Professional Documents
Culture Documents
Beneficial Actions of Nitrates in Cardiovascular Disease
Beneficial Actions of Nitrates in Cardiovascular Disease
Uploaded by
Wilson BotelhoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Beneficial Actions of Nitrates in Cardiovascular Disease
Beneficial Actions of Nitrates in Cardiovascular Disease
Uploaded by
Wilson BotelhoCopyright:
Available Formats
Beneficial Actiohs of Nitrates in
Cardiovascular Disease
Jonathan Abrams, MD
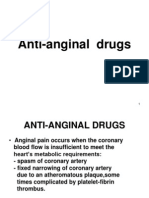
Nitroglycerin and the long-acting nitrates have been with lower systolic and diastolic pressures. These
used in cardiovascular medicine for > 100 years. changes are caused by a redistribution of the circu-
Nitrates are widely utilized for the various angina1 fating blood volume away from the heart to the ve-
syndromes and are also used in congestive heart fail- nous capacitance system, with a fall in venous return
ure and patients with left ventricular dysfunction. The to the heart. The afterload or arterial effects of nitrates
potential mechanisms for relief of myocardial isch- are also useful in decreasing myocardial oxygen con-
emia with nitrates are multiple. The nitrovasodilators sumption. Considerable evidence confirms a variety of
are a related group of drugs that result in the forma- mechanisms whereby nitrates increase coronary
tion of nitric oxide (NO) within vascular smooth mus- blood flow, including epicardial coronary artery di-
cle cells. NO stimulates the enzyme guanylate cyclase, lation, stenosis enlargement, enhanced collateral size
which results in increases in cyclic guanosine mono- and flow, improvement of endothelial dysfunction,
phosphate and vasodilation. In the presence of ath- and prevention or reversal of coronary artery vaso-
erosclerosis, endothelial dysfunction is ubiquitous and constriction. These effects help increase nutrient cor-
associated with decreased NO availability, probably onary blood flow to zones of myocardial ischemia.
due to increased destruction of NO by free radical Recent data with the nitroglycerin patch confirm that
anions. Nitrovasodilators, including the nitrates, sup- myocardial ischemia is decreased after nitrate admin-
ply exogenous NO to the vascular wall and improve istration. Nitroprusside, another nitrovasodilator, is a
the vasodilator state. When nitrates are administered, commonly used intravenous agent for lowering arte-
endothelial-dependent stimuli cause relaxation rather rial pressure and left ventricular filling pressure. This
than constriction in the setting of endothelial dys- drug is highly effective for the treatment of acute or
function. Nitrates also have antiplatelet effects, and severe hypertension and congestive heart failure.
recent evidence confirms that these drugs decrease However, there are data suggesting that nitroprusside
platelet aggregation and thrombosis formation. This may be deleterious in the presence of acute myocar-
may play an important role in the therapy of acute dial ischemia, perhaps by shunting blood away from
unstable myocardial ischemia, including unstable an- zones of jeopardized myocardial blood flow. There-
gina and myocardial infarction. Nitrate hemodynamic fore, nitroprusside cannot be recommended to treat
effects have been long known. They are primarily myocardial ischemia; intravenous nitroglycerin should
modulated through a decrease in myocardial work be used in this context.
that results from smaller cardiac chambers operating (Am J Cardiol 1996;77:3 1C-37C)
itroglycerin (NTG) and the long-acting ni- of action of the nitrates as they relate to the clinical
N trates are used by physicians for a variety of
cardiovascular conditions (Table I). The primary
syndromes for which these agents are used.
role of these drugs is in the prophylaxis and treat- NITRATES AND MYOCARDIAL
ment of myocardial ischemia in subjects with cor- ISCHEMIA
onary atherosclerosis. Less well known is their ef- The initial utilization of NTG in medicine was for
ficacy in ameliorating the signs and symptoms of acute attacks of angina pectoris. This indication re-
congestive heart failure and left ventricular dys- mains the most important role for these agents. Thus,
function. In intravenous formulation, NTG is used sublingual or oral spray NTG or, less commonly,
to treat severe hypertension and to control blood sublingual isosorbide dinitrate (ISDN) remain the
pressure in the operating room during certain sur- worldwide gold standards for relief of angina1 chest
gical procedures. Important advantages of the ni- pain. Intelligent preadministration of these drugs be-
trates relates to their many mechanisms of action; fore anticipated physical activity or emotional stress
their proven efficacy in many cardiovascular dis- is an important but infrequently utilized approach to
eases; and their reassuring safety and adverse ef- the prevention of angina. Most of the known mech-
fect profile. The dominant negatives of nitrate ther- anisms of nitrate action can be invoked as being im-
apy include headache and nitrate tolerance. The portant in preventing or eliminating myocardial isch-
latter is discussed in detail elsewhere in this sym- emia. It is likely that different actions are more (or
posium. Table II outlines the various mechanisms less) important in individual patients, in whom there
are a variety of ways for myocardial ischemia to be
From the Department of Medicine [Cardiology), University of New triggered. Several recent reports of transdermal NTG
Mexico School of Medicine, Albuquerque, New Mexico.
Address for re rints. Jonathan Abrams, MD, Department of Med-
in patients with chronic stable angina demonstrate
icine, University o P New Mexico School of Medicine, 22 1 1 lomas the potency and efficacy of nitrates in alleviating
Boulevard NE, Albuquerque, New Mexico 8713 1. exercise-induced myocardial ischemia.“* Although
0 1996 by Excerpto Medica, Inc. 0002.9149/96/$15.00 31c
All rights reserved. PII SOOO2-9149(96)00186-5
TABLE I Clinical Indications for Nitrates
Condition Comments
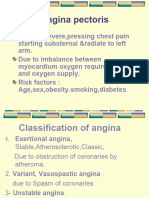
l Acute attacks of angino pectoris Highly effective
l Prophylaxis of chronic stable angina Comparable efficacy to calcium and beta blockers. Tolerance o problem
l Unstable ongino Intravenous nitroglycerin (NTG) very useful
l Acute myocardial infarction
-Control of chest pain and ischemia Often effective: use sublingual, intravenous NTG. Caution to avoid hypotension
-Hypertension, acute heart failure Very useful; intravenous or high-dose topical
-Routine 24-48 hour infusion of little positive data; consider in large anterior myocordial infarction (MI)
intravenous NTG
l Post-MI left ventricular remodeling Limited positive data. Uncertain benefits
l Chronic congestive heart failure Useful adjunct to angiotensinconverting enzyme (ACE) inhibitors-can use with hydrolozine.
