Professional Documents
Culture Documents
0 ratings0% found this document useful (0 votes)
14 viewsNow What-How Do I Protect Them From Harm
Now What-How Do I Protect Them From Harm
Uploaded by
MohammedThis document provides guidance on harm reduction strategies for critically ill patients in the ICU. It recommends pharmacologic deep venous thrombosis prophylaxis over mechanical options. It also recommends stress ulcer prophylaxis with a PPI or H2 blocker for intubated patients not receiving nutrition or those at high risk of gastrointestinal bleeding. Other harm reduction strategies include daily review of central lines and foley catheters to remove unnecessary devices, implementing ventilator associated pneumonia bundles, and using an ICU checklist to address quality and safety items.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You might also like
- Icu Protocols-1Document38 pagesIcu Protocols-1M.IMRAN ANJUM100% (1)
- ICU Note Writing GuidelinesDocument2 pagesICU Note Writing GuidelinesMohammedNo ratings yet
- 1b. Ambulatory AnesthesiaDocument47 pages1b. Ambulatory AnesthesiaBakingpancakes100% (5)
- Pre and Post Operative Care For Patient After Cardiac SurgeryDocument20 pagesPre and Post Operative Care For Patient After Cardiac SurgeryGayathri RNo ratings yet
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- Pre and Post Operative CareDocument9 pagesPre and Post Operative CareSara Abdi OsmanNo ratings yet
- Ulcer and DVT ProphylaxisDocument82 pagesUlcer and DVT ProphylaxisKiyasweet HaniNo ratings yet
- General Icu Care and PrinciplesDocument5 pagesGeneral Icu Care and Principles21910589No ratings yet
- Antibiotic Prophy and DVT PrevDocument27 pagesAntibiotic Prophy and DVT PrevzhouyueNo ratings yet
- Preoperative Preparation For Surgery: Presented By: Dr. Md. Mujibur Rahman Rony IMO, Ward: 24, Surgery Unit: 1 CMCHDocument31 pagesPreoperative Preparation For Surgery: Presented By: Dr. Md. Mujibur Rahman Rony IMO, Ward: 24, Surgery Unit: 1 CMCHginasti keistouNo ratings yet
- GDL Fever OncologyDocument16 pagesGDL Fever OncologyZaini GhazaliNo ratings yet
- Enhanced Recovery After SurgeryDocument60 pagesEnhanced Recovery After Surgeryvacha sardarNo ratings yet
- L11 Medically Compromised Patients 2Document59 pagesL11 Medically Compromised Patients 2elle70503No ratings yet
- NHMRC VTE Prevention Guideline Summary For CliniciansDocument2 pagesNHMRC VTE Prevention Guideline Summary For CliniciansRatnaSuryati100% (1)
- Deep Vein ThrombosisDocument22 pagesDeep Vein ThrombosisEznal MahidinNo ratings yet
- Clinical Diagnosis ofDocument14 pagesClinical Diagnosis ofNor Shuhada HaronNo ratings yet
- DVT Prophylaxis Safety ContraindicatDocument1 pageDVT Prophylaxis Safety Contraindicata1b14No ratings yet
- Management of Hemophilia: Dr. Zoona Qazi Post Graduate ResidentDocument33 pagesManagement of Hemophilia: Dr. Zoona Qazi Post Graduate ResidentZuna QaziNo ratings yet
- Day Case SurgeryDocument5 pagesDay Case SurgerylasseypetNo ratings yet
- Principles of Anesthesia Perioperative CareDocument28 pagesPrinciples of Anesthesia Perioperative CareHammy LizerNo ratings yet
- Day Care AnesthesiaDocument68 pagesDay Care AnesthesiaSri Sruthi PichikaNo ratings yet
- Anticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveDocument3 pagesAnticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveShoyeb KhanNo ratings yet
- Bundle Care ApproachDocument13 pagesBundle Care ApproachSmriti SrivastavaNo ratings yet
- Medically Compromised PatientsVoiceDocument30 pagesMedically Compromised PatientsVoiceGeorge CharchNo ratings yet
