Professional Documents
Culture Documents
Out-Of-hospital Cardiac Arrest Survival in Athens 2019
Out-Of-hospital Cardiac Arrest Survival in Athens 2019
Uploaded by
Yannis ZoldenbergCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Out-Of-hospital Cardiac Arrest Survival in Athens 2019
Out-Of-hospital Cardiac Arrest Survival in Athens 2019
Uploaded by
Yannis ZoldenbergCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/334327962
Out-of-hospital cardiac arrest survival in Athens: Data from a Greek public
hospital
Article in Emergency Care Journal · July 2019
DOI: 10.4081/ecj.2019.8249
CITATIONS READS
0 68
7 authors, including:
Zisimangelos Solomos Konstantinos Miltiadou
Médecins du Monde, Greece Attikon University Hospital
9 PUBLICATIONS 0 CITATIONS 13 PUBLICATIONS 8 CITATIONS
SEE PROFILE SEE PROFILE
Aikaterini Petropoulou
National and Kapodistrian University of Athens
7 PUBLICATIONS 56 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Biomaterials View project
All content following this page was uploaded by Zisimangelos Solomos on 09 July 2019.
The user has requested enhancement of the downloaded file.
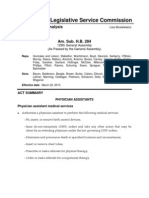
Emergency Care Journal 2019; volume 15:8249
Out-of-hospital cardiac arrest survival in Athens:
Data from a Greek public hospital
Zisimangelos S. Solomos,1 Maria S. Τatsi,2 Victoria E. Psomiadou,3 Angeliki D. Tsifi,4
Dimitrios S. Theodoridis,5 Aikaterini P. Petropoulou,6 Konstantinos G. Miltiadou7
1
Internal Medicine, ‘Medecins du Monde’, Greek Delegation, Athens; 2Department of General Surgery,
Pammakaristos General Hospital, Athens; 3Department of Gynaecological Oncology, Metaxa Memorial
Cancer Hospital, Piraeus; 4Intensive Care Unit, Konstantopouleio-Patision General Hospital, Athens;
5
Department of Haematology, Konstantopouleio-Patision General Hospital, Athens; 6Dental School,
University of Athens, Athens; 7Hepatogastroenterology Unit, 2nd Department of Internal Medicine -
Propaedeutic, Research Institute and Diabetes Center, Medical School, National and Kapodistrian
University, Attikon University General Hospital, Athens, Greece
tion (ROSC) and 24-hour survival ratios. Our secondary objective
Abstract was to estimate 30-day survival. Demographic data was also col-
Although out-of-hospital cardiac arrests (OHCA) are a major lected. 283 OHCA were included in the study. The mean age was
67.2 years and the male: female ratio was 2. Medical history was
ly
cause of mortality internationally, data regarding survival in
Greece remains scarce and inconclusive. The aim of this study is available for 33.6% of patients. 72.1% of cases were transferred to
on
to assess the immediate and 24-hour survival of OHCA sufferers the emergency department by ambulance and 2.8% by private
during a 5-year period in a public hospital in Athens. A retrospec- means of transport. Cardiopulmonary resuscitation was attempted
on 57.6% of cardiac arrests, 8.6% regained ROSC and 6.1% sur-
tive study was conducted on all cardiac arrests that were trans-
e
vived for 24 hours. The 30-day survival was expected to be less
ferred to our hospital during a five-year period (2011-2015). Our
than 3.5%. In our institution, ROSC, 24-hour and expected 30-day
us
primary objective was to calculate return of spontaneous circula-
survival were lower than the European average and in accordance
with the recent prospective Eureca One study. However, data from
our institution cannot be generalised and multicenter studies are
al
required in order to clarify OHCA outcomes in Greece.
ci
Correspondence: Zisimangelos S. Solomos, Internal Medicine,
er
‘Medecins du Monde’, Greek Delegation, Dimitrakopoulou str. 130,
P.C. 11741, Koukaki Area, Athens, Greece. Introduction
m
Tel: +302103809899.
E-mail: zisimosmed@gmail.com Out-of-hospital cardiac arrest (OHCA) is a major cause of mor-
tality internationally, with 275,000 and 420,000 annual deaths in
om
Key words: Out-of-hospital cardiac arrest; Cardiopulmonary resuscita- Europe and the United States respectively.1 Data regarding the sur-
tion; Mortality; Greek hospital. vival of OHCA victims in Greece remain scarce and mostly derive
from a handful of single-center studies2,3 that do not estimate 30-day
-c
Contributions: ZSS and KGM authored and edited the manuscript; survival or survival to hospital discharge, in contrast with similar
ADT, VEP, MST, APP, DST searched and extracted data from medical
studies from other European Union (EU) countries.4 Additionally,
on
files. ZSS and APP analysed the data.
