Professional Documents
Culture Documents
Jurnal Aki
Jurnal Aki
Uploaded by
nelly muslimahOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Aki
Jurnal Aki
Uploaded by
nelly muslimahCopyright:
Available Formats
original article http://www.kidney-international.
org
& 2007 International Society of Nephrology
see commentary on page 963
Modified RIFLE criteria in critically ill children with
acute kidney injury
A Akcan-Arikan1, M Zappitelli1, LL Loftis2, KK Washburn1, LS Jefferson2 and SL Goldstein1
1
Renal Section, Department of Pediatrics, Baylor College of Medicine, Texas Children’s Hospital, Houston, Texas, USA and 2Section of
Critical Care Medicine, Department of Pediatrics, Baylor College of Medicine, Texas Children’s Hospital, Houston, Texas, USA
A classification system has been proposed to standardize the More than 30 acute kidney injury (AKI) definitions exist in the
definition of acute kidney injury in adults. These criteria of published literature.1 Lack of a standardized definition that can
risk, injury, failure, loss, and end-stage renal disease were be applied across patient populations (1) impedes rational
given the acronym of RIFLE. We have modified the criteria comparison of studies that assess preventive and therapeutic
based on 150 critically ill pediatric RIFLE (pRIFLE) patients to AKI strategies, (2) limits generalization of data generated from
assess acute kidney injury incidence and course along with single center studies, and (3) prevents patient stratification
renal and/or non-renal comorbidities. Of these children, based on AKI severity. Recent pediatric AKI epidemiological
11 required dialysis and 24 died. Patients without acute data for critically ill children demonstrates a shift from primary
kidney injury in the first week of intensive care admission renal disease to injury secondary to other systemic illnesses
were less likely to subsequently develop renal Injury or and/or their treatment.2,3 Widespread availability of aggressive
Failure; however, 82% of acute kidney injury occurred in this treatment options, such as bone marrow and solid organ
initial week. Within this group of 123 children, 60 reached transplantation for children, has led to increased exposure to
pRIFLEmax for Risk, 32 reached Injury, and 31 reached nephrotoxic medications and more critically ill children
Failure. Acute kidney injury during admission was an receiving intensive care. The incidence of pediatric AKI in this
independent predictor of intensive care; hospital length of at-risk population still remains unknown.
stay and an increased risk of death independent of the The reported mortality from AKI is still as high as 60% in
Pediatric Risk of Mortality (PRISM II) score (odds ratio 3.0). critically ill children.4 Most of the reported clinical studies of
Our results show that a majority of critically ill children pediatric AKI focus on patients requiring renal replacement
develop acute kidney injury by pRIFLE criteria and do so early therapy (RRT), who have clearly experienced severe renal
in the course of intensive care. Acute kidney injury is injury.5–10 However, recent studies demonstrate that even a
associated with mortality and may lead to increased hospital modest rise in serum creatinine (SCr) is a risk factor for
costs. We suggest that the pRIFLE criteria serves to mortality in adult and pediatric patients.11,12 Thus, SCr may
characterize the pattern of acute kidney injury in critically ill be an insensitive marker of early AKI and reliance on SCr
children. hampers early AKI recognition. Extensive study has focused
Kidney International (2007) 71, 1028–1035. doi:10.1038/sj.ki.5002231; upon investigation of urinary biomarkers that detect AKI
published online 28 March 2007 earlier than a rise in SCr.13–15
KEYWORDS: acute renal failure; children; critical illness; epidemiology A new classification system, termed the ‘RIFLE criteria,’ has
been proposed for use in critically ill adult patients by the Acute
Dialysis Quality Initiative group.1 RIFLE (acronym for Risk for
renal dysfunction, Injury to the kidney, Failure of kidney
function, Loss of kidney function, and End-stage renal disease
(ESRD)) aims to standardize the definition of AKI by stratifying
patients based on changes in SCr levels from baseline and/or an
abrupt decrease in urine output (UOP). We aimed to study a
modified pediatric version of the RIFLE criteria (pRIFLE) to (1)
describe the epidemiology and clinical course of AKI in
critically ill children and (2) explore the potential relationships
between AKI and renal and non-renal morbidities.
Correspondence: SL Goldstein, Renal Section, Department of Pediatrics,
Baylor College of Medicine, Texas Children’s Hospital, 6621, Fannin Street, RESULTS
MC3-2482, Houston, TX 77030, USA. E-mail: stuartg@bcm.tmc.edu Group characteristics
Received 21 December 2006; revised 21 January 2007; accepted 6 We prospectively enrolled 150 critically ill patients (55.3%
February 2007; published online 28 March 2007 males) over a 12-month period. Mean age was 6.476.4 years
1028 Kidney International (2007) 71, 1028–1035
A Akcan-Arikan et al.: AKI in critically ill children original article
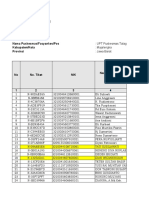
(median ¼ 4 years, range ¼ 1 month–21 years). Mean Pedia- Table 1 | Comparison of characteristics of patients with versus
tric Risk of Mortality (PRISM II) score at pediatric intensive without AKI
care unit (PICU) admission was 14.978.4 (median ¼ 15). Control n=27 AKI by RIFLE
Seventy-one percent of patients had preexisting chronic (18%) n=123 (82%)
conditions. All patients received invasive mechanical ventila- Continuous variables
tion (mean duration ¼ 14.5717.6days; median ¼ 9, Mean7s.d., median
range ¼ 1–100 days). Fifty-three percent (80/150) of patients Age (years) 6.076.6 (1.25) 6.576.3 (4.0)
Weight (kg) 21.7718.1 (12.0) 26.1723.6 (16.0)
received vasoactive medications (17.5% received one, 18.1% Height (cm) 103.9738.2 (87.0) 104.7738.4 (102.2)
two and 17.4% three or more). Mean PICU and hospital PRISM IIa 12.477.2 (13.0) 15.478.6 (16.0)
length of stay (LOS) were 16.6722.4 and 33.7738.1 days, Baseline eCCl 132746 (119) 1597100 (129)
respectively (median (range) ¼ 10 (2–192), and 21 (2–24), (ml/min/1.73 m2)b
Peak mean airway 15.078.2 (12.0) 17.279.2 (14.0)
respectively). Twenty-eight days and overall hospital mortal- pressure (mm Hg)
ity were 14% and 16%, respectively. Eleven patients (7.3%) Days ventilated 10.7711.3 (8.0) 15.8718.7 (9.0)
received acute RRT. PICU length of stay 10.176.2 (9.0) 18.0724.3 (11.0)*
Mean baseline estimated creatinine clearance (eCCl) for Hospital length of 20.5716.6 (14.0) 36.6740.1 (22.0)**
stay
the entire cohort was 154793 ml/min/1.73 m2 (med-
ian ¼ 124 ml/min/1.73 m2, range ¼ 41–924 ml/min/1.73 m2). Categorical variables, N (%)
Forty-one patients (27%) did not have baseline SCr values Ethnicity
and were assigned baseline eCCl of 100 ml/min/1.73 m2. Caucasian 11 (40.7) 41 (33.3)
African-American 5 (18.5) 25 (20.3)
Twenty-six patients had known pre-admission chronic Hispanic 8 (29.6) 55 (44.7)
neuromuscular disorders (NMd) associated with prolonged Asian 3 (11.1) 2 (1.6)
immobilization, resulting in severely decreased muscle mass
Male 11 (40.7) 56 (45.5)
(e.g., muscular dystrophy, cerebral palsy, quadriplegia, etc.).
