Professional Documents
Culture Documents
C1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel Method
C1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel Method
Uploaded by
DIVINA KYLE YGOOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
C1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel Method
C1 IH Lab L3 ABO Forward Reverse Typing Manual and Gel Method
Uploaded by
DIVINA KYLE YGOCopyright:
Available Formats
LESSON 3: ABO FORWARD/REVERSE TYPING (Manual and Gel Method)
OUTLINE ABO ANTIGEN − They are SALINE AGGLUTININS with OPTIMAL
I. INTRODUCTION − Antigens detected in blood bank testing, including REACTIVITY at 4°C.
A. ABO Antigen ABO antigens, are located on the surface of the red − As previously described,
B. ABO ANTIBODIES o ABO antigens are present on the surface of red
blood cell.
II. FORWARD TYPING
o ABO is known as carbohydrates cells, (detected in forward typing)
A. SLIDE METHOD; B.TUBE METHOD
III. REVERSE TYPING o Chromosome 9 gene—encodes for the enzyme. o Antibodies are found in plasma or serum.
IV. BEDSIDE BLOOD TYPING These enzymes place the carbohydrates for A (detected in reverse typing)
V. ABO FORWARD-BACKWARD AND RH-TYPING USING GEL and B to the red cells. If none (no − ROUTINE TESTING for antigens and antibodies is
CARD TECHNOLOGY carbohydrate)—O group. performed as a forward and reverse grouping.
A. ABO DISCREPANCIES
B. TECHNICAL ERRORS
C. RESOLVING ABO DISCREPANCIES
FORWARD TYPING (DIRECT)
− Forward typing is done using KNOWN ANTISERA to
INTRODUCTION detect ABO antigens present on the patient’s red
− The MAJOR BLOOD GROUP SYSTEMS are the primary cells.
focus of blood banking and transfusion therapy. This − ABO antigens are also present on lymphocytes, o Antisera has antibodies that uses manufactured
includes the ABO system, which is the most thrombocytes, organs, endothelial cells, and polyclonal Ab (more sensitive to Ag as it can
important of all blood groups in both transfusion and epithelial cell. react with different types of epitopes) or
transplant medicine. o ABO is tested in transplant EXCEPT in corneal monoclonal Ab (specific epitope only: mostly
− It is the only blood group system in which individuals transplant because it has low antigen weak reaction)
ALREADY HAVE ANTIBODIES in their serum to expression. − There are two methods through which this procedure
antigens that are absent from their red blood cells − Antigens of the ABO system are well-developed in is performed: Slide (rapid and often used in
(RBCs) without any prior exposure to RBCs through ADULTS. They are detectable at 5 to 6 weeks of emergencies; also used in screening for blood
transfusion or pregnancy (and transplantation). gestation. transfusion) and Tube method (more sensitive & used
− however, NEWBORNS demonstrate weaker antigens, more often; uses red cell suspension).
− Due to the presence of these antibodies, transfusion but ABO antigens are fully developed by two to four
of an incompatible ABO type may result in immediate years of age. PRINCIPLE
lysis of donor RBCs. Even today, transfusion of the o ABO antigen or Forward is tested rather than − Red cells from the specimen are reacted with reagent
wrong ABO group remains a cause of death in reverse in children less than2-4y.o. ANTISERA (anti-A and anti-B). AGGLUTINATION OF
hemolytic transfusion reaction fatalities. RED CELLS indicates presence of corresponding
ABO ANTIBODIES antigen (agglutinogen) on red cells.
− For this reason, ABO forward and reverse typing is − A person normally produce antibodies directed
necessary. Direct or forward typing is DONE FIRST, against the A and/or B antigen(s) that is absent from SPECIMEN :
but the result must be correlated with the their erythrocytes. − Capillary blood from finger prick (often for
interpretation of the serum grouping to ensure that − These antibodies have been described as NATURALLY emergency cases), or venous blood collected in EDTA
both point to the same ABO group. OCCURRING because they are produced without any anticoagulant.
o Correlate forward with reverse (must be same) exposure to RBCs. − The reagent MANUFACTURER’S PACKAGE INSERT
o Ex. For Blood Type A: − Mostly these antibodies are IgM. must be consulted to determine specific specimen
In forward: reacts in Anti-A; − ABO antibodies are typically ISOAGGLUTININS. requirements.
In reverse: reacts with Anti-B o Reacts on same species (human to human)
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 1
LESSON 3: ABO FORWARD/REVERSE TYPING (MANUAL AND GEL METHOD)
o Generally, CLOTTED OR ANTICOAGULATED 1. A clean and dry glass slide is divided into two 5. By tilting the slide backwards and forwards (in
BLOOD SAMPLES may be used for ABO testing sections with a glass marking pencil. The sections rotating motion) examine for agglutination after
(in reverse). are labeled as anti-A, anti-B, and Anti-D to identify exactly two minutes.
o The RED CELLS may be suspended in the antisera (see Figure 1)
autologous serum, plasma, or saline, or they
may be washed and resuspended in saline.
