Professional Documents
Culture Documents
Does Oral Health
Does Oral Health
Uploaded by
Ana-Maria DucuCopyright:
Available Formats
You might also like
- SWOT ColgateDocument7 pagesSWOT ColgateGokul KesavarajNo ratings yet
- All-On-4, For PatientsDocument28 pagesAll-On-4, For PatientsmmsbabakNo ratings yet
- Iatrogenic Factors Responsible For Periodontal DiseaseDocument57 pagesIatrogenic Factors Responsible For Periodontal DiseaseJaimini Dave100% (1)
- Bab 1-5 Manajemen HcuDocument7 pagesBab 1-5 Manajemen Hcuretno indriyaniNo ratings yet
- Evaluation of Gingival Issues Encountered by Adults Receiving Fixed Orthodontic Treatment in Dakshina Kannada Population: A Questionnaire StudyDocument7 pagesEvaluation of Gingival Issues Encountered by Adults Receiving Fixed Orthodontic Treatment in Dakshina Kannada Population: A Questionnaire StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Comparing Oral Care of Dental and Engineering StudentsDocument7 pagesComparing Oral Care of Dental and Engineering StudentsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- CDH3881 Doughty WebDocument7 pagesCDH3881 Doughty Webk.henryhindsNo ratings yet
- Scheerman 2019Document11 pagesScheerman 2019Nita Sofia RakhmawatiNo ratings yet
- Appropriate Oral Hygiene Motivation Method For Patients With Fixed AppliancesDocument5 pagesAppropriate Oral Hygiene Motivation Method For Patients With Fixed AppliancesMelati WiraNo ratings yet
- Knowledge, Attitude and Perception On Clinical Implications of Behavior Management Techniques in UG Students: A Questionnaire SurveyDocument4 pagesKnowledge, Attitude and Perception On Clinical Implications of Behavior Management Techniques in UG Students: A Questionnaire SurveySantika IndahsariNo ratings yet
- The Effect of Fixed Orthodontic Appliances and Fluoride Mouthwash On The Oral Microbiome of Adolescents - A Randomized Controlled Clinical TrialDocument17 pagesThe Effect of Fixed Orthodontic Appliances and Fluoride Mouthwash On The Oral Microbiome of Adolescents - A Randomized Controlled Clinical Trialsurya saputraNo ratings yet
- Ejpd 2018 19 3 3Document6 pagesEjpd 2018 19 3 3Javier Cabanillas ArteagaNo ratings yet
- Healthcare 10 00406Document12 pagesHealthcare 10 00406AamirNo ratings yet
- Oral Hygiene Practices and Oral Health Knowledge Among Students in Split, CroatiaDocument13 pagesOral Hygiene Practices and Oral Health Knowledge Among Students in Split, CroatiaAamirNo ratings yet
- Evaluation of Brushing Techniques TaughtDocument5 pagesEvaluation of Brushing Techniques TaughtJavier Cabanillas ArteagaNo ratings yet
- Effectiveness of Brushing Teeth in Patients With Reduced Oral Hygiene by Laypeople: A Randomized, Controlled StudyDocument12 pagesEffectiveness of Brushing Teeth in Patients With Reduced Oral Hygiene by Laypeople: A Randomized, Controlled StudyMarco Antonio García LunaNo ratings yet
- 7 DB 6Document6 pages7 DB 6AamirNo ratings yet
- IndianJDent7270-2422731 064347Document6 pagesIndianJDent7270-2422731 064347zppmd7pjd6No ratings yet
- Comm Dent Oral Epid - 2017 - SteinDocument8 pagesComm Dent Oral Epid - 2017 - SteinSherienNo ratings yet
- Distribution of White Spot Lesions Among Orthodontic Patients Attending Teaching Institutes in KhartoumDocument7 pagesDistribution of White Spot Lesions Among Orthodontic Patients Attending Teaching Institutes in Khartoumlilik eka radiatiNo ratings yet
- Final File 5d79d83f30ce45.26319674Document6 pagesFinal File 5d79d83f30ce45.26319674Maulida Dara HarjantiNo ratings yet
- Taf PDFDocument14 pagesTaf PDFrania azzahraNo ratings yet
- ManuscriptDocument24 pagesManuscriptaetuazonNo ratings yet
- Contemporary Undergraduate Implant Dentistry Education A Systematic ReviewDocument13 pagesContemporary Undergraduate Implant Dentistry Education A Systematic ReviewfloraNo ratings yet
- Andriani Andriani, Ratna Wilis, Intan Liana, Cut Ratna Keumala, Sisca Mardelita, Elfi ZaharaDocument5 pagesAndriani Andriani, Ratna Wilis, Intan Liana, Cut Ratna Keumala, Sisca Mardelita, Elfi ZaharaKarissa NavitaNo ratings yet
- Ref 7Document19 pagesRef 7indah anggarainiNo ratings yet
- Brushing Techniques Reseach Latest-1Document25 pagesBrushing Techniques Reseach Latest-1Wajahat Ullah JanNo ratings yet
- Use of Short Term Orthodontics by The Specialist OrthodontistDocument5 pagesUse of Short Term Orthodontics by The Specialist OrthodontistPaul HartingNo ratings yet
- Are Educating and Promoting Interventions Effective in Oral Health?: A Systematic ReviewDocument11 pagesAre Educating and Promoting Interventions Effective in Oral Health?: A Systematic ReviewRiska Endah CahyaniNo ratings yet
- Utilization of Sealants and Conservative Adhesive Resin Restoration For Caries Prevention by Dental StudentsDocument8 pagesUtilization of Sealants and Conservative Adhesive Resin Restoration For Caries Prevention by Dental StudentsannisaramadantiNo ratings yet
- Research Project PaperDocument6 pagesResearch Project Paperapi-369452069No ratings yet
- Effects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialDocument13 pagesEffects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialMohammed Falih HassanNo ratings yet
- BMC Oral HealthDocument8 pagesBMC Oral Healthina09No ratings yet
- Public Health Dentistry Thesis TopicsDocument5 pagesPublic Health Dentistry Thesis Topicss0kuzej0byn2100% (2)
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RNo ratings yet
- GJHS 8 211Document6 pagesGJHS 8 211Susi SimangunsongNo ratings yet
- Oral Health Academics' Conceptualisation of Health Promotion and Perceived Barriers and Opportunities in Dental Practice: A Qualitative StudyDocument13 pagesOral Health Academics' Conceptualisation of Health Promotion and Perceived Barriers and Opportunities in Dental Practice: A Qualitative StudySarbu AndraNo ratings yet
- Case ReportDocument10 pagesCase ReportoniNo ratings yet
- Ijerph 18 00789 v4Document24 pagesIjerph 18 00789 v4Katia BarreraNo ratings yet
- Impact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyDocument10 pagesImpact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyKornist BufuNo ratings yet
- Influence of Subjective Factors Over Hygiene Habits of Complete Denture WearersDocument8 pagesInfluence of Subjective Factors Over Hygiene Habits of Complete Denture WearersIJAR JOURNALNo ratings yet
- Sry Devi 2016 JURNAL READING 3 (PROSTO) PDFDocument5 pagesSry Devi 2016 JURNAL READING 3 (PROSTO) PDFBersama BisaNo ratings yet
- 465 Kaul N - 062018 PDFDocument12 pages465 Kaul N - 062018 PDFVibhor Kumar JainNo ratings yet
- 2 Master Article 2Document5 pages2 Master Article 2neetika guptaNo ratings yet
- 6.14 - EN Relação Entre Tratamento Ortodôntico e Saúde Gengival-Um Estudo Retrospectivo.Document8 pages6.14 - EN Relação Entre Tratamento Ortodôntico e Saúde Gengival-Um Estudo Retrospectivo.JOHNNo ratings yet
- Amhsr 2 14Document5 pagesAmhsr 2 14Archana KrishnaNo ratings yet
- Admin,+Artikel+2 Ira+Liasari+Dkk+45 48Document4 pagesAdmin,+Artikel+2 Ira+Liasari+Dkk+45 48ALFEARA YUNIARNo ratings yet
- Abstrakt oiTOPU EnglishDocument1 pageAbstrakt oiTOPU EnglishNatasa MarticNo ratings yet
- s00784 019 03194 3Document9 pagess00784 019 03194 3shaikhwasif9597No ratings yet
- 10 33631-Sabd 1055376-2182384Document10 pages10 33631-Sabd 1055376-2182384rose1999.rjNo ratings yet
