Professional Documents
Culture Documents
Idiopathic Pulmonary Vein Thrombosis, Case Report
Idiopathic Pulmonary Vein Thrombosis, Case Report
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Idiopathic Pulmonary Vein Thrombosis, Case Report
Idiopathic Pulmonary Vein Thrombosis, Case Report
Copyright:
Available Formats
Volume 7, Issue 10, October – 2022 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Idiopathic Pulmonary Vein Thrombosis, Case Report
Rawan Albashrawi , internal medicine , Imam Abdulrahman university, KSA
Abstract:- Pulmonary vein thrombosis is a rare entity, History is clear from hypercoagulability diseases or
however it requires high clinical suspicion to be predisposing rheumatological conditions.
diagnosed due to lack of specific symptoms. Clinical
presentation ranges from silent event and incidental Vital signs upon presentation were stable with a heart
finding to fatal event and end organ damage. Early rate of 92 bpm, blood pressure 112/72 mmHg, respiratory
diagnosis is essential to prevent systemic complications. rate 19 per minute, and oxygen saturation of 96 % room air.
[1]
Cardiovascular and chest examination were normal.
Keywords:- Idiopathic , Pulmonary vein , CT angiogram. Rest of physical examination was unremarkable with no
noticed rashes or scars apart from previous sites of dialysis
I. INTRODUCTION line insertion, however right femoral central line was
noticed with no signs of active infection.
We describe a case of young female with multiple co-
morbidities who presented with chest pain and multiple Initial laboratory investigation indicated
episodes of haemoptysis. WBC of : 7 k/uL stable Hgb Level of 11.8 g/dL and
normal Platelets count 206 Bill/L
II. CASE REPORT Her renal function test was within her baseline with a
Bun of 60 ,Cr of 10.49 and normal electrolytes ( Na :
A 55-Year-old female known to have diabetes mellitus 135 K : 4.6 Cl : 101 ).
type II complicated by retinopathy and nephropathy, Her inflammatory markers and coagulation profile
hypertension, morbid obesity with BMI of 40 kg/m2 , end- were within normal range
stage renal disease on regular haemodialysis for two years ESR : 24 mm/hr CRP : 0.17 mg/dL and Pt : 32 sec
duration. History of multi dialysis access failure and one PTT : 13.3 sec and negative Troponin: 0.005
episode of treated line related right sided
infective endocarditis one year prior to her presentation. Chest x-ray was unremarkable while chest CT
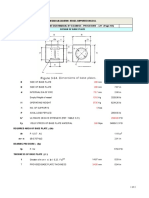
Brought to our hospital with a complain of two angiography, which was done to rule out septic emboli,
haemoptysis episodes of bright red blood with clots, the showed Left lower lobe pulmonary vein filling defect likely
amount was estimated to be around a total of 20-30 ml each representing left lower lobe pulmonary vein
episode, combined with Left side pleuritic chest pain. She thrombosis. (Figure 1)
denied any history of dyspnoea, fever, recent infection, Echocardiography was negative for thrombus or
surgery, or intervention. No other systemic symptoms were vegetation.
reported. Her social History does not illustrate any illicit
drug usage, smoking or alcohol drinking and her Family
Fig. 1: Chest CT angiogram showing left pulmonary vein filling defect.
IJISRT22OCT655 www.ijisrt.com 603
Volume 7, Issue 10, October – 2022 International Journal of Innovative Science and Research Technology
ISSN No:-2456-2165
Patient was investigated further to promote the REFERENCES
predisposing factor of her current diagnosis. This workup
included Serology for Vasculitis (ANA ,C-ANCA, P- [1.] Barreiro TJ, Kollipara VK, and Gemmel
ANCA) , Thrombophilia workup (JAK2 V617F mutation , DJ. 2018. Idiopathic pulmonary vein
Factor V and II assay ,antiphospholipid syndrome,Anti- thrombosis? Respirol. Case Rep. 6(1): 1– 4.
thrombin III level , protein C and S Levels ) And [2.] Chaaya G, Vishnubhotla P (January 23, 2017)
malignancy workup (Tumour markers , CT CAP . Pulmonary Vein Thrombosis: A Recent Systematic
Mammogram and endocervical pap smear). All workups Review. Cureus 9(1): e993.
came back negative and No identifiable cause was [3.] Alexander GR, Reddi A, and Reddy D. 2009. Idiopathic
determined to be the underlying culprit, for which patient pulmonary vein thrombosis: a rare cause of massive
was labelled to have idiopathic pulmonary vein thrombosis. hemoptysis. Ann. Thorac. Surg. 88(1): 281– 283.