- Preoperative AssessmentDocument26 pagesPreoperative Assessmentkaukab azimNo ratings yet
- COVID-19 Drugs & Treatment: BWH Quick-Reference GuideDocument1 pageCOVID-19 Drugs & Treatment: BWH Quick-Reference GuideBoules AtefNo ratings yet
- Prevention of Infective Endocarditis AHA EditDocument17 pagesPrevention of Infective Endocarditis AHA EditDampee ReturnNo ratings yet
- Bedside Sheets Safety FullDocument6 pagesBedside Sheets Safety FullHue LeNo ratings yet
- Quick Guide DVTDocument26 pagesQuick Guide DVTdrkrsticNo ratings yet
- Pre-Operative AssessmentDocument62 pagesPre-Operative AssessmentRochelle BaileyNo ratings yet
- Whipple's OperationDocument35 pagesWhipple's OperationSunaina AdhikariNo ratings yet
- NPO Means "Nothing by Mouth," From The LatinDocument4 pagesNPO Means "Nothing by Mouth," From The Latin14 zarwa hassanNo ratings yet
- Fast HugDocument41 pagesFast HugBharti NaraNo ratings yet
- Preoperative PreparationsDocument26 pagesPreoperative PreparationsReda IsmaeelNo ratings yet
- Anaesthesia For A Patient With Coagulation DisorderDocument33 pagesAnaesthesia For A Patient With Coagulation DisorderNdenwaneku OkuwaNo ratings yet
- DR Rudi IPDI2017 Insersi Kateter Peritonel Dan Komplikasiny 1Document73 pagesDR Rudi IPDI2017 Insersi Kateter Peritonel Dan Komplikasiny 1julia sianturi100% (1)
- Acute Nonvariceal Upper Gastrointestinal Bleeding - DynaMedDocument139 pagesAcute Nonvariceal Upper Gastrointestinal Bleeding - DynaMedJosué RamosNo ratings yet
- Rapid Sequence Induction and Intubation (RSII) For Anesthesia - UpToDateDocument35 pagesRapid Sequence Induction and Intubation (RSII) For Anesthesia - UpToDateSofíaNo ratings yet
- Periprocedural Management With Antithrombotic Therapy Adult Inpatient Ambulatory Guideline 20201029Document14 pagesPeriprocedural Management With Antithrombotic Therapy Adult Inpatient Ambulatory Guideline 20201029Joanne HoNo ratings yet
- Gui Iia Uk PDFDocument2 pagesGui Iia Uk PDFluckevNo ratings yet
- Friedman VTE Bundle PDFDocument24 pagesFriedman VTE Bundle PDFGerman Parra CNo ratings yet
- Apixaban Eliquis MonographDocument14 pagesApixaban Eliquis MonographTran Minh NgocNo ratings yet
- PreoperativeDocument34 pagesPreoperativeTasha NurfitrianiNo ratings yet
- Warfarin Perioperative ManagementDocument8 pagesWarfarin Perioperative Managementzoran cukovicNo ratings yet
- Bowels Open 6 Times Per 24 Hours: Document ControlDocument7 pagesBowels Open 6 Times Per 24 Hours: Document ControlKeith PohlNo ratings yet
- 7 Preop and Postoperative CareDocument71 pages7 Preop and Postoperative CareHailemariam MebratuNo ratings yet
- Preoperative Management of MedsDocument25 pagesPreoperative Management of Medsres.uditacharyaNo ratings yet
- Anesthesia For Emergency AppendectomyDocument44 pagesAnesthesia For Emergency AppendectomyPrincess Lorenzo MiguelNo ratings yet
- PID TreatmentDocument17 pagesPID Treatmenttriana_nimanNo ratings yet
- Anesthesia For Day Care SurgeryDocument60 pagesAnesthesia For Day Care Surgerymedico_bhalla93% (15)
- Periodontics يرﻛﺷ ﺎﮭﻣ د: Periodontal management of medically compromised patientsDocument8 pagesPeriodontics يرﻛﺷ ﺎﮭﻣ د: Periodontal management of medically compromised patientsYehya Al KhashabNo ratings yet
- 于跃远 - Dental and Alveolar SurgeryDocument26 pages于跃远 - Dental and Alveolar SurgeryIsak ShatikaNo ratings yet
- Emergency Laparotomy PDFDocument13 pagesEmergency Laparotomy PDFbushra mughalNo ratings yet
- Antibiotc ProphylaxisDocument22 pagesAntibiotc Prophylaxisgitama9904No ratings yet
- PRE ANAESTHETIC ASSESSMENT New 1Document41 pagesPRE ANAESTHETIC ASSESSMENT New 1lokeswara reddyNo ratings yet
