Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
17 viewsCC Lec 7 Blood Gases
CC Lec 7 Blood Gases
Uploaded by
Junea SeeThe document summarizes acid-base regulation by the lungs and kidneys. The lungs regulate acid-base balance by controlling carbon dioxide excretion. The kidneys regulate acid-base balance through bicarbonate reabsorption and acid excretion. The major buffer systems that help maintain blood pH include the bicarbonate-carbonic acid buffer, phosphate buffer, protein buffer, and hemoglobin buffer. Each buffer system functions through different mechanisms to neutralize acids and bases in the blood and help maintain a normal pH.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Test Bank For High Acuity Nursing 6th Edition Kathleen Dorman WagnerDocument18 pagesTest Bank For High Acuity Nursing 6th Edition Kathleen Dorman WagnerDavidRobinsonfikq100% (41)
- Mechanical Ventilation Learning Package: Sharon-Ann Shunker, CNC, Liverpool ICU SWSLHD 2/3/2016Document75 pagesMechanical Ventilation Learning Package: Sharon-Ann Shunker, CNC, Liverpool ICU SWSLHD 2/3/2016Hanni HarahapNo ratings yet
- Mtap421 BloodgasesDocument11 pagesMtap421 BloodgasesNhelomar ManlinconNo ratings yet
- Applications of The Henderson Hasselbalch EquationDocument8 pagesApplications of The Henderson Hasselbalch EquationSittie Fahieda AloyodanNo ratings yet
- Acid-Base Balance: Editor: Dr. Husnil Kadri, MkesDocument66 pagesAcid-Base Balance: Editor: Dr. Husnil Kadri, MkesDwi SiregarNo ratings yet
- Acid Base Balance Respiratory (2024)Document42 pagesAcid Base Balance Respiratory (2024)khilmiaNo ratings yet
- ABGDocument7 pagesABGEva Marie GaaNo ratings yet
- Chapter 1 Acid-Base Regulation: Lesser Amounts of Organic Acid Derive From The FollowingDocument52 pagesChapter 1 Acid-Base Regulation: Lesser Amounts of Organic Acid Derive From The FollowingMarwa RagabNo ratings yet
- Blood GasesDocument51 pagesBlood Gasesrbm121415chyNo ratings yet
- Acid-Base BalanceDocument7 pagesAcid-Base BalanceMichelle Mae JulianaNo ratings yet
- Acid-Base Balance, Dr. MiaDocument45 pagesAcid-Base Balance, Dr. MiaeuiskurNo ratings yet
- CC2 - Lec9 1Document5 pagesCC2 - Lec9 1Glecy PaciaNo ratings yet
- Blood Gases, PH, and Buffer SystemDocument22 pagesBlood Gases, PH, and Buffer SystemtabletvodaNo ratings yet
- Peran Ginjal Dalam Kesetimbangan Asam Basa DarahDocument30 pagesPeran Ginjal Dalam Kesetimbangan Asam Basa DarahgardamdNo ratings yet
- Blood Gases, PH and Buffer Systems: DefinitionsDocument4 pagesBlood Gases, PH and Buffer Systems: DefinitionsMj TizonNo ratings yet
- 835 Regulation of Acid Base Balance 2019Document26 pages835 Regulation of Acid Base Balance 2019sanofazal786No ratings yet
- Acid BaseDocument10 pagesAcid BaseFiona Marie Kyla TunayNo ratings yet
- Acid Base BalanceDocument104 pagesAcid Base BalanceKevin VillaranteNo ratings yet
- Acid Base Im Balance-2a - 3.05.2021Document75 pagesAcid Base Im Balance-2a - 3.05.2021Kavya FouzdarNo ratings yet
- 3 Acid Base ImbalanceDocument5 pages3 Acid Base ImbalanceSJane FeriaNo ratings yet
- Cchm2 MidtermsDocument22 pagesCchm2 MidtermsMACOB, ETHELHYN JHANE100% (1)
- Acid Base BalanceDocument38 pagesAcid Base Balancelady birdNo ratings yet
- Acid Base Disorders-MD3Document44 pagesAcid Base Disorders-MD3juliuskahabi1No ratings yet
- Acid-Base BalanceDocument11 pagesAcid-Base Balancemostafadiab074No ratings yet
- Introduction To Biochemistry Proteins Buffers in Blood Plasma and CellsDocument5 pagesIntroduction To Biochemistry Proteins Buffers in Blood Plasma and CellsGwyn Louise CarolinoNo ratings yet
- 9 - (D) Acid Base Balance Dec 4.17Document61 pages9 - (D) Acid Base Balance Dec 4.17khaledNo ratings yet
- Fluid-Electrolytes and Acid-Base Disturbance in Surgery: Haidi Hu, MD, PHDDocument68 pagesFluid-Electrolytes and Acid-Base Disturbance in Surgery: Haidi Hu, MD, PHDHUNEL KimNo ratings yet
- Acid Base Regulation and Its DisordersDocument80 pagesAcid Base Regulation and Its DisordersPirate CoolNo ratings yet
- Acid Base Balance DR NaimDocument136 pagesAcid Base Balance DR NaimTaimoor Ul HassanNo ratings yet
- Acid-Base Balance and Its DisordersDocument37 pagesAcid-Base Balance and Its Disordersmaria angela SaldajenoNo ratings yet
- Daily Acid Load: Carbonic or Volatile Acid (H CO Carbonic AcidsDocument11 pagesDaily Acid Load: Carbonic or Volatile Acid (H CO Carbonic AcidsPrastia StratosNo ratings yet
- BCH 201 ModuleDocument15 pagesBCH 201 ModuleJoyNo ratings yet
- Hydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionDocument15 pagesHydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionElisha WorworNo ratings yet
- Gangguan Asam BasaDocument51 pagesGangguan Asam BasaYudhistira YuliandraNo ratings yet
- Acid Base Balance OR OR Regulation of Blood PHDocument175 pagesAcid Base Balance OR OR Regulation of Blood PHhirendra patel100% (1)
- 1st Chap-2Document40 pages1st Chap-2RJ Noor JanNo ratings yet
- Physiology of Acid Base Balance by Dr. ROOMIDocument70 pagesPhysiology of Acid Base Balance by Dr. ROOMIMudassar Roomi100% (1)
- Acid Base PhysiologyDocument54 pagesAcid Base PhysiologyDiana AyónNo ratings yet
- Acid Base Regulation - ppt@BVSCAH-6th SemDocument95 pagesAcid Base Regulation - ppt@BVSCAH-6th SemDr. Prakash PanthiNo ratings yet
- Draft ACID BASEDocument5 pagesDraft ACID BASEkimmynemil80No ratings yet
- Acid Base BalanceDocument50 pagesAcid Base BalanceEgun Nuel DNo ratings yet
- CO + H O H + Hco: Overall ReactionDocument12 pagesCO + H O H + Hco: Overall ReactionLuke ShantiNo ratings yet
- Acid Base DisorderDocument48 pagesAcid Base DisorderAGUNG SETIADI NUGROHONo ratings yet
- 14-Acid-Base DisordersDocument19 pages14-Acid-Base Disordersمصطفى محمد جواد كاظمNo ratings yet
- Blood Gases, PH, and Buffer SystemDocument22 pagesBlood Gases, PH, and Buffer SystemAhmed GaberNo ratings yet
- Cc2lec - Module 4Document6 pagesCc2lec - Module 4LUKENo ratings yet
