Professional Documents
Culture Documents
© Simtipro SRL: Understanding Transfusion-Related Acute Lung Injury (TRALI) and Its Complex Pathophysiology
© Simtipro SRL: Understanding Transfusion-Related Acute Lung Injury (TRALI) and Its Complex Pathophysiology
Uploaded by
Moncef PechaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
© Simtipro SRL: Understanding Transfusion-Related Acute Lung Injury (TRALI) and Its Complex Pathophysiology
© Simtipro SRL: Understanding Transfusion-Related Acute Lung Injury (TRALI) and Its Complex Pathophysiology
Uploaded by
Moncef PechaCopyright:
Available Formats
TRANSFUSION MEDICINE AND Understanding transfusion-related
acute lung injury (TRALI) and its
TRANSFUSION COMPLICATIONS
Editorial complex pathophysiology
Stefan F. van Wonderen1, Robert B. Klanderman2, Alexander P.J. Vlaar1
Two well-executed studies in this issue of Blood Transfusion by Sivakaanthan and
l
Chiaretti and colleagues both arrive at the same conclusion: we still do not know
Sr
Amsterdam UMC Location
1
enough about transfusion-related acute lung injury (TRALI). TRALI is a very serious
University of Amsterdam, complication of blood transfusion and one of the leading causes of transfusion‐related
Department of Intensive Care and morbidity and mortality in developed countries1,2. TRALI has an acute onset (within
Laboratory of Experimental Intensive 6 hours of transfusion) and is characterized by hypoxemia (P/F ≤300 or SpO2 <90% on
O
Care and Anesthesiology, room air), clear evidence of bilateral pulmonary edema on imaging, and the absence of
Amsterdam, the Netherlands;
any evidence of hydrostatic pulmonary edema. First and foremost, TRALI is a clinical
2
Amsterdam UMC Location
PR
diagnosis. While we have come a long way in understanding its pathogenesis, including
University of Amsterdam,
identifying anti-human leukocyte antigen (HLA) or human neutrophil antigen (HNA)
Department of Anesthesiology,
Amsterdam, the Netherlands antibodies, biomarkers can only support the diagnosis, not refute it.
In the study by Sivakaanthan et al., all passively reported TRALI cases in Queensland,
Australia, were analyzed over a 20-year period3. TRALI was a rare occurrence (48
TI
cases; 1/130,000 transfused units) and as expected, a decrease in cases was seen after
implementation of risk-reduction strategies during the study period (i.e., use of male
predominant plasma [2012], plateletpheresis panel of only male donors [2016]). Of all the
M
cases studied, 48% were antibody-mediated TRALI and possible TRALI, with 33% of cases
being non-antibody mediated, which are higher figures than those found in previous
studies4. Other cases were classified as uncategorized TRALI due to the lack of donor
SI
testing to define concordance. Moreover, the percentage of non-antibody-mediated cases
was higher after implementation of male predominant plasma.
This study highlights several interesting points. First, the overall incidence is low; however,
TRALI is notoriously underdiagnosed and under-reported by passive surveillance5-7.
©
This study used the 2004 Canadian Consensus definition for TRALI, identifying cases
as either “TRALI” or “possible TRALI”. Especially cases of “possible TRALI” are under-
recognized, where, in the presence of an underlying condition (such as sepsis or trauma),
post-transfusion pulmonary edema occurs5,6. A redefinition was only introduced in 20198.
In this study, TRALI is subdivided into two groups: TRALI type I (without ARDS risk factor)
and TRALI type II (with an ARDS risk factor or with mild, stable ARDS; Table I). While type
I TRALI remains unchanged in definition, the confusing term “possible TRALI” is no longer
used because it cannot be correctly attributed. In addition, in type II, TRALI can now be
diagnosed in patients that have already experienced an acute worsening of pulmonary
Correspondence: Alexander P.J. Vlaar edema. Implementation of the 2019 TRALI redefinition in future studies will broaden the
e-mail: a.p.vlaar@amsterdamumc.nl
inclusion range, and patients with pre-existing risk factors will no longer be excluded.