REAGENT :
Anti-A= Blue (Asul)
Anti B= Yellow (Banana) 6. Result:
Anti-D= Clear1 POSITIVE (+): Little clumps of red cells are seen
floating in a clear liquid.
A. SLIDE METHOD NEGATIVE (–): Red cells are floating
2. Using Pasteur pipette/ Applicator stick, place one
− Slide test is quick and needs only simple equipment. homogeneously in a uniform suspension.
drop of the WHOLE BLOOD into the Sections that
− It can be used in blood donation camps and in case of are labeled. (see Figure 1)
an emergency.
− However, it is NOT RECOMMENDED as a routine test
in blood banks since weakly reactive antigens on cells
on forward grouping and low titer anti-A and anti-B
on reverse grouping may be MISSED.
MATERIALS
Glass slide Gum label Table 1: Grading of Reaction
Applicator sticks Marking pen 3. Place one drop of anti-A serum, one drop of anti-B Record Description of Reaction
Pasteur pipette 70% Alcohol serum, and one drop of Anti-D in the center of the Macroscopic Readings**
Cotton EDTA corresponding section of the slide. (At least 1 is to +4 One solid agglutinate;
PPE Syringe (23 or 21 G) 1 ratio). background is clear.
Blood lancet +3 Several large agglutinates;
background is clear
PROCEDURE +2 Medium sized agglutinates;
background is clear
1 Many small agglutinates;
background is turbid
Microscopic Readings***
4. Mix antiserum and blood by using a separate stick W Barely visible agglutination;
or a separate corner of a slide for each section over turbid background
Figure 1. Slide labelled with Anti-A, Anti-B and Anti-D an area about 1 inch in diameter. (See Figure 2) NEG No agglutination or hemolysis of red cells.
Cells float freely
EXAMPLE (picture):
Agglutination 4+;
Yellow= Blood Type B
Figure 2: Mixed slide with blood and Anti-Sera Note:
Ideally, the reaction must be 4+ or 3+
Negative is confirmed under microscope.
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 2
LESSON 3: ABO FORWARD/REVERSE TYPING (MANUAL AND GEL METHOD)
B. TUBE METHOD 8. Remove each tube and EXAMINE FOR HEMOLYSIS.
PRINCIPLE: o Usually, after centrifuge, “tinataktak ‘yung
− Because of the dire clinical consequences associated bottom” to disturb the cell. If it is true
agglutination: “kahit anong taktak, hindi
with ABO incompatibilities, ABO typing and ABO
mawawala ‘yung aggltsn”
compatibility testing remain the foundation of
pretransfusion testing and an important component 9. Using an AGGLUTINATION VIEWER, gently
of typing before transplantation. resuspend each cell button, and examine for
agglutination.
10. Grade each reaction and record the results.
SPECIMEN:
− Capillary blood from finger prick, or venous blood 4. To each of these tubes, add one drop of the
collected in EDTA anticoagulant. corresponding antisera.
− The REAGENT MANUFACTURER’S PACKAGE insert NOTE: Use a free floating drop. Do
must be consulted to determine specific specimen not touch the dropper to the side of
requirements. the tube. Always add antisera
o Generally, clotted or anticoagulated blood BEFORE cells.
samples may be used for ABO testing.
o The red cells may be suspended in autologous
serum, plasma, or saline, or they may be
washed and resuspended in saline.
REAGENT:
5. Using a transfer pipet, add one drop of the well-
Anti-A= Blue
mixed 3% cell suspension to each of these three
Anti B= Yellow
tubes.
Anti-D= Clear
NOTE: Use a free floating drop. Do
Patients Red cell suspension
not touch the pipet to the side of the
tube.
PROCEDURE
1. Prepare a 3% suspension of patient’s red cells.
(Includes RC washing)
2. Label three small test tubes with the patient’s name 6. Gently mix all tubes.
and identification number and the step 3. 7. SEROFUGE all three test tubes for 15 seconds.
3. Each of these tubes should then be labeled as
follows: Figure 3.
o First tube: “Anti-A” On the left side, tube with anti A and a drop of 3% red
o Second tube: “Anti-B” cell suspension
o Third tube: “Anti-D” On the right, tube with anti B and a drop of 3% red cell
NOTE: Labeling should be done with suspension.
care since CLERICAL ERRORS are the NOTE: One more tube will be needed for Anti-D.
most frequent errors in the blood
bank.