although the superiority of cardiopulmonary resuscitation (CPR)
Conflict of interest: the authors declare no potential conflict of interest. certified from uncertified medical personnel in increasing OHCA
N
survival has been well described in regional studies,2,5 inadequacies
Funding: none. in CPR skills of the medical and nursing staff in various Greek hos-
pitals, especially in institutions with relatively small incidence of
Conference presentation: data from the study were submitted as two cardiac arrests,6 have been reported in the literature.7-10
poster presentations at the 2016 World Congress of Internal Medicine The aim of this study is to assess the immediate and 24-hour
(22-25 August, Bali, Indonesia) and at the 2016 European Resuscitation
survival of OHCA victims, as well as CPR efficiency of healthcare
Congress (24-25 September, Reykjavik, Iceland).
personnel during a 5-year period in a public hospital emergency
Received for publication: 24 April 2019. department (ER) in Athens, in order to increase the available data
Revision received: 3 June 2019. regarding OHCA mortality in Greece.
Accepted for publication: 6 June 2019.
This work is licensed under a Creative Commons Attribution 4.0
License (by-nc 4.0). Materials and Methods
©Copyright:the Author(s), 2019 A retrospective study was conducted on all OHCA victims that
Licensee PAGEPress, Italy were transferred to the ER of our institution (Pammakaristos
Emergency Care Journal 2019; 15:8249 General Hospital of Athens), during a five-year period (2011-
doi:10.4081/ecj.2019.8249 2015). Our hospital is a middle-sized public general hospital, with
approximately 170 beds that is located in a densely populated area
[page 64] [Emergency Care Journal 2019; 15:8249]
Article
of the (Kato Patisia) center of Athens. It is on call every 4 days and, From those OHCA patients on whom CPR was performed,
along with 2 middle-sized (Konstantopouleio, Amalia Fleming) 8.6% (14) regained ROSC and 6.1% (10) survived for 24 hours
and 3 larger (Giorgos Gennimatas, Tzaneio, Sotiria) tertiary hospi- (Table 2 and Figure 1). The immediate ROSC and 24-hour survival
tals,11 covers the emergencies for the entire urban population of rates for the whole 5-year period (including the total number of
Athens (approximately 3 million).12 OHCA, irrespective of CPR provision or not) in our hospital were
Upon occurrence of an OHCA, the dispatched ambulance con- 5% and 3.5% respectively. The 30-day survival and survival to
tacts the hospital several minutes before arriving to the ER, in hospital discharge ratios could not be calculated in this particular
order for the resuscitation team to be assembled. The latter usually study, but can be expected to be equal to or less than the calculated
consists of the (resident or senior) internist, cardiologist and anes- 24-hour survival ratio (3.5%).
thesiologist on call, as well as at least one nurse. The CPR is pro-
vided in a specifically equipped resuscitation room in the ER and
commences immediately upon arrival of the ambulance. If return
of spontaneous circulation (ROSC) occurs, the patient is admitted Discussion
to one of the hospital’s advanced care units (total capacity of six According to the data acquired from our institution during the
beds) for monitoring. The national Emergency Medical Services 5-year study period, initiation of resuscitation efforts by our arrest
(EMS/EKAV) center is then contacted and the survivor is regis-
tered as a tertiary hospital intensive care unit (ICU) candidate. In
case of ICU bed availability, the EMS center arranges for the trans-
fer of the patient with an ambulance. In case of bed unavailability,
the registration of the survivor is renewed every 24 hours by the
current hospital’s doctor on call.
ly
After the submission of the research protocol and the approval
from the institution’s scientific and administrative committees,
on
access to the hospital’s archive was granted. All OHCA entries in
the ER patient registry for the years 2011-2015 were collected. The
data acquired, included date of ER admission, sex, age, means of
e
transport to the hospital (ambulance or private), whether CPR was us
provided to the victim, outcome of CPR (ROSC or death) and
where available, medical history. In case of ROSC and hospital
admission, the patients’ medical records were collected from the
al
hospital’s archive to assess 24-hour survival.
Our primary objective was to calculate ΟHCA immediate
ci
(ROSC) and 24-hour survival ratios. Our secondary objectives
er
were to calculate ROSC per CPR attempt ratio and to estimate 30-
day survival and survival to hospital discharge.
m
Figure 1. Out-of-hospital cardiac arrest (OHCA) victims, car-
Cardiac arrest victims above 90 years of age or with a history
diopulmonary resuscitation (CPR) attempts, immediate and 24-
of generalized neoplastic disease were excluded from the study, as
h survivors per year of study. ROSC, return of spontaneous circu-
om
benefit from CPR on those patients was already expected to be
lation.
insignificant.13-17
-c
Table 1. Medical history of out-of-hospital cardiac arrests
on
Results
patients.