Consider for all symptomatic subjects on ACE inhibitors and digitalis
l Acute heart failure/pulmonary edema Highly effective-especially intravenous NTG
l Hypertension Useful in intravenous formulation. limited positive doto in systolic hypertension of the elderly
in oral formulotion
TABLE II Mechanism of Action of Nitrates: Relationship to Clinical Indications*
Acute attacks and prophylaxis of stable angina pectoris Decreased myocordiol oxygen consumption
-Decreased LV dimension
-Decreased LV filling pressure
-Decreased LV systolic pressure
-Decreased vascular impedence
Increased coronary blood supply
-Epicardial coronary artery dilation
-Coronary stenosis enlorgement
-Improved coronary endotheliol function
-Dilaton of coronary collaterals or small distal coronary vessels
Unstable angina Same OS above, plus ontiplotelet antithrombotic action
Acute myocardial infarction Same as above, plus antiplatelet ontithrombotic action
Congestive heart failure
Systolic dysfunction Decreased LV and RV dimensions (few data in congestive heart failure)
Decreased LV and RV filling pressure
Decreased orterial pressure
Decreased systemic vascular resistance
Decreased PA and RA pressure
Improved endothelial function
Coronary artery disease patients: increased coronary blood flow
Diastolic dysfunction Decreased mitral regurgitation
Decreased LV filling pressure
Hypertension Decreased systolic blood pressure
Decreased systemic vascular resistance
Decreased LV prelood, uncertain importance
* LV = left ventricular; PA = pulmonary artery; RA = right otrial; RV = right ventricular.
these studies do not provide insight as to the pre- rently under investigation. This discussion will em-
cise mechanisms of NTG action in reducing myo- phasize NTG, nitroprusside, ISDN, and isosorbide-
cardial ischemia in a given subject, they carefully 5mononitrate (ISMN) .
document and quantitate the magnitude of im- Cellular mechanisms: NTG, as the prototype com-
provement in ischemia reduction that is induced by pound, is a short-lived agent with a half-life of sev-
the drug (Figure l).’ Another recent study con- eral minutes. It is rapidly converted to NO at or
firms earlier work suggesting that nitrates improve near the plasma membrane of the vascular smooth
nutrient coronary blood flow to regional zones of muscle cell. For years it was believed that NTG
myocardial ischemia.3 goes through a stepwise denitration process re-
sulting in the release to NO, but it appears that
NTG directly forms either NO itself or a nitrosy-
MECHANISMS OF ACTION OF THE lated entity known as a nitrosothio14 (Figure 2).
NITROVASODIIATORS The conversion of NTG (and the other nitrates) to
The nitrovasodilators are a related group of drugs NO is enzymatic. The enzyme has been partially
that result in the formation and release of nitric oxide characterized; of potential importance, a thiol moi-
(NO) from the parent molecule (Table III). A va- ety forms part of the enzyme structure.” Nitrate ox-
riety of metabolic or biochemical steps exist for these ide or nitrosothiols formed from NTG activate the
agents; some (the organic nitrates) are enzymatically cytoplasmic enzyme guanylate cyclase (Figure 2).
converted to NO. Nitroprusside and molsidomine This catalyzes the formation of cyclic guanosine
form NO directly. Many new NO donors are cur- monophosphate from guanosine diphosphate. Cy-
32C THE AMERICAN jOURNA1 OF CARDIOLOGY@ VOL. 77 MAY 30, 1996
clic guanosine monophosphate, a second messen-
ger, induces a shift in intracellular calcium within
the sarcoplasmic reticulum, resulting in a transient
fall in intracellular calcium and subsequent vaso-
relaxation.6 Nitroprusside and molsidomine pro-
duce NO in a nonenzymatic fashion; nitrate toler-
ance does not appear to be a problem with these
compounds.
Endothelial function: It has been known for some
time that arterial vasomotor function is predomi-
nantly related to phasic release of a NO-like sub-
stance from endothelial cells. NO itself (or a close
intermediate) is produced in endothelial cells in
response to vascular shear stress or a variety of
receptor-mediated stimuli (e.g., serotonin, thrombin,
histamine). This process, which is mediated by I SmJDvl mJDY2 mum1 muDv2
a putative endothelium-derived relaxing factor
FIGURE 1. Nitroglycerin patch efficacy in reducing exercise-in-
(EDW, ’ is responsible for vasodilation of large duced ischemia in patients with angina. Mean and individual po-
arteries and the microcirculation. Prostacyclin, a tient changes in exercise-induced left ventricular (1~) perfusion
cyclic adenosine monophosphate-mediated vaso- defects from study 1 (baseline placebo patch) to study 2 (active
dilator, is also involved in endothelial cell regu- nitrate versus lacebo patch). Nitroglycerin patch therapy signifi-
lation of vasodilation. cantly reduc fxr the mean quantitative thallium perfusion defect
size compared with placebo therapy (‘p = 0.04). Bold lines indi-
EDRF (NO) is involved in other important cate the 7 patients receiving active patch therapy who reduced
functions of the endothelium, including antiplate- their perfusion defect size by 2 10% (absolute). (Reprinted with
let and antithrombotic activity and processes that permission from I Am Co// Car&o/.‘)
impede or suppress smooth muscle cell prolifera-
tion and atherosclerosis. Although most available
data regarding EDRF involves its vasodilating ac- TABLE III Nitrovasodilators
tions, many believe that normal or abnormal EDRF Exogenous
production or degradation is intimately related to Currently available in the United States
fundamental characteristics of the vascular wall it- Nitroglycerin
self, including smooth muscle cell function and lsosorbide dinitrate
Isosorbide5mononitrate
atherogenesis.’ Sodium nitroprusside
Endothelial dysfunction and nitrates: Abnormal en- Not available or approved in the United States
dothelial function has been well documented in cor- Nicorandil (also a K’ channel blocker)
onary atherosclerosis. Most of this research involves Molsidomine (converted to SIN-l, the active moiety, in the
endothelial modulation of vasomotor function and liver)
Nitrosothiols [research only)
documents impaired vasodilator responses to a va- Endogenous
riety of stimuli in the presence of abnormal endothe- Endothelium-derived relaxing factor (nitric oxide or closely
lial function in atherosclerotic blood vessels. The related compound)
dominant finding in such studies is a derangement of
maximal or normal dilator capacity. In the presence
of overt atherosclerosis, and also in apparently nor- exogenous endothelial-dependent stimuli (e.g., ace-
mal arteries in subjects with diabetes, high choles- tylcholine, reactive hyperemia) are proportional to
terol, hypertension, or heart failure, endothelial va- the degree of atherosclerosis. Coronary stenosis con-
sodilator capacity is impaired.’ The administration striction is an advanced form of endothelial dys-
of NTG or other nitrates results in normal or near- function; it is likely that transient decreases in the
normal vasodilation, presumably because the nitrate caliber of atherosclerotic lesions are important trig-
directly supplies NO to the vascular endothelium and gers of myocardial ischemia.