- s40368 021 00631 4Document14 pagess40368 021 00631 4سارة العبيديNo ratings yet
- 4 Master ArticleDocument8 pages4 Master Articleneetika guptaNo ratings yet
- Int Endodontic J - 2023 - DuncanDocument58 pagesInt Endodontic J - 2023 - DuncanAli FaridiNo ratings yet
- Eos 130 0Document10 pagesEos 130 0Jacqueline FelipeNo ratings yet
- Entry Reentry, Allied, and Alternative Careers An IWLC Working Group ReportDocument2 pagesEntry Reentry, Allied, and Alternative Careers An IWLC Working Group ReportMega Arti UtamiNo ratings yet
- Future Dental Journal: E.A. Abdallah, N.E. Metwalli, A.S. BadranDocument7 pagesFuture Dental Journal: E.A. Abdallah, N.E. Metwalli, A.S. BadranNoviyana Idrus DgmapatoNo ratings yet
- Jurnal 5, EAPD - ECC - Management - 2016,, Best Clinical Practice Guidance For Management of Early CariesDocument10 pagesJurnal 5, EAPD - ECC - Management - 2016,, Best Clinical Practice Guidance For Management of Early CariesZulccPaluNo ratings yet
- Hopcraft Et Al-2008-Australian Dental Journal PDFDocument7 pagesHopcraft Et Al-2008-Australian Dental Journal PDFtea metaNo ratings yet
- Palliative Dental 2014Document6 pagesPalliative Dental 2014Isteicy CortezNo ratings yet
- Erosion Guidelines - 2021 - V4 - MJDocument32 pagesErosion Guidelines - 2021 - V4 - MJAARON DIAZ RONQUILLONo ratings yet
- Oral Health ElderlyDocument2 pagesOral Health ElderlyatikramadhaniNo ratings yet
- association_between_mouth_breathing_habit_and_dental_cariesa_retrospectiveDocument5 pagesassociation_between_mouth_breathing_habit_and_dental_cariesa_retrospectiveHaider AltahanNo ratings yet
- Treatment Planning in Restorative Dentistry and Implant ProsthodonticsFrom EverandTreatment Planning in Restorative Dentistry and Implant ProsthodonticsNo ratings yet
- Ribba2006 Mathematical Model For CancerDocument19 pagesRibba2006 Mathematical Model For CancerAna-Maria DucuNo ratings yet
- Extrusion Bioprinting of Soft Materials: An Emerging Technique For Biological Model FabricationDocument31 pagesExtrusion Bioprinting of Soft Materials: An Emerging Technique For Biological Model FabricationAna-Maria DucuNo ratings yet
- Nanodiamonds 2019Document7 pagesNanodiamonds 2019Ana-Maria DucuNo ratings yet
- The Effects of Annealing Temperature On The Permittivity and Electromagnetic Attenuation Performance of Reduced Graphene OxideDocument6 pagesThe Effects of Annealing Temperature On The Permittivity and Electromagnetic Attenuation Performance of Reduced Graphene OxideAna-Maria DucuNo ratings yet
- Demonstration Of Β- (Alxga1-X) 2O3/Ga2O3 Double Heterostructure Field Effect TransistorsDocument6 pagesDemonstration Of Β- (Alxga1-X) 2O3/Ga2O3 Double Heterostructure Field Effect TransistorsAna-Maria DucuNo ratings yet
- Dendron Conjugated Graphene Oxide For Efficient Gene DeliveryDocument17 pagesDendron Conjugated Graphene Oxide For Efficient Gene DeliveryAna-Maria DucuNo ratings yet
- Spanget Larsen2019Document18 pagesSpanget Larsen2019Ana-Maria DucuNo ratings yet
- 1 s2.0 S1369702118312422 MainDocument9 pages1 s2.0 S1369702118312422 MainAna-Maria DucuNo ratings yet
- 10 1016@j Mtbio 2019 100002Document8 pages10 1016@j Mtbio 2019 100002Ana-Maria DucuNo ratings yet
- Hybrid Biomicromotors: Articles You May Be Interested inDocument24 pagesHybrid Biomicromotors: Articles You May Be Interested inAna-Maria DucuNo ratings yet
- Stretchable Sensors For EnvironmentalDocument24 pagesStretchable Sensors For EnvironmentalAna-Maria DucuNo ratings yet
- 1 s2.0 S0167577X13010252 MainDocument3 pages1 s2.0 S0167577X13010252 MainAna-Maria DucuNo ratings yet
- Correlation Between Dislocations and Leakage Current of P-N Diodes On A Free-Standing Gan SubstrateDocument5 pagesCorrelation Between Dislocations and Leakage Current of P-N Diodes On A Free-Standing Gan SubstrateAna-Maria DucuNo ratings yet
- 1 s2.0 S135964621730101X MainDocument5 pages1 s2.0 S135964621730101X MainAna-Maria DucuNo ratings yet
- Wireless Power Transfer Inspired by The Modern Trends in ElectromagneticsDocument20 pagesWireless Power Transfer Inspired by The Modern Trends in ElectromagneticsAna-Maria DucuNo ratings yet
- A Gas Sensor Array For The Simultaneous Detection of Multiple VocsDocument8 pagesA Gas Sensor Array For The Simultaneous Detection of Multiple VocsAna-Maria DucuNo ratings yet
- 1 s2.0 S0042207X17300544 MainDocument19 pages1 s2.0 S0042207X17300544 MainAna-Maria DucuNo ratings yet
- Food Analysis Efa Fat Protein Net Carbs Sugar 3 1 19Document7 pagesFood Analysis Efa Fat Protein Net Carbs Sugar 3 1 19Ana-Maria DucuNo ratings yet
- 1-S2.0-S0143720818319612-Main - Art Chromo Sensor 2018Document7 pages1-S2.0-S0143720818319612-Main - Art Chromo Sensor 2018Ana-Maria DucuNo ratings yet
- Oe 27 24 34803Document21 pagesOe 27 24 34803Ana-Maria DucuNo ratings yet
- 1 s2.0 S0030402621008779 MainDocument11 pages1 s2.0 S0030402621008779 MainAna-Maria DucuNo ratings yet
- 1 s2.0 S0003267021000313 MainDocument6 pages1 s2.0 S0003267021000313 MainAna-Maria DucuNo ratings yet
- How To Write An Expert Opinion LetterDocument3 pagesHow To Write An Expert Opinion LetterAna-Maria DucuNo ratings yet
- 1 s2.0 S0265931X17309888 MainDocument7 pages1 s2.0 S0265931X17309888 MainAna-Maria DucuNo ratings yet
- Origin of Negative Anomalous Nernst Thermopower in Mn-Ga Ordered AlloysDocument7 pagesOrigin of Negative Anomalous Nernst Thermopower in Mn-Ga Ordered AlloysAna-Maria DucuNo ratings yet
- 1 s2.0 S0003267015008442 MainDocument8 pages1 s2.0 S0003267015008442 MainAna-Maria DucuNo ratings yet
- Modifications in The Nanoparticle-Protein Interactions For Tuning The Protein Adsorption and Controlling The Stability of ComplexesDocument8 pagesModifications in The Nanoparticle-Protein Interactions For Tuning The Protein Adsorption and Controlling The Stability of ComplexesAna-Maria DucuNo ratings yet
- 1 s2.0 S0038092X20312573 MainDocument10 pages1 s2.0 S0038092X20312573 MainAna-Maria DucuNo ratings yet
- NSA 333467 Prospective Application of Nanoparticles Green Synthesized UDocument17 pagesNSA 333467 Prospective Application of Nanoparticles Green Synthesized UAna-Maria DucuNo ratings yet
- Ef Ficient Spin Excitation Via Ultrafast Damping-Like Torques in AntiferromagnetsDocument7 pagesEf Ficient Spin Excitation Via Ultrafast Damping-Like Torques in AntiferromagnetsAna-Maria DucuNo ratings yet
- ĐỀ 02 thptqgDocument6 pagesĐỀ 02 thptqgHà Vy NguyễnNo ratings yet
- Keywords:-Data Collection and Evaluation, UKGSDocument11 pagesKeywords:-Data Collection and Evaluation, UKGSInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Composite in Everyday Practice - How To Choose The Right Material and Simplify Application Techniques in The Anterior TeethDocument24 pagesComposite in Everyday Practice - How To Choose The Right Material and Simplify Application Techniques in The Anterior TeethTania Azuara100% (1)
- Habits and Social Norms Leading To Childhood CariesDocument16 pagesHabits and Social Norms Leading To Childhood Cariesapi-522555065No ratings yet
- NP 1Document73 pagesNP 1Aldous SerranoNo ratings yet
- Toothpaste Consumer SurveyDocument6 pagesToothpaste Consumer SurveyVishakha BhosaleNo ratings yet
- Journal Pone 0208246 PDFDocument12 pagesJournal Pone 0208246 PDFMirza AryantoNo ratings yet