[4.] Barreiro TJ, Kollipara VK, and Gemmel
Patient was started initially on Heparin infusion then DJ. 2018. Idiopathic pulmonary vein
shifted to oral anticoagulation warfarin with target INR 2-3 thrombosis? Respirol. Case Rep. 6(1):1–4.
Sec. Five days later and before discharge Chest CT [5.] Ngo, D. (2021, July 21). Idiopathic pulmonary vein
angiogram was repeated and revealed a regression of thrombosis treated with apixaban. Wiley Online
previously seen thrombus. Library. Retrieved May 6, 2022, from
https://onlinelibrary.wiley.com/doi/full/10.1002/rcr2.80
III. DISCUSSION 3
Idiopathic pulmonary vein thrombosis is extremely
rare entity with unknown incidence as most cases are exist
as case reports. This could be due to sufficient venous
collateral networks that drain the lungs. Despite this fact
early recognition is extremely important and lifesaving to
prevent systemic end organ damage [3]. Clinical
presentation for pulmonary venous thrombosis is
nonspecific and needs high clinical suspicion for diagnose.
However most reported symptoms are chest pain, cough,
shortness of breath and haemoptysis.
Aetiology for pulmonary venous thrombosis can be
classified into post-operative and non-post-
operative.[2]Causes For the non-post operative are mainly
infection, Malignancy, congenital malformation, mitral
valve stenosis or idiopathic. Up to our knowledge this case
represents the15th incidenceof Idiopathic pulmonary vein
thrombosis. [5]
Since clinical presentation and physical examination
along with simple chest x-ray cannot Diagnose pulmonary
vein thrombosis, higher modalities of imaging are required.
Chest CT angiogram, pulmonary angiogram, Chest MRI and
transoesophageal ECHO. [4]
Treatment of Pulmonary vein thrombosis can be
achieved by antibiotic, anticoagulation or even
thrombectomy. Systemic anticoagulation usually is usually
initiated. most of previously reported cases were treated
with Warfarin, Dabigatran and rivaroxaban, interestingly
One case was reported to be treated successfully with
apixaban in 2021. [5]
IJISRT22OCT655 www.ijisrt.com 604
You might also like
- TM 11398Document592 pagesTM 11398krill.copco50% (2)
- Leg Support Calculation PDFDocument2 pagesLeg Support Calculation PDFSanjay MoreNo ratings yet
- Airport Literature StudyDocument15 pagesAirport Literature StudySoundar Rajan100% (2)
- PDF 64982 2 10 20210118Document8 pagesPDF 64982 2 10 20210118Marsya Yulinesia LoppiesNo ratings yet
- 45 1057Document5 pages45 1057Gabriela PinticanNo ratings yet
- Endomyocardial Biopsy Facilitates Diagnosis of Eosinophilic Granulomatosis With Polyangiitis (EGPA) : A Case ReportDocument5 pagesEndomyocardial Biopsy Facilitates Diagnosis of Eosinophilic Granulomatosis With Polyangiitis (EGPA) : A Case Reportjinmao1010No ratings yet
- A Rare Case of Cardiac Tamponade Due To TuberculosisDocument4 pagesA Rare Case of Cardiac Tamponade Due To TuberculosisDewinsNo ratings yet
- Endocard BartonDocument4 pagesEndocard BartonKrull TTTeamNo ratings yet
- 1 s2.0 S2213007121000289 MainDocument4 pages1 s2.0 S2213007121000289 MainHi GamingNo ratings yet
- A Review On Dengue and Treatments 13 23Document3 pagesA Review On Dengue and Treatments 13 23Karina Mega WNo ratings yet
- Clinical Presentation: by Dr. Raffiq AbbasDocument36 pagesClinical Presentation: by Dr. Raffiq AbbasKarthick UnleashNo ratings yet
- Insuficiencia Por EndocarditisDocument4 pagesInsuficiencia Por EndocarditisKatherin TorresNo ratings yet
- A Rare Cause of Endocarditis: Streptococcus PyogenesDocument3 pagesA Rare Cause of Endocarditis: Streptococcus PyogenesYusuf BrilliantNo ratings yet
- Infective EndocarditisDocument5 pagesInfective Endocarditismustafa malvi100% (1)
