Professional Documents
Culture Documents
A To Z of Relex Smile: All You Need To Know: Review Article
A To Z of Relex Smile: All You Need To Know: Review Article
Uploaded by
StefanOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A To Z of Relex Smile: All You Need To Know: Review Article
A To Z of Relex Smile: All You Need To Know: Review Article
Uploaded by
StefanCopyright:
Available Formats
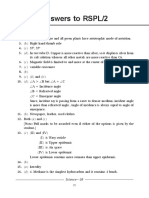
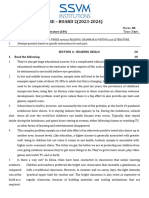
DJO Vol. 32, No.
1, July-September 2021
Review Article
A to Z of ReLEx SMILE: All you need to know
Sanjana Vatsa, Pallavi Dhawan, Shana Sood
Department of Cornea and Refractive Services, Dr. Agarwal’s Eye Hospital, Bangalore, India.
ReLEx SMILE (Refractive lenticule exchange - Small incision lenticule extraction) is a new generation of laser vision
correction, performed using the Visumax femtosecond laser system (Carl Zeiss Meditec AG, Jena, Germany) for
the correction of myopia and myopic astigmatism. It ensures greater biomechanical stability, lesser chances of dry
eyes and predictable visual and refractive outcomes, making it the procedure of choice for myopic corrections. This
article explains in detail regarding the pre-operative work up, steps of the surgical procedure, laser parameters,
Abstract intra-operative complications such as suction loss, opaque bubble layer, dark spots, cap tear, lenticular adhesion
and post-operative complications such as interface haze, interface debris, diffuse lamellar keratitis etc. and their
management. The learning curve of SMILE being steeper than that of LASIK, well experienced surgeon and a well
co-operative patient would ensure better surgical outcomes, minimising the complications. It also briefly explains
about the options available for enhancement post SMILE.
Delhi J Ophthalmol 2021;32; 25-31; Doi http://dx.doi.org/10.7869/djo.683
Keywords: SMILE, Laser Refractive Procedure, Femtosecond Laser, Visumax, Myopia.
Introduction Pre Operative Counselling
The first report of refractive intrastromal lenticule extraction Patient is adequately counselled about the procedure and
was published in 1996 with the use of picosecond (10-12) an informed consent is taken. Topical anaesthetic drops
lasers.1 Femtosecond laser assisted refractive lenticule (proparacaine 0.5%) are instilled to both the eyes. Excessive
extraction procedure using the Intralase machine (Abott use of topical anaesthetic is avoided as it may loosen the
Medicals Optics, USA) was published years later in 2003.2 epithelium and in-turn affect the femtosecond laser delivery
Femtosecond laser offers a unique edge over other lasers resulting in black spots and thus difficult dissection.
as it has better precision and less collateral damage. This
technique was perfected and the VisuMax femtosecond Surgical Procedure
laser system (Carl Zeiss Meditec AG, Jena, Germany) was It involves 4 important steps - Docking, femtosecond laser
developed, which delivers fixed patterns of femtosecond delivery, lenticule dissection and lenticule extraction.
laser pulses to create an intrastromal refractive lenticule at
a particular depth along with side cuts at desired positions a. Docking
and works by the principle of photo-disruption. The patient is made to lie down supine on the operating
table. The docking cone is attached to the femtosecond
SMILE (Small Incision Lenticule Extraction) is the most laser delivery system. Selection of the cone depends on
advanced refractive surgery for the correction of myopia the corneal white-to-white diameter (Figure 1, 2). The eye
and myopic astigmatism, with a high level of safety,
efficacy and precision.Unlike LASIK, SMILE is a bladeless
procedure with a small incision of 2-4mm, with lesser
incidence of symptomatic dry eyes post surgery because
of better preservation of corneal innervation.3,4,5 Due to the
pattern of arrangement of the corneal lamellae, a vertical cut
causes more loss of tensile strength than a parallel cut. The
vertical cut in LASIK is almost 270 degrees, while the side
cut in SMILE is only 40 degrees causing lesser disturbance
of corneal biomechanics and thereby providing better
biomechanical stability.6,7
Pre Operative Evaluation
• Uncorrected distance visual acuity (UCVA), corrected Figure 1: Suction cone
distance visual acuity (CDVA) and vision with pinhole
• Manifest and cycloplegic refraction
• Intraocular pressure measurement by Non contact
tonometry
• Slit lamp biomicroscopy
• Dilated fundus examination
• Dry eye assessment (Schirmer's I and II)
• Topography with Pentacam
• Aberrometry
• Specular microscopy
• Anterior segment OCT (if available) Figure 2: Under surface of the Suction cone
E-ISSN: 2454-2784 P-ISSN: 0972-0200 25 Delhi Journal of Ophthalmology
DJO Vol. 32, No. 1, July-September 2021
to be operated is positioned under the cone and patient is
asked to fixate on the green blinking light (Figure 3). The