Patients with available history (n=95)
During the 5-year period of the study, 301 OHCA were trans-
N
ferred to the hospital’s ER. 6% (18) were excluded from the dedi-
Arterial hypertension 7
cated part of the study because they met the exclusion criteria
Chronic obstructive pulmonary disease 4
(above 90 years of age, generalized neoplastic disease) thus reduc- Central motor neuron disease 2
ing the study population to 283 cases. Congenital cardiac disease 2
The mean age of the patients was 67.2 years and the male:
female ratio was 2. Medical history was documented for only
Aortic aneurysm 1
33.6% (95) of OHCA victims, with 32.6% (31) of them having
Alcohol or substance abuse 4
coronary artery disease (Table 1). 72.1% (204) of cases were trans-
Presence of pacemaker 7
ferred to the ER by ambulance, 2.8% (8) were transferred by pri-
Coronary artery disease 31
vate means of transport, while in 25.1% (71) of the cases the means Cardiomyopathies 3
of transport was not documented. Cardiac valvular disease 3
CPR was attempted on 57.6% (163) of cardiac arrests. No sur-
vival benefit was expected from CPR provision for the rest 42.4%
Diabetes Mellitus 10
(120) of the cases (prolonged cardiac arrest with no bystander or
Stroke 2
EMS personnel provision of CPR for >15 min, extensive delay of
No history 4
ambulance response and travel time to ER, presence of asystole for
Other 15
more than 30 min prior to ER transfer), thus CPR was not attempt- Patients with undocumented history (n=188).
ed by the hospital’s medical personnel. Total (n=283)
[Emergency Care Journal 2019; 15:8249] [page 65]
Article
Table 2. Summary data per year of study.
Year OHCA (n=283) CPR attempts (n=163) ROSC (n=14) 24-hour survivors (n=10)
2011 51 20 3 3
2012 58 34 3 0
2013 62 38 2 2
2014 59 37 3 2
2015 53 34 3 3
OHCA, out-of-hospital cardiac arrests; CPR, cardiopulmonary resuscitation; ROSC, return of spontaneous circulation.
healthcare personnel was considered futile for 42.4% of OHCA eral hospitals, the majority of which are middle-sized (100-200
victims that were transferred to the ER department, thus CPR was beds) that offer mostly secondary healthcare like our institu-
not attempted on them. Our findings are in good agreement with tion, while only 30 out of 124 public hospitals are either spe-
the Eureca One prospective study that included one-month OHCA cialized centers (18) or large hospitals (more than 400 beds)
outcome data from 27 European countries and was published in that offer advanced tertiary care.20 The level of the CPR train-
2016. According to the study, in Greece, approximately 54% of ing of our institution’s healthcare personnel could not be
patients either die on scene or are pronounced dead on arrival at assessed in this particular study. However, given the fact that
hospital.1 A possible explanation for this excess mortality could be advanced life support (ALS) certification is not a prerequisite
the long ambulance response and travel time to the ER, possibly as for a doctor to work in a Greek hospital20 and due to the inex-
ly
a result of the reduction of the Greek EMS ambulance fleet and its istence of Emergency Care specialty in the Greek medical cur-
on
deficient maintenance due to the recent cuts in public health expen- riculum,21 we can presume that there are no major differences
diture as a result of the ongoing financial crisis that adds up to an in CPR efficiency between the study’s reference and other
already inefficient EMS response mechanism.18 The unavailability Greek hospitals, although circumstantial dissimilarities cannot
e
of Automatic External Defibrillators in public areas19 and lack of be excluded.
civilian training on how to use them, as well as the low rates of
bystander CPR could also be contributing factors. The latter is also
- us
The extraction of the study’s data in a period that represents the
peak of Greece’s economic recession and which featured major
implied in the Eureca One study which places Greece 25th out of health expenditure cutbacks18 may not be indicative of pre or
al
27 countries in CPR provision (32 attempts per 100,000 arrests per after crisis OHCA survival in our institution and could also be
year) by both bystanders and EMS personnel.1 a limitation of the study.
ci
The percentage of ROSC in patients on whom CPR was
attempted (8.6%) indirectly reflects this hospital ER personnel’s
er
CPR performance and is again in accordance with Eureca One’s Conclusions
reported similar rate for Greece (9%) which was the lowest among
m
In our institution, the immediate, 24-hour and expected 30-day
27 countries.1
survival were lower than the European average and in accordance
Our study however carries several limitations:
om
with the recent prospective Eureca One study. Although, the results
- The 30-day mortality and the survival-to hospital discharge
of this retrospective study cannot be generalized as they originate
ratio, that are more accurate survival indexes, as well as the
from a single centre, they contribute to the limited existing data
neurological outcome of the survivors could not be measured
-c
regarding OHCA survival in our country. The conduction of simi-
in this particular study. This is due to the hospital’s policy of
lar efforts by other medical institutions as well as multicenter stud-
on
transferring long-term (>24h) cardiac arrest survivors to terti-
ies cannot be overemphasized in order to acquire a clearer picture
ary hospital ICUs, making follow-up of the patients difficult.
