Professional Documents
Culture Documents
Proposalto IPSfor Addiction Speciality Subsection 3
Proposalto IPSfor Addiction Speciality Subsection 3
Uploaded by
faradayzzzOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Proposalto IPSfor Addiction Speciality Subsection 3
Proposalto IPSfor Addiction Speciality Subsection 3
Uploaded by
faradayzzzCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/26492633
Proposal to the Indian Psychiatric Society for adopting a specialty
section on addiction medicine (alcohol and other substance abuse)
Article in Indian Journal of Psychiatry · October 2007
DOI: 10.4103/0019-5545.37669 · Source: DOAJ
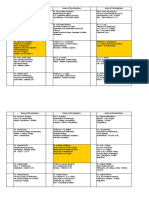
CITATIONS READS
14 215
25 authors, including:
Vivek Benegal Alok Bajpai
National Institute of Mental Health and Neuro Sciences Regency Hospital, Kanpur
229 PUBLICATIONS 4,076 CITATIONS 1 PUBLICATION 14 CITATIONS
SEE PROFILE SEE PROFILE
Debasish Basu Digvijay Goel
Postgraduate Institute of Medical Education and Research 12 PUBLICATIONS 185 CITATIONS
309 PUBLICATIONS 3,799 CITATIONS
SEE PROFILE
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Prescription drug misuse in Bangalore, India: characteristics and patterns View project
Psychiatry Training View project
All content following this page was uploaded by Debasish Basu on 14 May 2014.
The user has requested enhancement of the downloaded file.
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Indian Journal of
Psychiatry OFFICIAL PUBLICATION OF THE INDIAN PSYCHIATRIC SOCIETY ISSN 0019-5545
Honorary Editor Section Editors Mahendra K. Nepal - Nepal
Swaminath G. Literary psychiatry: Ajit V. Bhide Mario Maj - Italy
Professor and Head, Art and Psychiatry: R. Raguram Mohan K. Issac - Australia
Department of Psychiatry, Pedro Ruiz - USA
Dr. B. R. Ambedkar Medical College,
Cultural Psychiatry: Shiv Gautham
Kadugondanahalli, Bangalore - 560045 The History Page: T. V. Asokan R. Srinivasa Murthy - Jordan
Ph: 080-23152508/23209217 Rohan Ganguli - USA
Mobile: 9845007121 Indian Advisory Board Rudra Prakash- USA
Email: swamyg@sify.com Sanjay Dube- USA
A.B. Ghosh P. Raghurami Reddy Sekhar Saxena- Geneva
Honorary Chief Advisor
A. K. Agarwal P. K. Dalal Sheila Hollins- UK
T. S. Sathyanarayana Rao Abraham Varghese Prasanna Raj
Professor and Head, Tony Elliott- UK
Department of Psychiatry, Ajit V. Bhide R. Ponnudurai Vijoy K Varma- USA
J. S. S. Medical College, Mysore - 570004 Col. G. R. Golechha S.M.Channabasavanna Vikram Patel- UK
Mobile: 9845282399 G. G. Prabhu S. C. Malik
Email: tssrao19@yahoo.com J. W. Sabhaney S. C. Tiwari Distinguished Past Editors
Editorial Office K. Kuruvilla Shridhar Sharma N. N. De 1949 to 1951
Department of Psychiatry, K. A. Kumar Narendra N. Wig L. P. Verma 1951 to 1958
J. S. S. Medical College, Hospital, S. Kalyanasundaram R. Sathianathan A. N. Bardhan 1958 to 1960
Ramanuja Road, Mysore – 570004 P. Kulhara Indira Sharma Lt. Col. M. R. Vachha 1961 to 1967
Ph: 0821 -2653845 Ext 309
Direct: 2442840 (Tele), 0821-2433898 (Fax)
A. Venkoba Rao 1968 to 1976
Email: editor@indianjpsychiatry.org International Advisory Board B. B. Sethi 1977 to 1984
Allan Tasman - USA S. M. Channabasavanna 1985 to 1988
Honorary Associate Editor A. K. Agarwal 1989 to 1992
Roy Abraham Kallivayalil
Anand Pandurangi - USA
Asha Mishra - USA K. Kuruvilla 1993 to 1996
Mob: 9447020020, J. K. Trivedi 1997 to 2002
E-mail: roykalli@gmail.com Bruce Singh - Australia
Utpal Goswami 2003
Dinesh Bhugra - UK
Honorary Deputy Editor T. S. S. Rao 2004
George Christodoulou - Greece Nimesh G. Desai 2005 to 2006
E. Mohandas
Mob: 9447086355 Harischandra Gambheera - Sri Lanka T. S. S. Rao 2007
E-mail: emohandas53@gmail. com Haroon Rashid Chaudhury - Pakistan
Helen Herrman - Australia Statistical Consultants
Editorial Board
J. Sreenivasaraghavan - USA A. K. Prabhakar, Mysore
Ajit Avasti
Behare Prakash Balkrishna
Juan E. Mezzich - USA P. Nagabhushan, Mysore
Chittaranjan Andrade Levent Kuey - Turkey B. S. Ramesh, Mysore
K. S. Jacob
K. S. Shaji
Margoob Mushtaq Ahmed Subscription (total 5 issues).The IJPpublishes original work in all
Nizamie S. Haque Subscribers should contact the ofÞce of the Þelds of Psychiatry. All correspondence including
Sanjay Gupta Honorary Editor, IJP for subscription requests. manuscripts for publication should be sent
Venugopal Jhanwar Annual subscription rates for year 2007 to the Honorary Editor, Indian Journal of
Vinay Kumar
L. S. S. Manickam (Local co-ordinator) (5 issues, postage included) are as follows: Psychiatry, Department of Psychiatry. Dr. B. R.
India Overseas Ambedkar Medical College, Kadugondanahalli,
Journal Committee Institution Rs 3,500 US$ 140 Bangalore - 560045.
Ajai R. Singh A. K. Kala Individual Rs 2,400 US$ 100 E-mail: editor@indianjpsychiatry.org.
B. N. Gangadhar G. Prasad Rao Copyright: @ 2007 The Indian Psychiatric Society.
Govind M. Bang Jayanth Chatterjee Queries from member/non-members about
J. K. Trivedi M. S. Bhatia missing or faulty copies should be addressed Unless so stated, the material in the Indian
Joseph P. Varghese Prathap Tharyan within three months. Payment should be
P. S. V. N Sharma S. M. Agarwal Journal of Psychiatry does not necessarily reßect
S. Nambi Smitha N. Deshpande in the form of Bank Draft in favour of the views of the Editor or the Indian Psychiatric
Shiv Gautham U. C. Garg ‘Honorary Editor, Indian Journal of Psychiatry’, Society. The publishers are not responsible for
Vihang N Vahia payable at Mysore. any error or omission of fact.
