Professional Documents
Culture Documents
2009 12 6b292ce7
2009 12 6b292ce7
Uploaded by
AbdallahCopyright:
Available Formats
You might also like
- High-Yield Product FinalDocument99 pagesHigh-Yield Product FinalChristianNo ratings yet
- Eros & The Pineal - A Layman's Guide To Cerebral Solataire - Albert MostDocument7 pagesEros & The Pineal - A Layman's Guide To Cerebral Solataire - Albert Mosttyson100% (1)
- Get Tested: STD Vs Sti STD Vs StiDocument2 pagesGet Tested: STD Vs Sti STD Vs StiJanna May Villafuerte100% (2)
- EPQ On The Mental Health SystemDocument15 pagesEPQ On The Mental Health SystemAdam100% (2)
- Genioplasty Oral SurgeryDocument45 pagesGenioplasty Oral SurgeryFourthMolar.com100% (2)
- Omega-6/Omega-3 Ratio and Brain-Related Functions: Shlomo YehudaDocument20 pagesOmega-6/Omega-3 Ratio and Brain-Related Functions: Shlomo YehudaJonas SkadbergNo ratings yet
- Omega-3 DHA and EPA For Cognition, Behavior, and Mood: Clinical Findings and Structural-Functional Synergies With Cell Membrane PhospholipidsDocument21 pagesOmega-3 DHA and EPA For Cognition, Behavior, and Mood: Clinical Findings and Structural-Functional Synergies With Cell Membrane PhospholipidsHerlina HasibuanNo ratings yet
- Omega-3 Fatty Acids and Their Role in Central Nervous SystemDocument17 pagesOmega-3 Fatty Acids and Their Role in Central Nervous Systempokolio silvaNo ratings yet
- Natural Brain Enhancers Nutrients That RDocument52 pagesNatural Brain Enhancers Nutrients That RMaksymNo ratings yet
- Summary of Clinical Research For LaminineDocument10 pagesSummary of Clinical Research For LaminineDocAxi Maximo Jr AxibalNo ratings yet
- Difference Between Vegetable and Animal Omega 3 Fatty AcidsDocument3 pagesDifference Between Vegetable and Animal Omega 3 Fatty AcidsnicodipietroNo ratings yet
- MontoyaParra2018 Article StatusOfNutrientsImportantInBrDocument20 pagesMontoyaParra2018 Article StatusOfNutrientsImportantInBrYohana RumahorboNo ratings yet
- Neuromedicterranea Omega 3 y Salud MentalDocument13 pagesNeuromedicterranea Omega 3 y Salud MentalDORIS JANETHNo ratings yet
- Nutrients: A Nutrient Combination That Can Affect Synapse FormationDocument10 pagesNutrients: A Nutrient Combination That Can Affect Synapse Formationlina ningdyarNo ratings yet
- The Role of Omega-3 Fatty Acids in Mood DisordersDocument9 pagesThe Role of Omega-3 Fatty Acids in Mood DisordersARESS RIPNo ratings yet
- Dyall Epadpadha R Fan15Document16 pagesDyall Epadpadha R Fan15võ thị lệNo ratings yet
- PGM 2009 11 2083Document10 pagesPGM 2009 11 2083TASSIA CHRISTINNE BRITO COELHONo ratings yet
- 1 s2.0 S0304394023002033 MainDocument14 pages1 s2.0 S0304394023002033 MainAntonio Luiz PereiraNo ratings yet
- What Are Essential Fatty Acids?: Shorter Telomeres Are Associated With Bad Diet, Diseases and Early DeathDocument25 pagesWhat Are Essential Fatty Acids?: Shorter Telomeres Are Associated With Bad Diet, Diseases and Early DeathDavid James PNo ratings yet
- 6 Vol. 10 Issue 11 Nov 2019 IJPSR RA 11687Document7 pages6 Vol. 10 Issue 11 Nov 2019 IJPSR RA 11687Charles OnunekwuNo ratings yet
- 135 - Possible MecanismsDocument19 pages135 - Possible MecanismsEduardo BacelarNo ratings yet
- Nootropics SupplementsPDFDocument7 pagesNootropics SupplementsPDFnitinsharma12345wweNo ratings yet
- Morgese and Trabace, 2016Document20 pagesMorgese and Trabace, 2016Mohsin ZafarNo ratings yet
- Food For MoodDocument15 pagesFood For MoodDaniele LimaNo ratings yet
- Transdermal Selegiline PatchesDocument14 pagesTransdermal Selegiline PatchessujithaNo ratings yet
- 5.supplementation With Flaxseed Oil Rich in Alpha-Linolenic Acid Improves Verbal Fluency in Healthy Older AdultsDocument12 pages5.supplementation With Flaxseed Oil Rich in Alpha-Linolenic Acid Improves Verbal Fluency in Healthy Older Adultsvõ thị lệNo ratings yet
- Importance of Fatty Acids in Physiopathology of Human Body: Katalin Nagy and Ioana-Daria TiucaDocument20 pagesImportance of Fatty Acids in Physiopathology of Human Body: Katalin Nagy and Ioana-Daria TiucaStefan Tri PrabhataNo ratings yet
- Endocrine SystemDocument6 pagesEndocrine SystemynaNo ratings yet
- Chemicals in The Brain: Nervous System (Ms Socky)Document26 pagesChemicals in The Brain: Nervous System (Ms Socky)Jovelyn Morales JosolNo ratings yet
- Fotuhi 2009Document13 pagesFotuhi 2009peri umardianaNo ratings yet
- BiomedicineDocument10 pagesBiomedicinevrish Dhwaj AshwlayanNo ratings yet
- Qualia Mind Energy ShotDocument4 pagesQualia Mind Energy ShotPaulo Henrique Haß FilhoNo ratings yet
- Biological Theories of AgingDocument29 pagesBiological Theories of AgingdulceRN67% (3)
- Omega-3 Polyunsaturated Fatty Acids in The Treatment of SchizophreniaDocument7 pagesOmega-3 Polyunsaturated Fatty Acids in The Treatment of SchizophreniaPedro PriorNo ratings yet
- Dietary Essential Fatty Acids and Brain Function A Developmental Perspective On MechanismsDocument9 pagesDietary Essential Fatty Acids and Brain Function A Developmental Perspective On MechanismsBarbara Sakura RiawanNo ratings yet
- Phosphodiesterase WhatisinanenzymeDocument13 pagesPhosphodiesterase WhatisinanenzymentondojuniorchinoisNo ratings yet
- Sirtuin 5-Mediated Lysine Desuccinylation Protects Mitochondrial Metabolism Following Subarachnoid Hemorrhage in MiceDocument11 pagesSirtuin 5-Mediated Lysine Desuccinylation Protects Mitochondrial Metabolism Following Subarachnoid Hemorrhage in MicenicolaspanppNo ratings yet
- Protein Kinase Inhibition By: - 3 Fatty AcidsDocument9 pagesProtein Kinase Inhibition By: - 3 Fatty AcidsStepss StepsNo ratings yet
- Essential & Non-Essential Fatty AcidsDocument4 pagesEssential & Non-Essential Fatty AcidsVikash KushwahaNo ratings yet
- Essential Fatty Acid and Human BrainDocument4 pagesEssential Fatty Acid and Human BrainDwi Rahayu FitriawatiNo ratings yet
- 2021 Essential Brain Hygiene EguideDocument26 pages2021 Essential Brain Hygiene EguideHector SolarNo ratings yet
- The Role of Eicosanoids in The Brain: Review ArticleDocument9 pagesThe Role of Eicosanoids in The Brain: Review ArticleDr. Kaushal Kishor SharmaNo ratings yet
- Folic Acid Exerts Antidepressant Effects by Upregulating - JÁ FOIDocument8 pagesFolic Acid Exerts Antidepressant Effects by Upregulating - JÁ FOICamila VasquesNo ratings yet
- Review: Taurine: A "Very Essential" Amino Acid: Harris Ripps, Wen ShenDocument14 pagesReview: Taurine: A "Very Essential" Amino Acid: Harris Ripps, Wen Shenit's me ebeth tjhinNo ratings yet
- NeurotransmitterDocument7 pagesNeurotransmitterSweety DhillonNo ratings yet
- pjbf7k8s0j0.1Document1 pagepjbf7k8s0j0.1terje.yngvar.traneNo ratings yet
- Copy of Jacob Oakden Draft 2Document14 pagesCopy of Jacob Oakden Draft 2api-740081698No ratings yet
- Early Intervention Psych - 2021 - Susai - Omega 3 Fatty Acid in Ultra High Risk Psychosis A Systematic Review Based OnDocument14 pagesEarly Intervention Psych - 2021 - Susai - Omega 3 Fatty Acid in Ultra High Risk Psychosis A Systematic Review Based OnMitchel Cordova LoaizaNo ratings yet
- Nihms 123081Document15 pagesNihms 123081Jose PerezNo ratings yet
- Human Physiology An Integrated Approach 7Th Edition Silverthorn Solutions Manual Full Chapter PDFDocument36 pagesHuman Physiology An Integrated Approach 7Th Edition Silverthorn Solutions Manual Full Chapter PDFcleopatrabanhft1vh7100% (14)
- 414 1685 1 PBDocument13 pages414 1685 1 PBMuhammad Sona KhanNo ratings yet
- Implications of Lipid Biology For The Pathogenesis of SchizophreniaDocument12 pagesImplications of Lipid Biology For The Pathogenesis of SchizophreniaScheckyNo ratings yet