- Acid Base Balance NotesheetDocument12 pagesAcid Base Balance NotesheetMariam MohammedNo ratings yet
- CLINICAL CHEMISTRY 2 LecDocument14 pagesCLINICAL CHEMISTRY 2 LecMACOB, ETHELHYN JHANENo ratings yet
- Acid Base2005Document64 pagesAcid Base2005AgusNo ratings yet
- O.M.O - Acid Base Balance and DisordersDocument50 pagesO.M.O - Acid Base Balance and DisordersIiiNo ratings yet
- BicarbonateDocument5 pagesBicarbonateRace MendezNo ratings yet
- Acid-Base BalanceDocument38 pagesAcid-Base BalanceNym Angga SantosaNo ratings yet
- Disorders of Acid Base BalanceDocument45 pagesDisorders of Acid Base BalanceTee Sze WayNo ratings yet
- Acid Base BalanceDocument5 pagesAcid Base BalanceAnila zafarNo ratings yet
- Acid - Base BalancesDocument68 pagesAcid - Base Balancesjames makulaNo ratings yet
- Acid-Base BalanceDocument94 pagesAcid-Base BalanceJagan KumarNo ratings yet
- Pengaturan Asam-Basa & ElektrolitDocument40 pagesPengaturan Asam-Basa & ElektrolitArifuddinZrNo ratings yet
- Discussion 5 Blood Gases LectureDocument139 pagesDiscussion 5 Blood Gases LectureFaith Tambong100% (1)
- Acid Base RehabDocument54 pagesAcid Base RehabKushie GuezyNo ratings yet
- Acid-Base Balance and DisodersDocument86 pagesAcid-Base Balance and DisodersPrincewill SeiyefaNo ratings yet
- Biochemistry Applied to the Brewing Processes - Mashing, Boiling, CoolingFrom EverandBiochemistry Applied to the Brewing Processes - Mashing, Boiling, CoolingNo ratings yet
- CC2 Lab 13Document10 pagesCC2 Lab 13Junea SeeNo ratings yet
- Cc2 Lec 13 Trace ElementsDocument21 pagesCc2 Lec 13 Trace ElementsJunea SeeNo ratings yet
- Cc2 Lec EnzymesDocument25 pagesCc2 Lec EnzymesJunea SeeNo ratings yet
- Cc2lec 14 Intro To ToxiDocument30 pagesCc2lec 14 Intro To ToxiJunea SeeNo ratings yet
- Acid-Base Disorders in The Critically Ill PatientDocument11 pagesAcid-Base Disorders in The Critically Ill PatientAniAliciaOrtizCastleNo ratings yet
- Acid Base BalanceDocument167 pagesAcid Base BalancePratap Sagar Tiwari100% (1)
- THAM MonographDocument34 pagesTHAM MonographzaaklcxNo ratings yet
- Harvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateDocument21 pagesHarvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateOluwaseun TosinNo ratings yet
- Acid Base BalanceDocument27 pagesAcid Base BalanceKamran Khan KhalilNo ratings yet
- Final GusDocument57 pagesFinal GusDebbi YuniseraniNo ratings yet
- Acid Base Balance Flashcards QuizletDocument1 pageAcid Base Balance Flashcards QuizletapolloNo ratings yet
- Arterial Blood Gas InterpretationDocument69 pagesArterial Blood Gas InterpretationostuffeNo ratings yet
- Physiology Handbook December 2022 PDFDocument280 pagesPhysiology Handbook December 2022 PDFrachel wongNo ratings yet
- Hand Out 3 Respiratory System Overview PDFDocument12 pagesHand Out 3 Respiratory System Overview PDFGrape JuiceNo ratings yet
- Fluid and ElectrolytesDocument13 pagesFluid and ElectrolytesMarcus, RN100% (7)
- 'Block E With Keys and Hints ' With YouDocument36 pages'Block E With Keys and Hints ' With YouAbdullah TanoliNo ratings yet
- Anatomy and Physiology of Respiratory SystemDocument34 pagesAnatomy and Physiology of Respiratory SystemSamson SeiduNo ratings yet
- Indication For Arterial Blood Gas AnalysisDocument10 pagesIndication For Arterial Blood Gas AnalysisRohini RaiNo ratings yet
- Steps in ABG Analysis Using The Tic-Tac-Toe MethodDocument4 pagesSteps in ABG Analysis Using The Tic-Tac-Toe MethodSeanmarie CabralesNo ratings yet
- Fluid Electrolytes and Acid Base BalanceDocument23 pagesFluid Electrolytes and Acid Base BalanceJohn MalkovicNo ratings yet
- MineralsDocument70 pagesMineralsVioletteNo ratings yet
- Chemistry of Life: By: Ruth Abigail C. ValdezDocument39 pagesChemistry of Life: By: Ruth Abigail C. ValdezPanJan BalNo ratings yet
- Human Anatomy and Physiology by Hema Seliya-3Document7 pagesHuman Anatomy and Physiology by Hema Seliya-3Priya YadavNo ratings yet
- Laboratory Animal Nutrition Nutrient Requirement of Mice Rat Rabbit Guinea PigDocument66 pagesLaboratory Animal Nutrition Nutrient Requirement of Mice Rat Rabbit Guinea PigyohanNo ratings yet
- Fluid Electrolytes and Acid Base BalanceDocument108 pagesFluid Electrolytes and Acid Base BalancesayednourNo ratings yet
- ABIDocument27 pagesABIekramNo ratings yet
- Effects of Malaria Parasitaemia On Electrolytes (NA, K, CL, HCO3) and Some Liver Enzymes (AST and ALT) in Patient Attending University of Maiduguri Teaching HospitalDocument19 pagesEffects of Malaria Parasitaemia On Electrolytes (NA, K, CL, HCO3) and Some Liver Enzymes (AST and ALT) in Patient Attending University of Maiduguri Teaching HospitalAcademic JournalNo ratings yet
- Sodium Bicarbonate in J AftDocument9 pagesSodium Bicarbonate in J AftMohd Faizal SimonNo ratings yet
- Acid Base Disorders DR Kwaifa - PPTX 1Document99 pagesAcid Base Disorders DR Kwaifa - PPTX 1DICKSONNo ratings yet
- University of Makati College of Allied Health Studies Center of NursingDocument32 pagesUniversity of Makati College of Allied Health Studies Center of NursingE.J. PelayoNo ratings yet
- 003Document358 pages003Gordana UzelacNo ratings yet
- PhysioEx Exercise 10 Activity 3 - Balamad, Maria Karla M.Document3 pagesPhysioEx Exercise 10 Activity 3 - Balamad, Maria Karla M.Maria Karla BalamadNo ratings yet
CC Lec 7 Blood Gases
CC Lec 7 Blood Gases
Uploaded by
Junea See0 ratings0% found this document useful (0 votes)
17 views10 pagesThe document summarizes acid-base regulation by the lungs and kidneys. The lungs regulate acid-base balance by controlling carbon dioxide excretion. The kidneys regulate acid-base balance through bicarbonate reabsorption and acid excretion. The major buffer systems that help maintain blood pH include the bicarbonate-carbonic acid buffer, phosphate buffer, protein buffer, and hemoglobin buffer. Each buffer system functions through different mechanisms to neutralize acids and bases in the blood and help maintain a normal pH.