Published by Advertisements Correspondence related to
The appearance of advertisements or product/
Medknow Publications on behalf of booking of advertisements should be addressed to services information in the various sections in
Editor, Indian Journal of Psychiatry the editorial ofÞce. the Journal does not constitute an endorsement
A-108/109 Kanara Business Centre,
The Indian Journal of Psychiatry is an ofÞcial or approval by the Journal and/or its publisher
Ghatkopar (E), Mumbai 400075, India.
Phone: 66491818, Fax: 66491817 publication of the Indian Psychiatric Society. It is of the quality or value of the said product or of
E-mail: publishing@medknow.com published quarterly with one additional supplement claims made for it by its manufacturer.
Indian J Psychiatry 49(4), Oct-Dec 2007 305
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Indian Journal of
Psychiatry OFFICIAL PUBLICATION OF THE INDIAN PSYCHIATRIC SOCIETY Volume 49, No. 4, October-December 2007
CONTENTS
EDITOR SPEAKS
They also serve who stand and wait.…: G. Swaminath 227
EDITORIAL
You can lead a horse to the water: G. Swaminath 228
GUEST EDITORIAL
Criminal behavior: A dispassionate look at parental disciplinary practices: T. S. Sathyanarayana Rao 231
AWARD PAPERS
Acute and transient psychosis: A paradigmatic approach: Savita Malhotra 233
Schizophrenia is a disorder of aberrant neurodevelopment: A synthesis of evidence from clinical and structural,
functional and neurochemical brain imaging studies: Ganesan Venkatasubramanian 244
ORIGINAL ARTICLES
A 5-year course of predominantly obsessive vs. mixed subtypes of obsessivecompulsive
disorder: S. B. Math, Jaideep Thoduguli, Y. C. Janardhan Reddy, P. N. Manoj, A. Zutshi, R. P. Rajkumar,
A. M. Adarsh 250
Cannabis-related psychosis: Presentation and effect of abstinence: Vani Kulhalli, Mohan Isaac, Pratima Murthy 256
Pesticide poisoning in non-fatal deliberate self-harm: A public health issue: Study from Sundarban delta, India:
A. N. Chowdhury, Sohini Banerjee, Arabinda Brahma, M. K. Biswas 262
BRIEF COMMUNICATION
Repetitive love proposing: A case report and review of phenomenology of impulsivity and compulsivity:
Narayana Manjunatha, Devvarta Kumar, Haque S. Nizamie 267
REVIEW ARTICLE
Clozapine: Current perspective: Ram K. Solanki, Paramjeet Singh, Mukesh K. Swami 271
COMMENTARY
Proposal to the Indian Psychiatric Society for adopting a specialty section on addiction medicine (alcohol and other
substance abuse): Vivek Benegal, Alok Bajpai, Debasish Basu, Neelam Bohra, Sudipto Chatterji, RB Galgali,
DS Goel, Mohan K Isaac, Venugopal Jhanwar, Rajkumar Lenin, PM Madhavan, AK Mittal, E Mohandas,
Thyloth Murali, Pratima Murthy, Rajesh Nagpal, S Nambi, C Ram Subramaniam, Shubhangi Parkar,
Prasad Rao, MS Reddy, Alok Sarin, TP Sudhakar, BM Tripathi, Matthew Varghese 277
VIEW POINT
Clinical practice guidelines for psychiatrists: Indian Psychiatric Society guidelines vs. international guidelines:
A critical appraisal: Dishanter Goel, Jitendra Kumar Trivedi 283
CASE REPORTS
A case of neuroleptic malignant syndrome induced by olanzapine in postpartum period: Mehmet Üstündağ,
Murat Orak, Cahfer Güloğlu, Mustafa Burak Sayhan, Mahmut Taş 287
Indian J Psychiatry 49(4), Oct-Dec 2007 303
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Mania as an unique life event: Manu Arora, Piyali Mukherjee, Samir Kumar Praharaj, Vinod Kumar Sinha 290
A case presented with ‘‘as if’’ phenomenon: Soumitra Ghosh, Kushal K. Tamuli, Sabita Dihingia 292
LITERARY PSYCHIATRY
Compulsive gambling in ancient Indian texts: Ajit V. Bhide 294
LETTERS TO EDITOR
Rejoinder in reply to critical appraisal on ‘‘factitious schizophrenia’’: Rajnish Raj, Balwant Singh Sidhu 296
More on responsibility of psychiatrists in Indian setting: Prakash Gangdev 298
A rare case of head (scalp) trauma with foreign body: Gurvinder Pal Singh 299
EVENTS AND HAPPENINGS 297
AUTHOR INDEX - 2007 300
TITLE INDEX - 2007 302
The copies of the journal to members of the association are sent by ordinary post. The editorial board, association or publisher will not
be responsible for non-receipt of copies. If any of the members wish to receive the copies by registered post or courier, kindly contact the
journal’s / publisher’s office. If a copy returns due to incomplete, incorrect or changed address of a member on two consecutive occasions,
the names of such members will be deleted from the mailing list of the journal. Providing complete, correct and up-to-date address is the
responsibility of the members. Copies are sent to subscribers and members directly from the publisher’s address; it is illegal to acquire
copies from any other source. If a copy is received for personal use as a member of the association/society, one cannot resale or give-away
the copy for commercial or library use.
304 Indian J Psychiatry 49(4), Oct-Dec 2007
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
COMMENTARY
Proposal to the Indian Psychiatric Society for adopting a specialty section
on addiction medicine (alcohol and other substance abuse)
Vivek Benegal, Alok Bajpai, Debasish Basu, Neelam Bohra, Sudipto Chatterji, RB Galgali, DS Goel, Mohan
K Isaac, Venugopal Jhanwar, Rajkumar Lenin, PM Madhavan, AK Mittal, E Mohandas, Thyloth Murali,
Pratima Murthy, Rajesh Nagpal, S Nambi, C Ram Subramaniam, Shubhangi Parkar, Prasad Rao, MS Reddy,
Alok Sarin, TP Sudhakar, BM Tripathi, Matthew Varghese
Members, Indian Psychiatric Society
The Indian Psychiatric Society, laudably, has a few special overall prevalence of alcohol dependence to be 6.9/1000 for
subsections catering to the advance and development of India, with urban and rural rates of 5.8/1000 and 7.3/1000
certain areas of mental-health care. These are devoted to population. The rates among men and women were 11.9
areas or disciplines which are special to the health of the and 1.7 respectively. It is also well recognized that the
people of India but for historical reasons have not received prevalence rates are not uniform and vary widely within
the attention they deserve and therefore require affirmative the country. The prevalence rates for alcohol- and other
action and special nurturing. substance-use disorders are much higher – for example,
in some of the northeastern states (prevalence of alcohol
This document outlines the need to adopt a similar approach use was above 65% among men and above 50% in Arunachal
to persons with alcohol- and drug-related problems in India Pradesh).[1]
and to create a specialty section on Addiction Medicine,
under the purview of the Indian Psychiatric Society. The figures for prevalence of substance use may at first
appear deceptively small, especially the figures for alcohol
BACKGROUND use, when compared to global estimates; but the absolute
numbers are huge. Also, it is increasingly apparent that
Alcohol, tobacco and other substance abuse affects a the health burden, as well as the social cost attributable
disproportionately large section of people in India to alcohol misuse, is due in greater measure to persons
The current prevalence rates among male adults (i.e., with hazardous use than to persons with dependent use.