- Home: Correspondence:: Ala N Aragon's Research Review - July 2015)Document26 pagesHome: Correspondence:: Ala N Aragon's Research Review - July 2015)Andra SpatarNo ratings yet
- Research Paper On Protein StructureDocument6 pagesResearch Paper On Protein Structurezyfepyfej0p2100% (1)
- Omega-3 Literature ReviewDocument8 pagesOmega-3 Literature Reviewn1dihagavun2100% (1)
- Insights from Ayurveda for translational stem cellDocument7 pagesInsights from Ayurveda for translational stem cellRavi P ShaliwalNo ratings yet
- Acid Linoleic (Não)Document6 pagesAcid Linoleic (Não)Tuyết Nhỏ Thiên ThầnNo ratings yet
- Nutricion y EsquizofreniaDocument13 pagesNutricion y EsquizofreniacelliasttNo ratings yet
- Animal Physiology Midterm QuestionsDocument10 pagesAnimal Physiology Midterm QuestionsDani GutiérrezNo ratings yet
- Topographical Distribution of The Human Brain To Plukenetia Volubilis-Based Omega-3,6,9 Enriched Egg ConsumptionDocument13 pagesTopographical Distribution of The Human Brain To Plukenetia Volubilis-Based Omega-3,6,9 Enriched Egg ConsumptionIAES IJAINo ratings yet
- 100 Brain Optimization TipsDocument3 pages100 Brain Optimization TipsBrad Richardson100% (1)
- Organic ChemistryDocument236 pagesOrganic ChemistryAbdallahNo ratings yet
- Role of Long-Chain Polyunsaturated Fatty Acids in Infant NutritionDocument4 pagesRole of Long-Chain Polyunsaturated Fatty Acids in Infant NutritionAbdallahNo ratings yet
- Effect of Long-Chain Polyunsaturated Fatty Acids in Infant Formula On Problem Solving at 10 Months of AgeDocument4 pagesEffect of Long-Chain Polyunsaturated Fatty Acids in Infant Formula On Problem Solving at 10 Months of AgeAbdallahNo ratings yet
- 2020 11 07 - 214806Document4 pages2020 11 07 - 214806AbdallahNo ratings yet
- Final TCS ModuleDocument24 pagesFinal TCS Modulemae cudalNo ratings yet
- Brfo193 Radiotherapy Dose Fractionation Third-Edition PDFDocument137 pagesBrfo193 Radiotherapy Dose Fractionation Third-Edition PDFMed MedNo ratings yet
- Developmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsDocument71 pagesDevelopmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsvadimmadanNo ratings yet
- Sexually Transmitted InfectionDocument16 pagesSexually Transmitted InfectionSonam ChaudharyNo ratings yet
- The Interaction of Herbs and DrugsDocument17 pagesThe Interaction of Herbs and DrugsCarleta StanNo ratings yet
- Manila Police District (MPD) As of January 2022: Action PNCO, DSTU OIC, Training Section C, DPRMDDocument15 pagesManila Police District (MPD) As of January 2022: Action PNCO, DSTU OIC, Training Section C, DPRMDShan Dave TupasNo ratings yet
- Heart Failure Clinical Records DatasetDocument14 pagesHeart Failure Clinical Records Datasetpanca saputraNo ratings yet
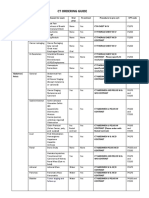
- CT Ordering Guide: Tumor Staging and Follow UpDocument2 pagesCT Ordering Guide: Tumor Staging and Follow UpanonNo ratings yet
- Immunology 9Th Edition Male David Full ChapterDocument61 pagesImmunology 9Th Edition Male David Full Chaptertodd.wimbush786100% (10)
- Eye Essentials Cataract Assessment Classification and Management PDFDocument245 pagesEye Essentials Cataract Assessment Classification and Management PDFihsansiregarNo ratings yet
- Dr. Heston Standing Orders LandscapeDocument3 pagesDr. Heston Standing Orders LandscapeJosh Heston100% (1)
- Hypertension in PregnancyDocument29 pagesHypertension in PregnancyArchana KumariNo ratings yet
- Lesson 1 The Basics of First AidDocument70 pagesLesson 1 The Basics of First AidDJ JoeNo ratings yet
- 05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFDocument6 pages05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFrisda aulia putriNo ratings yet
- Mtap-Semr1-Week 2-Diabetes and Glucose MonitoringDocument9 pagesMtap-Semr1-Week 2-Diabetes and Glucose MonitoringJessoliver GalvezNo ratings yet
- Drugs Used in Pregnancy, Labour and Puerperium: Presented By:-Ms Lisa Chadha F.Y. MSC Nursing Bvcon, PuneDocument87 pagesDrugs Used in Pregnancy, Labour and Puerperium: Presented By:-Ms Lisa Chadha F.Y. MSC Nursing Bvcon, PuneSanjay Kumar SanjuNo ratings yet
- Assessment Three: Analysis of Legal and Professional Issues (2,200-Word Assignment, 50% of Available Mark)Document2 pagesAssessment Three: Analysis of Legal and Professional Issues (2,200-Word Assignment, 50% of Available Mark)Ayesha NaseerNo ratings yet
- Frequently Asked Questions On The Referral To Treatment (RTT) Data CollectionDocument24 pagesFrequently Asked Questions On The Referral To Treatment (RTT) Data Collectionraduben5403No ratings yet
- Anesthesia-Assisted Vs Buprenorphine - or Clonidine-Assisted Heroin Detoxification and Naltrexone InductionDocument11 pagesAnesthesia-Assisted Vs Buprenorphine - or Clonidine-Assisted Heroin Detoxification and Naltrexone InductionAndy PurnomoNo ratings yet
- 5 Paragraph Expository Essay OutlineDocument3 pages5 Paragraph Expository Essay Outlineb71bpjha100% (2)
- Colorectal Cancer Prevention and Early DetectionDocument33 pagesColorectal Cancer Prevention and Early DetectionNesyah AyuNo ratings yet
- 01.2 Craniotomy and CraniectomyDocument1 page01.2 Craniotomy and Craniectomyfebi novrizalNo ratings yet
- Fatty Liver Genomics PDFDocument25 pagesFatty Liver Genomics PDFVineeth VijayanNo ratings yet
- Poc ScoliosisDocument20 pagesPoc ScoliosisSugar Capule - ManuelNo ratings yet
- SepsisDocument8 pagesSepsisLEONELA VALDES CABELLONo ratings yet
- Heller Bergman 1953Document11 pagesHeller Bergman 1953Sirine AjourNo ratings yet
- Tic Disorders: by Rawan ChakasDocument17 pagesTic Disorders: by Rawan ChakasRawan ChakasNo ratings yet
2009 12 6b292ce7
2009 12 6b292ce7
Uploaded by
AbdallahOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2009 12 6b292ce7
2009 12 6b292ce7
Uploaded by
AbdallahCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/42438067
Essential fatty acids and human brain
Article in Acta neurologica Taiwanica · December 2009
Source: PubMed
CITATIONS READS
107 6,820
3 authors, including:
Chia-Yu Chang Jen-Yin Chen
Chi-Mei Medical Center Chi-Mei Medical Center
47 PUBLICATIONS 912 CITATIONS 81 PUBLICATIONS 650 CITATIONS
SEE PROFILE SEE PROFILE
All content following this page was uploaded by Chia-Yu Chang on 11 March 2015.
The user has requested enhancement of the downloaded file.
Review Article
231
Essential Fatty Acids and Human Brain
Chia-Yu Chang1,2, Der-Shin Ke1, and Jen-Yin Chen3
Abstract- The human brain is nearly 60 percent fat. We’ve learned in recent years that fatty acids are
among the most crucial molecules that determine your brain’s integrity and ability to perform. Essential
fatty acids (EFAs) are required for maintenance of optimal health but they can not synthesized by the body
and must be obtained from dietary sources. Clinical observation studies has related imbalance dietary intake
of fatty acids to impaired brain performance and diseases.
Most of the brain growth is completed by 5-6 years of age. The EFAs, particularly the omega-3 fatty
acids, are important for brain development during both the fetal and postnatal period. Dietary decosa-
hexaenoic acid (DHA) is needed for the optimum functional maturation of the retina and visual cortex, with
visual acuity and mental development seemingly improved by extra DHA. Beyond their important role in
building the brain structure, EFAs, as messengers, are involved in the synthesis and functions of brain neu-
rotransmitters, and in the molecules of the immune system. Neuronal membranes contain phospholipid
pools that are the reservoirs for the synthesis of specific lipid messengers on neuronal stimulation or injury.
These messengers in turn participate in signaling cascades that can either promote neuronal injury or neuro-
protection.