Original Description:
Blood gases clinical chemistry
Original Title
Cc Lec 7 Blood Gases
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe document summarizes acid-base regulation by the lungs and kidneys. The lungs regulate acid-base balance by controlling carbon dioxide excretion. The kidneys regulate acid-base balance through bicarbonate reabsorption and acid excretion. The major buffer systems that help maintain blood pH include the bicarbonate-carbonic acid buffer, phosphate buffer, protein buffer, and hemoglobin buffer. Each buffer system functions through different mechanisms to neutralize acids and bases in the blood and help maintain a normal pH.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
17 views10 pagesCC Lec 7 Blood Gases
CC Lec 7 Blood Gases
Uploaded by
Junea SeeThe document summarizes acid-base regulation by the lungs and kidneys. The lungs regulate acid-base balance by controlling carbon dioxide excretion. The kidneys regulate acid-base balance through bicarbonate reabsorption and acid excretion. The major buffer systems that help maintain blood pH include the bicarbonate-carbonic acid buffer, phosphate buffer, protein buffer, and hemoglobin buffer. Each buffer system functions through different mechanisms to neutralize acids and bases in the blood and help maintain a normal pH.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 10
1 | CC2LEC WEEK 7
BLOOD GASES both the generation of bicarbonate irons and
they rate of urinary excretion
Regulation of Acid-Base balance: lungs and
• 50-100 mmol/L of acid Must be excreted daily
kidneys
by the kidneys resulting to urine pH of 4.5
• Most of the carbon dioxide (CO2) with water Plasma and urine bicarbonate
(H2O) to form carbonic acid (h2co3), which
dissociates immediately into H+ and • Increase bicarbonate ( HCO3): IV
bicarbonate (HCO3) – the reaction is Infusions of lactate, acetate and HCO3
accelerated by carbonic anhydrase • Decrease bicarbonate ( HCO3): use of
• The dissociation of h2co3 increase hco3 in diuretics, reduced reabsorption and chronic
RBC causing it to diffuse into the plasma nephritis
• HCO3 and H2CO3 are renewable – even • If bicarbonate is below 25mmol/L or if plasma
before renal mechanisms restore the carbon dioxide rises above normal, the tubule
constituents, the lung alters the ration of can reabsorb all the bicarbonate in the
numerator (hco3) to denominator (h2co3) by glomerular filtrate, leaving none of the
blowing off CO2 excretion in urine
• A small amount of bicarbonate is normally
Lungs
excreted in the urine (about 10 mEq/ Day)
• Respiratory control of carbon dioxide (co2) • The kidneys excrete considerable amounts of
excretion allows rapid and very sensitive acid and base for acid-base regulation
adjustment in blood pH • Urinary excretion of bicarbonate when
• as the lungs eliminate excess carbon dioxide plasma reached 26-30 mmol/L
to resist accumulating hydrogen, the
ACIDS
proportion between bicarbonate (hco3) and
carbonic acid (h2co3) readjust to 20:1, ● Substance that can yield a hydrogen ion (H) or
although the absolute concentration of each hydronium ion when dissolved in water
can fall below normal ● Representing the (+) charged molecule
• by regulating the rate of carbon dioxide
excretion, the lungs can maintain the ratio at o Positively charged molecule
or about 20:1, thereby minimizing pH BASE
changes
• the carbon dioxide diffuses into the alveoli ● Substance that can yield hydroxyl ions (OH)
and is eliminated through ventilation ● Negatively (-) charged molecule
• slow or non-removal of carbon dioxide by the
BUFFER
lungs results to increase in hydrogen ion
concentration -respiratory acidosis ● Could be any compound which is a
• Rapid or fast elimination of carbon dioxide combination of weak acid or weak base and
results to decrease hydrogen ion its salt, is a system that resist changes in pH
concentration – respiratory alkalosis ● Maintain normal body pH: 7.35 - 7.45
● Basically, its major function is to
Kidneys
maintain/prevent sudden fluctuations in the pH.
• The most important function of the kidney in ★ Effectiveness of buffer is determined based
acid base homeostasis is excretion of acid on:
which is equivalent to generation of alkali or o pK of buffering system – ionization
reabsorption of bicarbonate from the constant (pKa)
glomerular filtrate (proximal tubules of the o pH of the environment
kidneys) and add it to the blood ● Plasma – (major buffer system) bicarbonate-
• acid is excreted in the form of ammonia carbonic acid buffer system;
(nh4+) and titratable acid
o pK of 6.1
• Hydrogen ions are also excreted by the
kidney both by direct excretion and through ● Bicarbonate-carbonic acid – major system
indirect disposal in the form of ammonium ion
• bicarbonate concentration (HCO3) is under
renal control, in that the kidneys regulate
2 | CC2LEC WEEK 7
DIFFERENT BUFFER SYSTEM ● Effective buffer because it holds or carries
oxygen, so it has the ability to uphold oxygen
★ BICARBONATE-CARBONIC ACID BUFFER and replace it with carbon dioxide
SYSTEM
● Principal mammalian buffer system → Hemoglobin is considered to be an effective buffer
● Major extracellular blood buffer primarily because it is the one responsible for carrying
● basis on how pH is determined oxygen and replace it with carbon dioxide
mathematically (Henderson-Hasselbalch
equation)
● Helps in the maintenance of carbon-dioxide,
● made up of acids combine with
in which it facilitates its diffusion across
bicarbonates in the blood
different gradients
○ conjugate base/ Neutral salts
(bicarbonate salts)
★ PROTEIN BUFFER SYSTEM
○ Carbonic acid (weak acid)
● H2CO3 (Carbonic acid) unstable, changing to
● Helps in maintaining the buffer due to the
H2O and CO2 in fluid
charges which is present under surface
** in the blood circulation, bicarbonate and carbonic ● Proteins are made up of amino acids. The
exist in 2 different forms: structure of an amino acid contains a carboxyl end
and amino end. (Positively charged and negatively
a. bicarbonate: exist in blood circulation as it
charged end)
is; primary regulation is through the function
● exist in 2 forms: H+ protein, B protein
of kidneys (renal regulation)
● capability to bind or release excess hydrogen as
b. Carbonic acid: unstable compound, readily
required within the blood circulation
changes to water and carbon dioxide once
● Protein tends to become more (+) in an
reaches the plasma
acidic environment and more (-) in basic
** the measurement of carbonic acid is environment (alkaline)
based on pCO2 (partial pressure of carbon ○ Has the capability to act as a
dioxide) minor buffer system
● plasma proteins (charges on their surface)
★ PHOSPHATE BUFFER SYSTEM→ also helps in ○ pH > pl → (-) charge
the maintenance of normal blood pH ○ pH < pl → (+) charge
● made up of 2,3-diphosphoglycerate →
primary phosphate form that act as a buffer BICARBONATE(HCO3)
● it increases the amount of NaHCO3 (sodium ● The second largest fraction of the anions
bicarbonate) in ECF (more alkaline)
in the plasma. It includes the ionized
● its function is to increase the amount of sodium bicarbonate (HCO3), carbonate and the
bicarbonate in the extracellular fluid making it carbamino compounds.
