that infects both males and females. Gonorrhea most often affects the urethra,
rectum or throat. In females, gonorrhea can also infect the cervix.
Causative Agent: Neisseria gonorrhoeae bacterium
Mode of transmission: It is transmitted through sexual contact with the penis, vagina, mouth, or anus
of an infected partner. It can also be spread perinatally from mother to baby during childbirth.
Incubation period: It usually takes 3 to 21 days.
Clinical manifestations:
✓ Male – obvious signs because same opening for reproduction and urination
- Urethritis, dysuria
- Redness and edema of urinary meatus
- Purulent urethral discharge
- Frequent gonorrhea - scar in the epididymis – obstruct flow of sperm cell -sterility
✓ Female – shows symptoms if they have Pelvic Inflammatory Disease; urethra is not usually
affected
- Urethral discharge
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
- Frequent gonorrhea - Narrowing of the fallopian tube – ectopic pregnancy/ sterility
✓ Gonococcal septicemia
- Tender papillary skin lesion (pustular, hemorrhagic or necrotic)
- Migratory polyarthralgia
- Polyarthritis
- tenosynovitis
Pathognomonic Sign/s:
Pus draining from the genitalia in the morning
Medical management/s:
- Culture and sensitivity
▪ Urethral discharge
▪ Swab/scrape directly on the anterior urethra
- Cervical smear/ Pap smear
- Penicillin – Benzathine Penicillin G
- Cephalosporin – Ceftriaxone, Cefuroxime
- Tetracycline – Doxycycline
Nursing responsibilities:
- Use standard precautions when obtaining specimens for laboratory examination and when
caring for the patient.
- Isolate the patient with an eye infection.
- If the patient has gonococcal arthritis, apply moist heat to ease the pain in the affected joints.
- Before treatment, determine if the patient has any drug sensitivities.
- Monitor the patient for complications.
- Tell the patient that until cultures prove negative, he’s still infectious and should avoid
unprotected sexual contact.
- Urge the patient to inform his sexual partners of his infection so that they can seek treatment.
- Advise the partner of an infected person to receive treatment even if she doesn’t have positive
cultures.
- Counsel the patient and his sexual partners to be tested for human immunodeficiency virus
and hepatitis B infection.
- Instruct the patient to be careful when coming in contact with his bodily discharges so that he
doesn’t contaminate his eyes.
- Tell the patient to take anti-infective drugs for the length of time prescribed.
- Promoting screening to asymptomatic patients who may be at risk of STIs
- Referring all people with suspected or confirmed gonorrhea to a GUM clinic or other local
specialist sexual health service
- Managing people in primary care when referral is not possible or acceptable
- To prevent reinfection, tell the patient to avoid sexual contact with anyone suspected of being
infected, to use condoms during intercourse, to wash genitalia with soap and water before
and after intercourse.
Syphilis
- It is also known as Pox, Lues, Bad Blood Disease which is a bacterial infection usually spread by
sexual contact
Causative Agent: Treponema Pallidum
Mode of transmission: It can be spread from person-to-person by direct contact with a syphilitic sore,
known as a chancre. Chancres can occur in, on, or around the penis, vagina, anus, rectum, and lips or
mouth. Syphilis can spread during vaginal, anal, or oral sex.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Incubation period: The average time between acquisition of syphilis and the start of the first symptom
is 21 days. However, this can range from 10 to 90 days.