The goal of this review is to give a new understanding of how EFAs determine our brain’s integrity and
performance, and to recall the neuropsychiatric disorders that may be influenced by them. As we further
unlock the mystery of how fatty acids affect the brain and better understand the brain’s critical dependence
on specific EFAs, correct intake of the appropriate diet or supplements becomes one of the tasks we under-
take in pursuit of optimal wellness.
Key Words: Essential fatty acids, Human brain, Omega-3 fatty acids
Acta Neurol Taiwan 2009;18:231-241
INTRODUCTION fat had little influence on the brain. Today we know dif-
ferently. We’ve learned in recent years that fatty acids
The human brain is nearly 60 percent fat. Doctors are among the most crucial molecules that determine
probably ignored this fact because they thought dietary your brain’s integrity and ability to perform.
From the 1Department of Neurology, Chi-Mei Medical Center, Reprint requests and correspondence to: Chia-Yu Chang, MD.
Tainan, Taiwan; 2Institute of Biotechnology, College of Department of Neurology, Chi-Mei Medical Center, No. 901,
Engineering, Southern Taiwan University, Tainan, Taiwan; Chung Hwa Road, Yung Kang City, Tainan County 710,
3
Department of Anesthesia, Chi-Mei Medical Center, Tainan, Taiwan.
Taiwan. E-mail: chiayu.chang7@msa.hinet.net
Received July 1, 2009. Revised August 17, 2009.
Accepted September 11, 2009.
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
232
Essential fatty acids (EFAs) are required for mainte- are able to decrease the cholesterol level in the neuronal
nance of optimal health but they can not synthesized by membrane, which would otherwise decrease membrane
the body and must be obtained from dietary sources. fluidity, which in turn would make it difficult for the cell
They are also called polyunsaturated fatty acids to carry out its normal functions and increase the cell’s
(PUFAs). There are two classes of PUFAs--omega-6 and susceptibility to injury and death(3). These consequences
omega-3. The parent omega-6 fatty acid, linoleic acid for cell function are not restricted to absolute levels of
(LA) is desaturated in the body to form arachidonic acid EFAs alone, rather it appears that the relative amounts of
while parent omega-3 fatty acid alpha-linolenic acid omega-3 FAs and omega-6 FAs in the cell membranes
(ALA) is desaturated by microsomal enzyme system are responsible for affecting cellular function and subse-
through a series of metabolic steps to form eicosapen- quently promoting the pathogenesis of many chronic dis-
taenoic acid (EPA) and decosahexaenoic acid (DHA)(1). eases, including cardiovascular disease, cancer, osteo-
Some of these long-chain metabolites form precursors to porosis, and inflammatory and autoimmune diseases(4).
respective prostaglandins, thromboxanes, leukotrienes, Very high levels of FAs and lipids can be found in
and prostacyclin, which have a tremendous effect on the two structural components: the neuronal membrane and
brain’s blood flow, immune system and the neurotrans- the myelin sheath. About 50% of the neuronal membrane
mitter system(2) (Fig.). is composed of FAs, while in the myelin sheath lipids
Among the significant components of cell mem- constitute about 70%. The lipid component has a rela-
branes are the phospholipids that contain fatty acids tively high turnover rate, in contrast to the protein com-
(FAs). The types of FAs in the diet determine the types ponent that is especially stable(5). The integrity of the
of FAs that are available to the composition of the cell myelin is of utmost importance for the proper functions
membranes. A phospholipid made from a saturated fat of axons in the nervous system. Breakage or lesions in
has a different structure and is less fluid than one that the myelin can lead to disintegration of many of the ner-
incorporates an EFA. In addition, LA and ALA per se vous system functions. Recent studies emphasize the
have an effect on the neuronal membrane fluidity. They major role of dietary EFA to the normal functions of
oil of corn,
flax,
safflower,
pumpkin,
sunflower,
soybean,
sesame
walnut
oils of
primrose,
borage, cold water
black flsh,
currant algae
Figure. Metabolic pathway for essential
fatty acids.
GLA: gamma linolenic acid; PGs:
prostaglandins; TXs: thromboxanes;
LTs: leukotrienes.
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
233
myelin. Moreover, the EFAs are important in the active level of the omega-3 FAs was too low(11). Researchers of
phase of the myelin synthesis. If EFAs are not available Purdue University found that individuals with symptoms
in this phase or are metabolically blocked, amyelination, of hyperactivity and attention deficit had lower levels of
dysmyelination, or demyelanation may occur(6). If EFA the omega-3 FA and DHA in their blood(12). All these
deficiency occurs during the postnatal period, a major clinical observation studies related imbalance dietary
delay in the myelination process will occur, accompanied intake of FAs to impaired brain performance and dis-
by impaired learning, motor, vision, and auditory abnor- eases in some genetic vulnerable individuals.
malities(7). The goal of this review is to give a new under-
standing of how EFAs determine our brain’s integrity and EFAs and brain development
performance, and to recall the clinical conditions of the Most of the brain growth is completed by 5-6 years
brain that may be influenced by them. of age. At birth brain weight is 70% of an adult, 15%
brain growth occurs during infancy and remaining brain
DIETARY SOURCES OF EFAs growth is completed during preschool years (13). The
EFAs, particularly the omega-3 FAs, are important for
The main dietary sources of omega-6 FAs are veg- brain development during both the fetal and postnatal
etable oils like sunflower oil, safflower oil, sesame oil, period. Both omega-3 and omega-6 FAs play important
and corn oil. The rich dietary sources of omega-3 FAs roles in neuronal growth, development of synaptic pro-
are vegetable oils like flaxseed or canola oil, peanut oil, cessing of neural cell interaction, and expression of
walnut oil, green leafy vegetables, oily cold-water fish genes regulating cell differentiation and growth. Dietary
(mackerel, sardine, and salmon etc.) and fish oil. It is DHA is needed for the optimum functional maturation of
from these EFAs that our bodies make the vital brain-fats the retina and visual cortex, with visual acuity and men-
and the vital messengers that help regulate a vast array of tal development seemingly improved by extra DHA(14). In
body activity. Without the EFAs, our bodies run out of addition, the fetus and placenta are dependent on mater-
the building blocks our cells require to maintain peak nal EFA supply for their growth and development, with
function(8). Returning to the dietary trends of humans, DHA-supplemented infants showing signif icantly
we’ll recall that ancient diets contained a ratio of omega- greater mental and psychomotor development scores and
6 to omega-3 FAs estimated to be roughly 1:1. Today the breast-fed children do even better(15). Reduced DHA is
ratio is more on the order of 15:1-17:1(4) In addition, to also associated with impairments in cognitive and behav-
such “acquired” dietary imbalances that lessen omega-3 ioral performance, which are particularly important dur-
intakes, the healthy human organism has limited capacity ing brain development(16). From above findings we may
to elaborate the long chain DHA and EPA from shorter- suggest that providing proper FA balance during the
chain precursors. Metabolic biochemists have calculated infant period increases the opportunity to ensure that any
that five percent or less of dietary ALA is converted to child can realize his or her peak potential. It also raises
EPA, and less than 0.5 percent of dietary ALA makes it the possibility that a child suffering from learning,
to DHA(9). This change ratio of FAs appears to have sig- behavior, or other brain-related problems might be
nificant implications for brain function. When scientists helped if FA balance is restored while he or she still a
studied the brain of people with multiple sclerosis, they child. To achieve this we must be sure that nursing moth-
found that the brain tissue was very low in important ers have adequate ALA, and DHA in their diets.
fatty acids such as DHA(10). They also found low levels of
omega-3 FAs in blood and almost no omega-3 FAs THE ROLE OF EFAs IN BRAIN
stored in fat tissues. Doctors in Australia who studied the STRUCTURES AND FUNCTIONS
blood of people with moderate to severe depression
found the balance of EFAs was significantly altered; the Because the brain is predominantly made of fat,
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
234
almost all of its structures and functions have a crucial ulation of gene expression (PUFA influences on the
dependency upon EFAs, which we get directly from our signal transduction pathways and modifies mRNA activ-
food. ity)(22).
