Professional Documents
Culture Documents
Comparison Between Two Postdentin Bond Strength Measurement
Comparison Between Two Postdentin Bond Strength Measurement
Uploaded by
Pao JanacetOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Comparison Between Two Postdentin Bond Strength Measurement
Comparison Between Two Postdentin Bond Strength Measurement
Uploaded by
Pao JanacetCopyright:
Available Formats
www.nature.
com/scientificreports
OPEN Comparison between two post-
dentin bond strength measurement
methods
Received: 5 April 2017 Laikuan Zhu1,2, Yuping Li3, Yung-Chung Chen4, Carola A. Carrera3, Chong Wu5 & Alex Fok3
Accepted: 25 January 2018
Published: xx xx xxxx The push-out (PO) test and the diametral compression (DC) test were performed to compare the merits
of two post-dentin bond strength measurement methods. Compared with the push-out test, the disk in
DC provided post-dentin bond strength measurements that were more precise. The load-displacement
curves from the DC test were much smoother and more linear up to the point of fracture when
compared to those from the PO test. Compared to the PO test, DC is easier to perform for determining
the bond strength between posts and dentin. No specimen alignment is needed in the DC test, and it
produces a smaller standard deviation in the measured bond strength. The main disadvantage of the
DC test, however, is that finite element analysis (FEA) is required to calculate the bond strength. The
shear bond strength given by the PO test based on the simple formula is not valid, though, and the peak
failure load is dependent on friction at the post-dentin interface.
Teeth with extensive loss of coronal hard tissue after endodontic treatment require the placement of posts inside
the root canals to support the restorations above1. Post loosening and root fracture are the most common rea-
sons for the failure of such endodontically treated teeth2. With the post debonded from the surrounding dentin,
very high stresses can be created by the occlusal forces in the restored tooth, leading to root fracture3. Therefore,
a strong and durable bond between the intracanal post and root dentin is vital for the longevity of the restored
tooth.
The bond strength between intracanal posts and root dentin can be determined by several mechanical tests;
for example, the microtensile test4, pull-out test5 and push-out test6. The specimens used for the microtensile test
have to be trimmed to a complex shape, which makes them prone to pre-test failures7. In contrast, the specimens
used for the push-out (PO) test require minimal machining, and they appear to have a more homogeneous stress
distribution around the post circumference when examined using finite element analysis (FEA)8. Therefore, the
PO test is commonly used for evaluating the bond strength of intracanal filling materials8–10. However, it has some
limitations. First of all, FEA has shown that the fracture-initiating stress is tensile rather than shear, thus invalidat-
ing the formula used to calculate the bond strength. Second, the measurements it produces have a large standard
deviation11,12. Third, PO bond strengths could be affected by geometric factors of the specimen and loading jig13.
Further, friction between the post and dentin causes the push-out force to continue to increase after the initial
fracture14,15. Therefore, the bond strength measured by the PO test, based usually on the maximum load, is likely
to be an overestimate.
The diametral compression (DC) test, or the Brazilian disk test, has been widely used for measuring the tensile
strength of brittle materials. The stress distribution and failure mode in the specimen have also been investigated
in detail16. A modified DC test has successfully been used to measure the dentin bond strength of intracanal posts
and direct composite restorations17,18. The bond strengths determined by this test seemed to have lower coeffi-
cients of variation (~15%).
1
Department of Endodontics and Operative Dentistry, Ninth People’s Hospital, Shanghai Jiao Tong University School
of Medicine, Shanghai, 200011, China. 2Shanghai Key Laboratory of Stomatology & Shanghai Research Institute
of Stomatology, National Clinical Research Center of Stomatology, Shanghai, 200011, China. 3Minnesota Dental
Research Center for Biomaterials and Biomechanics, School of Dentistry, University of Minnesota, Minneapolis, MN,
55455, USA. 4Institute of Oral Medicine, College of Medicine National Cheng Kung University Taiwan, Tainan, 701,
Taiwan. 5Division of Biostatistics, School of Public Health, University of Minnesota, Minneapolis, MN, 55455, USA.
Correspondence and requests for materials should be addressed to L.Z. (email: zhulk1997@163.com) or A.F. (email:
alexfok@umn.edu)
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 1
www.nature.com/scientificreports/
Figure 1. Typical load-time curves from the mechanical tests. (A) from a DC test; (B) from a PO test. Note that
displacement = time × 0.5 mm/min.
PBS TC
Resin cement Coefficients of Variation RMGI Coefficients of Variation Resin cement Coefficients of Variation RMGI Coefficients of Variation
DC 20.01 ± 2.76 13.79% 17.42 ± 3.39 19.46% 19.43 ± 2.48 12.76% 15.39 ± 2.00 13.00%
PO 8.04 ± 3.93 48.88% 6.75 ± 2.50 37.04% 5.87 ± 3.12 53.15% 5.14 ± 2.66 51.75%
Table 1. Bond strength (MPa) of post-dentin disks for each group. The data shown are the means ± standard
deviations. DC – diametral compression; PO – push-out test.
The purpose of this study was to compare the merits of the DC and PO tests and to try to offer an appropriate
method to measure the bond strength of intracanal post with root dentin. The null hypothesis was that there was
no significant difference between the two methods to measure the post-dentin interfacial bond strength.
Results
Load-displacement curves. Load-displacement curves were obtained from all runs. Typical load-time
curves from the two mechanical tests are presented in Fig. 1. The others were similar. Note that displacement can
be obtained by multiplying time with the rate of loading (0.5 mm/min). The curves from the DC test were much
smoother and more linear from the point of initial contact between the specimen and the loading member up to
the point of fracture. In contrast, those from the PO test had many load peaks and troughs throughout the loading
history, with the load continuing to increase following the initial failure and a gradual reduction in load capacity
after the peak load was reached.
Bond strength of post-dentin disks. The bond strengths for the different groups are shown in Table 1.
The results showed that the tensile bond strengths measured by the DC test (15.39 ± 2.00–20.01 ± 2.76 MPa)
were higher than the shear bond strength determined by the PO test (5.14 ± 2.66–8.04 ± 3.93 MPa) for both of
the materials and pretreatments used in this study (p = 0.000). On the other hand, the coefficients of variation of
the tensile bond strength from DC (13.00–19.46%) were much lower than those of the shear bond strength given
by the PO test (37.04–53.15%) for each of the cases.
