Professional Documents
Culture Documents
Communicating Complexity: Using A Diagnostic Classification System For Edentulous Patients
Communicating Complexity: Using A Diagnostic Classification System For Edentulous Patients
Uploaded by
waf51Copyright:
Available Formats
You might also like
- UE 2 Cours 3 MétrologieDocument57 pagesUE 2 Cours 3 MétrologieLia MohamedNo ratings yet
- The Completely Edentulous Mandible: Treatment Plans For Fixed RestorationsDocument15 pagesThe Completely Edentulous Mandible: Treatment Plans For Fixed Restorationswaf51No ratings yet
- MemoiregguillemainDocument62 pagesMemoiregguillemainFeriel FerielNo ratings yet
- Herbs That Kill Cancer and HIVDocument6 pagesHerbs That Kill Cancer and HIVsilentweaponsquietwars100% (2)
- Maladie Parondontale-FrDocument27 pagesMaladie Parondontale-FrHina HinsNo ratings yet
- Evaluation Preoperatoire de La Difficulte en Endodontie2009Document7 pagesEvaluation Preoperatoire de La Difficulte en Endodontie2009tahari nabilaNo ratings yet
- Cartographie Des RisquesDocument6 pagesCartographie Des RisquesMAROUANI El HoussainNo ratings yet
- Rapport de Stage 2023Document10 pagesRapport de Stage 2023imane1997elgoualNo ratings yet
- Questions-Reponses Presse Presse Irct Insuffisance Renale Chronique TerminaleDocument10 pagesQuestions-Reponses Presse Presse Irct Insuffisance Renale Chronique TerminalehalimarhbNo ratings yet
- Tribune Chirurgie - PR J.P. ChambonDocument4 pagesTribune Chirurgie - PR J.P. ChambonLe Quotidien du MédecinNo ratings yet
- Recommandation Obesite - Prise en Charge Chirurgicale Chez LadulteDocument26 pagesRecommandation Obesite - Prise en Charge Chirurgicale Chez LadulteEmmanuelNo ratings yet
- Lvrea 252 P 252Document9 pagesLvrea 252 P 252yoli.rubia1990No ratings yet
- S7 Kamoun HDocument26 pagesS7 Kamoun H02299249No ratings yet
- Ami Expertise Infirmiere en Soins Palliatifs VF PUBLIEDocument3 pagesAmi Expertise Infirmiere en Soins Palliatifs VF PUBLIEJohann LaangryNo ratings yet
- Luxembourg Referentiel NationalDocument19 pagesLuxembourg Referentiel NationalMed ZiouiNo ratings yet
- Bupha TD 2020 Jungling NicolasDocument112 pagesBupha TD 2020 Jungling NicolasYasmine ChnitirNo ratings yet
- Bien Démarrer en Implantologie (PDFDrive)Document4 pagesBien Démarrer en Implantologie (PDFDrive)tamouza chaouiNo ratings yet
- EB1 Sujet SHSDocument12 pagesEB1 Sujet SHSLolly PoproNo ratings yet
- Evaluation Des Techniques de Pose Des Bandes de Compression Medicale Chez Les Patients Porteurs D'ulceDocument9 pagesEvaluation Des Techniques de Pose Des Bandes de Compression Medicale Chez Les Patients Porteurs D'ulcePampam PereraNo ratings yet
- Diagnostic Des Kystes Des Maxillaires Et Lésions Apparentées Basé Sur Des Critères RadiologiquesDocument54 pagesDiagnostic Des Kystes Des Maxillaires Et Lésions Apparentées Basé Sur Des Critères RadiologiquesYamina IhaddadeneNo ratings yet
- Évaluation Du Transfert Des Connaissance Suite À Une FormationDocument15 pagesÉvaluation Du Transfert Des Connaissance Suite À Une FormationSaidi SoundosNo ratings yet
- Antibioprophylaxie 2017 CRC - CaDocument37 pagesAntibioprophylaxie 2017 CRC - CaHamza BaibaiNo ratings yet
- Relation Médecin Chirurgien Dentiste PatientDocument15 pagesRelation Médecin Chirurgien Dentiste PatientAna MariaNo ratings yet
- La PassationDocument25 pagesLa PassationKamalNo ratings yet
- PJ1 Systeme Priorisation Acces Chirurgie Pandemie v4 4Document32 pagesPJ1 Systeme Priorisation Acces Chirurgie Pandemie v4 4luysykaaNo ratings yet
- PDF - Vol 98-11-N°11Document9 pagesPDF - Vol 98-11-N°11kepipranave-9084No ratings yet
- 2-Elaboration Livret Therapeutique DMDocument26 pages2-Elaboration Livret Therapeutique DMpharmatb.hisNo ratings yet
- Nursing in OncologyDocument7 pagesNursing in OncologyDarine FallehNo ratings yet
- AH 604 GuideDocument51 pagesAH 604 GuideSamira MoussaNo ratings yet
- Pratiques Avancées Et Formation Spécifique Des IDE de Réanimation: Résultats de L 'Enquête de La SRLF 2013Document2 pagesPratiques Avancées Et Formation Spécifique Des IDE de Réanimation: Résultats de L 'Enquête de La SRLF 2013Najeh OmriNo ratings yet
- Fiche de LectureDocument6 pagesFiche de LectureMck AbdelhamidNo ratings yet
- Les Matériaux de Pansements Dans Le Traitement de PlaiesDocument1 pageLes Matériaux de Pansements Dans Le Traitement de PlaiesKouekam Gustave TientcheuNo ratings yet
- Iqss 2019 Aide Utilisation Proms EdsDocument18 pagesIqss 2019 Aide Utilisation Proms Edshouda.chaikhiNo ratings yet
- GuidelinesDocument8 pagesGuidelinesRabia khouildiNo ratings yet
- 026 AO MBEDE Prothèse Adjointe Partielle ActualiséDocument5 pages026 AO MBEDE Prothèse Adjointe Partielle ActualiséGhita SaafNo ratings yet
- L'administration Intraveineuse Des Substances de Contraste en Imagerie Médicale Au CHUQDocument87 pagesL'administration Intraveineuse Des Substances de Contraste en Imagerie Médicale Au CHUQCH BtissamNo ratings yet
- Mémoire: Maître Ès Sciences (M. SC.)Document146 pagesMémoire: Maître Ès Sciences (M. SC.)moulay ImeneNo ratings yet
- 2 - AFAR - Prise en Charge Des Infections Intra Abdominales PDFDocument25 pages2 - AFAR - Prise en Charge Des Infections Intra Abdominales PDFDavid HernándezNo ratings yet
- Traiter Un Edentement Partiel Par Prothèse Fixée Implantaire - ATDocument6 pagesTraiter Un Edentement Partiel Par Prothèse Fixée Implantaire - ATmmghizlanemmNo ratings yet
- T. Levent, J. Alibert, E. Desantis, P. Paradis: Article OriginalDocument7 pagesT. Levent, J. Alibert, E. Desantis, P. Paradis: Article OriginalHarouna RachidNo ratings yet
- POSITIVISME LOGIQUE Rhumatologie Par Les Residents Marocains Revue de Rhumatologie n63Document9 pagesPOSITIVISME LOGIQUE Rhumatologie Par Les Residents Marocains Revue de Rhumatologie n63EDDAOUDI MOHAMEDNo ratings yet
- CV-A-PARE-FR en EsDocument5 pagesCV-A-PARE-FR en Essssslim220890No ratings yet
- Recommendations Chirurgie Cataracte PDFDocument23 pagesRecommendations Chirurgie Cataracte PDFWady Ben JalelNo ratings yet
