Professional Documents
Culture Documents
Delirium Pathway - OTLPCM002-3
Delirium Pathway - OTLPCM002-3
Uploaded by
Iftida YatiCopyright:
Available Formats
You might also like
- DSM 5 Clinical Cases NotesDocument1 pageDSM 5 Clinical Cases Notestim clayNo ratings yet
- Epilepsy Management Plan TemplateDocument2 pagesEpilepsy Management Plan TemplateIPNo ratings yet
- Generic Run Report: Prehospital Patient Care ChartDocument2 pagesGeneric Run Report: Prehospital Patient Care ChartBCF PRODUCTIONNo ratings yet
- Depression PsychoticDocument10 pagesDepression Psychoticharumimiaomiao_198930% (1)
- Chapter 21 Antidepressant AgentsDocument4 pagesChapter 21 Antidepressant AgentsNicolle Lisay IlaganNo ratings yet
- Group Medical Appointments: An Introduction for Health ProfessionalsFrom EverandGroup Medical Appointments: An Introduction for Health ProfessionalsRating: 5 out of 5 stars5/5 (1)
- Well Being: Striving For Good Health in Tribal CommunitiesDocument39 pagesWell Being: Striving For Good Health in Tribal CommunitiesRose Weeks100% (1)
- DeliriumDocument27 pagesDeliriumBushra EjazNo ratings yet
- Behaviors: How To Respond When Dementia Causes Unpredictable BehaviorsDocument12 pagesBehaviors: How To Respond When Dementia Causes Unpredictable BehaviorsJohn GurungNo ratings yet
- Easter Word HuntDocument1 pageEaster Word Huntmihaela165No ratings yet
- Aetiology: PhysiologicalDocument4 pagesAetiology: PhysiologicalLeong Zhee ChuanNo ratings yet
- Antidepressants: I. Cyclic AntidepressantDocument17 pagesAntidepressants: I. Cyclic AntidepressantVaibhav KrishnaNo ratings yet
- SchizophreniaDocument1 pageSchizophreniaBrittNo ratings yet
- Presented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Document17 pagesPresented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Akanksha KapoorNo ratings yet
- CEP BPSD Discussion Guide ENG RFCG Updated2019 PDFDocument8 pagesCEP BPSD Discussion Guide ENG RFCG Updated2019 PDFM.DalaniNo ratings yet
- AIMS. Scales-Abnormal-Involuntary-Movement-Scale PDFDocument2 pagesAIMS. Scales-Abnormal-Involuntary-Movement-Scale PDFVictoria RomeroNo ratings yet
- Generic Normal Psychiatric Established-Patient Med CheckDocument2 pagesGeneric Normal Psychiatric Established-Patient Med CheckkeishaNo ratings yet
- Antipsychotic DrugsDocument47 pagesAntipsychotic DrugsIkram UddinNo ratings yet
- My Basal GangliaDocument18 pagesMy Basal GangliaPriya GKNo ratings yet
- Eating Disorders: by Dr. Min Min Phyo 20 August 2019Document74 pagesEating Disorders: by Dr. Min Min Phyo 20 August 2019thu thuNo ratings yet
- Geriatric Giants - DR SeymourDocument108 pagesGeriatric Giants - DR SeymourSharon Mallia100% (1)
- Tension Headaches: What Is A Tension Headache? HighlightsDocument9 pagesTension Headaches: What Is A Tension Headache? HighlightsIndryNo ratings yet
- Notes On J K BaxterDocument4 pagesNotes On J K Baxteraleaf17No ratings yet
- Psychiatry 3rd EditionDocument205 pagesPsychiatry 3rd EditionIva LučićNo ratings yet
- Communication Skills Behavioural Treatment For OCDDocument5 pagesCommunication Skills Behavioural Treatment For OCDTeslim RajiNo ratings yet
- Dual Diagnosis - Clinical and Therapeutic Aspects (Maremmani 03)Document92 pagesDual Diagnosis - Clinical and Therapeutic Aspects (Maremmani 03)antonelloveltriNo ratings yet
- Vascular DementiaDocument57 pagesVascular Dementiadrkadiyala2No ratings yet