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 3
LESSON 3: ABO FORWARD/REVERSE TYPING (MANUAL AND GEL METHOD)
BEDSIDE BLOOD TYPING REVERSE TYPING (INDIRECT)
(From Cluster 2’s Trans—R.V.Laurezo) − Reverse blood grouping is a procedure another way
Test card is already embedded with anti-sera. confirm ABO blood group based on the presence or
PROCEDURE absence of anti-A and anti-B in serum using known A
and B red cells. (Usually, known A1 and B cells: can be
manufactured/ manually made in laboratory)
− It is CROSS CHECK for forward typing.
− Performing both forward and reverse grouping
provides a check for accuracy.
− Because of the LACK OF SYNTHESIZED
IMMUNOGLOBULINS, anti-A and Anti-B in newborns
and very young infants, this procedure is NOT
PERFORMED on infants below 4 months of age.
− Reverse grouping is synonymous with backward
typing, indirect typing and serum typing.
INTERPRETATION OF RESULT: PRINCIPLE:
− Because of the dire clinical consequences associated
1. Agglutination of tested red cells and either hemolysis
with ABO incompatibilities, ABO typing and ABO
or agglutination in tests with serum or plasma
compatibility testing remain the foundation of
constitute POSITIVE TEST RESULTS.
pretransfusion testing and an important component
2. A smooth cell suspension after resuspension of the cell
of typing before transplantation.
button is a NEGATIVE TEST RESULT. (Follow the
grading in table 1)
3. Interpretation of serum or plasma and red cell tests SPECIMEN:
for ABO is given in the table 5. − Patients plasma/serum from EDTA tube or red top.
4. Any discrepancy between the results of the tests with − The REAGENT MANUFACTURER’S PACKAGE INSERT
serum or plasma and red cells should be resolved must be consulted to determine specific specimen
before an interpretation is recorded for the patient’s requirements.
or donor’s ABO group. Step 1. Place one drop of isotonic saline solution (NSS) o Generally, clotted or anticoagulated blood
5. Mixed-field agglutination should be investigated for on each reaction field and auto-control field. samples may be used for ABO testing.
possible cause. (Mix of agglutinated and o The RED CELLS may be suspended in
unagglutinated; often in gel method) Step 2. Add one drop of the recipient’s blood to each autologous serum, plasma, or saline, or they
field in the upper panel of the card and one drop of may be washed and resuspended in saline.
NOTE: donor blood to each field in the lower panel of the card.
All reagents must be used in accordance with the REAGENT:
manufacturer’s instructions. Step 3. Stir each field with an applicator stick for − Unkown Sera/serum of patient
approx. 30 seconds. The reagents must dissolve − Known A and B (2-5% Red Cell Suspension)
POSITIVE REACTIONS characteristically show 3+ to
4+ agglutination by reagent ABO antibodies; completely. − Normal Saline Solution (0.85-0.95%)
reactions between test serum and reagent red cells
Step 4. Gently rock the card back and forth for approx. PROCEDURE
are often weaker.
30 to 60 seconds, then check each field for 1. Prepare 3% Red cell suspension of A and B cells
The serum tests may be incubated at room
agglutination. (After 3 washing)
temperature for 5 to 15 minutes to enhance weak
Step 5. Dry the reaction mixtures and cover with self-
reactions (used in weak rx on reverse typing).
adhesive film before filling the card.
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 4
LESSON 3: ABO FORWARD/REVERSE TYPING (MANUAL AND GEL METHOD)
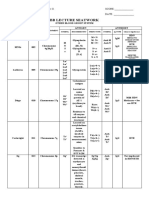
Table 5. Routine ABO Grouping
Reaction Reaction of Interpre Prevalence
of Red Serum with - tation (%) in US
Cells Reagent Population
with Red Cells
Antisera (Serum
(Red Cell Grouping)
Grouping)
2. Label 2 Wasserman test tubes as A and B (see figure
ABO Groups
European
Ethnicity
Ethnicity
A1 Cells
O Cells
B Cells
Anti-A
Anti-B
African
3)
3. Follow the table below.
Table 3. Guide in the interpretation of Backward Blood o o + + o O 45 49
Groupings
+ o o + o A 40 27
Patients Known 3% Red Known 3% Red cell
serum type cell suspension suspension of B o + + o o B 11 20
of A cells cells + + o o o AB 4 4
A o + o o + + + Bombay Rare Rare
B + o
AB o o No reaction with O cells since they do not produce
O + + anti-H; all has H precursor (O has the greatest H);
Table 2
Type A has H cells, “natatbunan lang ng A
CONTENT TUBE 1 (A) TUBE 2 (B) cells”but can still be detected
Unkown serum/ serum 2 drops 2 drops Table 4. Reverse Typing Interpretation BOMBAY: has no A, B and H antigen—sometimes
of patient Blood INTERPRETATION is masks as O cells (False O cells); but since it has
Known 3% Red cell 1 drop - type no/ weak H antigen: it produces Anti-H causing
Suspension of A cells A Agglutination in B cells with no agglutination reaction with O cells that is filled with H antigen.
