Professional Documents
Culture Documents
Normal Immunisation Schedule For All People in The UK
Normal Immunisation Schedule For All People in The UK
Uploaded by
Shashwat BajpaiCopyright:
Available Formats
You might also like
- Pharaoh Menes' Death After An Anaphylactic Reaction - The End of A Myth PDFDocument2 pagesPharaoh Menes' Death After An Anaphylactic Reaction - The End of A Myth PDFAlan KneeverNo ratings yet
- Diphtheria: Questions and Answers: Information About The Disease and VaccinesDocument3 pagesDiphtheria: Questions and Answers: Information About The Disease and VaccinesGlenn KristieNo ratings yet
- Mat UkimmunizationDocument4 pagesMat UkimmunizationNav KovNo ratings yet
- VaccinationDocument11 pagesVaccinationYogesh ShakyaNo ratings yet
- Types of ImmunizationsDocument21 pagesTypes of Immunizationsmacmactongos100% (6)
- Immunization Review GPDocument46 pagesImmunization Review GPKishore ChandkiNo ratings yet
- Expanded Program ImmunizationDocument4 pagesExpanded Program ImmunizationLheiDanielMariellMonteroNo ratings yet
- EPI Vaccines Revised Oct 2010Document18 pagesEPI Vaccines Revised Oct 2010Jei JayNo ratings yet
- Hepatitis B: Your Doctor. DR Michael Jones, Medical EditorDocument9 pagesHepatitis B: Your Doctor. DR Michael Jones, Medical Editormmbrelvi2757No ratings yet
- ImmunisationDocument29 pagesImmunisationOjambo FlaviaNo ratings yet
- Updated September 2016: PneumoniaDocument5 pagesUpdated September 2016: PneumoniaYidnekachew Girma Assefa100% (1)
- PneumoniaDocument8 pagesPneumoniaJonathan Pangibitan Jr.No ratings yet
- Infectious Pertusis-6 (Muhadharaty)Document5 pagesInfectious Pertusis-6 (Muhadharaty)dr.salam.hassaniNo ratings yet
- Epi ReportDocument5 pagesEpi ReportAce FabrigasNo ratings yet
- Lecture 5 - Whooping CoughDocument37 pagesLecture 5 - Whooping CoughShaimaa AbdulkadirNo ratings yet
- Multi Vaccine InfantsDocument4 pagesMulti Vaccine Infantssharu4291No ratings yet
- Macdona Masali AssignmentDocument5 pagesMacdona Masali AssignmentMasali MacdonaNo ratings yet
- Immunization EPI Huda 201212Document5 pagesImmunization EPI Huda 201212Aerish TupazNo ratings yet
- Vaccines: General Medical Conditions - PediatricsDocument21 pagesVaccines: General Medical Conditions - PediatricsSarah AlyssaNo ratings yet
- Baby Vaccinations: Centers For Disease Control and PreventionDocument4 pagesBaby Vaccinations: Centers For Disease Control and PreventionJha NetNo ratings yet
- TB LeafletDocument12 pagesTB LeafletAnggun PuspaNo ratings yet
- Pertussis Key Messages BBHW 9-20-2010Document4 pagesPertussis Key Messages BBHW 9-20-2010nerd_fetishNo ratings yet
- World's Deadliest Disease and Remains A Major Public Health Problem in The PhilippinesDocument17 pagesWorld's Deadliest Disease and Remains A Major Public Health Problem in The Philippineslorella_abejuelaNo ratings yet
- Uiip Flu Fact SheetDocument4 pagesUiip Flu Fact Sheetapi-277123092No ratings yet
- Vaccin UriDocument16 pagesVaccin Uriexact_euNo ratings yet
- zimbabwe vaccinationDocument2 pageszimbabwe vaccinationnothandomushati4No ratings yet
- Flu Vaccine: Information For People at RiskDocument8 pagesFlu Vaccine: Information For People at Riskkovi mNo ratings yet
- Pediatric ImmunizationDocument33 pagesPediatric ImmunizationAlaa Rached Khalid AlmekdadNo ratings yet
- TB in Children - Getting, Diagnosing, Preventing TB: TB/HIV Co-InfectionDocument10 pagesTB in Children - Getting, Diagnosing, Preventing TB: TB/HIV Co-InfectionKirt Earl RicardoNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument30 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- MCQ ImmunologyDocument79 pagesMCQ Immunologypriya009100% (2)
- HIV and ChildrenDocument32 pagesHIV and ChildrenzidabyNo ratings yet
- Vaccination and ImmunizationDocument39 pagesVaccination and ImmunizationAugust DelvoNo ratings yet
- Tambahan TransleteDocument9 pagesTambahan TransleteRamadhana PutraNo ratings yet
- Bronchiolitis: Juan Manuel LozanoDocument18 pagesBronchiolitis: Juan Manuel LozanoFelipe CamposNo ratings yet
- Routine Childhood Immunization Schedule SPRING 2016Document1 pageRoutine Childhood Immunization Schedule SPRING 2016extraxen3690No ratings yet