- Antipsychotic Deprescribing Algorithm PDFDocument2 pagesAntipsychotic Deprescribing Algorithm PDFFitri Amelia RizkiNo ratings yet
- 2 Af 5 VERTIGODocument35 pages2 Af 5 VERTIGOmuneceNo ratings yet
- AntipsychoticsDocument22 pagesAntipsychoticsvinodksahuNo ratings yet
- Pharmacotherapy of Alzheimers DiseaseDocument69 pagesPharmacotherapy of Alzheimers DiseaseCAROL ANN PATITICONo ratings yet
- Antipsychotic-Induced Extrapyramidal Syndromes andDocument144 pagesAntipsychotic-Induced Extrapyramidal Syndromes andSeiska Mega100% (1)
- Bariatric Surgery BH Grand RoundsDocument39 pagesBariatric Surgery BH Grand Roundsapi-440514424No ratings yet
- PDF VersionDocument6 pagesPDF Versionservicesmi123100% (1)
- Module 3 Biochemistry of The BrainDocument12 pagesModule 3 Biochemistry of The BrainSakshi Jauhari100% (1)
- Mental Health Medications For Children - Fact Sheets - Yale MedicineDocument5 pagesMental Health Medications For Children - Fact Sheets - Yale MedicinewaleskacrzNo ratings yet
- Mental Status ExamDocument1 pageMental Status Examjnyg008No ratings yet
- Stress Management Techniques Evidencebased Procedures That Reduce Stress and Promote Health PDFDocument16 pagesStress Management Techniques Evidencebased Procedures That Reduce Stress and Promote Health PDFMaica MagbitangNo ratings yet
- Basal Ganglia: Sridharan Neelamegan MMCDocument23 pagesBasal Ganglia: Sridharan Neelamegan MMCRetrocasualty Find OutNo ratings yet
- DEPRESSDocument23 pagesDEPRESSWong Chew Nie100% (1)
- Chief ComplaintDocument3 pagesChief Complaintjose acasusoNo ratings yet
- Degenerative Diseases of The Brain 2Document66 pagesDegenerative Diseases of The Brain 2Janie-Vi Villamor Ismael-GorospeNo ratings yet
- Mindfulness MattersDocument9 pagesMindfulness MattersumifNo ratings yet
- Johari WindowDocument10 pagesJohari WindowIra SinghNo ratings yet
- Dementia: Dr. Sharlene Alick OrtizDocument32 pagesDementia: Dr. Sharlene Alick OrtizShary AlickNo ratings yet
- Headache OverviewDocument29 pagesHeadache OverviewFiqna SyaniNo ratings yet
- SchiDocument23 pagesSchiMichelle SatairapanNo ratings yet
- AntideprresentDocument54 pagesAntideprresentHadiqa KhanNo ratings yet
- Eating Disorder Lecture 10Document39 pagesEating Disorder Lecture 10Mawadh AlsbhiNo ratings yet
- Background: Binge EatingDocument15 pagesBackground: Binge EatingCintaAllah Sokmo100% (1)
- Dementia Evaluation and TreatmentDocument12 pagesDementia Evaluation and Treatmentrofi modiNo ratings yet
- Antiepileptics (Autosaved)Document57 pagesAntiepileptics (Autosaved)vishal singhNo ratings yet
- Vertigo & Its ManagementDocument32 pagesVertigo & Its Managementramchandra joshiNo ratings yet
- AlzheimerDocument8 pagesAlzheimerkavithaNo ratings yet
- Lewy Body Dementias Dementia With Lewy Bodies And.9Document29 pagesLewy Body Dementias Dementia With Lewy Bodies And.9Cristina GhizdavetNo ratings yet
- Drug StudyDocument10 pagesDrug StudyRubie Ann TillorNo ratings yet
- Sedative-Hypnotics (SeH) and AnxiolyticsDocument101 pagesSedative-Hypnotics (SeH) and Anxiolyticsmatchees-gone rogueNo ratings yet
- Schizophrenia & Other Psychotic DisordersabpsychDocument12 pagesSchizophrenia & Other Psychotic DisordersabpsychMary HiboNo ratings yet
- Perinatal+Anxiety+and+Depressive+Disorders PPG v3.0Document13 pagesPerinatal+Anxiety+and+Depressive+Disorders PPG v3.0tanmai nooluNo ratings yet