In the brain, there is little LA or ALA. The brain FAs that form the structure of your cell membranes
prefers arachidonic acid (AA) and DHA. For the brain, become messengers when a call to action is sent out.
these two fatty acids might be considered essential(17). In Neuronal membranes contain phospholipid pools that are
a developing fetus, AA is taken from the mother to help the reservoirs for the synthesis of specific lipid messen-
develop the fetal brain. In infancy, AA is present in gers on neuronal stimulation or injury(23). These messen-
breast milk to further promote brain development. At gers in turn participate in signaling cascades that can
about one year, a child is normally able to make enough either promote neuronal injury or neuroprotection.
of its own AA(18). Thus, for the adult, dietary AA is no Prostaglandins are synthesized as a result of cyclooxyge-
longer as important. Actually, when AA levels are too nase activity. In the first step of the AA cascade, the
high in the lipids of cell membranes, there is a tendency short-lived precursor, prostaglandin H2, is synthesized.
toward formation of inflammatory substances such as Additional steps in the cascade result in the synthesis of
prostaglandin E2, leukotrienes, and thromboxane A2. an array of prostaglandins, which participate in numer-
Over the past two decades we have learned that DHA is ous physiological and neurological processes (24). The
the critical long-chain omega-3 fatty acid found in the prostaglandins derived from membrane EFAs include
brain. Our bodies have the ability to make DHA from PGE1, PGE2, and PGE3. PGE1 is important in the ner-
essential fatty acid ALA, but this process is often very vous system as it affects the release of compounds from
inefficient(19). Thus we seem to have a requirement for nerve cells that transmit nerve impulses. It tends to have
preformed DHA in the diet that cannot be met by other anti-inflammatory properties and is immune enhancing.
fatty acids. In this way, DHA may be a conditionally PGE2 is a highly inflammatory substance. It can cause
EFA and essential for the brain. swelling, increased pain sensitivity, and increased blood
Beyond their important role in building the brain viscosity. Leukotrienes are related to PGE2 in that they
structure, EFAs have another crucial role -- as messen- are made from the fatty acid AA. PGE3 tends to be mild-
gers. EFAs are involved in the synthesis and functions of ly anti-inflammatory and immune enhancing. It is
brain neurotransmitters, and in the molecules of the thought to counter the effects of the powerful inflamma-
immune system(20). It is noted that omega-3 deficiency tory PGE2. It prevents blood platelets from clumping
reduces the dopamine vesicle density in the cortex and and helps prevent blood vessel spasm. FAs important in
causes malfunction of the dopaminergic mesocorticolim- PGE3 formation, like EPA and DHA, can also reduce
bic pathway(21). The role of EFAs in immune function is AA in the cells. This reduces the chance of producing
complicated since omega-3 and omega-6 have different messengers from AA and is one way that these FAs can
effects on various immune components and is largely alter the production of highly inflammatory messengers.
dependent on the omega-3 to omega-6 ratio. Several In another way, the membrane DHA might play a role of
mechanisms have been proposed for EFAs to mediate neuroprotection. It is the precursor of oxygenation prod-
their immunological functions in several disorders such ucts now known as the docosanoids, some of which are
as Alzheimer and schizophrenia. These include mem- powerful counter-proinflammatory mediators. The medi-
brane fluidity (changes that might effect the capability of ator 10,17S-docosatriene (neuroprotectin D1, NPD1)
cytokines to bind to their respective receptors on the cell counteracts leukocyte infiltration, NF-kappa activation,
membrane); lipid peroxidation (decrease in free radical- and proinflammatory gene expression in brain ischemia-
induced tissue damage); prostaglandin production (an reperfusion and is an apoptostatic mediator, potently
indirect mechanism whereby prostaglandins, which are counteracting oxidative stress-triggered apoptotic DNA
derivatives of PUFA, modify cytokine activity); and reg- damage in retinal pigment epithelial cells(23).
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
235
EFAs AND MENTAL PERFORMANCE fatty fish. Overall cognitive performance and psychomo-
tor speed were positively correlated with DHA/EPA sta-
Given the fatty nature of the brain, it seems quite tus. High intakes of cholesterol and saturated fat were
logical that the mental performance of some individuals both linked to increased cognitive impairment in this
with FA imbalance might be affected. Hibbeln et al.(25) middle-aged population.
recently have reported beneficial effects on child devel- Recent studies have associated def icits in DHA
opment with maternal seafood intakes of more than 340 abundance with cognitive decline during aging and in
g per week. They found that maternal seafood intake neurodegenerative disease(29). The importance of DHA-
during pregnancy of less than 340 g per week was asso- derived NPD1 has been underscored in the homeostatic
ciated with increased risk of their children being in the regulation of brain cell survival and repair involving neu-
lowest quartile for verbal intelligence quotient. In addi- rotrophic, antiapoptotic and antiinflammatory signaling.
tion, low maternal seafood intake was also associated Emerging evidence suggests that NPD1 synthesis is acti-
with increased risk of suboptimum outcomes for proso- vated by growth factors and neurotrophins. It has impor-
cial behaviour, fine motor, communication, and social tant determinant and regulatory interactions with the
development scores. In another study, Lucas A(26) also molecular-genetic mechanisms affecting beta-amyloid
pointed to a beneficial effect of human milk on neurode- precursor protein and amyloid beta peptide neurobiology.
velopment. Children who had consumed mother’s milk
in the early weeks of life had a significantly higher IQ at EFAs AND NEUROPSYCHIATRIC
7.5-8 years than did those who received no maternal DISORDERS
milk. There was a dose-response relation between the
proportion of mother’s milk in the diet and subsequent DHA/EPA in relation to dementia and mild
IQ. Furthermore, there is also evidence that healthy indi- cognitive impairment
viduals can expect cognitive benefit from EFAs, mainly In the past decade, epidemiological studies indicate
EPA and DHA. Fontani et al.(27) conducted a double-blind relatively high DHA and EPA intake is linked to lower
RCT on 33 healthy volunteers ages 22-51. For 35 days, relative risk of dementia incidence or progression. In
subjects consumed either 4 g fish oil/day ( 800 mg DHA 1997, Kalmijn et al.(30) reported on a longitudinal cohort
and 1,600 mg EPA) or 4 g olive oil as placebo. The study, in which 5,386 participants ages 55 or older were
DHA/EPA group improved significantly over placebo on screened for dementia. Dietary habits were evaluated
several mood parameters: vigor, anger, anxiety, fatigue, using a semi-quantitative food frequency questionnaire
depression, and confusion. Measures of attention and and then re-evaluated after 2.1 years. Fish consumption
reaction time were also improved. Participants demon- was inversely related to dementia incidence (RR=0.4,
strated marked improvement in sustained attention and a 95% CI=0.2-0.9), and more specifically to the risk of
significant reduction in errors on the attention test. developing Alzheimer’s disease (RR=0.3, 95% CI=0.1-
Accelerated cognitive decline in middle age can 0.9). In a Chicago community study, 815 residents ages
make an individual more vulnerable to dementia in later 65-94 were evaluated via a self-reported food question-
life. Evidence is accumulating to suggest omega-3 FA naire and tracked for an average 3.9 years(31). A total of
deficiency contributes to accelerated cognitive decline. 131 participants developed Alzheimer’s disease. Those
An epidemiology team led by Kalmijn tested 1,613 sub- who consumed a fish meal once weekly had a statistical-
jects, ages 45-70, for various cognitive functions at base- ly significant 60-percent decreased risk of Alzheimer’s
line and after five years and correlated the results with disease, compared with those who rarely or never ate
habitual food consumption reported on a self-adminis- fish (RR=0.4, 95% CI=0.2-0.9). Total omega-3 and
tered food questionnaire(28). Subjects exhibiting the most DHA intake, but not EPA intake alone, were significant-
impaired cognitive function (lowest 10 percent of the ly associated with this lessened Alzheimer risk. This
group score) also had the lowest intake of DHA/EPA or suggests an intake of as little as 30 mg/day DHA/EPA
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
236
from fish might confer more protection against cognitive In a recent systematic review(35), Issa AM et al. found
decline than eating no fish at all. a trend in favor of omega-3 FAs (fish and total omega-3
Longitudinal cohort studies can be more objective consumption) toward reducing risk of dementia and
when blood or tissue is analyzed for specific nutrients. improving cognitive function. Although the available
As part of the U.S. Framingham Heart Study, a cohort of data are insufficient to draw strong conclusions about the
899 men and women (median age 76 years), who were effects of omega-3 FAs on cognitive function in normal
free of dementia at baseline, were followed for a mean aging or on the incidence or treatment of dementia they
9.1 years for development of all-cause dementia and still suggest a possible association between omega-3 FAs
Alzheimer’s disease(32). Ninety-nine new cases of demen- and reduced risk of dementia.
tia (including 71 of Alzheimer’s disease) occurred.
Baseline and follow-up blood samples were tested for EPA and Huntington disease
fatty acids in the plasma phospholipid fraction. After Huntington disease (HD) features abnormal multipli-
controlling for other variables, subjects in the upper cation of a specific DNA sequence on chromosome 4:
quartile of plasma phospholipid DHA levels had approx- cytosine-adenine-guanine (CAG). Healthy people have
imately half the relative risk of developing all-cause just one CAG sequence at this spot; people with HD can
dementia (RR=0.53, 95% CI=0.29-0.97; p≤0.04) com- have several dozen CAG sequences. As a rule, the more
pared to subjects in the three lower quartiles. The upper CAGs the HD patient has, the more severe their dis-
quartile (n=488) had a mean DHA intake of 180 mg/day ease(36). On a suspicion that certain omega-3 responsive
and a mean f ish intake of 3.0 servings per week pathways could be involved, a team of British
(p<0.001). In 2006, a team from Stockholm’s Karolinska researchers have been using purified EPA in its ethyl
University Hospital published a double-blind RCT of ester form (“ethyl-EPA”) as potential therapy for HD(37).
DHA and EPA for 174 patients with mild-to-moderate They conducted a small RCT with ethyl-EPA on seven
Alzheimer’s disease (33). Patients received either 1.7 g in-patients with advanced (stage III) HD. After six
DHA and 0.6 g EPA daily or a placebo for six months, months, the four patients who received ethyl-EPA
after which all received the DHA/EPA supplements for demonstrated improvement on the orofacial component
six more months. After the first six months, decline in of the Unified Huntington Disease Rating Scale, while
cognitive function did not differ between groups. the three placebo patients had deteriorated (p<0.03).