- Pneumonia: Key FactsDocument28 pagesPneumonia: Key FactsAri Widiastuti NiPutuNo ratings yet
- Kristia Carpio Pulmonary TuberculosisDocument31 pagesKristia Carpio Pulmonary TuberculosiskisNo ratings yet
- Flu and The Flu VaccineDocument3 pagesFlu and The Flu VaccinenursunbNo ratings yet
- Act (2) UNIDAD I.JoseVenturayElianaMedinaDocument5 pagesAct (2) UNIDAD I.JoseVenturayElianaMedinaEliana MedinaNo ratings yet
- Nursing Care For MeaslesDocument5 pagesNursing Care For MeaslesChristian Eduard de DiosNo ratings yet
- Getting To Know Influenza and Avian Flu: PneumoniaDocument2 pagesGetting To Know Influenza and Avian Flu: PneumoniaDiana Laura LeiNo ratings yet
- Vaccines CHNDocument2 pagesVaccines CHNLyra LorcaNo ratings yet
- Epidemiology of TBDocument4 pagesEpidemiology of TByam pdNo ratings yet
- Tuberculosis: Cause and TransmissionDocument6 pagesTuberculosis: Cause and TransmissionAnkit SharmaNo ratings yet
- Whooping Cough (Pertussis) InformationDocument2 pagesWhooping Cough (Pertussis) InformationtombstoneepitaphNo ratings yet
- All About TBDocument11 pagesAll About TBkhaizysikNo ratings yet
- Oleh: Ns. Hana Ariyani, M. KepDocument23 pagesOleh: Ns. Hana Ariyani, M. KepMuhammad Rizal alimuddinNo ratings yet
- Typhoid Fever WHODocument1 pageTyphoid Fever WHONurdiana QoirunisaNo ratings yet
- Pediatric Lower Respiratory Tract InfectionsDocument18 pagesPediatric Lower Respiratory Tract InfectionsSasa AbassNo ratings yet
- Vaccination Basic Information: Since There Is No Alternative To ImmunizationDocument8 pagesVaccination Basic Information: Since There Is No Alternative To ImmunizationVishal ParmarNo ratings yet
- Informe TBCDocument8 pagesInforme TBCihdanny333No ratings yet
- Epi 2020 For SharingDocument69 pagesEpi 2020 For SharingEmmy Krisha Marie PatrimonioNo ratings yet
- Tuberculosis FAQs 12 September 2022Document6 pagesTuberculosis FAQs 12 September 2022htp64ztm5gNo ratings yet
- Prophylactics of PneumoniaDocument31 pagesProphylactics of PneumoniaJoisy AloorNo ratings yet
- Pertussis OutbreakDocument2 pagesPertussis Outbreakk.agnes12No ratings yet
- Your Child's Best Defense: ImmunizationsDocument2 pagesYour Child's Best Defense: ImmunizationsNoble ChunNo ratings yet
- Case Study For TuberculosisDocument7 pagesCase Study For TuberculosisGabbii CincoNo ratings yet
- HIV AND AIDS IN CHILDREN Part2Document47 pagesHIV AND AIDS IN CHILDREN Part2Kazau FwalangaNo ratings yet
- Health Advice and Immunizations for TravelersFrom EverandHealth Advice and Immunizations for TravelersNo ratings yet
- Mapeh Pamphlet8Document4 pagesMapeh Pamphlet8Yethelesia XIINo ratings yet
- OnchocerciasisDocument5 pagesOnchocerciasislordbennett505No ratings yet
- Assignment2 PDFDocument4 pagesAssignment2 PDFJavier GonzalezNo ratings yet
- Botany AssignmentDocument21 pagesBotany Assignmentabdul hadiNo ratings yet
- Medical History Form Template IlijaDocument2 pagesMedical History Form Template IlijaИлија РадосављевићNo ratings yet
- Vol 6 Suppissue1Document7 pagesVol 6 Suppissue1spiridon_andrei2011No ratings yet
- Communicable Disease Control in Complex EmergenciesDocument14 pagesCommunicable Disease Control in Complex EmergenciesDika Agustinus AndikaNo ratings yet
- Biopharmaceu Tical Classification System (BCS) Class IIDocument2 pagesBiopharmaceu Tical Classification System (BCS) Class IIGULSHAN MADHURNo ratings yet
- 23101-Article Text-71139-1-10-20211130Document9 pages23101-Article Text-71139-1-10-20211130fino nauvalinoNo ratings yet
- Immunology Serology in Laboratory Medicine 5th Edition Turgeon Test BankDocument9 pagesImmunology Serology in Laboratory Medicine 5th Edition Turgeon Test BankMarkJoneskjsme100% (15)
- Pengaruh Perilaku Dan Status Gizi Terhadap Kejadian TB Paru Di Kota PekalonganDocument40 pagesPengaruh Perilaku Dan Status Gizi Terhadap Kejadian TB Paru Di Kota PekalonganAnonymous PGuZwT0IKNo ratings yet
- Blood Banking by BMTDocument126 pagesBlood Banking by BMTRachel Marie M. Gania100% (2)
- IB Biology Topic 11 - Animal Physiology HL Revision SheetDocument1 pageIB Biology Topic 11 - Animal Physiology HL Revision SheetLexieNo ratings yet