Blood Transfus 2022; 20: 443-445 DOI 10.2450/2022.0232-22
© SIMTIPRO Srl
All rights reserved - For personal use only 443
No other use without premission
van Wonderen SF et al
Table I - Revised 2019 consensus redefinition for transfusion-related “two-hit” event threshold model. Alternatively, multiple
acute lung injury
pathways have been found that also support a “one-hit”
Patients who have no risk factors for ARDS and meet the
following criteria
event12,14. In the “two-hit” pathway, the first hit is an
underlying condition such as sepsis or shock, which primes
I. Acute onset
neutrophils in the lungs15. The second hit is caused by
Hypoxemia (P/F-ratio 300 or SpO2 <90% on room
II.
air)
mediators (antibody-mediated [HLA or HNA antibodies] or
A. Clear evidence of bilateral pulmonary edema on
non-antibody-mediated elements [e.g., biological response
TRALI III.
Type I
imaging modifiers, or aged products]) present in the transfusion
No evidence of LAH, or if LAH is present, it is that activate neutrophils, thereby damaging the endothelial
IV. judged to not be the main contributor to the
hypoxemia barrier, resulting in pulmonary edema12,15.
B. Onset during or within 6 hours of transfusion
Anti-HNA-3a is a strong trigger for neutrophil activation.
However, priming of neutrophils was required in vitro
No temporal relationship to an alternative risk
l
C.
factor for ARDS (using lipopolysaccharide [LPS] as the “first hit”) in
Sr
addition to serum containing antibodies (“second hit”).
Patients who have risk factors for ARDS or who have
existing mild ARDS (P/F-ratio of 200-300), and meet the The authors show that addition of serum anti-HNA-3a
following criteria
TRALI
to HNA-3aa homozygous neutrophils and human lung
Findings as described in categories A and B of
Type II A.
TRALI Type I, and
microvascular endothelial cells (HLMVECs) resulted in
O
Stable respiratory status in the 12 hours before endothelial damage. This was not observed, however,
B.
transfusion in HNA-3ab heterozygous or HNA-3bb homozygous
neutrophils. Patients with non-compatible genotypes
Adapted from Vlaar et al., Transfusion, 20198.
PR
ARDS: acute respiratory distress syndrome; LAH: left-atrial hypertension;
P/F-ratio: PaO2/FiO2-ratio. (HNA-3ab or HNA-3bb) might be at lower risk of
anti-HNA-3a-mediated TRALI compared to homozygous
While mitigation strategies can reduce the incidence patients13. Although we still do not know enough about
of antibody-mediated TRALI, in this study, the TRALI, this study may explain some of the variation in
TI
proportion of non-antibody-mediated TRALI increased. severity and onset of symptoms in patients.
Non-concordant antibodies were found in 25% of the Due to the significant differences in these sera, further
non-antibody-mediated (possible) TRALI cases, which investigations (e.g., different types [I or II] of HNA-3a
M
emphasizes just how much we still need to learn about TRALI and larger sample sizes) are warranted to
TRALI, while suggesting other pathophysiological understand this type of TRALI. It is important to note that
pathways. One of these mechanisms is reverse TRALI neutrophil activating pathways may not be distinct, and
SI
by which recipient-derived antibodies are hypothesized that multiple pathways overlap or proceed concurrently.
to be responsible for pathogenesis rather than the Besides the viability of HLMVECs, it would be interesting
donor-derived antibodies; first case reports have been to investigate the endothelial barrier function and
recently published9-12. permeability of HLMVEC, for example, by using electrical
©
The second study in this edition of Blood Transfusion, by cell-substrate impedance sensing (ECIS) technique or
Chiaretti and colleagues, investigated the in vitro effects classical Transwell assays, in the presence of anti-HNA3a
of anti-HNA-3a antibodies on human lung endothelium. serum to support previous findings, since anti-HNA-3a
Anti-HNA-3a antibodies are associated with severe TRALI. antibody-mediated TRALI may also be the result of
The severity may be caused by the potency of anti-HNA-3a disrupted VE-cadherin junctions and not only of damaged
antibodies and their strong leukoagglutinating ability 12. endothelial cells14.