subjects who had used within the last 1 month) according Hazardous use has been estimated at over 80 and 55% of all
to the NHS are as follows: alcohol 21.4% [62.5 million]; male and female users respectively.[3]
cannabis 3.0% [8.7 million]; opiates 0.7% [2 million]; any illicit
drug 3.6% [10.5 million]. These numbers, when applied to There is no such comfort of ‘low prevalence’ as far as
the total Indian population of 102.7 crores in 2001, provide tobacco use is concerned. There are currently about 240
prevalence rates of 60/1000, 8/1000 and 2/1000 population million tobacco users aged 15 years and above (195 million
respectively.[1] male users and 45 million female users) in India.[4]
Around 25% of current users were ‘dependent’ users. Prescription drug abuse, especially of sedatives/ hypnotics
Dependent users as a proportion of current users were [0.3 million as per the NHSDAA, 2003], is a growing problem,
17% for alcohol, 26% for cannabis and 22% for opiates. A which has gone largely unrecognized in India. Media reports
meta-analysis by Reddy and Chandrashekar[2] revealed an suggest rising abuse of stimulants by students as awakening
pills (for exams, etc.) or as recreational agents in ‘rave’
Correspondence: Dr. Vivek Benegal,
parties. Then there is the largely unstudied phenomenon
Dept. of Psychiatry, National of Institute of Mental Health and
Neuro Science, Bangalore - 560029, India. of inhalant abuse, which is widely prevalent among ‘hidden
E-mail: vbenegal@gmail.com populations’ such as street children.
How to cite this article: Benegal V, Bajpai A, Basu D, The prevalence is more than that of all severe mental
Bohra N, Chatterji S, Galgali RB, et al. Proposal to the disorders combined
Indian Psychiatric Society for adopting a specialty section on The gravity of the problem of substance-use disorders can
addiction medicine (alcohol and other substance abuse). . be highlighted by comparing their prevalence with that of
Indian J Psychiatry 2007;49:277-82. other psychiatric disorders. Recent studies have generated
Indian J Psychiatry 49(4), Oct-Dec 2007 277
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Benegal, et al.: Speciality section on addiction medicine
all-India prevalence rates for all severe mental disorders of to the entire country, was estimated at Rs. 244 billion
58/1000[2] to 73/1000.[5] for the year 2003–04; whereas the total excise revenues
generated from alcohol manufacture and sales was Rs. 216
The health burden attributable to substance misuse is billion.[20] An earlier study from Karnataka estimated that
inordinately high monetizable direct and indirect costs attributable to people
The impact of a health problem should not be gauged merely with alcohol dependence alone were more than three times
by its prevalence but by the health burden and social cost the profits from alcohol taxation and several times more
that it wreaks on society. Unfortunately, the focus of the than the annual health budget of that state.[21]
professional community, as well as public scrutiny, has been
primarily on the phenomenon of dependence or ‘addiction’ The cost of tobacco-attributable burden of just three groups
in the individual client. In this context, the excessive and of diseases – cancer, heart disease and lung disease – was
problematic use of a drug that is hard for the individual estimated at Rs. 308.33 billion in 2002-2003.[17]
to control becomes the target. The problems caused by,
and associated with, substance use are far broader. They Alcohol and substance dependence/ abuse is very
include problems partly or wholly caused by intoxication, often comorbid with other communicable and
such as injuries and some acute illnesses; long-term effects noncommunicable disorders
on health of a pattern of substance use that does not Axis 1 psychiatric disorders (psychosis, mood disorders,
otherwise disrupt social functioning; acute and chronic anxiety disorders) and substance abuse co-occur more
health problems caused by unsafe ways of using drugs frequently than can be explained by chance alone. Patients
otherwise unrelated to pharmacological effects (e.g., using with schizophrenia are 4.6 times more likely to have
dirty needles); impacts on other people (e.g., secondhand substance-use disorders than persons without mental
smoke); and impacts of the criminal justice system on illness (3 times higher for alcohol, 6 times higher for other
people engaging in illegal behavior. illicit drugs).[22] While it has been previously commonly held
that substance-use comorbidity in schizophrenia represents
Alcohol- and tobacco-related problems in India self-medication, an attempt by patients to alleviate adverse
Hospital admission rates due to the adverse effects of positive and negative symptoms, cognitive impairment
alcohol consumption are disproportionately high. Several or medication side effects; recent advances suggest that
studies indicate that nearly 20–30% of admissions/ increased vulnerability to addictive behavior may reflect
consultations are due to alcohol-related problems (direct the impact of the neuropathology of schizophrenia on the
or indirect) in different health-care settings but are neural circuitry mediating drug reward and reinforcement.
under-recognized by primary-care physicians.[6,7] Alcohol Thus, schizophrenic patients may have a predilection for
misuse has been implicated in over 20% of traumatic brain addictive behavior as a primary disease symptom in parallel
injuries[8]and 60% of all injuries reporting to emergency to, and in many cases independent from, their other
rooms.[9] It has a disproportionately high association symptoms. There is also early evidence that the pathology
with deliberate self-harm,[10] high-risk sexual behavior,[11] in the neurobiological substrates that underlie mood and
HIV infection, tuberculosis,[12] esophageal cancer,[13] liver anxiety disorders also subserves the predisposition to
disease[14] and duodenal ulcer.[15] A recent estimate from substance-use problems.[23]
surveillance of major noncommunicable diseases in India
placed the burden due to alcohol as the numero uno among Substance abuse, especially of alcohol and tobacco, and a
all noncommunicable disorders.[16] spectrum of high-risk behaviors , which often go together,
are common risk factors for most of the noncommunicable
There are 700,000 deaths per year due to smoking and disorders (like hypertension, diabetes, heart disease,
800,000 to 900,000 per year due to all forms of tobacco cancer), which are assuming increasingly larger proportions
use/ exposure in India. For the next 20 years, there will be a of the health burden on the Indian society.[3]
faster trajectory of rise in tobacco-related deaths. Many of
the deaths (>50%) will occur below 70 years of age.[17] Drug abuse and addiction also have tremendous implications
for the health of the public, since drug use, directly or
The social cost due to alcohol- and tobacco-related problems indirectly, is now seen as a major vector for the transmission
is prohibitively high. of many serious infectious diseases, particularly HIV/ AIDS,
hepatitis and tuberculosis; and is instrumental in one of the
Alcohol misuse wreaks a high social cost. In addition to the largest sources of mortality and morbidity in India, namely,
health costs, there are indirect costs linked to a wide variety road traffic accidents and violence.[20]
of social implications (family disruption, marital disharmony,
impact on development of children, deprivation of the family, Substance use disorders, especially involving alcohol and
absenteeism and industrial loss, crime and violence, etc.).[18– tobacco, are grave public health problems
20]
The social cost attributable to alcohol use, extrapolated It obviously follows from the above statements that
278 Indian J Psychiatry 49(4), Oct-Dec 2007
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Benegal, et al.: Speciality section on addiction medicine
substance-use disorders need to be recognized as public experiences gained from the successes and mistakes of the
health problems and that there is urgency for psychiatrists community psychiatry movement in India.