bed is moved up till the curved contact glass interface
applanates the corneal surface (Figure 4). Excess saline in the
conjunctival sac is removed. Once the contact lens touches
the cornea, a meniscus tear film appears and the fixation
light becomes clearly visible to the patient. Care is taken to
make sure that it is purely a corneal suction and that there
is no conjunctival tissue prolapse into the cone. The patient
is asked to focus on the green light and suction is activated
Figure 5: Suction bar indicating the level of suction
Figure 3: Fixation light
Figure 6: Stage of lenticule creation
Figure 4: Docking
(Figure 5). The treatment is centred on the coaxial corneal
light reflex (CCLR) and the centration is confirmed using Figure 7: Completion of lenticule side cut and beginning of cap formation
the infrared light. The suction achieved is gentle and the
maximum suction pressure generated by the VisuMax laser
system is approximately 30-35 mmHg.8 In cases where there
is significant preoperative astigmatism (>0.75D), manual
compensation for cyclotorsion may be performed by gently
rotating the cone after activation of suction and aligning it to
0°-180° axis.9
b. Femtosecond Laser Delivery
The VisuMax laser system delivers femtosecond laser pulses
at a wavelength of 1,043 nm and frequency of 500 kHz to
create an intrastromal refractive lenticule.8 The posterior
surface of the lenticule is created first in a spiral in fashion
followed by the creation of side-cut and then the anterior cap
creation occurs in a spiral out fashion. Finally a 2 – 4 mm Figure 8: Completion of anterior cap formation
incision is created superiorly.10 (Figure. 6, 7, 8, 9)
E-ISSN: 2454-2784 P-ISSN: 0972-0200 26 www.djo.org.in
DJO Vol. 32, No. 1, July-September 2021
Figure 9: Incision creation Figure 10: Delineation of the anterior plane
Conventionally, the treatment parameters are set at an
anterior cap depth of 120 µm (range 100–160 µm) and
minimum lenticule thickness at edge of 15 µm (ranging from
10– 30µm), optical zone ranging from 6.0 – 7.0 mm with no
transition zone for spherical errors and 0.10 mm transition
zone for astigmatism. The cap diameter is set to 1 mm larger
than the lenticule diameter. The pulse energy is set between
100 and 160 nJ. Total suction time is approximately 25–35
seconds (depending on the mode used). Laser parameters
in various treatment modes are as shown in the table below
(Table 1).11
Table 1: Laser Parameters In Various Treatment Modes
Laser Expert Mode Standard Mode Fast Mode Figure 11: Delineation of the posterior plane
Parameters
Pulse energy 140–200 nJ 130 nJ 170 nJ
Energy 28–40 26 34
offset(1 offset
= 5 nJ)
Track Lenticule Lenticule and Lenticule and
distance (µm) and cap: 4.50 cap: 3.00 cap: 4.50
Lenticule Lenticule side Lenticule and
side and cap and cap side cut: cap side cuts:
side cut: 2.00 2.00 2.00
Spot distance Lenticule Lenticule and Lenticule and
(µm) and cap: 4.50 cap: 3.00 cap: 4.50
Lenticule Lenticule side Lenticule side
side and cap and cap side cut: and cap side Figure 12: Gas bubble escape sign
side cut: 2.00 2.00 cut: 2.00
c. Lenticule Dissection
The incision is opened and the edge of the lenticule is
identified by delineating the anterior and posterior planes
(Figure.10, 11). The anterior lenticular plane is separated from
the overlying cap by blunt lamellar dissection, followed by
the posterior plane dissection. A small peripheral area is left
un-dissected till the end to provide counter-traction during
posterior plane dissection and to prevent the lenticule from
folding on to one side.
Gas Bubble Escape Sign (GBE)
The GBE sign refers to the escape of gas bubbles on
delineation of the lenticular planes, followed by an
immediate improvement in the clarity of the interface Figure 13: Before the escape of gas bubbles
(Figure 12, 13, 14). A study by Ganesh et al. showed that GBE
sign indicates an optimized laser energy pattern, which may
E-ISSN: 2454-2784 P-ISSN: 0972-0200 27 Delhi Journal of Ophthalmology
DJO Vol. 32, No. 1, July-September 2021
Intraoperative Complications
1. Suction Loss
Risk factors: Deep set eyes, narrow palpebral fissure,
excessive eyelid squeezing, flat keratometric power, loose
corneal epithelium, excessive reflex tearing, patient’s
inability to maintain fixation or follow instructions.17,18
Patient should be well counselled pre-operatively to fixate
on the green light and avoid any eye movements or head
movements. A self-retaining speculum should be inserted to
ensure adequate exposure. Excess fluid in the conjunctival
sac should be cleared before docking. The presence of a fluid
meniscus in the periphery after docking is a sign of imminent
Figure 14: Increase in the clarity of the interface after the escape of gas suction loss and it is advisable to release the suction and re-
bubbles dock in such cases to prevent intra-operative complications.