- Enquête Connaissances TRT Patients Antithrombotiques 2017Document4 pagesEnquête Connaissances TRT Patients Antithrombotiques 2017hachemNo ratings yet
- 08 Evaluation de La Qualit Des Soins Aux Cliniques Universitaires de KinshasaDocument11 pages08 Evaluation de La Qualit Des Soins Aux Cliniques Universitaires de KinshasaMariano OKENo ratings yet
- Cano Systemictherstandards FDocument18 pagesCano Systemictherstandards Fmahrezbh05No ratings yet
- RPP Stage MouniaDocument7 pagesRPP Stage Mouniabenaddimounia23No ratings yet
- Technologies de L'information Et de La Communication (Tic) Dans La Formation Infirmière InitialeDocument6 pagesTechnologies de L'information Et de La Communication (Tic) Dans La Formation Infirmière InitialeMBOWAMBA LOBOMBONo ratings yet
- Approche Reflexive Finale-1Document25 pagesApproche Reflexive Finale-1lamourmed1994No ratings yet
- Note Cadrage Indicateurs Alerte Version Mel Novembre2020Document8 pagesNote Cadrage Indicateurs Alerte Version Mel Novembre2020Antoine SoulNo ratings yet
- Beautiful - Ai - Implication de L'assistant Dentaire Dans L'efficacité de La Prise en Charge Des PatientsDocument9 pagesBeautiful - Ai - Implication de L'assistant Dentaire Dans L'efficacité de La Prise en Charge Des PatientsfacturationcieramotorsNo ratings yet
- 01 Glossaire Final4Document223 pages01 Glossaire Final4vazagusNo ratings yet
- Élaboration D'une Politique de Gestion Et de Maintenance Des Équipements Biomedicaux Gérés Par Le Service Biomedical PDFDocument104 pagesÉlaboration D'une Politique de Gestion Et de Maintenance Des Équipements Biomedicaux Gérés Par Le Service Biomedical PDFkawtarlawthiNo ratings yet
- Chaquesasensi (2016) Limites para El Camuflaje en ORto PDFDocument24 pagesChaquesasensi (2016) Limites para El Camuflaje en ORto PDFSamanta SalazarNo ratings yet
- Le Développement de La Chirurgie Ambulatoire Et Ses Conséquences Sur La Qualité de La Prise en ChargeDocument43 pagesLe Développement de La Chirurgie Ambulatoire Et Ses Conséquences Sur La Qualité de La Prise en ChargeMarcel BertrandNo ratings yet
- La Greffe Des Cellules Adipeuses Dans Lesthetique de La Face: Technique Et IndicationsDocument8 pagesLa Greffe Des Cellules Adipeuses Dans Lesthetique de La Face: Technique Et IndicationsIJAR JOURNALNo ratings yet
- ProgrammeDocument27 pagesProgrammeraissakapapa8No ratings yet
- Fichier Produit 2861Document4 pagesFichier Produit 2861Nai maNo ratings yet
- Draft de La DF GUIDE PAOSP Janvier 2024Document24 pagesDraft de La DF GUIDE PAOSP Janvier 2024NAWAL NAKHLINo ratings yet
- TracheotomiseDocument24 pagesTracheotomisekassebrihabNo ratings yet
- Assuring Optimal Trauma Care-The RoleDocument8 pagesAssuring Optimal Trauma Care-The RolerisnayektiNo ratings yet
- Dentisterie 2.0 : Une Odyssée dans les Innovations et Pratiques AvancéesFrom EverandDentisterie 2.0 : Une Odyssée dans les Innovations et Pratiques AvancéesNo ratings yet
- 2016COIR DigitalvsconventionalimpressionDocument9 pages2016COIR Digitalvsconventionalimpressionwaf51No ratings yet
- Accuracy and Reliability of Intraoral Scanners: Are They The Better Option?Document9 pagesAccuracy and Reliability of Intraoral Scanners: Are They The Better Option?waf51No ratings yet
- 65 - JPOR - 2019 - 356 EnciaDocument8 pages65 - JPOR - 2019 - 356 Enciawaf51No ratings yet
- Use of Diagnostic and Surgical Stent A SimplifiedDocument7 pagesUse of Diagnostic and Surgical Stent A Simplifiedwaf51No ratings yet
- A Review of The Recent Literature On Maxillary Overdenture With Dental ImplantsDocument5 pagesA Review of The Recent Literature On Maxillary Overdenture With Dental Implantswaf51No ratings yet
- Residual Ridge ResorptionDocument38 pagesResidual Ridge Resorptionwaf51No ratings yet
- 3DPrinted Materials For Permanent Restorations in IndirectDocument19 pages3DPrinted Materials For Permanent Restorations in Indirectwaf51No ratings yet
- 1548-1336 (2004) 030 0030 Aocarc 2 0 Co 2Document10 pages1548-1336 (2004) 030 0030 Aocarc 2 0 Co 2waf51No ratings yet
- 1 s2.0 S277255962200013X MainDocument10 pages1 s2.0 S277255962200013X Mainwaf51No ratings yet
- TARLOWimplantstentarticleDocument3 pagesTARLOWimplantstentarticlewaf51No ratings yet
- Implant Surgical Guides From The Past To The PresentDocument6 pagesImplant Surgical Guides From The Past To The Presentwaf51No ratings yet
- Philosophy and Physics of Mandibular Hinge Axis: A Review: International Journal of Scientific Research April 2014Document3 pagesPhilosophy and Physics of Mandibular Hinge Axis: A Review: International Journal of Scientific Research April 2014waf51No ratings yet
- ATWOODDocument15 pagesATWOODwaf51No ratings yet
- ANTERIORPOINTOFREFERENCEDocument6 pagesANTERIORPOINTOFREFERENCEwaf51No ratings yet
- 3D Printing Guide Implant Placement A Case ReportDocument5 pages3D Printing Guide Implant Placement A Case Reportwaf51No ratings yet
- The Third Point of Reference and Its EffDocument7 pagesThe Third Point of Reference and Its Effwaf51No ratings yet
- Evaluation of Two Facebow/Semi-adjustable Articulator Systems For Orienting Maxillary Cast On Articulators: A Pilot StudyDocument5 pagesEvaluation of Two Facebow/Semi-adjustable Articulator Systems For Orienting Maxillary Cast On Articulators: A Pilot Studywaf51No ratings yet
- Maxillary Immediate Denture: A Case Report: International Journal of Medical and Health ResearchDocument3 pagesMaxillary Immediate Denture: A Case Report: International Journal of Medical and Health Researchwaf51No ratings yet
- Textbook of Prosthodontics PDFDriveDocument864 pagesTextbook of Prosthodontics PDFDrivewaf51No ratings yet
- Effect of Joint Surface Contours On The Transverse and Impactstrength of Denture Base Resin Repaired by Various Methods. An Invitro StudyDocument12 pagesEffect of Joint Surface Contours On The Transverse and Impactstrength of Denture Base Resin Repaired by Various Methods. An Invitro Studywaf51No ratings yet
- 補 綴 誌,J Jpn Prosthodont Soc, 31: 1405∼1412, 1987Document8 pages補 綴 誌,J Jpn Prosthodont Soc, 31: 1405∼1412, 1987waf51No ratings yet
- 1 INTRO Module 2 Roles of The Professional Nurse - DRDocument8 pages1 INTRO Module 2 Roles of The Professional Nurse - DREileen Kay A. MañiboNo ratings yet