smooth muscle in the media.*-” It is believed that Nitrates, through their capacity to provide NO di-
endothelial dysfunction in humans is often caused rectly to the arterial media, are categorized as en-
by accelerated destruction of EDRF and NO, prob- dothelial independent vasodilator agents.‘-” Thus,
ably due in part to the presence of excess oxygen- NTG, nitroprusside, and the other organic nitrates
free radical activity.” result in predictable near-normal coronary vasodi-
Patients with an elevated low density cholesterol, lation in the presence of endothelial dysfunction.
hypertension, or a history of smoking often have an This has led to the concept that nitrates act as ex-
impairment of endothelial vasodilator responsive- ogenous EDRF-like agents, supplying or replenish-
ness. Further, the presence of overt atherosclerosis ing NO to the vessel wall when normal NO avail-
is an important marker that endothelial dysfunction ability is diminished by disease processes.*-” This
is present; the greater the severity of the atheroscle- construct points to the potentially unique role of ni-
rotic process, the more the impairment of endothe- trovasodilators in patients with vascular disease, hy-
lial-modulated vasodilation. Abnormal responses to pertension, or heart failure, states often associated
A SYMPOSIUM: NITRATES IN HEART FAllURE 33C
ENOOTHELIUM VASCULAR SMOOTH MUSCLE
FIGURE 2. Nitrovasodilators, endo-
thelium-dependent vasodilators, and
vascular smooth muscle relaxation.
EDRF = endothelium-derived relaxing
factor; GC = guanylate cyclase; GTP
= guanosine triphosphate; NO = ni-
tric oxide; R’SH and RSH = 2 distinct
1
NO
pools of intracellular
groups; R’SSR’ = disulfide
sulfhydryl
roups.
(Re rinted with permission !r om Ko-
RSH ,I wa Puk E, Fung H-L. Pharmacology
S-nitrosothiol’
J and phannacokinetics of nitrates. In:
(RSNO) - RSNO:: Abrams J, Pepine C, Thadani U, eds.
. . Medical Therapy of lschemic Heart
Endothelium Disease: Nitrates, Beta Blockers, and
-dependent *EDRF Calcium Antagonists. Boston: Little,
vosodi lotors Brown, 1992: 152.)
I /
*
with NO penia. Of interest, in the presence of normal decreased coronary artery spasm or vasoconstriction,
or intact endothelial function, NTG appears to have particularly at or near the site of intimal disruption.
a lessened vasodilator capability, perhaps in part re- These nitrate effects, in addition to a nitrate related
lated to continuous basal release of NO by the en- decrease in myocardial oxygen consumption and in-
dothelial cell layer decreasing the potential maximal crease in nutrient coronary blood flow, should be
vasorelaxation induced by nitrate-derived NO. salutary in such patients.
In any case, the concept of exogenous EDRF
(NO) supplied by NTG and the organic nitrates, is HEMODYNAMIC ACTIONS
useful, and helps explain the efficacy of these rather Nitrates dilate veins, arteries, and arterioles
old-fashioned drugs in patients with vascular abnor- through the previously described cascade of intra-
malities. 8-‘“,‘2,13Prevention or reversal of coronary cellular events leading to NO production and acti-
artery and atherosclerotic lesion vasoconstriction, l3 vation of cyclic guanosine monophosphate (Figure
or overt coronary spasm, are more readily explained 2). In the smaller, distal vessels of the microcircu-
in the context of NO supplementation from an ex- lation, NTG and the organic nitrates appear to have
ogenous pharmaceutic NO donor. little vasodilator capacity, perhaps because the en-
Nitrates and thrombosis: It has been long recog- zyme responsible for nitrate bioconversion to NO is
nized that NTG and other organic nitrates have an not present in these vessels.9 Veins take up nitrates
antiaggregatory effect on platelet function. The re- more avidly than arteries, and venodilation is pro-
sults of early experiments were controversial, how- nounced at lower plasma concentration of nitrate.
ever, and the actual importance of nitrate antiplatelet Nitroprusside is a potent vasodilator; at relatively
action has been clouded by uncertainty. In recent low infusion rates, nitroprusside is more active than
years, however, considerable evidence has become NTG in dilating arteries and arterioles. Further, ni-
available supporting a robust role for these agents in troprusside relaxes the microcirculation and is more
interfering with platelet function and subsequently likely to decrease coronary resistance than NTG (see
decreasing platelet thrombotic activity. A variety of below ) .