- A 54 Year Old Man With Migratory Pulmonary ConsoliDocument4 pagesA 54 Year Old Man With Migratory Pulmonary Consolilincolnbasilio1No ratings yet
- Vaccines 10 01286 PDFDocument7 pagesVaccines 10 01286 PDFAarathi raoNo ratings yet
- Systemic AmiloidosisDocument4 pagesSystemic AmiloidosisioannesturrisoricisNo ratings yet
- Bilateral Pulmonary Embolism Mimicking Acute Chest Syndrome in A Patient With Sickle Cell Disease: Acase Report and Review of The LiteratureDocument4 pagesBilateral Pulmonary Embolism Mimicking Acute Chest Syndrome in A Patient With Sickle Cell Disease: Acase Report and Review of The LiteratureIJAR JOURNALNo ratings yet
- 10.1007@s00296 008 0601 0Document3 pages10.1007@s00296 008 0601 0Kuber RawaNo ratings yet
- A Case of Recurrent Hemoptysis Caused by Pulmonary Actinomycosis Diagnosed Using Transbronchial Lung Biopsy After Bronchial Artery Embolism and A Brief Review of The LiteratureDocument8 pagesA Case of Recurrent Hemoptysis Caused by Pulmonary Actinomycosis Diagnosed Using Transbronchial Lung Biopsy After Bronchial Artery Embolism and A Brief Review of The LiteratureNiatazya Mumtaz SagitaNo ratings yet
- Cric2018 7237454Document4 pagesCric2018 7237454Muhammad Nur Ardhi LahabuNo ratings yet
- Cerebellar Stroke in A COVID-19 Infected Patient. A Case ReportDocument6 pagesCerebellar Stroke in A COVID-19 Infected Patient. A Case ReportMuhammad Reza FirdausNo ratings yet
- Catheter-Directed Thrombolysis of Iliocaval Thrombosis in Patients With COVID-19Document13 pagesCatheter-Directed Thrombolysis of Iliocaval Thrombosis in Patients With COVID-19oscarNo ratings yet
- TMP 155 BDocument7 pagesTMP 155 BFrontiersNo ratings yet
- 4Document16 pages4Ihsanul Ma'arifNo ratings yet
- Infected Pulmonary Infarction Case ReportDocument8 pagesInfected Pulmonary Infarction Case ReportSebastian Felipe Sierra UmañaNo ratings yet
- OMICS Journal of Radiology: Pulmonary Hypertension Secondary To Cardiac Hydatid Cyst EmbolismDocument2 pagesOMICS Journal of Radiology: Pulmonary Hypertension Secondary To Cardiac Hydatid Cyst EmbolismAgusNo ratings yet
- CID COVID - CASO CLINICODocument5 pagesCID COVID - CASO CLINICOAlejandra Marín OlavarríaNo ratings yet
- Spontaneous Mediastinal Hemorrhage in A Patient With End Stage Renal Disease: An Unusual Case of Uremic BleedingDocument5 pagesSpontaneous Mediastinal Hemorrhage in A Patient With End Stage Renal Disease: An Unusual Case of Uremic BleedingFoscamNo ratings yet
- BCR 2012 008352 PDFDocument4 pagesBCR 2012 008352 PDFaknbdgNo ratings yet
- 1 s2.0 S2666084921008056 MainDocument6 pages1 s2.0 S2666084921008056 Mainnina purnamasariNo ratings yet
- Unusual Course of Infective Endocarditis Acute RenDocument5 pagesUnusual Course of Infective Endocarditis Acute Renrr_eeyNo ratings yet
- MainDocument3 pagesMainGAlei LeoNo ratings yet
- Mca 8699Document3 pagesMca 8699mohdmuntazahmedNo ratings yet
- Revisi A Suspected COVID - 2Document11 pagesRevisi A Suspected COVID - 2Nicholas PranandaNo ratings yet
- Infectious Endocarditissecondary To Neisseria SPP in Patients With Cardiac Prostheses: Rare Entity and Difficult DiagnosisDocument6 pagesInfectious Endocarditissecondary To Neisseria SPP in Patients With Cardiac Prostheses: Rare Entity and Difficult DiagnosisIJAR JOURNALNo ratings yet
- Severe Pah With Renal FailureDocument7 pagesSevere Pah With Renal FailureBinod KumarNo ratings yet
- Jurnal Maju DR ArifDocument6 pagesJurnal Maju DR ArifRefta Hermawan Laksono SNo ratings yet
- Jurnal CovidDocument15 pagesJurnal CovidFitriani NurFadillahNo ratings yet
- St-Elevation Myocardialinfarction Inpatients With Covid-19 (About A Case Report and Review of The Litterature)Document5 pagesSt-Elevation Myocardialinfarction Inpatients With Covid-19 (About A Case Report and Review of The Litterature)IJAR JOURNALNo ratings yet