- PT Pauh Mandiri Sejahtera: Jl. Manggis Raya No 41 RT 28 RW 06, Panorama, Singaran Pati, Kota Bengkulu, 38226Document3 pagesPT Pauh Mandiri Sejahtera: Jl. Manggis Raya No 41 RT 28 RW 06, Panorama, Singaran Pati, Kota Bengkulu, 38226AINANo ratings yet
- Bookstyle ContentDocument17 pagesBookstyle ContentCindy SaquilonNo ratings yet
- Planning For A Health Career: Unit 4Document34 pagesPlanning For A Health Career: Unit 4Lanie Tamacio BadayNo ratings yet
- Brand Analysis - PepsodentDocument15 pagesBrand Analysis - PepsodentSamirNo ratings yet
- ChildrenDocument2 pagesChildrendentdeepNo ratings yet
- Soumya Prajapati MNI PROJECTDocument36 pagesSoumya Prajapati MNI PROJECTUplaksh KumarNo ratings yet
- Seniors' Oral Care:: A Guide For Personal Support WorkersDocument40 pagesSeniors' Oral Care:: A Guide For Personal Support WorkersAvina Anin NasiaNo ratings yet
- Local Media2398984275540957743Document27 pagesLocal Media2398984275540957743Rey YuyNo ratings yet
- Assessment of Periodontal Status in Patients With Rheumatoid Arthritis in Kelantan, Malaysia: A Preliminary StudyDocument5 pagesAssessment of Periodontal Status in Patients With Rheumatoid Arthritis in Kelantan, Malaysia: A Preliminary StudyemmypuspitasariNo ratings yet
- Mohammad Ali LeghariDocument64 pagesMohammad Ali LeghariNaoNo ratings yet
- Lesson PlanDocument4 pagesLesson Planpsuliongrl1659No ratings yet
- CariesCare-International Consensus-Manuscript BDJ-corrected 12062019Document13 pagesCariesCare-International Consensus-Manuscript BDJ-corrected 12062019pocket4love4yeahNo ratings yet
- Pregnancy CengizDocument10 pagesPregnancy Cengizkirana_patrolinaNo ratings yet
- Case Study 1Document5 pagesCase Study 1api-612911534No ratings yet
- 3patient History C.C, Dent HX, Habits 2Document21 pages3patient History C.C, Dent HX, Habits 2ابو العزNo ratings yet
- Personal Hygiene: Mr. Genesis Arn M. Latido, RN InstructorDocument41 pagesPersonal Hygiene: Mr. Genesis Arn M. Latido, RN InstructorJohn David Seven RocamoraNo ratings yet
- Catalogue PierrotDocument44 pagesCatalogue PierrotGuntur SetiawanNo ratings yet
- Stephen Legaspi CsaDocument15 pagesStephen Legaspi CsaKhristian Joshua G. JuradoNo ratings yet
- Toothbrush Its Design and Modifications An OvervieDocument9 pagesToothbrush Its Design and Modifications An OvervierklonNo ratings yet
- Manual Vs ElectricDocument5 pagesManual Vs ElectricnasyaNo ratings yet
Does Oral Health
Does Oral Health
Uploaded by
Ana-Maria DucuOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Does Oral Health
Does Oral Health
Uploaded by
Ana-Maria DucuCopyright:
Available Formats
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/230840930
Does oral health counseling effectively improve oral hygiene of orthodontic
patients?
Article in European Journal of Paediatric Dentistry · September 2012
Source: PubMed
CITATIONS READS
19 805
5 authors, including:
Maja Lalic Ema Aleksic
14 PUBLICATIONS 36 CITATIONS
University Business Academy in Novi Sad
17 PUBLICATIONS 36 CITATIONS
SEE PROFILE
SEE PROFILE
All content following this page was uploaded by Ema Aleksic on 21 May 2014.
The user has requested enhancement of the downloaded file.
M. Lalic, E. Aleksic*, M. Gajic, J. Milic*, was similar. Counseling is a promising approach
D. Malesevic** that warrants further attention in a variety of dental
contexts.
Faculty of Stomatology Pancevo,
University Business Academy of Novi Sad, Serbia
Department of Preventive and Pediatric Dentistry,
*Department of Orthodontics
Keywords Dental education; Motivational interview;
**Department of Informatics and Statistics
Oral health counseling; Oral hygiene; Orthodontic
patients.
e-mail: majajevtic@open.telekom.rs
Introduction
Does oral health
Orthodontic treatment increases the risk of carious
counseling effectively lesions and gingival inflammation, with consequent
harm to the patient and a high risk of compromising
improve oral hygiene treatment outcome Lucchese et al., 2001; Lucchese
and Storti, 2011]. Caries risk is related to appliances
of orthodontic which increase the number of sites where plaque can
accumulate, as well as to changes in the bacterial flora
patients? and the age of the patient [Opsahl et al., 2010]. Gingival
inflammation is also a common finding in orthodontic
patients. The severity of gingival inflammation is in
correlation with oral hygiene status because oral
cleaning procedures are more difficult in presence of
abstract orthodontic appliances and their components [Baricevic
et al., 2011].
Aim The aim of this study was to compare the Before starting orthodontic treatment, individual
effectiveness of oral health counseling sessions with caries risk should be determined, and according to
traditional oral hygiene education in orthodontic its results adequate preventive measures should be
patients with fixed appliances. applied [Todd et al., 1999; Madléna et al., 2000;
Materials and methods Study design: randomised Benson et al., 2005]. Patients need to be educated
control trial with experimental and control group. how to maintain proper oral hygiene in order to
A group of 99 adolescents with fixed orthodontic prevent negative side effects of orthodontic appliances
appliances were randomly assigned to oral health [Türkkahraman et al., 2005]. Authors reported that oral
counseling (experimental) or traditional health hygiene motivation methods used in dental education
education (control) group. Subjects in the control can affect the outcome of treatment. Educational
group received verbal instructions and a demonstration methods are generally classified as verbal [Huber et
of the modified Bass brushing technique on a model. al., 1972; Boyd, 1983; Yeung et al., 1989], written
The experimental group also received the verbal [McGlynn et al., 1987] or visual-based [Lees and Rock,
information with demonstration on the model and 2000]. A demonstration of the brushing technique
in addition a personalised 40-minutes counseling with a model, supported by verbal instructions,
session on oral hygiene. Plaque Index (PI) and gingivitis illustrations catalogue or instructional video, followed
(G) were recorded before, 1 and 6 months after the by supervised application by the patient, seems to be
counseling session/traditional education. the most effective method for patients to adopt any
Results Oral health counseling and traditional brushing technique [Addy et al., 1999; Renton-Harper
education improved the oral hygiene of orthodontic et al., 1999; Yetkin et al., 2007]. In recent years, there
patients. PI values were significantly lower after 6 have been attempts to integrate cognitive behavioural
months compared to the baseline in both groups, techniques with interventions targeting cleaning
but the prevalence of gingival inflammation remained behaviour by forming action plans for when, where and
significantly lower only in the experimental group. how to perform daily self-care [Jönsson et al., 2006;
Conclusion Oral health counseling increased plaque Schüz et al., 2006; Sniehotta et al., 2007]. Individual
removal efficacy and control of gingival inflammation. brushing recommendations should be targeted to
The efficiency of counseling and traditional education individual goals and problems. One of the cognitive–
behavioural techniques applied to dental education
European Journal of Paediatric Dentistry vol. 13/3-2012 181
Lalic M. et al.