The management of suction loss depends on the stage at
which it occurs. If it occurs at the stage where more than
10% of lenticule has been formed, SMILE procedure is
abandoned and is converted to LASIK. However, at all other
stages re-docking can be done and can proceed with SMILE
by reducing the lenticule diameter and cap diameter by 0.2-
0.4mm.
2. Vertical Gas Breakthrough
This may occur if there is a focal break or a scar in the
bowman’s layer and in cases of epithelial basement membrane
dystrophy.19,20 Gas bubbles created during cap/ lenticule
creation can track through anterior corneal scars onto the
surface of cornea. These bubbles can block the successive
laser pulses leading to incomplete lenticule creation in the
Figure 15: Extraction of separated lenticule using lenticule forceps
area of gas bubble and thus causing difficult dissection
intra-operatively and can also lead to the formation of a
ease the lenticular dissection and thus provide better quality buttonhole which can cause post-operative complications
of vision in the immediate post-operative period.12 such as epithelial in-growth and scarring.21 Surface ablative
procedures can be considered for the correction of refractive
d. Lenticule Extraction error at a later date after ensuring complete healing of the
After making sure that the lenticule is well separated and is buttonhole.22
free from all sides, it is extracted through the small incision
using a microforceps. After extraction, the lenticule is spread 3. Opaque Bubble Layer (OBL)
out over the surface of the cornea and is examined for its OBL is formed when excess of gas and water bubbles get
completeness (Figure 15) trapped between the stromal lamellae, unable to pass
uniformly through the lamellar interface, which in turn
Currently, ReLEx SMILE corrects myopia of up to −10.00 D, makes the lenticular dissection difficult (Figure 16). It can
myopic astigmatism up to −5.00 D and a spherical equivalent
(SE) of up to −12.5 D.13,14
Visual Recovery After Smile
Although visual outcomes have been good after SMILE,
visual recovery is relatively slower compared to LASIK. The
backscattered light intensity is seen to be higher in SMILE
due to the activated keratocytes, extracellular matrix and
irregularity of the interface which may be attributed to the
slower visual recovery.15
Post-Operative Dryness
Reinstein et al. found that corneal sensation was reduced in
the early postoperative period after SMILE, but recovered to
baseline in 89% of the eyes by 6 months.16
Figure 16: Opaque bubble layers (OBL)
E-ISSN: 2454-2784 P-ISSN: 0972-0200 28 www.djo.org.in
DJO Vol. 32, No. 1, July-September 2021
Figure 17 : Dark spots Figure 19 : Epithelial defect near the incision site
Figure 18 : Dark spots Figure 20 : Cap tear
be observed in cases with too high or too low laser energy
settings. Risk factors include thicker corneas and older
patients with denser peripheral collagen that prevent the
escape of gas bubbles.23
4. Dark Spots
Debris/meibomian secretions entrapped between the contact
glass and the cornea causes incomplete laser delivery in that
area resulting in the formation of dark spots and subsequent
difficult dissection. (Figure 17, 18) Care should be taken to
dissect the area gently to prevent lenticular tear.
5. Cap Lenticular Adhesion
It results from an inadvertent dissection of the posterior Figure 21: Lenticule tear during extraction
lenticular plane before separating the anterior surface
19). This can be prevented by limiting the use of anaesthetic
from the overlying cap. Care should be taken to carefully
drops. A bandage contact lens is placed postoperatively till
delineate the anterior plane and dissect it completely to
the epithelium heals.25
ensure complete separation of the cap from the underlying
lenticule. Improper management of cap lenticular adhesion
7. Cap Tear
can lead to suboptimal visual outcomes with an increased
Cap tear can occur in the hands of an in-experienced surgeon,
incidence of cap tears, side-cut tears, retained lenticular
due to micro-adhesions and/or excessive intra-operative
fragments and iatrogenic damage to the corneal stroma.24
manipulation (Figure 20). Small tears usually heal well,
whereas larger tears extending upto the visual axis can affect
6. Epithelial Defects
visual outcomes. It is advisable to place a bandage contact
Excessive use of topical anaesthetic drops can cause
lens until the tear heals, in addition to frequent lubrication.
iatrogenic loosening of the epithelium, which in-turn can
cause epithelial defect during lenticule dissection (Figure
E-ISSN: 2454-2784 P-ISSN: 0972-0200 29 Delhi Journal of Ophthalmology
DJO Vol. 32, No. 1, July-September 2021
8. Lenticule Tear
This occurs in an attempt to pull the lenticule without
dissecting it completely from all sides, more so in cases
of low myopic correction where the lenticule is very
thin and can inadvertently tear during dissection or
removal (Figure 21). Care should be taken to ensure
complete dissection and separation of lenticule from
all sides before pulling it out through the incision.