- Unusual Pattern of Arterial Macrothrombosis Causing Stroke in A Young Adult Recovered From COVID-19Document5 pagesUnusual Pattern of Arterial Macrothrombosis Causing Stroke in A Young Adult Recovered From COVID-19Audrey Beatrice ReyesNo ratings yet
- Clinical Examination: A Trigger But Not A Substitute For Hemodynamic EvaluationDocument3 pagesClinical Examination: A Trigger But Not A Substitute For Hemodynamic EvaluationGdfgdFdfdfNo ratings yet
- Management of Infective Endocarditis: Valve DiseaseDocument17 pagesManagement of Infective Endocarditis: Valve DiseaseLaura AmaliaNo ratings yet
- Cerebral Air Embolism - A Rare Complication of Computed Tomography Guided Lung BiopsyDocument4 pagesCerebral Air Embolism - A Rare Complication of Computed Tomography Guided Lung BiopsyBRNSS Publication Hub InfoNo ratings yet
- Tuberculous Pericarditis Leading To Cardiac Tamponade Importance of Screening Prior To ImmunosuppressionDocument3 pagesTuberculous Pericarditis Leading To Cardiac Tamponade Importance of Screening Prior To ImmunosuppressionLink BuiNo ratings yet
- m20 2003 PDFDocument14 pagesm20 2003 PDFTobias Ernesto Rivas GarciaNo ratings yet
- 30143-Article Text-56534-1-10-20220323Document5 pages30143-Article Text-56534-1-10-20220323Octavia SohanggrainyNo ratings yet
- Bradycardia As A Rare Sign of Pulmonary EmbolismDocument5 pagesBradycardia As A Rare Sign of Pulmonary Embolismh.jaradNo ratings yet
- Pi Is 0272638621007721Document12 pagesPi Is 0272638621007721Carlos QuirogaNo ratings yet
- SVT and DengueDocument4 pagesSVT and Denguefrengki prasNo ratings yet
- Emp2 12098Document4 pagesEmp2 12098Miva MaviniNo ratings yet
- Endocarditis Caused by Unusual Streptococcus Species (Streptococcus Pluranimalium)Document4 pagesEndocarditis Caused by Unusual Streptococcus Species (Streptococcus Pluranimalium)Soria M JorgeNo ratings yet
- Laco 2008Document5 pagesLaco 2008Cruz Castro DanielaNo ratings yet
- Unilateral Common Carotid Artery Dissection in A PDocument3 pagesUnilateral Common Carotid Artery Dissection in A PidhebeatrickNo ratings yet
- Acute Respiratory Distress Syndrome: David SweetDocument204 pagesAcute Respiratory Distress Syndrome: David SweetJelenaNo ratings yet
- Left Hemothorax: Unusual Manifestation of Aortic DissectionDocument5 pagesLeft Hemothorax: Unusual Manifestation of Aortic DissectionIJAR JOURNALNo ratings yet
- 392 2009 Article 69Document11 pages392 2009 Article 69PutraChamplenxNo ratings yet
- COVID-19 Update: Covid-19-Associated Coagulopathy: Richard C. BeckerDocument14 pagesCOVID-19 Update: Covid-19-Associated Coagulopathy: Richard C. Beckersumenep nursalamNo ratings yet
- Postgradmedjournal - Purulent PericarditisDocument5 pagesPostgradmedjournal - Purulent Pericarditisfretzie enguitoNo ratings yet
- 2020 Article 2134Document14 pages2020 Article 2134Maysa HasanahNo ratings yet
- Bilateral Massive Pulmonary Embolism Secondary To Decompression Sickness: A Case ReportDocument4 pagesBilateral Massive Pulmonary Embolism Secondary To Decompression Sickness: A Case ReportPatricio Toledo FuenzalidaNo ratings yet
- Anti-Neutrophil Cytoplasmic Antibody (ANCA) Associated VasculitisFrom EverandAnti-Neutrophil Cytoplasmic Antibody (ANCA) Associated VasculitisRenato Alberto SinicoNo ratings yet
- Inflammatory Diseases of Blood VesselsFrom EverandInflammatory Diseases of Blood VesselsGary S. HoffmanNo ratings yet