interventions is motivational interviewing (MI), a brief chronic diseases were excluded from this study. We
counseling approach that provides strategies to move conducted a randomised clinical trial composed of two
patients from inaction to action. Aim of counseling is groups. The patients were randomly assigned to either
to identify what maintains behaviours, including the the experimental or the control group.
ambivalence about modifying inadequate daily self-
care routine, and to encourage and support people in Control group
adopting improved oral hygiene regime [Bundy, 2004]. In the control group, patients received a prophylactic
Four principles guide the implementation of MI: treatment (use of plaque disclosure agents,
› expression of empathy: the counselor understands prophylactic plaque removal and topical application of
the individual’s feelings without judging; fluoride varnish), combined with traditional chair-side
› exploring ambivalence: through open-ended education. The dentists demonstrated the modified Bass
questions, the counselor facilitates the individual’s brushing technique with a model, and provided verbal
formulation of arguments for for changing daily oral instructions. After the demonstration, the adolescent
cleaning habits; practiced brushing under dentist’s supervision.
› rolling with the resistance: the counselor focuses on
creating a new perspective for the importance of Experimental group
behavioural change; The children in the experimental group received the
› supporting self-efficacy: the counselor facilitates same prophylactic treatment, verbal instructions and
development of the individual’s confidence to cope the demonstration of the brushing technique with a
with obstacles and succeed in changing oral hygiene model, followed by supervised self-application. In
related habits [Ismail et al., 2011]. addition, they received one 40-minute session with
Process avoids scolding, warning or exhorting patient elements of Motivational Interviewing (MI) counseling
to change. Instead, the dentist provides the advice to increase compliance and motivation for brushing.
and emphasises a patient’s choice, discovers and uses
discrepancies that the patient identifies between his or MI protocol
her current behaviour and desired goals. The dentist Two trained dentists (ML and EA) performed
encourages the patient to choose what he/she feels able counseling according to the written MI protocol. The
to do and helps the patient to evaluate good and bad counseling sessions were audio recorded in order
consequences of that behaviour [Rollnick et al., 1992]. to ensure that the MI protocol was being delivered
The aim of this study was to describe and evaluate consistently. At the beginning of counseling, the
an individually-tailored educational method based on dentists stated the purpose of counseling and self-
MI counseling for oral hygiene self-care in patients management and provided information on the aetiology
with fixed orthodontic appliances. More specifically, of gingival inflammation. The dentists discussed with
this study aims to describe the effects of MI counseling the adolescents their brushing habits and possible
on dental plaque control and gingival health, one and reasons that might affect cleaning behaviours (i.e. early
six months after the counseling intervention, and to rising or going to the bed late at night and being too
compare them with the outcomes of traditional dental sleepy to brush, forgetting to clean the teeth, fatigue,
education regarding oral hygiene. lack of time, personal relevance of having clean teeth,
parental control). The adolescents assessed their need
for change in oral hygiene habits (frequency of tooth
Material and methods brushing and cleaning around the brackets and in
the interdental spaces). The dentists gave advices on
This study was conducted in the dental clinic at the how to improve the hygiene, concerning the patient’s
Department of Paediatric and Preventive dentistry, need for improving oral cleanliness. Positive behaviours
Faculty of Stomatology Pancevo, Serbia. The study were encouraged, problems identified and possible
conformed to the Declaration of Helsinki. The Ethics solutions offered. The plan and schedule for brushing,
Committee of the Faculty approved the study. The interdental cleaning and use of fluoride rinses was
purpose of this study was explained to all of the suggested in accordance to the individual preferences.
patients and their parents, who signed an informed The dentists discussed the options and encouraged the
consent form. patients to talk. The dentists helped them to set the
individual long-term goals related to the oral health
Subjects (i.e. the elimination of gingival bleeding, improvement
A total of 104 patients (53 males and 51 females, 13-14 of breath freshness). The dentists used strategies
years old) referred for treatment with fixed orthodontic that reinforce the process of habits modification,
appliances to the Department of Orthodontics, which included problems in performing regular and
participated in this study scheduled between February thorough brushing, adolescents’ feelings and personal
2011 and August 2011. Patients with systemic or importance of teeth and oral health.
182 European Journal of Paediatric Dentistry vol. 13/3-2012
Oral Health Counseling for Orthodontic Patients
Clinical examination and 50 females), so eventually the experimental group
Prior to the beginning of the study, two calibrated consisted of 48 patients (26 female and 22 male) and
examiners recorded the prevalence of gingival the control group of 51 (24 female and 27 male).
inflammation (a percentage of subjects with localised Both MI counseling and traditional dental education
or generalised gingivitis) and the Plaque Index (PI) resulted in significant reduction of dental plaque. Figure
according to Sillness & Löe. Follow-ups were conducted 1 illustrates the changes of Plaque Index from baseline
after one- and six-month period. We recorded the (PI 0) to one- (PI 1) and six-month (PI 2) follow-up in
Plaque Index and the presence of gingival inflammation the experimental and the control group. According
in the experimental and the control group. to the results of ANOVA for repeated measurements,
no significant differences in PI values between the
Statistical analysis groups were observed at the baseline (p=0.582), after
We used ANOVA for repeated measures and Paired one (p=0.056) and six months (p=0.625). We used a
Samples T-test to compare the mean values of Plaque Paired Samples T- test to compare the values of the
Index (PI), and Fisher’s Exact Test to compare the Plaque Index within the groups at different times of
prevalence of gingival inflammation at different times measurement (Table 1). In both groups, PI values were
of measurement. In all tests, p value less than 0.05 was significantly lower at the follow-ups compared to the
considered to be statistically significant. We performed baseline, although there was an increase of PI values
the statistical analysis using the SPSS statistical software from one- to the six-month follow-up period.
(SPSS for Windows, release 17.0, SPSS, Chicago, IL). At the baseline, 66.7% of subjects had gingivitis, its
prevalence significantly decreased after one month in
both groups (Fig. 2, 3). After six months, prevalence
Results of gingival inflammation increased in both groups,
but not significantly compared to the previous value.
The response rate was 95.2% (99 patients, 49 males Compared to the baseline measurement (G2 vs. G0),
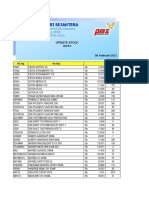
3.00 fig 1 The Plaque Index
experimental group
values at the baseline (PI0),
control group one- (PI1) and six-month
2.50 2.43
(PI2) follow-ups in the
2.15
max con. experimental and the control
2.31
2.00 2.15 min con. group.
1.92
1.75
min exp.
1.56
1.51
1.50 max exp
1.34
1.21 1.31
1.06
1.00
0.70
0.53 0.56 tabLE 1 Comparison of the
.50 Plaque Index values at the
0.44
baseline (PI0), one- (PI1)
0.34 and six-month (PI2) in the
.00
PI 0 PI 1 PI 2
experimental and control
group.
Paired Differences 95% Confidence Interval of the Difference
Mean SD SE Lower Upper t df p
Experimental group
PI 0 - PI 1 0.496 0.393 0.057 0.382 0.610 8.74 47 <0.001
PI 0 - PI 2 0.251 0.333 0.048 0.155 0.348 5.23 47 <0.001
PI 1 - PI 2 -0.245 0.306 0.044 -0.334 -0.156 -5.55 47 <0.001
Control group
PI 0 - PI 1 0.300 0.337 0.047 0.205 0.395 6.34 50 <0.001
PI 0 - PI 2 0.173 0.364 0.051 0.071 0.275 3.39 50 0.001
PI 1 - PI 2 -0.127 0.355 0.050 -0.227 -0.027 -2.54 50 0.014
European Journal of Paediatric Dentistry vol. 13/3-2012 183
Lalic M. et al.