In this study, the authors interestingly investigated The increase in non-antibody-mediated TRALI and
patient factors, i.e., the difference in endothelial damage mechanistic genotype studies serve as a reminder that
and endothelial cytotoxicity based on the recipient’s we do not understand all pathways leading to TRALI. A
neutrophil HNA-3 genotype and phenotype13. From recent example of this is solvent/detergent treated pooled
a pathophysiological point of view, TRALI follows a plasma (SDP)-associated TRALI. SDP is in theory safer as
Blood Transfus 2022; 20: 443-445 DOI 10.2450/2022.0232-22
444 All rights reserved - For personal use only
No other use without premission
Understanding TRALI and its complex pathophysiology
it is produced by pooling plasma from multiple donors 6. Peters AL, Van De Weerdt EK, Goudswaard EJ, Binnekade JM, Zwaginga
JJ, Beckers EAM, et al. Reporting transfusion-related acute lung injury by
which dilutes any harmful antibodies below detectable clinical and preclinical disciplines. Blood Transfus 2018; 16: 227-234. doi:
levels16,17. The previous approach which adopted the use 10.2450/2017.0266-16.
7. Wallis JP. Transfusion-related acute lung injury (TRALI)--under-
of male-only plasma had resulted in a 50-75% decrease diagnosed and under-reported. Br J Anaesth 2003; 90: 573-576. doi:
in the incidence of TRALI18-20. However, since the use of 10.1093/bja/aeg101.
8. Vlaar APJ, Toy P, Fung M, Looney MR, Juffermans NP, Bux J, et al.
SDP, years have passed without any documented cases A consensus redefinition of transfusion-related acute lung injury.
of TRALI20,21. Nevertheless, a recent case series, as well Transfusion 2019; 59: 2465-2476. doi: 10.1111/trf.15311.
as a retrospective study which examined the periods 9. De Clippel D, Emonds MP, Compernolle V. Are we underestimating reverse
TRALI? Transfusion 2019; 59: 2788-2793. doi: 10.1111/trf.15431.
both before and after the implementation of SDP, also 10. Jug R, Anani W, Callum J. A possible case of recipient anti-neutrophil
presented cases of TRALI after transfusion of SDP22,23. and anti-human leukocyte antigen antibody-mediated fatal reverse
transfusion-related acute lung injury. Transfusion 2021; 61: 1336-1340.
The work of Sivakaanthan and Chiaretti and colleagues doi: 10.1111/trf.16330.
provides a reminder that: 1) TRALI is still a cause for 11. Bayat B, Nielsen KR, Bein G, Traum A, Burg-Roderfeld M, Sachs UJ.
l
Transfusion of target antigens to preimmunized recipients: a new
concern; 2) it is a life-threatening complication; and 3) mechanism in transfusion-related acute lung injury. Blood Adv 2021; 5:
Sr
3975-3985. doi: 10.1182/bloodadvances.2020003843.
some pathophysiological mechanisms for TRALI still
12. Tung JP, Chiaretti S, Dean MM, Sultana AJ, Reade MC, Fung YL. Transfusion-
remain to be identified. To improve transfusion products related acute lung injury (TRALI): Potential pathways of development,
and develop mitigation strategies for TRALI, we first strategies for prevention and treatment, and future research directions.
Blood Rev 2022; 53: 100926. doi: 10.1016/j.blre.2021.100926.
have to understand alternative pathophysiological 13. Chiaretti S, Burton M, Hassel P, Radenkovic F, Devikashri N, Sultana AJ, et
O
pathways, for example, the inf luence of neutrophil al. Human neutrophil antigen 3 genotype impacts neutrophil-mediated
endothelial cell cytotoxicity in a two-event model of TRALI. Blood
HNA-3 genotype and phenotype, SDP TRALI, reverse Transfus 2022; 20: 465-474. doi: 10.2450/2022.0013-22.
TRALI, lipid mediators, and donor-related factors.
PR 14. Bayat B, Tjahjono Y, Sydykov A, Werth S, Hippenstiel S, Weissmann N,
et al. Anti-human neutrophil antigen-3a induced transfusion-related
To better study these mechanisms, we remain reliant acute lung injury in mice by direct disturbance of lung endothelial
on vigilant clinicians to report cases, as well as the cells. Arterioscler Thromb Vasc Biol 2013; 33: 2538-2548. doi: 10.1161/
ATVBAHA.113.301206.
hemovigilance surveillance systems. Adopting the 2019 15. Silliman CC. The two-event model of transfusion-related acute lung
redefinition will allow patients to be pooled thereby injury. Crit Care Med 2006; 34 (Suppl 5): S124-131. doi: 10.1097/01.