- Legal and Ethical Aspects of Mental Health CareDocument5 pagesLegal and Ethical Aspects of Mental Health CarebrajshekharNo ratings yet
- Ebook OCDDocument22 pagesEbook OCDMagda MoldovanNo ratings yet
- Pandemic Mental - Learn the Secrets to Stay Positive and Improve your Mental Health During this PandemicFrom EverandPandemic Mental - Learn the Secrets to Stay Positive and Improve your Mental Health During this PandemicNo ratings yet
- AuthorsDocument10 pagesAuthorsIftida YatiNo ratings yet
- Efektivitas Edukasi Video Dalam Upaya Pencegahan Diare Pada Anak Kelas 3 Madrasah Hasyim Asyari Pulosari TulungagungDocument11 pagesEfektivitas Edukasi Video Dalam Upaya Pencegahan Diare Pada Anak Kelas 3 Madrasah Hasyim Asyari Pulosari TulungagungIftida YatiNo ratings yet
- 234-Article Text-987-2-10-20221101Document6 pages234-Article Text-987-2-10-20221101Iftida YatiNo ratings yet
- FOI 3647 20bDocument20 pagesFOI 3647 20bIftida YatiNo ratings yet
- Pola Makan Dan Konsumsi Alkohol Sebagai Faktor Risiko Hipertensi Pada LansiaDocument12 pagesPola Makan Dan Konsumsi Alkohol Sebagai Faktor Risiko Hipertensi Pada LansiaIftida YatiNo ratings yet
- Consent - What You Have A Right To Expect: A Guide For ParentsDocument12 pagesConsent - What You Have A Right To Expect: A Guide For Parentshanzierox3825No ratings yet
- Kegawatan Respirasi May2016-FkumyDocument62 pagesKegawatan Respirasi May2016-FkumyAgustina Tri P. DNo ratings yet
- Neurologic Ncle XDocument6 pagesNeurologic Ncle XAngelica Superable Nacion100% (2)
- Canadian Association of General Surgeons Evidence Based Reviews in Surgery. 12Document3 pagesCanadian Association of General Surgeons Evidence Based Reviews in Surgery. 12Javier Vladimir Ramírez BlancoNo ratings yet
- NCM 104: Community Health Nursing (Lecture) : Topic: National Health Programs of The Doh - Family Health ServicesDocument10 pagesNCM 104: Community Health Nursing (Lecture) : Topic: National Health Programs of The Doh - Family Health ServicesChloe TangonanNo ratings yet
- Advanced Dental Documentation ActivitiesDocument2 pagesAdvanced Dental Documentation Activitiesjenea tNo ratings yet
- Productflyer - 978 1 58829 211 7Document1 pageProductflyer - 978 1 58829 211 7Nadya Rahmawati PutriNo ratings yet
- Elfa El Yana (Ne 2)Document6 pagesElfa El Yana (Ne 2)Elfa El YanaNo ratings yet
- Winchester Public School Pediculosis (Head Lice) : Our GoalsDocument2 pagesWinchester Public School Pediculosis (Head Lice) : Our GoalsFebby Indah NurcahyatiNo ratings yet
- Micronutrient Program: PGI Ebarle, Danica PGI Trinidad, Precious BDocument10 pagesMicronutrient Program: PGI Ebarle, Danica PGI Trinidad, Precious BPrecious TrinidadNo ratings yet
- Prostho Prelim LectureDocument12 pagesProstho Prelim LectureChristine LomuntadNo ratings yet
- HealthallergyDocument11 pagesHealthallergyMary Rose QuimanjanNo ratings yet
- Scientific Rationale For Benefits of BreasfteedingDocument7 pagesScientific Rationale For Benefits of BreasfteedingArfian Deny PNo ratings yet
- Introduction of Teaching Strategies For The Middle To Late ChildhoodDocument2 pagesIntroduction of Teaching Strategies For The Middle To Late Childhoodjessa bella materNo ratings yet
- Mommies Act (Lyn18446)Document32 pagesMommies Act (Lyn18446)Senator Cory BookerNo ratings yet