- Chap22 ManagementofPatientswithConditionsoftheUpperRespiratoryTractDocument3 pagesChap22 ManagementofPatientswithConditionsoftheUpperRespiratoryTractRichfel Andrea UriarteNo ratings yet
- Allergy Test PapersDocument5 pagesAllergy Test PapersDaniel MoncadaNo ratings yet
- Eczematous EruptionsDocument27 pagesEczematous EruptionsSmartcool SoNo ratings yet
- Principle of Infection ControlDocument15 pagesPrinciple of Infection ControlChristel DilleraNo ratings yet
- Farmakoterapi Gastroenteritis: Widyati Farmasis Klinik Rsal DR RamelanDocument17 pagesFarmakoterapi Gastroenteritis: Widyati Farmasis Klinik Rsal DR RamelanViona PrasetyoNo ratings yet
- Morgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2114-2211)Document98 pagesMorgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2114-2211)Wiwik SundariNo ratings yet
- Acne Vulgar & ImpetigoDocument20 pagesAcne Vulgar & Impetigosadaf nasirNo ratings yet
- Antibodies and AntigensDocument1 pageAntibodies and AntigensKaty DonNo ratings yet
- Herpes ZosterDocument12 pagesHerpes ZosterJoan MolinaNo ratings yet
- Q1. What Is Vaccine?: Vaccinology Lecture NotesDocument31 pagesQ1. What Is Vaccine?: Vaccinology Lecture Notesحوراء موجد هادي غاويNo ratings yet
- HIV Based On Harrison's Principles of Medicine 21 EdDocument4 pagesHIV Based On Harrison's Principles of Medicine 21 EdBatch V Med 2 SY 21-22No ratings yet
- Penyelidikan Kejadian Luar Biasa (KLB) Demam Chikungunya Di Kelurahan Talawaan Kab. Minahasa Utara Provinsi Sulawesiu UtaraDocument12 pagesPenyelidikan Kejadian Luar Biasa (KLB) Demam Chikungunya Di Kelurahan Talawaan Kab. Minahasa Utara Provinsi Sulawesiu UtaraRena SajaNo ratings yet
- VIDAS SARS-COV-2 IgG Package InsertDocument11 pagesVIDAS SARS-COV-2 IgG Package InsertcassNo ratings yet
- Zotero As at 18 March 2020Document1,239 pagesZotero As at 18 March 2020Br LaNo ratings yet
- Bio-Energetic Frequency ChartsDocument37 pagesBio-Energetic Frequency ChartsHayden JamesNo ratings yet
- Arayat Holy Child Educational Foundation Inc.: Medicine A of 12 STEM 3Document9 pagesArayat Holy Child Educational Foundation Inc.: Medicine A of 12 STEM 3Lamour ManlapazNo ratings yet
Normal Immunisation Schedule For All People in The UK
Normal Immunisation Schedule For All People in The UK
Uploaded by
Shashwat BajpaiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Normal Immunisation Schedule For All People in The UK
Normal Immunisation Schedule For All People in The UK
Uploaded by
Shashwat BajpaiCopyright:
Available Formats
Page 1 of 5
Immunisation - Usual UK Schedule
Immunisation has caused dramatic improvements in health. Because of immunisation, diseases such as diphtheria, tetanus, pertussis (whooping cough), measles and polio, which used to be major causes of ill health, are now rare in many countries. Some immunisations are offered to all people through the childhood immunisation programme. Some are offered to at-risk groups - listed below.
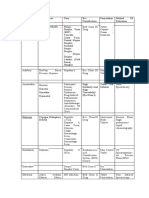
Normal immunisation schedule for all people in the UK
AGE 2 months Immunisation (Vaccine Given) DTaP/IPV(polio)/Hib (diphtheria, tetanus, pertussis (whooping cough), polio, and Haemophilus influenzae type b) - all-in-one injection, plus: PCV (pneumococcal conjugate vaccine) - in a separate injection. DTaP/IPV(polio)/Hib (2nd dose), plus: MenC (meningitis C) - in a separate injection. DTaP/IPV(polio)/Hib (3rd dose), plus: MenC (2nd dose) - in a separate injection, plus: PCV (2nd dose) - in a separate injection. Hib/MenC (combined as one injection - 4th dose of Hib and 3rd dose of MenC) plus: MMR (measles, mumps and rubella - combined as one injection), plus: PCV (3rd dose) - in a separate injection. Pre-school booster of: DTaP/IPV(polio) (diphtheria, tetanus, pertussis (whooping cough) and polio), plus: MMR (second dose) - in a separate injection. HPV (human papillomavirus) - three injections The second injection is given 1-2 months after the first one. The third is given about six months after the first one. Td/IPV(polio) booster (a combined injection of tetanus, low-dose diphtheria, and polio). Influenza and PCV if you are aged 65 or over or in a high-risk group. Td/IPV(polio) - at any age if you were not fully immunised as a child.
