Professional Documents
Culture Documents
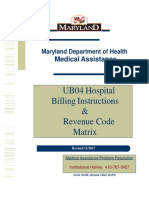
Ub04 Instructions
Ub04 Instructions
Uploaded by
krishna EnagaluruOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ub04 Instructions
Ub04 Instructions
Uploaded by
krishna EnagaluruCopyright:
Available Formats
UB-04 CLAIM FORM INSTRUCTIONS
FIELD
FIELD NAME INSTRUCTIONS
NUMBER
1 Billing Provider Name & Enter the name and address of the hospital/facility
Address submitting the claim.
2 Pay to Address Pay to address if different than field 1.
3a Patient Control Number Enter your facility's unique account number
assigned to the patient, up to 20 alpha/numeric
characters. This number will be printed on the RA
and will help you identify the patient.
3b Medical Record Number Number assigned to patient’s medical record by
provider. Up to 30 alpha/numeric characters. (see
above)
4 Type of Bill Enter the four digit code that identifies the specific type
of bill and frequency of submission. The first digit is a
leading zero. See National Uniform Billing
Committee for guidelines.
5 Federal Tax Number Enter the facility's tax identification number.
6 Statement Covers Period Enter the beginning and ending service dates of
for the period covered on the claim in MMDDYY
format.
PR0041 V1.5 01/25/18
7 Administrative Necessary Days Not required
8b Patient Name Enter the patient's name exactly as it is spelled
on the Medicaid ID card using the Last, First name, MI
format.
9 Patient Address Enter the patient’s mailing address including
street address, city, state and zip code.
10 Birth Date Enter the patient's date of birth in MMDDCCYY
format.
11 Sex Enter "M" for Male, "F" for Female or "U" for
unknown.
12 Admission Date Enter the start date of this episode of care. Use the
MMDDCCYY format.
13 Admission Hour Enter the hour (using a two-digit code below) that
the patient entered the facility.
1:00 a.m. - 01 2:00 a.m. - 02
3:00 a.m. - 03 4:00 a.m. - 04
5:00 a.m. - 05 6:00 a.m. - 06
7:00 a.m. - 07 8:00 a.m. - 08
9:00 a.m. - 09 10:00 a.m. - 10
11:00 a.m. – 11 12:00 noon - 12
1:00 p.m. - 13 2:00 p.m. - 14
3:00 p.m. - 15 4:00 p.m. - 16
5:00 p.m. - 17 6:00 p.m. - 18
7:00 p.m. - 19 8:00 p.m. - 20
9:00 p.m. - 21 10:00 p.m. - 22
11:00 p.m. - 23 12:00 a.m. – 00
14 Admit Type Enter one of the following primary reason for
admission codes:
1 = Emergency
2 = Urgent
3 = Elective
PR0041 V1.5 01/25/18
4 = Newborn
5 = Trauma
9 = Information Not Available
15 Source of Admission Enter one of the following source of admission
codes:
1 = Physician Referral
2 = Clinic Referral
3 = HMO Referral
4 = Transfer from Hospital
5 = Transfer from SNF
6 = Transfer From Another Health Care Facility
7 = Emergency Room
8 = Court/Law Enforcement
9 = Information Not Available
In the Case of Newborn
1 = Normal Delivery
2 = Premature Delivery
3 = Sick Baby
4 = Extramural Birth
16 Discharge Hour Enter the hour (using a two-digit code below) that
the patient was discharged from the facility.
1:00 a.m. - 01 2:00 a.m. - 02
3:00 a.m. - 03 4:00 a.m. - 04
5:00 a.m. - 05 6:00 a.m. - 06
7:00 a.m. - 07 8:00 a.m. - 08
9:00 a.m. - 09 10:00 a.m. - 10
11:00 a.m. - 11 12:00 noon - 12
1:00 p.m. - 13 2:00 p.m. - 14
3:00 p.m. - 15 4:00 p.m. - 16
5:00 p.m. - 17 6:00 p.m. - 18
7:00 p.m. - 19 8:00 p.m. - 20
9:00 p.m. - 21 10:00 p.m. - 22
11:00 p.m. - 23 12:00 a.m. – 00
17 Patient Discharge Status Enter the two-digit code for the patient's status (as of
the "through" date). See NUBC manual for specific
codes.