- Acute Pancreatitis in AdultsDocument107 pagesAcute Pancreatitis in AdultsBurhan MinervaNo ratings yet
- Cellulitis in Adults - Guideline Flowchart Hospital in The Home Guideline For Management at HomeDocument2 pagesCellulitis in Adults - Guideline Flowchart Hospital in The Home Guideline For Management at HomeAnonymous 4txA8N8etNo ratings yet
- Pre-Operative Fasting (Report)Document7 pagesPre-Operative Fasting (Report)Carlo Paul Castro SanaNo ratings yet
- HYSTERECTOMY Tuazon SapanDocument58 pagesHYSTERECTOMY Tuazon SapanMonette Abalos MendovaNo ratings yet
- Acute Upper Gi HaemorrhageDocument12 pagesAcute Upper Gi HaemorrhageMuhamad NaqibNo ratings yet
- Pre-Operative Nursing CareDocument79 pagesPre-Operative Nursing CarePeter FrimpongNo ratings yet
- سياسات٠٣Document1 pageسياسات٠٣MohammedNo ratings yet
- سياسات٥١Document3 pagesسياسات٥١MohammedNo ratings yet
- سياسات٣٢Document1 pageسياسات٣٢MohammedNo ratings yet
- سياسات٠٤Document1 pageسياسات٠٤MohammedNo ratings yet
- Attendee Report - View History of PDFS, Images and VideosDocument1 pageAttendee Report - View History of PDFS, Images and VideosMohammedNo ratings yet
- Conclusions ALI ARDSDocument4 pagesConclusions ALI ARDSMohammedNo ratings yet
- Emergency Call Codes PolicyDocument3 pagesEmergency Call Codes PolicyMohammedNo ratings yet
- Flow MonitoringDocument1 pageFlow MonitoringMohammedNo ratings yet
- 4 6005681254219908298Document5 pages4 6005681254219908298MohammedNo ratings yet
- BDC Dka Treatment Protocol 2018 85Document12 pagesBDC Dka Treatment Protocol 2018 85MohammedNo ratings yet
- Gaat 15 I 1 P 88Document2 pagesGaat 15 I 1 P 88MohammedNo ratings yet
- FrassDocument2 pagesFrassMohammedNo ratings yet
- 003 DkaDocument9 pages003 DkaMohammedNo ratings yet
- 366 - Informed Consent FormDocument2 pages366 - Informed Consent FormMohammedNo ratings yet
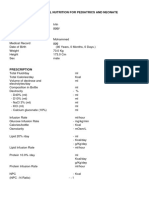
- 01 Guidelines For Creating TPN OrdersDocument6 pages01 Guidelines For Creating TPN OrdersMohammedNo ratings yet
- Categorized by Conditions and Components, and by Patient Acuity, As Described in "The Model of The Clinical Practice of Emergency Medicine"Document2 pagesCategorized by Conditions and Components, and by Patient Acuity, As Described in "The Model of The Clinical Practice of Emergency Medicine"MohammedNo ratings yet
- Volume Versus Pressure ControlDocument1 pageVolume Versus Pressure ControlMohammedNo ratings yet
- 03 Oa Evaluation of CerebralDocument6 pages03 Oa Evaluation of CerebralMohammedNo ratings yet
- Abcds During A Code Blue Response in An Adult Patient PostDocument4 pagesAbcds During A Code Blue Response in An Adult Patient PostMohammedNo ratings yet
- Educational Summary Report 10740Document6 pagesEducational Summary Report 10740MohammedNo ratings yet
- Braden Risk Assessment Tool: Category Descriptor Score Score ScoreDocument1 pageBraden Risk Assessment Tool: Category Descriptor Score Score ScoreMohammedNo ratings yet
- Medical Record General Admission ConsentDocument1 pageMedical Record General Admission ConsentMohammedNo ratings yet
- Learner: Mohammed Saif: Grades For Year: ALLDocument2 pagesLearner: Mohammed Saif: Grades For Year: ALLMohammedNo ratings yet
Now What-How Do I Protect Them From Harm
Now What-How Do I Protect Them From Harm
Uploaded by
Mohammed0 ratings0% found this document useful (0 votes)