Mean eCCl for the NMd subset was 2327173 ml/min/ Comorbidities
1.73 m2 (median ¼ 213 ml/min/1.73 m2). Mean baseline eCCl Present 17 (63) 89 (72.4)
for the non-NMd cohort (n ¼ 124) was 138755 ml/min/ Hematology/oncology 1 (3.7) 15 (12.2)
Cardiology 2 (7.4) 20 (16.3)
1.73 m2 (median ¼ 118 ml/min/1.73 m2). Otherb 14 (52) 55 (44.7)
Incidence and clinical course of AKI Admitting diagnosis
Twenty-seven patients did not develop AKI and served as Pneumonia 11 (41) 40 (33)
SIRSc/sepsis/septic 5 (18.5) 33 (26.8)
controls, 123 patients (82%) developed AKI by pRIFLE:
shock
48.8% of these reached pRIFLEmax R (n ¼ 60), 26.0% Cardiac arrest 6 (22) 12 (10)
reached I (n ¼ 32), and 25.2% reached F (n ¼ 31). Table 1 Other 5 (18.5) 38 (30.9)
displays the comparison of characteristics between
Clinical
patients with and without AKI. There were no statistically Need for pressors 13 (48.2) 66 (53.7)
significant differences in any of the baseline demographic Need for RRTd 0 11 (8.9)
characteristics between patients with vs without AKI. 28-Day mortality 3 (11.1) 18 (14.6)
PICU admission diagnoses, comorbidities, vasopressor re- AKI, acute kidney injury; eCCl, estimated creatinine clearance; PICU, pediatric
quirements, peak mean airway pressures, and days of intensive care unit; RIFLE, risk, injury, failure, loss and end-stage renal disease.
*Po0.07; **Po0.05.
ventilation also did not differ between patients with vs a
PRISM, Pediatric Risk of Mortality II score.
b
without AKI. Other includes the following diagnostic categories: endocrine, failure to thrive,
gastrointestinal, rheumatologic, neurological (cerebral palsy, and epilepsy), ortho-
Higher pRIFLEmax strata were associated with higher pedic, pulmonary, psychiatric.
PRISM II scores. Mean PRISM II scores for controls, R, I, and c
d
SIRS, systemic inflammatory response syndrome.
RRT, Renal replacement therapy.
F were 12.477.2, 13.077.7, 15.978.0, and 19.679.3,
respectively (Po0.001 by one-way analysis of variance).
Mean time to onset of the first pRIFLE stratum was Twenty-six percent of patients with initial pRIFLE R or I
3.373.1 days after PICU admission (median ¼ 2, progressed to a higher pRIFLE stratum. Patients with initial
range ¼ 1–14 days). Eighty-two percent (101/123) of patients pRIFLE I were more likely to progress to pRIFLEmax F than
developed AKI within the first 7 days of PICU admission those with initial pRIFLE R (12/31 (39%) vs 3/76 (4%),
(Figure 1). Patients who did not develop AKI within the first Po0.0001).
7 days of PICU admission were very unlikely to subsequently Figure 2 summarizes AKI distribution and outcomes
develop severe AKI (negative predictive value (NPV) of comparing patients with and without chronic NMd. We
reaching pRIFLEmax I or F ¼ 95.1%, Po0.001; NPV of chose to examine the NMd group separately because it is
reaching pRIFLEmax F ¼ 97.7%, Po0.001). Patients who unknown whether change in SCr/eCCl is as reliable a marker
remained free of AKI in the first 7 days did not receive RRT of change in renal function in this unique group, owing to
(NPV 100%, P ¼ 0.03). severely reduced muscle mass. The AKI prevalence and AKI
Kidney International (2007) 71, 1028–1035 1029
original article A Akcan-Arikan et al.: AKI in critically ill children
severity distribution did not differ between patients with vs pRIFLE F and no RRT vs 22% in those who received RRT,
without NMd. P40.05), PICU LOS and hospital LOS were longer in those
Eleven patients received RRT. Continuous venovenous who received dialysis (PICU LOS: 12.678.5 (median ¼ 10) vs
hemodialysis was provided for 10 patients; one patient 25.3713.1 days (median ¼ 22), respectively; hospital LOS:
initiated hemodialysis but was converted to continuous 40.7759.0 (median ¼ 22) vs 60.6740.0 days (median ¼ 46)
venovenous hemodialysis after two treatments. Nine of these respectively, both Po0.05). This may have been explained by
patients had pRIFLE F AKI and two had pRIFLE I at RRT the fact that 71% (5/7) of non-surviving patients with
initiation. The decision to initiate RRT was made on the basis pRIFLE F AKI who did not receive RRT died within 24 h of
of clinical and laboratory grounds by the attending pRIFLEmax F attainment.
nephrologist and not by using pRIFLE criteria. Two patients
with pRIFLE I AKI were stem cell transplant recipients who Distribution of pRIFLE by SCr vs UOP criteria
required RRT for fluid overload prevention per our Ninety-seven patients (81.5%) fulfilled pRIFLECr criteria and
institution’s protocol,16 and the remaining nine patients 65 (54.6%) fulfilled pRIFLEUOP criteria at some time during
were dialyzed primarily for uremia. These nine patients were the study period. Of the 11 patients who received dialysis,
older than the remaining 22 patients with pRIFLE F AKI who four had not attained pRIFLEUOP status before initiating
did not receive RRT (10.475.5 vs 6.576.6 years, Po0.05), dialysis. These four patients were included in the group who
but did not differ significantly in gender distribution, PRISM only attained pRIFLECr for this analysis. All patients
II score, nor proportion diagnosed with sepsis (not shown). requiring dialysis attained their pRIFLECrmax before initia-
Although mortality was similar in the groups (29% for tion of dialysis.
Table 2 lists outcome based on the type of RIFLE criteria
achieved. Forty-three patients (35.0%) attained both pRI-
40 FLECr and pRIFLEUOP AKI (pRIFLECr þ UOP), 58 (47.2%)
pRIFLEmax only pRIFLECr criteria and 22 (17.9%) attained only
35
pRIFLEF
30 pRIFLEUOP (Table 2). Patients with pRIFLECr only tended
Number of patients
25
to be younger (Table 2). Patients with pRIFLEUOP only had
20
lower PRISM II scores (Po0.05, analysis of variance), and
none of them died or required dialysis. Mortality was
15
higher for patients with pRIFLECr (SCr only or SCr þ urine
10
output) compared with the group that only attained
5
pRIFLEUOP criteria (both Po0.05). Mortality in the
0 pRIFLECr þ UOP group did not differ compared with the
1 2 3 3 3 6 7 >8
Day of PICU admission pRIFLECr only group.
Table 3 displays pRIFLECrmax and pRIFLEUOPmax for the
Figure 1 | Distribution of the day of admission that subjects
reached pRIFLEmax (n ¼ 123) and pRIFLE F stratum (n ¼ 31). 43 patients who attained pRIFLE AKI criteria by both SCr
Black bars indicate numbers of subjects attaining their pRIFLEmax AKI and UOP categories. Only six patients attained a pRIFLEUOP-
on a given day, and gray bars indicate numbers of subjects attaining max that was worse than their pRIFLECrmax; none of whom
their first pRIFLE F on a given day. The majority of subjects (82%)
received dialysis or died. Only four patients attained any
reached their maximum pRIFLE stratum for AKI (black) within the first
week of admission, and most patients who reached pRIFLE F AKI did pRIFLEUOP before attaining any pRIFLECr; none of these
so within the first week of admission (25/31 ¼ 81%, gray bars). patients later received dialysis.