more alkaline because sodium bicarbonate is a ○ Bicarbonate is also classified under
negatively charged molecule electrolytes
● 16% of non-bicarbonate buffer value ● Normal range is from 22-26 mmol/L (22-26
utilization of RBC meq/L)
→ RBCs would be the primary utilization ● Conjugate base representative of the
buffer major system
★ HEMOGLOBIN-OXYHEMOGLOBIN BUFFER
SYSTEM CARBONIC ACID (H2CO3)
● maintains pH level (venous and arterial ● Weak acid
blood) ● This fraction of blood, plasma or serum
● 1 gram of hemoglobin carries 1.39 mL of includes the undissociated carbonic acid
oxygen → (each mole of hemoglobin binds with and the physically dissolved anhydrous
1 mol of oxygen, more than 95% of your CO2. Since CO2 concentration is higher than
hemoglobin binds with oxygen) HCO3. (bicarbonate)
○ 95% of hemoglobin binds in ● Readily dissociated into water and carbon dioxide
oxygen once it reaches the blood circulation
3 | CC2LEC WEEK 7
● The symbol cdCO2 (conc. of dissolved CO2) pH
is frequently used is measured from pCO2
multiplied by the solubility coefficient of CO2 ➢ The negative logarithm of hydrogen ion
(0.03). → represents carbonic acid level activity
● 0.03 – solubility coefficient ➢ Normal average range → 7.35-7.45
● 0.0307 OR 0.0306 – complete solubility • In terms of clinical significance, pH inside the
coefficient. body must be maintained between 7.35- 7.45
● Normal range is from 1.05-1.45 mmol/L
● Weak acid representative of major buffer Major factors regulating blood pH:
system.
● Readily dissociated into H2O and CO2 1. Chemical buffers → Primary line in order
when it reaches the blood circulation. to prevent fluctuations in the pH.
➢ HCO3 and H2CO3 buffer system,
● Weak acid representative of major buffer (bicarbonate and carbonate buffer
system. system) proteins, hemoglobin,
electrolytes
PARTIAL PRESSURE OF CO2 (pCO2)
➢ With charges
● The pressure or tension exerted by CO2 gas
dissolved in blood. 2. Respiratory regulatory mechanism →
● It is a measurement of efficiency of gas exchange lungs (responsible for the respiratory
happening within the lungs and blood. regulatory mechanism) and kidney (2
● It is an index of efficiency of gas exchange in major organs)
the lungs and not a measure of CO2 ➢ Secondary line/ second line of
concentration in the blood. defense
● Normal range is 35-45 mmHg. ➢ Maintains/regulates the level of
● In pH determination, it is used to determine carbonic acid
carbonic acid level by multiplying it with ➢ Increase in the release of CO2
solubility coefficient. ➢ Increases CO2 concentration by
CARBON DIOXIDE COMBINING POWER (CO2 decreasing exhalation or respiratory
combining power) rate to decrease release of CO2
➢ Lungs regulate the level of carbonic
● The value of CO2 combining power is an acid
index of the amount of CO2 that can be
bound by serum, plasma, or whole blood as 3. Renal regulatory mechanism → kidney
HCO3 at a pCO2 of 40 mmHg at 25°C. ➢ Secondary line
● Normal range → 24-30 mmol/L ➢ Excretion or reabsorption
● Amount of CO2 that is maybe bound
within the blood circulation ➢ Regulates/maintain the level of
bicarbonate
TOTAL CARBON DIOXIDE CONCENTRATION
(ctCO2) → sum of all bicarbonate compounds as well as HENDERSON-HASSELBALCH EQUATION
carbonic acid
● Formerly known as CO2 content. (Carbon
dioxide content)
● Refers to the total concentration of CO2 in the
blood consisting of ionized HCO3, CO3,
carbamino compound) and unionized fraction
(H2CO3) and physically dissolved CO2.
● Normal range → 21-28 mmol/L
● Sum of major buffer system (HCO3 and
carbonic acid H2CO3)
4 | CC2LEC WEEK 7
• It expresses acid-base relationship and is due to the metabolic diversity composing
relates the pH of a solution to the dissociation venous samples
properties of the weak acid
• It indicates that pH depends on the ratio of e. If venous and capillary blood: should
HCO3/pCO2 undergo arterialization (capillary is
• When kidneys and the lungs are functioning preferred since it is a mixture of venous
properly, a 20:1 ratio of HCO3 to H2CO3 will and arterial blood)
be maintained, and it is expressed by the i. Arterialization → inducing
Henderson-Hasselbalch equation. vasodilation and maintain good blood
flow to get the nearest arterial
BLOOD COLLECTION FOR BLOOD GAS AND pH sample
ANALYSIS ii. Warming up the area of extraction
using warming pad
- Responsibility of respiratory therapist →
iii. Not applicable to low blood pressure
capable of collecting the sample and perform
(systole is <95mmHg), conditions
blood gas analysis
that induce vasoconstriction, patients
- Always keep sample using anaerobic technique
undergoing oxygen therapy,
in blood collection prevents too much exposure in
newborns, newborns with respiratory
the ambient air (CO2 in air is less than those
distress syndrome
present in blood) → when exposed, further
decreases because cells will be taking up METHOD OF DETERMINATION
oxygen
Measurement of pO2 (oxygen)
1. The pCO2 of air (0.2 mmHg) is much less than in
● ISE: Clarke pO2 electrode (clark)
blood (38 mmHg) so that when blood is exposed
○ principle: based on amperometric or
to air, the ctCO2 and pCO2 decreases and the pH
polarographic measurement of oxygen
increases.
○ oxygen is equivalent to Clarke
a. Preferred sample is whole blood using
electrode
arterial blood collection (mainly because
● Gasometric analysis
venous blood sample oxygen level is
● Calculation from oxygen saturation, pH and
significantly lower as compared to arterial
temperature by means of the standard O2
blood)
dissociation curve → like in hematology (shift to
i. The blood which is passing
left, right..)