3 months
4 months
Between 12 and 13 months
Around 3 years and four months
Around 12-13 years (girls) Around 13-18 years Adults
Note:
Diphtheria, tetanus, pertussis (whooping cough), polio and Hib are combined into one injection - the DTaP/IPV(polio)/Hib vaccine. Pneumococcal conjugate vaccine (PCV) is a separate injection and was added to the routine immunisation schedule in September 2006. Meningitis C vaccine (MenC) is sometimes given as a separate injection but is combined with Hib for one injection. Td/IPV(polio) is tetanus, low-dose diphtheria and polio vaccines combined as one injection. Polio immunisation changed in 2004. The polio vaccine is now combined with DTaP/Hib or Td and given by injection. It used to be given by mouth (oral vaccine) as a few drops of vaccine on the tongue.
Page 2 of 5
Measles, mumps and rubella vaccines are combined into one injection - MMR. Immunisation against human papillomavirus (HPV) was introduced in the UK for girls in 2008.
Further immunisations for special at-risk groups
If you travel abroad If you travel abroad it is recommended that you should be protected against the local infections if immunisations are available. Ideally, see your practice nurse or GP for advice on travel at least two months prior to your departure. Doctors and nurses are regularly updated with immunisation requirements for every country in the world. Seasonal influenza immunisation (the flu jab) Seasonal influenza is the strain of influenza virus that arrives in the UK each autumn. The actual strain varies from year to year and a new immunisation is developed each year to protect against the prevailing strain. This year, 2010-11, the influenza immunisation will provide protection also against the influenza A virus (H1N1v) strain. The aim is to protect people who are more likely to develop complications from flu. You should be immunised against flu each autumn if you are aged 65 or over. Also, people of any age in any of the following at-risk groups. If you:
Have any chronic (ongoing) lung diseases. Examples include: chronic bronchitis, emphysema, cystic fibrosis and severe asthma (needing regular steroid inhalers or tablets). It is also recommended for any child who has previously been admitted to hospital with a chest infection. Have a chronic heart disease. Examples include: angina, heart failure or if you have ever had a heart attack. Have a serious kidney disease. Examples include: nephrotic syndrome, kidney failure, a kidney transplant. Have a serious liver disease such as cirrhosis. Have diabetes. Have a poor immune system. Examples include: if you are receiving chemotherapy or steroid treatment (for more than a month), if you have HIV/AIDS or if you have had your spleen removed. Have certain serious diseases of the nervous system, such as multiple sclerosis, or have had a stroke in the past. Live in a nursing home or other long-stay residential care accommodation.
In addition to the main at-risk groups of people listed above:
You should be immunised if you are the main carer for an elderly or disabled person whose welfare may be at risk if you fall ill with influenza. Staff involved in direct patient care may be offered a flu jab from their employer. Pregnant women. Even if you are otherwise healthy it is now recommended that all pregnant women receive the influenza immunisation. People who work in close contact with poultry.
Pneumococcal immunisation Pneumococcus is a bacterium that can cause pneumonia and meningitis. Immunisation against pneumococcus with the pneumococcal conjugate vaccine (PCV) became part of the routine childhood immunisation programme in the summer of 2006. In addition, people who are at increased risk of infection with this bacterium should be immunised. For children under five years old this is with the (routine) PCV plus a one-off dose of pneumococcal polysaccharide vaccine (PPV) as soon as possible after the second birthday. For people aged over five years, it is with a one-off dose of pneumococcal polysaccharide vaccine (PPV). You are at increased risk, and should be immunised, if you:
Are aged 65 or over.
Page 3 of 5
Do not have a spleen or if your spleen does not work properly. Have a chronic (ongoing) serious lung disease. Examples include chronic bronchitis, emphysema, cystic fibrosis and severe asthma (needing regular steroid inhalers or tablets). Are a child who has previously been admitted to hospital with pneumonia. Have a chronic heart disease. Examples include congenital heart disease, angina, heart failure or if you have ever had a heart attack. Have a serious chronic kidney disease. Examples include nephrotic syndrome, kidney failure or if you have had a kidney transplant. Have a chronic liver disease such as cirrhosis or chronic hepatitis. Have diabetes which requires insulin or tablets to control it. Have a poor immune system. Examples include if you who are receiving chemotherapy or steroid treatment (for more than a month), if you have HIV/AIDS or if you have previously had your spleen removed. Have a cochlear implant. Have a cerebrospinal fluid (CSF) shunt (a shunt to drain the fluid that surrounds the brain). Are a child aged under five years who has previously had a pneumococcal disease such as pneumococcal meningitis or pneumococcal bacteraemia.