14 views1 pageThis document provides guidance on harm reduction strategies for critically ill patients in the ICU. It recommends pharmacologic deep venous thrombosis prophylaxis over mechanical options. It also recommends stress ulcer prophylaxis with a PPI or H2 blocker for intubated patients not receiving nutrition or those at high risk of gastrointestinal bleeding. Other harm reduction strategies include daily review of central lines and foley catheters to remove unnecessary devices, implementing ventilator associated pneumonia bundles, and using an ICU checklist to address quality and safety items.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides guidance on harm reduction strategies for critically ill patients in the ICU. It recommends pharmacologic deep venous thrombosis prophylaxis over mechanical options. It also recommends stress ulcer prophylaxis with a PPI or H2 blocker for intubated patients not receiving nutrition or those at high risk of gastrointestinal bleeding. Other harm reduction strategies include daily review of central lines and foley catheters to remove unnecessary devices, implementing ventilator associated pneumonia bundles, and using an ICU checklist to address quality and safety items.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
14 views1 pageNow What-How Do I Protect Them From Harm
Now What-How Do I Protect Them From Harm
Uploaded by
MohammedThis document provides guidance on harm reduction strategies for critically ill patients in the ICU. It recommends pharmacologic deep venous thrombosis prophylaxis over mechanical options. It also recommends stress ulcer prophylaxis with a PPI or H2 blocker for intubated patients not receiving nutrition or those at high risk of gastrointestinal bleeding. Other harm reduction strategies include daily review of central lines and foley catheters to remove unnecessary devices, implementing ventilator associated pneumonia bundles, and using an ICU checklist to address quality and safety items.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 1
I Need To Protect My Patient From Harm In the ICU… Now What Do I Do?
Deep Venous Thrombosis (DVT) Prophylaxis
• A single form of prophylaxis is indicated in all critically ill patients
• Rely on pharmacologic over mechanical (sequential compression devices) unless
contraindications to pharmacologic prophylaxis present (active bleeding, HIT, platelet <50k)
• Options for pharmacologic DVT prophylaxis:
- Unfractionated heparin: usual dose 5000 U SQ Q8 hours
- Low-molecular weight heparin (enoxaparin): usual dose 40 mg SQ daily
May be preferred for COVID-19 due to daily dosing
Contraindicated in eGFR < 30
• Call for Help! Consult the pharmacist for patients at the extremes of body mass
Stress Ulcer Prophylaxis
• Primary indications:
- Intubated, not receiving enteral nutrition (discontinue once on full nutrition)
- High risk for gastrointestinal bleeding (prior history, coagulopathy, high dose steroids)
• Primary options: proton pump inhibitor (PPI) or H2 blocker
• If patient is on a PPI or H2 blocker prior to admission, continue it
Other Harm Reduction Strategies
• Review indications for central venous catheters on a daily basis and whether they can be
removed.
• Ventilator Associated Pneumonia (VAP) Prevention Bundle for all intubated patients
- Semi-upright positioning (Head of bed >30o)
- Oral hygiene with chlorhexidine
- Careful monitoring of endotracheal tube cuff pressures
- Daily assessment of readiness to extubate
• Review indications for foley catheter and remove as soon as able.
- Invasive mechanical ventilation does not mandate placement of catheter
- Risk of discontinuing catheter must be weighed vs. risk of skin break down and nursing
care
• Review “ICU Checklist” every day on rounds to ensure these and other quality safety
dashboard items are addressed.