All 150 patients
NMd No NMd
N=26 N =124
AKI No AKI AKI No AKI
N =21 (80.8%) N =5 (19.2%) N=102 (82.3%) N =22 (17.7%)
maxR maxI or F maxR maxI or F
9/21 (42.9%) 12/21 (57.1%) 51/102 (50%) 51/102 (50%)
1/9 (11.1%) 6/12 (50%) death 2/5 (40%) death 4/51 (7.8%) 7/51 (13.7%) death 1/22 (4.6%)
death 0 RRT 1/12 (8.3%)RRT 0 RRT death 0 RRT 10/51 (19.6%) RRT death
Figure 2 | Flow diagram indicating the distribution of AKI and outcome (survival and need for RRT), comparing patients with and
without chronic a neuromuscular disease (NMd, neuromuscular disease; maxR/maxI/maxF, maxiumum pRIFLE stratum attained
during admission; RRT, renal replacement therapy).
1030 Kidney International (2007) 71, 1028–1035
A Akcan-Arikan et al.: AKI in critically ill children original article
Table 2 | Comparison of characteristics and outcomes of Table 3 | Two-by-two table depicting the maximum pRIFLECr
patients with AKI, based on their attainment of pRIFLE and maximum pRIFLEUOP attained during the study period, in
criteria by urine output only (pRIFLEUOP), by SCr only patients who attained pRIFLE AKI by SCr and urine output
(pRIFLECr), or by both (pRIFLECr+UOP) criteria
pRIFLEUOP pRIFLECr onlya pRIFLESCr+UOP Urine pRIFLEmax
only N=22 N=58 N=43
R I F Total
Age SCr pRIFLEmax
Mean7s.d. 8.575.9 (7.5) 4.375.8 (1.0)b 8.676.4 (8.0) R 13 5 1 19
(median) I 5 3 0 8
F 3 3 10 16
PRISM Total 21 10 9 43
Mean7s.d. 10.677.8 (8.0)c 15.877.9 (15.5) 17.479.1 (18.0)
(median) AKI, acute kidney injury; pRIFLE, pediatric risk, injury, failure, loss and end-stage renal
disease; SCr, serum creatinine.
Dark gray: six patients had higher pRIFLEUOPmax than pRIFLECrmax.
Males Light gray: 26 patients had the same pRIFLEUOPmax as their pRIFLECrmax.
N/total (%) 12/22 (54.6) 28/58 (48.3) 27/43 (62.8)
28-Day mortality
N/total (%) 0 9/58 (15.5)d 9/43 (20.9)d
the early reversal group received RRT than in the group with
Need for dialysis persistent AKI (1/22 (4.5%) vs 10/30 (33.3%), respectively,
N/total (%) 0 5/58 (8.6) 6/43 (14.0)e Po0.03); this association was also independent of age and
gender (logistic regression, P ¼ 0.0001).
pRIFLEmax
pRIFLEmax R
N/total (%) 18/22 (81.8) 29/58 (50.0) 13/43 (30.2) Outcomes
pRIFLEmax I AKI and LOS (PICU and hospital). In univariate analyses,
N/total (%) 3/22 (13.6) 16/58 (27.6) 13/43 (30.2) patients with AKI tended to have a longer PICU LOS when
pRIFLEmax F
N/total (%) 1/22 (4.5) 13/58 (22.4) 17/43 (39.5)
compared with control patients (18.0724.3 vs 10.176.2
ANOVA, analysis of variance; AKI, acute kidney injury; KI, kidney injury; pRIFLE,
days, P ¼ 0.06). Hospital LOS was significantly longer for
pediatric risk, injury, failure, loss and end-stage renal disease; PRISM, Pediatric Risk of patients with AKI compared with the control group
Mortality score; SCr, serum creatinine.
a
(36.6740.1 vs 20.5716.6 days, P ¼ 0.04). Table 4 lists Cox
Patients who attained pRIFLE urine output criteria only after dialysis was initiated
were included in the SCr pRIFLE only group. regression analysis for PICU and hospital LOS adjusting for
b
AKI patients who only attained pRIFLE criteria by SCr were statistically significantly age and gender and accounting for death as a censoring
younger than patients in the other groups (Po0.05, ANOVA).
c
KI patients who only attained pRIFLE criteria by urine output had statistically
event. The presence of any AKI, of pRIFLEmax I or F, and of
significantly lower PRISM scores than the other two groups. pRIFLEmax F during the study period were each indepen-
d
28-day mortality was higher in both AKI groups with SCr pRIFLE criteria attainment dently associated with longer hospital LOS. The presence of
(Po0.05) compared with the group with only urine output pRIFLE criteria.
e
The need for dialysis tended to be higher in both groups that attained SCr pRIFLE AKI during the study period was independently associated
criteria compared with the group that only attained urine output pRIFLE criteria, but with longer PICU LOS. The presence of AKI pRIFLE I or F on
the difference did not achieve statistical significance (Po0.1).
admission was associated with longer hospital LOS. Patients
with persistent admission AKI (no improvement within 48 h)
AKI on admission: early reversal vs persistent AKI did not demonstrate longer hospital or PICU LOS, compared
We examined separately a subgroup of patients with AKI at with all other patients.
the time of admission to the PICU (Figure 3). Fifty-two
(42.3%) patients had AKI on the day of admission: 16 Mortality
(30.8%) had pRIFLE R, 21 (40.4%) had pRIFLE I, and 15 Figures 2 and 3 display the distribution of survival outcome,
(28.8%) had pRIFLE F. Patients with AKI on admission had examining the whole sample (Figure 2) and those with AKI
higher PRISM II scores than patients who developed AKI on admission (Figure 3). Overall mortality rates did not
after day 1 (18.978.9 vs 12.877.4, P ¼ 0.0001). A higher differ between patients with AKI (14.6%) vs those without
proportion of patients with AKI on admission received RRT AKI (11.1%). However, patients with pRIFLEmax I or F
than patients who developed AKI after day 1 (10/52 vs 1/71 during admission had over twice the mortality than patients
(P ¼ 0.001)); the association between AKI on admission and with pRIFLEmax R or controls (21 vs 8%, respectively,
the need for dialysis was independent of age and gender Po0.05). Patients with pRIFLEmax F also had over twice the
(logistic regression, P ¼ 0.004). mortality rate of the rest of the cohort (25.8% for
Renal function substantially improved (as defined by a pRIFLEmax F vs 10.9% for all others, P ¼ 0.03).
decrease in pRIFLE stratum) within 48 h (‘early reversal’) in Patients with chronic NMd had a higher mortality rate
46% of patients with AKI at PICU admission. Early reversal than the rest of the cohort (35 vs 10%, Po0.05; Figure 2).