PR0041 V1.5 01/25/18
18-28 Condition Codes Enter two digit alpha numeric codes up to eleven
occurrences to identify conditions that may affect
processing of this claim. See NUBC manual for
specific codes.
29 Accident State Enter two-digit state abbreviation, if applicable.
30 Accident Date Date accident occurred, if applicable in MMDDYY
31-34 Occurrence Codes and Enter up to four code(s) and associated date(s) for
Dates any significant event(s) that may affect processing
of this claim in format MMDDYY. See NUBC
manual for specific codes.
35-36 Occurrence Span Enter the span of occurrence dates as indicated in
31 – 35 in MMDDYY format.
37 Not Required
38 Responsible Party Name and Enter the responsible party name and address. Name
Address should be entered in Last name, First name, MI format.
39 - 41 Value Code and Amount Enter up to three value codes to identify special
circumstances that may affect processing of this
claim, if applicable. See NUBC manual for specific
codes.
In the Amount box, enter the number, amount, or
UCR value associated with that code.
42 Revenue Code Maximum allowed lines per claim is 92.
42 Revenue Code Enter a four digit Revenue Code beside each
service described in column 43.
The first digit is a leading zero. See NUBC manual
for specific codes.
After the last Revenue Code, enter "0001"
corresponding with the Total Charges amount in
column 47. (PAPER CLAIMS ONLY)
PR0041 V1.5 01/25/18
43 Description Enter a brief description that corresponds to the
Revenue Code in column 42.
List applicable NDC if field 44 is a J code which
requires an NDC (see current J Code table).
Report the N4 qualifier in the first two (2)
positions, left justified, followed immediately by
the 11 character NDC number. Immediately
following the last character of the NDC (no space)
the Unit of Measurement Qualifier immediately
followed by the quantity with a floating decimal
with a limit of 3 characters to the right of the
decimal point.
Unit of Measurement:
F2 - International Unit
GR - Gram
ML - Milliliter
UN - Unit
To report more than one NDC per HCPC use the
NDC attachment form.
44 HCPC Utilized for outpatient bills.
If billing for an injectable code must display an NDC in
field 43, if J code entered requires an NDC (see J code
table).
45 Service Date Enter the date this service was provided in MMDDYY
format.
46 Service Units Enter the number of hospital accommodation days or
units of service (such as pints of blood) which were
rendered.
PR0041 V1.5 01/25/18
47 Total Charges Enter the total amount charged for each line of
service. Also, enter the total of all charges after
the last amount in this column.
48 Non-Covered Charges Enter the amount, if any that is not covered by the
primary payer for this service.
50 Payer Enter the three-digit carrier code and name of the
primary payer on line A and other payers on lines
B and C. (Medicaid is always the payer of last resort.)
If the patient has Medicaid only, enter “RI
Medicaid” on line A.
If Medicare is the primary payer, indicate Part A
or Part B coverage. Carrier codes are found at:
http://www.eohhs.ri.gov/Portals/0/Uploads/Documents/
carrier_code.pdf
51 Health Plan ID The number used by the health plan to identify
itself. Carrier codes are found at:
http://www.eohhs.ri.gov/Portals/0/Uploads/Documents/
carrier_code.pdf
52 Release of Information Enter "Y" for yes or "N" for no.
53 Assignment of Benefits Enter "Y" for yes.
54 Prior Payments Enter the amounts paid by the other insurance
payers listed in field 50, if applicable. If payment is
made by other insurance, proof of payment (e.g.,
EOB) must be attached to the claim form.
55 Estimated Amount Due The amount estimated to be due.
56 National Provider Identifier Unique identifier assigned to the provider. Seven
Billing Provider (NPI) digit RI Medicaid Provider ID if not
submitting NPI.
PR0041 V1.5 01/25/18
57 Other Provider Identifier Taxonomy must be entered if NPI is entered in
field 56. This ID must be entered in line A,B,C that
corresponds to the line in which the “RI Medicaid”
payer information is entered in field 50.
58 Insured's Name If other health insurance is involved, enter the
insured's name.