Post Operative Complications
1. Interface Haze
It may be observed in the immediate post-operative period
due to suboptimal laser energy levels and in cases of
difficult dissection due to OBL / sticky lenticule. It usually
resolves well with topical steroids and cyclosporine eye
drops without having an impact on the long term visual and
refractive outcomes.26
2. Interface Debris
Lint fibres / debris on the instrument / meibomian secretions
Figure 22: Interface debris
can be inadvertently introduced into the stromal pocket
during lenticule dissection. (Figure 22) Interface wash is meibomian secretions, surgical debris into the interface
advisable in cases of excess intra-operative manipulation to have been attributed to this condition. The incidence of DLK
wash out the debris if any. Minimal debris not involving the following SMILE has been reported as between 0.04 and
pupillary axis remains inert without affecting the visual and 1.6 percent.28,29 Zhao et al. found that DLK was associated
refractive outcomes.27 with larger lenticular diameter and thinner lenticules.24 The
proximity of the larger diameter lenticules to the limbus and
3. Diffuse Lamellar Keratitis (DLK) limbal vasculature may cause more inflammatory reaction.
It represents an acute inflammatory response characterised Thinner lenticules may represent a greater technical
by accumulation of white granular cells in the interface. challenge increasing the intra‐operative manipulation and
(Figure 23) Patient may present with discomfort, thereby possible inflammatory response.30 Mild cases are
photophobia and blurring of vision. A definitive cause treated with intense topical steroids and severe cases with a
is unknown, although factors such as introduction of combination of topical and oral steroids.
Post Smile Enhancement
The simplest way to perform an enhancement after SMILE
is photorefractive keratectomy (PRK). An alternative to this
is converting the SMILE cap into a flap and then ablating
the stromal bed to correct the residual refractive error. A
special software called the “Circle” (Carl Zeiss Meditec AG)
has been developed to convert the original SMILE cap into a
complete flap.31
Post Operative Treatment
Antibiotics (preferably Fluoroquinolones), Steroids
(Prednisolone eye drops) in tapering dose and lubricants are
used commonly. Cyclosporine 0.1% eye drops can also be
added to prevent and treat interface haze.In patients who are
steroid responders, low potent steroids along with pressure
lowering agents are to be used.
Post Op Follow Up
Day 1, 1 week, 1 month, 3 months, 6 months and 1 yearly. On
each follow up visits visual acuity (Uniocular and binocular),
Intra ocular pressure and corneal interface clarity are looked
at.
Figure 23: Diffuse lamellar keratitis
E-ISSN: 2454-2784 P-ISSN: 0972-0200 30 www.djo.org.in
DJO Vol. 32, No. 1, July-September 2021
References 21. Harissi-Dagher M, Todani A, Melki SA. Laser in situ keratomileusis
buttonhole: classification and management algorithm. J Cataract
1. Blum M, Täubig K, Gruhn C, Sekundo W, Kunert KS. Five-year Refract Surg. 2008 Nov;34(11):1892-9.
results of Small Incision Lenticule Extraction (ReLEx SMILE). Br J 22. Brenner JE, Mohinani AB, Janbatian HY, Melki S. Early Surface
Ophthalmol. 2016Sep;100(9):1192-5. Ablation on Aborted LASIK Flaps. J Refract Surg. 2019 Feb
2. Chansue E, Tanehsakdi M, Swasdibutra S, McAlinden C. Efficacy, 1;35(2):121-125.
predictability and safety of small incision lenticule extraction 23. Liu CH, Sun CC, Hui-Kang Ma D, Chien-Chieh Huang J, Liu CF,
(SMILE). Eye Vis (Lond). 2015Aug 31;2:14. Chen HF, Hsiao CH. Opaque bubble layer: incidence, risk factors,
3. Seven I, Vahdati A, Pedersen IB, Vestergaard A, Hjortdal J, Roberts and clinical relevance. J Cataract Refract Surg. 2014 Mar;40(3):435-
CJ, Dupps WJ Jr. Contralateral Eye Comparison of SMILE and 40.
Flap-Based Corneal Refractive Surgery: Computational Analysis of 24. Ramirez-Miranda A, Ramirez-Luquin T, Navas A, Graue-
Biomechanical Impact. J Refract Surg. 2017 Jul1;33(7):444-453. Hernandez EO. Refractive Lenticule Extraction Complications.
4. Li M, Niu L, Qin B, Zhou Z, Ni K, Le Q, Xiang J, Wei A, Ma W, Cornea. 2015;34(Suppl 10):S65–S67.
Zhou X. Confocal comparison of corneal reinnervation after small 25. Titiyal JS, Kaur M, Rathi A, Falera R, Chaniyara M, Sharma N.
incision lenticule extraction(SMILE) and femtosecond laser in situ Learning Curve of Small Incision Lenticule Extraction: Challenges
keratomileusis (FS-LASIK). PLoS One. 2013 Dec 9;8(12):e81435. and Complications. Cornea. 2017 Nov;36(11):1377-1382.