to liaise with other medical specialties, the public health
delivery system, as well as organizations working in the Substance-use disorders constitute a large proportion
area of development. As specialists in bio-behavioral of the clinical load in both private and public-health
disorders, psychiatrists are in an ideal position to do so, and psychiatric practice
the problem requires the involvement of diverse medical Substance-use disorders already form more than 20% of the
professionals. case load of psychiatric practitioners, often, as noted above,
inextricably associated with mood, anxiety and psychotic
Here, one needs to exercise caution and steer clear of disorders. However, as a recent piquant exchange on a
the ‘me-too’ syndrome, wherein one creates a specialized popular Indian psychiatrists’ bulletin board revealed, many
discipline which clamors for an independent share of psychiatrists are loath to take on clients with substance-
limited health-care resources. It would be prudent for use disorders, preferring to refer them on to a very short
the psychiatrist community to work in tandem with, and list of colleagues who will see them. This is often related
to juxtapose its strength and skill-sets with, the existing to a feeling of helplessness and frustration faced with the
networks and delivery systems for communicable and usual picture of recidivism that typifies the natural history
noncommunicable disorders. of persons with alcohol and drug disorders.
Addiction medication is an area where the psychiatrist can Practitioners have an attitude of therapeutic nihilism
fruitfully work in tandem with other medical specialists, and towards addiction medicine and the addicted patient
in some ways this will be a good medium to get psychiatry These experiences translate into an attitude of therapeutic
into the mainstream. So the advantage can be mutual. nihilism, which unfortunately is widely prevalent across the
medical community. There are several factors which appear
Alcohol and tobacco use are also strongly affected by the to contribute to this way of thinking:
economic and political compulsions of the day. One needs
to only look at the recent imbroglio over the issue of scary Lack of education about alcohol and substance abuse: Only a
pictures of consequences of tobacco use on cigarette packs very small portion of the undergraduate medical syllabus,
and the subsequent backtracking by the Ministry of Health and even the postgraduate psychiatry syllabus, is devoted to
in the face of pressure from the tobacco lobby.[24] Similarly, this area, and it is limited only to the medical complications
the pursuit of a rational alcohol policy has been vitiated by of alcoholism.
economic compulsions of the states and the misdirected
coercion of market economics. Thus, there is very little Negative attitudes about alcoholism: Physicians and
debate on the recent active moves of the grape-growers’ psychiatrists in training often see late-stage alcoholics, who
lobby to have the Finance Ministry re-designate wine as an often evoke feelings of aversion, hostility and helplessness.
agricultural product. Some physicians tend to see alcoholics and drug addicts as
bad or morally weak.
Macro-level interventions in these domains are likely to
be more effective and cost-effective. Intensive advocacy at Discomfort with related social issues: Since alcoholism involves
several levels should therefore be a part of any endeavor in not just medical issues but significant psycho-social issues
this area. The Framework Convention on Tobacco Control also, many physicians are uncomfortable dealing with it.
(FCTC) is a classic example and could provide the template
for such initiatives at the national/ international level. The Pessimism about treatment: There are many physicians who
negative economics of addictions (e.g., the social costs feel that addiction is not treatable. Part of the helplessness
of alcohol and tobacco overshadowing tax revenues from and pessimism occurs because of the experience with
these commodities) must be carefully articulated as these late-stage problem drinkers, where the treatment is not
are potent advocacy tools. It is also necessary to examine always successful. The physician must remember that
and publicize the cost-effectiveness of interventions to early detection of, and intervention to resolve, alcohol-,
control substance abuse . The role of the industry and its tobacco- and other substance-related problems offers the
vested interests (e.g., the powerful liquor and tobacco best results.
lobbies), as well as the complicity of medical professionals
and pharmacists (as in benzodiazepine and other over-the- It is not surprising, then, that the field of addiction psychiatry
counter–medication misuse), should also be a focus of any currently suffers the same pariah status that psychiatry was
remedial strategies. once ‘favored’ with among other medical professionals. The
drug rehabilitation centers of the early 21st century often
The psychiatric community is specially equipped to provide serve the same function that the leprosaria and asylums of
leadership to such activities and bring to bear the valuable the early 20th century did: seclusion and restraint!
Indian J Psychiatry 49(4), Oct-Dec 2007 279
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Benegal, et al.: Speciality section on addiction medicine
Leadership in the field of advocacy and policy making or learning, judgment, reward and motivation (possibly due to
legislation has been ceded to nonmedical, nonpsychiatric a maturational lag affecting myelination). This may result in
bodies a trait of central nervous system hyperexcitability, usually
To a large extent, this pessimism also arises from the fact manifest as a spectrum of externalizing behaviors marked
that till lately, there have not been too many effective by compromised impulse control, high novelty-seeking or
treatments. Here one must invoke the late Abraham Maslow, sensation-seeking behavior, increased response to reward,
who famously said: “If your only tool is a hammer, all your a tendency to pay more attention to immediate rewards
problems look like nails!” For far too long, treatment and neglect long-term outcomes when making decisions,
strategies have been limited by a single-hammer model reduced response to punishment and a disregard for social
dominated by an abstinence paradigm and equipped with norms. This is associated with heightened reinforcement
limited behavioral-change strategies. from alcohol and drugs coupled with impaired early warning
of intoxication. A significant portion of this research has
Unconscionably, physicians in frustration have attempted to come out of India! In effect then, drug dependence, in
curb the uncontrollable behaviors of persons with drug and large part, may be the epiphenomenon of, or a variable
alcohol problems with antipsychotics and electroconvulsive expression of, a generalized disinhibitory complex, which
therapies. This has only served to alienate them from this has been hypothesized to predispose to mood disorder,
client group. One has only to attend a survivors’ group anxiety disorder and perhaps schizophrenia! Susceptible
meeting to realize the hostility that psychiatrists in general individuals may be self-medicating themselves and initially
are viewed with. even successfully reversing, or compensating for, their low
motivational responses to normal rewards.[25]
Not surprisingly, the onus of treating these clients has
shifted either to survivor groups like the Alcoholics This is important to assert; because, for far too long,
Anonymous and Narcotics Anonymous; or to nonmedical, despite the lip service paid to the medical and bio-psycho-
nonpsychiatric rehabilitation agencies. Unsurprisingly, the social model of alcohol and other substance dependence,
leadership in the field of advocacy and policy making or practitioners have rarely been able to distance themselves
legislation in the area has also been ceded to nonmedical, from the prevalent social discourse which regards drug users
nonpsychiatric bodies. through the lenses of the moral model as ‘losers – who are
too weak to stop and who deserve what they get!’