However, in a subgroup with less severe cognitive dys- MRI brain scans revealed the placebo was associated
function (Mini-Mental State Exam score >27 points), a with progressive cerebral atrophy and ethyl-EPA was
signif icantly slower decline was observed in the associated with beneficial changes. Three years later, the
DHA/EPA group. A similar slowing was observed in the group completed a multicenter, double-blind RCT(38). A
placebo group after crossover to DHA/EPA for the sec- total of 135 Huntington patients received either 2 g/day
ond six months. These findings suggest patients with ethyl-EPA or placebo. The primary endpoint was the
mild Alzheimer deterioration could benefit from taking a score at 12 months on the Total Motor Score 4 (TMS-4)
mixed dietary supplement formulation containing both subscale. The ethyl-EPA group as a whole failed to show
DHA and EPA. statistically signif icant improvement on TMS-4.
Mild cognitive impairment (MCI) is currently the Nevertheless, a subgroup including patients with fewer
condition most predictive for subsequent progression to CAG showed significantly better TMS-4 improvement(39).
dementia. MCI features severely impaired memory with-
out substantial loss of other cognitive functions. Omega-3 FAs and depression
Approximately 10-15 percent of MCI subjects progress If omega-3 FAs play a role in depressive disorders,
to dementia within a year of diagnosis. Individuals cog- then it would be expected that countries consuming
nitively impaired but not demented tend to have abnor- greater amounts of these FAs (primarily through fish
mally low blood levels of DHA and EPA(34). intake) would have a lower prevalence of depression.
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
237
Actually, in a research conducted by Joseph Hibbeln of symptoms is likely associated with neural cell membrane
the National Institutes of Health it was found that a sig- dysfunction, most likely signal transduction abnormali-
nificant negative correlation between worldwide fish ties. The levels of seafood intake per capita in various
consumption and prevalence of depression(40). In another countries of the world roughly correlate with the respec-
research involving a random sample within a nation, fre- tive prevalence rates of BD in community samples(45).
quent fish consumption in the general population is asso- The greater the seafood consumption per capita in a
ciated with a decreased risk of depression(41). country, the lower the prevalence of bipolar spectrum
Maternal postpartum depression (also called “perina- disorders. Countries that consume a lot of fish on aver-
tal depression”) has been linked to omega-3 FA deficien- age (e.g., Iceland, Korea, and Taiwan) have relatively low
cy. As reviewed in Freeman(42), a survey of mother’s milk incidence, while countries that consume very little fish
in 23 countries determined that lower DHA content or (e.g., Germany, Switzerland, and Hungary) have up to
lower seafood consumption was associated with higher seven times the incidence of countries with high fish
rates of postpartum depression. Freeman noted that pilot intake. Noaghiul and Hibbeln estimated a “vulnerability
trials of supplementation with DHA and EPA have pro- threshold” for BD at seafood consumption below 50
duced mixed results and called for larger and better- pounds of seafood/person/year.
designed trials to resolve this condition that endangers To date, four published double-blind trials on
both mother and child. DHA/EPA for BD have been published. The first was a
Su and colleagues(43) recently reported a beneficial 1999 trial that found significantly longer remission of
effect of omega-3 FAs in a 8 week duration double-blind bipolar symptomology from a high-dose DHA and EPA
placebo controlled trial of 22 patients with major depres- mixture (9.6 g/day) compared to placebo(46). Three more
sive disorder using fish oil (daily dose of 2.2 g/day EPA double-blind trials were published in 2006 with differing
and 1.1 g/day DHA) or an olive oil placebo. Of the results. In the largest trial, Frangou et al found signifi-
patients completing the trial, the omega-3 FA group cant improvement using EPA only (ethyl-EPA) in 75
achieved a significantly greater reduction in depressive patients, with 1 g/day working just as well as 2 g/day(47).
symptoms than the placebo group. In a recent meta-ana- Keck et al found no significant differences between
lytic review of double-blind, placebo-controlled trials of placebo and 6 g/day EPA (no DHA) in 61 patients(48).
antidepressant efficacy of omega-3 FAs, Lin PY and his Marangell et al conducted a small study on 10 patients
colleague (44) reviewed ten double-blind, placebo-con- using only DHA and reported only that DHA was “well
trolled studies in patients with mood disorders receiving tolerated”(49). In a recent Cochrane review Montgomery P
omega-3 FAs with the treatment period lasting 4 weeks et al.(50) found that only one study, involving 75 partici-
or longer. They found a significant antidepressant effect pants, provided data for analysis and showed positive
of omega-3 FAs (effect size = 0.61, p= .003) and the effects of omega-3 as an adjunctive treatment for depres-
dosage of EPA did not change the antidepressant effica- sive but not manic symptoms in bipolar disorder from
cy significantly. However, significant heterogeneity five studies. But they concluded that these findings must
among these studies and publication bias were noted. be regarded with caution owing to the limited data avail-
They therefore concluded that it is still premature to vali- able.
date this finding due to publication bias and heterogene-
ity. More large-scale, well-controlled trials are needed to Omega-3 FA and schizophrenia
find out the favorable target subjects, therapeutic dose of FAs have also been the focus of intense study in the
EPA, and the composition of omega-3 FAs in treating psychotic disorder schizophrenia (51). A “phospholipid
depression. membrane hypothesis of schizophrenia”, as reviewed in
2000 by Fenton and colleagues(52), encompasses abnor-
Omega-3 FAs and bipolar disorder malities of long-chain omega-6 FAs such as AA, as well
Bipolar disorder (BD) with its complex spectrum of as DHA and EPA. Fenton et al. list multiple analyses of
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
238
RBC membranes (recognized markers for EFA status) That’s because most modern diets contain too much
that consistently document depletion of AA, DHA, and omega-6 and far too little omega-3. In reality, balance of
EPA. Also noted were studies documenting depletion in EFAs is critical. We don’t want to go overboard on any
plasma, thrombocytes, and post-mortem brain tissue of particular FA.
schizophrenia patients(52). How does one know whether supplementation is
Six double-blind RCTs with DHA/EPA have been necessary? Physical signs and symptoms of deficiency
conducted recently, involving 390 patients with schizo- include excessive thirst, frequent urination, rough dry
phrenia or schizoaffective disorder(53-57). Four of these hair and skin, and follicular keratosis(60). The current
documented clinical benefit from 2/g EPA daily for three knowledge base on DHA/EPA for brain function does
months. One trial found high-EPA fish oil performed not generate a rational daily intake recommendation.
better than high-DHA fish oil or placebo(53). Another Hibbeln, from his studies on national seafood intakes
dose-ranging trial of ethyl-EPA found 2 g/day worked and affective disorder incidence, suggested pregnant
better than 1 g or 4 g daily(54). Two trials by the same women might want to consume a minimum 650 mg/day
group examined ethyl-EPA’s effect on tardive dyskinesia of DHA and EPA (with a minimum 300 mg/day of
associated with pharmaceutical management of schizo- DHA) to prevent postpartum depression(40). Although
phrenia. In a 2002 trial, Emsley et al found benefit at 3 high doses of ALA can increase tissue EPA levels, ALA
g/day(55), but a later 2006 trial did not demonstrate bene- does not have the same effect on DHA levels(61), render-
fit at the lower dose of 2 g/day(57). Because all these clini- ing supplementation necessary. For vegetarians cultivat-
cal studies using omega 3 FA supplementation showed ed microalgae are a good source of DHA.
the inconsistent results in different doses of ethyl-EPA as
compared with placebo a recent Cochrane review(58) con- CONCLUSIONS
cluded that the use of omega-3 FAs for schizophrenia
still remains experimental and a large well designed, Although the current clinical literature on EFAs for
conducted studies is needed. brain function is still relatively small compared to the lit-
erature on circulatory benefits, the weight of the current
EPA supplementation in borderline personality evidence strongly supports their utility for cognition,
disorder behavior, and mood, as well as for early brain develop-
Borderline personality disorder may also respond to ment and overall mental performance. As we further
omega-3 supplementation. In a double blind, placebo- unlock the mystery of how FAs affect the brain, we may
controlled trial, 30 female subjects with moderately be able to change the course of our individual lives and
severe BPD received 1 g/day EPA only (as ethyl-EPA) or perhaps even society by making wise dietary changes.
a placebo for two months. Those taking ethyl-EPA expe-
rienced significantly diminished aggression and less REFERENCES
severe depression(59).
1. Singh M. Essential fatty acids, DHA and human brain.
CORRECT INTAKE OF EFAs Indian J Pediatr 2005;72:239-42.
FOR BRAIN BENEFITS 2. Das UN. Essential Fatty acids- a review. Curr Pharm
Biotechnol 2006;7:467-82.