Known 3% Red cell - 1 drop in A cells demonstrate that the serum do (Simply, it produces antibodies against O cells)
Suspension of B cells have antibodies for B cells, thus indication
that the individual is Blood type A.
B Agglutination in A cells with no agglutination
4.Cover the tubes with Nescofilm. in B cells demonstrate that the serum do ABO FORWARD-BACKWARD AND RH-TYPING USING
5.Mix gently and centrifuge all the tubes for 15 have antibodies for A cells, thus indication GEL CARD TECHNOLOGY
seconds at 3,400 rpm that the individual is Blood type B. − The GEL TECHNOLOGY METHOD was developed by
6. Gently dislodge the cell bottom and examine for AB Agglutination is not present in both A and B DR. YVES LAPIERRE in 1985.
hemolysis or agglutination. cells, demonstrate that the serum do not − This technology uses DEXTRAN ACRYLAMIDE GEL
have antibodies for either A or B cells, thus particles to trap agglutinated red cells. This method
indicating that the individual is Blood type was developed to standardized traditional tube
AB. testing methods.
O Agglutination is present in both A and B cells, − Because of this new technology, it was found that the
demonstrate that the serum do have gel particles are IDEAL MATERIAL FOR TRAPPING THE
antibodies for both A and B cells, thus AGGLUTINATE.
indicating that the individual is Blood Type
O. − Compared with the traditional tube testing, the GEL
TEST provides a more stable and well defined
endpoints of the agglutination reaction.
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 5
LESSON 3: ABO FORWARD/REVERSE TYPING (MANUAL AND GEL METHOD)
− It can be used to PERFORM DIFFERENT TESTS such as: PROCEDURES Figure 2: Sample grade reaction
o ABO forward and reverse grouping, A. PREPARATION OF RED CELL SUSPENSION Negative 0 Well-defined pellet of non-
o Rh typing, agglutinated red blood cells at
1. Prepare tube containing 0.1 ml washed packed RBC
o Direct antiglobulin test, the bottom of the gel column and
and 4.9 mL NSS. This will produce a 2% RED CELL
o antibody screening,
SUSPENSION no visible agglutinated cells in the
o identificaton of antibodies, and rest of gel column.
2.Transfer 2.5 mL of 2% red cell suspension to a separate
o compatability testing. Barely visible small-sized clumps
tube containing 2.5 mL NSS. This dilution will produce
1% RED CELL SUSPENSION. w+ of agglutinated cells in the lower
− For FORWARD ABO BLOOD GROUPINGS, card has part of the gel column and
3. Set this cell suspension aside.
gels that contain anti-A and anti-B and Anti-AB. a pellet of unagglutinated cells at
− MICROTUBES WITH BUFFERED GEL are used for ABO the bottom.
B. ABO FORWARD AND RH TYPING USING THE GEL
reverse grouping. 1+ Some small-sized clumps of
− The Rh typing card contain anti-D, anti-C, anti-E, anti- CARD
agglutinated cells most
c, anti-e and a control. (reactions in the gel method 1. Flip the cover foil
frequently in the lower half of the
are graded from +1 to +4, including mixed filled) 2. Dispense 50 uL of 1% red cell suspension using an
gel column.
− automatic pipettor on each well labeled A, B, and D
A small pellet may also be
of the gel card. Avoid hitting the gel as you deliver the Positive observed at the bottom of the gel
red cells.
column.
3. Cover the well with the foil again. You may secure the
2+ Small or medium-sized clumps of
cover using a Nescofilm.
4. Centrifuge for 15 seconds at 3,400 rpm using a specially agglutinated cells throughout the
gel column.
designed gel card centrifuge.
5. Observe and interpret the results A few unagglutinated cells may
be visible at the bottom of the gel
column.
C. ABO BACKWARD TYPING USING THE GEL CARD
3+ Medium-sized clumps of
1. Flip the cover foil agglutinated cells in the upper
2. Dispense 50 uL of the unknown plasma sample using half of the gel column.
an automatic pipettor on each well labeled CTL, A1, 4+ A well-defined band of
and B of the gel card. Avoid hitting the gel as you
agglutinated red blood cells in
deliver you your sample.
the top part gel column.
3. Cover the well with the foil again. You may secure the
MATERIALS/EQUIPMENT A few agglutinated cells may be
cover using a Nescofilm.
Commercially available gel Gum label (optional) visible below the band.
4. Centrifuge for 15 seconds at 3,400 rpm using a specially
card for ABO forward and Nescofilm Mixed-field. A band of red blood
designed gel card centrifuge.
backward typing Marking pen 5. Observe and interpret the result. cells at the top part of the gel or
mf dispersed throughout the gel
Gloves Test tube rack
column, and
Centrifuge Automatic pipette
a pellet in the gel bottom as a
Wasserman test tubes Micropipettor
NEGATIVE RESULT.