regarding cardiac arrest outcomes in Greece. This could play an
However, in our institution, the 30-day and overall survival for
N
important role in the redesign of a more efficient EMS response
the 5-year period of the study can be expected to be equal to or
mechanism.
less than the calculated 24-hour survival (3.5% overall, 6,1%
with CPR attempted) which is lower than the EU average4 and
confirms Eureca One’s 30-day survival estimates for Greece
(less than 5%).1
- This is a retrospective, single-center study with a relatively
References
small number of patients, thus inferences about nationwide 1. Gräsner J-T, Lefering R, Koster RW, et al. EuReCa ONE, 27
OHCA survival in Greece cannot be drawn with certainty from Nations, ONE Europe, ONE Registry: A prospective one
the current data. In addition, this particular hospital’s OHCA month analysis of out-of-hospital cardiac arrest outcomes in 27
survival rate could be affected by certain institutional features countries in Europe. Resuscitation 2016;105:188-95.
(public general hospital and not specialized tertiary center, 2. Chalkias A, Koutsovasilis A, Mystrioti D, et al. Outcomes of
possible inadequate medical personnel’s cardiac arrest training cardiopulmonary resuscitation efforts in a Greek tertiary hos-
and experience, suboptimal composition of resuscitation team pital. Acute Card Care 2013;15:34-7.
and local cardiac arrest protocols). Nevertheless, according to 3. Galatianou I, Karlis G, Apostolopoulos A, et al. Body mass
the country’s National Healthcare System infrastructural fea- index and outcome of out-of-hospital cardiac arrest patients
tures, the reference hospital is rather representative of the not treated by targeted temperature management. Am J Emerg
mean emergency care provider institution in Greece. 106 out of Med 2017;35:1247-51.
124 public hospitals in Greece that admit emergencies are gen- 4. Vargas M, Sutherasan Y, Pelosi P. Out-of-hospital cardiac
[page 66] [Emergency Care Journal 2019; 15:8249]
Article
arrest and survival to hospital discharge: a series of systemic arrest in community-dwelling adults ? Acad Emerg Med
reviews and meta-analyses. In: Vincent JL, ed. Annual update 2000;7:762-8.
in intensive care and emergency medicine 2015. Switzerland: 14. Funada A, Goto Y, Maeda T, et al. Improved survival with
Springer International Publishing; 2015. pp 289-314. favorable neurological outcome in elderly individuals with
5. Greif R, Lockey AS, Conaghan P, et al. European out-of-hospital cardiac arrest in Japan - A nationwide observa-
Resuscitation Council Guidelines for Resuscitation 2015: tional cohort study. Circ J 2016;80:1153-62.
Section 10. Education and implementation of resuscitation. 15. Fukuda T, Ohashi-Fukuda N, Matsubara T, et al. Trends in out-
Resuscitation 2015;95:288-301. comes for out-of-hospital cardiac arrest by age in Japan: an
6. Passali C, Pantazopoulos I, Dontas I, et al. Evaluation of nurs- observational study. Medicine (Baltimore) 2015;94:e2049.
es’ and doctors’ knowledge of basic & advanced life support 16. Libungan B, Lindqvist J, Strömsöe A, et al. Out-of-hospital
resuscitation guidelines. Nurse Educ Pract 2011;11:365-9. cardiac arrest in the elderly: A large-scale population-based
7. Pantazopoulos I, Aggelina A, Barouxis D, et al. Cardiologists’ study. Resuscitation 2015;94:28-32.
knowledge of the 2005 American Heart Association 17. Bossaert LL, Perkins GD, Askitopoulou H, et al. European
Resuscitation Guidelines: The Athens Study. Heart Lung J Crit Resuscitation Council Guidelines for Resuscitation 2015:
Care 2011;40:278-84. Section 11. The ethics of resuscitation and end-of-life deci-
8. Kyriakou F, Iacovidou N, Garofalakis I, et al. Residents’ resus- sions. Resuscitation 2015;95:302-11.
citation training and theoretical knowledge in a Greek General 18. Kotsiou OS, Srivastava DS, Kotsios P, et al. The emergency
Hospital. Eur J Emerg Med 2011;18:34-7. medical system in Greece: opening Aeolus’ bag of winds. Int J