- A. General Data B. Chief Complaint/Presenting Problem C. History of Present Illness (Put Emphasis On OLDCAARTS) 1Document2 pagesA. General Data B. Chief Complaint/Presenting Problem C. History of Present Illness (Put Emphasis On OLDCAARTS) 1Eryll Paolo AleaNo ratings yet
- Best Zome For Wright Loss - Google SearchDocument1 pageBest Zome For Wright Loss - Google Searchhdksjwj hdjjNo ratings yet
- Veterinary Surgery ThesisDocument6 pagesVeterinary Surgery Thesislbbzfoxff100% (2)
- Cluster HeadacheDocument2 pagesCluster HeadachenanikNo ratings yet
- International Human Resource Management INE3023: Ihrm Trends & Future Future ChallengesDocument29 pagesInternational Human Resource Management INE3023: Ihrm Trends & Future Future ChallengesHuyền Oanh ĐinhNo ratings yet
- Xerox Document Centre 535/545/555, CC35-WCP55F Service Manual - Adobe PDF VersionDocument70 pagesXerox Document Centre 535/545/555, CC35-WCP55F Service Manual - Adobe PDF VersionKeroo MagdyNo ratings yet
- Sintomas Somaticos AdultosDocument2 pagesSintomas Somaticos AdultosMiguel Angel FloresNo ratings yet
- Module 3 - Application of Curriculum Development ApproachesDocument5 pagesModule 3 - Application of Curriculum Development ApproachesAngela BarrettNo ratings yet
- NCCN 2022Document178 pagesNCCN 2022Rizka IbonitaNo ratings yet
- Training and Development of HDFC BankDocument109 pagesTraining and Development of HDFC BankMaster Printers100% (1)
- ICICI Lombard Health Care Policy Number: 4034i/ff P/04812914/00/000Document3 pagesICICI Lombard Health Care Policy Number: 4034i/ff P/04812914/00/000arjunNo ratings yet
- WHO Drug InformationDocument99 pagesWHO Drug Informationchromicutting100% (1)
- HirarcDocument34 pagesHirarcBungsu HiperkesNo ratings yet
- Integrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Document12 pagesIntegrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Joud D.No ratings yet
- Budget of Work For Personal DevelopmentDocument17 pagesBudget of Work For Personal DevelopmentAngelica Velaque Babsa-ay AsiongNo ratings yet
- Impact of Attitude Towards Negative News On Psychological Disorder: A Case Study of Universities Students of Khyber Pakhtunkhwa, PakistanDocument6 pagesImpact of Attitude Towards Negative News On Psychological Disorder: A Case Study of Universities Students of Khyber Pakhtunkhwa, PakistanaalijaaproductionsNo ratings yet
- Communication in NursingDocument4 pagesCommunication in NursingDavid EtukudoNo ratings yet
- Anca, Etal (2023) Sdo FormatDocument27 pagesAnca, Etal (2023) Sdo FormatDENNIS AGUDONo ratings yet
- Community Health Nursing Vol. 2: Christian Parabuac Bachelor of Sciene in Nursing Level 3. Prof. Cherry Ann DuranteDocument50 pagesCommunity Health Nursing Vol. 2: Christian Parabuac Bachelor of Sciene in Nursing Level 3. Prof. Cherry Ann DuranteLeya Thaobunyuen100% (1)
- Guidelines For Pregnant Women and Nursing Mothers: Covid-19Document4 pagesGuidelines For Pregnant Women and Nursing Mothers: Covid-19Gbadeyanka O WuraolaNo ratings yet
- Nursing TheoriesDocument21 pagesNursing TheoriesReal TetisoraNo ratings yet
- Halitosis QuestionnaireDocument3 pagesHalitosis Questionnairealumera50% (2)
- Anjani Ayuningtyas KD NIM: 18.1422.S (4B)Document4 pagesAnjani Ayuningtyas KD NIM: 18.1422.S (4B)dilan mileaNo ratings yet
- Icknield Newsletter December 2023Document20 pagesIcknield Newsletter December 202322hzamanNo ratings yet
- 7b. Orientation Module 2Document4 pages7b. Orientation Module 2Fuad AddaieNo ratings yet
- Ayush Dubai3Document1 pageAyush Dubai3deepakmukhiNo ratings yet
- Occupational HealthDocument16 pagesOccupational HealthfaarehaNo ratings yet
- Hazard Identification and Risk Assessment TemplateDocument3 pagesHazard Identification and Risk Assessment TemplateSejal SatputeNo ratings yet
Communicating Complexity: Using A Diagnostic Classification System For Edentulous Patients
Communicating Complexity: Using A Diagnostic Classification System For Edentulous Patients
Uploaded by
waf51Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Communicating Complexity: Using A Diagnostic Classification System For Edentulous Patients
Communicating Complexity: Using A Diagnostic Classification System For Edentulous Patients
Uploaded by
waf51Copyright:
Available Formats
P R A T I Q U E C L I N I Q U E
Communicating Complexity:
Using a Diagnostic Classification System
for Edentulous Patients
(Savoir expliquer les traitements complexes : Utilisation d’un système
de classification des diagnostics pour les patients édentés)
• Randall D. Mazurat, BSc, DDS, MDEd •
• Nita M. Mazurat, DDS •
S o m m a i r e
Les dentistes qui exercent en cabinet privé et dans les facultés de médecine dentaire ont à traiter un nombre
appréciable de patients édentés qui requièrent des traitements complexes. Le Collège américain des prosthodon-
tistes a élaboré un système de classification de l’édentation complète, qui peut guider la planification du traitement
global et la prise en charge des patients avec des prothèses complètes. Ce système repose sur des variables de
diagnostic précises et fait appel à un modèle basé sur une liste de contrôle qui peut être appliqué facilement et rapi-
dement. Même s’il existe à ce jour peu de données publiées permettant d’établir un lien direct entre la classifica-
tion et le pronostic, le système peut néanmoins être utilisé par les étudiants en médecine dentaire et les dentistes
praticiens pour déterminer les caractéristiques démographiques des patients édentés. De fait, le système a notam-
ment été utilisé par des étudiants de premier cycle d’une école de médecine dentaire, pour déterminer la pertinence
d’un traitement pour des patients et diriger les patients ayant besoin de traitements complexes vers une équipe
enseignant-étudiant appropriée. Le fait de discuter du système de classification avec les patients aide en outre le
dentiste à expliquer la complexité du traitement requis et pourrait aussi faciliter la conciliation attentes-résultats.