Hemolysis in the microtube with
REAGENT/ SAMPLES
the very few or no red blood cells
− Normal saline solution in a wash bottle (85%-95%)
H in the gel column.
− ANTICOAGULATED BLOOD from a patient: Centrifuge
Report if hemolysis is present in
for 5 minutes at 3,400 rpm to separate the plasma:
the microtube but not in the
a. Wash the packed red blood cells
sample.
b. Set aside the plasma
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 6
LESSON 3: ABO FORWARD/REVERSE TYPING (MANUAL AND GEL METHOD)
transplantation, DISCREPANCY GROUPS
Acquired B antigen, (weak rx with GROUP 1: Ab: Weak Ab, Missing Ab
Anti-B in forward typing; this is GROUP 2: Ag: Weak Ag, Missing Ag
only acquired as they are usually GROUP 3: Plasma proteins: Rouleaux formation
Type A) Miscellaneous: Mixed
B (A) Phenomenon,
Out of group transfusion. Note:
Mixed-filled Recent Transfusion, Discrepancy usually has weak reaction
cell reactivity Transplantation, (can be Always check the history of patient
transplant of hematopoietic cell or **Ex. In ABO subgroup: A reaction with forward
bone marrow that may produce Anti-A, and 1+ rx in A1 cell in reverse: Usually, it is A2
different cell) subgroup because it has few Anti-A1 Ab.
ABO DISCREPANCIES Fetomaternal Hemorrhage,
− When a discrepancy is encountered, the DISCREPANT Twin or dispermic/chimerism EXAMPLE: Evaluate then Solution
RESULTS must be recorded, but interpretation of the o Chimerism: (there may be
ABO group must be delayed until the discrepancy has mixing of cells between
been resolved. the twin who are alive and Observe for the weak rx
− If the SPECIMEN IS FROM A DONOR UNIT, the unit deceased: creating 2 Evaluate:
must be quarantined and cannot be released for populations of cells; or o Anti-A: 4+ (Type A); Anti-B: 1+ (weak rx)
transfusion. there may be an exchange o Anti-A,B: 4+ ✔ (strong rx since it has rx with
− When an ABO discrepancy is identified in a patient, of red cells between the Anti-A)
it may be necessary to transfuse group O red cells twins, and antibodies are
pending an investigation. It is important to obtain a o A1 cells: 0 ✔ (No rx since it has no Ab against
not being produced) A)
sufficient pretransfusion blood sample from the o Dispermic- an egg cell is
patient to complete any additional studies that may o Anti-B: 4+ ✔ (Has Ab against B cells)
fertilized by 2 sperm (very
be required. Observation:
rare)
o Anti-A Individual with few amount of
Weak/Missing Group 1 discrepancy
Red Cell Testing Problems and Problems with Serum Antigen B. This may be ACQUIRED B
Serum Age related (less than 4 to 6
or Plasma Testing o Check px medical history
reactivty months old, elderly),
Category Causes Solution:
ABO subgroup**, o You may mix the px cell and serum= If it has
Weak/ ABO Subgroup, Hypogammaglobulinemia,
Missing Red Leukemia, no rx: Confirmed A cellls (since A cells must
(decreased IgG) not react on its own plasma)
cell Activity transfusion, transplantation o Then, to confirm Anti-B, use polyclonal
intrauterine transfusion, Extra serum Cold autoantibody, antisera= If it has no rx: ABO discrepancy:
transplantation, reactivity cold alloantibody, (previous Possibly it is Acquired B
excessive soluble blood group exposure, transfusion,
substance (usually in underlying transplantation, pregnancy)
pathological conditions; found serum antibody to reagent
excessively in plasma; it may mask constituent,
the red cell or it may interfere Excess serum proteins, (may be
with antisera causing weak rx) due to improperly washed red cell)
Extra red cell Autoagglutinins/excess protein transfusion of plasma proteins,
reactivity coating red cells, transplantation,
Unwashed red cells (plasma Infusion of intravenous immune
proteins), globulins
antibodies to patient’s serum to
reagent constituent,
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 7
LESSON 3: ABO FORWARD/REVERSE TYPING (MANUAL AND GEL METHOD)
TECHNICAL ERRORS REFERENCES
Technical problems with a sample or during testing can also Notes from the discussion of Ms. Janielle M. Fajardo, RMT,
lead to problems in ABO grouping, including: MLS (ACSPi)
1. Specimen mix up. Cavite State University Immunohematology Laboratory
2. Too heavy or too light red cell suspensions. handouts: Lesson 3
3. Failure to add reagents. -Cardona, C.C, Martin , G.L, and Garcia- Meim, R. (2016)
4. Missed observation of hemolysis. Laboratory Manual in Blood Banking 2nd Edition
5. Failure to follow the manufacturer’s Kung M. K., Grossman B.,J, Hilyer, C.D., Westhoff (2014)
instructions. Technical Manual 18th Edition
Whitlock, S. A., Immunohematology for Medical
6. Under- or overcentrifugation of tests.
Laboratory Technicians 2010
7. Incorrect interpretation or recording of test
results.