of AKI was more likely to occur in patients with pRIFLE R on Because AKI rates were not different in the NMd group, NMd
admission (10/16, 62.5%), than in those with pRIFLE I (8/21, was not a confounder of the effect of AKI on mortality. Using
38.1%) or F (4/15, 26.7%) on admission. Fewer patients in logistic regression, controlling for age, gender, PRISM II
Kidney International (2007) 71, 1028–1035 1031
original article A Akcan-Arikan et al.: AKI in critically ill children
52 patients with AKI on admission
Admission
pRIFLE stratum 16 (30.8%) R 36 (69.2%) I or F
48 h after
admission 10/16 (62.5%) 6/16 (37.5%) 12/36 (33.3%) 24/36 (66.7%)
No PersAKI PersAKI No PersAKI PersAKI
Final 1/10 (10%) died 1/6 (16.7%) died 6/24 (25%) died
0 died 7/24 (29.2%) RRT
outcome 0 RRT 1/6 (16.7%) RRT and died
1/12 (8.3%) RRT
2/16 (12.5%) total deaths 2/24 (8.3%) RRT and died
8/24 (33.3%) total deaths
No difference in % PersAKI had higher % deaths*
deaths or % RRT. No difference in % RRT (p=0.06)
Figure 3 | Flow diagram of the course of AKI, for patients with AKI on the day of admission (n ¼ 52). Most deaths occurred in
patients with pRIFLE I or F on admission who had persistent AKI, defined as lack of improvement in AKI pRIFLE stratum within 48 h.
Table 4 | The effect of different criteria for AKI on hospital score, the association between AKI during admission and
and PICU length of stays, independent of age and gendera mortality was no longer significant (Table 5). However, when
Hospital LOS- PICU LOS- AKI was defined only by SCr criterion, pRIFLECrmax I or F
adjusted HR adjusted HR was independently associated with an increased risk of
(95% CI)b (95% CI)b mortality (Table 5). When PRISM II score was removed from
AKI during the PICU stay all regression models, the effects of the different expressions
Using SCr+urine output criteria of AKI on mortality appeared more important, with most
Any AKI during admxc 0.6 (0.4–0.9)* 0.6 (0.4–0.9)* odds ratios increasing substantially (Table 5).
pRIFLEmax I or F 0.6 (0.4–0.9)* 0.7 (0.5–0.9)*
pRIFLEmax F 0.6 (0.4–0.9)* 0.8 (0.5–1.2) The presence of AKI on admission was not an indepen-
dent risk factor for mortality. Patients with AKI on admission
Using SCr criterion only who did not improve in pRIFLE stratum within 48 h
Any AKI during admxc 0.5 (0.3–0.7)* 0.4 (0.3–0.6)* (persistent AKI, n ¼ 30) did not have a higher risk of
pRIFLEmax I or F 0.5 (0.4–0.8)* 0.6 (0.4–0.8)*
pRIFLEmax F 0.6 (0.4–0.9)* 0.7 (0.5–1.1) mortality compared with the rest of the cohort, when
controlled for age, gender, and PRISM II score (Table 5).
AKI on admission to PICU
Using SCr+urine output criteria
AKI on admx 0.7 (0.5–1.01) 0.9 (0.6–1.2) DISCUSSION
AKI pRIFLE I or F on admx 0.6 (0.4–0.9)* 0.7 (0.5–1.03) The current prospective study shows pRIFLE to serve well to
AKI on admx with persistent 0.8 (0.5–1.1) 0.8 (0.6–1.3) both classify pediatric AKI epidemiology and reflect the
AKId
AKI pRIFLE I or F on admx 0.7 (0.4–1.1) 0.8 (0.5–1.2)
course of AKI in children admitted to the PICU. AKI
with persistent AKI classification using pRIFLE criteria revealed that AKI is very
common in critically ill pediatric patients and is associated
Using SCr criterion only with significant morbidity.
AKI on admx 0.7 (0.5–0.96) 0.8 (0.6–1.2)
AKI pRIFLE I or F on admx 0.6 (0.4–0.9)* 0.7 (0.5–1.03)** AKI occurred very early in the PICU course, most often
AKI on admx with persistent 0.8 (0.5–1.1) 0.8 (0.6–1.3) within the first week of admission, and patients who did not
AKId develop AKI within the first 7 days of PICU admission were
AKI pRIFLE I or F on admx 0.7 (0.4–1.1) 0.8 (0.5–1.2) very unlikely to develop AKI later. These data support
with persistent AKI
previous pediatric studies demonstrating that children
AKI, acute kidney injury; CI, confidence intervals; HR, hazard ratio; LOS, length of
stays; PICU, pediatric intensive care unit; pRIFLE, pediatric risk, injury, failure, loss and develop their maximum number of organ failures early in
end-stage renal disease; SCr, serum creatinine. the intensive care unit (ICU) course, an epidemiologic
*Hazard ratio is significantly less than 1.0, indicating that the specified AKI criterion
was associated with a longer length of stay (longer time to discharge).
pattern that differs from adult patients.17,18 In addition,
**P=0.07. patients who did not demonstrate renal function improve-
a
All analyses were also conducted including PRISM score, which is a risk of mortality ment within 48 h of ICU admission were at greater risk of
score, but there was no effect of this factor on results shown.
b
All Cox proportional hazards models fulfilled assumption of proportional hazard receiving RRT, which is similar to studies in adult patients.19
based on Schoenfeld residuals.
c
These data suggest the need to study the effect of early
Admx, admission.
d
Persistent AKI was defined as a lack of improvement in pRIFLE AKI status by 48 h
initiation of aggressive measures to both prevent and treat
after admission. AKI for critically ill children with AKI who do not improve
1032 Kidney International (2007) 71, 1028–1035
A Akcan-Arikan et al.: AKI in critically ill children original article
Table 5 | Association of different criteria for AKI and mortality finding is important since PRISM II does not contain a direct
and the effect of controlling for severity of illness (PRISM II measure of renal function in its calculation. Surprisingly, the
score) prevalence of comorbidities, sepsis or other admission
28-Day mortality diagnoses were no different for patients with vs without
Adjusted OR AKI, even though AKI was associated with mortality,
Adjusted OR (95% CI)a (no suggesting that AKI is an independent risk factor for death.
(95% CI)a PRISM II score) Although this observation is consistent with similar results
AKI during the PICU stay from recent study of RIFLE criteria in critically ill adult
Using SCr + urine criteria patients,20,21 it should be interpreted with caution because
Any AKI during admxb 1.1 (0.3–4.3) 1.4 (0.4–5.1)
our sample size may not have been large enough to detect
pRIFLEmax I or worse 1.9 (.7–5.1) 1.7 (0.6–4.8)
differences between subgroups. Future study should evaluate
Using only SCr criterion the interaction of diagnosis and AKI on mortality risk. When
Any AKI during admxb 2.9 (0.8–10.9) 3.6 (1.0–13.1) PRISM II scores were excluded from analysis, the effect of
pRIFLEmax I or worse 3.0 (1.1–8.1)* 3.8 (1.4–10.0)*
AKI on mortality appeared substantially stronger, stressing
AKI on admission to PICU the importance of controlling for severity of illness when
Using SCr + urine criteria assessing for associations between AKI and mortality.