Immunisation against tuberculosis (the BCG vaccine) The BCG vaccine (BCG stands for bacillus Calmette-Gurin) is offered to the following people in the UK:
All infants (0-12 months old) living in areas of the UK where there is a high rate of tuberculosis (TB). That is, areas where the incidence of TB is 40 cases per 100,000 people per year or greater. Infants whose parents or grandparents were born in a country with a high rate of TB. That is, countries where the incidence of TB is 40 cases per 100,000 people per year or greater. The following groups of people who have not previously been immunised:
Children (under 16 years) who have come to live in the UK from countries where TB is common (at least 40 cases per 100,000 people per year) and have not been immunised before. Children between the ages of 6-16 years who have a parent or grandparent who was born in a country where the incidence of TB is 40 cases per 100,000 people per year or greater. Children under 16 years old who are close contacts of an individual who has active TB affecting their lungs. Children under 16 years old who were born in, or have lived for more than three months in, a country where the incidence of TB is 40 cases per 100,000 people per year or greater. People at an increased risk due to their job. For example, health workers, prison staff, etc.
Note: until 2005, all schoolchildren in the UK were routinely given the BCG vaccine at about the age of 13. The policy changed in autumn 2005 and those now immunised are in the groups listed above. The policy change was due to the changing patterns of TB in the UK. Rates of the disease are now very low in many parts of the country and children living in these areas have a very low risk of infection. However, in other areas, rates of TB are increasing. This is why the BCG vaccine is now mainly targeted at babies living in areas where there is an increasing rate of TB cases. Your doctor or midwife will be able to tell you if you live in an area with a high rate of TB. Children who would previously have been offered BCG through the schools' programme will now be screened for risk factors, tested and immunised as appropriate.
Page 4 of 5
Hepatitis B immunisation This is advised for people who are at increased risk of contracting hepatitis B. For example:
Workers who are likely to come into contact with blood products, or are at increased risk of needlestick injuries, assault, etc. For example: nurses, doctors, dentists, medical laboratory workers, prison wardens, etc. Also, staff at residential centres where there is a risk of scratching or biting by residents. People who inject street drugs, their sexual partners and children. People who change sexual partners frequently. People who live in close contact with someone infected with hepatitis B. (You cannot catch hepatitis B from touching people or normal social contact. However, close regular contacts are best immunised.) People who regularly receive blood transfusions (for example, haemophilia). People with certain kidney or liver diseases. People who live in residential accommodation for those with learning difficulties. People who attend day centres for people with learning difficulties may also be offered immunisation. Families adopting children from countries with a high or intermediate prevalence of hepatitis B when the hepatitis B status of the child is unknown. (It is, however, advisable for the child to be tested for hepatitis B.) Foster carers or if you live with foster children. Prison inmates. Travellers to countries where hepatitis B is common, who place themselves at risk when abroad. The risk behaviour includes sexual activity, injecting drug use, undertaking relief work and/or participating in contact sports. Also, if you may need a medical or dental procedure in these countries and the procedure may not be done with sterile equipment. Babies who are born to infected mothers.
Immunisation against chickenpox A vaccine is offered to healthcare workers (doctors, nurses, etc) who have not previously had chickenpox and so are not immune and may catch chickenpox. (About 1 in 10 adults has not had chickenpox as a child.) If you are not sure if you have had chickenpox then a blood test can check if you have previously had it. The aim is to protect healthcare workers from developing chickenpox, but also patients. If chickenpox does not occur in any healthcare staff, this protects patients with a poor immune system (such as people with leukaemia) who may catch chickenpox from a healthcare worker who may be developing a chickenpox infection without realising it. Close contacts of people with a poor immune system who are not immune to chickenpox should also have this immunisation. For example, brothers and sisters of a child with leukaemia who have not previously had chickenpox. Infection with chickenpox can be very serious for people with a poor immune system. Other situations In some special circumstances other immunisations are considered. For example, workers who handle animals may be offered rabies immunisation. Those in close contact with people who have certain forms of meningitis may be offered specific immunisations. Discuss with your doctor or practice nurse if you think you fall into one of these groups.
Adults - are you fully immunised?
Some adults are not fully immunised against polio and tetanus. These immunisations were first introduced into the UK in the late 1950s. If you were born before then you might not have received full protection from these illnesses. Your practice nurse will be able to advise you if you are unsure.
Page 5 of 5
Who should NOT be immunised?
There are very few reasons why people should not receive their full course of immunisations. Immunisations are generally safe and effective. For some immunisations the three most common reasons why it might not be advisable are:
Pregnancy and/or breast-feeding. If your immune system is not working properly. For example, people with HIV infection, people taking chemotherapy, and people taking high-dose steroids. If you have previously had a severe reaction to the same vaccine.
See the separate leaflets on individual immunisations for more details.
How does immunisation work?