Critical Care Skills for Non-Critical Care Providers
Harm Reduction
You might also like
- Icu Protocols-1Document38 pagesIcu Protocols-1M.IMRAN ANJUM100% (1)
- ICU Note Writing GuidelinesDocument2 pagesICU Note Writing GuidelinesMohammedNo ratings yet
- 1b. Ambulatory AnesthesiaDocument47 pages1b. Ambulatory AnesthesiaBakingpancakes100% (5)
- Pre and Post Operative Care For Patient After Cardiac SurgeryDocument20 pagesPre and Post Operative Care For Patient After Cardiac SurgeryGayathri RNo ratings yet
- Orthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingFrom EverandOrthopedic Inpatient Protocols: A Guide to Orthopedic Inpatient RoundingNo ratings yet
- Pre and Post Operative CareDocument9 pagesPre and Post Operative CareSara Abdi OsmanNo ratings yet
- Ulcer and DVT ProphylaxisDocument82 pagesUlcer and DVT ProphylaxisKiyasweet HaniNo ratings yet
- General Icu Care and PrinciplesDocument5 pagesGeneral Icu Care and Principles21910589No ratings yet
- Antibiotic Prophy and DVT PrevDocument27 pagesAntibiotic Prophy and DVT PrevzhouyueNo ratings yet
- Preoperative Preparation For Surgery: Presented By: Dr. Md. Mujibur Rahman Rony IMO, Ward: 24, Surgery Unit: 1 CMCHDocument31 pagesPreoperative Preparation For Surgery: Presented By: Dr. Md. Mujibur Rahman Rony IMO, Ward: 24, Surgery Unit: 1 CMCHginasti keistouNo ratings yet
- GDL Fever OncologyDocument16 pagesGDL Fever OncologyZaini GhazaliNo ratings yet
- Enhanced Recovery After SurgeryDocument60 pagesEnhanced Recovery After Surgeryvacha sardarNo ratings yet
- L11 Medically Compromised Patients 2Document59 pagesL11 Medically Compromised Patients 2elle70503No ratings yet
- NHMRC VTE Prevention Guideline Summary For CliniciansDocument2 pagesNHMRC VTE Prevention Guideline Summary For CliniciansRatnaSuryati100% (1)
- Deep Vein ThrombosisDocument22 pagesDeep Vein ThrombosisEznal MahidinNo ratings yet
- Clinical Diagnosis ofDocument14 pagesClinical Diagnosis ofNor Shuhada HaronNo ratings yet
- DVT Prophylaxis Safety ContraindicatDocument1 pageDVT Prophylaxis Safety Contraindicata1b14No ratings yet
- Management of Hemophilia: Dr. Zoona Qazi Post Graduate ResidentDocument33 pagesManagement of Hemophilia: Dr. Zoona Qazi Post Graduate ResidentZuna QaziNo ratings yet
- Day Case SurgeryDocument5 pagesDay Case SurgerylasseypetNo ratings yet
- Principles of Anesthesia Perioperative CareDocument28 pagesPrinciples of Anesthesia Perioperative CareHammy LizerNo ratings yet
- Day Care AnesthesiaDocument68 pagesDay Care AnesthesiaSri Sruthi PichikaNo ratings yet
- Anticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveDocument3 pagesAnticoagulation in Presence of Neuraxial Anesthesia (Guidelines Do Not Apply To Peripheral NerveShoyeb KhanNo ratings yet
- Bundle Care ApproachDocument13 pagesBundle Care ApproachSmriti SrivastavaNo ratings yet
- Medically Compromised PatientsVoiceDocument30 pagesMedically Compromised PatientsVoiceGeorge CharchNo ratings yet
- Preoperative AssessmentDocument26 pagesPreoperative Assessmentkaukab azimNo ratings yet
- COVID-19 Drugs & Treatment: BWH Quick-Reference GuideDocument1 pageCOVID-19 Drugs & Treatment: BWH Quick-Reference GuideBoules AtefNo ratings yet