AKI on admx 1.2 (0.4–3.4) 1.8 (0.7–4.6) Approximately 71% of patients who attained pRIFLE F
AKI pRIFLE I or worse 1.1 (0.4–3.4) 1.7 (0.6–4.8)
on admx
AKI did not receive RRT, which might suggest that the
AKI on admx with 2.6 (0.9–7.9) 3.9 (1.4–10.6)*,d pRIFLE criteria is overly sensitive for identifying severe AKI.
persistent AKIc However, over two-thirds of these patients died within 24 h
AKI pRIFLE I or worse on 2.3 (0.8–7.2) 3.4 (1.2–9.8)*,d of pRIFLEmax F attainment. Had these patients survived, it is
admx with persistent AKI
possible that they would have required RRT. Although these
Using only SCr criterion findings are purely descriptive, they do further indicate that
AKI on admx 1.7 (0.6–5.0) 2.5 (1.0–6.5) patients with severe AKI tend to be more severely ill, and that
AKI pRIFLE I or worse on 1.3 (0.5–4.0) 2.0 (0.7–5.4) future studies evaluating risk factors for initiation of RRT
admx
AKI on admx with persistent 2.6 (0.9–7.9) 3.9 (1.4–10.6)*,d may need to account for censoring owing to death.
AKIc Our evaluation for potential differences in outcome as a
AKI pRIFLE I or worse on 2.3 (0.8–7.2) 3.4 (1.2–9.8)*,d function of attaining AKI by serum SCr vs UOP vs both
admx with persistent AKI
revealed that SCr demonstrated stronger associations with
AKI, acute kidney injury; CI, confidence intervals; LOS, length of stays; OR, odds ratio;
PICU, pediatric intensive care unit; PRISM, Pediatric Risk of Mortality score; pRIFLE,
outcomes. Future studies may be needed to determine if UOP
pediatric risk, injury, failure, loss and end-stage renal disease; SCr, serum creatinine. is in fact necessary for early AKI diagnosis; however, we still
*Po0.05. suggest assessment of both the SCr and UOP measures for
a
In the first column, all odds ratios are adjusted for age, gender, and Pediatric Risk of
Mortality score; in the second column, odds ratios are only adjusted for age and AKI.
gender.
b
Potential limitations of our study include the relatively
Admx, admission.
c
Persistent AKI was defined as no improvement in pRIFLE AKI status by 48 h after
small sample size of 150; however, this cohort comprises the
admission. largest prospective evaluation of pediatric AKI and the only
d
When PRISM II score was removed from the logistic regression model, AKI on study describing AKI in a general PICU population (as
admission with persistent AKI was a significant predictor of mortality (only adjusted
for age and gender). opposed to specific subgroups). Another potential concern is
the use of an assumed baseline eCCl of 100 ml/min/1.73 m2
for patients without a known baseline creatinine, in about
within 24–48 h. Numerous single center and one multicenter one-fourth of the patients. The potential danger of this
study of children requiring continuous renal replacement assumption would be to misdiagnose a patient with AKI
therapy have shown a strong association between the degree based on a relative decrease in eCCl if in fact the patient had
of fluid overload at continuous renal replacement therapy chronic kidney disease. Whether or not such misdiagnosis
initiation and mortality.7–10,16 We suggest that the pRIFLE would lead to unnecessary evaluation or treatment is
criteria may be used to provide guidance as to the potential currently not known, but clinicians should exercise caution
for renal function improvement and may assist in clinical when classifying patients with AKI using pRIFLE, or any
decisions regarding RRT initiation. The high prevalence of system using eCCl change, when a baseline creatinine level is
AKI on admission to PICU in our sample suggests that study unknown. Finally, the decision to initiate RRT was not
of risk factors (clinical and biochemical) for developing AKI, directed by a clinical algorithm as part of this study, but
may need to include data from patients before ICU rather was left to the discretion of the attending nephrologist.
admission. Thus, RRT provision was not a hard end point for this study.
Other secondary outcomes were notable as well. The Because of the dependency of SCr levels on muscle mass, it
presence of RIFLE I or F AKI (defined by SCr criterion only) is extremely difficult to interpret in patients with severely
during admission was associated with an increased risk of reduced muscle mass (such as those with quadriplegia,
mortality, even when adjusted for PRISM II score. This cerebral palsy or other neuromuscular disorders), as is
Kidney International (2007) 71, 1028–1035 1033
original article A Akcan-Arikan et al.: AKI in critically ill children
Table 6 | Pediatric-modified RIFLE (pRIFLE) criteria they fulfilled either UOP (pRIFLEUOP) or SCr (pRIFLECr) criterion
or both (Table 1). At the end of follow-up, patients were classified
Estimated CCl Urine output
according to the maximum pRIFLE stratum achieved within the 14
Risk eCCl decrease by 25% o0.5 ml/kg/h for 8 h days of observation (pRIFLEmax). Additional data collected
Injury eCCl decrease by 50% o0.5 ml/kg/h for 16 h included demographics, PICU admission and discharge diagnoses,
Failure eCCl decrease by 75% or o0.3 ml/kg/h for 24 h or
the presence of chronic illnesses, duration of invasive mechanical
eCCl o35 ml/min/1.73 m2 anuric for 12 h
Loss Persistent failure 44 weeks ventilation, peak mean airway pressure reached, maximal number of
End End-stage renal disease vasoactive medication infusions, and the need for dialysis. PRISM II
stage (persistent failure 43 scores25 were recorded for each patient on PICU admission, as a
months) surrogate marker for severity of illness. Hospital and PICU LOS, and
eCCl, estimated creatinine clearance; pRIFLE, pediatric risk, injury, failure, loss and 28 day and hospital mortality were recorded.
end-stage renal disease.
Comparison of pre-renal azotemia vs acute tubular necrosis
Intravascular fluid depletion is a common cause of increased SCr/
evidenced by our data where patients in the NMd category decreased glomerular filtration rate in the pediatric setting
had mean eCCl of 232 ml/min/1.73 m2. We thus questioned (commonly referred to as ‘pre-renal azotemia’), particularly early
whether the pRIFLE criteria would be less useful in this in the PICU admission. Such patients will often respond solely to
group. The finding that the distribution of AKI severity was fluid repletion, with a return of SCr to baseline values within
almost identical in the NMd group (Figure 2) is highly 24–48 h of fluid resuscitation. On the basis of this rationale, we
suggestive that change in eCCl, as assessed by pRIFLE, is a chose to compare the renal outcome and mortality of patients with
valid way of evaluating AKI in patients with severely reduced early AKI reversal (improving pRIFLE stratum within 48 h of ICU
muscle mass. What is not known is whether progressive admission) vs patients with persistent AKI (no improvement in
muscle – wasting associated with prolonged ICU admis- pRIFLE stratum by 48 h), to serve as a surrogate for pre-renal
azotemia vs acute tubular necrosis.
sion,22,23 which may be associated with declining levels of
SCr independent of renal function, leads to a decrease in the
Statistical analysis
utility of pRIFLE for describing AKI. All statistical analyses were performed using STATAs (StataCorp,
We conclude that multidimensional AKI classification and College Station, TX, USA) software. Continuous variables were
stratification systems, such as pRIFLE, can serve well to expressed as mean7s.d. and median, and categorical variables as
improve understanding of AKI epidemiology and potentially proportions (%). Continuous variables were compared using
optimize evaluation and treatment for AKI in children. analysis of variance and Student’s t-test. w2 and Fisher’s exact tests
Furthermore, as SCr and UOP seem to be late markers of were used for comparison of categorical variables. The outcomes
renal injury, use of classification systems will be essential to examined were mortality, and PICU and hospital LOS. Multiple
assess the potential utility of urine and other serum logistic regression was used to evaluate the presence of AKI and
biomarkers to detect AKI earlier and direct therapies to other relevant variables as risk factors for mortality. Cox-multiple
prevent or mitigate AKI in children prior to a rise in SCr regression was performed to evaluate the effect of AKI on time to
PICU and hospital discharge, accounting for death as a censoring
concentration.
event. Continuous variables with a non-normal distribution were
log-transformed to a normal distribution for use in parametric
MATERIALS AND METHODS analyses. In all analyses, a P-value of o0.05 was considered
We prospectively studied patients admitted to the Texas Children’s statistically significant.