through the vein is what we
● Transcutaneous monitoring → non-invasive
called deoxygenated blood
method where electrode with gel casing to
ii. If mababa yung oxygen sa
maintain the temperature of the skin between
venous blood mas mataas
43-44 C is placed on the patient
naman ang kanyang PCO2
which is 2-8mmHg higher **@ 43-44 C will cause arterialization of
compare to arterial blood capillaries and can somehow measure oxygen
through diffusion of oxygen through skin
b. Ideally collected using glass syringe
(because glass is less porous) and ** method is different from using pulse
lyophilized heparin (powdered form) as oximeter
anticoagulant (liquid heparin results to
Measurement of pCO2 (carbon dioxide)
dilution of sample) → liquid heparin is not
advisable ● Severinghaus electrode: pCO2 electrode
○ principle: based on pH measurement of a
c. Arterial blood sample is preferred because stationary NaHCO3 (SODIUM
Venous blood oxygen level is significantly BICARBONATE) solution which is in
lower but higher pCO2 (2-8 mmHg higher) equilibrium with the test solution and the
→ acidic pH (0.02-0.05 pH lower) test via CO2 permeable membrane
● gasometric analysis
d. Arterial blood is the more preferred specimen ● Henderson Hasselbach equation from pH and
for blood gas analysis because it is of more total CO2
uniform composition than venous blood. This
5 | CC2LEC WEEK 7
● CO2 equilibrium curve from a measured pH ● Caprylic alcohol → prevents foaming/ air
value interpolated bubble formation
● Mercury → separates the sample and other
Measurement of pH reagents, prevents introduction of air and
● pH electrode seals gasometer because the process should
○ Principle: based on polarographic be anaerobic
principle ● Distilled water → washes the sample and
● Typically measured using pH meters or reagent into the reaction chamber
electrodes ** Gasometric analysis is a continuous flow
● Henderson-Hasselbalch equation derivation type of analyzer – all reagents and samples will
be passing through a single analytic pathway
→ Derivation of pH using the HendersonHasselbalch using a peristaltic pump
equation – used as a mathematical derivation for
determining pH based on partial pressure of carbon **Do not use air bubble as separator in
dioxide and bicarbonate level. analyzer → will cause false results due to
production of air → we use mercury
● Nomogram and slide rule → used for plotting
of data ● Alternative Method
● Siggard- Anderson Alignment nomogram - replacing lactic acid with sulfuric acid for the
release of carbon dioxide; methodology is still
Measurement of Ct CO2 (total concentration of the same
CO2) ○ principle: involves the release of CO2
carbon dioxide gas when the sample is
● Gasometric Analysis added to H2SO4 (sulfuric acid) with
2 types: would vary depending on the volume subsequent monitoring of this release with a
of blood pair of pCO2 electrodes (reference and
sample electrodes). The rate of change in pH
a. Macro gasometric method – utilizes more of the buffer inside the pCO2 electrode is a
than 1mL of sample measure of the concentration of its CO2 in
b. micro gasometric method – utilizes less the sample
than 1mL of sample
→measurement is done through electrochemical
2 types of Gasometric Analysis analysis
a. Van Slyke Gasometric Analysis CRITERIA & CONDITIONS for BLOOD GAS
b. Manometric Method using Natelson ANALYSIS – conditions for analysis
Microgasometer
○ Principle: carbon dioxide is released 1. All procedures should be considered “STAT”
front HCO3 by the addition of lactic acid. procedure
The CO2 and other gases are extracted - specimen turnaround time must be short →
under a partial vacuum. The pressure within an hour after extraction should be
difference at constant value before and processed
after absorption of CO2 by NaOH is the **introduction of POTC (point of care_ –
amount of CO2 present in the sample performed on bedside, if none keep sample
- chemicals will be used in order to liberate in ice
the different blood gasses and specific
chemicals which will be used to a. if delayed 20-30 mins: pH lowers by
differentiate oxygen and carbon dioxide 0.01
b. avoid glycolysis – conversion of
Reagents in Natelson Microgasometer Glucose to acetyl coenzyme A to
● 10% lactic acid → releases CO2 from HCO3 produce ATP leading to the liberation of
(bicarbonate ion) CO2 and water
● 12% NaOH → for total reabsorption of CO2 ** blood continuous its metabolic
gas as Na2CO3 process even on lyophilized heparin of
● NaHSO3 → for reabsorption of O2 arterial sample
6 | CC2LEC WEEK 7
** increased pCO2 = increase H2CO3 If respiratory: either retention by decreasing the
(carbonic acid) = decreased pH exhalation of CO2 or increasing the exhalation of
CO2 (hyperventilation and hypoventilation
2. Specimen must be kept at anaerobic
condition METABOLIC ACIDOSIS→ will occur if there is a
- if not, blood will take up oxygen – decrease in bicarbonate
increase O2 = decreased pCO2 =
decreased H2CO3 = increased pH ● caused by bicarbonate deficiency
- how to maintain the anaerobic: empty ● production of increased amount of acid
air in syringe ang bend the needle with ○ diabetic ketoacidosis
cork; do not use winged blood collection ○ lactic acidosis (alcoholism)
- remove air bubble ○ renal failure
3. Specimen w/c cannot be analyzed ○ diarrhea
immediately →must be placed in an ice slurry – ** common involving the excretion of
not advisable due to thermal equilibrium bicarbonate (HCO3- bicarbonate ion)
• Decrease in pH ● Compensation: hyperventilation → will
• Blood is still metabolically active and capable decrease the pCO2/ excrete carbon dioxide
of undergoing glycolysis ● Acidosis: increased in H+ concentration
○ (+) hyperkalemia and hyperchloremia
ACID-BASE DISTURBANCES
● Normochloremic in DKA (diabetic
Acidosis→ decrease in pH, lower than 7.35 ketoacidosis)
● pCO2 drops 1 to 1.3 mmHg per mEq/L fall in
- general term applied for any condition where HCO3
the pH of the blood and the bicarbonate
concentration of the blood are below METABOLIC ALKALOSIS → will occur if there is an
normal increase in bicarbonate
- compensation is alkalosis
● caused by bicarbonate excess
Alkalosis→ increase in Ph, above 7.45 ● conditions
○ vomiting with loss of chloride form
- general term applied for any condition with an the stomach
increase in blood pH (above normal ● Compensation: hypoventilation → will
range) characterized by an elevation in the increased pCO2 concentration → increase
H+ ion accepting buffer of the plasma carbonic acid
(UCO3) and a reduction in the H+ ion ● (+) hypokalemia, hypochloremia
substances (H2CO3) ● For every 10mEq/L rise in bicarbonates, the
- compensation is acidosis pCO2 rises by 6 mmHg
Metabolic RESPIRATORY ACIDOSIS →increase in carbonic
- the affected is bicarbonate (HCO3) acid
concentration ● Excessive accumulation of CO2 (carbon
- compensation is respiratory dioxide)
Respiratory ● Conditions
○ chronic obstructive pulmonary
- the affected is carbonic acid (H2CO3) disease (COPD)
concentration ○ myasthenia gravis
- compensation is metabolic ○ CNS disease
○ drug overdose (morphine,
** whenever there is an imbalance with 1 of the barbiturates and opiates)
regulatory mechanism, the other regulatory ○ pneumonia