- Bosh Orientation PresentationDocument47 pagesBosh Orientation Presentationsafety officerNo ratings yet
- Subarachno Id Hemorrhag E: DONE BY: Rawan AlebousDocument54 pagesSubarachno Id Hemorrhag E: DONE BY: Rawan AlebousHiba AliNo ratings yet
- Salford Royal NHS Foundation Trust AHP Long Term Placement RequestsDocument4 pagesSalford Royal NHS Foundation Trust AHP Long Term Placement RequestsMD Luthfy LubisNo ratings yet
- Kumpulan Jurnal MedicinusDocument48 pagesKumpulan Jurnal MedicinusFatikhatul BaruniNo ratings yet
- KoledokolitiasisDocument6 pagesKoledokolitiasisnadya nazwinnNo ratings yet
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesNez TraehNo ratings yet
- Kielene Copy: Nararapat Na Maging Bukas Ang Aborsyon para Sa Lahat NG Kababaihan (Panig NG Di Sang-Ayon)Document11 pagesKielene Copy: Nararapat Na Maging Bukas Ang Aborsyon para Sa Lahat NG Kababaihan (Panig NG Di Sang-Ayon)Kielene PalosNo ratings yet
- Journal Reading FixDocument20 pagesJournal Reading FixElsa MayoraNo ratings yet
- CATARACTSDocument2 pagesCATARACTSHanee Kaye TagubaNo ratings yet
- NCM 112 LEC Topic 14 Communicable DiseasesDocument6 pagesNCM 112 LEC Topic 14 Communicable DiseasesViviene Faye FombuenaNo ratings yet
- 2006 Canadian Dementia GuidelinesDocument197 pages2006 Canadian Dementia GuidelinesjamesNo ratings yet
- Hospital Org-ChartDocument1 pageHospital Org-ChartEric OrnaNo ratings yet
- EHS Awareness (EHS Tips For Harmattan Season) - Ghana - Feb W7, 2020Document12 pagesEHS Awareness (EHS Tips For Harmattan Season) - Ghana - Feb W7, 2020JonathanNo ratings yet
Delirium Pathway - OTLPCM002-3
Delirium Pathway - OTLPCM002-3
Uploaded by
Iftida YatiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Delirium Pathway - OTLPCM002-3
Delirium Pathway - OTLPCM002-3
Uploaded by
Iftida YatiCopyright:
Available Formats
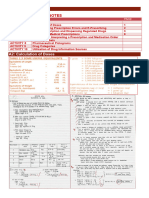
DELIRIUM CARE PATHWAY
Guidance to the detection and management of delirium in adult inpatients
1. RECOGNISE
DELIRIUM CARE PATHWAY
History of sudden change from usual cognitive baseline (often fluctuating)
Obtain collateral history from relative/ friend/carer/GP
Look for: Hypoactivity, Lethargy, Reduced consciousness, Attention deficit,
Guidance to the detection
Sleep disturbance, andHyperactivity,
Hallucinations, management of delirium
slurred in adult inpatients
speech, Confusion Predisposing factors:
Age > 65 years, immobility, pain,
2. DIAGNOSE dementia, sensory impairment,
pelvic/limb/NOF #, previous
Complete 4AT (on reverse) record score and delirium diagnosis in notes episodes of delirium
4 or above: possible delirium +/- cognitive impairment
1-3: possible cognitive impairment
0: delirium or severe cognitive impairment unlikely (but delirium still
possible if [4] information incomplete)
3. CONSIDER CAUSE Precipitating factors:
• Investigations: FBC, UEs, CRP, LFT, Ca, B12, Folate, TFT, Urinalysis, CXR, ECG, Infection, acute illness, surgery,
consider neuroimaging (CT/MRI), bladder scan, rule out constipation, cognitive polypharmacy, catheterisation,
impairment pain assessment scale (on intranet), medication review metabolic disorder, electrolyte
disturbance, dehydration, low
BP, hypoxia, pain, environment,
4. MANAGEMENT: START DELIRIUM CAREPLAN constipation, urine retention ,
Some medications such as
Medical Environmental steroids etc.