RESOLVING ABO DISCREPANCIES
1. Repeat the test with the same sample
2. Incubating red cells at 4°C, (if the weak rx is for
Ab) using enzyme-treated red cells, and
conducting adsorption and elution studies.
3. RETESTED using different monoclonal and
human polyclonal reagents. (In forward)
4. To resolve an ABO discrepancy caused by an
anti-A1 in a group A individual, red cells should
be tested with DOLICHOS BIFLORUS LECTIN,
which agglutinates group A1 but not A2 and
weaker A subgroups.
Reaction occurs: A1 group
No reaction: A2 group
5. Testing at 37°C without centrifugation and
cold autoadsorption
6. Saline replacement or saline dilution can be
used to distinguish rouleaux from
agglutination and identify ABO antibodies.
Group 3 Discrepancy; true
agglutination: even after washing,
aggltn remains
Rouleaux: after NSS, “nawawala ‘yung
false aggltn”
7. AUTOAGGLUTINATION caused by IgM can
also be inhibited or dispersed by incubating
red cells in the presence of either
DITHIOTHREITOL or 2-
AMINOETHYLISOTHIOURONIUM BROMIDE
EDLET CHRISTINE S. DIONISIO | BSMT 3B-3-1 8
You might also like
- Modern Blood Banking Transfusion Practices 5th Ed. by Denise HarmeningDocument568 pagesModern Blood Banking Transfusion Practices 5th Ed. by Denise HarmeningFarah TayyabNo ratings yet
- Stell & Maran S Text Book of Head and Neck Surgery and Oncology: Fifth EditionDocument1 pageStell & Maran S Text Book of Head and Neck Surgery and Oncology: Fifth EditionSanthosh Kumar D PNo ratings yet
- Blood Bank (2 Week) : Antibody ScreensDocument5 pagesBlood Bank (2 Week) : Antibody ScreensAngela Reyes100% (1)
- Urinalysis and Body Fluids for Cls & MltFrom EverandUrinalysis and Body Fluids for Cls & MltNo ratings yet
- Modern Blood Banking & Transfusion Practices Ed6 Harmening-235-257Document23 pagesModern Blood Banking & Transfusion Practices Ed6 Harmening-235-257ivanlchNo ratings yet
- ABO DiscrepanicesDocument12 pagesABO DiscrepanicesGlenn PerezNo ratings yet
- 3 ABO Discrepancies Other ProblemsDocument65 pages3 ABO Discrepancies Other ProblemsRuel Maddawin100% (2)
- CaseDocument1 pageCaseHAJI RASHIDNo ratings yet
- Cmo 14 s2006Document72 pagesCmo 14 s2006Shurei RanNo ratings yet
- Blood Bank TypingDocument34 pagesBlood Bank TypingSkylarNo ratings yet
- 68th AACC Annual Scientific Meeting Abstract eBookFrom Everand68th AACC Annual Scientific Meeting Abstract eBookNo ratings yet
- Blood Banking Course BookDocument2 pagesBlood Banking Course BookShukr Wesman BlbasNo ratings yet
- Must To Know HemaDocument44 pagesMust To Know HemaKaycee Gretz LorescaNo ratings yet
- ImmunohematologyDocument11 pagesImmunohematologydtimtiman100% (1)
- SerologyDocument84 pagesSerologyngsusannasuisum100% (2)
- Hematology2 - Laboratory TestsDocument3 pagesHematology2 - Laboratory Testskthmnts100% (1)
- Coombs TestDocument15 pagesCoombs TestFatema AminNo ratings yet
- Blood Bank ProceduresDocument33 pagesBlood Bank Procedures99noname100% (1)
- Serologic Tests Part 1Document4 pagesSerologic Tests Part 1Joshua TrinidadNo ratings yet
- Lab 5 Coombs TestsDocument26 pagesLab 5 Coombs TestsJennifer DixonNo ratings yet
- RH BLOOD GROUPDocument23 pagesRH BLOOD GROUPWho KnowsNo ratings yet
- Resolution of Abo DiscrepanciesDocument4 pagesResolution of Abo DiscrepanciesPatrick MabugatNo ratings yet
- Histopathology Review BookletDocument21 pagesHistopathology Review BookletMarie Llanes100% (2)
- Immunoserology: Medical Technology Assessment Progam 1 Discussed By: Mr. Mark MendrosDocument8 pagesImmunoserology: Medical Technology Assessment Progam 1 Discussed By: Mr. Mark MendrosLea Juan100% (1)
- Board Exam Topic ChecklistDocument3 pagesBoard Exam Topic ChecklistVianney Angeli LorenzanaNo ratings yet