Resin cement produced significantly higher tensile bond strengths (19.43 ± 2.48 or 20.01 ± 2.76 MPa) than
resin-modified glass ionomer (RMGI) (15.39 ± 2.00 or 17.42 ± 3.39 MPa) with (p = 0.000) or without (p = 0.011)
thermal cycling (TC). After TC, the tensile bond strength of the RMGI group (15.39 ± 2.00 MPa) was signifi-
cantly lower (p = 0.028) than that of the control group (17.42 ± 3.39 MPa), but there was no significant differ-
ence (p = 0.487) in the tensile bond strength of the resin cement specimens between the TC group and the PBS
(phosphate-buffered saline) group (20.01 ± 2.76 and 19.43 ± 2.48 MPa). The shear bond strengths given by the
PO test, on the other hand, presented no significant difference between any of the groups (8.04 ± 3.93, 6.75 ± 2.50,
5.87 ± 3.12 and 5.14 ± 2.66 MPa).
Failure mode analysis. As shown in Table 2, resin cement and RMGI produced different failure modes in
the mechanically tested specimens. With resin cement, adhesive failure between the cement and dentin was the
most frequent failure mode in both the DC and PO tests. Without thermo-cycling, all the specimens failed at the
cement-dentin interface. With thermo-cycling, 5% of the resin cement specimens showed mixed-mode failure,
i.e., cohesive failure within the cement mixed with adhesive failure between the cement and dentin, in both the
DC and PO test. In contrast, the RMGI disks showed predominantly mixed-mode failure in all four cases. The
next major failure mode in the RMGI disks was adhesive failure between the cement and dentin, followed by
adhesive failure between the post and cement, which was not seen in the resin cement specimens or RMGI spec-
imens after thermal cycling.
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 2
www.nature.com/scientificreports/
Diametral compression test Push-out test
PBS TC PBS TC
Failure Mode Resin cement RMGI Resin cement RMGI Resin cement RMGI Resin cement RMGI
CD 20(100) 9(45) 19(95) 5(25) 20(100) 5(25) 19(95) 7(35)
CP 0(0) 2(10) 0(0) 3(15) 0(0) 0(0) 0(0) 0(0)
Mixed 0(0) 9(45) 1(5) 12(60) 0(0) 15(75) 1(5) 13(65)
Table 2. Number (percentage) of specimens failed with a particular fracture mode under the different
experimental conditions. CD: adhesive failure between the cement and dentin; CP: adhesive failure between the
cement and post; Mixed: cohesive failure within the cement mixed with adhesive failure between the cement
and dentin/post.
Figure 2. 3D micro-CT images of AgNO3 that had infiltrated through the exposed dentin and along the post-
dentin interface. (A) Resin cement with PBS. (B) Resin cement with TC. (C) RMGI with PBS. (D) RMGI with
TC.
Figure 3. Depths of AgNO3 infiltration in post-dentin disks.
Interfacial leakage. Figure 2 shows the micro-CT images of silver nitrate penetration in the post-dentin
disks. The RMGI disks exhibited more interfacial leakage than the resin cement ones, with or without TC. In the
RMGI disks, the infiltrated depth of silver nitrate with and without TC was 0.19 ± 0.03 mm and 0.18 ± 0.04 mm,
respectively. In the resin cement disks, it was 0.12 ± 0.08 mm and 0.06 ± 0.05 mm, respectively (Fig. 3).
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 3
www.nature.com/scientificreports/
Figure 4. SEM images of post-dentin disks after silver nitrate penetration. (a) RMGI with PBS. (b) RMGI with
TC. (c) Resin cement with PBS. (d) Resin cement with TC. P, post; C, cement; D, dentin.
Figure 5. Schematic diagrams of the mechanical tests to determine post-dentin interfacial bond strength.
SEM images of the post-dentin disks immersed in silver nitrate (Fig. 4) demonstrated that leakage started
from the surface margin between the cement and dentin, propagated along the corresponding interface and then
entered the dentinal tubules. Significant cracking can also be seen in the RMGI layer.
Discussion
Based on the results from this study, the null hypothesis that there would be no significant difference between the
post-dentin bond strengths measured by the two methods should be rejected.
Although human teeth were not used in this study, there are published papers5,19–22 which show that bovine
teeth are good substitutes for human teeth, and the former are more readily available. While the measured bond
strengths from using bovine teeth may be slightly different from those using human teeth, the main conclusion
that diametral compression is a better test method than the push-out test is unlikely to depend on the tooth tissue
used.
The DC test, as an indirect tensile test, induces a tensile stress in the direction transverse to the applied
compressive load which splits the round specimen into two halves along the loading diameter and part of the
post-dentin interface. By using digital image correlation and measuring acoustic emission, it has been shown
that debonding at the post-dentin interface took place before fracture of the dentin in the disk specimen17. This
is essential for the test to be valid for bond strength measurement. The load-displacement curves obtained from
the DC test were much smoother and more linear up to the point of fracture when compared with those from
the PO test (Fig. 1). Therefore, it was easier to pick out the final failure load from the DC test results, from which
the post-dentin interfacial bond strength could be calculated using the load-stress relationship determined from
the FEA17. In contrast, there were many load peaks and troughs on the curves from the PO test, making it hard
to identify the failure load. Previous studies14,15 showed that friction between the post and dentin resulted in a
stick-slip motion between them during loading beyond initial failure, which led to the many peaks and troughs
on the load-displacement curves from the PO test. Another study further showed that the maximum peak load
was controlled by the amount of friction between the post and dentin23, indicating that the effect of the material’s
fracture properties was secondary. This may explain the small difference in the PO bond strength between the
different groups. More importantly, FEA has shown that the stress along the interface is far from uniform, and
the failure initiation stress is a combination of both shear and tension, the proportions of which being dependent
on the material properties and dimensions of the different components of the specimen18. Therefore, the bond
strength given by the PO test based on the simple formula cannot be regarded as a true material property.