5. Soong HK, Malta JB. Femtosecond lasers in ophthalmology. Am J 26. Ivarsen A, Asp S, Hjortdal J. Safety and complications of more than
Ophthalmol. 2009 Feb;147(2):189-197.e2. 1500 small‐incision lenticule extraction procedures. Ophthalmology
6. Wang B, Naidu RK, Chu R, Dai J, Qu X, Zhou H. Dry Eye Disease 2014; 121: 822–828.
following Refractive Surgery: A 12-Month Follow-Up of SMILE 27. Chan C, Lawless M, Sutton G, Versace P, Hodge C. Small incision
versus FS-LASIK in High Myopia. J Ophthalmol. 2015;2015:132417. lenticule extraction (SMILE) in 2015. Clin Exp Optom. 2016;99:204–
7. Knox Cartwright NE, Tyrer JR, Jaycock PD, Marshall J. Effects of 212. doi:10.1111/cxo.12380
variation in depth and side cut angulations in LASIK and thin-flap 28. Moshirfar M, McCaughey MV, Reinstein DZ, Shah R, Santiago-
LASIK using a femtosecond laser: a biomechanical study. J Refract Caban L, Fenzl CR. Small-incision lenticule extraction. J Cataract
Surg. 2012 Jun;28(6):419-25. Refract Surg. 2015 Mar;41(3):652-65.
8. Titiyal JS, Kaur M, Shaikh F, Gagrani M, Brar AS, Rathi A. Small 29. Zhao J, He L, Yao P, Shen Y, Zhou Z, Miao H, Wang X, Zhou X.
incision lenticule extraction (SMILE) techniques: patient selection Diffuse lamellar keratitis after small-incision lenticule extraction. J
and perspectives. Clin Ophthalmol. 2018 Sep 5;12:1685-1699. Cataract Refract Surg. 2015 Feb;41(2):400-7.
9. Ganesh S, Brar S, Pawar A. Results of Intraoperative Manual 30. Zhao J, He L, Yao P, Shen Y, Zhou Z, Miao H, Wang X, Zhou X.
Cyclotorsion Compensation for Myopic Astigmatism in Patients Diffuse lamellar keratitis after small-incision lenticule extraction. J
Undergoing Small Incision Lenticule Extraction (SMILE). J Refract Cataract Refract Surg. 2015 Feb;41(2):400-7.
Surg. 2017 Aug 1;33(8):506-512. 31. Riau AK, Ang HP, Lwin NC, Chaurasia SS, Tan DT, Mehta JS.
10. Shah R, Shah S, Sengupta S. Results of small incision lenticule Comparison of four different VisuMax circle patterns for flap
extraction: All-in-one femtosecond laser refractive surgery. J creation after small incision lenticule extraction. J Refract Surg. 2013
Cataract Refract Surg. 2011;37(1):127–137. Apr;29(4):236-44.
11. Titiyal JS, Kaur M. Small Incision Lenticule Extraction (SMILE):
Surgical Technique and Challenges (Comprehensive Text and
Video Guide) 1st ed. New Delhi: Jaypee Brothers; 2018. Cite This Article as: Sanjana Vatsa, Pallavi Dhawan, Shana Sood,
12. Ganesh S, Brar S, Arra RR. Gas Bubble Escape Sign: A New OA to Z of ReLEx SMILE: All you need to know Delhi Journal of
Intraoperative Sign to Predict Immediate Visual Quality After Small Ophthalmology.2021; Vol 32, No (1): 25 - 31.
Incision Lenticule Extraction. J Refract Surg. 2019 Jul 1;35(7):467-
472. Acknowledgments: Nil
13. Vestergaard AH. Past and present of corneal refractive surgery:
aretrospective study of long-term results after photorefractive Conflict of interest: None declared
keratectomy and a prospective study of refractive lenticule
extraction. Acta Ophthalmol. 2014 Mar;92 Thesis 2:1-21. Source of Funding: None
14. Kamiya K, Shimizu K, Igarashi A, Kobashi H. Visual and
refractive outcomes of femtosecond lenticule extraction and small- Date of Submission: 23 Dec 2020
Date of Acceptance: 12 Jan 2021
incision lenticule extraction for myopia. Am J Ophthalmol. 2014
Jan;157(1):128-134.e2.
15. Agca A, Ozgurhan EB, Yildirim Y, Cankaya KI, Guleryuz NB,
Alkin Z, Ozkaya A, Demirok A, Yilmaz OF. Corneal backscatter Address for correspondence
analysis by in vivo confocal microscopy: fellow eye comparison of
small incision lenticule extraction and femtosecond laser-assisted Sanjana Vatsa
LASIK. J Ophthalmol. 2014;2014:265012. MBBS, MS, FPRS, FCRS
16. Reinstein DZ, Archer TJ, Gobbe M, Bartoli E. Corneal sensitivity Department of Consultant, Cornea and
after small-incision lenticule extraction and laser in situ Refractive Services, Dr. Agarwal’s Eye
keratomileusis. J Cataract Refract Surg. 2015 Aug;41(8):1580-7. Hospital, Bangalore, India.
17. Wong CW, Chan C, Tan D, Mehta JS. Incidence and management
Email : sanjana_5388@yahoo.com
of suction loss in refractive lenticule extraction. J Cataract Refract
Surg. 2014 Dec;40(12):2002-10.