9. Plagisou L, Tsironi M, Zyga S, et al. Assessment of nursing Environ Res Public Health 2018;15-745.
staff’s theoretical knowledge of cardiovascular resuscitation in 19. ToVima team. Application helps you find location of available
an NHS public hospital. Hell J Cardiol 2015;56:149-53. public AEDs. Greece: ToVima; 2017. Available from:
ly
10. Xanthos T, Akrivopoulou A, Pantazopoulos I, et al. Evaluation https://www.tovima.gr/2017/10/18/society/app-sas-boitha-na-
of nurses’ theoretical knowledge in Basic Life Support: a study breite-poy-yparxoyn-aytomatoi-ekswterikoi-apinidwtes/
on
in a district Greek hospital. Int Emerg Nurs 2012;20:28-32. Accessed: 3 April 2019.
11. Ministry of Health. Hospitals on call. 2019. Available from: 20. Economou C, Kaitelidou D, Karanikolos M, Maresso A.
http://www.moh.gov.gr Accessed: 2 June 2019. Greece: Health system review. Health Systems in Transition
e
12. Hellenic Statistical Authority. 2011 Census. 2011. Available 2017;19:1-192.
from: http://www.statistics.gr/en/home/ Accessed: 2 June
us
21. Athens Doctor's Association. Establishing and renaming of
2019. medical specialties. 2018. Available from: http://www.isa-
13. Swor RA, Jackson RE, Tintinalli JE, Pirrallo RG. Does thens.gr/images/eggrafa/FEK-metonomasia-eidikotitwn-
al
advanced age matter in outcomes after out-of-hospital cardiac 4138.pdf Accessed: 2 June 2019.
ci
er
m
om
-c
on
N
[Emergency Care Journal 2019; 15:8249] [page 67]
View publication stats
You might also like
- DW - Ped & Vehicle ListDocument13 pagesDW - Ped & Vehicle ListRayes0% (1)
- EMS EvaluationDocument21 pagesEMS EvaluationColleen FarrellNo ratings yet
- Working at Height Rescue Mock Drill!Document36 pagesWorking at Height Rescue Mock Drill!S RNo ratings yet
- Commonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFDocument12 pagesCommonly Used IV Cardiac Medications For Adults Pocket Reference Card PDFYannis Zoldenberg100% (1)
- Marketing Mix For Hospital ServicesDocument5 pagesMarketing Mix For Hospital ServicesReema Negi100% (4)
- Tjem 21 14Document6 pagesTjem 21 14Iyan MirazaNo ratings yet
- Dehydration and Clinical Outcome in Hospitalised Older Adults: A Cohort StudyDocument8 pagesDehydration and Clinical Outcome in Hospitalised Older Adults: A Cohort StudyJonathan EdbertNo ratings yet
- Hyponatremia in Tuberculous MeningitisDocument11 pagesHyponatremia in Tuberculous MeningitisBelinda Putri agustiaNo ratings yet
- Insomnia and Risk of Cardiovascular Disease: A Meta-AnalysisDocument8 pagesInsomnia and Risk of Cardiovascular Disease: A Meta-AnalysisFerdy LainsamputtyNo ratings yet
- Insomnia and Risk of Cardiovascular Disease: A Meta-AnalysisDocument8 pagesInsomnia and Risk of Cardiovascular Disease: A Meta-AnalysisFerdy LainsamputtyNo ratings yet
- Utility of Cytometric Parameters and Indices As Predictors of Mortality in Patients With SepsisDocument6 pagesUtility of Cytometric Parameters and Indices As Predictors of Mortality in Patients With SepsisPablo VélezNo ratings yet
- European Consensus For The Management of Patients With Differentiated Thyroid Carcinoma of The Follicular EpitheliumDocument17 pagesEuropean Consensus For The Management of Patients With Differentiated Thyroid Carcinoma of The Follicular Epitheliumelibet87No ratings yet
- Urine Dipstick of Sputum For The Rapid Diagnosis of Community Acquired PneumoniaDocument4 pagesUrine Dipstick of Sputum For The Rapid Diagnosis of Community Acquired PneumoniaStephen JohanNo ratings yet
- Review Article: Consensus Guidelines For The Diagnosis and Clinical Management of Erdheim-Chester DiseaseDocument10 pagesReview Article: Consensus Guidelines For The Diagnosis and Clinical Management of Erdheim-Chester DiseaseNadun MethwadaneNo ratings yet
- 1 s2.0 S110996662200149X MainDocument8 pages1 s2.0 S110996662200149X MainLiaaNo ratings yet