Hospital PICU using pediatric-modified RIFLE (pRIFLE) criteria
(Table 6) to define the clinical course of AKI in the critically ill ACKNOWLEDGMENTS
pediatric patients. All children aged between 30 days to 21 years with We thank Dr Curtis Kennedy for providing us with data from his
respiratory failure (defined as requiring invasive mechanical critical care clinical and laboratory database. A substantial portion of
ventilation) and/or cardiovascular failure (defined as requiring this work was performed, while the second author, M. Zappitelli, was
infusion of vasoactive medication(s)) who had indwelling Foley receiving postdoctoral research fellowship support from the Kidney
catheters were eligible for enrollment. Patients with known end- Research Scientist Core Education and National Training (KRESCENT)
program.
stage renal disease at PICU admission or who were immediately
status-post renal transplant were excluded. The Institutional Review
REFERENCES
Board of Baylor College of Medicine approved the study protocol
1. Bellomo R, Ronco C, Kellum JA et al. Acute renal failure – definition,
and parents/legal guardians provided written informed consent outcome measures, animal models, fluid therapy and information
before patient enrollment. technology needs: the Second International Consensus Conference
UOP and SCr concentrations were recorded daily for up to 14 of the Acute Dialysis Quality Initiative (ADQI) Group. Crit Care 2004; 8:
R204–212.
days and eCCl was calculated using the Schwartz formula.24 For
2. Hui-Stickle S, Brewer ED, Goldstein SL. Pediatric ARF epidemiology
determination of baseline eCCl, the lowest value of SCr in the 3 at a teritary care center from 1999 to 2001. Am J Kidney Dis 2005; 45:
months preceding study enrollment was obtained from the hospital 96–101.
database. If no previous SCr was available, the patient was assumed 3. Moghal NE, Brocklebank JT, Meadow SR. A review of acute renal
failure in children: incidence, etiology and outcome. Clin Nephrol 1998;
to have normal renal function and assigned a baseline eCCl of
49: 91–95.
100 ml/min/1.73 m2, as suggested. Data were reviewed daily and 4. Flynn JT. Choice of dialysis modality for management of pediatric acute
patients were assigned to the appropriate pRIFLE strata (R, I or, F) if renal failure. Pediatr Nephrol 2002; 17: 61–69.
1034 Kidney International (2007) 71, 1028–1035
A Akcan-Arikan et al.: AKI in critically ill children original article
5. Bunchman TE, McBryde KD, Mottes TE et al. Pediatric acute renal failure: 15. Parikh CR, Jani A, Melnikov VY et al. Urinary interleukin-18 is a marker of
outcome by modality and disease. Pediatr Nephrol 2001; 16: 1067–1071. human acute tubular necrosis. Am J Kidney Dis 2004; 43: 405–414.
6. Fargason CA, Langman CB. Limitations of the pediatric risk of mortality 16. Michael M, Kuehnle I, Goldstein SL. Fluid overload and acute renal
score in assessing children with acute renal failure. Pediatr Nephrol 1993; failure in pediatric stem cell transplant patients. Pediatr Nephrol 2004; 19:
7: 703–707. 91–95.
7. Foland JA, Fortenberry JD, Warshaw BL et al. Fluid overload before 17. Proulx F, Fayon M, Farrell CA et al. Epidemiology of sepsis and multiple
continuous hemofiltration and survival in critically ill children: a organ dysfunction syndrome in children. Chest 1996; 109: 1033–1037.
retrospective analysis. Crit Care Med 2004; 32: 1771–1776. 18. Proulx F, Gauthier M, Nadeau D et al. Timing and predictors of death in
8. Goldstein SL, Somers MJ, Baum MA et al. Pediatric patients with multi- pediatric patients with multiple organ system failure. Crit Care Med 1994;
organ dysfunction syndrome receiving continuous renal replacement 22: 1025–1031.
therapy. Kidney Int 2005; 67: 653–658. 19. Levy MM, Macias WL, Vincent JL et al. Early changes in organ function
9. Goldstein SL, Currier H, Graf C et al. Outcome in children receiving predict eventual survival in severe sepsis. Crit Care Med 2005; 33:
continuous venovenous hemofiltration. Pediatrics 2001; 107: 1309–1312. 2194–2201.
10. Gillespie RS, Seidel K, Symons JM. Effect of fluid overload and dose of 20. Hoste EA, Clermont G, Kersten A et al. RIFLE criteria for acute kidney
replacement fluid on survival in hemofiltration. Pediatr Nephrol 2004; 19: injury are associated with hospital mortality in critically ill patients: a
1394–1399. cohort analysis. Crit Care 2006; 10: R73.
11. Chertow GM, Burdick E, Honour M et al. Acute kidney injury, mortality, 21. Hoste EA, Kellum JA. RIFLE criteria provide robust assessment of kidney
length of stay, and costs in hospitalized patients. J Am Soc Nephrol 2005; dysfunction and correlate with hospital mortality. Crit Care Med 2006; 34:
16: 3365–3370. 2016–2017.
12. Goldstein SL, Denfield S, Mott A et al. Mild renal insufficiency is associated 22. Banwell BL, Mildner RJ, Hassall AC et al. Muscle weakness in critically ill
with poor outcome in children with acute decompensated heart failure: children. Neurology 2003; 61: 1779–1782.
evidence for a pediatric cardiorenal syndrome. J Am Soc Nephrol 2005; 16: 23. Deconinck N, Van Parijs V, Beckers-Bleukx G et al. Critical illness myopathy
534A [abstract]. unrelated to corticosteroids or neuromuscular blocking agents.
13. Mishra J, Dent C, Tarabishi R et al. Neutrophil gelatinase-associated Neuromuscul Disord 1998; 8: 186–192.
lipocalin (NGAL) as a biomarker for acute renal injury after cardiac 24. Schwartz GJ, Brion LP, Spitzer A. The use of plasma creatinine
surgery. Lancet 2005; 365: 1231–1238. concentration for estimating glomerular filtration rate in infants, children,
14. Han WK, Bailly V, Abichandani R et al. Kidney injury molecule-1 (KIM-1): a and adolescents. Pediatr Clin North Am 1987; 34: 571–590.
novel biomarker for human renal proximal tubule injury. Kidney Int 2002; 25. Pollack MM, Ruttimann UE, Getson PR. Pediatric risk of mortality (PRISM)
62: 237–244. score. Crit Care Med 1988; 16: 1110–1116.