59 Patient's Relationship to Insured Enter the code for the patient's relationship to the
insured.
01 = Spouse
18 = Self
19= Child
20 = Employee
21 = Unknown
39 = Organ Donor
40 = Cadaver Donor
53 = Life Partner
G8 = Other Relationship
60 Insured’s Unique Identifier Enter recipient's Medicaid ID.
This ID must be entered in line A,B,C that
corresponds to the line in which the RI Medicaid
payer information is entered in field 50.
1234567890
61 Group Name Enter the name of insured's other group health
coverage, if applicable.
62 Insurance Group Number Enter insured's group number, if applicable.
63 Treatment Authorization Number that designates that treatment has been
Number Authorized, if applicable.
64 Document Control Number Control number assigned to the original bill.
65 Employer Name Name of employer providing health coverage.
66 Diagnosis and Procedure Code Enter 9 for ICD 9 coding or 0 for ICD-10 coding
Qualifier depending on date(s) of service.
67 Principal Diagnosis Code on Enter the appropriate ICD diagnosis code that describes
Admission the nature of the illness or injury.
PR0041 V1.5 01/25/18
67A - Q Other Diagnosis Codes Enter up to 16 ICD codes for other
diagnoses.
68 Not Required
69 Admitting Diagnosis Code Enter the ICD diagnosis code that describes the
patient’s condition at the time of admission.
70 Patient’s Reason for Visit Enter the ICD diagnosis code that describes the
patient’s reason for visit.
71 PPS Code Not Required
72 External Cause of Injury Code Enter the ICD diagnosis code pertaining to external
cause of injuries.
74 Principal Procedure Code and Enter the ICD code that identifies the principal
Date procedure performed. Enter the date of that
procedure.
74A-E Other Procedure Codes Enter other ICD codes identifying all significant
procedures performed. Enter the date of those
procedures.
75 Not Required
76 Attending Provider Name and Enter NPI of individual in charge of patient care.
Identifiers If UPIN number is entered, qualifier must be 1G.
Enter the last and first name below.
77 Operating Physician Name and Required when surgical procedure is performed.
Identifiers Enter the NPI. If UPIN number is entered,
qualifier must be 1G. Enter the last and first
name.
78 Other Provider Name and Enter the NPI. If UPIN number is entered,
Identifiers qualifier must be 1G. Enter the last and first
name.
79 Other Provider Identifier If required for your provider type, enter the NPI for the
Ordering, Referring, or Prescribing provider.
80 Remarks Field/Signature Enter the provider signature or authorized agent’s
original signature. Stamps, copies, or initials are not
acceptable. Must be an original signature.
81cc Code-Code Field Enter B3 in the qualifier if fields 76-79 contain an NPI.
Enter the corresponding provider taxonomy of
provider NPI’s entered in locations
76a – 81CCa
PR0041 V1.5 01/25/18
77b – 81CCb
78c – 81CCc
79d – 81CCd
PR0041 V1.5 01/25/18
You might also like
- Form - Bupa Claim FormDocument2 pagesForm - Bupa Claim FormJoe Sayavongsa100% (3)
- Ansi Bhma A156.40 2015 PDFDocument34 pagesAnsi Bhma A156.40 2015 PDFShawn DeolNo ratings yet
- CMS 1450 (UB 04) InstructionsDocument12 pagesCMS 1450 (UB 04) InstructionsKarna Palanivelu67% (3)
- HSTP II HMIS Hospital Heath Centre and Health PostDocument367 pagesHSTP II HMIS Hospital Heath Centre and Health PostDagmawitNo ratings yet
- PNC - A3-1Document5 pagesPNC - A3-1dabashgetNo ratings yet