18. Qiu PJ, Yang YB. Analysis and management of intraoperative
complications during small-incision lenticule extraction. Int J
Ophthalmol. 2016 Nov 18;9(11):1697-1700.
19. Shah DN, Melki S. Complications of femtosecond-assisted
laser in-situ keratomileusis flaps. Semin Ophthalmol. 2014 Sep-
Nov;29(5-6):363-75.
20. dos Santos AM, Torricelli AA, Marino GK, Garcia R, Netto MV,
Bechara SJ, Wilson SE. Femtosecond Laser-Assisted LASIK Flap
Complications. J Refract Surg. 2016 Jan;32(1):52-9. Quick Response Code
E-ISSN: 2454-2784 P-ISSN: 0972-0200 31 Delhi Journal of Ophthalmology
You might also like
- Referat SMILEDocument10 pagesReferat SMILEarumNo ratings yet
- Moderator - DR Prof. R.K. Bundela Presented by - Dr. Mohd Raza .Document44 pagesModerator - DR Prof. R.K. Bundela Presented by - Dr. Mohd Raza .alpana100% (1)
- JurdingDocument10 pagesJurdingThobias AndrewNo ratings yet
- Smile HistoryDocument12 pagesSmile HistoryCindyNo ratings yet
- Are Intrastromal Treatments The Future of Refractive Surgery?Document11 pagesAre Intrastromal Treatments The Future of Refractive Surgery?lacisag100% (1)
- Ophthalmology Femtosecond LaserDocument5 pagesOphthalmology Femtosecond LaserChandrika MaluftiNo ratings yet
- 049 - Pigm Vac Irdx JCRS 27 1166Document3 pages049 - Pigm Vac Irdx JCRS 27 1166أحمد ساميNo ratings yet
- ReLExCourseHandout IC80 Reinstein - 2013Document13 pagesReLExCourseHandout IC80 Reinstein - 2013David MartínezNo ratings yet
- Huang2008ChangGungMedJ, Refractive SurgeryDocument16 pagesHuang2008ChangGungMedJ, Refractive SurgeryNabita AuliaNo ratings yet
- Ophthalmology Femtosecond LaserDocument8 pagesOphthalmology Femtosecond LaserChandrika MaluftiNo ratings yet
- Flap Thickness and The Risk of ComplicationsDocument20 pagesFlap Thickness and The Risk of ComplicationsDarwin VasquezNo ratings yet
- Nylon LoopDocument4 pagesNylon LooporlandgpicadoNo ratings yet
- Newer Trends in Lamellar Keratoplasty: Dr. Hijab MehtaDocument6 pagesNewer Trends in Lamellar Keratoplasty: Dr. Hijab MehtaNur Zulaekha Soraya YayaNo ratings yet
- (ACTANEURCH) Clinoidectomia Anterior Como Lo Hice - Hedge - 2013Document5 pages(ACTANEURCH) Clinoidectomia Anterior Como Lo Hice - Hedge - 2013Edwin Abelardo Huaricallo VilcaNo ratings yet
- Surgical Procedure SmileDocument8 pagesSurgical Procedure SmilearumNo ratings yet
- Tugas Baca RS IndraDocument28 pagesTugas Baca RS IndraMade Surya DinajayaNo ratings yet
- Surgical Management of Senile CataractDocument39 pagesSurgical Management of Senile CataractKarthik ChellaNo ratings yet
- Lasik Technology Review in MalaysiaDocument20 pagesLasik Technology Review in Malaysiakey3hseNo ratings yet
- Referat Smile FixfixDocument24 pagesReferat Smile FixfixarumNo ratings yet
- Anterior Segment OctDocument53 pagesAnterior Segment OctA.c. RaghuNo ratings yet
- Objective Evaluation of The Visual Benefit in Contact Lens Fitting After Complicated LASIK-3Document9 pagesObjective Evaluation of The Visual Benefit in Contact Lens Fitting After Complicated LASIK-3Eduard CarrilloNo ratings yet
- Lasik Complication Loss of ElectricityDocument3 pagesLasik Complication Loss of ElectricityDarwin VasquezNo ratings yet
- Cataract: The Role of Nurses in Diagnosis, Surgery and AftercareDocument5 pagesCataract: The Role of Nurses in Diagnosis, Surgery and AftercareFara Sakina RahmaNo ratings yet
- Principles of Vitreoretinal Surgery - Scleral Buckle: Dr. Sumit Kumar MishraDocument49 pagesPrinciples of Vitreoretinal Surgery - Scleral Buckle: Dr. Sumit Kumar MishraSriniwasNo ratings yet
- Unit3 VLSITechnologyDocument76 pagesUnit3 VLSITechnologyAastha ShuklaNo ratings yet
- Jurnal Referat MataDocument8 pagesJurnal Referat MataWinda KristantiNo ratings yet
- Lasik: Patient Doesn't Ask For ADocument3 pagesLasik: Patient Doesn't Ask For AVidge GrospeNo ratings yet
- Lectura 1Document8 pagesLectura 1Carmen Pérez JuradoNo ratings yet