TI
CCM.0000214292.62276.8E.
advancing research ef forts. We hope to see the study 16. Sachs UJ, Kauschat D, Bein G. White blood cell-reactive antibodies are
of large international cohorts to further investigate the undetectable in solvent/detergent plasma. Transfusion 2005; 45: 1628-
1631. doi: 10.1111/j.1537-2995.2005.00587.x.
pathophysiological mechanisms of TRALI and promote 17. Marietta M, Franchini M, Bindi ML, Picardi F, Ruggeri M, De Silvestro G. Is
M
its prevention. solvent/detergent plasma better than standard fresh-frozen plasma? A
systematic review and an expert consensus document. Blood Transfus
2016; 14: 277-286. doi: 10.2450/2016.0168-15.
The Authors declare no conf licts of interest. 18. Eder AF, Herron RM Jr., Strupp A, Dy B, White J, Notari EP, et al. Effective
SI
reduction of transfusion-related acute lung injury risk with male-
predominant plasma strategy in the American Red Cross (2006-2008).
Transfusion 2010; 50: 1732-1742. doi: 10.1111/j.1537-2995.2010.02652.x.
REFERENCES 19. Schmickl CN, Mastrobuoni S, Filippidis FT, Shah S, Radic J, Murad MH,
1. Stainsby D, Jones H, Asher D, Atterbury C, Boncinelli A, Brant L, et al. et al. Male-predominant plasma transfusion strategy for preventing
Serious hazards of transfusion: a decade of hemovigilance in the UK. transfusion-related acute lung injury: a systematic review. Crit Care Med
©
Transfus Med Rev 2006; 20: 273-282. doi: 10.1016/j.tmrv.2006.05.002. 2015; 43: 205-225. doi: 10.1097/CCM.0000000000000675.
2. Food and Drug Administration. Fatalities Reported to FDA Following 20. Saadah NH, van Hout FMA, Schipperus MR, le Cessie S, Middelburg RA,
Blood Collection and Transfusion Annual Summary for FY2019. Available Wiersum-Osselton JC, et al. Comparing transfusion reaction rates for
online: https://www.fda.gov/media/147628/download. Accessed on various plasma types: a systematic review and meta-analysis/regression.
28/03/2022. Transfusion 2017; 57: 2104-2114. doi: 10.1111/trf.14245.
3. Sivakaanthan A, Swain F, Pahn G, Goodison K, Gutta N, Holdsworth R, et 21. Hellstern P, Solheim BG. The use of solvent/detergent treatment in
al. Transfusion-related acute lung injury (TRALI): a retrospective review of pathogen reduction of plasma. Transfus Med Hemother 2011;38: 65-70.
reported cases in Queensland, Australia over 20 years. Blood Transfus 2022; doi: 10.1159/000323552.
20: 454-464. doi: 10.2450/2022.0020-22. 22. Klanderman RB, van Mourik N, Eggermont D, Peters AL, Tuinman PR,
4. van Stein D, Beckers EA, Sintnicolaas K, Porcelijn L, Danovic F, Bosman R, et al. Incidence of transfusion-related acute lung injury
Wollersheim JA, et al. Transfusion-related acute lung injury reports in the temporally associated with solvent/detergent plasma use in the ICU: A
Netherlands: an observational study. Transfusion 2010; 50: 213-220. doi: retrospective before and after implementation study. Transfusion 2022;
10.1111/j.1537-2995.2009.02345.x. 62: 1752-1762. doi: 10.1111/trf.17049.
5. Vlaar AP, Wortel K, Binnekade JM, van Oers MH, Beckers E, Gajic O, et 23. Klanderman RB, Bulle EB, Heijnen JWM, Allen J, Purmer IM, Kerkhoffs
al. The practice of reporting transfusion-related acute lung injury: a JH, et al. Reported transfusion-related acute lung injury associated with
national survey among clinical and preclinical disciplines. Transfusion solvent/detergent plasma - A case series. Transfusion 2022; 62: 594-599.
2010; 50: 443-451. doi: 10.1111/j.1537-2995.2009.02415.x. doi: 10.1111/trf.16822.