- UB-04 Claim Form InstructionsDocument10 pagesUB-04 Claim Form InstructionsJonna CaballeroNo ratings yet
- Medical Report and ReceiptDocument5 pagesMedical Report and Receiptkumarsam087No ratings yet
- NTUC Pa Paid Claim Form (08 2017)Document5 pagesNTUC Pa Paid Claim Form (08 2017)pat5355No ratings yet
- ME In-G Ie: Claim FormDocument4 pagesME In-G Ie: Claim FormnithiananthiNo ratings yet
- Cpahb HospitalDocument6 pagesCpahb HospitalHihiNo ratings yet
- Health Premium PlatinumDocument3 pagesHealth Premium Platinumகமலேஷ் குமார்No ratings yet
- ERP Assignment 103Document10 pagesERP Assignment 103Ralph SoansNo ratings yet
- Genins Claim Form (New)Document3 pagesGenins Claim Form (New)pratikwagh112002No ratings yet
- Health Center/Clinic/Hospital: Out Patient Department (OPD) RegisterDocument4 pagesHealth Center/Clinic/Hospital: Out Patient Department (OPD) RegisterGetu Tadele100% (2)
- Medical Insurance Claim Form (Corporate)Document3 pagesMedical Insurance Claim Form (Corporate)hari198902234No ratings yet
- Claim Form & Other Documents To Be Submitted To Lic Branch/ Divisional Offices OnlyDocument1 pageClaim Form & Other Documents To Be Submitted To Lic Branch/ Divisional Offices OnlyAnonymous W9VINoTza100% (1)
- Medical and Vision Claim Form en 06 - 2018Document2 pagesMedical and Vision Claim Form en 06 - 2018andreas widyoNo ratings yet
- Healt Form LatestDocument9 pagesHealt Form LatestSadab AhmadNo ratings yet
- Certificate of Hospital Treatment - 17062019Document2 pagesCertificate of Hospital Treatment - 17062019Everest HospitalNo ratings yet
- AUS Bupa Global Claim Form EN APR21 0028299Document8 pagesAUS Bupa Global Claim Form EN APR21 0028299ALJABERNo ratings yet
- Claims Reimbursement Form: Member General InformationDocument1 pageClaims Reimbursement Form: Member General InformationHarold TanNo ratings yet
- Linelist Register For HIV POS PBFA and HEIs - Oct 2023Document12 pagesLinelist Register For HIV POS PBFA and HEIs - Oct 2023Migori ArtNo ratings yet
- Form BUPADocument4 pagesForm BUPAterusunduhNo ratings yet
- Bupa Global Claim FormDocument8 pagesBupa Global Claim FormALJABERNo ratings yet
- Bupa International Claim Form: 1 Patient'S DetailsDocument4 pagesBupa International Claim Form: 1 Patient'S DetailsRealty SolutionsNo ratings yet
- Aditya Birla Health Insurance Co. LimitedDocument4 pagesAditya Birla Health Insurance Co. LimitedAdeep MathurNo ratings yet
- 2-GMC Claim Check - ListDocument2 pages2-GMC Claim Check - ListChayan HalderNo ratings yet
- CF05b Path Accident and Sickness Medical ES ADocument3 pagesCF05b Path Accident and Sickness Medical ES ARedención Apostol SantiagoNo ratings yet
- Crisis Cover Kids Claim FormDocument16 pagesCrisis Cover Kids Claim FormHihiNo ratings yet
- Domiciliary Treatment - Claim Form - Borl: Details of Primary InsuredDocument1 pageDomiciliary Treatment - Claim Form - Borl: Details of Primary InsuredHimanshu Chouksey100% (1)
- NEW Domiciliary Claim Form PDFDocument1 pageNEW Domiciliary Claim Form PDFHimanshu ChoukseyNo ratings yet
- MSE Clinical Observer Application April 2021 v2Document6 pagesMSE Clinical Observer Application April 2021 v2M. GNo ratings yet
- Claim - Form - MediassitDocument4 pagesClaim - Form - MediassitKashish BangaloreNo ratings yet
- New MRD PresentationDocument40 pagesNew MRD PresentationBAHHEP BAHHEPNo ratings yet
- 5 6212887793887085843 PDFDocument11 pages5 6212887793887085843 PDFeruditeNo ratings yet