Clinical manifestations:
✓ Primary
▪ Chancre
- Painless moist ulcer that heals spontaneously with or without treatment
- Genitals or extragenital (face, fingers, tongue, anal, lips)
▪ Regional lymphadenopathy
✓ Secondary/ Infectious
▪ Highly communicable
▪ Flu-like symptoms
▪ Fever, headache, body malaise, sore throat
▪ Skin rashes, condyloma lata/ condylomata lata
- Lesions fused together found under the breast or genitalia
▪ Oral mucous patches
▪ Patchy alopecia
▪ Thinning of pubic hair
▪ Generalized lymphadenopathy
✓ Latent Phase
▪ Asymptomatic (1 to 2 yrs)
▪ May still spread infection
✓ Tertiary/ Late Stage
▪ Gumma – infiltrating tumor (skin, bone, liver)
▪ Not communicable
▪ CV changes – aortitis, aneurysms
▪ CNS degeneration – paresthesia, abnormal reflexes, shooting pains, dementia, psychosis
Pathognomonic Sign/s:
Maculopapular rash (seen in 50–70% of patients) that may affect the palms and soles
Chancre
Medical management/s:
- Darkfield microscope
- Serologic test
▪ FTA-ABS (Flourescent Treponema Antibody Absorption Test) – DEFINITIVE
▪ VDRL (Venereal Disease Research Laboratory)
o RPR (Rapid Plasma Reagin)
- Primary, secondary or early latent syphilis
o single dose of intramuscular (IM) penicillin G benzathine 2.4 million units.
o Alternative therapies: doxycycline 100 mg orally (PO) twice daily for 14 days or
ceftriaxone 1 to 2 gm IM or intravenously (IV) daily for 10 to 14 days or tetracycline
100 mg PO 4 times daily for 14 days.
- Late latent syphilis
o IM penicillin G benzathine 2.4 million units once weekly for 3 weeks.
o Alternative therapies: doxycycline 100 mg PO twice daily for 28 days or tetracycline
100 mg PO four times daily for 28 days.
- Tertiary syphilis
o IM penicillin G benzathine 2.4 million units once weekly for 3 weeks.
- Neurosyphilis
o treated IV penicillin G aqueous 18-24 million units daily for 10 to 14 days.
Nursing responsibilities:
- Educate patient on safe sex practice
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
- Encourage the use of condoms
- Encourage treatment of a partner
- Administer benzathine penicillin
- Educate patient on avoiding sex with an infected partner
- Listen to the heart for the murmur of aortic regurgitation
- Check the chest x-ray report (syphilis can cause aortic aneurysms)
- Assess neurologic and mental status (rule out tertiary syphilis)
- Assess genitals to ensure healing has occurred
Chancroid
- It is also known as soft chancre which is a sexually transmitted disease (STD) that results in
sores on your genitals
Causative Agent: Haemophilus ducreyi
Mode of transmission: It is spread by sexual contact with an infected individual. The bacteria are more
likely to invade the sexual organs at the point of a pre-existing injury, such as a small cut or scratch.
The likelihood of transmission is greater if a person is very active sexually and does not practice
personal hygiene.
Incubation period: The incubation period for chancroid is about three to seven days
Clinical manifestations:
✓ Raised and painful bumps on the skin of your genitals.
✓ Ulcers with ragged soft edges that develop from these bumps.
✓ Reddened and shiny skin on the sores.
✓ Leakage of pus and infectious fluid.
✓ Spreading and connecting of these sores into larger areas.
Pathognomonic Sign/s:
Painful ulcer
Medical management/s:
- azithromycin
- ceftriaxone
- ciprofoxacin
- erythromycin
Nursing responsibilities:
- Use standard precautions whenever you may come into contact with genital secretions – for
instance, when collecting specimens and performing a physical examination.
- Administer anti-ineffective medications and, possibly, analgesics as ordered.
- Provide topical care by washing the affected area with soap and water, followed by a bacterial
agent. Don’t allow the area to remain moist; this can enhance the growth of the organism.
- Report all cases of chancroid to the local board of health if required in your state.
- Examine the patient’s sexual contacts and refer them for treatment, even if they’re
asymptomatic.
- Monitor the effectiveness of analgesic administration by asking the patient to rate his pain before
and after receiving the drug.
- Inspect the ulcers for signs of healing as well as signs of localized infection.
- Instruct the patient to take his anti-infective medication for the period prescribed.
- Teach the patient not to apply creams, lotions, or oils on or near his genitalia or on other lesion
sites.
- Advice the patient to abstain from sexual contact until follow-up evaluation shows that healing is
complete usually about 2 weeks after treatment begins.
- Inform patient that condoms may provide protection from future infection.