- Analysis of Opaque, Peel-Off and Flex Rejects in the Electro Plating Process Using the Six Sigma Dmaic MethodDocument18 pagesAnalysis of Opaque, Peel-Off and Flex Rejects in the Electro Plating Process Using the Six Sigma Dmaic MethodInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Study to Effect of Reminiscence Therapy on Psychological Well-Being among Elderly Residing in Selected Old Age HomeDocument5 pagesA Study to Effect of Reminiscence Therapy on Psychological Well-Being among Elderly Residing in Selected Old Age HomeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Application of Project Management using CPM (Critical Path Method) and Pert (Project Evaluation and Review Technique) in the Nava House Bekasi Cluster Housing Development ProjectDocument12 pagesApplication of Project Management using CPM (Critical Path Method) and Pert (Project Evaluation and Review Technique) in the Nava House Bekasi Cluster Housing Development ProjectInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Comprehensive Review on the Therapeutic Potential of PectinDocument6 pagesA Comprehensive Review on the Therapeutic Potential of PectinInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Application of the Economic Order Quantity (EOQ) Method on the Supply of Chemical Materials in the Laboratory of PT. Fajar Surya Wisesa TbkDocument15 pagesApplication of the Economic Order Quantity (EOQ) Method on the Supply of Chemical Materials in the Laboratory of PT. Fajar Surya Wisesa TbkInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Rare Complication: Cardiac Arrest and Pulmonary Embolism in Polyarteritis NodosaDocument5 pagesA Rare Complication: Cardiac Arrest and Pulmonary Embolism in Polyarteritis NodosaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Impact of Integrated Border Security System on Human Trafficking in Bangladesh: The Mediating Effect of the Use of Advanced TechnologyDocument12 pagesThe Impact of Integrated Border Security System on Human Trafficking in Bangladesh: The Mediating Effect of the Use of Advanced TechnologyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Quality Control to Reduce Appearance Defects at PT. Musical InstrumentDocument11 pagesQuality Control to Reduce Appearance Defects at PT. Musical InstrumentInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Forecasting PM10 Concentrations Using Artificial Neural Network in Imphal CityDocument10 pagesForecasting PM10 Concentrations Using Artificial Neural Network in Imphal CityInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Analysis of Carton Packaging Quality Control Using Statistical Quality Control Methods at PT XYZDocument10 pagesAnalysis of Carton Packaging Quality Control Using Statistical Quality Control Methods at PT XYZInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Quizlet's Usefulness for Vocabulary Learning: Perceptions of High-Level and Low-Level Chinese College EFL LearnersDocument5 pagesQuizlet's Usefulness for Vocabulary Learning: Perceptions of High-Level and Low-Level Chinese College EFL LearnersInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Enhancing Estimating the Charge Level in Electric Vehicles: Leveraging Force Fluctuation and Regenerative Braking DataDocument6 pagesEnhancing Estimating the Charge Level in Electric Vehicles: Leveraging Force Fluctuation and Regenerative Braking DataInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Entrepreneurial Adult Education as a Catalyst for Youth Employability in Disadvantaged AreasDocument9 pagesEntrepreneurial Adult Education as a Catalyst for Youth Employability in Disadvantaged AreasInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- The Role of Leadership Training in Developing Effective Police SupervisorsDocument17 pagesThe Role of Leadership Training in Developing Effective Police SupervisorsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Health Care - An Android Application