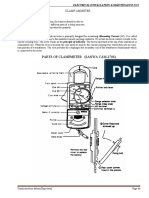
The DC test was much easier to perform compared to the PO test. As shown in Fig. 5, no alignment was nec-
essary for the specimen in the DC test provided the two parallel horizontal plates are sufficiently rigid. For the
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 4
www.nature.com/scientificreports/
Figure 6. FEA model for the diametral compression (DC) test. Due to symmetry, only a quarter of the disk
needs to be modeled.
PO test, on the other hand, the plunger, the post of the disk specimen, and the hole of the support plate all needed
to be aligned concentrically (Fig. 5). A previous study13 also showed that the diameter of the plunger affected the
push-out bond strength measured. Moreover, Fig. 1 shows that the DC test took less time to perform than the PO
test (60 s vs. 300 s).
As presented in Table 1, the standard deviations of the bond strength values given by the PO test were much
higher than those given by the DC test. The coefficients of variation of the bond strength given by the DC method
were no more than 20%, which were in accordance with those from a previous study17. In contrast, the coefficients
of variation of the bond strength from the PO test were around 50%, which also agreed with other studies10–12.
Therefore, the PO technique could be less discriminatory in measuring the bond strength of different restorative
systems. Stick-slip motions due to friction are highly nonlinear and history-dependent, which may explain the
large variability in the PO test results.
The mean values of the tensile bond strength from the DC test were higher than the shear bond strength from
the PO test. It may be true that the shear bond strength of these restorative systems is lower than their tensile
bond strength. However, as mentioned above, the stress distribution along the post-dentin interface in the PO test
specimen is far from uniform, with stress concentrations occurring near the free edges. The actual failure-causing
stress, which is tensile, could therefore be much higher than the average shear stress given by the simple formula.
This difference in stress distribution may explain why different measurement methods could lead to different val-
ues of the same bond strength10. If the maximum tensile stress was used instead to calculate the PO bond strength,
values closer to those given by the DC test might be obtained.
A major disadvantage of the DC test is that FEA (Fig. 6) is required to calculate the tensile bond strength
from the failure load. In contrast, a simple formula is used with the PO test to calculate the shear bond strength.
However, as mentioned, the stress distribution in the PO test specimen is not that of simple shear. As a result, it
will also be affected by the geometrical and material parameters13, and FEA is required to calculate the correct
bond strength.
Aging could affect the post-dentin bond strength. In this study, TC was used to simulate the clinical challenge
in vitro. There were no statistically significant differences in the shear bond strengths given by the PO test between
the groups due to the large coefficients of variation of the results, even though reduction by TC was observed. In
contrast, the tensile bond strength of the thermo-cycled RMGI group given by the DC test was significantly lower
than that of the group without TC. Specimens prepared with resin cement appeared to show stronger resistance to
thermal degradation. The better discriminatory power of the DC method was mainly due to the lower coefficients
of variation in its measured bond strength. A previous study also showed that the bond strengths of various resin
cements to root canal dentin using fiber-reinforced composite posts were significantly reduced by TC24.
The failure-mode analysis revealed that failure occurred predominantly at the interface between the cements
and dentin. The same result was found in other similar studies24–27. The mixed failure mode was also common
in the RMGI specimens, probably because RMGI is relatively brittle, as shown by the cracks in the RMGI layer
(most likely due to drying of the specimens) in the SEM images (Fig. 4). Debonding between the post and dentin
increases the risk of failure of endodontically treated teeth3, which could be accelerated by interfacial leakage.
Micro-CT was used to assess interfacial leakage because it is non-destructive, quantitative and 3D in its analysis.
The results from micro-CT and SEM revealed that interfacial leakage took place between the cements and dentin,
and the volume of silver nitrate penetration in the RMGI disks were much higher than that in the resin cement
disks. One reason for this difference could be that RMGI is a high-shrinkage cement, which resulted in premature
interfacial debonding during setting. Therefore, the cement-dentin interface seemed to be the weakest part of the
restorative system, where the majority of failures initiated.
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 5
www.nature.com/scientificreports/
It may be of interest to compare with the pull-out test, which is another popular test for bond strength test-
ing28–30. It is considered that pull-out test is the best test according to distribution of stress30. However, a large
number of fiber posts have to be used to prepare specimens in pull-out test because a few millimeters of the post
out of the root canal should be leave for pulling action, which leads to the high cost of the experiment28,29. While
for DC test and PO test, the roots filled with fiber posts were trimmed and sliced into disks, which decreased
the use of the fiber posts in our study. On the other side, it is true that the ‘pull-out’ test may suffer less from
post-failure interfacial friction because of the taper of the post. However, similar to the push-out test, failure
of its specimens is likely to be caused by tensile, rather than shear, stress around the surface margin. It is also
well known in experimental mechanics that tensile tests are more problematic due to errors associated with
alignment and local stresses at the attachment points. The actual stress distribution and, hence, failure load will
therefore depend on the geometry and mechanical properties of the materials that form the specimen. As shown
in Fig. 5, the specimens used in our study are easier to perform than the specimens used in pull-out test in other
studies28,30. Clinically, all teeth are subjected to compressive occlusal loads, mixed with some shear or bending,
the degree of mixture being dependent on whether they are anterior or posterior. But they are never subjected to
simple pull-out or tensile load, except during extraction. Of course, further studies are necessary to carry out to
compare the pull-out test with DC test in the future.
Methods
Preparation of post-dentin disks. Forty bovine incisors, which were cleaned by removing the soft tissues
and stored in 0.1% thymol solution at 4 ° C, were used to prepare the specimens. The crown portion above the
cementum-enamel junction (CEJ) and a 3-mm long apical portion of the incisors were cut off with a low-speed
diamond saw (Isomet, Buehler, Lake Bluff, IL, USA). The root canals were enlarged to a 2-mm parallel post space
with a lower speed drill, and then the remaining roots were trimmed into cylinders with an outer diameter of 5
mm. The cylinders were then randomly divided into two groups and inserted with the cylindrical part of fiber
posts (RelyXTM Fiber Posts, 3M ESPE, St. Paul, MN, USA) that were luted with resin cement (RelyXTM Unicem
2, 3M ESPE, St. Paul, MN, USA) or RMGI (RelyXTM Luting Plus, 3M ESPE, St. Paul, MN, USA), following the
manufacturer’s protocol. Finally, the restored cylinders were sliced into 2-mm thick disks, and then stored in
de-ionized water at 4 °C no more than 24 h before testing. The bovine teeth were obtained commercially. All
methods were carried out in accordance with the relevant guidelines and regulations.