Mots clés MeSH : denture, complete; mouth, edentulous/classification; patient care planning
© J Can Dent Assoc 2003; 69(8):511–4
Cet article a fait l’objet d’une révision par des pairs.
T
he need for complete dentures, and consequently the profession runs the risk that this area of dentistry will be lost
need for training in the fabrication of complete to alternative providers. To encourage practitioners to main-
dentures, will not decline in the foreseeable future. tain or increase their interest and skills in the area of complete
Although the proportion of the total population with dentures will require the provision of continuing education for
complete dentures has declined, this decline has been offset by dentists and dental laboratory technicians in all areas of
the increase in the overall population, in particular the increase complete denture prosthodontics and the development of
in the older adult population who have complete dentures, reasonable treatment fees and fee guides that offer sufficient
and by specific patient groups who choose complete denture compensation for providing these services.
therapy for socio-economic reasons. Two recent articles in the Given the changing demographics of the patients who use
Journal of Prosthetic Dentistry1,2 provide convincing evidence of complete dentures (i.e., patients are older, with more years of
a significant continuing need for complete denture services in denture wear and more medical problems) the complexity of
North America, a need that may largely go unmet because of a treatment can be expected to increase. The greater time requi-
projected decrease in dental practitioners. The general red to manage and satisfy the needs of patients with complete
practitioner may thus be expected to provide more rather then dentures, as well as the greater responsibilities associated with
less service in the area of complete dentures; otherwise, the such care, requires compensation commensurate with the task.
Journal de l’Association dentaire canadienne Septembre 2003, Vol. 69, N° 8 511
Mazurat, Mazurat
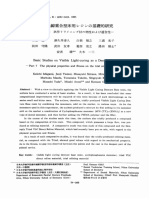
Figure 1 : Class I. Mandibular bone height 21 mm or greater. Figure 2: Class IV. Mandibular bone height 10 mm or less
Figure 3: Class IV. No anterior or posterior vestibule. Figure 4: Class IV. Redundant tissue. Major soft-tissue revision
required.
Providing complete denture therapy that reflects the needs of The American College of Prosthodontists (ACP) has
individual patients is not a new concept; however, both third- developed a classification system for complete edentulism that
party payers and patients appear to believe that “one fee fits is based on specific diagnostic criteria. Edentulism is divided
all,” an unreasonable assumption that should be challenged.
into 4 levels of difficulty or complexity: Classes I, II, III and
A formal system of classifying edentulous patients might help
in this regard. Determining patients’ treatment needs accor- IV. Class IV designates patients who require the most difficult
ding to preset criteria may help in setting a reasonable fee for degree or complexity of treatment. The classes are differentia-
treatment and in identifying patients who are best treated by ted from each other according to the following features:3
means of referral to a prosthodontist.
• The skill level required to treat that class of patient: Does
Reasons for a Classification System the patient require novice or expert treatment?
Classifying edentulous patients according to preset • The necessity for modification of basic clinical or
criteria can be an aid in numerous aspects of treatment: laboratory procedures: Will more complicated procedures
• establishing a basis for diagnostic and treatment or more time be required for treatment?
procedures
• Overall management and complexity of treatment: Will
• justifying treatment procedures and fees to third-party
payers and patients expert intervention and referral be required?
• screening patients treated in dental faculties for assignment A brief summary of the salient features of the classification
to undergraduate or graduate students system is provided here. For a comprehensive review of the
• providing data for review of treatment outcome rationale for developing the system, application of the system
• simplifying communication in discussions of treatment and the diagnostic criteria used, the reader is directed to the
with patients and colleagues. original references.3,4
512 Septembre 2003, Vol. 69, N° 8 Journal de l’Association dentaire canadienne
Using a Diagnostic Classification System for Edentulous Patients
Table 1 Diagnostic criteria for Class III Table 2 Diagnostic criteria for Class IV
patients patients
Diagnostic variable Criterion No. of Diagnostic variable Criterion No. of
patients patients
Mandibular bone height Class III 9 Mandibular bone height Class IV 14
Maxillary ridge morphology Type C 5 Maxillary ridge morphology Type D 0
Mandibular muscle attachment Type C 11 Mandibular muscle attachment Type D or E 7
Maxillomandibular relationship Class III 10 Maxillomandibular relationship Class III 6
Soft-tissue procedures required Minor 1 Soft-tissue procedures required Minor 1
Interarch space Limited Interarch space Limited
(18–20 mm) 2 (18–20 mm) 0
Tongue Large 4 Tongue Large 1
Modifying variable Not specified 4 Modifying variable Not specified 6
Total 29 Total 20
Diagnostic Criteria for Classifying Patients then 10 mm of residual bone height would be assigned to
To apply the classification system, the clinician uses a Class IV (Fig. 2), the most complex category, no matter how
checklist or worksheet to focus attention on specific diagnostic favourable the rest of the variables. It is important to complete
variables. The items in the checklist are ordered according to as much of the worksheet as possible because this yields an
the objectivity of their assessment (i.e., the ease with which individualized patient profile that will help in determining the
they can be measured and assessed), not their order of signifi- prognosis and formulating the treatment plan, as well as
cance. The following diagnostic variables, in descending order assisting in communications with the patient.