- Icmr Specimen Referral Form For Covid-19 (Sars-Cov2) : (If Yes, Attach Prescription If No, Test Cannot Be Conducted)Document3 pagesIcmr Specimen Referral Form For Covid-19 (Sars-Cov2) : (If Yes, Attach Prescription If No, Test Cannot Be Conducted)Aakansha GuptaNo ratings yet
- Claims Reimbursement Form: Member General InformationDocument1 pageClaims Reimbursement Form: Member General InformationFirmament DevelopmentNo ratings yet
- Itemized Sample Billing StatementDocument2 pagesItemized Sample Billing StatementAriel CruzNo ratings yet
- The Oriental Insurance Company Limited: Hospitalisation and Domiciliary Hospitalisation Benefit Policy Claim FormDocument5 pagesThe Oriental Insurance Company Limited: Hospitalisation and Domiciliary Hospitalisation Benefit Policy Claim FormMallesh ArjaNo ratings yet
- House Job Application Form 2020Document3 pagesHouse Job Application Form 2020fatimabakhsh419No ratings yet
- Mumbai Claim FormDocument5 pagesMumbai Claim FormsunsangraNo ratings yet
- Medical OpinionDocument1 pageMedical OpinionefmezahnNo ratings yet
- D StatmentDocument8 pagesD StatmentHihiNo ratings yet
- SGP Generic Claim FormDocument5 pagesSGP Generic Claim FormSanny HamdaniNo ratings yet
- IRDAI Registration No. 103. Reliance General Insurance Company LimitedDocument2 pagesIRDAI Registration No. 103. Reliance General Insurance Company LimitedSumit BhallaNo ratings yet
- Maid Claim FormDocument4 pagesMaid Claim FormHihiNo ratings yet
- Hospital Benefit Claim FormDocument7 pagesHospital Benefit Claim FormEmmanuel MichaelNo ratings yet
- Claims Reimbursement Form (For MRC) : Member General Information (Required)Document2 pagesClaims Reimbursement Form (For MRC) : Member General Information (Required)lecky youNo ratings yet
- In-Patient Claim Form: (To Be Filled by Claimant Employee)Document2 pagesIn-Patient Claim Form: (To Be Filled by Claimant Employee)Khan LalaNo ratings yet
- Claim Submission Checklist - pdf4454101871738174528Document2 pagesClaim Submission Checklist - pdf4454101871738174528Bireswar SamajpatiNo ratings yet
- 1 Claim FormDocument36 pages1 Claim Formkarmayukh1No ratings yet
- Laporan Lampiran Ba Kesesuaian KlinikDocument5 pagesLaporan Lampiran Ba Kesesuaian KlinikYENI AYU OKTAVIANo ratings yet
- Insurance Claim FormDocument9 pagesInsurance Claim FormRahmaNo ratings yet
- DME Medical Billing Book 1662598386Document46 pagesDME Medical Billing Book 1662598386Nelson ANo ratings yet
- Clinical Face Sheet: 8 40 - A.M. - P.M. - A.M. - P.MDocument21 pagesClinical Face Sheet: 8 40 - A.M. - P.M. - A.M. - P.MRyrey Abraham PacamanaNo ratings yet
- Hospitalization Reimbursment Claim FormDocument4 pagesHospitalization Reimbursment Claim FormFarhan aliNo ratings yet
- Cross-Training: The Medical Assistant WorkbookFrom EverandCross-Training: The Medical Assistant WorkbookNo ratings yet
- Credit Report Secrets: How to Understand What Your Credit Report Says About You and What You Can Do About It!From EverandCredit Report Secrets: How to Understand What Your Credit Report Says About You and What You Can Do About It!Rating: 1 out of 5 stars1/5 (2)
- 2018 Fidelis Care Medicare Advantage Dual Advantage Provider Tip SheetDocument2 pages2018 Fidelis Care Medicare Advantage Dual Advantage Provider Tip Sheetkrishna EnagaluruNo ratings yet
- Welcome To HDFC Bank NetBankingDocument2 pagesWelcome To HDFC Bank NetBankingkrishna EnagaluruNo ratings yet
- Ab 02142Document6 pagesAb 02142krishna EnagaluruNo ratings yet