- Refractive Surgeries: DR - Jyoti Shetty Medical Director, Bangalore West Lions Superspeciality Eye HospitalDocument69 pagesRefractive Surgeries: DR - Jyoti Shetty Medical Director, Bangalore West Lions Superspeciality Eye Hospitalprajwal ghimireNo ratings yet
- Intacs: By-Dr. Shirish Patel Moderator - Dr. Mukesh ParyaniDocument16 pagesIntacs: By-Dr. Shirish Patel Moderator - Dr. Mukesh ParyanineovisioncareNo ratings yet
- Long Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofDocument9 pagesLong Term Follow-Up Safety and E Myopia Refractive Surgery: Ffectiveness ofayurNo ratings yet
- Conductive Keratoplasty For The Correction of HyperopiaDocument10 pagesConductive Keratoplasty For The Correction of HyperopiaAchmad Deddy FatoniNo ratings yet
- Wa0000Document7 pagesWa0000Ocha24 TupamahuNo ratings yet
- Clinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKDocument10 pagesClinical Study: Comparison of The Optical Quality Between Small Incision Lenticule Extraction and Femtosecond Laser LASIKnicoNo ratings yet
- Femto Laser in OphthalmologyDocument11 pagesFemto Laser in Ophthalmologylycan007No ratings yet
- 21 A Scan and B ScanDocument59 pages21 A Scan and B Scanjay daxiniNo ratings yet
- Clinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisDocument5 pagesClinical Study: Photorefractive Keratectomy For Residual Myopia After Myopic Laser in Situ KeratomileusisayurNo ratings yet
- Post-Keratoplasty Astigmatism Management by RelaxiDocument7 pagesPost-Keratoplasty Astigmatism Management by Relaximedamif3No ratings yet
- Laser in ProsthodonticsDocument84 pagesLaser in ProsthodonticsmarwaNo ratings yet
- FlaplasikDocument7 pagesFlaplasikjorge vegaNo ratings yet
- Cornealtopographybysuraj 160507151045Document112 pagesCornealtopographybysuraj 160507151045Ridho HariyadiNo ratings yet
- 2016 08 01 Cls Post Operative CL FittingDocument12 pages2016 08 01 Cls Post Operative CL FittingLina FierroNo ratings yet
- Sanchit Singla 100905089 Eic 3 (Attending Tute With Eic 2)Document29 pagesSanchit Singla 100905089 Eic 3 (Attending Tute With Eic 2)sanchit2418No ratings yet
- Tear Film White Paper 020310Document4 pagesTear Film White Paper 020310Prasi YusNo ratings yet
- PM190 ch1Document6 pagesPM190 ch1曾詠翔No ratings yet
- Vis AnteDocument16 pagesVis AntejochigNo ratings yet
- Prepared by Guided by K.S.Vaghosi Prof. G.D.Karadkar M.E.Part - Ii (Production) Roll No - 139 Mech. DepttDocument42 pagesPrepared by Guided by K.S.Vaghosi Prof. G.D.Karadkar M.E.Part - Ii (Production) Roll No - 139 Mech. DepttKetan VaghosiNo ratings yet
- 97 Physics DraftDocument5 pages97 Physics DraftMatthew OoiNo ratings yet
- Large-Stroke Varifocal Mirror With Hydraulic Actuation For Endoscopic Laser SurgeryDocument7 pagesLarge-Stroke Varifocal Mirror With Hydraulic Actuation For Endoscopic Laser SurgeryAndrea JacassiNo ratings yet
- Performance of A 1.35na Arf Immersion Lithography System For 40Nm ApplicationsDocument14 pagesPerformance of A 1.35na Arf Immersion Lithography System For 40Nm ApplicationscaokovskyNo ratings yet
- Ijo 68 2773Document6 pagesIjo 68 2773julia.soaresrNo ratings yet
- Cataract 20surgery 2029 05 2008 131224024457 Phpapp01Document61 pagesCataract 20surgery 2029 05 2008 131224024457 Phpapp01sachin48No ratings yet
- Small Incision Lenticule ExtractionDocument5 pagesSmall Incision Lenticule ExtractionvrlftrNo ratings yet
- Calculation of Toric Intraocular Lenses Using Multivariate RegressionDocument9 pagesCalculation of Toric Intraocular Lenses Using Multivariate RegressionRonald PuchaNo ratings yet
- Laser AktuDocument17 pagesLaser AktuMohitNo ratings yet
- Clinical Application of Laser in DentistryDocument42 pagesClinical Application of Laser in DentistryRabeea KittaniNo ratings yet
- CXL Te Istanbul 2011Document59 pagesCXL Te Istanbul 2011Ana_BiosooftNo ratings yet
- Limbal Relaxing Incisions FixedDocument18 pagesLimbal Relaxing Incisions Fixedaswan bagasNo ratings yet