of objectivity, are used:
Example of Application of the System in an
• mandibular bone height, measured radiographically
(Figs. 1 and 2)
Undergraduate Clinic
All 76 patients examined in the third-year complete-
• morphologic features of the maxillary residual ridge denture clinic at the University of Manitoba’s faculty of
(Figs. 3 and 4) dentistry from January 2002 to January 2003 were classified
• mandibular muscle attachment using the ACP classification system. There were 12 patients in
• maxillomandibular relationship Class I (least complex), 15 in Class II, 29 in Class III and
• presence of conditions requiring preprosthetic surgery 20 in Class IV (most complex).
Data on the diagnostic variables used in the classification
• interarch space of Class III and Class IV patients are presented in Tables 1
• tongue anatomy and 2.
• modifying variables, such as systemic disease, psychosocial Most patients had more then one diagnostic variable by
factors or temporomandibular disorders (TMD). which they were categorized as Class III or Class IV. Aspects of
Explicit guidelines are provided on the worksheet3,4 to the anatomy of the mandibular ridge (either bone height or
guide the practitioner in applying the classification system. muscle attachment) were the variables most commonly deter-
mining these classifications.
Use of the Classification System Modifying variables are variables that would make conven-
Practitioners who want to use the classification system tional treatment or patient management very difficult, such as
should consult the original references3,4 and make copies of the severe systemic disease, major psychosocial problems requiring
worksheet for their own use. The worksheet is usually comple- professional intervention, severe TMD symptoms, maxillofa-
ted at the time of the initial screening appointment. It focuses cial defects and patients whose dental problems have been
the examination on the specific diagnostic variables required refractory to previous treatment. Most of the patients designa-
and allows rapid classification of patients. If there are problems ted as Class III or Class IV on the basis of a modifying varia-
in determining the patient’s status in any particular category, ble had conditions refractory to previous treatment, for exam-
the practitioner should leave that item blank and continue ple, patients who were dissatisfied with previous appropriate
with the rest of the items. This is a “no-tolerance” type of clas- treatment, patients who had gone without any prosthesis for
sification system, and as such a single variable with a complex many years, patients who were unable or unwilling to wear
rating is enough to classify the patient in a more complex dentures, and patients whose expectations were unlikely to be
(higher-level) category. No-tolerance systems emphasize the met given their previous intolerance of conventional complete
impact of each variable on the overall determination of class, dentures.
and the final classification is determined by the variable with The ACP classification system has been used to determine
the highest level of complexity. For instance, a patient with less the suitability of patients for treatment by undergraduates,
Journal de l’Association dentaire canadienne Septembre 2003, Vol. 69, N° 8 513
Mazurat, Mazurat
to assign patients to staff–student pairs and, most importantly,
Le Dr R. Mazurat est professeur agrégé, Département de dentisterie
to heighten the awareness of all those involved as to the restauratrice, Université du Manitoba, Winnipeg.
complexity of treatment undertaken in the undergraduate La Dre N. Mazurat est professeure adjointe, Département de
clinic. Discussion of the classification with the student and dentisterie restauratrice, Université du Manitoba, Winnipeg.
the patient during the treatment planning appointments Écrire au : Dr Randall D. Mazurat, Université du Manitoba,
has emphasized the unique aspects of each individual’s 780, av. Bannatyne, Winnipeg MB R3E 0W2. Courriel :
rmazurat@ms.umanitoba.ca.
treatment. Students and staff know from the outset the Les auteurs n’ont aucun intérêt déclaré financier.
complexity of the cases and also have an indication of cases
with an unfavourable prognosis.
Three patients categorized as Class IV on the basis of Références
multiple variables were deemed inappropriate for undergra- 1. Douglass CW, Shih A, Ostry L. Will there be a need for complete
dentures in the United States in 2020? J Prosthet Dent 2002; 87(1):5–8.
duate treatment; however, the other 73 patients were
2. Douglass CW, Watson AJ. Future needs for fixed and removable partial
eventually treated in the undergraduate clinic. The complex dentures in the United States. J Prosthet Dent 2002; 87(1):9–14.
Class IV patients were assigned to students supervised by full- 3. McGarry TJ, Nimmo A, Skiba JF, Ahlstrom RH, Smith CR,
time prosthodontic staff members. Although any treatment Koumjian JH. Classification system for complete edentulism.
given at this level of the curriculum requires constant supervi- J Prosthodont 1999; 8(1):27–39.
sion, management of Class IV patients requires additional 4. McGarry TJ, Nimmo A, Skiba JF, Ahlstrom RH, Smith CR,
Koumjian JH. Classification system for complete edentulism. Dent Today
judicious hands-on intervention by staff, notably when the 2001; 20(10):90–5.
final impression for the mandibular arch is being made. If
there were an abundance of edentulous patients available for
treatment at this level of the undergraduate curriculum, it
would be desirable to refer more of the complex Class IV
patients for graduate or specialist care. However, a review of
the patients treated from January 2002 to January 2003 revea-
led only 6 cases in which treatment was deemed an early
failure, where success was determined by patient satisfaction,
and treatment was deemed a failure when the patient was
unable to wear the dentures for any reason. There did not
appear to be any correlation between the patient’s classification
and the failure rate. Of the 6 patients with early failure, 3 were
unsatisfied with the esthetic appearance of the dentures, 1 was
unsatisfied with the substitution of resin denture teeth for
their previous porcelain teeth, 1 found the new denture
uncomfortable, and 1 was unable to accommodate to wearing
the denture because of gagging. Only one of these patients was
a Class IV patient. The patient had never worn dentures, had
a severe Class II maxillomandibular relationship, had unreaso-
nable esthetic expectations, had severe gagging and had a
problem with alcohol abuse.
Experience in the undergraduate clinic indicates that
patient management, specifically meeting patients’ expecta-
tions with regard to esthetic appearance, had a greater impact
than the students’ ability to carry out the clinical and techni-
cal procedures related to fabrication of technically acceptable
dentures. In other words, it was far easier to manage the oral
anatomy than the patients’ expectations. It will be interesting
to see if this early anecdotal observation persists as additional
reports of the validity of the ACP classification are published.