Blood Transfus 2022; 20: 443-445 DOI 10.2450/2022.0232-22
All rights reserved - For personal use only 445
No other use without premission
You might also like
- 1 s2.0 S0140673622014854 MainDocument12 pages1 s2.0 S0140673622014854 Mainsilvia100% (1)
- Review: Alexander P J Vlaar, Nicole P Juff ErmansDocument11 pagesReview: Alexander P J Vlaar, Nicole P Juff ErmanssinarNo ratings yet
- Transfusion-Related Acute Lung Injury: Review ArticleDocument9 pagesTransfusion-Related Acute Lung Injury: Review ArticleAinunNadzirohNo ratings yet
- Committeereport: A Consensus Rede Finition of Transfusion-Related Acute Lung InjuryDocument12 pagesCommitteereport: A Consensus Rede Finition of Transfusion-Related Acute Lung InjuryAdrian ArnasaputraNo ratings yet
- Transfusion-Related Acute Lung Injury Risk Mitigation: An UpdateDocument10 pagesTransfusion-Related Acute Lung Injury Risk Mitigation: An UpdateAlfa FebriandaNo ratings yet
- Dilemma in PEDocument7 pagesDilemma in PEGosia JasiewiczNo ratings yet
- Transfusion-Associated Circulatory Overload and Transfusion-Related Acute Lung InjuryDocument14 pagesTransfusion-Associated Circulatory Overload and Transfusion-Related Acute Lung InjuryKaemacCrackercherryzebraNo ratings yet
- (TRALI) Cudilo2015Document4 pages(TRALI) Cudilo2015abu abdirrahmanNo ratings yet
- Transfusion-Related Acute Lung Injury and TransfusDocument4 pagesTransfusion-Related Acute Lung Injury and TransfusShanaz NovriandinaNo ratings yet
- Seminar: Nuala J Meyer, Luciano Gattinoni, Carolyn S CalfeeDocument16 pagesSeminar: Nuala J Meyer, Luciano Gattinoni, Carolyn S CalfeeDiana AngelesNo ratings yet
- Trali Uptodate PDFDocument36 pagesTrali Uptodate PDFTety M. DorisNo ratings yet
- Transfusion-Related Acute Lung Injury (Trali) : Description and IncidenceDocument9 pagesTransfusion-Related Acute Lung Injury (Trali) : Description and IncidenceNanda SilvaNo ratings yet
- TraliDocument10 pagesTraliMatilde Silva GonçalvesNo ratings yet
- Transfusion-Related Acute Lung Injury: HistoryDocument20 pagesTransfusion-Related Acute Lung Injury: HistoryBladimir CentenoNo ratings yet
- Distinguishing TRALI and TACODocument6 pagesDistinguishing TRALI and TACOl1o2stNo ratings yet
- Transfusion-Related Acute Lung Injury: A Literature Review: ReviewarticleDocument9 pagesTransfusion-Related Acute Lung Injury: A Literature Review: ReviewarticlekereklovagNo ratings yet
- Subphenotyping ARDS in COVID-19 Patients: Consequences For Ventilator ManagementDocument10 pagesSubphenotyping ARDS in COVID-19 Patients: Consequences For Ventilator ManagementPaola Andrade ValenciaNo ratings yet
- Juffermans Et Al-2020-Intensive Care MedicineDocument8 pagesJuffermans Et Al-2020-Intensive Care MedicineHalonzo RománNo ratings yet
- Chen 2015Document6 pagesChen 2015nurminsyahNo ratings yet
- 4Document16 pages4Ihsanul Ma'arifNo ratings yet
- Transfusion-Related Acute Lung Injury - StatPearls - NCBI BookshelfDocument5 pagesTransfusion-Related Acute Lung Injury - StatPearls - NCBI Bookshelfindahmsafitri3No ratings yet
- Alveolar HaemorragicDocument12 pagesAlveolar Haemorragicmedicina146No ratings yet
- Z. Citasi Piis014067362030917xDocument3 pagesZ. Citasi Piis014067362030917xMastifa HanasitaNo ratings yet
- © Simtipro SRLDocument11 pages© Simtipro SRLMoncef PechaNo ratings yet
- Transfusion-Related Acute Lung Injury: Pearl Toy,, and Ognjen GajicDocument2 pagesTransfusion-Related Acute Lung Injury: Pearl Toy,, and Ognjen GajicMaulana Akbar LubisNo ratings yet