The body is given a vaccine which is a small dose of an inactive form of a bacterium or virus (germ), or a toxin (poison) made by the germ. As it is inactive, it does not cause infection. However, the body makes antibodies and/or immune cells (white blood cells) against the germ or toxin. Antibodies are proteins in the bloodstream that attack infecting germs. Once we are immunised the antibodies and/or immune cells are ready to attack the germ if it begins to invade our body. More antibody can quickly be made from cells which have previously made the particular antibody. For some bacteria and viruses it has been difficult to produce a vaccine, but technology is advancing and new vaccines will be available in the future. A newborn baby has passive immunity to several diseases, such as measles, mumps and rubella, from antibodies passed from its mother via the placenta. This passive immunity of babies usually only lasts for a few weeks or months but, for measles, mumps and rubella, it lasts up to one year. Immunisation with vaccines is called active immunity and provides long-term immunity.
Further information
Information on immunisation from the NHS Web: www.nhs.uk/Planners/vaccinations/Pages/Vaccinationchecklist.aspx
References
Immunisation against infectious disease - 'The Green Book', Dept of Health (various dates) Immunizations - childhood vaccination programme, Clinical Knowledge Summaries (February 2008) Chief Medical Officer: Changes to the BCG vaccination programme, Dept of Health (2005) The influenza immunisation programme 2010/11, Chief Medical Officer, Dept of Health (June 2010) Routine childhood immunisations from November 2010, Dept of Health
Comprehensive patient resources are available at www.patient.co.uk Disclaimer: This article is for information only and should not be used for the diagnosis or treatment of medical conditions. EMIS has used all reasonable care in compiling the information but make no warranty as to its accuracy. Consult a doctor or other health care professional for diagnosis and treatment of medical conditions. For details see our conditions. EMIS 2011 Reviewed: 18 Feb 2011 DocID: 4275 Version: 40 For the planned review period see the Data Creation and Quality Control Process.
You might also like
- Pharaoh Menes' Death After An Anaphylactic Reaction - The End of A Myth PDFDocument2 pagesPharaoh Menes' Death After An Anaphylactic Reaction - The End of A Myth PDFAlan KneeverNo ratings yet
- Diphtheria: Questions and Answers: Information About The Disease and VaccinesDocument3 pagesDiphtheria: Questions and Answers: Information About The Disease and VaccinesGlenn KristieNo ratings yet
- Mat UkimmunizationDocument4 pagesMat UkimmunizationNav KovNo ratings yet
- VaccinationDocument11 pagesVaccinationYogesh ShakyaNo ratings yet
- Types of ImmunizationsDocument21 pagesTypes of Immunizationsmacmactongos100% (6)
- Immunization Review GPDocument46 pagesImmunization Review GPKishore ChandkiNo ratings yet
- Expanded Program ImmunizationDocument4 pagesExpanded Program ImmunizationLheiDanielMariellMonteroNo ratings yet
- EPI Vaccines Revised Oct 2010Document18 pagesEPI Vaccines Revised Oct 2010Jei JayNo ratings yet
- Hepatitis B: Your Doctor. DR Michael Jones, Medical EditorDocument9 pagesHepatitis B: Your Doctor. DR Michael Jones, Medical Editormmbrelvi2757No ratings yet
- ImmunisationDocument29 pagesImmunisationOjambo FlaviaNo ratings yet
- Updated September 2016: PneumoniaDocument5 pagesUpdated September 2016: PneumoniaYidnekachew Girma Assefa100% (1)
- PneumoniaDocument8 pagesPneumoniaJonathan Pangibitan Jr.No ratings yet
- Infectious Pertusis-6 (Muhadharaty)Document5 pagesInfectious Pertusis-6 (Muhadharaty)dr.salam.hassaniNo ratings yet
- Epi ReportDocument5 pagesEpi ReportAce FabrigasNo ratings yet
- Lecture 5 - Whooping CoughDocument37 pagesLecture 5 - Whooping CoughShaimaa AbdulkadirNo ratings yet
- Multi Vaccine InfantsDocument4 pagesMulti Vaccine Infantssharu4291No ratings yet
- Macdona Masali AssignmentDocument5 pagesMacdona Masali AssignmentMasali MacdonaNo ratings yet
- Immunization EPI Huda 201212Document5 pagesImmunization EPI Huda 201212Aerish TupazNo ratings yet