- Chapter Blood: RBC Platelet HemostasisDocument89 pagesChapter Blood: RBC Platelet Hemostasisapi-19916399100% (1)
- Group 6 - Immunohematology - Blood BankingDocument8 pagesGroup 6 - Immunohematology - Blood Bankingjulo_05No ratings yet
- CLINICAL CHEMISTRY - Specimen CollectionDocument4 pagesCLINICAL CHEMISTRY - Specimen CollectionthedarkwingNo ratings yet
- Other Blood Group System AssignmentDocument5 pagesOther Blood Group System AssignmentMary ChristelleNo ratings yet
- Microscopic Examination of UrineDocument4 pagesMicroscopic Examination of UrineGlaiza Erika Baes GudaNo ratings yet
- Methods of Studying Fungi: Dr. Alice Alma C. BungayDocument74 pagesMethods of Studying Fungi: Dr. Alice Alma C. BungayKaycee Gretz LorescaNo ratings yet
- Blood Bank Guy Blood GroupsDocument19 pagesBlood Bank Guy Blood GroupsJessica TuNo ratings yet
- Flashcards in Abo Blood GroupDocument10 pagesFlashcards in Abo Blood GroupVincent ReyesNo ratings yet
- Clinical Chemistry KeyNotes For Board ExaminationDocument12 pagesClinical Chemistry KeyNotes For Board ExaminationPrincess Alen Aguilar100% (2)
- Isbb Review Questions - CompressDocument32 pagesIsbb Review Questions - CompressdmiahalNo ratings yet
- Blood BankDocument32 pagesBlood Bankpikachu100% (1)
- CSMLS Exam Guide Notes (Referrence Range)Document4 pagesCSMLS Exam Guide Notes (Referrence Range)software4us.2023No ratings yet
- IMHM321 Lecture Trans 3Document9 pagesIMHM321 Lecture Trans 3Brix BrixNo ratings yet
- Clinical ChemistryDocument7 pagesClinical ChemistryDale SuanoNo ratings yet
- Hematology Recall QuestionsDocument4 pagesHematology Recall QuestionsMai RodrigoNo ratings yet
- Hematology PDFDocument85 pagesHematology PDFammarNo ratings yet
- CC 1.01 Basic Principles of Clinical ChemistryDocument7 pagesCC 1.01 Basic Principles of Clinical ChemistryRobert JarvinaNo ratings yet
- Blood Bank 4 DiscpDocument20 pagesBlood Bank 4 DiscpHector de la CruzNo ratings yet
- New Microsoft Word DocumentDocument7 pagesNew Microsoft Word DocumentDocAxi Maximo Jr AxibalNo ratings yet
- Hematology Special StainDocument28 pagesHematology Special Stainandreea0dey100% (1)
- ISBB Aaaaa PDFDocument55 pagesISBB Aaaaa PDFSelena de LimaNo ratings yet
- Blood Smear Examination 1معدل Document74 pagesBlood Smear Examination 1معدل Kenesa100% (1)
- Blood Banking ReviewDocument442 pagesBlood Banking ReviewMayra Flor100% (2)
- Immunohema QuestionDocument19 pagesImmunohema QuestionLily Beauty100% (1)
- Hematology Ii Lectures Introduction To HemostasisDocument28 pagesHematology Ii Lectures Introduction To HemostasisJoshua Trinidad100% (1)
- ML7111 MCQs Answers Sep 2019Document10 pagesML7111 MCQs Answers Sep 2019Cleo Salvador100% (2)
- Crossmatching, Types, Principle, Procedure and InterpretationDocument5 pagesCrossmatching, Types, Principle, Procedure and InterpretationMerhan Fouda100% (1)
- Lab Policies Crossmatch Procedure Gel Method LabDocument7 pagesLab Policies Crossmatch Procedure Gel Method LabEli Buenaventura100% (2)
- HeamatologyDocument45 pagesHeamatologypikachuNo ratings yet
- Lesson 22 PDFDocument5 pagesLesson 22 PDFfaeNo ratings yet
- Antibody IdentificationDocument27 pagesAntibody Identificationhamaada100% (1)
- Blood Bank SOP 2015Document52 pagesBlood Bank SOP 2015ddophlaak labdeptNo ratings yet
- Clinical Chemistry Notes (Blanked) - ABI PDFDocument34 pagesClinical Chemistry Notes (Blanked) - ABI PDFAnya IgnacioNo ratings yet
- Disorders of Iron Kinetics and Heme MetabolismDocument12 pagesDisorders of Iron Kinetics and Heme MetabolismJoanne JardinNo ratings yet
- Blood Bank ManualDocument29 pagesBlood Bank ManualMarice Ferrufino SchmidtNo ratings yet
- Weak D Testing (Du) Testing Principle and ApplicationsDocument1 pageWeak D Testing (Du) Testing Principle and ApplicationsMai ÜüNo ratings yet