- TRALI Review 2009 PDFDocument11 pagesTRALI Review 2009 PDFTitin AliyaturNo ratings yet
- Risk Factors For Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewDocument11 pagesRisk Factors For Community-Acquired Pneumonia in Adults in Europe: A Literature ReviewKorwin TitlaNo ratings yet
- Sdra Reconocimiento Actual 2021Document16 pagesSdra Reconocimiento Actual 2021NATHALY JOVANA CONTRERAS HERRERANo ratings yet
- Articulo Trombocitipenia Por Vacuna CovidDocument10 pagesArticulo Trombocitipenia Por Vacuna CovidAlex de la RNo ratings yet
- From Gold 0 To Pre-CopdDocument10 pagesFrom Gold 0 To Pre-CopdLorena ZirondiNo ratings yet
- Acute Respiratory Distress Syndrome 2021 LancetDocument16 pagesAcute Respiratory Distress Syndrome 2021 LancetCláudia SilvaNo ratings yet
- Connective Tissue Disease-Associated Interstitial Lung Diseases: Unresolved IssuesDocument9 pagesConnective Tissue Disease-Associated Interstitial Lung Diseases: Unresolved IssuesNuntana ChampaNo ratings yet
- Int Care Med 2007Document5 pagesInt Care Med 2007sccNo ratings yet
- Chronic Airspace DiseasesDocument31 pagesChronic Airspace DiseasesAnkita ShahNo ratings yet
- Wu 2021Document8 pagesWu 2021Pulmonologi Dan Kedokteran Respirasi FK UNRINo ratings yet
- Review: Paolo Spagnolo, Giulio Rossi, Rocco Trisolini, Nicola Sverzellati, Robert P Baughman, Athol U WellsDocument14 pagesReview: Paolo Spagnolo, Giulio Rossi, Rocco Trisolini, Nicola Sverzellati, Robert P Baughman, Athol U Wellsandra mNo ratings yet
- 11 Acute Respiratory Distress Syndrome NEJM Thompson2017Document11 pages11 Acute Respiratory Distress Syndrome NEJM Thompson2017Camila Andrea PeñaNo ratings yet
- Anticoagulation in COVID-19: A Systematic Review, Meta-Analysis, and Rapid Guidance From Mayo ClinicDocument20 pagesAnticoagulation in COVID-19: A Systematic Review, Meta-Analysis, and Rapid Guidance From Mayo ClinicAndi Tiara S. AdamNo ratings yet
- Interstitial Pneumonia With Autoimmune Features Challenges and ControversieDocument19 pagesInterstitial Pneumonia With Autoimmune Features Challenges and ControversieVitória WasserNo ratings yet
- Analisis Comparativo Ipaf Vs EasDocument9 pagesAnalisis Comparativo Ipaf Vs Easpkh5qpp8j5No ratings yet
- Algoritma ARDSDocument7 pagesAlgoritma ARDSSri AgustinaNo ratings yet
- Accepted Manuscript: 10.1016/j.chest.2016.02.635Document21 pagesAccepted Manuscript: 10.1016/j.chest.2016.02.635Vic HNNo ratings yet
- Chronic Interstitial Lung Diseases in Children: Diagnosis ApproachesDocument30 pagesChronic Interstitial Lung Diseases in Children: Diagnosis Approachesgustavo adolfo rodriguez alzateNo ratings yet
- Copd 1Document8 pagesCopd 1Meinita M.DNo ratings yet
- PIIS1076633220302464Document1 pagePIIS1076633220302464India SunshineNo ratings yet
- Transfusion-Associated Circulatory Overload and Transfusion-Related Acute Lung InjuryDocument14 pagesTransfusion-Associated Circulatory Overload and Transfusion-Related Acute Lung InjuryGloria ThomasNo ratings yet
- Interpretación de Patrones Radiológicos Sugerentes de Covid-19 en PediatríaDocument9 pagesInterpretación de Patrones Radiológicos Sugerentes de Covid-19 en PediatríaJuan M SagnirbNo ratings yet
- Correspondence: Smell and Taste Dysfunction in Patients With COVID-19Document1 pageCorrespondence: Smell and Taste Dysfunction in Patients With COVID-19Dhyo Asy-shidiq HasNo ratings yet