100%
fig 2 The prevalence of
inflammation free
subject gingival inflammation at the
90% p<0.001
31.3% inflammation positive baseline (G0),
p=0.208
80% 45.8%
subject one- (G1) and six-month
70%
p=0.012 (G2) follow-ups in the
72.9% experimental group.
60%
50%
40%
68.8%
30%
54.2%
20%
27.1%
10%
0%
GI 0 GI 1 GI 2
100%
fig 3 The prevalence of
inflammation free
subject gingival inflammation at the
90%
inflammation positive baseline (G0), one- (G1) and
35.3%
80% p=0.017
subject six-month (G2) follow-ups in
51.0% p=0.161
70% 60.8%
the control group.
60% p=0.425
50%
40%
64.7%
30%
49.0%
20% 32.9%
10%
0%
GI 0 GI 1 GI 2
the value of gingivitis remained significantly lower only method, we were also interested to determine if it was
in the experimental group (p = 0.012). Between the possible for orthodontists and/or paedodontists to
groups, no statistically significant differences in the apply this method in their practices; this was confirmed
prevalence of gingival inflammation were observed at in the present study.
the baseline (p=0.286), one- (p=0.831) and six-month We believe that MI counseling is a suitable method
follow-up (p=0.689). for increasing the motivation and commitment for
improving oral hygiene behaviour, since the regular
check-ups during the orthodontic treatment, usually
Discussion scheduled once in a month, provide the opportunity
to reinforce the process of habit improvement. Still,
The presence of the fixed orthodontic appliances single MI counseling session in our study did not ensure
encourages the growth and retention of dental plaque, significantly greater long-time improvement in oral
which results in localised gingivitis [van Gastel et al., hygiene compared to the traditional education, although
2007]. Therefore, it is very important to ensure a PI values and prevalence of gingival inflammation in
continuous control over the plaque accumulation. the experimental group were lower than those in the
However, literature findings suggest that the control group at the follow-ups. The increase of mean
educational interventions have positive, but temporary PI values after six months in both groups, implicates
effect on plaque accumulation [Kayl and Locker, that constant effort in oral health education must be
1996; Ivanovic and Lekic, 1996]. In our study, both MI directed towards the motivation of the patients, and
counseling and the traditional education improved the that the behavioural change in some patients should
plaque removal efficacy among the patients. While our be reinforced with additional short counseling sessions
primary intention was to test an alternative educational during the regular check-ups [Weinstein et al., 2006].
184 European Journal of Paediatric Dentistry vol. 13/3-2012
Oral Health Counseling for Orthodontic Patients
Although the prevalence of gingivitis was similar of counseling practices in orthodontic patients
between the groups six months after the education, usually occurs in the context of difficult and critical
the percentage of adolescents with gingivitis in the period of development. Motivational interviewing
experimental group remained significantly lower technique avoids prescriptive character of traditional
compared to the baseline, while in the control group it dental education [Rollnick et al., 1992], and helps in
reached values similar to the initial ones. This suggested the reduction of the children’s resistance to change
that patients in the experimental group were more behaviours that increase the risk of developing the oral
consistent in oral hygiene. Still, this result must be disease.
interpreted with caution, because initial prevalence of The main challenge for future research is not only to
gingivitis was greater (but not statistically different) in find the effective ways to educate individuals how to
the experimental than in the control group. Our results adopt new skills and behaviours, but also to achieve
were consistent with findings of other authors, who long-term results regarding maintenance of good oral
reported that a short-term preventative programme health. The theoretical framework of counseling may
induced a transient improvement of gingival health but broaden counselors’ awareness of readiness for change
only during the instructional period [Ivanovic and Lekic, and foster child-centered and more efficient approach
1996]. The maintenance of improved gingival health to counseling and contribute to adapting appropriate
over longer periods requires prolonged, repeated counseling strategies in the context of child’s and
instructions [Emler et al., 1980]. adolescent’s oral hygiene history and life situation
Similar efficacy of a single MI counseling session [Kasilaet al., 2006].
and a traditionally approached oral hygiene education
in our study could be a result of numerous factors.
First, motivational counseling was provided to all the Conclusion
participants in the experimental group regardless of
their baseline motivation, which could have resulted in Increase of motivation among orthodontic patients
mixed effects as a function of initial readiness to change regarding sustainable oral hygiene regime might
the brushing habits [Martino et al., 2008]. Second, MI result in better oral health outcomes and prevent
in other contexts relies heavily on personal analysis of complications [Bardal et al., 2011]. However, the best
the pros and cons of the misbehaviour. In contrast to way to educate and motivate the patients in terms of
misbehaviours such as substance abuse, which have oral hygiene can’t be easily identified. According to our
clear negative effects, the oral hygiene may be less findings, the MI counseling effectively improved plaque
relevant, particularly for children and adolescents who control and gingival health of children, but the results
are undergoing physical, emotional and social changes. were similar to those provided by traditional dental
Third, the patients in both groups were probably education. Further research of oral hygiene counseling
highly motivated to improve their brushing habits since is required, as there is an evident need for improving
they were at the beginning of orthodontic treatment. and developing oral health education to meet the
Decline in motivation could be expected over time, personal needs of patients.
and the application of MI counseling might contribute
to long-term compliance with regard to preventive
recommendations [Weinstein et al., 2006]. References
The sample in this study was relatively small and all
the patients came from similar local environment, the › Addy M, Renton-Harper P, Warren P, Newcombe RG. An evaluation of
video instruction for an electric toothbrush. Comparative single-brushing
results, therefore, could not be generalised. cross-over study. J Clin Periodontol. 1999;26:289–293.
Motivation from the orthodontist for oral health › Bardal, P.A.P et al. Education and motivation in oral health: preventing
programmes, as well as the feedback, should be disease and promoting health in patients undergoing orthodontic
offered with kindness, objectivity, and respect, as it can treatment. Dental Press J. Orthod. 2011;16(3): 95-102.
influence the outcome of a programme [Clark, 1976]. › Baricevic M, Mravak-Stipetic M, Majstorovic M, Baranovic M , Baricevic
Health professionals tend to elicit information from D, Loncar B. Oral mucosal lesions during orthodontic treatment. Int J
Paediatr Dent. 2011;21:96–102.
children but to exclude them in the communication of › Benson, PE, Shah, AA, Millett, DT, Dyer, F, Parkin, N. Vine, RS. Fluorides,
decision-making and treatment [Kasila et al., 2006]. orthodontics and demineralization: a systematic review. J Orthod.
Developing child-centered approach and increasing 2005;32:102–114.
shared decision-making might lead to a shift in the › Boyd RL. Longitudinal evaluation of a system for self-monitoring
child-dentist relationship from being asymmetrical and plaque control effectiveness in orthodontic patients. J Clin Periodontol.
1983;10:380–388.
controlled by dentist towards a more equalitarian one.
› Bundy, C. Changing behaviour: using motivational interviewing
The MI counseling helps dealing with the resistance techniques. J R Soc Med. 2004; 97(s44):443–479.
and avoids telling the patients what to do, which can › Clark JR. Oral hygiene in the orthodontic practice: motivation,
be very important for the patients of specific ages, like responsibilities, and concepts. Am J Orthod. 1976;69:72–82.
schoolchildren and adolescents. The implementation › Emler BF, Windchy AM, Zaino SW, Feldman SM, Scheetz JP. The value of
European Journal of Paediatric Dentistry vol. 13/3-2012 185
Lalic M. et al.
repetition and reinforcement in improving oral hygiene performance. J of behavioral self-management on oral hygiene adherence among
Periodontol. 1980;51: 228–234. orthodontic patients. Am J Orthod. 1987;91:321–327.
› Huber SJ, Vernino AR, Nanda RS. Professional prophylaxis and its effect › Opsahl VS, Haignere-Rubinstein C, Lasfargues JJ, Chaussain C. Caries
on the periodontium of full-banded orthodontic patients. Angle Orthod. risk and orthodontic treatment. Int Orthod. 2010;8(1):28-45.