- Prevention of Infective Endocarditis AHA EditDocument17 pagesPrevention of Infective Endocarditis AHA EditDampee ReturnNo ratings yet
- Bedside Sheets Safety FullDocument6 pagesBedside Sheets Safety FullHue LeNo ratings yet
- Quick Guide DVTDocument26 pagesQuick Guide DVTdrkrsticNo ratings yet
- Pre-Operative AssessmentDocument62 pagesPre-Operative AssessmentRochelle BaileyNo ratings yet
- Whipple's OperationDocument35 pagesWhipple's OperationSunaina AdhikariNo ratings yet
- NPO Means "Nothing by Mouth," From The LatinDocument4 pagesNPO Means "Nothing by Mouth," From The Latin14 zarwa hassanNo ratings yet
- Fast HugDocument41 pagesFast HugBharti NaraNo ratings yet
- Preoperative PreparationsDocument26 pagesPreoperative PreparationsReda IsmaeelNo ratings yet
- Anaesthesia For A Patient With Coagulation DisorderDocument33 pagesAnaesthesia For A Patient With Coagulation DisorderNdenwaneku OkuwaNo ratings yet
- DR Rudi IPDI2017 Insersi Kateter Peritonel Dan Komplikasiny 1Document73 pagesDR Rudi IPDI2017 Insersi Kateter Peritonel Dan Komplikasiny 1julia sianturi100% (1)
- Acute Nonvariceal Upper Gastrointestinal Bleeding - DynaMedDocument139 pagesAcute Nonvariceal Upper Gastrointestinal Bleeding - DynaMedJosué RamosNo ratings yet
- Rapid Sequence Induction and Intubation (RSII) For Anesthesia - UpToDateDocument35 pagesRapid Sequence Induction and Intubation (RSII) For Anesthesia - UpToDateSofíaNo ratings yet
- Periprocedural Management With Antithrombotic Therapy Adult Inpatient Ambulatory Guideline 20201029Document14 pagesPeriprocedural Management With Antithrombotic Therapy Adult Inpatient Ambulatory Guideline 20201029Joanne HoNo ratings yet
- Gui Iia Uk PDFDocument2 pagesGui Iia Uk PDFluckevNo ratings yet
- Friedman VTE Bundle PDFDocument24 pagesFriedman VTE Bundle PDFGerman Parra CNo ratings yet
- Apixaban Eliquis MonographDocument14 pagesApixaban Eliquis MonographTran Minh NgocNo ratings yet
- PreoperativeDocument34 pagesPreoperativeTasha NurfitrianiNo ratings yet
- Warfarin Perioperative ManagementDocument8 pagesWarfarin Perioperative Managementzoran cukovicNo ratings yet
- Bowels Open 6 Times Per 24 Hours: Document ControlDocument7 pagesBowels Open 6 Times Per 24 Hours: Document ControlKeith PohlNo ratings yet
- 7 Preop and Postoperative CareDocument71 pages7 Preop and Postoperative CareHailemariam MebratuNo ratings yet
- Preoperative Management of MedsDocument25 pagesPreoperative Management of Medsres.uditacharyaNo ratings yet
- Anesthesia For Emergency AppendectomyDocument44 pagesAnesthesia For Emergency AppendectomyPrincess Lorenzo MiguelNo ratings yet
- PID TreatmentDocument17 pagesPID Treatmenttriana_nimanNo ratings yet
- Anesthesia For Day Care SurgeryDocument60 pagesAnesthesia For Day Care Surgerymedico_bhalla93% (15)
- Periodontics يرﻛﺷ ﺎﮭﻣ د: Periodontal management of medically compromised patientsDocument8 pagesPeriodontics يرﻛﺷ ﺎﮭﻣ د: Periodontal management of medically compromised patientsYehya Al KhashabNo ratings yet
- 于跃远 - Dental and Alveolar SurgeryDocument26 pages于跃远 - Dental and Alveolar SurgeryIsak ShatikaNo ratings yet
- Emergency Laparotomy PDFDocument13 pagesEmergency Laparotomy PDFbushra mughalNo ratings yet
- Antibiotc ProphylaxisDocument22 pagesAntibiotc Prophylaxisgitama9904No ratings yet