animal and human studies have confirmed important The classic view of nitrate hemodynamic actions
nitrate antiplatelet actions in this regard.14-17 relates to pronounced venodilation with an increase
Although it is difficult to attribute a beneficial in blood volume in the venous capacitance beds. In
contribution of nitrates in chronic stable angina re- effect, nitrates induce an autotransfusion of blood
lated to platelet and antithrombotic actions, it is ob- away from the heart and lungs to the splanchnic and
vious that a significant anti-platelet-thrombotic ef- peripheral circulations. Less blood returns to the
fect could be important in patients with unstable right heart; preload falls, and cardiac output and
angina or acute myocardial infarction. These so- stroke volume typically decrease. NTG is a potent
called syndromes of acute myocardial ischemia are and reliable agent for decreasing left and right ven-
associated with focal and perhaps generalized en- tricular filling pressure in the normal heart, as well
dothelial dysfunction; platelets help initiate the as in subjects with congestive heart failure and high
thrombotic cascade leading to intraluminal or mural pulmonary capillary pressure. Concomitant nitrate
thrombus and ongoing platelet-thrombin activation, actions on pulmonary and aortic compliance and im-
which would be favorably affected by nitrate anti- pedance result in decreasesin systolic pressure in the
platelet. activity. Such nitrate actions would lead to central circulations. Thus, pulmonary artery and aor-
34C THE AMERICAN JOURNAL OF CARDIOLOGY@ VOL. 77 MAY 30, 1996
FIGURE 3. Hemodynamic changes
(A) in hemodynamic variables after
bolus intravenous nitroglycerin in
normal (group 1) (n = 9; E./E, < 1)
(solid bars), hypertensive ( roup 2a)
(n = 9; E,/E,,> 1; ejection L ction
>40%) (hatched bars), and heart fail-
ure (group 2b) (n = 9; E./E.,> 1;
ejection fraction <40%) (open bars)
subiects. Prelood changes, defined OS
o decrease in end-diastolic volume
(EDV) ore greatest in roup 1 and in-
termediate in group 2% . Afterload
changes defined OS a decrease in ef-
fective aerial elastance (E,), are
greatest in groups 20 and 2b. In-
creases in stroke volume (Sv) consis-
tent with predominant afterlwd L
effects ore seen in groups 2a and 2b. Systo llic blood pressure (BP) decreased in all groups but to a lesser extent in group 2b.
*p ~0.05 versus group 1. tp <0.05 versus group 20. (Reprinted with permission from J Am co// Cardio/,‘q
tic systolic pressure falls with a relatively small de- becomes quite clear when one recognizes the im-
cline in diastolic pressures. Peripheral arterial vaso- portant physiologic effects of nitrates in this condi-
dilation contributes to an overall reduction in arterial tion. Nitrates are beneficial in heart failure, although
impedance and blood pressure. In the normal heart large amounts of these drugs are usually necessary
decreased left and right ventricular preload contrib- to achieve desired hemodynamic goals.
ute to the decrease in cardiac output and blood pres-
sure. CORONARY BLOOD SUPPLY
Nitroprusside is more potent in the arterial cir- NTG, and presumably the other nitrates, have sig-
culation than NTG on a per milligram basis and de- nificant actions on the coronary circulation (Table
creases arterial pressure to a greater degree than II). These are less well recognized than nitrate ef-
NTG. At high infusion rates and plasma concentra- fects on peripheral veins and arteries. The coronary
tions, however, intravenous NTG becomes more po- vasodilating actions of the nitrates probably play a
tent as a dilator of arteries and arterioles, and the significant role in the prevention and relief of myo-
drug’s hemodynamic effects become comparable to cardial ischemia in many patients with coronary ar-
nitroprusside. The decreases in left ventricular and tery disease. Although epicardial coronary artery va-
right ventricular preload and afterload translate into sodilation has been long recognized, and beneficial
smaller ventricular chamber size, with lower intra- nitrate effects on coronary collateral size and flow
cardiac systolic and diastolic pressures. These mul- are well known, several mechanisms of action of ni-
tiple actions result in decreased diastolic and systolic trates in the coronary bed have only recently been
left ventricular wall stress, and lower myocardial en- confirmed. These include the salutary effects on cor-
ergy demands.” In the presence of normal left ven- onary endothelial dysfunction, discussed before,8-‘0
tricular systolic function, stroke volume and cardiac coronary atherosclerotic stenosis dilation or enlarge-
output usually decline following NTG administra- ment, I3 and increased regional coronary blood flow
tion. However, in the setting of left ventricular sys- to viable myocardium downstream from a total cor-
tolic compromise, increased systemic vascular resis- onary artery obstruction via collateral and distal ves-
tance, or an elevated afterload, nitrates allow the left sel vasodilation.*’
ventricle to empty more efficiently, and stroke vol- It is quite difficult if not impossible to dissect out
ume may increase due to nitrate “unloading” ef- the benefits of NTG vis-a-vis decreasedmyocardial ox-
fects. I9 Nitroprusside is even more potent in this re- ygen consumption versus increased regional or nutrient
gard. A recent study suggests that the effects of NTG myocardial blood flow in a given patient with coronary
on left ventricle dimensions and stroke volume may
be, in part, determined by the underlying state of the
circulation. Thus, nitrate hemodynamic actions in the TABLE IV Hemodynamic Effects of Nitrates in the Normal
normal heart are different from that in the impaired Circulation and in Congestive Heart Failure with Left Ventricular
left ventricle with contractile dysfunction, or in hy- Contractile Dysfunction
pertensive patients who have an increased resting af- Normal
terload (Figure 3 ) .l9 LV CHF
Several differences in nitrate hemodynamic ef-
Blood pressure Decrease No change or modest decrease
fects are demonstrable in different physiologic states Heart rate Increase No change
(Table IV). It is important for the clinician to be LV filling pressure Decrease Decrease
aware of the diversity of nitrate actions related to the Stroke volume Decrease No change or modest increase
underlying status of the circulation. Further, the rel- CHF = congestive heart failure; LV = left ventricular.
evance of nitrate therapy in congestive heart failure
A SYMPOSIUM, NITRATES IN HEART FAILURE 35c
lieve that nitroprusside should be avoided in the set-
ting of acute myocardial ischemia so as to revent a
possible “coronary steal” phenomenon27l2ii Present
guidelines do not include nitroprusside as an anti-
ischemic agent in acute myocardial infarction or un-
stable angina.29However, for patients with myocar-
dial ischemia complicated by hypertension or acute
heart failure, nitroprusside remains an effective and
rapid acting nitrovasodilator of considerable potency
Late Treatment and safety so long as central aortic hypotension is
avoided. In the absence of acute ischemia, nitro-
--O--O--,,’
prusside is an ideal drug for treatment of acute pul-
monary edema and decompensated heart failure.