Thermo-cycling (TC). Twenty post-dentin disks from each group were thermo-cycled using a two-bath
thermo-cycler (Sabri Dental Enterprises, IL, USA) for 5000 cycles between 5 °C and 55 °C with a dwell time of 30
s in each bath and a transfer time of 10 s between them. After TC, the disks were collected for mechanical tests.
Control groups of post-dentin disks of the same sample size were stored in PBS buffer at 37 °C for the same dura-
tion as that of TC prior to mechanical testing.
Mechanical tests. The interfacial bond strengths of the post-dentin disks were determined using a universal
test machine (858 Mini Bionix II, MTS, MN, USA).
DC was performed with two parallel horizontal steel plates, as shown in Fig. 5. The load was applied in a
stroke-control mode at a loading speed of 0.5 mm/min. The fracture loads of the disks were determined from the
load-displacement curves.
For the PO test (Fig. 5), each disk was positioned on a metal support plate with a central opening (ø = 3
mm) larger than the inner diameter of the disk. The post segment was loaded with a metallic cylindrical plunger
(ø = 1.5 mm), also at a speed of 0.5 mm/min.
Bond strength calculation. For the DC test, the relationship between the maximum post-dentin interfacial
tensile stress and the force applied to the disk was established by using FEA, as shown in Fig. 6. 3D finite element
models were created using the commercial software HyperMesh (version 11.0, Altair, Troy, MI, USA). The fiber
post was considered transversely isotropic and a cement layer of 50 µm thick was also simulated in between den-
tin and fiber post. Young’s moduli for dentin, fiber post and cement were assumed to be 18.6, 9.5 and 7.7 GPa,
respectively17. Poisson’s ratios for them were 0.31, 0.27 and 0.35, respectively17. The models were analyzed by the
software ABAQUS (version 6.10, Rising Sun Mills, Providence, RI, USA). Due to symmetry, only a quarter of the
disk needed to be modeled. The materials and dentin were considered homogeneous, linear elastic and isotropic.
Appropriate boundary conditions (zero displacements in the normal direction) were prescribed along the vertical
and horizontal diameters. A downward point load was applied at the top of the disk to simulate the external load.
The post-dentin tensile bond strength was calculated using the failure load from the load-displacement curve.
For the PO test, the shear bond strength was calculated using the formula P/πdh, where P is the failure load, d
is the inner diameter of the disk, and h is the height of the disk.
Assessment of interfacial leakage between post and dentin. Micro-CT in combination with a radi-
opaque dye (silver nitrate, AgNO3) was used to assess leakage through the post-dentin margin31,32. Three freshly
prepared disks from each group were painted with an acid-resistant nail varnish, leaving one side of the post and
a perimeter of ~0.3-mm wide around it exposed. The painted disks were submerged into a 50% (w/w) solution
of AgNO3. After 24 h of storage at room temperature, they were taken out for micro-CT scanning (XT H 225,
Nikon Metrology Inc., Brighton, MI, USA). The scanning parameters were 90 kV, 90 μA, 708 ms of exposure, 720
projections and 4 frames per projection. After scanning, 3D reconstruction was performed using the software CT
Pro 3D (Nikon metrology, Inc., Brighton, MI, USA). A cylindrical volume of interest (VOI) was generated around
the posts to calculate the volume of silver nitrate that had penetrated into the post-dentin disks.
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 6
www.nature.com/scientificreports/
Scanning electron microscopy. Scanning electron microscopy (SEM) was used to examine the fracture
modes of the disks subjected to mechanical testing and the path of interfacial leakage of those immersed in
AgNO3. It was conducted in a tabletop scanning electron microscope (TM-3000, Hitachi, Japan) at an accel-
erating voltage of 15 kV and in combo observation mode. The fractured disks were fixed on an aluminum stub
with conductive carbon tapes. The painted post-dentin disks (n = 3 per group) treated in AgNO3 solution, as
performed in above, were sectioned longitudinally and polished with 1200 grit sandpapers before SEM scanning
to determine the infiltration depth.
Statistical analysis. Assumptions of normal distribution were evaluated by Kolmogorov-Smirnov test. Two
tailed t test was carried out by R (3.3.1, R Core Team, Vienna, Austria) to compare the bond strength between
the groups (resin cement vs. RMGI, with or without thermal cycling). The level of statistical significance was set
at 0.05.
Data availability statement. Materials and data are available from the corresponding authors.
References
1. Schwartz, R. S. & Robbins, J. W. Post placement and restoration of endodontically treated teeth: A literature review. J Endod 30,
289–301 (2004).
2. Ingle, J. I. B. L. & Baumgartner, J. C. Ingle’s endodontics. (6th ed. BC Decker Inc., 2008).
3. Santos, A. F. V. et al. Can Fiber Posts Increase Root Stresses and Reduce Fracture? J Dent Res 89, 587–591 (2010).
4. Monticelli, F. et al. Effects of adhesive systems and luting agents on bonding of fiber posts to root canal dentin. J Biomed Mater Res B
77B, 195–200 (2006).
5. Valandro, L. F., Andreatta, O. D., Valera, M. C. & de Araujo, M. A. M. The effect of adhesive systems on the pullout strength of a
fiberglass-reinforced composite post system in bovine teeth. J Adhes Dent 7, 331–336 (2005).
6. Boschian Pest, L., Cavalli, G., Bertani, P. & Gagliani, M. Adhesive post-endodontic restorations with fiber posts: push-out tests and
SEM observations. Dent Mater 18, 596–602 (2002).
7. Goracci, C., Grandini, S., Bossu, M., Bertelli, E. & Ferrari, M. Laboratory assessment of the retentive potential of adhesive posts: A
review. J Dent 35, 827–835 (2007).