Adequate lighting/use of
1. Correct and manage precipitating sensory aids (prescription
and predisposing factors glasses/hearing aids)
Staff continuity
2. If in distress with risk to Promotion of mobility and
self/others: senior review, encourage independence
document capacity and best Falls prevention strategies If no clinical
interest and consider: Orientation aides (clock and improvement is observed
calendar) after 72 hours:
Regular short term, low dose Promote sleep hygiene
antipsychotic (1 week or less) Provide occupation and Re-evaluate and
such as Haloperidol or distraction optimise management
Risperidone. Start at lowest Oral hydration and nutrition if Repeat 4AT
clinically appropriate dose, titrate safe to do so
cautiously according to For further advice and
Consider close supervision
symptoms. Contraindicated in guidance please
Involve relatives/carers in day
Parkinson’s disease, Lewy to day management (open contact Jo Dron or Iain
body syndromes and visiting times). Offer ‘ Delirium’ Tredway on 3208
prolonged QTc. leaflet. /6845 bleep 955
In lewy body dementias and
Parkinson’s disease use Avoid: restraints; confrontation; ward
Quetiapine. moves; unnecessary interventions/ Update September 2018
3. Repeat 4AT daily until investigations; catheters; excess OTLPCM002
environmental noise
resolved
4. Repeat 4AT as often as needed
You might also like
- DSM 5 Clinical Cases NotesDocument1 pageDSM 5 Clinical Cases Notestim clayNo ratings yet
- Epilepsy Management Plan TemplateDocument2 pagesEpilepsy Management Plan TemplateIPNo ratings yet
- Generic Run Report: Prehospital Patient Care ChartDocument2 pagesGeneric Run Report: Prehospital Patient Care ChartBCF PRODUCTIONNo ratings yet
- Depression PsychoticDocument10 pagesDepression Psychoticharumimiaomiao_198930% (1)
- Chapter 21 Antidepressant AgentsDocument4 pagesChapter 21 Antidepressant AgentsNicolle Lisay IlaganNo ratings yet
- Group Medical Appointments: An Introduction for Health ProfessionalsFrom EverandGroup Medical Appointments: An Introduction for Health ProfessionalsRating: 5 out of 5 stars5/5 (1)
- Well Being: Striving For Good Health in Tribal CommunitiesDocument39 pagesWell Being: Striving For Good Health in Tribal CommunitiesRose Weeks100% (1)
- DeliriumDocument27 pagesDeliriumBushra EjazNo ratings yet
- Behaviors: How To Respond When Dementia Causes Unpredictable BehaviorsDocument12 pagesBehaviors: How To Respond When Dementia Causes Unpredictable BehaviorsJohn GurungNo ratings yet
- Easter Word HuntDocument1 pageEaster Word Huntmihaela165No ratings yet
- Aetiology: PhysiologicalDocument4 pagesAetiology: PhysiologicalLeong Zhee ChuanNo ratings yet
- Antidepressants: I. Cyclic AntidepressantDocument17 pagesAntidepressants: I. Cyclic AntidepressantVaibhav KrishnaNo ratings yet
- SchizophreniaDocument1 pageSchizophreniaBrittNo ratings yet
- Presented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Document17 pagesPresented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Akanksha KapoorNo ratings yet
- CEP BPSD Discussion Guide ENG RFCG Updated2019 PDFDocument8 pagesCEP BPSD Discussion Guide ENG RFCG Updated2019 PDFM.DalaniNo ratings yet