- Optical Design of A New Folding Scanning System in MEMS-based LidarDocument8 pagesOptical Design of A New Folding Scanning System in MEMS-based Lidaryuguang liNo ratings yet
- SCIENCE 10-MODULE 4-Use of lenses-and-mirrors-FAJARDO, Mary RoseDocument49 pagesSCIENCE 10-MODULE 4-Use of lenses-and-mirrors-FAJARDO, Mary RoseMary Rose FajardoNo ratings yet
- Human Eye and Colourful World NotesDocument25 pagesHuman Eye and Colourful World NotesAzeem Iqbal100% (2)
- IMI - Prevention of Myopia and Its ProgressionDocument10 pagesIMI - Prevention of Myopia and Its ProgressionJesse James Arteaga PeraltaNo ratings yet
- Essential Vocabulary For College-Bound Students (Haller, Margaret A) (Z-Library)Document244 pagesEssential Vocabulary For College-Bound Students (Haller, Margaret A) (Z-Library)jeanjacquesnkouameNo ratings yet
- Human Eye - Shobhit NirwanDocument14 pagesHuman Eye - Shobhit NirwanbookssssNo ratings yet
- Lens and The EyeDocument58 pagesLens and The EyeEisle Keith Rivera TapiaNo ratings yet
- Fisio - Faal Special SenseDocument107 pagesFisio - Faal Special SensetiffsbronteNo ratings yet
- Surgical Options For Multifocality 3 (Edited With Comments FR Dr. Alio) - Sent To DR PicardoDocument22 pagesSurgical Options For Multifocality 3 (Edited With Comments FR Dr. Alio) - Sent To DR PicardoJoan BalgosNo ratings yet
- MyopiaDocument83 pagesMyopiaOphthalmology DiscussionNo ratings yet
- Toprank Nursing: Patrick Migel Mercado, RNDocument126 pagesToprank Nursing: Patrick Migel Mercado, RNNoreen PadillaNo ratings yet
- 1 Chapter 1 - Introduction To Data - Stats 250Document48 pages1 Chapter 1 - Introduction To Data - Stats 250Oliver BarrNo ratings yet
- How Much Astigmatism To Treat in Cataract SurgeryDocument5 pagesHow Much Astigmatism To Treat in Cataract SurgeryPaulaNo ratings yet
- MC - Ch15.1 (TS) EyesDocument12 pagesMC - Ch15.1 (TS) Eyes葡萄蘿蔔No ratings yet
- Unit 4 Laser and Of, 21PH12 - 22Document54 pagesUnit 4 Laser and Of, 21PH12 - 22Laksh HeeraNo ratings yet
- Screenshot 2024-02-24 at 07.32.43Document38 pagesScreenshot 2024-02-24 at 07.32.43Krishna NugrahaNo ratings yet
- Role of Atropine To Control Myopia in Indian Childrens A ReviewDocument5 pagesRole of Atropine To Control Myopia in Indian Childrens A ReviewRagni MishraNo ratings yet
- Biology IPDocument17 pagesBiology IPIshika RajputNo ratings yet
- Human Eye and Colourful World (PW)Document16 pagesHuman Eye and Colourful World (PW)Rahul ChoudharyNo ratings yet
- Clinical Accomodation ProblemsDocument15 pagesClinical Accomodation ProblemsdwindaNo ratings yet
- Health6 q1 Mod1 Personalhealthissuesandconcern v1Document23 pagesHealth6 q1 Mod1 Personalhealthissuesandconcern v1Lhen YanzonNo ratings yet
- Induction Deck - v2Document56 pagesInduction Deck - v2tanisha satijaNo ratings yet
- Lenses and Mirrors: Enrichment ActivityDocument2 pagesLenses and Mirrors: Enrichment ActivityAnh NguyenNo ratings yet
- Prevention and Management of Childhood Progressive MyopiaDocument9 pagesPrevention and Management of Childhood Progressive MyopiaJENNY MARITZA SANCHEZ ESPINOSANo ratings yet
- Human Eye and Colourful WorldDocument39 pagesHuman Eye and Colourful WorldSridhar NNo ratings yet
- CH 11 Human EyeDocument4 pagesCH 11 Human EyekniFe VisualzNo ratings yet
- Science 10 - Set 2 - DS 1Document10 pagesScience 10 - Set 2 - DS 1DhejehNo ratings yet
- Astigmatic Refractive Correction: Jackson Cross: Basic Optics, Chapter 13Document141 pagesAstigmatic Refractive Correction: Jackson Cross: Basic Optics, Chapter 13PAM ALVARADONo ratings yet
- BCLA YOUR CHILD & MYOPIA Factsheet FVDocument2 pagesBCLA YOUR CHILD & MYOPIA Factsheet FVJorge CarcacheNo ratings yet
- 1.myopia Laser Surgery - Sight Restoration or Blindness - What The Experts Aren't Telling YouDocument5 pages1.myopia Laser Surgery - Sight Restoration or Blindness - What The Experts Aren't Telling YouElvaNo ratings yet
- Share 5 - 6242427251804083142Document10 pagesShare 5 - 624242725180408314211084thevijaymillenniuminNo ratings yet