- How Do Sepsis Survivors Experience Life After Sepsis? A Danish Qualitative Study Exploring Factors of ImportanceDocument7 pagesHow Do Sepsis Survivors Experience Life After Sepsis? A Danish Qualitative Study Exploring Factors of Importancestardust.m002No ratings yet
- Correlation of Serum Lactate Levels With Survival in Patients With SepsisDocument6 pagesCorrelation of Serum Lactate Levels With Survival in Patients With SepsisIJAR JOURNALNo ratings yet
- Extracorporeal Membrane Oxygenation For Refractory Cardiac Arrest: A Retrospective Multicenter StudyDocument10 pagesExtracorporeal Membrane Oxygenation For Refractory Cardiac Arrest: A Retrospective Multicenter StudyFraternity LiviNo ratings yet
- Causes, Timing, and Modes of Death in A Tertiary Pediatric Intensive Care UnitDocument9 pagesCauses, Timing, and Modes of Death in A Tertiary Pediatric Intensive Care UnitMarcos Chusin MontesdeocaNo ratings yet
- 2016 Article 174Document8 pages2016 Article 174Alfeus GradyNo ratings yet
- Sincope y TEP JAMA 2018Document7 pagesSincope y TEP JAMA 2018coniestivillNo ratings yet
- 6 Antithrombotic Therapy in Patients With Infective EndocarditisDocument12 pages6 Antithrombotic Therapy in Patients With Infective Endocarditisabdeali hazariNo ratings yet
- Diastolic Dysfunction and Mortality in Severe Sepsis and Septic ShockDocument9 pagesDiastolic Dysfunction and Mortality in Severe Sepsis and Septic ShockShinohara YuusukeNo ratings yet
- Early Prediction of Sepsis From Clinical Data Using Single Light-GBM ModelDocument4 pagesEarly Prediction of Sepsis From Clinical Data Using Single Light-GBM ModelArpan SoniNo ratings yet
- Tapia 2019Document9 pagesTapia 2019SANTOSH KUMAR BHASKARNo ratings yet
- Brignole Hamdan 2012 New Concepts in The Assessment of SyncopeDocument9 pagesBrignole Hamdan 2012 New Concepts in The Assessment of Syncopedrpradeepmd1982No ratings yet
- Ioi80197 463 473Document11 pagesIoi80197 463 473Phạm LinhNo ratings yet
- Aborto Septico Lanari-USA ICM 2004Document6 pagesAborto Septico Lanari-USA ICM 2004pastorizaariana25No ratings yet
- Content ServerDocument4 pagesContent ServerEkaSaktiWahyuningtyasNo ratings yet
- Concerns of Patients On Dialysis A Research Study PDFDocument15 pagesConcerns of Patients On Dialysis A Research Study PDFProdi S1- 1BNo ratings yet
- 2020 Covid 19 ECMO and LymphopeniaDocument1 page2020 Covid 19 ECMO and LymphopeniaDidier AdodoNo ratings yet
- Ischemic Stroke A Comparative Retrospective Study: Experience of Military Hospital of MeknesDocument20 pagesIschemic Stroke A Comparative Retrospective Study: Experience of Military Hospital of MeknesIJAR JOURNALNo ratings yet
- Choque Septico y Falla Multiorgano Relaciona Con Balance de FluidosDocument14 pagesChoque Septico y Falla Multiorgano Relaciona Con Balance de FluidosMiguel Angel Hernandez SerratoNo ratings yet
- Artb 2Document11 pagesArtb 2Claudia IrimieNo ratings yet
- Nerjm SesionDocument12 pagesNerjm SesionjorgeNo ratings yet
- Septic ShockDocument12 pagesSeptic ShockPatrick CommettantNo ratings yet
- ARO SOCRE Predictor Mortalidad 2015Document13 pagesARO SOCRE Predictor Mortalidad 2015raul serranoNo ratings yet
- Pathway ScabiesDocument11 pagesPathway ScabieslukmanNo ratings yet
- Academic Emergency Medicine 2024 Long Fluid Volumes in Adults WithDocument2 pagesAcademic Emergency Medicine 2024 Long Fluid Volumes in Adults WithAdrianaIDCNo ratings yet
- SPECTand PETin Alzheimers ValotasiouDocument14 pagesSPECTand PETin Alzheimers ValotasiouTony AndersonNo ratings yet
- 10 1016@j Jaad 2019 05 096Document8 pages10 1016@j Jaad 2019 05 096JohnNo ratings yet
- The Egyptian Heart JournalDocument4 pagesThe Egyptian Heart JournalVareshaNo ratings yet
- Aritmia 3Document1 pageAritmia 3Anonymous NVBCqKWHNo ratings yet