mechanism will try to compensate through different
compensatory mechanisms ** common in the decreased release of
CO2 causing accumulation
If metabolic: either excretion or reabsorption
● compensation: retention of bicarbonates →
reabsorb/ retain HCO3
7 | CC2LEC WEEK 7
● Bicarbonate rises 1 mEq/L for each 10 ● HCO3 (22-26 mEq/L) → evaluate the
mmHg rise in pCO2 metabolic process (kidney)
○ <22 – metabolic acidosis
RESPIRATORY ALKALOSIS→ decrease in carbonic ○ >26 – metabolic alkalosis
acid ● determine which is the primary and
● excessive carbon dioxide loss compensating disorder
● Conditions ○ pH
○ Anxiety ● Determine the degree of compensation
○ severe pain ○ non-compensatory
○ aspirin overdose ○ partial compensatory
○ hepatic cirrhosis ○ complete compensatory
● Compensation: decreased reabsorption of ● pO2 (81-100 mmHg) → adequate
bicarbonate in blood circulation by excreting oxygenation
more ○ pO2 hypoxia
● (+) hypokalemia ■ mild (61-80)
● Bicarbonate falls 2 mEq/L for each 10 mmHg ■ moderate (41-60)
fall in pCO2 ■ severe (40 or less)
CONSEQUENCES OF ACID-BASE IMBALANCE BLOOD GAS CALCULATION
● In alkalosis, tetany ensues due to Henderson- Hasselbalch Equation
hypocalcemia, which can lead to death
because of respiratory muscle spasm - equation in determination of pH
● In acidosis, there is an inhibition of the - primary source of equation of pH
neural mechanism which will then lead to
pH = pKa + log [conjugate base/ weak acid]
coma. A blood pH of 6.9 has proven fatal
pH = 6.1 + log [HCO3- / H2CO3+]
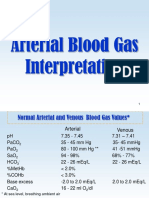
ARTERIAL BLOOD GAS REFERENCE RANGE
AT 37 DEGREE CELCIUS ● pKa → ionization constant of buffer
pH 7.35-7.45
system
pCO2 (mm Hg) 35-45
HCO3- (mmol/L) 22-26 ○ bicarbonate-carbonic acid system
Total CO2 content 23-27 = 6.1 pKa
(mmol/L) ● bicarbonate (HCO3-) → representative
pCO2 (mmol/L) 80-100 conjugate base
SO2 (%) >95 ● carbonic acid (H2CO3) → weak acid;
O2Hb (%) >95 called weak acid because upon entering
the blood circulation/ during gas
PARAMETERS OF INTEREST exchange, bicarbonate? readily
dissociates into water and carbon dioxide
● pH (7.35-7.45)
→ means of measuring carbonic acid is
○ <7.35 – acidosis
○ >7.45 – alkalosis through liberation of products
● pCO2 (35-45 mmHg) → Evaluate the ● partial pressure of CO2 (pCO2) – basis
ventilation (lungs) of carbonic acid/ representative of
○ <35 respiratory alkalosis carbonic acid
○ >45 respiratory acidosis ● total CO2 concentration (tCO2) – sum of
the bicarbonate and carbonic acid
Primary disturbance
22-29 mmol/L →metabolic alkalosis (tCO2 = HCO3- + H2CO3+)
HCO3 →metabolic acidosis
35-45 mmHg →respiratory alkalosis ** carbonic acid is not directly determined but is
pCO2 →respiratory acidosis known through pCO2
● H2CO3 = pCO2 (0.003)
0.03 → solubility coefficient
8 | CC2LEC WEEK 7
pH = 6.1 + log [HCO3 / pCO2 x 0.03] compensatio pH pCO2 HCO3
n
if tCO2 & pCO2 is only given:
Non abn abn N
pH = 6.1 + log [tCO2 - (pCO2x0.03) / pCO2
x0.03] N Abn
** in our body we have different buffer system Partial abn abn abn
responsible in maintaining the pH) at normal
level Complete N abn abn
PARAMETERS ** non compensatory → one buffer system
(pCO2 or HCO3) did not compensate for any
1. pH = 7.35 - 7.45 deviation with the other buffer system
○ acidosis – <7.35
○ alkalosis – >7.45 ** partial/ complete compensatory →
2. Primary Disturbance characterized by abnormal concentration on
○ HCO3 = 22-29 mmol/L both buffer systems. compensation on the buffer
■ metabolic acidosis – decreased with one another
HCO3 (bicarbonate ion) = <22 ~ Partial → condition where in bicarbonate
■ metabolic alkalosis – increased and carbonic acid did its compensatory
HCO3 = >29
mechanism but not sufficient enough to
** metabolic conditions are named as normalize the pH
such because bicarbonate is primarily ~ Complete → condition where in
regulated by kidney (renal regulatory bicarbonate and carbonic acid did its
mechanism) → absorbed or excreted
compensatory mechanism, normalizing the
○ pCO2 (representative of H2CO3- pH concentration
sulfurous acid) = 35-45 mmHg 4. Degree of Oxygenation
■ respiratory acidosis – increased
in acid → >45 pO2 = 85-105 mmHg or mmol/L
■ respiratory alkalosis – decreased
** pO2 → not included in the equation; just
in pCo2 → <35
evaluate based on the given
** respiratory because the means to
** clinically significant – below normal → find
regulate CO2 is through gas exchange
the category of condition with hypoxemia (low
with O2 (respiratory regulatory
oxygen in the blood) – not detected by oximeter
mechanism). Primary organ to lungs.
3. Degree of Compensation – mechanism of Degree of hypoxemia mmHg
body to revert back to normal pH level.
- mechanism involving 1 buffer system
mild >61; <84 (61-84)
adjusting for the other buffer system
which has a primary disturbance moderate >41: <60 (41-60)
- example: respiratory acidosis →
kidney (HCO2) will compensate by severe <40
inducing metabolic alkalosis
NORMAL >90
OXYGENATION
9 | CC2LEC WEEK 7
Sample Problem 1: Note:
pH = ? 7.31 → abn = acidosis In looking for primary disturbance:
pCO2 = 47 mmHg → abn = acidosis ** pH normal → biggest deviation from normal
range
HCO3 = 23 mmol/L → N
** pH is abnormal → base on the pH
pO2 = 65 mmHg → mild hypoxemia
1. Which of the following represents the Henderson–
Hasselbalch equation as applied to blood pH?
Degree of compensation → non compensatory A. pH = 6.1 + log HCO3–/PCO2
primary disturbance (base is on the pH) → B. pH = 6.1 + log HCO3–/(0.03 × PCO2)
respiratory acidosis
C. pH = 6.1 + log dCO2/HCO3–
interpretation: patient has non-compensatory
D. pH = 6.1 + log (0.03 × PCO2)/HCO3–
respiratory acidosis with mild hypoxemia
2. What is the PO2 of calibration gas containing
** primary disturbance should correlate with the
pH if no, repeat 20.0% O2, when the barometric pressure is 30 in.?
Sample problem 2: A. 60 mm Hg
pH = ? 7.42 → N B. 86 mm Hg
pCO2 = 49 mmHg → abn = respiratory acidosis C. 143 mm Hg
HCO3 = 31 mmol/L → abn = metabolic alkalosis D. 152 mm Hg
pO2 = 90 → N 3. What is the blood pH when the partial pressure of
carbon dioxide (PCO2) is 60 mm Hg and the
evaluate:
bicarbonate concentration is 18 mmol/L?
complete compensated – can determine primary
A. 6.89
disturbance or proceed without it
B. 7.00
** how to know the disturbance: buffer system
with biggest deviation from the normal range C. 7.10
Interpretation/ evaluation: complete D. 7.30
compensatory with normal oxygenation /
complete compensatory, respiratory acidosis What is the PCO2 if the dCO2 is 1.8 mmol/L?
with normal oxygenation
A. 24 mm Hg
Sample problem 3:
B. 35 mm Hg
pH = ? 7.46 → abn = alkalosis
C. 60 mm Hg
pCO2 = 29 mmHg –. abn = respiratory alkalosis
D. 72 mm Hg
HCO3 = 20 mmol/L → abn = metabolic acidosis
What is the maximum recommended storage time
pO2 = 55 mmHg → moderate hypoxemia and temperature for an arterial blood gas sample
Interpretation/ evaluation: partial drawn in a plastic syringe
compensatory, respiratory alkalosis with
D. 30 min 22 degree Celsius
moderate hypoxemia
10 | C C 2 L E C W E E K 7
Which condition results in metabolic acidosis with
severe hypokalemia and chronic alkaline urine?