- Vaccines: General Medical Conditions - PediatricsDocument21 pagesVaccines: General Medical Conditions - PediatricsSarah AlyssaNo ratings yet
- Baby Vaccinations: Centers For Disease Control and PreventionDocument4 pagesBaby Vaccinations: Centers For Disease Control and PreventionJha NetNo ratings yet
- TB LeafletDocument12 pagesTB LeafletAnggun PuspaNo ratings yet
- Pertussis Key Messages BBHW 9-20-2010Document4 pagesPertussis Key Messages BBHW 9-20-2010nerd_fetishNo ratings yet
- World's Deadliest Disease and Remains A Major Public Health Problem in The PhilippinesDocument17 pagesWorld's Deadliest Disease and Remains A Major Public Health Problem in The Philippineslorella_abejuelaNo ratings yet
- Uiip Flu Fact SheetDocument4 pagesUiip Flu Fact Sheetapi-277123092No ratings yet
- Vaccin UriDocument16 pagesVaccin Uriexact_euNo ratings yet
- zimbabwe vaccinationDocument2 pageszimbabwe vaccinationnothandomushati4No ratings yet
- Flu Vaccine: Information For People at RiskDocument8 pagesFlu Vaccine: Information For People at Riskkovi mNo ratings yet
- Pediatric ImmunizationDocument33 pagesPediatric ImmunizationAlaa Rached Khalid AlmekdadNo ratings yet
- TB in Children - Getting, Diagnosing, Preventing TB: TB/HIV Co-InfectionDocument10 pagesTB in Children - Getting, Diagnosing, Preventing TB: TB/HIV Co-InfectionKirt Earl RicardoNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument30 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- MCQ ImmunologyDocument79 pagesMCQ Immunologypriya009100% (2)
- HIV and ChildrenDocument32 pagesHIV and ChildrenzidabyNo ratings yet
- Vaccination and ImmunizationDocument39 pagesVaccination and ImmunizationAugust DelvoNo ratings yet
- Tambahan TransleteDocument9 pagesTambahan TransleteRamadhana PutraNo ratings yet
- Bronchiolitis: Juan Manuel LozanoDocument18 pagesBronchiolitis: Juan Manuel LozanoFelipe CamposNo ratings yet
- Routine Childhood Immunization Schedule SPRING 2016Document1 pageRoutine Childhood Immunization Schedule SPRING 2016extraxen3690No ratings yet
- Pneumonia: Key FactsDocument28 pagesPneumonia: Key FactsAri Widiastuti NiPutuNo ratings yet
- Kristia Carpio Pulmonary TuberculosisDocument31 pagesKristia Carpio Pulmonary TuberculosiskisNo ratings yet
- Flu and The Flu VaccineDocument3 pagesFlu and The Flu VaccinenursunbNo ratings yet
- Act (2) UNIDAD I.JoseVenturayElianaMedinaDocument5 pagesAct (2) UNIDAD I.JoseVenturayElianaMedinaEliana MedinaNo ratings yet
- Nursing Care For MeaslesDocument5 pagesNursing Care For MeaslesChristian Eduard de DiosNo ratings yet
- Getting To Know Influenza and Avian Flu: PneumoniaDocument2 pagesGetting To Know Influenza and Avian Flu: PneumoniaDiana Laura LeiNo ratings yet
- Vaccines CHNDocument2 pagesVaccines CHNLyra LorcaNo ratings yet
- Epidemiology of TBDocument4 pagesEpidemiology of TByam pdNo ratings yet
- Tuberculosis: Cause and TransmissionDocument6 pagesTuberculosis: Cause and TransmissionAnkit SharmaNo ratings yet
- Whooping Cough (Pertussis) InformationDocument2 pagesWhooping Cough (Pertussis) InformationtombstoneepitaphNo ratings yet
- All About TBDocument11 pagesAll About TBkhaizysikNo ratings yet
- Oleh: Ns. Hana Ariyani, M. KepDocument23 pagesOleh: Ns. Hana Ariyani, M. KepMuhammad Rizal alimuddinNo ratings yet
- Typhoid Fever WHODocument1 pageTyphoid Fever WHONurdiana QoirunisaNo ratings yet
- Pediatric Lower Respiratory Tract InfectionsDocument18 pagesPediatric Lower Respiratory Tract InfectionsSasa AbassNo ratings yet
- Vaccination Basic Information: Since There Is No Alternative To ImmunizationDocument8 pagesVaccination Basic Information: Since There Is No Alternative To ImmunizationVishal ParmarNo ratings yet
- Informe TBCDocument8 pagesInforme TBCihdanny333No ratings yet
- Epi 2020 For SharingDocument69 pagesEpi 2020 For SharingEmmy Krisha Marie PatrimonioNo ratings yet
- Tuberculosis FAQs 12 September 2022Document6 pagesTuberculosis FAQs 12 September 2022htp64ztm5gNo ratings yet
- Prophylactics of PneumoniaDocument31 pagesProphylactics of PneumoniaJoisy AloorNo ratings yet
- Pertussis OutbreakDocument2 pagesPertussis Outbreakk.agnes12No ratings yet