- ISTH Interim Guidance On Recognition and Management of Coagulopathy in COVID-19Document8 pagesISTH Interim Guidance On Recognition and Management of Coagulopathy in COVID-19hellonduttyNo ratings yet
- 1 s2.0 S0140673622014398 MainDocument14 pages1 s2.0 S0140673622014398 Maintaaaatan.04No ratings yet
- A Case Series Describing The Epidemiology and Clinical Characteristics of COVID-19 Infection in Jilin ProvinceDocument4 pagesA Case Series Describing The Epidemiology and Clinical Characteristics of COVID-19 Infection in Jilin Provinceabeer alrofaeyNo ratings yet
- HHS Public Access: SyphilisDocument49 pagesHHS Public Access: Syphilisfaty basalamahNo ratings yet
- JMV 25815Document2 pagesJMV 25815fadil ahmadiNo ratings yet
- Reaksi Transfusi, TRALI Vs TACODocument12 pagesReaksi Transfusi, TRALI Vs TACOifadhrohayatNo ratings yet
- Pulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of LiteratureDocument5 pagesPulmonary Tuberculosis Presenting With Acute Respiratory Distress Syndrome (Ards) : A Case Report and Review of Literatureamelya asryNo ratings yet
- Complicatii PneumonieDocument9 pagesComplicatii PneumonieTatiana JalbaNo ratings yet
- Pathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Document5 pagesPathological Evidence of Pulmonary Thrombotic Phenomena in Severe COVID 19Victor AugustoNo ratings yet
- Acute Respiratory Distress Syndrome: Etiology, Pathogenesis, and Summary On ManagementDocument15 pagesAcute Respiratory Distress Syndrome: Etiology, Pathogenesis, and Summary On ManagementLiri AndiyaniNo ratings yet
- (PULMO) 2012 ARDS - The New Berlin DefinitionDocument4 pages(PULMO) 2012 ARDS - The New Berlin DefinitionerikaNo ratings yet
- J Jaad 2008 12 046Document3 pagesJ Jaad 2008 12 046Moncef PechaNo ratings yet
- Life History of Cutaneous Vascular Lesions in Sneddon's SyndromeDocument8 pagesLife History of Cutaneous Vascular Lesions in Sneddon's SyndromeMoncef PechaNo ratings yet
- J Ekir 2020 12 039Document8 pagesJ Ekir 2020 12 039Moncef PechaNo ratings yet
- Soares Et Al 2016 Prognosis of Critically Ill Patients With Cancer and Acute Renal DysfunctionDocument14 pagesSoares Et Al 2016 Prognosis of Critically Ill Patients With Cancer and Acute Renal DysfunctionMoncef PechaNo ratings yet
- © Simtipro SRLDocument8 pages© Simtipro SRLMoncef PechaNo ratings yet
- © Simtipro SRLDocument11 pages© Simtipro SRLMoncef PechaNo ratings yet
- © Simtipro SRLDocument8 pages© Simtipro SRLMoncef PechaNo ratings yet
- 150QCM EmbryologieDocument66 pages150QCM EmbryologieMoncef PechaNo ratings yet
- © Simtipro SRL: A New Blood Group System: Scientific Relevance and Media ResonanceDocument2 pages© Simtipro SRL: A New Blood Group System: Scientific Relevance and Media ResonanceMoncef PechaNo ratings yet
- General Transfusion Practice Quiz For Rotating Medical StaffDocument3 pagesGeneral Transfusion Practice Quiz For Rotating Medical StaffaymenNo ratings yet
- HematologyDocument8 pagesHematologySameera Al MerriNo ratings yet
- Medical Devices: Selection of Tests For Interactions With Blood 10993-4Document10 pagesMedical Devices: Selection of Tests For Interactions With Blood 10993-4Muhammad ImranNo ratings yet
- Anemia Defisiensi Besi Pada Pasien Dengan Ulkus Peptikum: Laporan KasusDocument4 pagesAnemia Defisiensi Besi Pada Pasien Dengan Ulkus Peptikum: Laporan KasusAzura SyahadatiNo ratings yet