- AIMS. Scales-Abnormal-Involuntary-Movement-Scale PDFDocument2 pagesAIMS. Scales-Abnormal-Involuntary-Movement-Scale PDFVictoria RomeroNo ratings yet
- Generic Normal Psychiatric Established-Patient Med CheckDocument2 pagesGeneric Normal Psychiatric Established-Patient Med CheckkeishaNo ratings yet
- Antipsychotic DrugsDocument47 pagesAntipsychotic DrugsIkram UddinNo ratings yet
- My Basal GangliaDocument18 pagesMy Basal GangliaPriya GKNo ratings yet
- Eating Disorders: by Dr. Min Min Phyo 20 August 2019Document74 pagesEating Disorders: by Dr. Min Min Phyo 20 August 2019thu thuNo ratings yet
- Geriatric Giants - DR SeymourDocument108 pagesGeriatric Giants - DR SeymourSharon Mallia100% (1)
- Tension Headaches: What Is A Tension Headache? HighlightsDocument9 pagesTension Headaches: What Is A Tension Headache? HighlightsIndryNo ratings yet
- Notes On J K BaxterDocument4 pagesNotes On J K Baxteraleaf17No ratings yet
- Psychiatry 3rd EditionDocument205 pagesPsychiatry 3rd EditionIva LučićNo ratings yet
- Communication Skills Behavioural Treatment For OCDDocument5 pagesCommunication Skills Behavioural Treatment For OCDTeslim RajiNo ratings yet
- Dual Diagnosis - Clinical and Therapeutic Aspects (Maremmani 03)Document92 pagesDual Diagnosis - Clinical and Therapeutic Aspects (Maremmani 03)antonelloveltriNo ratings yet
- Vascular DementiaDocument57 pagesVascular Dementiadrkadiyala2No ratings yet
- Antipsychotic Deprescribing Algorithm PDFDocument2 pagesAntipsychotic Deprescribing Algorithm PDFFitri Amelia RizkiNo ratings yet
- 2 Af 5 VERTIGODocument35 pages2 Af 5 VERTIGOmuneceNo ratings yet
- AntipsychoticsDocument22 pagesAntipsychoticsvinodksahuNo ratings yet
- Pharmacotherapy of Alzheimers DiseaseDocument69 pagesPharmacotherapy of Alzheimers DiseaseCAROL ANN PATITICONo ratings yet
- Antipsychotic-Induced Extrapyramidal Syndromes andDocument144 pagesAntipsychotic-Induced Extrapyramidal Syndromes andSeiska Mega100% (1)
- Bariatric Surgery BH Grand RoundsDocument39 pagesBariatric Surgery BH Grand Roundsapi-440514424No ratings yet
- PDF VersionDocument6 pagesPDF Versionservicesmi123100% (1)
- Module 3 Biochemistry of The BrainDocument12 pagesModule 3 Biochemistry of The BrainSakshi Jauhari100% (1)
- Mental Health Medications For Children - Fact Sheets - Yale MedicineDocument5 pagesMental Health Medications For Children - Fact Sheets - Yale MedicinewaleskacrzNo ratings yet
- Mental Status ExamDocument1 pageMental Status Examjnyg008No ratings yet
- Stress Management Techniques Evidencebased Procedures That Reduce Stress and Promote Health PDFDocument16 pagesStress Management Techniques Evidencebased Procedures That Reduce Stress and Promote Health PDFMaica MagbitangNo ratings yet
- Basal Ganglia: Sridharan Neelamegan MMCDocument23 pagesBasal Ganglia: Sridharan Neelamegan MMCRetrocasualty Find OutNo ratings yet
- DEPRESSDocument23 pagesDEPRESSWong Chew Nie100% (1)
- Chief ComplaintDocument3 pagesChief Complaintjose acasusoNo ratings yet
- Degenerative Diseases of The Brain 2Document66 pagesDegenerative Diseases of The Brain 2Janie-Vi Villamor Ismael-GorospeNo ratings yet
- Mindfulness MattersDocument9 pagesMindfulness MattersumifNo ratings yet
- Johari WindowDocument10 pagesJohari WindowIra SinghNo ratings yet