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
Granuloma Inguinale
- It is also known as donovanosis which is a sexually transmitted disease (STD) that is rarely seen in
the United States. The disease is commonly found in tropical and subtropical areas such as
southeast India, Guyana, and New Guinea. There are about 100 cases reported per year in the
United States. Most of these cases occur in people who have traveled to or are from places where
the disease is common.
Causative Agent: Klebsiella granulomatis
Mode of transmission: The mode of transmission of granuloma inguinale primarily occurs through
sexual contact; however, it is hypothesized to have low infectious capabilities because repeated
exposure is necessary for clinical infection to occur.
Incubation period: Symptoms of granuloma inguinale usually begin 1 to 12 weeks after infection.
Clinical manifestations:
✓ Sores in the anal area
✓ Small, beefy-red bumps on the genitals or around the anus
✓ skin gradually wears away
Pathognomonic Sign/s:
painless bumps turn into raised, beefy-red, velvety nodules (granulation tissue)
Medical management/s:
- Culture of tissue sample (hard to do and not routinely available)
- Scrapings or biopsy of lesion
- Trimethoprim-sulfamethoxazole
- doxycycline
- erythromycin
- ciprofloxacin
- azithromycin
Nursing responsibilities:
- Educate the patient about the regular and correct use of condoms
- Encourage people on the avoidance of unsafe sex practices, such as frequently changing sex
- partners or having sexual intercourse with prostitutes or with partners who have other sex
- partners
- Prompt diagnosis and treatment of the infection (to prevent spread to other people)
- Identification of the sexual contacts of infected people, followed by counseling or treatment of
- these contacts
Viral
Lymphogranuloma Venerium
- It is an ulcerative disease of the genital area
Causative Agent: Chlamydia trachomatis serovars L1, L2, and L3
Mode of transmission: It is spread through unprotected anal, oral or vaginal sexual contact, especially
if there is trauma to the skin or mucous membranes. It can also be spread via sharing of sex toys
between partners
Incubation period: The incubation period for LGV ranges from three to 30 days after infection for a
primary lesion and from 10 days up to several months if a bubo is the first manifestation
Clinical manifestations:
✓ Primary stage
- small, painless papule that can ulcerate to form a herpetiform lesion or chancre
- Mucopurulent discharge of the rectum, urethra, or cervix
✓ Secondary stage/Inguinal Stage
- painful inguinofemoral lymphadenopathy, "buboes".
- proctitis and infection of the perirectal and pelvic lymph nodes
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
- pelvic, lower abdominal, or low back pain
- nodes appear fleshy and show diffuse reticulosis.
- suppurative granulomatous lymphadenitis and peri lymphadenitis occur with matting of
the nodes.
- nodes coalesce to form stellate abscesses.
✓ Tertiary stage
- anogenitorectal syndrome
- resultant rectal stricture
- elephantiasis of the genitalia.
- Proctocolitis
- perirectal abscesses
- ischiorectal abscesses
- rectovaginal fistulas
- anal fistulas
- rectal stricture
Pathognomonic Sign/s:
Painful inguinofemoral lymphadenopathy, "buboes"
Medical management/s:
- Doxycycline
- erythromycin base
- azithromycin
Nursing responsibilities:
- Encourage patient to practice safe sex
- Encourage the use of condoms
- Encourage patient to remain compliant with medications
- Check labs for culture results
- Administer antibiotics as ordered
- Check labs to ensure female is not pregnant as doxycycline cannot be given in pregnancy
- Encourage the patient to notify the partner to come in for a screening test
- Encourage patient to follow up in the STD clinic
Herpes simplex
- It is most commonly known as herpes which is characterized into two types: HSV1 and HSV2.
Many people live with asymptomatic HSV, which means they have the virus without ever
having an outbreak or active episode of herpes
Causative Agent: Herpes Simplex Virus (HSV)
Mode of transmission:
▪ HSV-1 is mainly transmitted by oral-to-oral contact which is transmitted through oral secretions
or sores on the skin, can be spread through kissing or sharing objects such as toothbrushes or
eating utensils
▪ HSV-2 is a transmitted through sexual contact with someone who has genital HSV-2 infection.