As we better understand the brain’s critical depen- 3. Fernstrom JD. Effects of dietary polyunsaturated fatty acids
dence on specific EFAs, correct intake of the appropriate on neuronal function. Lipids 1999;34:161-9.
diet or supplements becomes one of the appropriate tasks 4. Simopoulos AP. Evolutionary aspects of diet, the omega-
we undertake in pursuit of optimal wellness. In this 6/omega-3 ratio and genetic variation: nutritional implica-
review, we may have gathered the impression that tions for chronic diseases. Biomed Pharmacother 2006;60:
omega-3 FAs are more important than omega-6 FAs. 502-7.
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
239
5. Yehuda S, Rabinovitz S, Mostofsky DI. Essential fatty acid supplementation and conversion to n-3 long-chain
acids and the brain: from infancy to aging. Neurobiol polyunsaturated fatty acids in humans. Prostaglandins
Aging 2005;26:98-102. Leukot Essent Fatty Acids 2009;80:85-91.
6. Salvati S, Attorri L, Avellino C, et al. Diet, lipids and brain 20. Yehuda S, Rabinovitz S, Mostofsky DI. Essential fatty
development. Dev Neurosci 2000;22:481-7. acids and the brain: from infancy to aging. Neurobiol
7. Stockard JE, Saste MD, Benford VJ, et al. Effect of docosa- Aging 2005;26:98-102.
hexaenoic acid content of maternal diet on auditory brain- 21. Yehuda S, Rabinovitz S, Carasso RL, et al. Fatty acids and
stem conduction times in rat pups. Dev Neurosci 2000;22: brain peptides. Peptides 1998;9:407-19.
494-9. 22. Yao JK, van Kammen DP. Membrane phospholipids and
8. Das UN. Essential fatty acids: biochemistry, physiology cytokine interaction in schizophrenia. Int Rev Neurobiol
and pathology. Biotechnol J 2006;1:420-39. 2004;59:297-326.
9. Plourde M, Cunnane SC. Extremely limited synthesis of 23. Bazan NG. Lipid signaling in neural plasticity, brain repair,
long chain polyunsaturates in adults: implications for their and neuroprotection. Mol Neurobiol 2005;32:89-103.
dietary essentiality and use as supplements. Appl Physiol 24. Privett OS, Phillips F, Fukazawa T, et al. Studies on the
Nutr Metab 2007;32:619-34. relationship of the synthesis of prostaglandins to the biolog-
10. Nightingale S, Woo E, Smith AD, et al. Red blood cell and ical activity of essential fatty acid. Biochim Biophys Acta
adipose tissue fatty acids in mind inactive multiple sclero- 1972;280:348-55.
sis. Acta Neurol Scand 1990;82:43-50. 25. Hibbeln JR, Davis JM, Steer C, et al. Maternal seafood
11. Adams PB, Lawson S, Sanigorski A, et al. Arachidonic consumption in pregnancy and neurodevelopmental out-
acid to eicosapentaenoic acid ratio in blood correlates posi- comes in childhood (ALSPAC study): an observational
tively with clinical symptoms of depression. Lipids 1996; cohort study. Lancet 2007;369:578-85.
31:S157-61. 26. Lucas A, Morley R, Cole TJ, et al. Breast milk and subse-
12. Stevens LJ, Zentall SS, Abate ML, et al. Omega-3 fatty quent intelligence quotient in children born preterm. Lancet
acids in boys with behavior, learning, and health problems. 1992;339:261-4.
Physiol Behav 1996;59:915-20. 27. Fontani G, Corradeschi F, Felici A, et al. Cognitive and
13. Clandinin MT, Jumpsen J, Suh M. Relationship between physiological effects of Omega-3 polyunsaturated fatty acid
fatty acid accretion, membrane composition, and biologic supplementation in healthy subjects. Eur J Clin Invest
functions. J Pediatr 1994;125:S25-32. 2005;35:691-9.
14. Uauy R, Dangour AD. Nutrition in brain development and 28. Kalmijn S, van Boxtel MP, Ocke M, et al. Dietary intake of
aging: role of essential fatty acids. Nutr Rev 2006;64(5 Pt fatty acids and fish in relation to cognitive performance at
2):S24-33. middle age. Neurology 2004;62:275-80.
15. Makrides M, Neumann MA, Byard RW, et al. Fatty acid 29. Lukiw WJ, Bazan NG. Docosahexaenoic acid and the aging
composition of brain, retina, and erythrocytes in breast- and brain. J Nutr 2008;138:2510-4.
formula-fed infants. Am J Clin Nutr 1994;60:189-94. 30. Kalmijn S, Launer LJ, Ott A, et al. Dietary fat intake and
16. Innis SM. Dietary (n-3) fatty acids and brain development. the risk of incident dementia in the Rotterdam Study. Ann
J Nutr 2007;137:855-9. Neurol 1997;42:776-82.
17. Hadders-Algra M. Prenatal long-chain polyunsaturated 31. Morris MC, Evans DA, Bienias JL, et al. Consumption of
fatty acid status: the importance of a balanced intake of fish and n-3 fatty acids and risk of incident Alzheimer dis-
docosahexaenoic acid and arachidonic acid. J Perinat Med ease. Arch Neurol 2003;60:940-6.
2008;36:101-9. 32. Schaefer EJ, Bongard V, Beiser AS, et al. Plasma phos-
18. Agostoni C. Role of long-chain polyunsaturated fatty acids phatidylcholine docosahexaenoic acid content and risk of
in the first year of life. J Pediatr Gastroenterol Nutr 2008; dementia and Alzheimer disease: the Framingham Heart
47:S41-4. Study. Arch Neurol 2006;63:1545-50.
19. Brenna JT, Salem N Jr, Sinclair AJ, et al. Alpha-Linolenic 33. Freund-Levi Y, Eriksdotter-Jonhagen M, Cederholm T, et
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
240
al. Omega-3 fatty acid treatment in 174 patients with mild 47. Frangou S, Lewis M, McCrone P. Efficacy of ethyl-eicos-
to moderate Alzheimer disease: OmegAD study: a random- apentaenoic acid in bipolar depression: randomised double-
ized double-blind trial. Arch Neurol 2006;63:1402-8. blind placebo-controlled study. Br J Psychiatry 2006;188:
34. Conquer JA, Tierney MC, Zecevic J, et al. Fatty acid analy- 46-50.
sis of blood plasma of patients with Alzheimer’s disease, 48. Keck PE Jr, Mintz J, McElroy SL. Double-blind, random-
other types of dementia, and cognitive impairment. Lipids ized, placebo-controlled trials of ethyl-eicosapentanoate in
2000;35:1305-12. the treatment of bipolar depression and rapid cycling bipo-
35. Issa AM, Mojica WA, Morton SC, et al. The efficacy of lar disorder. Biol Psychiatry 2006;60:1020-2.
omega-3 fatty acids on cognitive function in aging and 49. Marangell LB, Suppes T, Ketter TA. Omega-3 fatty acids in
dementia: a systematic review. Dement Geriatr Cogn bipolar disorder: clinical and research considerations.
Disord 2006;21:88-96. Prostaglandins Leukot Essent Fatty Acids 2006;75:315-21.
36. Martin JB, Gusella JF. Huntington’s disease. Pathogenesis 50. Montgomery P, Richardson AJ. Omega-3 fatty acids for
and management. N Engl J Med 1986;315:1267-76. bipolar disorder. Cochrane Database Syst Rev 2008;(2):
37. Puri BK, Bydder GM, Counsell SJ, et al. MRI and neu- CD005169.
ropsychological improvement in Huntington disease fol- 51. American Psychiatric Association: Diagnostic and statisti-
lowing ethyl-EPA treatment. Neuroreport 2002;13:123-6. cal manual of mental disorders. Fourth edit. Washington,
38. Puri BK, Leavitt BR, Hayden MR, et al. Ethyl-EPA in DC: American Psychiatric Association, 1994.
Huntington disease: a double-blind, randomized, placebo- 52. Fenton WS, Hibbeln J, Knable M. Essential fatty acids,
controlled trial. Neurology 2005;65:286-92. lipid membrane abnormalities, and the diagnosis and treat-
39. Murck H, Manku M. Ethyl-EPA in Huntington disease: ment of schizophrenia. Biol Psychiatry 2000;47:8-21.
potentially relevant mechanism of action. Brain Res Bull 53. Peet M, Brind J, Ramchand CN, et al. Two double-blind
2007;72:159-64. placebo-controlled pilot studies of eicosapentaenoic acid in
40. Hibbeln JR. Fish consumption and major depression. the treatment of schizophrenia. Schizophr Res 2001;49:
Lancet 1998;351:1213. 243-51.