Implementation and Analyzing user Experience Using PythonDocument7 pagesHealth Care - An Android Application Implementation and Analyzing user Experience Using PythonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Intrusion Detection System with Ensemble Machine Learning Approaches using VotingClassifierDocument4 pagesIntrusion Detection System with Ensemble Machine Learning Approaches using VotingClassifierInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Synthetic and Natural Vitamin C Modulation of Leaded Paint-Induced Nephrotoxicity of Automobile Painters in Ile-Ife, Nigeria.Document21 pagesSynthetic and Natural Vitamin C Modulation of Leaded Paint-Induced Nephrotoxicity of Automobile Painters in Ile-Ife, Nigeria.International Journal of Innovative Science and Research TechnologyNo ratings yet
- Visitor Perception Related to the Quality of Service in Todo Tourism VillageDocument10 pagesVisitor Perception Related to the Quality of Service in Todo Tourism VillageInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Gravity Investigations Applied to the Geological Framework Study of the Mambasa Territory in Democratic Republic of CongoDocument9 pagesGravity Investigations Applied to the Geological Framework Study of the Mambasa Territory in Democratic Republic of CongoInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Developing Digital Fluency in Early Education: Narratives of Elementary School TeachersDocument11 pagesDeveloping Digital Fluency in Early Education: Narratives of Elementary School TeachersInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A New Model of Rating to Evaluate Start-ups in Emerging Indian MarketDocument7 pagesA New Model of Rating to Evaluate Start-ups in Emerging Indian MarketInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- A Proof of Concept Using BLE to Optimize Patients Turnaround Time (PTAT) in Health CareDocument14 pagesA Proof of Concept Using BLE to Optimize Patients Turnaround Time (PTAT) in Health CareInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Financial Prudence as Determinant of Employees’ Interest in Graduate StudyDocument13 pagesFinancial Prudence as Determinant of Employees’ Interest in Graduate StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Design and Implementation of Software-Defined ReceiverDocument8 pagesDesign and Implementation of Software-Defined ReceiverInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Optimizing Bio-Implant Materials for Femur Bone Replacement:A Multi-Criteria Analysis and Finite Element StudyDocument5 pagesOptimizing Bio-Implant Materials for Femur Bone Replacement:A Multi-Criteria Analysis and Finite Element StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Crop Monitoring System with Water Moisture Levels Using ControllerDocument8 pagesCrop Monitoring System with Water Moisture Levels Using ControllerInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Inclusive Leadership in the South African Police Service (SAPS)Document26 pagesInclusive Leadership in the South African Police Service (SAPS)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Naturopathic Approaches to Relieving Constipation: Effective Natural Treatments and TherapiesDocument9 pagesNaturopathic Approaches to Relieving Constipation: Effective Natural Treatments and TherapiesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Fahfi/Mochaina Illegal Gambling Activities and its Average Turnover within Limpopo ProvinceDocument8 pagesFahfi/Mochaina Illegal Gambling Activities and its Average Turnover within Limpopo ProvinceInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Year Wise Analysis and Prediction of Gold RatesDocument8 pagesYear Wise Analysis and Prediction of Gold RatesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Quatre Agro Enterprise Private LimitedDocument25 pagesQuatre Agro Enterprise Private Limitedp23pallavNo ratings yet