One needs to mention here that the standards of treatment
of clients with addictive disorders are variable, at best. Also, the growing literature on the long-lasting neuro-
The various agencies involved differ widely in the methods adaptations consequent to prolonged exposure to substances
they utilize and in a mostly unregulated field; there are of abuse is beginning to delineate the neuropathology that
numerous instances of clients being subjected to practices gives rise to the characteristic behavioral changes which
which are questionable, at best, and often highly unethical account for the recurring and relapsing nature of the illness.
and dangerous. Slowly, these advances from the laboratory benches are being
translated into changes in behavioral and pharmacological
It is incumbent upon the members of the society to use strategies for more efficacious treatment. There are recent
their collective influence to bring some regulation and reports on the efficacy of newer pharmacological agents
standardization of procedures into the field, being guided by and audits of individual and population-level interventions
evidence . A good point to start from is the documentation which are more efficacious than earlier remedies.[26–28]
on treatment protocols that the society has previously A special and concerted effort is required to test and
generated, as well as the guidelines generated by the document these interventions and make them broad based,
ministries of Health and Social Justice and Welfare. while at the same time bringing them into public notice.
Addictive disorders are bio-behavioral disorders which And the community of psychiatrists is well positioned
are strongly impacted by economic and political to spearhead these efforts at advancing the study of the
influences bio-behavioral determinants of this array of disorders and
However, one needs to assert here that psychiatrists, incorporating the opportunities derived from research into
because of their training as bio-behavioral specialists, are day-to-day practice.
best positioned to coordinate the management of this array
of problems. Increasingly, these recurrent and relapsing Addiction medicine is a prominent and active subsection
illnesses are being recognized to be a resultant of the in most international psychiatric bodies
unfortunate pairing of substance use with a neurobiological It is instructive to look at the status of addiction medicine,
diathesis modulated by environmental influences. Recent within the structure of other international psychiatric bodies.
studies have demonstrated that susceptible individuals In the USA, for example, doctors focusing on addiction
have smaller volumes in brain areas critical for attention, medicine are medical specialists who focus on addictive
280 Indian J Psychiatry 49(4), Oct-Dec 2007
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Benegal, et al.: Speciality section on addiction medicine
disease and have had special study and training focusing on use disorders are often common to, and frequently
the prevention and treatment of such diseases. There are complicate, the development and outcome of a whole
two routes to specialization in the addiction field: one via host of medical disorders and social ills. Synergizing
a psychiatric pathway and the other outside of psychiatry. with other stakeholders mentioned above, in sharing
The American Society of Addiction Medicine notes that of methodologies, will strengthen each other’s effort to
approximately 40% of its members are psychiatrists, while mutually benefit both in terms of intervention impact
the remainder has received medical training in other fields. as well as the collective bargaining power to advocate
change. Such co-action will also reduce the competing
The facts stated above underline the urgent need for the and conflicting ‘me-too’ demands stemming from parallel
Indian Psychiatric Society to constitute a specialty section agencies working towards similar ends, which overwhelm
(with appropriate regional representation) devoted to limited resources of finance and manpower and weaken
Addiction Medicine, within its ambit. the effectiveness of the discourse for change;
AIMS AND OBJECTIVES • Formulate and recommend standards of treatment and
rehabilitation of persons or populations affected directly
The specialty section on Addiction Medicine will be or indirectly by substance-use disorders. In addition, it
required to: will be necessary to obtain recommendations for syllabi
• Promote and advance the bio-psycho-social contributions and commission resources for the education and training
to the science and practice of Addiction Medicine in all of medical and nonmedical personnel involved in the
its different manifestations; field;
• Promote a] the improvement of the health of persons • Safeguard the interest of psychiatrists and fellow
directly or indirectly impacted by alcohol- and other professionals engaged in the practice of Addiction
substance-related problems and b] prevention, control, Medicine in India and promote ethical standards in the
treatment and relief of all alcohol- and other substance- practice of Addiction Medicine in India; and
related problems, as well as conditions which constitute
high risk for potential drug- and alcohol-related problems. • Promote research in the field of addiction science
This involves encouraging and enabling members of the with a focus on translating the benefits of research to
society to explore, extend and pursue ‘evidence-based’ the bedside and propagate the use of evidence-based
treatment strategies and prevention methods. This interventions in the daily delivery of mental-health care.
includes liaison with other stakeholders, including, but
not limited to, a] governmental agencies overseeing SUGGESTED ACTIVITIES
health, social justice and welfare, finance and human
development; b] nongovernmental agencies involved in 1. A web portal, linked to the web page of the Indian
direct care of persons with substance abuse, as well as Psychiatric Society, which will initially host information
agencies whose developmental programs are impacted of relevance to the practice of Addiction Medicine in
unfavorably by substance-abuse problems directly or India, with direct and indirect links to published or
indirectly, affecting their beneficiaries; and c] other unpublished scientific papers, databases, treatment
medical specialties and primary health-care providers. protocols, available treatment agencies, online resources,
This also requires sharing the expertise of members of etc.; and later, e-learning sites for online education and
the society and other professionals involved in diverse training.
fields such as school mental health, community-based
rehabilitation, epidemiology, drug trials, maintaining 2. Coordinating Continuing Medical Education (CME)
disease registries, to name just a few; pertaining to the aspect of the science and practice
of Addiction Medicine, with special emphasis on
• Actively engage in advocacy in order to influence policy underserved areas like the northeastern states, Andaman
making and legislation, keeping in mind that substance- and Nicobar Islands, etc.
use disorders and their consequences constitute a grave
public health disorder which imposes an unacceptably 3. Enabling and commissioning position papers on the
severe burden on the health and well-being of the impact of substance abuse in India, with a view to
people of India. This, above all, requires consistent influence public policy.
accumulation and dissemination of data on the
economic, social and health costs of substance abuse to 4. Engaging with relevant organizations to promote
the Indian society; and on the evidence of cost-efficacy of demand-reduction strategies, such as the police to
appropriate intervention. There is emerging conviction prevent drinking and driving, primary health providers
that the risk factors and consequences of substance- and emergency rooms for early detection and brief
Indian J Psychiatry 49(4), Oct-Dec 2007 281
[Downloaded free from http://www.indianjpsychiatry.org on Friday, October 15, 2010, IP: 59.94.246.251]
Benegal, et al.: Speciality section on addiction medicine
intervention. 10. Gururaj G, Isaac M. Epidemiology of suicides in Bangalore city. NIMHANS
Publication Gururaj, G. and Isaac, M. Epidemiology of Suicides in
Bangalore City. NIMHANS Publication: Bangalore; 2001. p. 34,43.
5. Pursuing the aim of working to safeguard vulnerable 11. Chandra PS, Krishna VA, Benegal V, Ramakrishna J. High-risk sexual
behaviour and sensation seeking among heavy alcohol users. Indian J
populations, e.g., inoculating children and adolescents Med Res 2003;117:88-92.
through skills training ; sensitizing physicians and 12. Rajeswari R, Chandrasekaran V, Suhadev M, Sivasubramaniam S, Sudha
pharmacists to prevent over-the-counter drug abuse, G, Renu, G. Factors associated with patient and health system delays in
the diagnosis of tuberculosis in South India. Int J Tuberculosis Lung Disord
especially for the elderly. 2002;6:789-95.