41. Tanskanen A, Hibbeln JR, Hintikka J, et al. Fish consump- 54. Peet M, Horrobin DF, E-E Multicentre Study Group. A
tion, depression, and suicidality in a general population. dose-ranging exploratory study of the effects of ethyl-eicos-
Arch Gen Psychiatry 2001;58:512-3. apentaenoate in patients with persistent schizophrenic
42. Freeman MP. Omega-3 fatty acids and perinatal depression: symptoms. J Psychiatr Res 2002;36:7-18.
a review of the literature and recommendations for future 55. Emsley R, Myburgh C, Oosthuizen P, et al. Randomized,
research. Prostaglandins Leukot Essent Fatty Acids placebo-controlled study of ethyl-eicosapentaenoic acid as
2006;75:291-7. supplemental treatment in schizophrenia. Am J Psychiatry
43. Su KP, Huang SY, Chiu CC, et al. Omega-3 fatty acids in 2002;159:1596-8.
major depressive disorder.A preliminary double-blind, 56. Fenton WS, Dickerson F, Boronow J, et al. A placebo-con-
placebo-controlled trial. Eur Neuropsychopharmacol trolled trial of omega-3 fatty acid (ethyl eicosapentaenoic
2003;13:267-71. acid) supplementation for residual symptoms and cognitive
44. Lin PY, Su KP. A meta-analytic review of double-blind, impairment in schizophrenia. Am J Psychiatry 2001;158:
placebo-controlled trials of antidepressant efficacy of 2071-4.
omega-3 fatty acids. J Clin Psychiatry. 2007;68:1056-61. 57. Emsley R, Niehaus DJ, Koen L, et al. The effects of eicos-
45. Noaghiul S, Hibbeln JR. Cross-national comparisons of apentaenoic acid in tardive dyskinesia: a randomized,
seafood consumption and rates of bipolar disorders. Am J placebo-controlled trial. Schizophr Res 2006;84:112-20.
Psychiatry 2003;160:2222-7. 58. Joy CB, Mumby-Croft R, Joy LA. Polyunsaturated fatty
46. Stoll AL, Severus WE, Freeman MP, et al. Omega 3 fatty acid supplementation for schizophrenia. Cochrane Database
acids in bipolar disorder: a preliminary double-blind, place- Syst Rev 2006;3:CD001257.
bo-controlled trial. Arch Gen Psychiatry 1999;56:407-12. 59. Zanarini MC, Frankenburg FR. Omega-3 fatty acid treat-
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
241
ment of women with borderline personality disorder: a dou- 18:155-72.
ble-blind, placebo-controlled pilot study. Am J Psychiatry 61. Francois CA, Connor SL, Bolewicz LC, et al. Supple-
2003;160:167-9. menting lactating women with flaxseed oil does not
60. Richardson AJ. Omega-3 fatty acids in ADHD and related increase docosahexaenoic acid in their milk. Am J Clin
neurodevelopmental disorders. Int Rev Psychiatry 2006; Nutr 2003;77:226-33.
Acta Neurologica Taiwanica Vol 18 No 4 December 2009
View publication stats
You might also like
- High-Yield Product FinalDocument99 pagesHigh-Yield Product FinalChristianNo ratings yet
- Eros & The Pineal - A Layman's Guide To Cerebral Solataire - Albert MostDocument7 pagesEros & The Pineal - A Layman's Guide To Cerebral Solataire - Albert Mosttyson100% (1)
- Get Tested: STD Vs Sti STD Vs StiDocument2 pagesGet Tested: STD Vs Sti STD Vs StiJanna May Villafuerte100% (2)
- EPQ On The Mental Health SystemDocument15 pagesEPQ On The Mental Health SystemAdam100% (2)
- Genioplasty Oral SurgeryDocument45 pagesGenioplasty Oral SurgeryFourthMolar.com100% (2)
- Omega-6/Omega-3 Ratio and Brain-Related Functions: Shlomo YehudaDocument20 pagesOmega-6/Omega-3 Ratio and Brain-Related Functions: Shlomo YehudaJonas SkadbergNo ratings yet
- Omega-3 DHA and EPA For Cognition, Behavior, and Mood: Clinical Findings and Structural-Functional Synergies With Cell Membrane PhospholipidsDocument21 pagesOmega-3 DHA and EPA For Cognition, Behavior, and Mood: Clinical Findings and Structural-Functional Synergies With Cell Membrane PhospholipidsHerlina HasibuanNo ratings yet
- Omega-3 Fatty Acids and Their Role in Central Nervous SystemDocument17 pagesOmega-3 Fatty Acids and Their Role in Central Nervous Systempokolio silvaNo ratings yet
- Natural Brain Enhancers Nutrients That RDocument52 pagesNatural Brain Enhancers Nutrients That RMaksymNo ratings yet
- Summary of Clinical Research For LaminineDocument10 pagesSummary of Clinical Research For LaminineDocAxi Maximo Jr AxibalNo ratings yet
- Difference Between Vegetable and Animal Omega 3 Fatty AcidsDocument3 pagesDifference Between Vegetable and Animal Omega 3 Fatty AcidsnicodipietroNo ratings yet
- MontoyaParra2018 Article StatusOfNutrientsImportantInBrDocument20 pagesMontoyaParra2018 Article StatusOfNutrientsImportantInBrYohana RumahorboNo ratings yet
- Neuromedicterranea Omega 3 y Salud MentalDocument13 pagesNeuromedicterranea Omega 3 y Salud MentalDORIS JANETHNo ratings yet
- Nutrients: A Nutrient Combination That Can Affect Synapse FormationDocument10 pagesNutrients: A Nutrient Combination That Can Affect Synapse Formationlina ningdyarNo ratings yet
- The Role of Omega-3 Fatty Acids in Mood DisordersDocument9 pagesThe Role of Omega-3 Fatty Acids in Mood DisordersARESS RIPNo ratings yet
- Dyall Epadpadha R Fan15Document16 pagesDyall Epadpadha R Fan15võ thị lệNo ratings yet
- PGM 2009 11 2083Document10 pagesPGM 2009 11 2083TASSIA CHRISTINNE BRITO COELHONo ratings yet
- 1 s2.0 S0304394023002033 MainDocument14 pages1 s2.0 S0304394023002033 MainAntonio Luiz PereiraNo ratings yet
- What Are Essential Fatty Acids?: Shorter Telomeres Are Associated With Bad Diet, Diseases and Early DeathDocument25 pagesWhat Are Essential Fatty Acids?: Shorter Telomeres Are Associated With Bad Diet, Diseases and Early DeathDavid James PNo ratings yet
- 6 Vol. 10 Issue 11 Nov 2019 IJPSR RA 11687Document7 pages6 Vol. 10 Issue 11 Nov 2019 IJPSR RA 11687Charles OnunekwuNo ratings yet
- 135 - Possible MecanismsDocument19 pages135 - Possible MecanismsEduardo BacelarNo ratings yet
- Nootropics SupplementsPDFDocument7 pagesNootropics SupplementsPDFnitinsharma12345wweNo ratings yet
- Morgese and Trabace, 2016Document20 pagesMorgese and Trabace, 2016Mohsin ZafarNo ratings yet
- Food For MoodDocument15 pagesFood For MoodDaniele LimaNo ratings yet
- Transdermal Selegiline PatchesDocument14 pagesTransdermal Selegiline PatchessujithaNo ratings yet
- 5.supplementation With Flaxseed Oil Rich in Alpha-Linolenic Acid Improves Verbal Fluency in Healthy Older AdultsDocument12 pages5.supplementation With Flaxseed Oil Rich in Alpha-Linolenic Acid Improves Verbal Fluency in Healthy Older Adultsvõ thị lệNo ratings yet
- Importance of Fatty Acids in Physiopathology of Human Body: Katalin Nagy and Ioana-Daria TiucaDocument20 pagesImportance of Fatty Acids in Physiopathology of Human Body: Katalin Nagy and Ioana-Daria TiucaStefan Tri PrabhataNo ratings yet
- Endocrine SystemDocument6 pagesEndocrine SystemynaNo ratings yet
- Chemicals in The Brain: Nervous System (Ms Socky)Document26 pagesChemicals in The Brain: Nervous System (Ms Socky)Jovelyn Morales JosolNo ratings yet
- Fotuhi 2009Document13 pagesFotuhi 2009peri umardianaNo ratings yet
- BiomedicineDocument10 pagesBiomedicinevrish Dhwaj AshwlayanNo ratings yet
- Qualia Mind Energy ShotDocument4 pagesQualia Mind Energy ShotPaulo Henrique Haß FilhoNo ratings yet
- Biological Theories of AgingDocument29 pagesBiological Theories of AgingdulceRN67% (3)
- Omega-3 Polyunsaturated Fatty Acids in The Treatment of SchizophreniaDocument7 pagesOmega-3 Polyunsaturated Fatty Acids in The Treatment of SchizophreniaPedro PriorNo ratings yet
- Dietary Essential Fatty Acids and Brain Function A Developmental Perspective On MechanismsDocument9 pagesDietary Essential Fatty Acids and Brain Function A Developmental Perspective On MechanismsBarbara Sakura RiawanNo ratings yet
- Phosphodiesterase WhatisinanenzymeDocument13 pagesPhosphodiesterase WhatisinanenzymentondojuniorchinoisNo ratings yet
- Sirtuin 5-Mediated Lysine Desuccinylation Protects Mitochondrial Metabolism Following Subarachnoid Hemorrhage in MiceDocument11 pagesSirtuin 5-Mediated Lysine Desuccinylation Protects Mitochondrial Metabolism Following Subarachnoid Hemorrhage in MicenicolaspanppNo ratings yet