- Dementia: Dr. Sharlene Alick OrtizDocument32 pagesDementia: Dr. Sharlene Alick OrtizShary AlickNo ratings yet
- Headache OverviewDocument29 pagesHeadache OverviewFiqna SyaniNo ratings yet
- SchiDocument23 pagesSchiMichelle SatairapanNo ratings yet
- AntideprresentDocument54 pagesAntideprresentHadiqa KhanNo ratings yet
- Eating Disorder Lecture 10Document39 pagesEating Disorder Lecture 10Mawadh AlsbhiNo ratings yet
- Background: Binge EatingDocument15 pagesBackground: Binge EatingCintaAllah Sokmo100% (1)
- Dementia Evaluation and TreatmentDocument12 pagesDementia Evaluation and Treatmentrofi modiNo ratings yet
- Antiepileptics (Autosaved)Document57 pagesAntiepileptics (Autosaved)vishal singhNo ratings yet
- Vertigo & Its ManagementDocument32 pagesVertigo & Its Managementramchandra joshiNo ratings yet
- AlzheimerDocument8 pagesAlzheimerkavithaNo ratings yet
- Lewy Body Dementias Dementia With Lewy Bodies And.9Document29 pagesLewy Body Dementias Dementia With Lewy Bodies And.9Cristina GhizdavetNo ratings yet
- Drug StudyDocument10 pagesDrug StudyRubie Ann TillorNo ratings yet
- Sedative-Hypnotics (SeH) and AnxiolyticsDocument101 pagesSedative-Hypnotics (SeH) and Anxiolyticsmatchees-gone rogueNo ratings yet
- Schizophrenia & Other Psychotic DisordersabpsychDocument12 pagesSchizophrenia & Other Psychotic DisordersabpsychMary HiboNo ratings yet
- Perinatal+Anxiety+and+Depressive+Disorders PPG v3.0Document13 pagesPerinatal+Anxiety+and+Depressive+Disorders PPG v3.0tanmai nooluNo ratings yet
- Legal and Ethical Aspects of Mental Health CareDocument5 pagesLegal and Ethical Aspects of Mental Health CarebrajshekharNo ratings yet
- Ebook OCDDocument22 pagesEbook OCDMagda MoldovanNo ratings yet
- Pandemic Mental - Learn the Secrets to Stay Positive and Improve your Mental Health During this PandemicFrom EverandPandemic Mental - Learn the Secrets to Stay Positive and Improve your Mental Health During this PandemicNo ratings yet
- AuthorsDocument10 pagesAuthorsIftida YatiNo ratings yet
- Efektivitas Edukasi Video Dalam Upaya Pencegahan Diare Pada Anak Kelas 3 Madrasah Hasyim Asyari Pulosari TulungagungDocument11 pagesEfektivitas Edukasi Video Dalam Upaya Pencegahan Diare Pada Anak Kelas 3 Madrasah Hasyim Asyari Pulosari TulungagungIftida YatiNo ratings yet
- 234-Article Text-987-2-10-20221101Document6 pages234-Article Text-987-2-10-20221101Iftida YatiNo ratings yet
- FOI 3647 20bDocument20 pagesFOI 3647 20bIftida YatiNo ratings yet
- Pola Makan Dan Konsumsi Alkohol Sebagai Faktor Risiko Hipertensi Pada LansiaDocument12 pagesPola Makan Dan Konsumsi Alkohol Sebagai Faktor Risiko Hipertensi Pada LansiaIftida YatiNo ratings yet
- Consent - What You Have A Right To Expect: A Guide For ParentsDocument12 pagesConsent - What You Have A Right To Expect: A Guide For Parentshanzierox3825No ratings yet
- Kegawatan Respirasi May2016-FkumyDocument62 pagesKegawatan Respirasi May2016-FkumyAgustina Tri P. DNo ratings yet
- Neurologic Ncle XDocument6 pagesNeurologic Ncle XAngelica Superable Nacion100% (2)
- Canadian Association of General Surgeons Evidence Based Reviews in Surgery. 12Document3 pagesCanadian Association of General Surgeons Evidence Based Reviews in Surgery. 12Javier Vladimir Ramírez BlancoNo ratings yet