Incubation period: The average incubation period for an initial herpes infection is 4 days (range, 2 to
12) after exposure. The vesicles break and leave painful ulcers that may take two to four weeks to
heal after the initial herpes infection.
Clinical manifestations:
✓ Skin may tingle, itch, or burn for a day or so.
✓ One or more painful, fluid-filled blisters may appear
✓ HSV 1
o blisters appear on the lips or around the mouth
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
o sores can appear anywhere on the skin.
✓ HSV 2
o sores typically occur on the penis, vagina, buttocks, or anus. Women can have sores
inside the vagina
o sores can appear anywhere on the skin.
✓ Fever
✓ Muscle aches
✓ Swollen lymph nodes (glands) in the neck (oral herpes) or groin (genital herpes) are possible.
✓ Have trouble urinating or have a burning feeling while urinating.
✓ Eye infection (herpes keratitis)
Pathognomonic Sign/s:
small blisters that break open, leaving painful sores
Medical management/s:
- Acyclovir
- Famciclovir
- Valacyclovir
Nursing responsibilities:
Oral herpes (herpes simplex type 1)
- If patient has sores on face, Remind him/her to:
o Do not kiss anyone
o Do not have oral sex
o Do not share items such as silverware, cups, towels, and lip balms
- Health teaching to prevent spreading the sores to other parts of the body by:
o Washing your hands after touching a cold sore.
o Using a cotton-tip swab to apply herpes medicine to a cold sore also help
Genital herpes (herpes simplex type 2)
- Educate the patient about the condition
- Tell patient to abstain from sexual activity
- Educate about the use of condoms
- Inform past, current and future partners about potential infection
- Instruct patient to gently clean the infected area with mild soap and water
- Advise the patient to wash hands before and after cleaning the infected area
- Advise the patient to use cotton undergarment
- Provide information and counseling and support groups in their area
Infectious mononucleosis
- It is also known as kissing disease which is a contagious infecton
Causative Agent: Epstein-Barr Virus
Mode of transmission: This virus spreads most commonly through bodily fluids, especially saliva.
However, these viruses can also spread through blood and semen during sexual contact, blood
transfusions, and organ transplantations.
Incubation period: Symptoms can take between 4 to 6 weeks to appear and usually do not last
beyond 4 months.
Clinical manifestations:
✓ extreme fatigue
✓ fever
✓ sore throat
✓ head and body aches
✓ swollen lymph nodes in the neck and armpits
✓ swollen liver or spleen or both
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
Saint Mary’s University
SCHOOL OF HEALTH and NATURAL SCIENCES
Nursing Department
Bayombong, Nueva Vizcaya
✓ rash
Pathognomonic Sign/s:
Swollen tonsils that appear red and with white lesions that may be oozing pus
Medical management/s:
- Monospot blood test
- Medications that reduce fever, pain, and sore throat
- Acetaminophen is the most commonly advised pain reliever
- Nonsteroidal Anti-Inflammatory Medications (NSAIDs) such as ibuprofen, naproxen, or aspirin
can also be used
- Corticosteroid injection, usually dexamethasone, rapidly reduces the swelling blocking the
throat
Nursing responsibilities:
- Obtain a history of exposure
- Check vitals and document presence of fever
- Encourage not sharing food or personal care items
- Encourage patient not to kiss
- Educate patient on avoiding sports for at least 6 weeks
- Encourage hydration
- Tell the patient not to take penicillin-like antibiotics as it may result in a rash
- Take acetaminophen for pain and headache
- Inform patients to miss school until symptoms subside
1st Floor, Constant Jurgens (UB) Building
Saint Mary’s University, Ponce St., Bayombong, Nueva Vizcaya, 3700 Philippines
Telephone: (078) 321-2221 ext. 122; Telefax: (078) 321-2117; Mobile No.: 0936-286-7269
You might also like
- 1.a HIV Treatment Hub (Assessment Checklist)Document15 pages1.a HIV Treatment Hub (Assessment Checklist)RMON IAN100% (2)
- Idoc - Pub Nursing Care Plan For Seizure NCPDocument2 pagesIdoc - Pub Nursing Care Plan For Seizure NCPACERET, IVAN LAURENTINE G.No ratings yet
- TetanusDocument32 pagesTetanusVinotheran MichaelNo ratings yet
- Common Communicable DiseasesDocument13 pagesCommon Communicable DiseasesSanthosh.S.U100% (1)
- FlipchartDocument24 pagesFlipchartSamantha Ishi LimNo ratings yet
- Diphtheria JellyDocument23 pagesDiphtheria JellyRexaurus EncarriosusNo ratings yet
- Communicable and Non Communicable DiseasesDocument24 pagesCommunicable and Non Communicable DiseasesACERET, IVAN LAURENTINE G.No ratings yet
- School PrerequistesDocument65 pagesSchool Prerequistesmanaribrahim309No ratings yet
- Name: Carlo M. Yao Bachelor of Science in NursingDocument33 pagesName: Carlo M. Yao Bachelor of Science in Nursingcarlo24_briggsNo ratings yet
- DengueDocument4 pagesDengueAdrian Jake LiuNo ratings yet
- Communicable Diseases HandoutsDocument15 pagesCommunicable Diseases HandoutsLloyd LozanoNo ratings yet
- CHAPTER Three CommunicableDocument25 pagesCHAPTER Three CommunicableAyro Business CenterNo ratings yet
- Case 3Document27 pagesCase 3Eduard GarchitorenaNo ratings yet
- ImpetigoDocument7 pagesImpetigoBenjamin VanlaltlansangaNo ratings yet
- ImpetigoDocument66 pagesImpetigozbestgurlNo ratings yet
- Communicable DiseasesDocument164 pagesCommunicable DiseasesJasmin Jacob33% (3)
- Chicken Pox (Varicella) - Acute MUMPS (Epidemic Parotitis) - An AcuteDocument7 pagesChicken Pox (Varicella) - Acute MUMPS (Epidemic Parotitis) - An AcutejunlynNo ratings yet
- Sexually Transmitted Infections and PregnancyDocument19 pagesSexually Transmitted Infections and PregnancyBeyins TiuNo ratings yet
- Bacillary DysenteryDocument8 pagesBacillary DysenteryRijane Tabonoc OmlangNo ratings yet
- Diphtheria HandoutsDocument8 pagesDiphtheria HandoutsRachelle Mae DimayugaNo ratings yet
- Communicable DiseasesDocument6 pagesCommunicable DiseasesLory LynNo ratings yet
- Chicken PoxDocument26 pagesChicken PoxKrishna GandhiNo ratings yet
- MEASLES Case DiscussionDocument21 pagesMEASLES Case DiscussionjuiceNo ratings yet
- RabiesDocument45 pagesRabiesVivienne MiguelNo ratings yet
- Brucellosis in NepalDocument22 pagesBrucellosis in NepalBinayaNo ratings yet
- DPT Hib 2015Document42 pagesDPT Hib 2015Hannan AliNo ratings yet
- Lerelyn Case Reading4Document53 pagesLerelyn Case Reading4Ma Lerelyn DatinguinooNo ratings yet
- Lec 8 Ulcerative Vesicular & Bullous LesionsDocument6 pagesLec 8 Ulcerative Vesicular & Bullous LesionsAbd 9961No ratings yet