- Protein Kinase Inhibition By: - 3 Fatty AcidsDocument9 pagesProtein Kinase Inhibition By: - 3 Fatty AcidsStepss StepsNo ratings yet
- Essential & Non-Essential Fatty AcidsDocument4 pagesEssential & Non-Essential Fatty AcidsVikash KushwahaNo ratings yet
- Essential Fatty Acid and Human BrainDocument4 pagesEssential Fatty Acid and Human BrainDwi Rahayu FitriawatiNo ratings yet
- 2021 Essential Brain Hygiene EguideDocument26 pages2021 Essential Brain Hygiene EguideHector SolarNo ratings yet
- The Role of Eicosanoids in The Brain: Review ArticleDocument9 pagesThe Role of Eicosanoids in The Brain: Review ArticleDr. Kaushal Kishor SharmaNo ratings yet
- Folic Acid Exerts Antidepressant Effects by Upregulating - JÁ FOIDocument8 pagesFolic Acid Exerts Antidepressant Effects by Upregulating - JÁ FOICamila VasquesNo ratings yet
- Review: Taurine: A "Very Essential" Amino Acid: Harris Ripps, Wen ShenDocument14 pagesReview: Taurine: A "Very Essential" Amino Acid: Harris Ripps, Wen Shenit's me ebeth tjhinNo ratings yet
- NeurotransmitterDocument7 pagesNeurotransmitterSweety DhillonNo ratings yet
- pjbf7k8s0j0.1Document1 pagepjbf7k8s0j0.1terje.yngvar.traneNo ratings yet
- Copy of Jacob Oakden Draft 2Document14 pagesCopy of Jacob Oakden Draft 2api-740081698No ratings yet
- Early Intervention Psych - 2021 - Susai - Omega 3 Fatty Acid in Ultra High Risk Psychosis A Systematic Review Based OnDocument14 pagesEarly Intervention Psych - 2021 - Susai - Omega 3 Fatty Acid in Ultra High Risk Psychosis A Systematic Review Based OnMitchel Cordova LoaizaNo ratings yet
- Nihms 123081Document15 pagesNihms 123081Jose PerezNo ratings yet
- Human Physiology An Integrated Approach 7Th Edition Silverthorn Solutions Manual Full Chapter PDFDocument36 pagesHuman Physiology An Integrated Approach 7Th Edition Silverthorn Solutions Manual Full Chapter PDFcleopatrabanhft1vh7100% (14)
- 414 1685 1 PBDocument13 pages414 1685 1 PBMuhammad Sona KhanNo ratings yet
- Implications of Lipid Biology For The Pathogenesis of SchizophreniaDocument12 pagesImplications of Lipid Biology For The Pathogenesis of SchizophreniaScheckyNo ratings yet
- Home: Correspondence:: Ala N Aragon's Research Review - July 2015)Document26 pagesHome: Correspondence:: Ala N Aragon's Research Review - July 2015)Andra SpatarNo ratings yet
- Research Paper On Protein StructureDocument6 pagesResearch Paper On Protein Structurezyfepyfej0p2100% (1)
- Omega-3 Literature ReviewDocument8 pagesOmega-3 Literature Reviewn1dihagavun2100% (1)
- Insights from Ayurveda for translational stem cellDocument7 pagesInsights from Ayurveda for translational stem cellRavi P ShaliwalNo ratings yet
- Acid Linoleic (Não)Document6 pagesAcid Linoleic (Não)Tuyết Nhỏ Thiên ThầnNo ratings yet
- Nutricion y EsquizofreniaDocument13 pagesNutricion y EsquizofreniacelliasttNo ratings yet
- Animal Physiology Midterm QuestionsDocument10 pagesAnimal Physiology Midterm QuestionsDani GutiérrezNo ratings yet
- Topographical Distribution of The Human Brain To Plukenetia Volubilis-Based Omega-3,6,9 Enriched Egg ConsumptionDocument13 pagesTopographical Distribution of The Human Brain To Plukenetia Volubilis-Based Omega-3,6,9 Enriched Egg ConsumptionIAES IJAINo ratings yet
- 100 Brain Optimization TipsDocument3 pages100 Brain Optimization TipsBrad Richardson100% (1)
- Organic ChemistryDocument236 pagesOrganic ChemistryAbdallahNo ratings yet
- Role of Long-Chain Polyunsaturated Fatty Acids in Infant NutritionDocument4 pagesRole of Long-Chain Polyunsaturated Fatty Acids in Infant NutritionAbdallahNo ratings yet
- Effect of Long-Chain Polyunsaturated Fatty Acids in Infant Formula On Problem Solving at 10 Months of AgeDocument4 pagesEffect of Long-Chain Polyunsaturated Fatty Acids in Infant Formula On Problem Solving at 10 Months of AgeAbdallahNo ratings yet
- 2020 11 07 - 214806Document4 pages2020 11 07 - 214806AbdallahNo ratings yet
- Final TCS ModuleDocument24 pagesFinal TCS Modulemae cudalNo ratings yet
- Brfo193 Radiotherapy Dose Fractionation Third-Edition PDFDocument137 pagesBrfo193 Radiotherapy Dose Fractionation Third-Edition PDFMed MedNo ratings yet
- Developmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsDocument71 pagesDevelopmental Dysplasia of The Hip: Dr. Bassel El-Osta SPR Trauma & OrthopaedicsvadimmadanNo ratings yet
- Sexually Transmitted InfectionDocument16 pagesSexually Transmitted InfectionSonam ChaudharyNo ratings yet
- The Interaction of Herbs and DrugsDocument17 pagesThe Interaction of Herbs and DrugsCarleta StanNo ratings yet
- Manila Police District (MPD) As of January 2022: Action PNCO, DSTU OIC, Training Section C, DPRMDDocument15 pagesManila Police District (MPD) As of January 2022: Action PNCO, DSTU OIC, Training Section C, DPRMDShan Dave TupasNo ratings yet
- Heart Failure Clinical Records DatasetDocument14 pagesHeart Failure Clinical Records Datasetpanca saputraNo ratings yet
- CT Ordering Guide: Tumor Staging and Follow UpDocument2 pagesCT Ordering Guide: Tumor Staging and Follow UpanonNo ratings yet
- Immunology 9Th Edition Male David Full ChapterDocument61 pagesImmunology 9Th Edition Male David Full Chaptertodd.wimbush786100% (10)
- Eye Essentials Cataract Assessment Classification and Management PDFDocument245 pagesEye Essentials Cataract Assessment Classification and Management PDFihsansiregarNo ratings yet
- Dr. Heston Standing Orders LandscapeDocument3 pagesDr. Heston Standing Orders LandscapeJosh Heston100% (1)
- Hypertension in PregnancyDocument29 pagesHypertension in PregnancyArchana KumariNo ratings yet
- Lesson 1 The Basics of First AidDocument70 pagesLesson 1 The Basics of First AidDJ JoeNo ratings yet
- 05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFDocument6 pages05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFrisda aulia putriNo ratings yet
- Mtap-Semr1-Week 2-Diabetes and Glucose MonitoringDocument9 pagesMtap-Semr1-Week 2-Diabetes and Glucose MonitoringJessoliver GalvezNo ratings yet
- Drugs Used in Pregnancy, Labour and Puerperium: Presented By:-Ms Lisa Chadha F.Y. MSC Nursing Bvcon, PuneDocument87 pagesDrugs Used in Pregnancy, Labour and Puerperium: Presented By:-Ms Lisa Chadha F.Y. MSC Nursing Bvcon, PuneSanjay Kumar SanjuNo ratings yet
- Assessment Three: Analysis of Legal and Professional Issues (2,200-Word Assignment, 50% of Available Mark)Document2 pagesAssessment Three: Analysis of Legal and Professional Issues (2,200-Word Assignment, 50% of Available Mark)Ayesha NaseerNo ratings yet
- Frequently Asked Questions On The Referral To Treatment (RTT) Data CollectionDocument24 pagesFrequently Asked Questions On The Referral To Treatment (RTT) Data Collectionraduben5403No ratings yet
- Anesthesia-Assisted Vs Buprenorphine - or Clonidine-Assisted Heroin Detoxification and Naltrexone InductionDocument11 pagesAnesthesia-Assisted Vs Buprenorphine - or Clonidine-Assisted Heroin Detoxification and Naltrexone InductionAndy PurnomoNo ratings yet
- 5 Paragraph Expository Essay OutlineDocument3 pages5 Paragraph Expository Essay Outlineb71bpjha100% (2)
- Colorectal Cancer Prevention and Early DetectionDocument33 pagesColorectal Cancer Prevention and Early DetectionNesyah AyuNo ratings yet
- 01.2 Craniotomy and CraniectomyDocument1 page01.2 Craniotomy and Craniectomyfebi novrizalNo ratings yet
- Fatty Liver Genomics PDFDocument25 pagesFatty Liver Genomics PDFVineeth VijayanNo ratings yet
- Poc ScoliosisDocument20 pagesPoc ScoliosisSugar Capule - ManuelNo ratings yet
- SepsisDocument8 pagesSepsisLEONELA VALDES CABELLONo ratings yet
- Heller Bergman 1953Document11 pagesHeller Bergman 1953Sirine AjourNo ratings yet
- Tic Disorders: by Rawan ChakasDocument17 pagesTic Disorders: by Rawan ChakasRawan ChakasNo ratings yet