- An International Sepsis Survey: A Study of Doctors' Knowledge and Perception About SepsisDocument5 pagesAn International Sepsis Survey: A Study of Doctors' Knowledge and Perception About SepsissmileybutterflyNo ratings yet
- Quick Sepsis-Related OrganDocument12 pagesQuick Sepsis-Related OrganArnavjyoti DasNo ratings yet
- 2019 Ischemic StrokeDocument9 pages2019 Ischemic StrokeFriska tampuboLonNo ratings yet
- Annals of Neurology - 2017 - Espay - Deconstructing Normal Pressure Hydrocephalus Ventriculomegaly As Early Sign ofDocument11 pagesAnnals of Neurology - 2017 - Espay - Deconstructing Normal Pressure Hydrocephalus Ventriculomegaly As Early Sign ofErika PérezNo ratings yet
- Stroke Scales and Trajectory of Recovery A Major Concern For Patients and Nurses AlikeDocument7 pagesStroke Scales and Trajectory of Recovery A Major Concern For Patients and Nurses AlikeAnonymous XO9RqHhOgiNo ratings yet
- Predicting 30-Day Case Fatality of Primary Inoperable Intracerebral Hemorrhage Based On Findings at The Emergency DepartmentDocument6 pagesPredicting 30-Day Case Fatality of Primary Inoperable Intracerebral Hemorrhage Based On Findings at The Emergency DepartmentNouchan NoupNo ratings yet
- Resuscitation: Intra-Thoracic Injuries Associated With Cardiopulmonary Resuscitation - Frequent and SeriousDocument5 pagesResuscitation: Intra-Thoracic Injuries Associated With Cardiopulmonary Resuscitation - Frequent and SeriousSwayam PrakashNo ratings yet
- Tomasi Et Al 2017Document5 pagesTomasi Et Al 2017Cristiane TomasiNo ratings yet
- Indian Heart Journal: Cardiac Arrest Due To Pulmonary EmbolismDocument5 pagesIndian Heart Journal: Cardiac Arrest Due To Pulmonary EmbolismARNo ratings yet
- Timed Up and Go - Diagnóstico de DemênciaDocument6 pagesTimed Up and Go - Diagnóstico de DemênciaMarta SilvaNo ratings yet
- Biomedical Journal: SciencedirectDocument6 pagesBiomedical Journal: SciencedirectFarihah SamarraNo ratings yet
- 10 1371@journal Pone 0226325Document26 pages10 1371@journal Pone 0226325Ged Marlid Kooumous MafongoNo ratings yet
- EcgrevDocument13 pagesEcgrevvicky_ani1986No ratings yet
- Ikeda 2018Document7 pagesIkeda 2018Fatih KızılyelNo ratings yet
- Guerchet 2012 RCA RC EDACDocument6 pagesGuerchet 2012 RCA RC EDACkouame2907No ratings yet
- Associations of Egg Consumption With CardiovascularDocument8 pagesAssociations of Egg Consumption With CardiovascularSofía PascalNo ratings yet
- AAFP SepsisDocument13 pagesAAFP SepsisANISA RACHMITA ARIANTI 2020No ratings yet
- 1201 FullDocument7 pages1201 FullDavy JonesNo ratings yet
- Fneur 13 853054Document8 pagesFneur 13 853054RAFAEL BRITONo ratings yet
- Arifin 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012085Document6 pagesArifin 2018 IOP Conf. Ser. Earth Environ. Sci. 125 012085محمود صابرNo ratings yet
- 1 s2.0 S003962571630090X MainDocument14 pages1 s2.0 S003962571630090X MainBenjamin NgNo ratings yet
- Cerebrospinal Fluid in Clinical NeurologyFrom EverandCerebrospinal Fluid in Clinical NeurologyFlorian DeisenhammerNo ratings yet
- MasteringChemistry ConstantsDocument3 pagesMasteringChemistry ConstantsYannis ZoldenbergNo ratings yet
- Brentons Mcat GuideDocument20 pagesBrentons Mcat GuideYannis ZoldenbergNo ratings yet
- Location of In-Hospital Cardiac Arrest in The United States 2016Document8 pagesLocation of In-Hospital Cardiac Arrest in The United States 2016Yannis ZoldenbergNo ratings yet
- Mrocwal 1Document133 pagesMrocwal 1Yannis ZoldenbergNo ratings yet
- s15 Miller Chap 2a LectureDocument19 pagess15 Miller Chap 2a LectureYannis ZoldenbergNo ratings yet
- Trends in Survival After In-Hospital Arrest During Nights and Weekends 2018Document10 pagesTrends in Survival After In-Hospital Arrest During Nights and Weekends 2018Yannis ZoldenbergNo ratings yet
- 2009 PiCCO Advanced Hemodynamic Monitoring PDFDocument15 pages2009 PiCCO Advanced Hemodynamic Monitoring PDFYannis ZoldenbergNo ratings yet