Kidney International (2007) 71, 1028–1035 1035
You might also like
- In The Womb Movie QuestionsDocument1 pageIn The Womb Movie Questionsapi-376200062No ratings yet
- Biology Standard Level Paper 2: 20 Pages © International Baccalaureate Organization 2014Document17 pagesBiology Standard Level Paper 2: 20 Pages © International Baccalaureate Organization 2014Calvin YangNo ratings yet
- Nihms 300455Document22 pagesNihms 300455Maria Eduarda CardosoNo ratings yet
- Chen 2013Document6 pagesChen 2013malaNo ratings yet
- Study of Clinical Profile of Patient With Acute Kidney DiseaseDocument7 pagesStudy of Clinical Profile of Patient With Acute Kidney DiseaseIJAR JOURNALNo ratings yet
- Diagnosis and Treatment of Acute Kidney Injury in PediatricsDocument13 pagesDiagnosis and Treatment of Acute Kidney Injury in PediatricsagungNo ratings yet
- Early Acute Kidney Injury Predicts Progressive Renal Dysfunction and Higher Mortality in Severely Burned AdultsDocument23 pagesEarly Acute Kidney Injury Predicts Progressive Renal Dysfunction and Higher Mortality in Severely Burned AdultsKartika JuwitaNo ratings yet
- Risk Factors For Mortality in Acute Kidney InjuryDocument6 pagesRisk Factors For Mortality in Acute Kidney Injuryredouane bennaiNo ratings yet
- Paper 2Document15 pagesPaper 2constanzanazarethNo ratings yet
- Hospital Acquired Acute Kidney Injury in Very Elderly Men: Clinical Characteristics and Short Term OutcomesDocument8 pagesHospital Acquired Acute Kidney Injury in Very Elderly Men: Clinical Characteristics and Short Term OutcomesfabiolaNo ratings yet
- Irnf 45 2166531Document9 pagesIrnf 45 2166531Romina Belen Mendez PerezNo ratings yet
- Søvik2019 Article AcuteKidneyInjuryInTraumaPatie PDFDocument13 pagesSøvik2019 Article AcuteKidneyInjuryInTraumaPatie PDFamal.fathullahNo ratings yet
- Vesconi 2009Document14 pagesVesconi 2009Nguyễn Đức LongNo ratings yet
- Article 1576845020 PDFDocument5 pagesArticle 1576845020 PDFFatima Habib JajjaNo ratings yet
- Kead 582Document2 pagesKead 582Alberto Sifuentes GiraldoNo ratings yet
- Emerick Et Al 1999 HepatologyDocument8 pagesEmerick Et Al 1999 Hepatologyagustinus salimNo ratings yet
- Ajkd 2023 Mortality and Major Adverse Kidney Events AkiDocument12 pagesAjkd 2023 Mortality and Major Adverse Kidney Events AkiAlexandra TofanNo ratings yet
- 467 2018 Article 4128Document8 pages467 2018 Article 4128yuwengunawan7No ratings yet
- INCIDENCE_RISK_FACTORS_AND_OUTCOME_OF_ACUTE_KIDNEYDocument5 pagesINCIDENCE_RISK_FACTORS_AND_OUTCOME_OF_ACUTE_KIDNEYalexfuma76No ratings yet
- Acute Kidney Injury in Dengue Virus Infection: MinireviewDocument5 pagesAcute Kidney Injury in Dengue Virus Infection: MinireviewIndra IhsanNo ratings yet
- Study of Etiology, Clinical Profile and Outcome of Acute Kidney (AKI) in Medical Intensive Care UnitDocument4 pagesStudy of Etiology, Clinical Profile and Outcome of Acute Kidney (AKI) in Medical Intensive Care UnitDavid Al HavizNo ratings yet
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyNo ratings yet
- Catheter Cardiovasc Interv 2021 May 27 Romeo FJDocument8 pagesCatheter Cardiovasc Interv 2021 May 27 Romeo FJFernando SousaNo ratings yet
- AKI Child W NS 2018Document4 pagesAKI Child W NS 2018Indah Nur LathifahNo ratings yet
- Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-AnalysisDocument19 pagesGlobal Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-AnalysisAngel ViolaNo ratings yet
- 10 1016@j Ajem 2020 01 046Document7 pages10 1016@j Ajem 2020 01 046Nurul Huda KowitaNo ratings yet
- 10 1016@j Ajem 2020 01 046Document7 pages10 1016@j Ajem 2020 01 046Nurul Huda KowitaNo ratings yet
- Afección Renal en PediatriaDocument12 pagesAfección Renal en PediatriaKarla Mariela Rodriguez LeonNo ratings yet
- Chawla 2011Document9 pagesChawla 2011samuel anchondoNo ratings yet
- 154-The Frequency and Aetiology of Repeated Kidney Injury Episodes Determine The Degree of Renal DamageDocument2 pages154-The Frequency and Aetiology of Repeated Kidney Injury Episodes Determine The Degree of Renal DamageCarlos Martinez SalgadoNo ratings yet
- Pathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaDocument7 pagesPathological Profile and Recovery Rate in Patients With Drug-Induced Acute Kidney Injury: A Retrospective Study From North-East IndiaIJAR JOURNALNo ratings yet
- AKI - Acute Kidney Injury Classification RIFLE and AKIN CriteriaDocument6 pagesAKI - Acute Kidney Injury Classification RIFLE and AKIN CriteriaIntan Siti HulaimaNo ratings yet
- Evidence-Based Nephrology: Rakesh Malhotra and Edward D. SiewDocument25 pagesEvidence-Based Nephrology: Rakesh Malhotra and Edward D. SiewnudhakoNo ratings yet
- Chronic Kidney Disease Increases Risk For Venous ThromboembolismDocument6 pagesChronic Kidney Disease Increases Risk For Venous ThromboembolismAndi WijayaNo ratings yet
- The Impact of Malnutritional Status On Survival in Elderly Hemodialysis PatientsDocument5 pagesThe Impact of Malnutritional Status On Survival in Elderly Hemodialysis PatientsTika MahelsaNo ratings yet
- Pi Is 2590059522001637Document3 pagesPi Is 2590059522001637carlos-laguadoNo ratings yet
- Global Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-AnalysisDocument18 pagesGlobal Prevalence of Chronic Kidney Disease - A Systematic Review and Meta-AnalysisMellya RizkiNo ratings yet
- En A11v22n2Document9 pagesEn A11v22n2RizkyaFarhanNo ratings yet
- Acute Kidney Injury in Children: Incidence, Awareness and Outcome-A Retrospective Cohort StudyDocument8 pagesAcute Kidney Injury in Children: Incidence, Awareness and Outcome-A Retrospective Cohort Studycantika larasatiNo ratings yet
- Fragasso2018 AKI TRRDocument14 pagesFragasso2018 AKI TRRLeydi johana Rodriguez alzateNo ratings yet
- The Paradoxical Protective Effect of Liver Steatosis On Severity and Functional Outcome of Ischemic StrokeDocument7 pagesThe Paradoxical Protective Effect of Liver Steatosis On Severity and Functional Outcome of Ischemic StrokewinnerfromparisNo ratings yet
- Chronic Kidney Disease in Children and AdolescentsDocument16 pagesChronic Kidney Disease in Children and AdolescentsFernanda SierraNo ratings yet
- Development and Validation of A Risk Prediction Model For End-Stage Renal Disease in Patients With Type 2 DiabetesDocument13 pagesDevelopment and Validation of A Risk Prediction Model For End-Stage Renal Disease in Patients With Type 2 DiabetesMarta CarolNo ratings yet