- Faculty of Dentistry Alexandria University, SyllabusDocument228 pagesFaculty of Dentistry Alexandria University, SyllabusMahmoud HeshamNo ratings yet
- Pilonidal Sinus Radiology Reference ArticleDocument1 pagePilonidal Sinus Radiology Reference ArticleHeron BeleiNo ratings yet
- Metropolice Annual Report 2021-22Document284 pagesMetropolice Annual Report 2021-22yogita goreNo ratings yet
- DateSheet HSSC 2011 WebDocument2 pagesDateSheet HSSC 2011 WebAxel BlazeNo ratings yet
- Machine Learning For Medical Diagnosis - Its Implications and SolutionsDocument15 pagesMachine Learning For Medical Diagnosis - Its Implications and Solutionsrichy amadiNo ratings yet
- Robbins e Cotran - Le Basi Patologiche Delle Malattie Vol. 2 Malattie Degli Organi e Degli Apparati (Italian Edition) (Unknown)Document4,674 pagesRobbins e Cotran - Le Basi Patologiche Delle Malattie Vol. 2 Malattie Degli Organi e Degli Apparati (Italian Edition) (Unknown)Francesco De PaolisNo ratings yet
- Harsh Mohan Textbook of Pathology, 7th Edition-17-22Document6 pagesHarsh Mohan Textbook of Pathology, 7th Edition-17-22Sebastian Moreno100% (2)
- Eyesi Direct BrochureDocument12 pagesEyesi Direct BrochureHaag-Streit UK (HS-UK)No ratings yet
- Laboratory Technician ResumeDocument9 pagesLaboratory Technician Resumedrrzjaifg100% (2)
- Chamberlain E Book SmallerDocument85 pagesChamberlain E Book SmallertarakaivaramNo ratings yet
- Dental Assisting CoursesDocument8 pagesDental Assisting Coursessongyifei0903No ratings yet
- 49 Anatomic Pathology GuidelinesDocument3 pages49 Anatomic Pathology GuidelinesJhOy XiNo ratings yet
- Pathologist Laboratory Medical Director in Denver CO Resume Joseph EastmanDocument5 pagesPathologist Laboratory Medical Director in Denver CO Resume Joseph EastmanJosephEastmanNo ratings yet
- Bethesda 2014Document11 pagesBethesda 2014David José FletesNo ratings yet
- Surgical Pathology of Liver TumorsDocument480 pagesSurgical Pathology of Liver TumorsGeorgiana BuhociNo ratings yet
- 2009 - Quality Assurance Guidelines For Surgeons in Breast Cancer ScreeningDocument40 pages2009 - Quality Assurance Guidelines For Surgeons in Breast Cancer ScreeningMomčilo MirićNo ratings yet
- PO Box 1118 PO Box 609 Dixon, CA 95620 Stockbridge, MI 49285Document2 pagesPO Box 1118 PO Box 609 Dixon, CA 95620 Stockbridge, MI 49285Osama BakheetNo ratings yet
- Cancer Stem Cells CD44 CD24 ESA CANINE MAMMARY TUMORDocument7 pagesCancer Stem Cells CD44 CD24 ESA CANINE MAMMARY TUMORvk_204veticoNo ratings yet
- ORLANDO D. GARCIA, JR., Doing Business Under The Name and Style COMMUNITY DIAGNOSTIC CENTER and BU CASTRO, Petitioners, vs. RANIDA D. SALVADOR and RAMON SALVADOR, Respondents.Document2 pagesORLANDO D. GARCIA, JR., Doing Business Under The Name and Style COMMUNITY DIAGNOSTIC CENTER and BU CASTRO, Petitioners, vs. RANIDA D. SALVADOR and RAMON SALVADOR, Respondents.Charles Roger RayaNo ratings yet
- 9 A31 Ad 01Document302 pages9 A31 Ad 01bhoopendrabisht100% (3)
- Principles of Medical Technology Practice 1Document6 pagesPrinciples of Medical Technology Practice 1Maw BerryNo ratings yet
- Red Cell Morphology in Peripheral Smear and Automated Counter 2019 PDFDocument6 pagesRed Cell Morphology in Peripheral Smear and Automated Counter 2019 PDFtufis02No ratings yet
- Form Blood RequisitionDocument2 pagesForm Blood Requisitionshubham kumar ram100% (1)
- (Handout) - MTLBE RA 5527Document15 pages(Handout) - MTLBE RA 5527Zach SastrillasNo ratings yet
- Exam Summar 12ug PG 080212Document24 pagesExam Summar 12ug PG 080212Neha Kelkar100% (1)
- Ra 5527Document56 pagesRa 5527Christian John Mabalot Carillo86% (7)
- Resumen Unidad 2Document31 pagesResumen Unidad 2yeseniaram073No ratings yet