1972;42:26–34. › Renton-Harper P, Addy M, Warren P, Newcombe RG. Comparison of video
› Ismail AI, Ondersma S, Jedele JM, Little RJ, Lepkowski JM. Evaluation and written instructions for plaque removal by an oscillating/rotating/
of a brief tailored motivational intervention to prevent early childhood reciprocating electric toothbrush. J Clin Periodontol. 1999;26:752–756.
caries. Community Dent Oral Epidemiol. 2011;39(5):433-448. › Rollnick, S, Heather, N, Bell, A. Negotiating behaviour change in medical
› Ivanovic M, Lekic P. Transient effect of a short-term educational settings: The development of brief motivational interviewing. J Ment
programme without prophylaxis on control of plaque and gingival Health. 1992;1(1): 25-37.
inflammation in school children. J Clin Periodontol. 1996;23(8):750-757. › Schüz B, Sniehotta FF, Wiedemann A, Seemann R. Adherence to a
› Jönsson B, Lindberg P, Oscarson N, Öhrn K. Improved compliance and daily flossing regimen in university students: effects of planning when,
self-care in patients with periodontitis - a randomized control trial. Int J where, how and what to do in the face of barriers. J Clin Periodontol.
Dent Hyg. 2006;4:77–83. 2006;33:612–619.
› Kasila K, Poskiparta M, Kettunen T, Pietilä I. Oral health counselling › Sniehotta FF, Araú.jo Soares SU, Dombrowski V. Randomized controlled
in changing schoolchildren’s oral hygiene habits: a qualitative study. trial of a one-minute intervention changing oral self-care behavior. J
Community Dent Oral Epidemiol. 2006;34(6):419-428. Dent Res. 2007;86:641–645.
› Kayl EJ, Locker D. Is dental health education effective? A systematic › Todd MA, Staley RN, Kanellis MJ, Donly KJ, Wefel JS. Effect of a fluoride
review of current evidence. Community Dent Oral Epidemiol. varnish on demineralization adjacent to orthodontic brackets. Am J
1996;24:(4): 231–235. Orthod Dentofacial Orthop. 1999;116(2):159-167.
› Lees A, Rock WP. A comparison between written, verbal and videotape › Türkkahraman H, Sayın O, Bozkurt FY, Yetkin Z, Kaya S, Önal S. Archwire
oral hygiene instruction for patients with fixed appliances. J Orthod. ligation techniques, microbial colonization, and periodontal status in
2000; 27:323–328. orthodontically treated patients. Angle Orthod. 2005;75:227–232.
› Lucchese A, Porcù F, Dolci F. Effects of various stripping techniques on › van Gastel J, Quirynen M, Teughels W, Carels C. The relationships
surface enamel. J Clin Orthod. 2001 Nov;35(11):691-5. between malocclusion, fixed orthodontic appliances and periodontal
› Lucchese A, Storti E. Morphological characteristics of primary enamel disease. A review of the literature. Aust Orthod J. 2007;23(2):121-
surfaces versus permanent enamel surfaces: SEM digital analysis. Eur J 129.
Paediatr Dent. 2011;12:179-83. › Weinstein P, Harrison R, Benton T. Motivating mothers to prevent
› Madléna M, Vitalyos G, Márton S, Nagy G. Effect of chlorhexidine varnish caries: confirming the beneficial effect of counseling. J Am Dent Assoc.
on bacterial levels in plaque and saliva during orthodontic treatment. J 2006;137(6):789-793.
Clin Dent. 2000;11(2):42-46. › Yetkin AZ, Sayın MO¨, O¨zat Y; Goster T, Atilla AO, Bozkurt FY.
› Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. Community Appropriate Oral Hygiene Motivation Method for Patients with Fixed
program therapist adherence and competence in motivational Appliances. Angle Orthod. 2007;77(6):1085-1089.
enhancement therapy. Drug Alcohol Depend. 2008; 96(1-2):37-48. › Yeung SC, Howell S, Fahey P. Oral hygiene program for orthodontic
› McGlynn FD, Le Compte EJ, Thomas RG, Courts FJ, Melamed BG. Effect patients. Am J Orthod Dentofacial Orthop. 1989;96:208–213.
186 European Journal of Paediatric Dentistry vol. 13/3-2012
View publication stats
You might also like
- SWOT ColgateDocument7 pagesSWOT ColgateGokul KesavarajNo ratings yet
- All-On-4, For PatientsDocument28 pagesAll-On-4, For PatientsmmsbabakNo ratings yet
- Iatrogenic Factors Responsible For Periodontal DiseaseDocument57 pagesIatrogenic Factors Responsible For Periodontal DiseaseJaimini Dave100% (1)
- Bab 1-5 Manajemen HcuDocument7 pagesBab 1-5 Manajemen Hcuretno indriyaniNo ratings yet
- Evaluation of Gingival Issues Encountered by Adults Receiving Fixed Orthodontic Treatment in Dakshina Kannada Population: A Questionnaire StudyDocument7 pagesEvaluation of Gingival Issues Encountered by Adults Receiving Fixed Orthodontic Treatment in Dakshina Kannada Population: A Questionnaire StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Comparing Oral Care of Dental and Engineering StudentsDocument7 pagesComparing Oral Care of Dental and Engineering StudentsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- CDH3881 Doughty WebDocument7 pagesCDH3881 Doughty Webk.henryhindsNo ratings yet
- Scheerman 2019Document11 pagesScheerman 2019Nita Sofia RakhmawatiNo ratings yet
- Appropriate Oral Hygiene Motivation Method For Patients With Fixed AppliancesDocument5 pagesAppropriate Oral Hygiene Motivation Method For Patients With Fixed AppliancesMelati WiraNo ratings yet
- Knowledge, Attitude and Perception On Clinical Implications of Behavior Management Techniques in UG Students: A Questionnaire SurveyDocument4 pagesKnowledge, Attitude and Perception On Clinical Implications of Behavior Management Techniques in UG Students: A Questionnaire SurveySantika IndahsariNo ratings yet
- The Effect of Fixed Orthodontic Appliances and Fluoride Mouthwash On The Oral Microbiome of Adolescents - A Randomized Controlled Clinical TrialDocument17 pagesThe Effect of Fixed Orthodontic Appliances and Fluoride Mouthwash On The Oral Microbiome of Adolescents - A Randomized Controlled Clinical Trialsurya saputraNo ratings yet
- Ejpd 2018 19 3 3Document6 pagesEjpd 2018 19 3 3Javier Cabanillas ArteagaNo ratings yet
- Healthcare 10 00406Document12 pagesHealthcare 10 00406AamirNo ratings yet
- Oral Hygiene Practices and Oral Health Knowledge Among Students in Split, CroatiaDocument13 pagesOral Hygiene Practices and Oral Health Knowledge Among Students in Split, CroatiaAamirNo ratings yet
- Evaluation of Brushing Techniques TaughtDocument5 pagesEvaluation of Brushing Techniques TaughtJavier Cabanillas ArteagaNo ratings yet
- Effectiveness of Brushing Teeth in Patients With Reduced Oral Hygiene by Laypeople: A Randomized, Controlled StudyDocument12 pagesEffectiveness of Brushing Teeth in Patients With Reduced Oral Hygiene by Laypeople: A Randomized, Controlled StudyMarco Antonio García LunaNo ratings yet
- 7 DB 6Document6 pages7 DB 6AamirNo ratings yet
- IndianJDent7270-2422731 064347Document6 pagesIndianJDent7270-2422731 064347zppmd7pjd6No ratings yet
- Comm Dent Oral Epid - 2017 - SteinDocument8 pagesComm Dent Oral Epid - 2017 - SteinSherienNo ratings yet