- Perceived Competence in Cardiopulmonary Resuscitation, Knowledge and Skills, Amongst 50 Qualified NursesDocument6 pagesPerceived Competence in Cardiopulmonary Resuscitation, Knowledge and Skills, Amongst 50 Qualified NursesYannis ZoldenbergNo ratings yet
- T - 14.5. N.A. Pupils 9.1 PDFDocument2 pagesT - 14.5. N.A. Pupils 9.1 PDFYannis ZoldenbergNo ratings yet
- Ed GeinDocument1 pageEd GeinYannis ZoldenbergNo ratings yet
- A01628 CH19Document36 pagesA01628 CH19Yannis ZoldenbergNo ratings yet
- Wisdom of The EgoDocument1,041 pagesWisdom of The EgoYannis Zoldenberg100% (1)
- David SolomonsDocument1 pageDavid SolomonsYannis ZoldenbergNo ratings yet
- I-35W Bridge Collapse and Response: Minneapolis, MinnesotaDocument60 pagesI-35W Bridge Collapse and Response: Minneapolis, MinnesotamadmaxberNo ratings yet
- TNB060210Document16 pagesTNB060210webmaster3777No ratings yet
- Curriculum Advanced Specialised Training Emergency MedicineDocument35 pagesCurriculum Advanced Specialised Training Emergency MedicineSenthooran ArudshivsmNo ratings yet
- Oldier Onors Rogram and Ospital With Riceless Ift: S H P H P GDocument8 pagesOldier Onors Rogram and Ospital With Riceless Ift: S H P H P GrotorbrentNo ratings yet
- Fire Officer Legal ResponsibilitiesDocument55 pagesFire Officer Legal ResponsibilitiesJohn K MurphyNo ratings yet
- Trauma GuidelinesDocument592 pagesTrauma GuidelinesAlvaro Perez Henriquez100% (1)
- Hubungan Ketepatan Penilaian Triase Dengan Tingkat Keberhasilan Penanganan Pasien Cedera Kepala Di Igd Rsu HKBP Balige Kabupaten Toba Samosir Melva ManurungDocument17 pagesHubungan Ketepatan Penilaian Triase Dengan Tingkat Keberhasilan Penanganan Pasien Cedera Kepala Di Igd Rsu HKBP Balige Kabupaten Toba Samosir Melva ManurungElvina MaharaniNo ratings yet
- Capsule Proposal For Training at GogognanDocument12 pagesCapsule Proposal For Training at GogognanBobby C. CabigonNo ratings yet
- Atls Indonesia: Download NowDocument4 pagesAtls Indonesia: Download NowGyidian UpaNo ratings yet
- Unit 4 ReadingDocument4 pagesUnit 4 ReadingElvantNo ratings yet
- Anaesthesia - 2022 - Spoelder - Transport of The Patient With Trauma A Narrative ReviewDocument7 pagesAnaesthesia - 2022 - Spoelder - Transport of The Patient With Trauma A Narrative Reviewomar gonzalezNo ratings yet
- Sample+Simulation+Scenarios 08-2017 MedPro+GroupDocument62 pagesSample+Simulation+Scenarios 08-2017 MedPro+GroupGursimran RajvanshNo ratings yet
- Covid 19 - CPRDocument2 pagesCovid 19 - CPRArabind Ach AryaNo ratings yet
- Fdny Proems 1st 2016Document40 pagesFdny Proems 1st 2016Hualy DelgadoNo ratings yet
- Emergency Room ThesisDocument8 pagesEmergency Room Thesisstephanieclarkolathe100% (2)
- Health Group 3Document39 pagesHealth Group 3Gilvert A. PanganibanNo ratings yet
- Penetrating TraumaDocument606 pagesPenetrating TraumaMajdEddeinAlmustafaNo ratings yet
- Drug StudyDocument6 pagesDrug StudyMargaret ArellanoNo ratings yet
- Redesigning The Emergency Ambulance PDFDocument40 pagesRedesigning The Emergency Ambulance PDFMauricio GarcíaNo ratings yet
- BLS Book (New)Document7 pagesBLS Book (New)Saman FirdousNo ratings yet
- Ohio Legislative Service Commission: Final AnalysisDocument36 pagesOhio Legislative Service Commission: Final AnalysisJames LindonNo ratings yet
- CBT - Emergency Medicine EditedDocument14 pagesCBT - Emergency Medicine Editedchristy INo ratings yet
- Carpentersville FOIA-Response Jan2011Document41 pagesCarpentersville FOIA-Response Jan2011Gordon T. PrattNo ratings yet
- Part 4: Pediatric Basic and Advanced Life SupportDocument58 pagesPart 4: Pediatric Basic and Advanced Life SupportCatiussaNo ratings yet
- CPG Early Management of Head InjuryDocument67 pagesCPG Early Management of Head Injurygillian102290100% (1)
- Trauma CareDocument34 pagesTrauma CareGovindarajan HariharanNo ratings yet