13. Chitra S, Ashok L, Anand L, Srinivasan V, Jayanthi V. Risk factors for
esophageal cancer in Coimbatore, southern India: A hospital-based case-
6. Examining the possibility of creating a national registry, control study. Indian J Gastroenterol 2004;23:117-8.
using standardized data-entry protocols. 14. Sarin SK, Bhatt A, Malhotra V, Sachdev G, Jiloha RC, Munjal GC. Pattern
of alcohol-related liver disease in dependent alcoholics: the Indian
dimension. Br J Addict 1988;83:279-84.
The proposal to constitute a specialty section on Addiction 15. Jain A, Buddhiraja S, Khurana B, Singhal R, Nair D, Arora P, et al. Risk
Medicine was first mooted by Dr. Varghese Punoose at the factors for duodenal ulcer in north India. Trop Gastroenterol 1999;20:36-
9.
IPS South Zone CME program at Kodaikanal in 2007. It was 16. Anand K. Assessment of burden and surveillance of major
seconded by Dr. M. S. Reddy and received enthusiastically noncommunicable diseases in India. World Health Organization (WHO),
South East Asia Regional Office, Workshop Document: New Delhi; 2000.
by the IPS President, Dr. I. R. S. Reddy. This document is 17. Reddy KS. Success of tobacco control in India: Research as a lever for
in continuation of that process; and we urge the Society public policy (Presentation at the Global Forum for Health 9. Internet
document. 2005. Available from: http://www.globalforumhealth.org/
to place the document before the appropriate body, to filesupld/forum9/CD%20Forum%209/papers/Reddy%20KS.pdf [Last
initiate the necessary processes so that the Society may accessed on 2007 Dec 10].
further debate and hopefully set in motion the steps to give 18. Bhatt RV. Domestic violence and substance abuse. Int J Gynaecol Obstet
1998;63:25-31.
substance to this proposal. 19. Rao KN, Begum S, Venkataramana V, Gangadharappa N. Nutritional
neglect and physical abuse in children of alcoholics. Indian J Pediatr
2001;68:843-5.
REFERENCES 20. Gururaj G, Girish N, Benegal V. Alcohol Control Series1: Burden and
Socio-Economic Impact of Alcohol - The Bangalore Study. World health
1. Ray R, Mondal AB, Gupta K, Chatterjee A, Bajaj P. The Extent, Pattern Organisation, Regional Office for South East Asia: New Delhi; 2006 (ISBN
and Trends of Drug Abuse in India: National Survey. United Nations Office 92 9022 2727).
on Drugs and Crimes and Ministry of Social Justice and Empowerment, 21. Benegal V, Velayudhan A, Jain S. Social costs of alcoholism: A Karnataka
Government of India: New Delhi; 2004. perspective. NIMHANS Jr 2000;18:6-7.
2. Reddy MV, Chandrashekar CR. Prevalence of mental and behavioral 22. Jagadeesha T, Benegal V. Psychosis among substance users. Curr Opin
disorders in India: A meta-analysis. Indian J Psychiatry 1998;40:149-57. Psychiatry 2006;19:239-45.
3. Benegal V. India:Alcohol and Public health (Invited Editorial). Addiction 23. Chambers R. A neurobiological basis for substance abuse comorbidity in
2005;100:1051-6. schizophrenia. Biol Psychiatry 2001;50:71-83.
4. Mini GK. Socioeconomic and demographic correlates of tobacco use and 24. Sinha K. Gory images on cigarette packets. Times of India 2007.
alcoholic consumption among Indian women. Indian J Community Med Available from: http://timesofindia.indiatimes.com/India/Gory_images_
2007;32:150-1. on_cigarette_packets/articleshow/2278867.cms [Last accessed on 2007
5. Ganguli HC. Epidemiological finding on prevalence of mental disorders in Dec 10].
India. Indian J Psychiatry 2000;42:14-20 25. Benegal V, Venkatsubramanian GV, Antony G, Jaykumar PN. Differences
6. Sri EV, Raguram R, Srivastava M. Alcohol problems in a general hospital: in brain morphology between subjects at high and low risk for alcoholism.
A prevalence study. J Indian Med Assoc 1997;95:505-6. Addict Biol 2007;12:122-32.
7. Benegal VA, Shantala Murthy P, Janakiramaiah N. Report on Development 26. Hawks D, Scott K, McBride N, Jones P, Stockwell T. Prevention of
of a Model District Programme for Prevention of Drug and Alcohol Psychoactive Substance Use. A Selected Review of What Works in the
Problems: WHO-NIMHANS Project [monograph on the Internet]. 2001. Area of Prevention. World Health Organization: Geneva; 2002.
Available from: http://www.nimhans.kar.nic.in/deaddiction/lit/mandya_ 27. Garbutt JC, Flannery B. Baclofen for alcoholism. Lancet 2007;370:1884-
distt_who.pdf. [Last accessed on 2007 Dec 10]. 5.
8. Gururaj G. Epidemiology of traumatic brain injuries: Indian scenario. 28. Muralidharan K, Rajkumar RP, Mulla U, Kayak RB, Benegal V. Baclofen in
Neurol Res 2002;24:24-8. the management of inhalant withdrawal: A case series. J Clin Psychiatry
9. Benegal V, Gururaj G, Murthy P. Project Report on a WHO Multi Primary Care Companion [In press].
Centre Collaborative Project On Establishing and Monitoring Alcohol’s
Involvement in Casualties; 2002. [Monograph on the Internet]. Available
from: http://www.nimhans.kar.nic.in/deaddiction/lit/alcohol%20and%20% Source of Support: Nil, Conflict of Interest: None declared
20injuries_who%20collab.pdf. [Last accessed 2007 Dec 10].