8. Soares, C. J. et al. Finite element analysis and bond strength of a glass post to intraradicular dentin: Comparison between
microtensile and push-out tests. Dent Mater 24, 1405–1411 (2008).
9. Drummond, J. L. In vitro evaluation of endodontic posts. Am J Dent 13, 5B–8B (2000).
10. Goracci, C. et al. The adhesion between fiber posts and root canal walls: comparison between microtensile and push-out bond
strength measurements. Eur J Oral Sci 112, 353–361 (2004).
11. Dimitrouli, M., Geurtsen, W. & Luhrs, A. K. Comparison of the push-out strength of two fiber post systems dependent on different
types of resin cements. Clin Oral Invest 16, 899–908 (2012).
12. Giachetti, L., Grandini, S., Calamai, P., Fantini, G. & Russo, D. S. Translucent fiber post cementation using light- and dual-curing
adhesive techniques and a self-adhesive material: Push-out test. J Dent 37, 638–642 (2009).
13. Chen, W. P., Chen, Y. Y., Huang, S. H. & Lin, C. P. Limitations of Push-out Test in Bond Strength Measurement. J Endod 39, 283–287
(2013).
14. Lin, G., Geubelle, P. H. & Sottos, N. R. Simulation of fiber debonding with friction in a model composite pushout test. Int J Solids
Struct 38, 8547–8562 (2001).
15. Chandra, N. & Ghonem, H. Interfacial mechanics of push-out tests: theory and experiments. Compos Part a-Appl S 32, 575–584
(2001).
16. Fahad, M. K. Stresses and failure in the diametral compression test. J Mater Sci 31, 3723–3729 (1996).
17. Huang, S. H. et al. A novel dentin bond strength measurement technique using a composite disk in diametral compression. Acta
Biomater 8, 1597–1602 (2012).
18. Huang, S. H., Lin, L. S., Fok, A. S. L. & Lin, C. P. Diametral compression test with composite disk for dentin bond strength
measurement - Finite element analysis. Dent Mater 28, 1098–1104 (2012).
19. Li, Y. et al. Degradation in the dentin-composite interface subjected to multi-species biofilm challenges. Acta Biomater 10, 375–383
(2014).
20. Nakamichi, I., Iwaku, M. & Fusayama, T. Bovine Teeth as Possible Substitutes in the Adhesion Test. J Dent Res 62, 1076–1081 (1983).
21. Schmalz, G., Hiller, K. A., Nunez, L. J., Stoll, J. & Weis, K. Permeability characteristics of bovine and human dentin under different
pretreatment conditions. J Endod 27, 23–30 (2001).
22. Schilke, R., Bauss, O., Lisson, J. A., Schuckar, M. & Geurtsen, W. Bovine dentin as a substitute for human dentin in shear bond
strength measurements. Am J Dent 12, 92–96 (1999).
23. Goracci, C. et al. The contribution of friction to the dislocation resistance of bonded fiber posts. J Endod 31, 608–612 (2005).
24. Bitter, K. et al. Effects of luting agent and thermocycling on bond strengths to root canal dentine. Int Endod J 39, 809–818 (2006).
25. Sahinkesen, G., Erdemir, U., Oktay, E. A. & Sancakli, H. S. The effect of post surface silanization and luting agents on the push-out
bond strengths of adhesively inserted fiber reinforced posts. Int J Adhes Adhes 31, 265–270 (2011).
26. Zicari, F. et al. Bonding effectiveness and sealing ability of fiber-post bonding. Dent Mater 24, 967–977 (2008).
27. Bitter, K., Paris, S., Pfuertner, C., Neumann, K. & Kielbassa, A. M. Morphological and bond strength evaluation of different resin
cements to root dentin. Eur J Oral Sci 117, 326–333 (2009).
28. Ebert, J. et al. Bond strength of adhesive cements to root canal dentin tested with a novel pull-out approach. J Endod 37, 1558–1561
(2011).
29. Castellan, C. S., Santos-Filho, P. C., Soares, P. V., Soares, C. J. & Cardoso, P. E. Measuring bond strength between fiber post and root
dentin: a comparison of different tests. J Adhes Dent 12, 477–485 (2010).
30. Khoroushi, M., Sheikhi, M., Khalilian-Gourtani, A. & Soleimani, B. Effect of root canal rinsing protocol on dentin bond strength of
two resin cements using three different method of test. J Clin Exp Dent 8, e246–254 (2016).
31. Carrera, C. A. et al. The use of micro-CT with image segmentation to quantify leakage in dental restorations. Dent Mater 31,
382–390 (2015).
32. Zhu, L. et al. Calibration of a lactic-acid model for simulating biofilm-induced degradation of the dentin-composite interface. Dent
Mater 33, 1315–1323 (2017).
Acknowledgements
This work was supported by the National Institute of Health (Grant No. R01 DE021366); the National Natural
Science Foundation of China (Grant No. 81200774); and Shanghai Colleges and Universities Young Teachers
Training Funding (Grant No. ZZjdyx13120).
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 7
www.nature.com/scientificreports/
Author Contributions
A.F. designed the research; L.K.Z., Y.P.L. and C.A.C. performed the experiments; Y.C.C. carried out FEA; C.W.
analyzed the data; L.K.Z. wrote the original draft; Y.P.L. and A.F. reviewed and edited the manuscript.
Additional Information
Competing Interests: The authors declare that they have no competing interests.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and
institutional affiliations.