- Derma 2Document40 pagesDerma 2tyleree3No ratings yet
- Inflammatory & Immunologic Diseases IIIDocument252 pagesInflammatory & Immunologic Diseases IIIiamaldrinoNo ratings yet
- NCM109 - Reviewer-Lp-1-To-Lp-4Document54 pagesNCM109 - Reviewer-Lp-1-To-Lp-4princessNo ratings yet
- Definition:: Pelvic Inflammatory Disease (Pid)Document20 pagesDefinition:: Pelvic Inflammatory Disease (Pid)Malueth AnguiNo ratings yet
- Diphtheria and MeaslesDocument35 pagesDiphtheria and MeaslesMurugesanNo ratings yet
- If Maglalagay Kayo Info. Separate Niyo Narin Yung Ilalagay Sa PPT Na Mga Keywords para Di Na Mahirapan MamayaDocument11 pagesIf Maglalagay Kayo Info. Separate Niyo Narin Yung Ilalagay Sa PPT Na Mga Keywords para Di Na Mahirapan MamayaJhay-r BaldoNo ratings yet
- UNIT I Disorders Spread by Droplet InfectionsDocument20 pagesUNIT I Disorders Spread by Droplet InfectionsAmmar BhattiNo ratings yet
- Diagnosis and Management of Monkeypox in Primary Care - PDFDocument50 pagesDiagnosis and Management of Monkeypox in Primary Care - PDFGardnerNo ratings yet
- Communicable DiseasesDocument7 pagesCommunicable DiseasesRaisa Robelle Quicho100% (1)
- Diptheria Converted 200726175940Document44 pagesDiptheria Converted 2007261759407dbnf4stjyNo ratings yet
- Monkey PoxDocument29 pagesMonkey PoxMalavika A GNo ratings yet
- Eruptive Fever DiseaseDocument61 pagesEruptive Fever DiseasePearl DiBerardino100% (2)
- Locally Endemic DiseasesDocument23 pagesLocally Endemic DiseasesERMIAS, ZENDY I.No ratings yet
- Pulmonary Tuberculosis (PTB)Document6 pagesPulmonary Tuberculosis (PTB)carls burg a. resurreccion100% (2)
- MumpsDocument11 pagesMumpsamirahaliNo ratings yet
- RabiesDocument28 pagesRabiesrouhanbinrashidNo ratings yet
- Nursing Therapeutics Specifically For Children and Adolescents With Infectious DiseasesDocument86 pagesNursing Therapeutics Specifically For Children and Adolescents With Infectious Diseasesgladz25No ratings yet
- Childhood Infectious DiseasesDocument17 pagesChildhood Infectious DiseasesRNStudent1No ratings yet
- 1.2 Leptospirosis Dengue Fever Malaria Filariais EncephalitisDocument95 pages1.2 Leptospirosis Dengue Fever Malaria Filariais Encephalitisesbercinio8528valNo ratings yet
- SGD Case Presentation 8Document34 pagesSGD Case Presentation 8Karen C. Del Rosario100% (1)
- Brucellosis: Kapil Puri Gaurav ShresthaDocument22 pagesBrucellosis: Kapil Puri Gaurav ShresthaBinayaNo ratings yet
- 4 - 5798623977551169101 ExportDocument3 pages4 - 5798623977551169101 Exportجميل قطيهNo ratings yet
- Infectious Diseases 2Document12 pagesInfectious Diseases 2Jean GolezNo ratings yet
- Clinical Management Protocol PDFDocument7 pagesClinical Management Protocol PDFAJEET KUMAR PANDEYNo ratings yet
- Catarrhal Stage: 1-2 Weeks Coryza, FeverDocument45 pagesCatarrhal Stage: 1-2 Weeks Coryza, FeverAbigail BrillantesNo ratings yet
- Viral InfectionsDocument34 pagesViral InfectionsAlaa MadmoujNo ratings yet
- HIV InfectionDocument13 pagesHIV Infectionsun shineNo ratings yet
- Bacterial Infection Magazine 2Document6 pagesBacterial Infection Magazine 2Cindy Mae de la TorreNo ratings yet
- Agent Source/Mot IP POC S/S Therapeutic MGMT Complications Nurisng ConsiderationsDocument13 pagesAgent Source/Mot IP POC S/S Therapeutic MGMT Complications Nurisng ConsiderationsKuennie SabalNo ratings yet