282 Indian J Psychiatry 49(4), Oct-Dec 2007
View publication stats
You might also like
- A Matter of Health - Rama KrishnaDocument1,205 pagesA Matter of Health - Rama Krishnaswoop1_100% (10)
- Critical Care Nursing A Holistic Approach 10th Edition Morton Test Bank PDFDocument6 pagesCritical Care Nursing A Holistic Approach 10th Edition Morton Test Bank PDFa806088253No ratings yet
- Adv. Social Psy Current Trends in Social Psychology and Ethical IssuesDocument29 pagesAdv. Social Psy Current Trends in Social Psychology and Ethical IssueskhadijaNo ratings yet
- A Thesis of Compilation of Research Pape PDFDocument632 pagesA Thesis of Compilation of Research Pape PDFNico RotaNo ratings yet
- ConferenceDocument12 pagesConferenceLokesh VishwakarmaNo ratings yet
- Journal Vol 6Document103 pagesJournal Vol 6Suellen Concessio FernandesNo ratings yet
- Yoga Vijnana Vol. 2Document71 pagesYoga Vijnana Vol. 2Dado MottaNo ratings yet
- Academic Rules N Procedures-8!3!22Document228 pagesAcademic Rules N Procedures-8!3!22STEP TO MEDICOSNo ratings yet
- IPSCPGSUDSynopsisBook2015 PDFDocument130 pagesIPSCPGSUDSynopsisBook2015 PDFSarbartha PramanikNo ratings yet
- Gerontology: Indian Journal ofDocument180 pagesGerontology: Indian Journal ofBala RajNo ratings yet
- Ros DirectoryDocument220 pagesRos DirectoryManoj KashyapNo ratings yet
- December 2021Document71 pagesDecember 2021Aghisna AmaliaputriNo ratings yet
- AstrologyDocument196 pagesAstrologySameer Rane100% (3)
- Oedipus The Deep Rooted Reality To HomosexualityDocument136 pagesOedipus The Deep Rooted Reality To HomosexualitySonali DeNo ratings yet
- Screenshot 2023-07-22 at 21.06.12Document28 pagesScreenshot 2023-07-22 at 21.06.12ariNo ratings yet
- I PSC PG Sud Comprehensive 2014Document531 pagesI PSC PG Sud Comprehensive 2014Kishore KumarNo ratings yet
- Tila Tail A Shiro Ab Hyang ADocument193 pagesTila Tail A Shiro Ab Hyang ARahul KhaliNo ratings yet
- Researchers World Vol. VIII, Issue 2 (7) - April - 2017 - P7Document132 pagesResearchers World Vol. VIII, Issue 2 (7) - April - 2017 - P7Sangeeta MittalNo ratings yet
- Estern Journal of PsychiatryDocument124 pagesEstern Journal of PsychiatryDr. Ranjan KumarNo ratings yet
- Sunil v. Joshi. Ayurveda and Panchakarma The Science of Healing and RejuvenationDocument317 pagesSunil v. Joshi. Ayurveda and Panchakarma The Science of Healing and RejuvenationSiren100% (11)
- Full PDF - Forensic MedicineDocument97 pagesFull PDF - Forensic MedicineStephen RatumoNo ratings yet
- Ojolhns 10 Issue II Dec 2016 ColorDocument66 pagesOjolhns 10 Issue II Dec 2016 ColorAnonymous ST1Ot2GAHxNo ratings yet
- Fortune Select Grand Ridge HotelDocument6 pagesFortune Select Grand Ridge HotelMohammad NasirNo ratings yet
- Effectiveness of Cognitive Behavioural and Relational Approaches in Sexual Disorder 60-69Document100 pagesEffectiveness of Cognitive Behavioural and Relational Approaches in Sexual Disorder 60-69iswarya vellaisamyNo ratings yet
- JPPvol 3 No 23Document104 pagesJPPvol 3 No 23SrishtyNo ratings yet
- AIIA JournalApril June 2019Document52 pagesAIIA JournalApril June 2019Rajesh7358No ratings yet
- UntitledDocument72 pagesUntitledKamaldeep SinghNo ratings yet
- A Yu Care Issue 12017Document53 pagesA Yu Care Issue 12017gopal08No ratings yet
- List of IPC MembersDocument59 pagesList of IPC Membersabhaybittu100% (1)
- CV Rabinarayan AcharyaDocument29 pagesCV Rabinarayan AcharyaMSKC100% (1)
- Gurbani Cured CancerDocument3 pagesGurbani Cured CancerSimrandeep Singh100% (1)
- Åyurvedic Check-List: Chaukhambha OrientaliaDocument114 pagesÅyurvedic Check-List: Chaukhambha OrientaliaNirav TrivediNo ratings yet
- Åyurvedic Check-List: Chaukhambha OrientaliaDocument114 pagesÅyurvedic Check-List: Chaukhambha OrientaliaNirav TrivediNo ratings yet
- Ijavol 5no 3sep-Dec20161Document161 pagesIjavol 5no 3sep-Dec20161Ayesha JadoonNo ratings yet
- 34 Jan 2011 PDFDocument136 pages34 Jan 2011 PDFNikita JoshiNo ratings yet
- Miracle of GurbaniDocument4 pagesMiracle of Gurbanijack_danielzNo ratings yet
- Teaching Staff ListDocument30 pagesTeaching Staff ListArth ArnavNo ratings yet
- National Webinar On Yoga Day, 21st June, 2021Document3 pagesNational Webinar On Yoga Day, 21st June, 2021NdjxnfNo ratings yet
- Training Models in IndiaDocument9 pagesTraining Models in Indiakimxyx.dNo ratings yet
- Gala Dhiren - Be Your Own Doctor With Acupressure PDFDocument139 pagesGala Dhiren - Be Your Own Doctor With Acupressure PDFbosesubrata100% (5)
- ULHASDocument6 pagesULHASVi LinhNo ratings yet
- 1000 Plus Psychiatry MCQ Book DranilkakunjeDocument141 pages1000 Plus Psychiatry MCQ Book DranilkakunjeChatura UdharaNo ratings yet
- Daftar Pustaka: Pitaka/suttavibhangaDocument7 pagesDaftar Pustaka: Pitaka/suttavibhangaHendry KurniawanNo ratings yet
- Icmp BrochureDocument21 pagesIcmp BrochureDhruv PatelNo ratings yet
- Somatoform Disorder - Current Concept and ControversiesDocument55 pagesSomatoform Disorder - Current Concept and ControversiesDhrubajyoti BhuyanNo ratings yet
- Bio DataDocument1 pageBio DataShashi_kantNo ratings yet
- Bharat Ayurved Medical College, Hospital & Research Centre, Roorkee Road, NH-58, P.O. Barla, Muzaffarnagar, Uttar PradeshDocument6 pagesBharat Ayurved Medical College, Hospital & Research Centre, Roorkee Road, NH-58, P.O. Barla, Muzaffarnagar, Uttar PradeshuttuttimailNo ratings yet
- AyuCaRe Vol 1 Issue 1Document52 pagesAyuCaRe Vol 1 Issue 1Priyanka SharmaNo ratings yet
- CV Amit KaushikDocument8 pagesCV Amit Kaushikbharrani shankarNo ratings yet
- 19-Article Text-62-1-10-20180126Document2 pages19-Article Text-62-1-10-20180126Minerva Medical Treatment Pvt LtdNo ratings yet
- Ayurveda Vol. 8 Issue No. 2 April June 2013Document68 pagesAyurveda Vol. 8 Issue No. 2 April June 2013Anonymous A3vTUVNo ratings yet
- 038 Health In1 PDFDocument281 pages038 Health In1 PDFbhatchinmay7100% (1)