NITRATE TOLERANCE
70 ’ ’ ’ ’ ’ ’ ’ ’ ’ ’ ’ ’ ’ This subject is considered elsewhere in this sup-
0 I 2 3 4 5 6 7 6 9 IO II plement. However, many nitrate actions are attenu-
12 13
WEEKS ated in the presence of nitrate tolerance. Nitrates
must and should be prescribed in a tolerance-avoid-
FIGURE 4. Intravenous nitroprusside in acute myocardial infarc- ance manner, with an appropriate nitrate-free inter-
tion. Approximately 400 patients in each group, nitroprusside val and pulsed dosing regimen. However, when in-
versus placebo. Cumulative percentage of patients surviving after
early treatment (within 9 hours of onset of acute myocardial in-
travenous NTG is given for acute myocardial
farction) and late treatment (later than 9 hours). (Reprinted with infarction or unstable angina, one should not rou-
permission from N Engl I Med.25) tinely stop the infusion in an effort to reverse or pre-
vent the appearance of nitrate tolerance. Rebound
vasoconstrictor forces and the withdrawal of favor-
artery disease.Perhaps both actions come into play in able hemodynamic action are potentially hazardous
most subjects. Nevertheless, the recognition that ni- consequences of abrupt cessation of intravenous
trates improve coronary blood flow to regions of myo- NTG in this setting. Intravenous NTG should be ta-
cardium subtended by a coronary stenosis or obstruc- pered slowly in patients with acute myocardial in-
tion represents an enhanced understanding of these farction or ischemia while the subject is being
valuable agents.Prevention or reversal of coronary ep- switched to oral therapy.
icardial artery and microcirculatory vasoconstriction as
well as stenosis vasodilation may be quite important in NITRATE FORMULATIONS
certain individuals. At present, NTG, ISDN, and ISMN are the only
organic nitrates that can be recommended. The
INTRAVENOUS NITRATES: choice of agent depends on a number of factors, in-
NITROGLYCERIN AND cluding the drug’s pharmacokinetic profile, available
NITROPRUSSIDE dosing or delivery systems, physician preference,
Sodium nitroprusside is a more potent arterial va- and cost. There are no reliable data to suggest im-
sodilator than NTG, and nitroprusside has an impor- portant differences among these compounds in clin-
tant dilating effect on the coronary microcirculation. ical effectiveness, potency, or likelihood of tolerance
Although the hemodynamic profile of nitroprusside induction. Further, it is presumed (but unproven)
helps explain its greater efficacy in lowering blood that the beneficial endothelial and peripheral circu-
pressure or in the therapy in decompensated conges- latory effects and direct coronary actions are similar
tive heart failure, 2’ serious questions have been among the available nitrate formulations. The side
raised as to whether nitroprusside is completely safe effect profiles appear to be comparable. Fortunately,
in the presence of coronary artery disease. It is pos- for patients and physicians, NTG and the organic
sible that the dilator actions of nitroprusside on the nitrates remain reliable and predictable pharmaceutic
resistance vessels of the coronary circulation may compounds that have multiple beneficial effects and
allow for an unwanted diversion of coronary blood considerable efficacy in clinical medicine.
flow away from zones of potential or actual myo-
cardial ischemia subtended by a tight coronary ste-
nosis. This concept has some basis in older animal 1. Mahmarian JJ, Fenimore N, Marks GF, et al. Transdermal nitroglycerin patch
and human data during acute infarction.22-24 Further, atherapy reduces the extent of exercise-induced myocardial &hernia: results of
double-blind, placebo-controlled trial using quantitative thallium-201-tomog-
a multicenter trial in acute myocardial infarction raphy. J Am Co11 Cardiol 1994;24:25-32.
demonstrated an increased mortality in patients 2. Parker JO, Amies MH, Hawkinson RW, et al. Intermittent transdermal nitro-
glycerin therapy in angina pectoris. Clinically effective without tolerance or
given a 48-hour nitroprusside infusion, treated rebound. Circulation 1995;91: 1368-1374.
within the first 9 hours (Figure 4) .25Another trial, 3. Fallen EL, Nabmia SC, Scheffel A, et al. Redistribution of myocardial blood
however, demonstrated a survival benefit with an flow with typical nitroglycerin in patients with coronary arterial disease. Cir-
culation 1995;91:1381-1388.
early nitroprusside infusion in acute infarction.26 Al- 4. Fung H-L, Chug S-J, Baer JA, Chong S, Kowaluk EA. Biochemical mech-
though this issue is not resolved, many experts be- anism of organic nitrate. action. Am J Cardiol 1992;70( suppl):4B- IOB.
36C THE AMERICAN JOURNAL OF CARDIOLOGY@ VOL. 77 MAY 30, 1996
5. Seth P, Fung H-L. Biochemical characterization of a membrane-bound en- 18. Greenberg H, Dwyer EM, Jameson AG, et al. Effects of nitroglycerin on
zyme responsible for generating nitric oxide from nitroglycerin in vascular the major determinants of myocardial oxygen consumption. An angiographic
smooth muscle cells. Biochem Phannacol 1993;641148 I- 1488. and hemodynamic assessment. Am .I Cardiol 1975;36:426-432.