Open Access This article is licensed under a Creative Commons Attribution 4.0 International
License, which permits use, sharing, adaptation, distribution and reproduction in any medium or
format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Cre-
ative Commons license, and indicate if changes were made. The images or other third party material in this
article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the
material. If material is not included in the article’s Creative Commons license and your intended use is not per-
mitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the
copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
© The Author(s) 2018
ScIENTIfIc Reports | (2018) 8:2350 | DOI:10.1038/s41598-018-20891-3 8
You might also like
- Field Evaluation of Undrained Shear Strength From Piezocone Penetration Tests in Soft Marine ClayDocument12 pagesField Evaluation of Undrained Shear Strength From Piezocone Penetration Tests in Soft Marine ClayDr.Ch.Rama Vara Prasad Assistant Professor, CE, VRSECNo ratings yet
- BD2F BS3F Service Manual OCRDocument340 pagesBD2F BS3F Service Manual OCRWere Wolf100% (2)
- C15 On-Highway Engine Electrical System: Harness and Wire Electrical Schematic SymbolsDocument2 pagesC15 On-Highway Engine Electrical System: Harness and Wire Electrical Schematic Symbolsminh le huu100% (3)
- Version 1.1 XLam Australia Design GuideDocument26 pagesVersion 1.1 XLam Australia Design Guidesant1411No ratings yet
- Kelly 1999Document10 pagesKelly 1999حسين يوسفNo ratings yet
- Content ServerDocument12 pagesContent ServerusrazvanNo ratings yet
- Analysis of Bond Stress Distribution For Prestressing Strand by StandardDocument8 pagesAnalysis of Bond Stress Distribution For Prestressing Strand by StandardSameerKareeeemNo ratings yet
- Shear Bond Strength Test Using Different Loading Conditions - A Finite Element AnalysisDocument4 pagesShear Bond Strength Test Using Different Loading Conditions - A Finite Element AnalysisAmitNo ratings yet
- Cono Morse Hung Chih Chang 2020Document8 pagesCono Morse Hung Chih Chang 2020Jose Manuel de la FuenteNo ratings yet
- J Korean Acad Conserv DentDocument22 pagesJ Korean Acad Conserv Dentsweet_apple921587No ratings yet
- Bonding Effectiveness of Composite-Dentin Interfaces After Mechanical Loading With A New Device (Rub&Roll)Document7 pagesBonding Effectiveness of Composite-Dentin Interfaces After Mechanical Loading With A New Device (Rub&Roll)Verônica Pereira de LimaNo ratings yet
- Tabelt HARDNESS and BULK DENSITYDocument8 pagesTabelt HARDNESS and BULK DENSITYAnkurNo ratings yet
- SPT Test Influenced by FrictionDocument6 pagesSPT Test Influenced by FrictionNabeel YounasNo ratings yet
- 2009 KarthikDocument8 pages2009 KarthikAnis SuissiNo ratings yet
- 25 Bulaqi 25Document10 pages25 Bulaqi 25Anaïs CATELINNo ratings yet
- (2014 PARMAR E JAMNU) Experimental Study On Direct Pull Out TestDocument6 pages(2014 PARMAR E JAMNU) Experimental Study On Direct Pull Out TestmanoelmangabeiraNo ratings yet
- Tensile Strength of Mass Concrete 913-938 PDFDocument28 pagesTensile Strength of Mass Concrete 913-938 PDFchutton681No ratings yet
- The Effect of Different Occlusal Contact Situations On Peri-Implant Bone Stress A Contact Finite Element Analysis of Indirect Axial LoadingDocument7 pagesThe Effect of Different Occlusal Contact Situations On Peri-Implant Bone Stress A Contact Finite Element Analysis of Indirect Axial LoadingPascal RachmanNo ratings yet
- C Attachment 76 673Document12 pagesC Attachment 76 673DrSuman ManandharNo ratings yet
- Ti6 4 PropertiesDocument9 pagesTi6 4 PropertiesSrihari DNo ratings yet
- Shear Tests On PhyllitesDocument8 pagesShear Tests On PhyllitesDelvin JacobsNo ratings yet
- Flexural Strength and Weibull Analysis of A Microhybrid and A Nanofill Composite Evaluated by 3-And 4-Point Bending TestsDocument6 pagesFlexural Strength and Weibull Analysis of A Microhybrid and A Nanofill Composite Evaluated by 3-And 4-Point Bending TestsIbrahim HaddamNo ratings yet
- 1 s2.0 S1365160918311225 MainDocument12 pages1 s2.0 S1365160918311225 Mainfalla85No ratings yet
- Composites: Part B: Adnan Fazal, Kevin S. FanceyDocument8 pagesComposites: Part B: Adnan Fazal, Kevin S. FanceyNicolás OjedaNo ratings yet
- Yield Characteristics Strengthening and Yield StreDocument20 pagesYield Characteristics Strengthening and Yield Stremouhidine.dhahriNo ratings yet
- Analysis and Discussion On Impact Shear Experiment Technique of Composite LaminateDocument4 pagesAnalysis and Discussion On Impact Shear Experiment Technique of Composite Laminate李华No ratings yet
- Modified Relationship Between Point Loading Strength and Uniaxial Compressive Strength by DEMDocument8 pagesModified Relationship Between Point Loading Strength and Uniaxial Compressive Strength by DEMDaniel SanchezNo ratings yet
- Fracture Strength and Fracture Patterns of Root-Filled Teeth Restored With Direct Resin Composite Restorations Under Static and Fatigue LoadingDocument8 pagesFracture Strength and Fracture Patterns of Root-Filled Teeth Restored With Direct Resin Composite Restorations Under Static and Fatigue LoadingLala LalaNo ratings yet
- Correlations Between Direct and Indirect StrengthDocument7 pagesCorrelations Between Direct and Indirect Strengthvishal kumarNo ratings yet