- Reducing Adolescents Mental Stress Via Motivational Role Key PDFDocument151 pagesReducing Adolescents Mental Stress Via Motivational Role Key PDFNazeer AhmadNo ratings yet
- Edoc - Pub 003-Acupressure PDFDocument151 pagesEdoc - Pub 003-Acupressure PDFNiki MavrakiNo ratings yet
- Yoga Vijnana Vol. 1Document84 pagesYoga Vijnana Vol. 1Artos100% (1)
- WHD Iapsm Quiz Preliminary RoundDocument2 pagesWHD Iapsm Quiz Preliminary RoundMazin Mohsen ali almolikyNo ratings yet
- Systematic Review and Meta AnalysisDocument100 pagesSystematic Review and Meta AnalysisĐạt HuỳnhNo ratings yet
- 767 Thesis-0812 PDFDocument196 pages767 Thesis-0812 PDFRahimshaikhNo ratings yet
- Textbook of Tuberculosis SampleDocument23 pagesTextbook of Tuberculosis Sampleanshumanshinde12040No ratings yet
- Ayurveda For All: Effective ayurvedic self cure for common and chronic ailmentsFrom EverandAyurveda For All: Effective ayurvedic self cure for common and chronic ailmentsRating: 4 out of 5 stars4/5 (2)
- Join Hands-2014Document14 pagesJoin Hands-2014faradayzzzNo ratings yet
- Smilebeggary 1Document10 pagesSmilebeggary 1faradayzzzNo ratings yet
- 14 of 1987 Central Rules (E)Document25 pages14 of 1987 Central Rules (E)faradayzzzNo ratings yet
- Aap NmbaDocument27 pagesAap NmbafaradayzzzNo ratings yet
- Open Record ViewDocument161 pagesOpen Record ViewfaradayzzzNo ratings yet
- Neurobiology Research Findings: How The Brain Works During ReadingDocument18 pagesNeurobiology Research Findings: How The Brain Works During ReadingfaradayzzzNo ratings yet
- Oil PalmDocument131 pagesOil PalmfaradayzzzNo ratings yet
- Appendix B: Business Plan Template: Applied Health StrategiesDocument34 pagesAppendix B: Business Plan Template: Applied Health StrategiesfaradayzzzNo ratings yet
- 3UBHT Integrated Business Plan v5.2Document184 pages3UBHT Integrated Business Plan v5.2faradayzzzNo ratings yet
- Start Up Business PlanDocument16 pagesStart Up Business PlanfaradayzzzNo ratings yet
- Training Schedule For 2016: Month Course Start Date IGC 1 Exam IGC 2 Exam Location Tutor MarketingDocument1 pageTraining Schedule For 2016: Month Course Start Date IGC 1 Exam IGC 2 Exam Location Tutor MarketingfaradayzzzNo ratings yet
- GSP Company ListDocument57 pagesGSP Company ListfaradayzzzNo ratings yet
- Web ContentDocument3 pagesWeb ContentfaradayzzzNo ratings yet
- Character Building FrameworkDocument6 pagesCharacter Building FrameworkfaradayzzzNo ratings yet
- Safety Culture AssesmentDocument2 pagesSafety Culture AssesmentfaradayzzzNo ratings yet
- Daba Abdissa, Tesfaye Adugna, Urge Gerema, and Diriba DerejeDocument6 pagesDaba Abdissa, Tesfaye Adugna, Urge Gerema, and Diriba DerejeIstiqomahsejatiNo ratings yet
- To Remove & Reinstall Heat Insulation Cover 350Document7 pagesTo Remove & Reinstall Heat Insulation Cover 350Saleem AkhtarNo ratings yet
- 2021-04-15 St. Mary's County TimesDocument40 pages2021-04-15 St. Mary's County TimesSouthern Maryland Online100% (1)
- Large Databases in Anaesthesiology: ReviewDocument6 pagesLarge Databases in Anaesthesiology: ReviewSoumya DasNo ratings yet
- CRISC Exam - Secrets of Passing Exam in First AttemptDocument13 pagesCRISC Exam - Secrets of Passing Exam in First AttemptPractise-Test57% (7)
- Las 7 First QuarterDocument3 pagesLas 7 First QuarterKirby FuentesNo ratings yet
- Week 2 (Lec-Lab) Mls 306 Clinical Parasitology Bsmls 3A: Ascaris LumbricoidesDocument4 pagesWeek 2 (Lec-Lab) Mls 306 Clinical Parasitology Bsmls 3A: Ascaris LumbricoidesHannah Beatrice Adame TamayoNo ratings yet
- Quizlet PDFDocument4 pagesQuizlet PDFsgkismetNo ratings yet
- Inroduction To Homoeopathic Materia Medica 2023Document10 pagesInroduction To Homoeopathic Materia Medica 2023mahitha sujithNo ratings yet
- Definisi, Etiologi GNAPSDocument6 pagesDefinisi, Etiologi GNAPSSitiMaghfirahHafizNo ratings yet
- Form Dokter 2020Document14 pagesForm Dokter 2020Sugi WilliamNo ratings yet
- Proximal BicepsDocument23 pagesProximal BicepsPrabath ChinthakaNo ratings yet
- Discovery Studio 2016 Help - Theory - ADMET DescriptorsDocument10 pagesDiscovery Studio 2016 Help - Theory - ADMET Descriptorssyahrul imranNo ratings yet
- My One Night Stand With CancerDocument5 pagesMy One Night Stand With CancerSydney RoslinNo ratings yet
- Group Health TeachingDocument7 pagesGroup Health TeachingKshitij Gaurav RaizadaNo ratings yet
- SDS Oli TrafoDocument10 pagesSDS Oli TrafoVaderFistNo ratings yet
- Sex Work Doesn't Come With A Beginner's ManualDocument156 pagesSex Work Doesn't Come With A Beginner's ManualAndrea LaraNo ratings yet
- Surgeon General's Workshop On Women's Mental HealthDocument93 pagesSurgeon General's Workshop On Women's Mental HealthHollie1230100% (3)
- PT1A - Salvadora, N. Assignment 1Document2 pagesPT1A - Salvadora, N. Assignment 1N.No ratings yet
- Nigeria Gyts 2008Document39 pagesNigeria Gyts 2008aimanNo ratings yet
- DokumenPSSR PDFDocument26 pagesDokumenPSSR PDFAssya MohammedNo ratings yet
- DR Maliha Hashmi: ContactDocument1 pageDR Maliha Hashmi: Contactnemoo80 nemoo90No ratings yet
- Proc No 513 Solid Waste Management Proclamation DownloadDocument8 pagesProc No 513 Solid Waste Management Proclamation DownloadephremNo ratings yet
- Environmental AND Social Management Plan: Nepal Electricity AuthorityDocument113 pagesEnvironmental AND Social Management Plan: Nepal Electricity AuthoritySubesh JoshiNo ratings yet
- Suturat Apo QepjetDocument62 pagesSuturat Apo QepjetAnonymous 3LOvwPNo ratings yet
- A Rhetorical Analysis of Pharmaceutical AdvertisingDocument45 pagesA Rhetorical Analysis of Pharmaceutical AdvertisingAgnes MalkinsonNo ratings yet
- Freud's Structural and Topographical Models of PersonalityDocument3 pagesFreud's Structural and Topographical Models of PersonalityWajiha Asad KiyaniNo ratings yet
- Nutrition & Dietetics - A Healthy Career ChoiceDocument11 pagesNutrition & Dietetics - A Healthy Career ChoiceVivek Pai KNo ratings yet