- Distribution of White Spot Lesions Among Orthodontic Patients Attending Teaching Institutes in KhartoumDocument7 pagesDistribution of White Spot Lesions Among Orthodontic Patients Attending Teaching Institutes in Khartoumlilik eka radiatiNo ratings yet
- Final File 5d79d83f30ce45.26319674Document6 pagesFinal File 5d79d83f30ce45.26319674Maulida Dara HarjantiNo ratings yet
- Taf PDFDocument14 pagesTaf PDFrania azzahraNo ratings yet
- ManuscriptDocument24 pagesManuscriptaetuazonNo ratings yet
- Contemporary Undergraduate Implant Dentistry Education A Systematic ReviewDocument13 pagesContemporary Undergraduate Implant Dentistry Education A Systematic ReviewfloraNo ratings yet
- Andriani Andriani, Ratna Wilis, Intan Liana, Cut Ratna Keumala, Sisca Mardelita, Elfi ZaharaDocument5 pagesAndriani Andriani, Ratna Wilis, Intan Liana, Cut Ratna Keumala, Sisca Mardelita, Elfi ZaharaKarissa NavitaNo ratings yet
- Ref 7Document19 pagesRef 7indah anggarainiNo ratings yet
- Brushing Techniques Reseach Latest-1Document25 pagesBrushing Techniques Reseach Latest-1Wajahat Ullah JanNo ratings yet
- Use of Short Term Orthodontics by The Specialist OrthodontistDocument5 pagesUse of Short Term Orthodontics by The Specialist OrthodontistPaul HartingNo ratings yet
- Are Educating and Promoting Interventions Effective in Oral Health?: A Systematic ReviewDocument11 pagesAre Educating and Promoting Interventions Effective in Oral Health?: A Systematic ReviewRiska Endah CahyaniNo ratings yet
- Utilization of Sealants and Conservative Adhesive Resin Restoration For Caries Prevention by Dental StudentsDocument8 pagesUtilization of Sealants and Conservative Adhesive Resin Restoration For Caries Prevention by Dental StudentsannisaramadantiNo ratings yet
- Research Project PaperDocument6 pagesResearch Project Paperapi-369452069No ratings yet
- Effects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialDocument13 pagesEffects of A Standard Versus Comprehensive Oral Care Protocol Among Intubated Neuroscience ICU Patients: Results of A Randomized Controlled TrialMohammed Falih HassanNo ratings yet
- BMC Oral HealthDocument8 pagesBMC Oral Healthina09No ratings yet
- Public Health Dentistry Thesis TopicsDocument5 pagesPublic Health Dentistry Thesis Topicss0kuzej0byn2100% (2)
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RNo ratings yet
- GJHS 8 211Document6 pagesGJHS 8 211Susi SimangunsongNo ratings yet
- Oral Health Academics' Conceptualisation of Health Promotion and Perceived Barriers and Opportunities in Dental Practice: A Qualitative StudyDocument13 pagesOral Health Academics' Conceptualisation of Health Promotion and Perceived Barriers and Opportunities in Dental Practice: A Qualitative StudySarbu AndraNo ratings yet
- Case ReportDocument10 pagesCase ReportoniNo ratings yet
- Ijerph 18 00789 v4Document24 pagesIjerph 18 00789 v4Katia BarreraNo ratings yet
- Impact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyDocument10 pagesImpact of Orthodontic Treatment On Oral Health-Related Quality of Life in The Slovak Republic: A Cross-Sectional StudyKornist BufuNo ratings yet
- Influence of Subjective Factors Over Hygiene Habits of Complete Denture WearersDocument8 pagesInfluence of Subjective Factors Over Hygiene Habits of Complete Denture WearersIJAR JOURNALNo ratings yet
- Sry Devi 2016 JURNAL READING 3 (PROSTO) PDFDocument5 pagesSry Devi 2016 JURNAL READING 3 (PROSTO) PDFBersama BisaNo ratings yet
- 465 Kaul N - 062018 PDFDocument12 pages465 Kaul N - 062018 PDFVibhor Kumar JainNo ratings yet
- 2 Master Article 2Document5 pages2 Master Article 2neetika guptaNo ratings yet
- 6.14 - EN Relação Entre Tratamento Ortodôntico e Saúde Gengival-Um Estudo Retrospectivo.Document8 pages6.14 - EN Relação Entre Tratamento Ortodôntico e Saúde Gengival-Um Estudo Retrospectivo.JOHNNo ratings yet
- Amhsr 2 14Document5 pagesAmhsr 2 14Archana KrishnaNo ratings yet
- Admin,+Artikel+2 Ira+Liasari+Dkk+45 48Document4 pagesAdmin,+Artikel+2 Ira+Liasari+Dkk+45 48ALFEARA YUNIARNo ratings yet
- Abstrakt oiTOPU EnglishDocument1 pageAbstrakt oiTOPU EnglishNatasa MarticNo ratings yet
- s00784 019 03194 3Document9 pagess00784 019 03194 3shaikhwasif9597No ratings yet
- 10 33631-Sabd 1055376-2182384Document10 pages10 33631-Sabd 1055376-2182384rose1999.rjNo ratings yet
- s40368 021 00631 4Document14 pagess40368 021 00631 4سارة العبيديNo ratings yet
- 4 Master ArticleDocument8 pages4 Master Articleneetika guptaNo ratings yet
- Int Endodontic J - 2023 - DuncanDocument58 pagesInt Endodontic J - 2023 - DuncanAli FaridiNo ratings yet
- Eos 130 0Document10 pagesEos 130 0Jacqueline FelipeNo ratings yet
- Entry Reentry, Allied, and Alternative Careers An IWLC Working Group ReportDocument2 pagesEntry Reentry, Allied, and Alternative Careers An IWLC Working Group ReportMega Arti UtamiNo ratings yet
- Future Dental Journal: E.A. Abdallah, N.E. Metwalli, A.S. BadranDocument7 pagesFuture Dental Journal: E.A. Abdallah, N.E. Metwalli, A.S. BadranNoviyana Idrus DgmapatoNo ratings yet
- Jurnal 5, EAPD - ECC - Management - 2016,, Best Clinical Practice Guidance For Management of Early CariesDocument10 pagesJurnal 5, EAPD - ECC - Management - 2016,, Best Clinical Practice Guidance For Management of Early CariesZulccPaluNo ratings yet
- Hopcraft Et Al-2008-Australian Dental Journal PDFDocument7 pagesHopcraft Et Al-2008-Australian Dental Journal PDFtea metaNo ratings yet
- Palliative Dental 2014Document6 pagesPalliative Dental 2014Isteicy CortezNo ratings yet
- Erosion Guidelines - 2021 - V4 - MJDocument32 pagesErosion Guidelines - 2021 - V4 - MJAARON DIAZ RONQUILLONo ratings yet
- Oral Health ElderlyDocument2 pagesOral Health ElderlyatikramadhaniNo ratings yet
- association_between_mouth_breathing_habit_and_dental_cariesa_retrospectiveDocument5 pagesassociation_between_mouth_breathing_habit_and_dental_cariesa_retrospectiveHaider AltahanNo ratings yet
- Treatment Planning in Restorative Dentistry and Implant ProsthodonticsFrom EverandTreatment Planning in Restorative Dentistry and Implant ProsthodonticsNo ratings yet
- Ribba2006 Mathematical Model For CancerDocument19 pagesRibba2006 Mathematical Model For CancerAna-Maria DucuNo ratings yet
- Extrusion Bioprinting of Soft Materials: An Emerging Technique For Biological Model FabricationDocument31 pagesExtrusion Bioprinting of Soft Materials: An Emerging Technique For Biological Model FabricationAna-Maria DucuNo ratings yet
- Nanodiamonds 2019Document7 pagesNanodiamonds 2019Ana-Maria DucuNo ratings yet
- The Effects of Annealing Temperature On The Permittivity and Electromagnetic Attenuation Performance of Reduced Graphene OxideDocument6 pagesThe Effects of Annealing Temperature On The Permittivity and Electromagnetic Attenuation Performance of Reduced Graphene OxideAna-Maria DucuNo ratings yet
- Demonstration Of Β- (Alxga1-X) 2O3/Ga2O3 Double Heterostructure Field Effect TransistorsDocument6 pagesDemonstration Of Β- (Alxga1-X) 2O3/Ga2O3 Double Heterostructure Field Effect TransistorsAna-Maria DucuNo ratings yet