6. Kukovetz WR, Holzmann S, Schmidt K. Cellular mechanisms of action ther- 19. Haber HL, Simek CL, Bergin JD, et al. Bolos intravenous nitroglycerin
apeutic nitric oxide donors. Eur Heart J 1991;12(suppl E):16-24. predominately reduces afterload in patients with excessive arterial &stance. J
7. Furchgott RF, Zawadski JV. The obligatory role of endothelial cells in the Am Co11 CardWl I993;22:25 l-257.
relaxation of arterial smooth muscle to acetylcholine. Nature 1980;228:373- 20. Pupita G, Maseri A, Kaski JC, et al. Myocardial ischemia caused by distal
376. coronary artery constriction in stable angina pectoris. N Erzgl J Med
8. Luscher TF. Endothelium-derived nitric oxide: the endogenous nitrovasodi- 1990;323:514-520.
later in the human cardiovascular system. Eur Heart J 1991;12( suppl E) :2- 21. Miller RR, Vismara LA, Zelis R, Amsterdam EA, Mason UT. Clinical use
1 I. of sodium nitroprusside in chronic ischemic heart disease: effect on peripheral
9. Harrison DG, Bates JN. The nitrovasodilators: new ideas about old drugs. vascular resistance and venoos tone on ventricular volume, pump and mechan-
Circulation 1993;87:1461-1467. ical performance. Circulation 1975;51:328-335.
10. Bassenge E, Zanzinger J. Nitrates in different vascular beds, nitrate toler- 22. Mann T. Cohn P, Holman BL, et al. Effect of nitroprusside on regional
il”CC%, and interactions with endothelial function. Am .I Cardiol myocardial blood flow in coronary artery disease. Results in 25 patients and
1992;70(suppl):23B-298. comparison with nitroglycerin. Circulation 1978;57:732-736.
11. Ohara Y, Peterson TE, Sayegh HS, Subramanian RR, Wilcox JN, Harrison 23. Chiariello M, Gold HK, Lainbach RC, et al. Comparison between the effects
DF. Dietary correction of hypercholesterolemia in the rabbit normalizes enoth- of nitropmsside and nitroglycerin on ischemic injury during acute myocardial
elial superoxide anion production. Circulation 1995;92:898-903. infarction. Circulation 1976;54:766-773.
12. Rafflenbeul W, Bassenge E, Lichtien P. Competition between endothelium- 24. Macho P, Vatner SF. Effects of nitroglycerin and nitroprusside on large and
dependent and nitroglycerin-induced coronary vasodilation. 2 Kardiol small coronary vessels in conscious dogs. Circulation 1981;64: llOl- 1107.
1989;78(suppl 2):45-47. 25. Cohn JN, Franciosa JA, Francis GS, et al. Effect of short-term infusion of
13. Ludmer PL, Selwyn AP, Shook TL, et al. Paradoxical vasoconstriction sodium nitroprusside on mortality rate in acute myocardial infarction compli-
induced by acetylcholine atherosclerotic arteries. N Engl JMed 1986;315:1046- cated by left ventricular failure. N Engl J Med 1982;306: 1129- 1135.
1051. 26. Dumer JD, Lie KI, van Chapelle FJL, Durrer D. Effect of sodium nitro-
14. Loscalzo J. Antiplatelet and antithrombotic effects of organic nitrates. Am prosside on mortality in acute myocardial infarction. N Engl J Med
J Cardiol 1992;7O(suppl): 18B-22B. 1982;306:1121-1128.
15. Lam JYT, Chesebro JH, Fuster V. Platelets, vasoconstriction and nitro- 27. Flaherty JT, Magee PA, Gardner TL, Potter A, Macallister NP. Comparison
glycerin during arterial wall injury: a new antithrombotic role for an old drug. of intravenous nitroglycerin and sodium nitroprosside for treatment of acute
Circulation 1988;78:712-716. hypertension developing after coronary artery bypass surgery. Circulation
16. Diodati J, Theroux P, Latour J-G, Lacoste L, Lam JY, Water D. Effects of 1982;66: 1072-1077.
nitroglycerin at therapeutic doses on platelet aggregation in unstable angina 28. Flaherty JT. Role of nitrates in acute myocardial infarction. In: Abrams J, Pepine
pectoris and acute myocardial infarction. Am J Cardiol 1990;66:683-688. C, Thadani U, eds. Medical Therapy of Ischemic Heart Disease: Nitrates, Beta Block-
17. Felts JD, Stamler J, Loscalzo J. Intravenous nitroglycerin infusion inhibits ers, and C&urn Antagonists. Boston: Little, Brown, 1992:309--328.
cyclic blood tlow responses caused by periodic platelet thrombus formation in 29. ACC/AHA Task Force. ACC/AHA guidelines for the early management
stenosed canine coronary arteries. Circularion 1991:83:2122-2127. of patients with acme myocardial infarction. Circulation 1990;82:664-707.