- PRE ANAESTHETIC ASSESSMENT New 1Document41 pagesPRE ANAESTHETIC ASSESSMENT New 1lokeswara reddyNo ratings yet
- Acute Pancreatitis in AdultsDocument107 pagesAcute Pancreatitis in AdultsBurhan MinervaNo ratings yet
- Cellulitis in Adults - Guideline Flowchart Hospital in The Home Guideline For Management at HomeDocument2 pagesCellulitis in Adults - Guideline Flowchart Hospital in The Home Guideline For Management at HomeAnonymous 4txA8N8etNo ratings yet
- Pre-Operative Fasting (Report)Document7 pagesPre-Operative Fasting (Report)Carlo Paul Castro SanaNo ratings yet
- HYSTERECTOMY Tuazon SapanDocument58 pagesHYSTERECTOMY Tuazon SapanMonette Abalos MendovaNo ratings yet
- Acute Upper Gi HaemorrhageDocument12 pagesAcute Upper Gi HaemorrhageMuhamad NaqibNo ratings yet
- Pre-Operative Nursing CareDocument79 pagesPre-Operative Nursing CarePeter FrimpongNo ratings yet
- سياسات٠٣Document1 pageسياسات٠٣MohammedNo ratings yet
- سياسات٥١Document3 pagesسياسات٥١MohammedNo ratings yet
- سياسات٣٢Document1 pageسياسات٣٢MohammedNo ratings yet
- سياسات٠٤Document1 pageسياسات٠٤MohammedNo ratings yet
- Attendee Report - View History of PDFS, Images and VideosDocument1 pageAttendee Report - View History of PDFS, Images and VideosMohammedNo ratings yet
- Conclusions ALI ARDSDocument4 pagesConclusions ALI ARDSMohammedNo ratings yet
- Emergency Call Codes PolicyDocument3 pagesEmergency Call Codes PolicyMohammedNo ratings yet
- Flow MonitoringDocument1 pageFlow MonitoringMohammedNo ratings yet
- 4 6005681254219908298Document5 pages4 6005681254219908298MohammedNo ratings yet
- BDC Dka Treatment Protocol 2018 85Document12 pagesBDC Dka Treatment Protocol 2018 85MohammedNo ratings yet
- Gaat 15 I 1 P 88Document2 pagesGaat 15 I 1 P 88MohammedNo ratings yet
- FrassDocument2 pagesFrassMohammedNo ratings yet
- 003 DkaDocument9 pages003 DkaMohammedNo ratings yet
- 366 - Informed Consent FormDocument2 pages366 - Informed Consent FormMohammedNo ratings yet
- 01 Guidelines For Creating TPN OrdersDocument6 pages01 Guidelines For Creating TPN OrdersMohammedNo ratings yet
- Categorized by Conditions and Components, and by Patient Acuity, As Described in "The Model of The Clinical Practice of Emergency Medicine"Document2 pagesCategorized by Conditions and Components, and by Patient Acuity, As Described in "The Model of The Clinical Practice of Emergency Medicine"MohammedNo ratings yet
- Volume Versus Pressure ControlDocument1 pageVolume Versus Pressure ControlMohammedNo ratings yet
- 03 Oa Evaluation of CerebralDocument6 pages03 Oa Evaluation of CerebralMohammedNo ratings yet
- Abcds During A Code Blue Response in An Adult Patient PostDocument4 pagesAbcds During A Code Blue Response in An Adult Patient PostMohammedNo ratings yet
- Educational Summary Report 10740Document6 pagesEducational Summary Report 10740MohammedNo ratings yet
- Braden Risk Assessment Tool: Category Descriptor Score Score ScoreDocument1 pageBraden Risk Assessment Tool: Category Descriptor Score Score ScoreMohammedNo ratings yet
- Medical Record General Admission ConsentDocument1 pageMedical Record General Admission ConsentMohammedNo ratings yet
- Learner: Mohammed Saif: Grades For Year: ALLDocument2 pagesLearner: Mohammed Saif: Grades For Year: ALLMohammedNo ratings yet