- Evaluation of Different in Vitro Testing Methods For Mechanical Properties of Veneer CeramicsDocument8 pagesEvaluation of Different in Vitro Testing Methods For Mechanical Properties of Veneer CeramicsDrg Sri Pandu UtamiNo ratings yet
- OgBayrak - Response Prediction by Plastic Hinge AnalysisDocument6 pagesOgBayrak - Response Prediction by Plastic Hinge AnalysisRui CbNo ratings yet
- Nonlinear Cohesive Interface Finite Element FormulationDocument232 pagesNonlinear Cohesive Interface Finite Element FormulationasimbuyukNo ratings yet
- 1 PBDocument5 pages1 PBeliasvissers36No ratings yet
- Correlations Between Direct and Indirect Strength PDFDocument7 pagesCorrelations Between Direct and Indirect Strength PDFgök kutkutNo ratings yet
- Asvanund P Et Al. 2011 (JPD) PDFDocument6 pagesAsvanund P Et Al. 2011 (JPD) PDFAlla MushkeyNo ratings yet
- Wellbore Stability Evaluation Method Based On The Continuous Tangent Envelope of A Mohr CircleDocument21 pagesWellbore Stability Evaluation Method Based On The Continuous Tangent Envelope of A Mohr CircleAhmed Nadhem AlshamsiNo ratings yet
- Ad 0603929Document57 pagesAd 0603929Anonymous uqEd11hn6fNo ratings yet
- Evaluation of The Force Degradation and Deformation of The Open Closed and Open SpringsDocument8 pagesEvaluation of The Force Degradation and Deformation of The Open Closed and Open SpringsALBERTO JESUS PACHECO DIAZNo ratings yet
- Iwamoto 2003Document6 pagesIwamoto 2003NICOLENo ratings yet
- DT FrctureDocument27 pagesDT FrctureR JNo ratings yet
- Flexible Adhesives Workshop Handout 12june01Document4 pagesFlexible Adhesives Workshop Handout 12june01vilukNo ratings yet
- Comparison of ShearDocument5 pagesComparison of ShearmergNo ratings yet
- J Conbuildmat 2011 08 002Document9 pagesJ Conbuildmat 2011 08 002Haider AliNo ratings yet
- Abdullah 2021 IOP Conf. Ser. Mater. Sci. Eng. 1144 012033Document8 pagesAbdullah 2021 IOP Conf. Ser. Mater. Sci. Eng. 1144 012033GenNo ratings yet
- RCT-implant StabilityDocument12 pagesRCT-implant Stabilityformula marolisNo ratings yet
- Stress Inhomogeneity in Powder Specimens Tested in The Jenike Shear Cell: Myth or Fact?Document10 pagesStress Inhomogeneity in Powder Specimens Tested in The Jenike Shear Cell: Myth or Fact?Andres VallebellaNo ratings yet
- Factor C 2014Document8 pagesFactor C 2014lourdesmaritzatancararamosNo ratings yet
- Jeong 2006bDocument13 pagesJeong 2006bSHARON RAPHAELNo ratings yet
- NSI FracTip Volume4 Number1Document2 pagesNSI FracTip Volume4 Number1Callum WoodwardNo ratings yet
- PRELIMINARY FINDINGS ON SIZE EFFECT IN ECC Structural Members in FlexureDocument10 pagesPRELIMINARY FINDINGS ON SIZE EFFECT IN ECC Structural Members in FlexuresardarumersialNo ratings yet
- Bulaqi 2015Document7 pagesBulaqi 2015Padmini ReddyNo ratings yet
- Effects of Core-To-Dentin Thickness Ratio On The Biaxial Flexural Strength, Reliability, and Fracture Mode of Bilayered Materials of Zirconia Core (Y-TZP) and Veneer Indirect Composite ResinsDocument8 pagesEffects of Core-To-Dentin Thickness Ratio On The Biaxial Flexural Strength, Reliability, and Fracture Mode of Bilayered Materials of Zirconia Core (Y-TZP) and Veneer Indirect Composite ResinsDanny Eduardo RomeroNo ratings yet
- Dynamic Failure of Metallic Cellular MaterialsDocument7 pagesDynamic Failure of Metallic Cellular MaterialsHuseinNo ratings yet
- REVIEW - The Microtensile Bond TestDocument12 pagesREVIEW - The Microtensile Bond TestElmer Acevedo0% (1)
- Bond Strength of Six Soft Denture Liners Processed Against Polymerized and Unpolymerized Poly (Methyl Methacryiate)Document5 pagesBond Strength of Six Soft Denture Liners Processed Against Polymerized and Unpolymerized Poly (Methyl Methacryiate)Naresh TeresNo ratings yet
- Experimental Study On Behavior of Time-Related Preload Relaxation ForDocument10 pagesExperimental Study On Behavior of Time-Related Preload Relaxation ForengenhariainovajdNo ratings yet
- Effects of Direct and Indirect Bonding Techniques PDFDocument9 pagesEffects of Direct and Indirect Bonding Techniques PDFAlvaro ChacónNo ratings yet
- Effect of Fabrication Technique and Thermal Cycling On The Bond Strength of CAD/CAM Milled Custom Fit Anatomical Post and Cores: An in Vitro StudyDocument8 pagesEffect of Fabrication Technique and Thermal Cycling On The Bond Strength of CAD/CAM Milled Custom Fit Anatomical Post and Cores: An in Vitro StudyDeisy Angarita FlorezNo ratings yet
- Stability of Implant-Abutment Interface With A Hexagon-Mediated Butt Joint: Failure Mode and Bending ResistanceDocument8 pagesStability of Implant-Abutment Interface With A Hexagon-Mediated Butt Joint: Failure Mode and Bending ResistancedwinugrohojuandaNo ratings yet
- New Local Compression Test To Estimate in Situ Compressive Strength of Masonry Mortar PDFDocument10 pagesNew Local Compression Test To Estimate in Situ Compressive Strength of Masonry Mortar PDFValentina Alvarado VesgaNo ratings yet
- An Approach To Compensate For The Influence of The System Normal Stiffness in CNS Direct Shear TestsDocument15 pagesAn Approach To Compensate For The Influence of The System Normal Stiffness in CNS Direct Shear TestsAdam LinesNo ratings yet
- Oral and Periodontal Risk Factors of Prosthetics Success For 3 Unit Natural Tooth-Supported Bridges Vs Implant-Supported Fixed Dental ProthesesDocument12 pagesOral and Periodontal Risk Factors of Prosthetics Success For 3 Unit Natural Tooth-Supported Bridges Vs Implant-Supported Fixed Dental ProthesesPao JanacetNo ratings yet