- Amina Ahmed Benchmark Solution Oet Writing Task Practice With CorretionDocument1 pageAmina Ahmed Benchmark Solution Oet Writing Task Practice With CorretionFïzã PäthäñNo ratings yet
- CR Unit 1 &11 (Part A &B)Document12 pagesCR Unit 1 &11 (Part A &B)durai muruganNo ratings yet
- BEL PE Question Papers For ECE With Answers - 6 Knowledge AddaDocument14 pagesBEL PE Question Papers For ECE With Answers - 6 Knowledge AddaVishwanand ThombareNo ratings yet
- Arthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832Document318 pagesArthur Lumley Davi̇ds-Sultan Ii. Mahmuta-1832cengizozakinciNo ratings yet
- Water Stability - What Does It Mean and How Do You Measure It ?Document9 pagesWater Stability - What Does It Mean and How Do You Measure It ?Richard EscueNo ratings yet
- Maharastra State Board of Technical Education MumbaiDocument23 pagesMaharastra State Board of Technical Education MumbaiMayuresh PadekarNo ratings yet
- Abb Reg615 Ansi Appl 859072 EndDocument124 pagesAbb Reg615 Ansi Appl 859072 EndjppreciadomNo ratings yet
- Understanding Your Electricity Bill in PakistanDocument13 pagesUnderstanding Your Electricity Bill in PakistanGhayas Ud-din DarNo ratings yet
- Module 1 What Is Geography and TourismDocument22 pagesModule 1 What Is Geography and TourismLeanne Abegail EstabilloNo ratings yet
- An Overview of Honey: Its Composition, Nutritional and Functional PropertiesDocument5 pagesAn Overview of Honey: Its Composition, Nutritional and Functional PropertiesSandeep SinghNo ratings yet
- Grammar 04 18Document5 pagesGrammar 04 18zsuzsi_harangoz2218No ratings yet
- Costing By-Product and Joint ProductsDocument36 pagesCosting By-Product and Joint ProductseltantiNo ratings yet
- Unit VII Lecture NotesDocument3 pagesUnit VII Lecture NotesSteve Sullivan100% (2)
- Spider-81 Hardware Spec 7.7Document7 pagesSpider-81 Hardware Spec 7.7KonradNo ratings yet
- NASA NOAA Earth Sciences Letter To TrumpDocument6 pagesNASA NOAA Earth Sciences Letter To TrumpMelissa Meehan BaldwinNo ratings yet
- Rotorcraft Aerodynamics: Muhammad Abdullah Tahir 180101034 Aero 17 (A)Document15 pagesRotorcraft Aerodynamics: Muhammad Abdullah Tahir 180101034 Aero 17 (A)Abdullah CheemaNo ratings yet
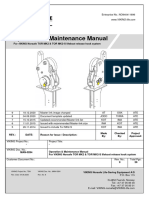
- SOM016 - Hook Release System For Life Boats. Norsafe TOR mk2.Document20 pagesSOM016 - Hook Release System For Life Boats. Norsafe TOR mk2.arfaoui salimNo ratings yet
- EQUILIBRIUMDocument1 pageEQUILIBRIUMMohammed IliasNo ratings yet
- COMPRE - MODULE 4 (Pharmacology and Toxicology) : Attempt ReviewDocument40 pagesCOMPRE - MODULE 4 (Pharmacology and Toxicology) : Attempt ReviewLance RafaelNo ratings yet
- Surveillance, Torture and Contr - Rosanne Marie SchneiderDocument135 pagesSurveillance, Torture and Contr - Rosanne Marie SchneiderMagic MikeNo ratings yet
- Credit Card Fraud Detection Using Improved Deep Learning ModelsDocument22 pagesCredit Card Fraud Detection Using Improved Deep Learning ModelsrauhNo ratings yet
- Hillfoot Data Sheets V5 1Document4 pagesHillfoot Data Sheets V5 1Kristijan IlicNo ratings yet
- 12 2f17 Vegetarian Argumentative EssayDocument7 pages12 2f17 Vegetarian Argumentative Essayapi-413258549No ratings yet
- Process SequenceDocument2 pagesProcess SequenceUmesh SakhareliyaNo ratings yet
- Jayvee Dime,,,,project in Physics Light and SoundDocument25 pagesJayvee Dime,,,,project in Physics Light and SoundJayvee DimeNo ratings yet
- 6 Landforms - SCIENCEDocument9 pages6 Landforms - SCIENCEArianne RealNo ratings yet