So far, there do not appear to be any published reports corre-
lating classification criteria with treatment success. The next
stage of the project at the University of Manitoba is to assess
outcomes at recall appointments and to determine whether
there is a relationship between classification of edentulism and
prognosis. C
514 Septembre 2003, Vol. 69, N° 8 Journal de l’Association dentaire canadienne
You might also like
- UE 2 Cours 3 MétrologieDocument57 pagesUE 2 Cours 3 MétrologieLia MohamedNo ratings yet
- The Completely Edentulous Mandible: Treatment Plans For Fixed RestorationsDocument15 pagesThe Completely Edentulous Mandible: Treatment Plans For Fixed Restorationswaf51No ratings yet
- MemoiregguillemainDocument62 pagesMemoiregguillemainFeriel FerielNo ratings yet
- Herbs That Kill Cancer and HIVDocument6 pagesHerbs That Kill Cancer and HIVsilentweaponsquietwars100% (2)
- Maladie Parondontale-FrDocument27 pagesMaladie Parondontale-FrHina HinsNo ratings yet
- Evaluation Preoperatoire de La Difficulte en Endodontie2009Document7 pagesEvaluation Preoperatoire de La Difficulte en Endodontie2009tahari nabilaNo ratings yet
- Cartographie Des RisquesDocument6 pagesCartographie Des RisquesMAROUANI El HoussainNo ratings yet
- Rapport de Stage 2023Document10 pagesRapport de Stage 2023imane1997elgoualNo ratings yet
- Questions-Reponses Presse Presse Irct Insuffisance Renale Chronique TerminaleDocument10 pagesQuestions-Reponses Presse Presse Irct Insuffisance Renale Chronique TerminalehalimarhbNo ratings yet
- Tribune Chirurgie - PR J.P. ChambonDocument4 pagesTribune Chirurgie - PR J.P. ChambonLe Quotidien du MédecinNo ratings yet
- Recommandation Obesite - Prise en Charge Chirurgicale Chez LadulteDocument26 pagesRecommandation Obesite - Prise en Charge Chirurgicale Chez LadulteEmmanuelNo ratings yet
- Lvrea 252 P 252Document9 pagesLvrea 252 P 252yoli.rubia1990No ratings yet
- S7 Kamoun HDocument26 pagesS7 Kamoun H02299249No ratings yet
- Ami Expertise Infirmiere en Soins Palliatifs VF PUBLIEDocument3 pagesAmi Expertise Infirmiere en Soins Palliatifs VF PUBLIEJohann LaangryNo ratings yet
- Luxembourg Referentiel NationalDocument19 pagesLuxembourg Referentiel NationalMed ZiouiNo ratings yet
- Bupha TD 2020 Jungling NicolasDocument112 pagesBupha TD 2020 Jungling NicolasYasmine ChnitirNo ratings yet
- Bien Démarrer en Implantologie (PDFDrive)Document4 pagesBien Démarrer en Implantologie (PDFDrive)tamouza chaouiNo ratings yet
- EB1 Sujet SHSDocument12 pagesEB1 Sujet SHSLolly PoproNo ratings yet
- Evaluation Des Techniques de Pose Des Bandes de Compression Medicale Chez Les Patients Porteurs D'ulceDocument9 pagesEvaluation Des Techniques de Pose Des Bandes de Compression Medicale Chez Les Patients Porteurs D'ulcePampam PereraNo ratings yet
- Diagnostic Des Kystes Des Maxillaires Et Lésions Apparentées Basé Sur Des Critères RadiologiquesDocument54 pagesDiagnostic Des Kystes Des Maxillaires Et Lésions Apparentées Basé Sur Des Critères RadiologiquesYamina IhaddadeneNo ratings yet
- Évaluation Du Transfert Des Connaissance Suite À Une FormationDocument15 pagesÉvaluation Du Transfert Des Connaissance Suite À Une FormationSaidi SoundosNo ratings yet
- Antibioprophylaxie 2017 CRC - CaDocument37 pagesAntibioprophylaxie 2017 CRC - CaHamza BaibaiNo ratings yet
- Relation Médecin Chirurgien Dentiste PatientDocument15 pagesRelation Médecin Chirurgien Dentiste PatientAna MariaNo ratings yet
- La PassationDocument25 pagesLa PassationKamalNo ratings yet
- PJ1 Systeme Priorisation Acces Chirurgie Pandemie v4 4Document32 pagesPJ1 Systeme Priorisation Acces Chirurgie Pandemie v4 4luysykaaNo ratings yet
- PDF - Vol 98-11-N°11Document9 pagesPDF - Vol 98-11-N°11kepipranave-9084No ratings yet
- 2-Elaboration Livret Therapeutique DMDocument26 pages2-Elaboration Livret Therapeutique DMpharmatb.hisNo ratings yet
- Nursing in OncologyDocument7 pagesNursing in OncologyDarine FallehNo ratings yet
- AH 604 GuideDocument51 pagesAH 604 GuideSamira MoussaNo ratings yet
- Pratiques Avancées Et Formation Spécifique Des IDE de Réanimation: Résultats de L 'Enquête de La SRLF 2013Document2 pagesPratiques Avancées Et Formation Spécifique Des IDE de Réanimation: Résultats de L 'Enquête de La SRLF 2013Najeh OmriNo ratings yet
- Fiche de LectureDocument6 pagesFiche de LectureMck AbdelhamidNo ratings yet
- Les Matériaux de Pansements Dans Le Traitement de PlaiesDocument1 pageLes Matériaux de Pansements Dans Le Traitement de PlaiesKouekam Gustave TientcheuNo ratings yet
- Iqss 2019 Aide Utilisation Proms EdsDocument18 pagesIqss 2019 Aide Utilisation Proms Edshouda.chaikhiNo ratings yet
- GuidelinesDocument8 pagesGuidelinesRabia khouildiNo ratings yet
- 026 AO MBEDE Prothèse Adjointe Partielle ActualiséDocument5 pages026 AO MBEDE Prothèse Adjointe Partielle ActualiséGhita SaafNo ratings yet
- L'administration Intraveineuse Des Substances de Contraste en Imagerie Médicale Au CHUQDocument87 pagesL'administration Intraveineuse Des Substances de Contraste en Imagerie Médicale Au CHUQCH BtissamNo ratings yet
- Mémoire: Maître Ès Sciences (M. SC.)Document146 pagesMémoire: Maître Ès Sciences (M. SC.)moulay ImeneNo ratings yet
- 2 - AFAR - Prise en Charge Des Infections Intra Abdominales PDFDocument25 pages2 - AFAR - Prise en Charge Des Infections Intra Abdominales PDFDavid HernándezNo ratings yet