- Dendron Conjugated Graphene Oxide For Efficient Gene DeliveryDocument17 pagesDendron Conjugated Graphene Oxide For Efficient Gene DeliveryAna-Maria DucuNo ratings yet
- Spanget Larsen2019Document18 pagesSpanget Larsen2019Ana-Maria DucuNo ratings yet
- 1 s2.0 S1369702118312422 MainDocument9 pages1 s2.0 S1369702118312422 MainAna-Maria DucuNo ratings yet
- 10 1016@j Mtbio 2019 100002Document8 pages10 1016@j Mtbio 2019 100002Ana-Maria DucuNo ratings yet
- Hybrid Biomicromotors: Articles You May Be Interested inDocument24 pagesHybrid Biomicromotors: Articles You May Be Interested inAna-Maria DucuNo ratings yet
- Stretchable Sensors For EnvironmentalDocument24 pagesStretchable Sensors For EnvironmentalAna-Maria DucuNo ratings yet
- 1 s2.0 S0167577X13010252 MainDocument3 pages1 s2.0 S0167577X13010252 MainAna-Maria DucuNo ratings yet
- Correlation Between Dislocations and Leakage Current of P-N Diodes On A Free-Standing Gan SubstrateDocument5 pagesCorrelation Between Dislocations and Leakage Current of P-N Diodes On A Free-Standing Gan SubstrateAna-Maria DucuNo ratings yet
- 1 s2.0 S135964621730101X MainDocument5 pages1 s2.0 S135964621730101X MainAna-Maria DucuNo ratings yet
- Wireless Power Transfer Inspired by The Modern Trends in ElectromagneticsDocument20 pagesWireless Power Transfer Inspired by The Modern Trends in ElectromagneticsAna-Maria DucuNo ratings yet
- A Gas Sensor Array For The Simultaneous Detection of Multiple VocsDocument8 pagesA Gas Sensor Array For The Simultaneous Detection of Multiple VocsAna-Maria DucuNo ratings yet
- 1 s2.0 S0042207X17300544 MainDocument19 pages1 s2.0 S0042207X17300544 MainAna-Maria DucuNo ratings yet
- Food Analysis Efa Fat Protein Net Carbs Sugar 3 1 19Document7 pagesFood Analysis Efa Fat Protein Net Carbs Sugar 3 1 19Ana-Maria DucuNo ratings yet
- 1-S2.0-S0143720818319612-Main - Art Chromo Sensor 2018Document7 pages1-S2.0-S0143720818319612-Main - Art Chromo Sensor 2018Ana-Maria DucuNo ratings yet
- Oe 27 24 34803Document21 pagesOe 27 24 34803Ana-Maria DucuNo ratings yet
- 1 s2.0 S0030402621008779 MainDocument11 pages1 s2.0 S0030402621008779 MainAna-Maria DucuNo ratings yet
- 1 s2.0 S0003267021000313 MainDocument6 pages1 s2.0 S0003267021000313 MainAna-Maria DucuNo ratings yet
- How To Write An Expert Opinion LetterDocument3 pagesHow To Write An Expert Opinion LetterAna-Maria DucuNo ratings yet
- 1 s2.0 S0265931X17309888 MainDocument7 pages1 s2.0 S0265931X17309888 MainAna-Maria DucuNo ratings yet
- Origin of Negative Anomalous Nernst Thermopower in Mn-Ga Ordered AlloysDocument7 pagesOrigin of Negative Anomalous Nernst Thermopower in Mn-Ga Ordered AlloysAna-Maria DucuNo ratings yet
- 1 s2.0 S0003267015008442 MainDocument8 pages1 s2.0 S0003267015008442 MainAna-Maria DucuNo ratings yet
- Modifications in The Nanoparticle-Protein Interactions For Tuning The Protein Adsorption and Controlling The Stability of ComplexesDocument8 pagesModifications in The Nanoparticle-Protein Interactions For Tuning The Protein Adsorption and Controlling The Stability of ComplexesAna-Maria DucuNo ratings yet
- 1 s2.0 S0038092X20312573 MainDocument10 pages1 s2.0 S0038092X20312573 MainAna-Maria DucuNo ratings yet
- NSA 333467 Prospective Application of Nanoparticles Green Synthesized UDocument17 pagesNSA 333467 Prospective Application of Nanoparticles Green Synthesized UAna-Maria DucuNo ratings yet
- Ef Ficient Spin Excitation Via Ultrafast Damping-Like Torques in AntiferromagnetsDocument7 pagesEf Ficient Spin Excitation Via Ultrafast Damping-Like Torques in AntiferromagnetsAna-Maria DucuNo ratings yet
- ĐỀ 02 thptqgDocument6 pagesĐỀ 02 thptqgHà Vy NguyễnNo ratings yet
- Keywords:-Data Collection and Evaluation, UKGSDocument11 pagesKeywords:-Data Collection and Evaluation, UKGSInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Composite in Everyday Practice - How To Choose The Right Material and Simplify Application Techniques in The Anterior TeethDocument24 pagesComposite in Everyday Practice - How To Choose The Right Material and Simplify Application Techniques in The Anterior TeethTania Azuara100% (1)
- Habits and Social Norms Leading To Childhood CariesDocument16 pagesHabits and Social Norms Leading To Childhood Cariesapi-522555065No ratings yet
- NP 1Document73 pagesNP 1Aldous SerranoNo ratings yet
- Toothpaste Consumer SurveyDocument6 pagesToothpaste Consumer SurveyVishakha BhosaleNo ratings yet
- Journal Pone 0208246 PDFDocument12 pagesJournal Pone 0208246 PDFMirza AryantoNo ratings yet
- PT Pauh Mandiri Sejahtera: Jl. Manggis Raya No 41 RT 28 RW 06, Panorama, Singaran Pati, Kota Bengkulu, 38226Document3 pagesPT Pauh Mandiri Sejahtera: Jl. Manggis Raya No 41 RT 28 RW 06, Panorama, Singaran Pati, Kota Bengkulu, 38226AINANo ratings yet
- Bookstyle ContentDocument17 pagesBookstyle ContentCindy SaquilonNo ratings yet
- Planning For A Health Career: Unit 4Document34 pagesPlanning For A Health Career: Unit 4Lanie Tamacio BadayNo ratings yet
- Brand Analysis - PepsodentDocument15 pagesBrand Analysis - PepsodentSamirNo ratings yet
- ChildrenDocument2 pagesChildrendentdeepNo ratings yet
- Soumya Prajapati MNI PROJECTDocument36 pagesSoumya Prajapati MNI PROJECTUplaksh KumarNo ratings yet
- Seniors' Oral Care:: A Guide For Personal Support WorkersDocument40 pagesSeniors' Oral Care:: A Guide For Personal Support WorkersAvina Anin NasiaNo ratings yet
- Local Media2398984275540957743Document27 pagesLocal Media2398984275540957743Rey YuyNo ratings yet
- Assessment of Periodontal Status in Patients With Rheumatoid Arthritis in Kelantan, Malaysia: A Preliminary StudyDocument5 pagesAssessment of Periodontal Status in Patients With Rheumatoid Arthritis in Kelantan, Malaysia: A Preliminary StudyemmypuspitasariNo ratings yet
- Mohammad Ali LeghariDocument64 pagesMohammad Ali LeghariNaoNo ratings yet
- Lesson PlanDocument4 pagesLesson Planpsuliongrl1659No ratings yet
- CariesCare-International Consensus-Manuscript BDJ-corrected 12062019Document13 pagesCariesCare-International Consensus-Manuscript BDJ-corrected 12062019pocket4love4yeahNo ratings yet
- Pregnancy CengizDocument10 pagesPregnancy Cengizkirana_patrolinaNo ratings yet
- Case Study 1Document5 pagesCase Study 1api-612911534No ratings yet
- 3patient History C.C, Dent HX, Habits 2Document21 pages3patient History C.C, Dent HX, Habits 2ابو العزNo ratings yet
- Personal Hygiene: Mr. Genesis Arn M. Latido, RN InstructorDocument41 pagesPersonal Hygiene: Mr. Genesis Arn M. Latido, RN InstructorJohn David Seven RocamoraNo ratings yet
- Catalogue PierrotDocument44 pagesCatalogue PierrotGuntur SetiawanNo ratings yet
- Stephen Legaspi CsaDocument15 pagesStephen Legaspi CsaKhristian Joshua G. JuradoNo ratings yet
- Toothbrush Its Design and Modifications An OvervieDocument9 pagesToothbrush Its Design and Modifications An OvervierklonNo ratings yet
- Manual Vs ElectricDocument5 pagesManual Vs ElectricnasyaNo ratings yet