- 2017 UB04 Hospital Instructions-Final 8FEB2018Document99 pages2017 UB04 Hospital Instructions-Final 8FEB2018krishna EnagaluruNo ratings yet
- Hospital Billing ScenariosDocument7 pagesHospital Billing Scenarioskrishna EnagaluruNo ratings yet
- CMS 2022 C2C RTBC EOB English 8 5X11 V4Document1 pageCMS 2022 C2C RTBC EOB English 8 5X11 V4krishna EnagaluruNo ratings yet
- Module 5 Rle - EvaluationDocument3 pagesModule 5 Rle - EvaluationKyle VargasNo ratings yet
- Principles of Learning and Motivation Part 2Document3 pagesPrinciples of Learning and Motivation Part 2Tobs AnchetaNo ratings yet
- DLL 10 - BioenergeticsDocument3 pagesDLL 10 - BioenergeticsJennifer Magango100% (1)
- Peripheral Testosterone MetabolismDocument8 pagesPeripheral Testosterone MetabolismAgung SentosaNo ratings yet
- Consolidated Teachers Individual Plan For Professional Development SCHOOL YEAR 2020-2021Document2 pagesConsolidated Teachers Individual Plan For Professional Development SCHOOL YEAR 2020-2021Anicadlien Ellipaw IninNo ratings yet
- PDBA Operations Course OutlineDocument12 pagesPDBA Operations Course OutlineQasim AbrahamsNo ratings yet
- Tagbino National High SchoolDocument2 pagesTagbino National High SchooldarelleNo ratings yet
- nnsm322m PDFDocument22 pagesnnsm322m PDFTLTPSNo ratings yet
- Application of IntegralsDocument14 pagesApplication of IntegralsSanjayNo ratings yet
- Writing Research Papers James D Lester PDFDocument4 pagesWriting Research Papers James D Lester PDFgahebak1mez2100% (1)
- 3 Phase Full Wave Bridge ConverterDocument4 pages3 Phase Full Wave Bridge Convertersubhasishpodder100% (1)
- Agrirobot PDFDocument103 pagesAgrirobot PDFMuhamad Azlan ShahNo ratings yet
- Vyshali Java ResumeDocument5 pagesVyshali Java ResumeKiran N9 ITNo ratings yet
- Machine (Mechanical) - Wikipedia, The Free EncyclopediaDocument10 pagesMachine (Mechanical) - Wikipedia, The Free EncyclopediabmxengineeringNo ratings yet
- Safir 9 Tonearm ManualDocument14 pagesSafir 9 Tonearm Manualmoma52No ratings yet
- Research Methodology - 9Document12 pagesResearch Methodology - 9OmeYadavNo ratings yet
- Green Ghost Chronicles - The Lost Book Outline - Tom Furman FitnessDocument49 pagesGreen Ghost Chronicles - The Lost Book Outline - Tom Furman Fitnessbarna284100% (1)
- Configure Anyconnect 00Document22 pagesConfigure Anyconnect 00Ruben VillafaniNo ratings yet
- Bus FestoDocument82 pagesBus FestoraphvalonNo ratings yet
- Encoder Serie Ria-40Document6 pagesEncoder Serie Ria-40Carlos NigmannNo ratings yet
- Harmonization of Strategic PlansDocument47 pagesHarmonization of Strategic PlansLisette Senoc-GarciaNo ratings yet
- Lesson Plan ON OxytocicsDocument18 pagesLesson Plan ON Oxytocicsrenu100% (2)
- Instron Low Velocity Impact TesterDocument179 pagesInstron Low Velocity Impact TesterEmre GuneyNo ratings yet
- SPM (SEN 410) Lecturer HandoutsDocument51 pagesSPM (SEN 410) Lecturer HandoutsinzovarNo ratings yet
- 459 - So FG13Document5 pages459 - So FG13ronni gunadi sNo ratings yet
- Prospective vs. Retrospective Delay Analysis: Rohit Singhal, Shishir Kant & Adarsh KumarDocument10 pagesProspective vs. Retrospective Delay Analysis: Rohit Singhal, Shishir Kant & Adarsh KumarKevin DonNo ratings yet
- CMACGM Service Description ReportDocument58 pagesCMACGM Service Description ReportMarius MoraruNo ratings yet
- Thesis Format Iit KanpurDocument7 pagesThesis Format Iit Kanpurvictoriathompsonaustin100% (2)
- Modal Adverb Lesson PlanDocument4 pagesModal Adverb Lesson Planapi-587326479100% (1)