- Aragon, Annie Lynn Silverio 2487019192Document5 pagesAragon, Annie Lynn Silverio 2487019192Samuel AragonNo ratings yet
- Blood Bank International Standard ISBT Science Series - 2008 - Hardwick - Blood ProcessingDocument29 pagesBlood Bank International Standard ISBT Science Series - 2008 - Hardwick - Blood ProcessingShan AhmadNo ratings yet
- Management TTPDocument14 pagesManagement TTPSutirtho MukherjiNo ratings yet
- HematDocument3 pagesHematMohit AbhyankarNo ratings yet
- The Study On The Anti - Anemic Effect of Banana Peel Extract Against Gentamicin - Induced Anemic Male Albino RATS (Rattus Norvegicus)Document32 pagesThe Study On The Anti - Anemic Effect of Banana Peel Extract Against Gentamicin - Induced Anemic Male Albino RATS (Rattus Norvegicus)Maraiah BautistaNo ratings yet
- An Introduction To Haematopoiesis Prof Vernon Louw Clinical Haematology University of Cape TownDocument35 pagesAn Introduction To Haematopoiesis Prof Vernon Louw Clinical Haematology University of Cape TownAmmaarah IsaacsNo ratings yet
- Isaac Typhoid NegativeDocument5 pagesIsaac Typhoid Negativeganesh khondeNo ratings yet
- Shalamar Hospital Laboratory: LLFFLLLLLLLLLLLLLLLLLLDocument1 pageShalamar Hospital Laboratory: LLFFLLLLLLLLLLLLLLLLLLAfaq MehmoodNo ratings yet
- Complete Blood Count (CBC) Normal Laboratory Study Values: DefinitionDocument6 pagesComplete Blood Count (CBC) Normal Laboratory Study Values: DefinitionGlare RhayneNo ratings yet
- The Child With Hematologic DisordersDocument149 pagesThe Child With Hematologic DisordersNics FranciscoNo ratings yet
- Blood Bank PracticalDocument24 pagesBlood Bank Practicalmoonfire2009No ratings yet
- Adobe Scan 09 Jan 2024Document2 pagesAdobe Scan 09 Jan 2024swapna vijayNo ratings yet
- Blood Donation Research Paper - LatestDocument10 pagesBlood Donation Research Paper - LatestEileen1113100% (2)
- Laboratory Report: Consultant PathologistDocument2 pagesLaboratory Report: Consultant Pathologisttafiki4253No ratings yet
- HPLC Vs HB ElectrophoresisDocument10 pagesHPLC Vs HB ElectrophoresisRajeev Rajeshuni100% (1)
- Heparin MedicationDocument1 pageHeparin Medicationtriagestation100% (2)
- (Blood Group) Department of Public Health Fall 2020, Lab Manual (PBH101L)Document2 pages(Blood Group) Department of Public Health Fall 2020, Lab Manual (PBH101L)MunniNo ratings yet
- Hemograma Buna 2023 BunaDocument71 pagesHemograma Buna 2023 BunaMirelDabuleanuNo ratings yet
- Hemoglobinopathy - WikipediaDocument9 pagesHemoglobinopathy - WikipediaEslam NassarNo ratings yet
- Case Study ON: Blood DyscrasiaDocument40 pagesCase Study ON: Blood DyscrasiaJM RomiasNo ratings yet
- COMPLETE BLOOD COUNT Lecture GuideDocument9 pagesCOMPLETE BLOOD COUNT Lecture GuideKaycee Gretz LorescaNo ratings yet
- Differential Diagnosis of Microcytic Anemia PDFDocument5 pagesDifferential Diagnosis of Microcytic Anemia PDFayms99No ratings yet
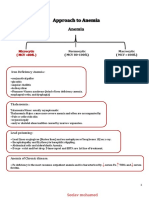
- Approach To AnemiaDocument4 pagesApproach To AnemiapNo ratings yet
- Presentation On AnaemiaDocument19 pagesPresentation On AnaemiaAnkit MalikNo ratings yet
- Sysmex SEED The Importance of Reticulocyte Detection PDFDocument8 pagesSysmex SEED The Importance of Reticulocyte Detection PDFRaluca BadeaNo ratings yet
- Vitamin B12 Deficiency and Anemia in 140 Taiwanese Female Lacto-VegetariansDocument13 pagesVitamin B12 Deficiency and Anemia in 140 Taiwanese Female Lacto-VegetariansLunaNo ratings yet