A. Diabetic ketoacidosis
B. Phenformin-induced acidosis
C. Renal tubular acidosis
D. Acidosis caused by starvation
Which of the following mechanisms is responsible
for metabolic acidosis?
A. Bicarbonate deficiency
B. Excessive retention of dissolved CO2
C. Accumulation of volatile acids
D. Hyperaldosteronism
6. Which of the following disorders is associated with
lactate acidosis?
A. Diarrhea
B. Renal tubular acidosis
C. Hypoaldosteronism
D. Alcoholism
Which of the following conditions is classified as
normochloremic acidosis?
A. Diabetic ketoacidosis
B. Chronic pulmonary obstruction
C. Uremic acidosis
D. Diarrhea
You might also like
- Test Bank For High Acuity Nursing 6th Edition Kathleen Dorman WagnerDocument18 pagesTest Bank For High Acuity Nursing 6th Edition Kathleen Dorman WagnerDavidRobinsonfikq100% (41)
- Mechanical Ventilation Learning Package: Sharon-Ann Shunker, CNC, Liverpool ICU SWSLHD 2/3/2016Document75 pagesMechanical Ventilation Learning Package: Sharon-Ann Shunker, CNC, Liverpool ICU SWSLHD 2/3/2016Hanni HarahapNo ratings yet
- Mtap421 BloodgasesDocument11 pagesMtap421 BloodgasesNhelomar ManlinconNo ratings yet
- Applications of The Henderson Hasselbalch EquationDocument8 pagesApplications of The Henderson Hasselbalch EquationSittie Fahieda AloyodanNo ratings yet
- Acid-Base Balance: Editor: Dr. Husnil Kadri, MkesDocument66 pagesAcid-Base Balance: Editor: Dr. Husnil Kadri, MkesDwi SiregarNo ratings yet
- Acid Base Balance Respiratory (2024)Document42 pagesAcid Base Balance Respiratory (2024)khilmiaNo ratings yet
- ABGDocument7 pagesABGEva Marie GaaNo ratings yet
- Chapter 1 Acid-Base Regulation: Lesser Amounts of Organic Acid Derive From The FollowingDocument52 pagesChapter 1 Acid-Base Regulation: Lesser Amounts of Organic Acid Derive From The FollowingMarwa RagabNo ratings yet
- Blood GasesDocument51 pagesBlood Gasesrbm121415chyNo ratings yet
- Acid-Base BalanceDocument7 pagesAcid-Base BalanceMichelle Mae JulianaNo ratings yet
- Acid-Base Balance, Dr. MiaDocument45 pagesAcid-Base Balance, Dr. MiaeuiskurNo ratings yet
- CC2 - Lec9 1Document5 pagesCC2 - Lec9 1Glecy PaciaNo ratings yet
- Blood Gases, PH, and Buffer SystemDocument22 pagesBlood Gases, PH, and Buffer SystemtabletvodaNo ratings yet
- Peran Ginjal Dalam Kesetimbangan Asam Basa DarahDocument30 pagesPeran Ginjal Dalam Kesetimbangan Asam Basa DarahgardamdNo ratings yet
- Blood Gases, PH and Buffer Systems: DefinitionsDocument4 pagesBlood Gases, PH and Buffer Systems: DefinitionsMj TizonNo ratings yet
- 835 Regulation of Acid Base Balance 2019Document26 pages835 Regulation of Acid Base Balance 2019sanofazal786No ratings yet
- Acid BaseDocument10 pagesAcid BaseFiona Marie Kyla TunayNo ratings yet
- Acid Base BalanceDocument104 pagesAcid Base BalanceKevin VillaranteNo ratings yet
- Acid Base Im Balance-2a - 3.05.2021Document75 pagesAcid Base Im Balance-2a - 3.05.2021Kavya FouzdarNo ratings yet
- 3 Acid Base ImbalanceDocument5 pages3 Acid Base ImbalanceSJane FeriaNo ratings yet
- Cchm2 MidtermsDocument22 pagesCchm2 MidtermsMACOB, ETHELHYN JHANE100% (1)
- Acid Base BalanceDocument38 pagesAcid Base Balancelady birdNo ratings yet
- Acid Base Disorders-MD3Document44 pagesAcid Base Disorders-MD3juliuskahabi1No ratings yet
- Acid-Base BalanceDocument11 pagesAcid-Base Balancemostafadiab074No ratings yet
- Introduction To Biochemistry Proteins Buffers in Blood Plasma and CellsDocument5 pagesIntroduction To Biochemistry Proteins Buffers in Blood Plasma and CellsGwyn Louise CarolinoNo ratings yet
- 9 - (D) Acid Base Balance Dec 4.17Document61 pages9 - (D) Acid Base Balance Dec 4.17khaledNo ratings yet
- Fluid-Electrolytes and Acid-Base Disturbance in Surgery: Haidi Hu, MD, PHDDocument68 pagesFluid-Electrolytes and Acid-Base Disturbance in Surgery: Haidi Hu, MD, PHDHUNEL KimNo ratings yet
- Acid Base Regulation and Its DisordersDocument80 pagesAcid Base Regulation and Its DisordersPirate CoolNo ratings yet
- Acid Base Balance DR NaimDocument136 pagesAcid Base Balance DR NaimTaimoor Ul HassanNo ratings yet
- Acid-Base Balance and Its DisordersDocument37 pagesAcid-Base Balance and Its Disordersmaria angela SaldajenoNo ratings yet
- Daily Acid Load: Carbonic or Volatile Acid (H CO Carbonic AcidsDocument11 pagesDaily Acid Load: Carbonic or Volatile Acid (H CO Carbonic AcidsPrastia StratosNo ratings yet
- BCH 201 ModuleDocument15 pagesBCH 201 ModuleJoyNo ratings yet
- Hydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionDocument15 pagesHydrogen Hydroxide: Acid-Base Balance Overview of Acids and Bases DescriptionElisha WorworNo ratings yet
- Gangguan Asam BasaDocument51 pagesGangguan Asam BasaYudhistira YuliandraNo ratings yet
- Acid Base Balance OR OR Regulation of Blood PHDocument175 pagesAcid Base Balance OR OR Regulation of Blood PHhirendra patel100% (1)
- 1st Chap-2Document40 pages1st Chap-2RJ Noor JanNo ratings yet
- Physiology of Acid Base Balance by Dr. ROOMIDocument70 pagesPhysiology of Acid Base Balance by Dr. ROOMIMudassar Roomi100% (1)
- Acid Base PhysiologyDocument54 pagesAcid Base PhysiologyDiana AyónNo ratings yet
- Acid Base Regulation - ppt@BVSCAH-6th SemDocument95 pagesAcid Base Regulation - ppt@BVSCAH-6th SemDr. Prakash PanthiNo ratings yet
- Draft ACID BASEDocument5 pagesDraft ACID BASEkimmynemil80No ratings yet
- Acid Base BalanceDocument50 pagesAcid Base BalanceEgun Nuel DNo ratings yet
- CO + H O H + Hco: Overall ReactionDocument12 pagesCO + H O H + Hco: Overall ReactionLuke ShantiNo ratings yet
- Acid Base DisorderDocument48 pagesAcid Base DisorderAGUNG SETIADI NUGROHONo ratings yet