- NCM 104: Community Health Nursing (Lecture) : Topic: National Health Programs of The Doh - Family Health ServicesDocument10 pagesNCM 104: Community Health Nursing (Lecture) : Topic: National Health Programs of The Doh - Family Health ServicesChloe TangonanNo ratings yet
- Advanced Dental Documentation ActivitiesDocument2 pagesAdvanced Dental Documentation Activitiesjenea tNo ratings yet
- Productflyer - 978 1 58829 211 7Document1 pageProductflyer - 978 1 58829 211 7Nadya Rahmawati PutriNo ratings yet
- Elfa El Yana (Ne 2)Document6 pagesElfa El Yana (Ne 2)Elfa El YanaNo ratings yet
- Winchester Public School Pediculosis (Head Lice) : Our GoalsDocument2 pagesWinchester Public School Pediculosis (Head Lice) : Our GoalsFebby Indah NurcahyatiNo ratings yet
- Micronutrient Program: PGI Ebarle, Danica PGI Trinidad, Precious BDocument10 pagesMicronutrient Program: PGI Ebarle, Danica PGI Trinidad, Precious BPrecious TrinidadNo ratings yet
- Prostho Prelim LectureDocument12 pagesProstho Prelim LectureChristine LomuntadNo ratings yet
- HealthallergyDocument11 pagesHealthallergyMary Rose QuimanjanNo ratings yet
- Scientific Rationale For Benefits of BreasfteedingDocument7 pagesScientific Rationale For Benefits of BreasfteedingArfian Deny PNo ratings yet
- Introduction of Teaching Strategies For The Middle To Late ChildhoodDocument2 pagesIntroduction of Teaching Strategies For The Middle To Late Childhoodjessa bella materNo ratings yet
- Mommies Act (Lyn18446)Document32 pagesMommies Act (Lyn18446)Senator Cory BookerNo ratings yet
- Bosh Orientation PresentationDocument47 pagesBosh Orientation Presentationsafety officerNo ratings yet
- Subarachno Id Hemorrhag E: DONE BY: Rawan AlebousDocument54 pagesSubarachno Id Hemorrhag E: DONE BY: Rawan AlebousHiba AliNo ratings yet
- Salford Royal NHS Foundation Trust AHP Long Term Placement RequestsDocument4 pagesSalford Royal NHS Foundation Trust AHP Long Term Placement RequestsMD Luthfy LubisNo ratings yet
- Kumpulan Jurnal MedicinusDocument48 pagesKumpulan Jurnal MedicinusFatikhatul BaruniNo ratings yet
- KoledokolitiasisDocument6 pagesKoledokolitiasisnadya nazwinnNo ratings yet
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesNez TraehNo ratings yet
- Kielene Copy: Nararapat Na Maging Bukas Ang Aborsyon para Sa Lahat NG Kababaihan (Panig NG Di Sang-Ayon)Document11 pagesKielene Copy: Nararapat Na Maging Bukas Ang Aborsyon para Sa Lahat NG Kababaihan (Panig NG Di Sang-Ayon)Kielene PalosNo ratings yet
- Journal Reading FixDocument20 pagesJournal Reading FixElsa MayoraNo ratings yet
- CATARACTSDocument2 pagesCATARACTSHanee Kaye TagubaNo ratings yet
- NCM 112 LEC Topic 14 Communicable DiseasesDocument6 pagesNCM 112 LEC Topic 14 Communicable DiseasesViviene Faye FombuenaNo ratings yet
- 2006 Canadian Dementia GuidelinesDocument197 pages2006 Canadian Dementia GuidelinesjamesNo ratings yet
- Hospital Org-ChartDocument1 pageHospital Org-ChartEric OrnaNo ratings yet
- EHS Awareness (EHS Tips For Harmattan Season) - Ghana - Feb W7, 2020Document12 pagesEHS Awareness (EHS Tips For Harmattan Season) - Ghana - Feb W7, 2020JonathanNo ratings yet