A SYMPOSIUM: NITRATES IN HEART FAllURE 37C
You might also like
- Antianginal Drugs Lecture NotesDocument10 pagesAntianginal Drugs Lecture NotesPrincewill SeiyefaNo ratings yet
- NitratesDocument21 pagesNitratesGAURI CHATURVEDINo ratings yet
- Nitrates in The Management of Chronic Coronary Syndrome - UpToDateDocument18 pagesNitrates in The Management of Chronic Coronary Syndrome - UpToDateijmp7No ratings yet
- Nitrates in The Management of Stable Angina Pectoris - UpToDateDocument20 pagesNitrates in The Management of Stable Angina Pectoris - UpToDateacesacesNo ratings yet
- Management of Systemic and Pulmonary HypertensionDocument5 pagesManagement of Systemic and Pulmonary HypertensionUCI COVID Pediátrico HNGAINo ratings yet
- IsdnDocument5 pagesIsdnWidya JelitaNo ratings yet
- NIH Public Access: Author ManuscriptDocument17 pagesNIH Public Access: Author ManuscriptNurmaLitaIINo ratings yet
- Cardiac PharmDocument6 pagesCardiac PharmJohn SmithNo ratings yet
- Antianginal and Antiischemic DrugsDocument18 pagesAntianginal and Antiischemic DrugsNaveen KumarNo ratings yet
- Treatment of Decompensated Heart FailureDocument15 pagesTreatment of Decompensated Heart FailuremagreaNo ratings yet
- Antianginal 171115034620Document34 pagesAntianginal 171115034620benny christantoNo ratings yet
- Drugs Used in Myocardial InfarctionDocument53 pagesDrugs Used in Myocardial InfarctionSandeep KannegantiNo ratings yet
- DR Triadhy Nugraha-Nitrates in Stable Coronary Artery DiseaseDocument23 pagesDR Triadhy Nugraha-Nitrates in Stable Coronary Artery DiseaseIgdrsui BoyolaliNo ratings yet
- Antianginal Drugs.. Prof. Dr. Adeeb Al-ZubaidyDocument19 pagesAntianginal Drugs.. Prof. Dr. Adeeb Al-ZubaidySara AbbasNo ratings yet
- 13.angina and Anti-Anginal DrugsDocument60 pages13.angina and Anti-Anginal Drugsbilalsiddique5365No ratings yet
- Acute Management of Unstable Angina and non-ST Segment Elevation Myocardial InfarctionDocument8 pagesAcute Management of Unstable Angina and non-ST Segment Elevation Myocardial InfarctionsavitageraNo ratings yet
- Pharmacotherapy of CADDocument27 pagesPharmacotherapy of CADhams elaklamNo ratings yet
- Case AnalysisDocument5 pagesCase AnalysisCharm TanyaNo ratings yet
- Anti-Angina DrugsDocument29 pagesAnti-Angina DrugsEbenezer SamuelNo ratings yet
- Emtyaz AntianginalDocument43 pagesEmtyaz AntianginalMuhammed MuhsinNo ratings yet
- Module 3.3 - CardioDocument12 pagesModule 3.3 - CardioCatherine Sinen ObinqueNo ratings yet
- Anti Anginal DrugsDocument26 pagesAnti Anginal DrugsAtharva PuranikNo ratings yet
- Anti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistDocument25 pagesAnti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistpradeephdNo ratings yet
- Cardioprotection by Opening of The K Channel in Unstable AnginaDocument7 pagesCardioprotection by Opening of The K Channel in Unstable Angina111111111111111111132222No ratings yet
- NIH Public Access: Nitroglycerin Use in Myocardial Infarction Patients: Risks and BenefitsDocument13 pagesNIH Public Access: Nitroglycerin Use in Myocardial Infarction Patients: Risks and BenefitsPratama InsaniNo ratings yet
- Pharmacology AnginaDocument28 pagesPharmacology AnginaalijanmarwatNo ratings yet
- Angina AssignmentDocument7 pagesAngina AssignmentvictoriaNo ratings yet
- Anti AnginalDocument2 pagesAnti AnginaltheamaciasNo ratings yet
- Antinanginal DrugsDocument43 pagesAntinanginal DrugsHUZAIFA YAMAANNo ratings yet
- Anesthetic Management of The Hypertensive Patient: Part II: Continuing Education in Honor of Norman Trieger, DMD, MDDocument8 pagesAnesthetic Management of The Hypertensive Patient: Part II: Continuing Education in Honor of Norman Trieger, DMD, MDFitri Aesthetic centerNo ratings yet
- Anti - Anginal MedicationDocument41 pagesAnti - Anginal MedicationShine StephenNo ratings yet
- NitratesDocument5 pagesNitrateshlau2uciNo ratings yet
- PharmaAntianginal DrugsDocument175 pagesPharmaAntianginal DrugsNidal AbboudNo ratings yet
- Should The Angiotensin Ii Antagonists Be Discontinued Before Surgery?Document20 pagesShould The Angiotensin Ii Antagonists Be Discontinued Before Surgery?yakuta_doc100% (2)
- Angina ManagmentDocument27 pagesAngina ManagmentAliImadAlKhasakiNo ratings yet
- Angina, Debkantha Gope PDFDocument9 pagesAngina, Debkantha Gope PDFdebkantha gopeNo ratings yet
- Angina PectorisDocument24 pagesAngina PectorisAshwin Raghav SankarNo ratings yet
- Angina Pectoris: Arun Dubey M.D. 2019Document18 pagesAngina Pectoris: Arun Dubey M.D. 2019mus zaharaNo ratings yet
- Subarachnoid Hemorrhage: An UpdateDocument24 pagesSubarachnoid Hemorrhage: An UpdateMaria de los Angeles ZamoranoNo ratings yet
- Pharmacology of Ischemic Heart DiseaseDocument51 pagesPharmacology of Ischemic Heart DiseaseabenezergebrekirstosNo ratings yet
- Angina PectorisDocument24 pagesAngina PectorisAyu PurbaNo ratings yet
- Chap132 PDFDocument4 pagesChap132 PDFKarina Dwi SwastikaNo ratings yet
- Hypertensionaha 109 133819Document4 pagesHypertensionaha 109 133819Zainal AbidinNo ratings yet
- Increased Nitric Oxide Production in Heart FailureDocument2 pagesIncreased Nitric Oxide Production in Heart Failureحسين مهديNo ratings yet
- L3 Angina - Dr. Yagub S SalehDocument7 pagesL3 Angina - Dr. Yagub S Salehnusaiba.alobaidyNo ratings yet
- Lectures Combined CardiologieDocument143 pagesLectures Combined CardiologiedocsNo ratings yet