- MaterialsDocument18 pagesMaterialsPao JanacetNo ratings yet
- Triclosan To Improve The Antimicrobial Performance of Universal AdhesivesDocument19 pagesTriclosan To Improve The Antimicrobial Performance of Universal AdhesivesPao JanacetNo ratings yet
- Evaluating The Fracture Resistance of Fiber Reinforced Composite Restorations - An in Vitro AnalysisDocument8 pagesEvaluating The Fracture Resistance of Fiber Reinforced Composite Restorations - An in Vitro AnalysisPao JanacetNo ratings yet
- Long-Term in Vitro Adhesive Properties of Two UniversalDocument13 pagesLong-Term in Vitro Adhesive Properties of Two UniversalPao JanacetNo ratings yet
- Combined Technique With Dentin PostDocument5 pagesCombined Technique With Dentin PostPao JanacetNo ratings yet
- Rehabilitation of A Mutilated Maxillary Central IncisorDocument5 pagesRehabilitation of A Mutilated Maxillary Central IncisorPao JanacetNo ratings yet
- Khandelwal 2011Document7 pagesKhandelwal 2011Pao JanacetNo ratings yet
- Efficacy of Ribbond and A Fibre Post On The Fracture Resistance of Reattached Maxillary Central Incisors With Two Fracture PatternsDocument6 pagesEfficacy of Ribbond and A Fibre Post On The Fracture Resistance of Reattached Maxillary Central Incisors With Two Fracture PatternsPao JanacetNo ratings yet
- Dental Alloys Used For Crown and Bridge Restorations by Dentyal Technicians in New ZealandDocument8 pagesDental Alloys Used For Crown and Bridge Restorations by Dentyal Technicians in New ZealandPao JanacetNo ratings yet
- MaterialsDocument13 pagesMaterialsPao JanacetNo ratings yet
- Comparing Castability of Nickel-Chromium, Cobalt-Chromium, and NonPrecious Gold Color AlloysDocument7 pagesComparing Castability of Nickel-Chromium, Cobalt-Chromium, and NonPrecious Gold Color AlloysPao JanacetNo ratings yet
- Effect of Sprue Design in Nickel-Chromium Cast Crown Margin (Bebedero)Document8 pagesEffect of Sprue Design in Nickel-Chromium Cast Crown Margin (Bebedero)Pao JanacetNo ratings yet
- Lec. 1 Introduction CHEN101 Fall 2020Document30 pagesLec. 1 Introduction CHEN101 Fall 2020ahmed kaedNo ratings yet
- NKB Report 1996 04E ImplementationISO717RatingMethodsEuropeDocument63 pagesNKB Report 1996 04E ImplementationISO717RatingMethodsEuropeMARCOS DE BARROSNo ratings yet
- Free Standing Masonry Wall Design Based On TMS 402-16/13 & ACI 318-19Document6 pagesFree Standing Masonry Wall Design Based On TMS 402-16/13 & ACI 318-19biceli samet1No ratings yet
- 03.technical Data of Oil-Immersed Hermetically Sealed TransformerDocument2 pages03.technical Data of Oil-Immersed Hermetically Sealed TransformerMachanical PtwitNo ratings yet
- Maxwells Theorem of Reciprocal Displacements Bettis LawDocument7 pagesMaxwells Theorem of Reciprocal Displacements Bettis LawJC DOBLON100% (1)
- Arteche DS Acf-36 enDocument2 pagesArteche DS Acf-36 enasistente.licitacionesNo ratings yet
- X V LWH V 256 Surface Area 2lw+2lh+2hwDocument7 pagesX V LWH V 256 Surface Area 2lw+2lh+2hwEDWINNo ratings yet
- Surveying FinalsDocument166 pagesSurveying Finalsmaykel.evascoNo ratings yet
- CHE 514 SyllabusDocument3 pagesCHE 514 SyllabusVictor GainaNo ratings yet
- Question Bank For MWE IAT 1Document2 pagesQuestion Bank For MWE IAT 1Ved BhandareNo ratings yet
- Ex - No (2) : The Slider-Crank and Scotch-Yoke MechanismDocument12 pagesEx - No (2) : The Slider-Crank and Scotch-Yoke MechanismMasoud doskiNo ratings yet
- Also Refer Last Year Question Papers in Stucor AppDocument10 pagesAlso Refer Last Year Question Papers in Stucor AppRaagul SNo ratings yet
- AbdisDocument23 pagesAbdisabdiNo ratings yet
- Heat Conduction-Composite WallDocument3 pagesHeat Conduction-Composite WallJady chess24No ratings yet
- CE8311 - Construction Materials Laboratory Manual - by LearnEngineering - in PDFDocument50 pagesCE8311 - Construction Materials Laboratory Manual - by LearnEngineering - in PDFGayu100% (1)
- Review of Related LiteratureDocument10 pagesReview of Related LiteratureJesselle CelestialNo ratings yet
- TECHNOLOGY5 AnswerDocument8 pagesTECHNOLOGY5 AnswerNashaat DhyaaNo ratings yet
- FiltersDocument7 pagesFiltersBhishma Kant VermaNo ratings yet
- IRDE Raipur (1), Karanpur (2), Dehradun Mob: 9997506700, 9536092109 Max Marks: 20 Time 1hrDocument1 pageIRDE Raipur (1), Karanpur (2), Dehradun Mob: 9997506700, 9536092109 Max Marks: 20 Time 1hrPrateek ChandnaNo ratings yet
- Iron Horse DCMDocument43 pagesIron Horse DCMBlack DiamoondNo ratings yet
- ACSEE Physics F5 T1 S2 ErrorsDocument2 pagesACSEE Physics F5 T1 S2 Errorskishka mbwiNo ratings yet
- Project Report of Air Cooler Using PeltierDocument49 pagesProject Report of Air Cooler Using PeltierSantosh BansodeNo ratings yet
- Fde MCQDocument14 pagesFde MCQahmedNo ratings yet
- High Energy Rate Forming ProcessesDocument47 pagesHigh Energy Rate Forming ProcessesArun SrivastanNo ratings yet
- 18bt01036 FFO Lab ManualDocument25 pages18bt01036 FFO Lab ManualSarthak LathiyaNo ratings yet
- Millimeter Wave Microstrip Patch Antenna For 5G MoDocument6 pagesMillimeter Wave Microstrip Patch Antenna For 5G MoOwaisKhanNo ratings yet
- Parts of Clampmeter (Sanwa Cam-270S) : Clamp AmmeterDocument4 pagesParts of Clampmeter (Sanwa Cam-270S) : Clamp AmmeterFERDINAND BANAGANo ratings yet