- Acute Kidney InjuryDocument10 pagesAcute Kidney InjuryMaya_AnggrainiKNo ratings yet
- Original Investigation A Meta-Analysis of The Association of Estimated GFR, Albuminuria, Age, Race, and Sex With Acute Kidney InjuryDocument11 pagesOriginal Investigation A Meta-Analysis of The Association of Estimated GFR, Albuminuria, Age, Race, and Sex With Acute Kidney Injurysiska tiaraNo ratings yet
- Prevalence of Chronic Kidney Disease in The United States: Original ContributionDocument10 pagesPrevalence of Chronic Kidney Disease in The United States: Original ContributionadityaNo ratings yet
- 10 1148@radiol 2019192094Document9 pages10 1148@radiol 2019192094msaenz.medNo ratings yet
- Terlipressin Is Superior To Noradrenaline PDFDocument11 pagesTerlipressin Is Superior To Noradrenaline PDFfcodoc321No ratings yet
- JCM 09 00619 v2Document14 pagesJCM 09 00619 v2Medicina FamiliarNo ratings yet
- Does Neutrophil To Lymphocyte Ratio Demonstrate deDocument5 pagesDoes Neutrophil To Lymphocyte Ratio Demonstrate deArifin Perdana IstimansyahNo ratings yet
- Izumita 2020Document5 pagesIzumita 2020AsimaJulianaSiregarNo ratings yet
- Nerjm SesionDocument12 pagesNerjm SesionjorgeNo ratings yet
- Chronic Kidney Disease Is Associated With A Higher 90-Day Mortality Than Other Chronic Medical Conditions in Patients With SepsisDocument8 pagesChronic Kidney Disease Is Associated With A Higher 90-Day Mortality Than Other Chronic Medical Conditions in Patients With Sepsisida ayu agung WijayantiNo ratings yet
- Samrt 2Document9 pagesSamrt 2Zai RojasNo ratings yet
- 1 s2.0 S1051227616301789 MainDocument7 pages1 s2.0 S1051227616301789 MainResearch OfficeNo ratings yet
- ACKD in DogsDocument9 pagesACKD in DogsGreomary Cristina MalaverNo ratings yet
- Markers of Disease Severity and Prolonged Length of Stay For Paediatric Diabetic KetoacidosisDocument6 pagesMarkers of Disease Severity and Prolonged Length of Stay For Paediatric Diabetic KetoacidosisSSR-IIJLS JournalNo ratings yet
- Endocan and CKDDocument8 pagesEndocan and CKDharimanNo ratings yet
- Research Article: Incidence and Risk Factors For Early Acute Kidney Injury in Nonsurgical Patients: A Cohort StudyDocument9 pagesResearch Article: Incidence and Risk Factors For Early Acute Kidney Injury in Nonsurgical Patients: A Cohort StudyAbdul RahimNo ratings yet
- Econo 3Document7 pagesEcono 3Abeer AbdullahNo ratings yet
- (10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenDocument6 pages(10920684 - Neurosurgical Focus) Predictors of Outcome of Subdural Empyema in ChildrenFatima RamirezNo ratings yet
- Recent Advances of Sarcopenia and Frailty in CKDFrom EverandRecent Advances of Sarcopenia and Frailty in CKDAkihiko KatoNo ratings yet
- AsanSM IIIDocument18 pagesAsanSM IIIRaj BharathNo ratings yet
- Lec 3 Safety ProgramDocument41 pagesLec 3 Safety ProgramZamirah PaningasanNo ratings yet
- PHED 10032 Individual, Dual, and Combative SportsDocument52 pagesPHED 10032 Individual, Dual, and Combative SportsMicmic CalivaNo ratings yet
- Blood Circulatory SystemDocument5 pagesBlood Circulatory SystemAathifa ThowfeekNo ratings yet
- Mattu Recent Cardiol Articles Youve Got To Know Icem 2023 LitupdatesDocument29 pagesMattu Recent Cardiol Articles Youve Got To Know Icem 2023 Litupdates85tq5nhsqbNo ratings yet
- Poisonous Plants With Special Reference To PakistanDocument85 pagesPoisonous Plants With Special Reference To Pakistanmughni5000100% (2)
- Mohsin Khan Safety Officer CVDocument2 pagesMohsin Khan Safety Officer CVMohsin KhanNo ratings yet
- C.K.Pithawala College of Engineering & TechnologyDocument6 pagesC.K.Pithawala College of Engineering & TechnologyParth AnajwalaNo ratings yet
- ReferencesDocument1 pageReferencesAlex 27No ratings yet
- Grade 8 PE Quarter 1Document35 pagesGrade 8 PE Quarter 1Anngela Arevalo BarcenasNo ratings yet
- Nursing Care Plan 5 Altered Nutrition: Less Than Body RequirementsDocument9 pagesNursing Care Plan 5 Altered Nutrition: Less Than Body Requirementsdbryant010183% (24)
- Lab Man Module 3 MidtermsDocument29 pagesLab Man Module 3 MidtermsAnne LaydaNo ratings yet
- Risk For Falls NCPDocument1 pageRisk For Falls NCPandayaannedhesireeNo ratings yet
- Weight Tracking Scale With Progress BarDocument2 pagesWeight Tracking Scale With Progress BarivanzeaNo ratings yet
- Kala Ko Nawala Paiyak Na KoDocument6 pagesKala Ko Nawala Paiyak Na KoNicole PadualNo ratings yet
- A6013 v1 SD Influenza Ag BrochureDocument2 pagesA6013 v1 SD Influenza Ag BrochureYunescka MorenoNo ratings yet
- Case TonsilitisDocument38 pagesCase TonsilitisSandip VaghelaNo ratings yet
- FSSC - FSSC 22000 V6 - 2023Document43 pagesFSSC - FSSC 22000 V6 - 2023posteraq374100% (1)
- Isolation and Molecular Characterization of Salmonella Enterica, Escherichia Coli O157-H7 and Shigella Spp. From Meat and Dairy Products in EgyptDocument6 pagesIsolation and Molecular Characterization of Salmonella Enterica, Escherichia Coli O157-H7 and Shigella Spp. From Meat and Dairy Products in EgyptAffan GaffarNo ratings yet
- GROUP 1 - Legal Considerations of Maternal Child Practice (Report)Document6 pagesGROUP 1 - Legal Considerations of Maternal Child Practice (Report)A C100% (2)
- Vocabulary Reading Grammar Listening Speaking Writing: Study HelplineDocument2 pagesVocabulary Reading Grammar Listening Speaking Writing: Study HelplineMDNo ratings yet
- Degree of Axis Correction in Valgus High Tibial OsteotomyDocument9 pagesDegree of Axis Correction in Valgus High Tibial Osteotomy洪侊增No ratings yet
- Laudit, Arnel Z.Document30 pagesLaudit, Arnel Z.Japs De la CruzNo ratings yet
- Bura - Stephane - Beyond ElizaDocument79 pagesBura - Stephane - Beyond ElizaphiloNo ratings yet
- Nama Puskesmas/Fasyankes/Pos Kabupaten/Kota Provinsi:: UPT Puskesmas Talaga: Majalengka: Jawa BaratDocument20 pagesNama Puskesmas/Fasyankes/Pos Kabupaten/Kota Provinsi:: UPT Puskesmas Talaga: Majalengka: Jawa BaratNoeNuraeniNo ratings yet
- Article Installation Guideline: - F07904 Net Insert Gondola SmallDocument3 pagesArticle Installation Guideline: - F07904 Net Insert Gondola SmallmohammadNo ratings yet
- Parish Safeguarding PolicyDocument2 pagesParish Safeguarding Policyapi-525213434No ratings yet
- Covid-19 Vaccine Trial Protocols ReleasedDocument2 pagesCovid-19 Vaccine Trial Protocols ReleasedChafik MegherbiNo ratings yet