- DR - Datten Bangun MSC - SPFK & DR - Tri Widyawati Msi, PHD Dept - Farmakologi & Therapeutik Fak - Kedokteran Usu MedanDocument50 pagesDR - Datten Bangun MSC - SPFK & DR - Tri Widyawati Msi, PHD Dept - Farmakologi & Therapeutik Fak - Kedokteran Usu MedanHabib Al KahfiNo ratings yet
- 0068C PDFDocument7 pages0068C PDFIntan Kusuma DewiNo ratings yet
- Intravenous NitroglycerinDocument8 pagesIntravenous NitroglycerinmagreaNo ratings yet
- Antianginal DrugsDocument25 pagesAntianginal DrugsTamta BokoveliNo ratings yet
- ABC of Heart FailureDocument12 pagesABC of Heart FailureJane PowerNo ratings yet
- AnginaDocument16 pagesAnginaMc_Lopez_1761No ratings yet
- Anti AnginaDocument16 pagesAnti AnginaAik NoeraNo ratings yet
- Antianginal Drugs (C.23)Document18 pagesAntianginal Drugs (C.23)Shervin AnggraeniNo ratings yet
- Anti Anginal DrugsDocument33 pagesAnti Anginal DrugsMuhammad AhmadNo ratings yet
- Antianginal Drugs DR Hussam 2023Document12 pagesAntianginal Drugs DR Hussam 2023ManWol JangNo ratings yet
- Digoxin in Heart Failure and Cardiac Arrhythmias: New Drugs, Old DrugsDocument5 pagesDigoxin in Heart Failure and Cardiac Arrhythmias: New Drugs, Old DrugsAbidia KamilNo ratings yet
- Unit 5 - Med. Chem. IIDocument4 pagesUnit 5 - Med. Chem. IIaaryasharmamrtNo ratings yet
- Bpharm 5 Sem Industrial Pharmacy 1 bp502t 2020Document1 pageBpharm 5 Sem Industrial Pharmacy 1 bp502t 2020Amol TupeNo ratings yet
- Pharma Made EasyDocument11 pagesPharma Made EasyLory Lyn100% (1)
- Ulcerative Colitis Diagnosis and ManagementDocument12 pagesUlcerative Colitis Diagnosis and ManagementCarmen MaldonadoNo ratings yet
- NCCN Pain ManagementDocument14 pagesNCCN Pain ManagementcoooleNo ratings yet
- Chapter 9 - Adrenergic AgonistsDocument4 pagesChapter 9 - Adrenergic AgonistsJoseph Campos SanchezNo ratings yet
- NHSCT/18/1204 Anaemia and Vitamin Supplementation in PregnancyDocument22 pagesNHSCT/18/1204 Anaemia and Vitamin Supplementation in Pregnancyana mariaNo ratings yet
- Drugs Used in Respiratory DiseasesDocument11 pagesDrugs Used in Respiratory DiseasesDH DipuNo ratings yet
- Najlaa Exam 12-03-17Document17 pagesNajlaa Exam 12-03-17Abdul SalamNo ratings yet
- Psychopharma NotesDocument3 pagesPsychopharma Noteszh4hft6pnzNo ratings yet
- Nursing Care Plan: Rationale: Increasing Paco2 andDocument14 pagesNursing Care Plan: Rationale: Increasing Paco2 andSean Menard FloresNo ratings yet
- Drugs Affecting Gastrointestinal Motility Drugs Affecting Gastrointestinal MotilityDocument34 pagesDrugs Affecting Gastrointestinal Motility Drugs Affecting Gastrointestinal MotilityJojo JustoNo ratings yet
- Efpia White-Paper Public-ProcurementDocument18 pagesEfpia White-Paper Public-ProcurementKaryofyllis TsiakitzisNo ratings yet
- Templet RKO FOPI 2021Document270 pagesTemplet RKO FOPI 2021Karin ArinciaNo ratings yet
- Complex Protrombina Huvh 01 10Document11 pagesComplex Protrombina Huvh 01 10Santiago Rodriguez MoralesNo ratings yet
- DMT of MNDDocument39 pagesDMT of MNDthelegend 2022No ratings yet
- Diana Anderson, D M Conning - Experimental Toxicology-Royal Society of Chemistry (1993) PDFDocument584 pagesDiana Anderson, D M Conning - Experimental Toxicology-Royal Society of Chemistry (1993) PDFJuanNo ratings yet
- Antibiotics in Endodontics - A Concise Review: Dr. Ramaprabha Balasubramaniam and Dr. Srilekha JayakumarDocument7 pagesAntibiotics in Endodontics - A Concise Review: Dr. Ramaprabha Balasubramaniam and Dr. Srilekha JayakumarMoslem CompanyNo ratings yet
- Manual of Policies and Procedures Center For Drug Evaluation and Research MAPP 5017.2 Rev. 1Document1 pageManual of Policies and Procedures Center For Drug Evaluation and Research MAPP 5017.2 Rev. 1Md. Yousuf BhuiyanNo ratings yet
- Acute Kidney Injury at The Neurocritical CareDocument10 pagesAcute Kidney Injury at The Neurocritical CareSamNo ratings yet
- Major Depression Disorder in Adults: A Review of AntidepressantsDocument8 pagesMajor Depression Disorder in Adults: A Review of AntidepressantsYaying BualuangNo ratings yet
- Adjunctive Amantadine Treatment For Aggressive Behavior in Children A Series of Eight CasesDocument4 pagesAdjunctive Amantadine Treatment For Aggressive Behavior in Children A Series of Eight Casesleorocha06No ratings yet
- Comparison of Benzyl Benzoate Lotion Versus Permet PDFDocument7 pagesComparison of Benzyl Benzoate Lotion Versus Permet PDFNicoleta PlesaNo ratings yet
- Tesamorelin Is Used To Stimulate GH and Its Lipolytic Effects, Helping To Decrease TheDocument19 pagesTesamorelin Is Used To Stimulate GH and Its Lipolytic Effects, Helping To Decrease TheGeraldine PatayanNo ratings yet
- HospitalDocument116 pagesHospitalKhadija KamranNo ratings yet
- Microemulsion 141121085401 Conversion Gate02 PDFDocument51 pagesMicroemulsion 141121085401 Conversion Gate02 PDFdinaNo ratings yet
- Zalameda ANSDocument32 pagesZalameda ANSNicole ObispoNo ratings yet
- Surgical Nursing Calculation PracticesDocument2 pagesSurgical Nursing Calculation PracticesJéssica OinonenNo ratings yet
- Phytochemical and Ethno-Pharmacological Profile of Crataeva Nurvala Buch-Hum (Varuna) : A ReviewDocument7 pagesPhytochemical and Ethno-Pharmacological Profile of Crataeva Nurvala Buch-Hum (Varuna) : A ReviewSalsabila IndrianiNo ratings yet
- Types of Bonds in Drug Receptor InteractionDocument12 pagesTypes of Bonds in Drug Receptor InteractionMirumbi Kefa MomanyiNo ratings yet