- Your Child's Best Defense: ImmunizationsDocument2 pagesYour Child's Best Defense: ImmunizationsNoble ChunNo ratings yet
- Case Study For TuberculosisDocument7 pagesCase Study For TuberculosisGabbii CincoNo ratings yet
- HIV AND AIDS IN CHILDREN Part2Document47 pagesHIV AND AIDS IN CHILDREN Part2Kazau FwalangaNo ratings yet
- Health Advice and Immunizations for TravelersFrom EverandHealth Advice and Immunizations for TravelersNo ratings yet
- Mapeh Pamphlet8Document4 pagesMapeh Pamphlet8Yethelesia XIINo ratings yet
- OnchocerciasisDocument5 pagesOnchocerciasislordbennett505No ratings yet
- Assignment2 PDFDocument4 pagesAssignment2 PDFJavier GonzalezNo ratings yet
- Botany AssignmentDocument21 pagesBotany Assignmentabdul hadiNo ratings yet
- Medical History Form Template IlijaDocument2 pagesMedical History Form Template IlijaИлија РадосављевићNo ratings yet
- Vol 6 Suppissue1Document7 pagesVol 6 Suppissue1spiridon_andrei2011No ratings yet
- Communicable Disease Control in Complex EmergenciesDocument14 pagesCommunicable Disease Control in Complex EmergenciesDika Agustinus AndikaNo ratings yet
- Biopharmaceu Tical Classification System (BCS) Class IIDocument2 pagesBiopharmaceu Tical Classification System (BCS) Class IIGULSHAN MADHURNo ratings yet
- 23101-Article Text-71139-1-10-20211130Document9 pages23101-Article Text-71139-1-10-20211130fino nauvalinoNo ratings yet
- Immunology Serology in Laboratory Medicine 5th Edition Turgeon Test BankDocument9 pagesImmunology Serology in Laboratory Medicine 5th Edition Turgeon Test BankMarkJoneskjsme100% (15)
- Pengaruh Perilaku Dan Status Gizi Terhadap Kejadian TB Paru Di Kota PekalonganDocument40 pagesPengaruh Perilaku Dan Status Gizi Terhadap Kejadian TB Paru Di Kota PekalonganAnonymous PGuZwT0IKNo ratings yet
- Blood Banking by BMTDocument126 pagesBlood Banking by BMTRachel Marie M. Gania100% (2)
- IB Biology Topic 11 - Animal Physiology HL Revision SheetDocument1 pageIB Biology Topic 11 - Animal Physiology HL Revision SheetLexieNo ratings yet
- Chap22 ManagementofPatientswithConditionsoftheUpperRespiratoryTractDocument3 pagesChap22 ManagementofPatientswithConditionsoftheUpperRespiratoryTractRichfel Andrea UriarteNo ratings yet
- Allergy Test PapersDocument5 pagesAllergy Test PapersDaniel MoncadaNo ratings yet
- Eczematous EruptionsDocument27 pagesEczematous EruptionsSmartcool SoNo ratings yet
- Principle of Infection ControlDocument15 pagesPrinciple of Infection ControlChristel DilleraNo ratings yet
- Farmakoterapi Gastroenteritis: Widyati Farmasis Klinik Rsal DR RamelanDocument17 pagesFarmakoterapi Gastroenteritis: Widyati Farmasis Klinik Rsal DR RamelanViona PrasetyoNo ratings yet
- Morgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2114-2211)Document98 pagesMorgan Mikhails Clinical Anesthesiology 6th Ed 2018 (2114-2211)Wiwik SundariNo ratings yet
- Acne Vulgar & ImpetigoDocument20 pagesAcne Vulgar & Impetigosadaf nasirNo ratings yet
- Antibodies and AntigensDocument1 pageAntibodies and AntigensKaty DonNo ratings yet
- Herpes ZosterDocument12 pagesHerpes ZosterJoan MolinaNo ratings yet
- Q1. What Is Vaccine?: Vaccinology Lecture NotesDocument31 pagesQ1. What Is Vaccine?: Vaccinology Lecture Notesحوراء موجد هادي غاويNo ratings yet
- HIV Based On Harrison's Principles of Medicine 21 EdDocument4 pagesHIV Based On Harrison's Principles of Medicine 21 EdBatch V Med 2 SY 21-22No ratings yet
- Penyelidikan Kejadian Luar Biasa (KLB) Demam Chikungunya Di Kelurahan Talawaan Kab. Minahasa Utara Provinsi Sulawesiu UtaraDocument12 pagesPenyelidikan Kejadian Luar Biasa (KLB) Demam Chikungunya Di Kelurahan Talawaan Kab. Minahasa Utara Provinsi Sulawesiu UtaraRena SajaNo ratings yet
- VIDAS SARS-COV-2 IgG Package InsertDocument11 pagesVIDAS SARS-COV-2 IgG Package InsertcassNo ratings yet
- Zotero As at 18 March 2020Document1,239 pagesZotero As at 18 March 2020Br LaNo ratings yet
- Bio-Energetic Frequency ChartsDocument37 pagesBio-Energetic Frequency ChartsHayden JamesNo ratings yet
- Arayat Holy Child Educational Foundation Inc.: Medicine A of 12 STEM 3Document9 pagesArayat Holy Child Educational Foundation Inc.: Medicine A of 12 STEM 3Lamour ManlapazNo ratings yet