- 14-Acid-Base DisordersDocument19 pages14-Acid-Base Disordersمصطفى محمد جواد كاظمNo ratings yet
- Blood Gases, PH, and Buffer SystemDocument22 pagesBlood Gases, PH, and Buffer SystemAhmed GaberNo ratings yet
- Cc2lec - Module 4Document6 pagesCc2lec - Module 4LUKENo ratings yet
- Acid Base Balance NotesheetDocument12 pagesAcid Base Balance NotesheetMariam MohammedNo ratings yet
- CLINICAL CHEMISTRY 2 LecDocument14 pagesCLINICAL CHEMISTRY 2 LecMACOB, ETHELHYN JHANENo ratings yet
- Acid Base2005Document64 pagesAcid Base2005AgusNo ratings yet
- O.M.O - Acid Base Balance and DisordersDocument50 pagesO.M.O - Acid Base Balance and DisordersIiiNo ratings yet
- BicarbonateDocument5 pagesBicarbonateRace MendezNo ratings yet
- Acid-Base BalanceDocument38 pagesAcid-Base BalanceNym Angga SantosaNo ratings yet
- Disorders of Acid Base BalanceDocument45 pagesDisorders of Acid Base BalanceTee Sze WayNo ratings yet
- Acid Base BalanceDocument5 pagesAcid Base BalanceAnila zafarNo ratings yet
- Acid - Base BalancesDocument68 pagesAcid - Base Balancesjames makulaNo ratings yet
- Acid-Base BalanceDocument94 pagesAcid-Base BalanceJagan KumarNo ratings yet
- Pengaturan Asam-Basa & ElektrolitDocument40 pagesPengaturan Asam-Basa & ElektrolitArifuddinZrNo ratings yet
- Discussion 5 Blood Gases LectureDocument139 pagesDiscussion 5 Blood Gases LectureFaith Tambong100% (1)
- Acid Base RehabDocument54 pagesAcid Base RehabKushie GuezyNo ratings yet
- Acid-Base Balance and DisodersDocument86 pagesAcid-Base Balance and DisodersPrincewill SeiyefaNo ratings yet
- Biochemistry Applied to the Brewing Processes - Mashing, Boiling, CoolingFrom EverandBiochemistry Applied to the Brewing Processes - Mashing, Boiling, CoolingNo ratings yet
- CC2 Lab 13Document10 pagesCC2 Lab 13Junea SeeNo ratings yet
- Cc2 Lec 13 Trace ElementsDocument21 pagesCc2 Lec 13 Trace ElementsJunea SeeNo ratings yet
- Cc2 Lec EnzymesDocument25 pagesCc2 Lec EnzymesJunea SeeNo ratings yet
- Cc2lec 14 Intro To ToxiDocument30 pagesCc2lec 14 Intro To ToxiJunea SeeNo ratings yet
- Acid-Base Disorders in The Critically Ill PatientDocument11 pagesAcid-Base Disorders in The Critically Ill PatientAniAliciaOrtizCastleNo ratings yet
- Acid Base BalanceDocument167 pagesAcid Base BalancePratap Sagar Tiwari100% (1)
- THAM MonographDocument34 pagesTHAM MonographzaaklcxNo ratings yet
- Harvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateDocument21 pagesHarvade College of Science, Business and Management Studies Polt 1-12, Harvade Close, Off Obada Road Abeokuta Ogun StateOluwaseun TosinNo ratings yet
- Acid Base BalanceDocument27 pagesAcid Base BalanceKamran Khan KhalilNo ratings yet
- Final GusDocument57 pagesFinal GusDebbi YuniseraniNo ratings yet
- Acid Base Balance Flashcards QuizletDocument1 pageAcid Base Balance Flashcards QuizletapolloNo ratings yet
- Arterial Blood Gas InterpretationDocument69 pagesArterial Blood Gas InterpretationostuffeNo ratings yet
- Physiology Handbook December 2022 PDFDocument280 pagesPhysiology Handbook December 2022 PDFrachel wongNo ratings yet
- Hand Out 3 Respiratory System Overview PDFDocument12 pagesHand Out 3 Respiratory System Overview PDFGrape JuiceNo ratings yet
- Fluid and ElectrolytesDocument13 pagesFluid and ElectrolytesMarcus, RN100% (7)
- 'Block E With Keys and Hints ' With YouDocument36 pages'Block E With Keys and Hints ' With YouAbdullah TanoliNo ratings yet
- Anatomy and Physiology of Respiratory SystemDocument34 pagesAnatomy and Physiology of Respiratory SystemSamson SeiduNo ratings yet
- Indication For Arterial Blood Gas AnalysisDocument10 pagesIndication For Arterial Blood Gas AnalysisRohini RaiNo ratings yet
- Steps in ABG Analysis Using The Tic-Tac-Toe MethodDocument4 pagesSteps in ABG Analysis Using The Tic-Tac-Toe MethodSeanmarie CabralesNo ratings yet
- Fluid Electrolytes and Acid Base BalanceDocument23 pagesFluid Electrolytes and Acid Base BalanceJohn MalkovicNo ratings yet
- MineralsDocument70 pagesMineralsVioletteNo ratings yet
- Chemistry of Life: By: Ruth Abigail C. ValdezDocument39 pagesChemistry of Life: By: Ruth Abigail C. ValdezPanJan BalNo ratings yet
- Human Anatomy and Physiology by Hema Seliya-3Document7 pagesHuman Anatomy and Physiology by Hema Seliya-3Priya YadavNo ratings yet
- Laboratory Animal Nutrition Nutrient Requirement of Mice Rat Rabbit Guinea PigDocument66 pagesLaboratory Animal Nutrition Nutrient Requirement of Mice Rat Rabbit Guinea PigyohanNo ratings yet
- Fluid Electrolytes and Acid Base BalanceDocument108 pagesFluid Electrolytes and Acid Base BalancesayednourNo ratings yet
- ABIDocument27 pagesABIekramNo ratings yet
- Effects of Malaria Parasitaemia On Electrolytes (NA, K, CL, HCO3) and Some Liver Enzymes (AST and ALT) in Patient Attending University of Maiduguri Teaching HospitalDocument19 pagesEffects of Malaria Parasitaemia On Electrolytes (NA, K, CL, HCO3) and Some Liver Enzymes (AST and ALT) in Patient Attending University of Maiduguri Teaching HospitalAcademic JournalNo ratings yet
- Sodium Bicarbonate in J AftDocument9 pagesSodium Bicarbonate in J AftMohd Faizal SimonNo ratings yet
- Acid Base Disorders DR Kwaifa - PPTX 1Document99 pagesAcid Base Disorders DR Kwaifa - PPTX 1DICKSONNo ratings yet
- University of Makati College of Allied Health Studies Center of NursingDocument32 pagesUniversity of Makati College of Allied Health Studies Center of NursingE.J. PelayoNo ratings yet
- 003Document358 pages003Gordana UzelacNo ratings yet
- PhysioEx Exercise 10 Activity 3 - Balamad, Maria Karla M.Document3 pagesPhysioEx Exercise 10 Activity 3 - Balamad, Maria Karla M.Maria Karla BalamadNo ratings yet