- Traiter Un Edentement Partiel Par Prothèse Fixée Implantaire - ATDocument6 pagesTraiter Un Edentement Partiel Par Prothèse Fixée Implantaire - ATmmghizlanemmNo ratings yet
- T. Levent, J. Alibert, E. Desantis, P. Paradis: Article OriginalDocument7 pagesT. Levent, J. Alibert, E. Desantis, P. Paradis: Article OriginalHarouna RachidNo ratings yet
- POSITIVISME LOGIQUE Rhumatologie Par Les Residents Marocains Revue de Rhumatologie n63Document9 pagesPOSITIVISME LOGIQUE Rhumatologie Par Les Residents Marocains Revue de Rhumatologie n63EDDAOUDI MOHAMEDNo ratings yet
- CV-A-PARE-FR en EsDocument5 pagesCV-A-PARE-FR en Essssslim220890No ratings yet
- Recommendations Chirurgie Cataracte PDFDocument23 pagesRecommendations Chirurgie Cataracte PDFWady Ben JalelNo ratings yet
- Enquête Connaissances TRT Patients Antithrombotiques 2017Document4 pagesEnquête Connaissances TRT Patients Antithrombotiques 2017hachemNo ratings yet
- 08 Evaluation de La Qualit Des Soins Aux Cliniques Universitaires de KinshasaDocument11 pages08 Evaluation de La Qualit Des Soins Aux Cliniques Universitaires de KinshasaMariano OKENo ratings yet
- Cano Systemictherstandards FDocument18 pagesCano Systemictherstandards Fmahrezbh05No ratings yet
- RPP Stage MouniaDocument7 pagesRPP Stage Mouniabenaddimounia23No ratings yet
- Technologies de L'information Et de La Communication (Tic) Dans La Formation Infirmière InitialeDocument6 pagesTechnologies de L'information Et de La Communication (Tic) Dans La Formation Infirmière InitialeMBOWAMBA LOBOMBONo ratings yet
- Approche Reflexive Finale-1Document25 pagesApproche Reflexive Finale-1lamourmed1994No ratings yet
- Note Cadrage Indicateurs Alerte Version Mel Novembre2020Document8 pagesNote Cadrage Indicateurs Alerte Version Mel Novembre2020Antoine SoulNo ratings yet
- Beautiful - Ai - Implication de L'assistant Dentaire Dans L'efficacité de La Prise en Charge Des PatientsDocument9 pagesBeautiful - Ai - Implication de L'assistant Dentaire Dans L'efficacité de La Prise en Charge Des PatientsfacturationcieramotorsNo ratings yet
- 01 Glossaire Final4Document223 pages01 Glossaire Final4vazagusNo ratings yet
- Élaboration D'une Politique de Gestion Et de Maintenance Des Équipements Biomedicaux Gérés Par Le Service Biomedical PDFDocument104 pagesÉlaboration D'une Politique de Gestion Et de Maintenance Des Équipements Biomedicaux Gérés Par Le Service Biomedical PDFkawtarlawthiNo ratings yet
- Chaquesasensi (2016) Limites para El Camuflaje en ORto PDFDocument24 pagesChaquesasensi (2016) Limites para El Camuflaje en ORto PDFSamanta SalazarNo ratings yet
- Le Développement de La Chirurgie Ambulatoire Et Ses Conséquences Sur La Qualité de La Prise en ChargeDocument43 pagesLe Développement de La Chirurgie Ambulatoire Et Ses Conséquences Sur La Qualité de La Prise en ChargeMarcel BertrandNo ratings yet
- La Greffe Des Cellules Adipeuses Dans Lesthetique de La Face: Technique Et IndicationsDocument8 pagesLa Greffe Des Cellules Adipeuses Dans Lesthetique de La Face: Technique Et IndicationsIJAR JOURNALNo ratings yet
- ProgrammeDocument27 pagesProgrammeraissakapapa8No ratings yet
- Fichier Produit 2861Document4 pagesFichier Produit 2861Nai maNo ratings yet
- Draft de La DF GUIDE PAOSP Janvier 2024Document24 pagesDraft de La DF GUIDE PAOSP Janvier 2024NAWAL NAKHLINo ratings yet
- TracheotomiseDocument24 pagesTracheotomisekassebrihabNo ratings yet
- Assuring Optimal Trauma Care-The RoleDocument8 pagesAssuring Optimal Trauma Care-The RolerisnayektiNo ratings yet
- Dentisterie 2.0 : Une Odyssée dans les Innovations et Pratiques AvancéesFrom EverandDentisterie 2.0 : Une Odyssée dans les Innovations et Pratiques AvancéesNo ratings yet
- 2016COIR DigitalvsconventionalimpressionDocument9 pages2016COIR Digitalvsconventionalimpressionwaf51No ratings yet
- Accuracy and Reliability of Intraoral Scanners: Are They The Better Option?Document9 pagesAccuracy and Reliability of Intraoral Scanners: Are They The Better Option?waf51No ratings yet
- 65 - JPOR - 2019 - 356 EnciaDocument8 pages65 - JPOR - 2019 - 356 Enciawaf51No ratings yet
- Use of Diagnostic and Surgical Stent A SimplifiedDocument7 pagesUse of Diagnostic and Surgical Stent A Simplifiedwaf51No ratings yet
- A Review of The Recent Literature On Maxillary Overdenture With Dental ImplantsDocument5 pagesA Review of The Recent Literature On Maxillary Overdenture With Dental Implantswaf51No ratings yet
- Residual Ridge ResorptionDocument38 pagesResidual Ridge Resorptionwaf51No ratings yet
- 3DPrinted Materials For Permanent Restorations in IndirectDocument19 pages3DPrinted Materials For Permanent Restorations in Indirectwaf51No ratings yet
- 1548-1336 (2004) 030 0030 Aocarc 2 0 Co 2Document10 pages1548-1336 (2004) 030 0030 Aocarc 2 0 Co 2waf51No ratings yet
- 1 s2.0 S277255962200013X MainDocument10 pages1 s2.0 S277255962200013X Mainwaf51No ratings yet
- TARLOWimplantstentarticleDocument3 pagesTARLOWimplantstentarticlewaf51No ratings yet
- Implant Surgical Guides From The Past To The PresentDocument6 pagesImplant Surgical Guides From The Past To The Presentwaf51No ratings yet
- Philosophy and Physics of Mandibular Hinge Axis: A Review: International Journal of Scientific Research April 2014Document3 pagesPhilosophy and Physics of Mandibular Hinge Axis: A Review: International Journal of Scientific Research April 2014waf51No ratings yet
- ATWOODDocument15 pagesATWOODwaf51No ratings yet