- A. Infectious ProcessDocument22 pagesA. Infectious ProcessKyla Malapit GarvidaNo ratings yet
- LeprosyDocument10 pagesLeprosyRizweta DestinNo ratings yet
- Case Discussion ImpetigoDocument3 pagesCase Discussion ImpetigolouisNo ratings yet
- Skin Lichen Planus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandSkin Lichen Planus, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Parental 1Document11 pagesParental 1ACERET, IVAN LAURENTINE G.No ratings yet
- Quizlet Personality DisordersDocument27 pagesQuizlet Personality DisordersACERET, IVAN LAURENTINE G.No ratings yet
- Perioperative Nursing PDFDocument10 pagesPerioperative Nursing PDFACERET, IVAN LAURENTINE G.No ratings yet
- TPN and EtDocument11 pagesTPN and EtACERET, IVAN LAURENTINE G.No ratings yet
- Ass Device PDFDocument14 pagesAss Device PDFACERET, IVAN LAURENTINE G.No ratings yet
- TPNDocument6 pagesTPNACERET, IVAN LAURENTINE G.100% (2)
- ASSSSDocument21 pagesASSSSACERET, IVAN LAURENTINE G.No ratings yet
- Suctioning 3Document2 pagesSuctioning 3ACERET, IVAN LAURENTINE G.No ratings yet
- Parental 2Document8 pagesParental 2ACERET, IVAN LAURENTINE G.No ratings yet
- Fluid and ElectrolytesDocument8 pagesFluid and ElectrolytesACERET, IVAN LAURENTINE G.No ratings yet
- Therapeutic Communication With Older AdultsDocument4 pagesTherapeutic Communication With Older AdultsACERET, IVAN LAURENTINE G.No ratings yet
- Adult CareDocument44 pagesAdult CareACERET, IVAN LAURENTINE G.No ratings yet
- Care of Patients With Problems of The Hematologic SystemDocument12 pagesCare of Patients With Problems of The Hematologic SystemACERET, IVAN LAURENTINE G.No ratings yet
- Assessment MememeDocument2 pagesAssessment MememeACERET, IVAN LAURENTINE G.No ratings yet
- Health StatisticsDocument2 pagesHealth StatisticsACERET, IVAN LAURENTINE G.No ratings yet
- Activity or Developmental Task TheoryDocument15 pagesActivity or Developmental Task TheoryACERET, IVAN LAURENTINE G.No ratings yet
- 1 - CoparDocument30 pages1 - CoparACERET, IVAN LAURENTINE G.No ratings yet
- Med Surg CV SystemDocument9 pagesMed Surg CV SystemACERET, IVAN LAURENTINE G.No ratings yet
- Chapter 2Document16 pagesChapter 2ACERET, IVAN LAURENTINE G.No ratings yet
- nURSING ASESSEMENTDocument82 pagesnURSING ASESSEMENTACERET, IVAN LAURENTINE G.No ratings yet
- NCM 107 Rle Individual and Group Case Study NCM 107 InstructorsDocument35 pagesNCM 107 Rle Individual and Group Case Study NCM 107 InstructorsACERET, IVAN LAURENTINE G.No ratings yet
- Paeds AssessmentDocument29 pagesPaeds AssessmentACERET, IVAN LAURENTINE G.No ratings yet
- Concept of CHNDocument34 pagesConcept of CHNACERET, IVAN LAURENTINE G.No ratings yet
- Communicable and Non Communicable DiseasesDocument24 pagesCommunicable and Non Communicable DiseasesACERET, IVAN LAURENTINE G.No ratings yet
- Vi. Course of Visit Home Visit: 1st Day - Establish RapportDocument5 pagesVi. Course of Visit Home Visit: 1st Day - Establish RapportACERET, IVAN LAURENTINE G.No ratings yet
- Home Visit - 3rd DayDocument2 pagesHome Visit - 3rd DayACERET, IVAN LAURENTINE G.No ratings yet
- HOME VISIT - 1st Day Establish RapportDocument2 pagesHOME VISIT - 1st Day Establish RapportACERET, IVAN LAURENTINE G.No ratings yet