- ANTERIORPOINTOFREFERENCEDocument6 pagesANTERIORPOINTOFREFERENCEwaf51No ratings yet
- 3D Printing Guide Implant Placement A Case ReportDocument5 pages3D Printing Guide Implant Placement A Case Reportwaf51No ratings yet
- The Third Point of Reference and Its EffDocument7 pagesThe Third Point of Reference and Its Effwaf51No ratings yet
- Evaluation of Two Facebow/Semi-adjustable Articulator Systems For Orienting Maxillary Cast On Articulators: A Pilot StudyDocument5 pagesEvaluation of Two Facebow/Semi-adjustable Articulator Systems For Orienting Maxillary Cast On Articulators: A Pilot Studywaf51No ratings yet
- Maxillary Immediate Denture: A Case Report: International Journal of Medical and Health ResearchDocument3 pagesMaxillary Immediate Denture: A Case Report: International Journal of Medical and Health Researchwaf51No ratings yet
- Textbook of Prosthodontics PDFDriveDocument864 pagesTextbook of Prosthodontics PDFDrivewaf51No ratings yet
- Effect of Joint Surface Contours On The Transverse and Impactstrength of Denture Base Resin Repaired by Various Methods. An Invitro StudyDocument12 pagesEffect of Joint Surface Contours On The Transverse and Impactstrength of Denture Base Resin Repaired by Various Methods. An Invitro Studywaf51No ratings yet
- 補 綴 誌,J Jpn Prosthodont Soc, 31: 1405∼1412, 1987Document8 pages補 綴 誌,J Jpn Prosthodont Soc, 31: 1405∼1412, 1987waf51No ratings yet
- 1 INTRO Module 2 Roles of The Professional Nurse - DRDocument8 pages1 INTRO Module 2 Roles of The Professional Nurse - DREileen Kay A. MañiboNo ratings yet
- A. General Data B. Chief Complaint/Presenting Problem C. History of Present Illness (Put Emphasis On OLDCAARTS) 1Document2 pagesA. General Data B. Chief Complaint/Presenting Problem C. History of Present Illness (Put Emphasis On OLDCAARTS) 1Eryll Paolo AleaNo ratings yet
- Best Zome For Wright Loss - Google SearchDocument1 pageBest Zome For Wright Loss - Google Searchhdksjwj hdjjNo ratings yet
- Veterinary Surgery ThesisDocument6 pagesVeterinary Surgery Thesislbbzfoxff100% (2)
- Cluster HeadacheDocument2 pagesCluster HeadachenanikNo ratings yet
- International Human Resource Management INE3023: Ihrm Trends & Future Future ChallengesDocument29 pagesInternational Human Resource Management INE3023: Ihrm Trends & Future Future ChallengesHuyền Oanh ĐinhNo ratings yet
- Xerox Document Centre 535/545/555, CC35-WCP55F Service Manual - Adobe PDF VersionDocument70 pagesXerox Document Centre 535/545/555, CC35-WCP55F Service Manual - Adobe PDF VersionKeroo MagdyNo ratings yet
- Sintomas Somaticos AdultosDocument2 pagesSintomas Somaticos AdultosMiguel Angel FloresNo ratings yet
- Module 3 - Application of Curriculum Development ApproachesDocument5 pagesModule 3 - Application of Curriculum Development ApproachesAngela BarrettNo ratings yet
- NCCN 2022Document178 pagesNCCN 2022Rizka IbonitaNo ratings yet
- Training and Development of HDFC BankDocument109 pagesTraining and Development of HDFC BankMaster Printers100% (1)
- ICICI Lombard Health Care Policy Number: 4034i/ff P/04812914/00/000Document3 pagesICICI Lombard Health Care Policy Number: 4034i/ff P/04812914/00/000arjunNo ratings yet
- WHO Drug InformationDocument99 pagesWHO Drug Informationchromicutting100% (1)
- HirarcDocument34 pagesHirarcBungsu HiperkesNo ratings yet
- Integrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Document12 pagesIntegrating CAM Practices Into The Conventional Health Systems (Integrative Medicine)Joud D.No ratings yet
- Budget of Work For Personal DevelopmentDocument17 pagesBudget of Work For Personal DevelopmentAngelica Velaque Babsa-ay AsiongNo ratings yet
- Impact of Attitude Towards Negative News On Psychological Disorder: A Case Study of Universities Students of Khyber Pakhtunkhwa, PakistanDocument6 pagesImpact of Attitude Towards Negative News On Psychological Disorder: A Case Study of Universities Students of Khyber Pakhtunkhwa, PakistanaalijaaproductionsNo ratings yet
- Communication in NursingDocument4 pagesCommunication in NursingDavid EtukudoNo ratings yet
- Anca, Etal (2023) Sdo FormatDocument27 pagesAnca, Etal (2023) Sdo FormatDENNIS AGUDONo ratings yet
- Community Health Nursing Vol. 2: Christian Parabuac Bachelor of Sciene in Nursing Level 3. Prof. Cherry Ann DuranteDocument50 pagesCommunity Health Nursing Vol. 2: Christian Parabuac Bachelor of Sciene in Nursing Level 3. Prof. Cherry Ann DuranteLeya Thaobunyuen100% (1)
- Guidelines For Pregnant Women and Nursing Mothers: Covid-19Document4 pagesGuidelines For Pregnant Women and Nursing Mothers: Covid-19Gbadeyanka O WuraolaNo ratings yet
- Nursing TheoriesDocument21 pagesNursing TheoriesReal TetisoraNo ratings yet
- Halitosis QuestionnaireDocument3 pagesHalitosis Questionnairealumera50% (2)
- Anjani Ayuningtyas KD NIM: 18.1422.S (4B)Document4 pagesAnjani Ayuningtyas KD NIM: 18.1422.S (4B)dilan mileaNo ratings yet
- Icknield Newsletter December 2023Document20 pagesIcknield Newsletter December 202322hzamanNo ratings yet
- 7b. Orientation Module 2Document4 pages7b. Orientation Module 2Fuad AddaieNo ratings yet
- Ayush Dubai3Document1 pageAyush Dubai3deepakmukhiNo ratings yet
- Occupational HealthDocument16 pagesOccupational HealthfaarehaNo ratings yet
- Hazard Identification and Risk Assessment TemplateDocument3 pagesHazard Identification and Risk Assessment TemplateSejal SatputeNo ratings yet