- Phenol MSDSDocument1 pagePhenol MSDSGermán Cárdenas AlvarezNo ratings yet
- Final Research Essay DropboxDocument12 pagesFinal Research Essay Dropboxapi-584319388No ratings yet
- Origin of The Pantaneiro Horse in Brazil: Additional Keywords Palabras Clave AdicionalesDocument11 pagesOrigin of The Pantaneiro Horse in Brazil: Additional Keywords Palabras Clave AdicionalesmmbasquesNo ratings yet
- A 1 CDocument8 pagesA 1 CRajiv Ranjan100% (1)
- Case Report 3 MukokelDocument3 pagesCase Report 3 MukokelWidychii GadiestchhetyaNo ratings yet
- Management of Sleep Disorders in ElderlyDocument20 pagesManagement of Sleep Disorders in ElderlyRiyaSinghNo ratings yet
- (Livestock Health Ii (Livestock Parasites)Document5 pages(Livestock Health Ii (Livestock Parasites)Brian BrianNo ratings yet
- AmpkDocument9 pagesAmpkEgieAprianNo ratings yet
- Chap# 9 / IGCSE Biology/ 0610 Animal TransportDocument6 pagesChap# 9 / IGCSE Biology/ 0610 Animal TransportAtif MohammadNo ratings yet
- HBS-Distance Learning - Heart Diagram LabelingDocument4 pagesHBS-Distance Learning - Heart Diagram LabelingCin CinNo ratings yet
- 33 MCQs On Renal Physiology USMLE Step 1 ForumDocument23 pages33 MCQs On Renal Physiology USMLE Step 1 ForumAisha YolaNo ratings yet
- SNV Emo Demos Case Study - January 2019Document8 pagesSNV Emo Demos Case Study - January 2019zvitaNo ratings yet
- History and Literary Works of Alexander PopeDocument9 pagesHistory and Literary Works of Alexander PopeYang MarañoNo ratings yet
- Cervical Cancer in PregnancyDocument21 pagesCervical Cancer in Pregnancymineresearch100% (1)
- Molecular-Docking Study of Malaria DrugDocument14 pagesMolecular-Docking Study of Malaria DrugJubairNo ratings yet
- Differential Diagnosis: Giant Cystic Abdominal Masses in Children and Adolescents: UltrasonicDocument5 pagesDifferential Diagnosis: Giant Cystic Abdominal Masses in Children and Adolescents: UltrasonicGoran MaliNo ratings yet
- Chronic Myeloid LeukemiaDocument26 pagesChronic Myeloid LeukemiaasaleemnaNo ratings yet
- IDLife ID Nutrition FAQDocument7 pagesIDLife ID Nutrition FAQIdlife SupplementsNo ratings yet
- Dar ProspectusDocument280 pagesDar ProspectusAntony Obanda100% (1)
- LLENAS - DLL Sci 9 - Sept 5 9 KMLDocument6 pagesLLENAS - DLL Sci 9 - Sept 5 9 KMLNicole Eve Pelaez-AbarrientosNo ratings yet
- Whooping Cough Letter Shahala Middle SchoolDocument2 pagesWhooping Cough Letter Shahala Middle SchoolKGW NewsNo ratings yet
- Managment of Trauma Patient in ERDocument46 pagesManagment of Trauma Patient in ERtofanNo ratings yet
- Hollow Organ InjuryDocument47 pagesHollow Organ InjuryreginaNo ratings yet
- Angelman Syndrome: Genetic ProfileDocument4 pagesAngelman Syndrome: Genetic ProfileChelseaNo ratings yet
- Reading For Journal WritingDocument4 pagesReading For Journal WritingRAPIDAH BINTI OMAR KPM-GuruNo ratings yet
- Assignment of Pathology 401: Submitted byDocument5 pagesAssignment of Pathology 401: Submitted byaymen gulzarNo ratings yet
- Medical Reimbursement AptranscoDocument13 pagesMedical Reimbursement AptranscopenusilaNo ratings yet
- Dermatology System - Answer KeysDocument5 pagesDermatology System - Answer KeysF6imNo ratings yet
- 5096 s07 Ms 2Document7 pages5096 s07 Ms 2mstudy1234560% (1)