Professional Documents
Culture Documents
Article 1
Article 1
Uploaded by
Fakhar Mahmood ShahidCopyright:
Available Formats
You might also like
- Digoxin: Mechanism of ActionDocument4 pagesDigoxin: Mechanism of ActionahmedNo ratings yet
- Assessment of Palpitation Complaints Benign Paroxysmal Positional VertigoDocument6 pagesAssessment of Palpitation Complaints Benign Paroxysmal Positional VertigoHappy PramandaNo ratings yet
- T Wave Alternans For Ventricular Arrhythmia Risk StratificationDocument5 pagesT Wave Alternans For Ventricular Arrhythmia Risk StratificationSalim VelaniNo ratings yet
- Effect of Nocturnal Oxygen Therapy On Electrocardiographic Changes Among Patients With Congestive Heart FailureDocument3 pagesEffect of Nocturnal Oxygen Therapy On Electrocardiographic Changes Among Patients With Congestive Heart FailureNurAfifahNo ratings yet
- Lapkas Pediatrik NLDocument31 pagesLapkas Pediatrik NLHannaTashiaClaudiaNo ratings yet
- AV Bloc Induces TDPDocument13 pagesAV Bloc Induces TDPMirza AlfiansyahNo ratings yet
- In-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisDocument15 pagesIn-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisAnonymous OU6w8lX9No ratings yet
- Journal of Nursing: Basic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest RadiographyDocument8 pagesJournal of Nursing: Basic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest RadiographyNiala AlmarioNo ratings yet
- SVT Mayo 2008Document12 pagesSVT Mayo 2008muhanasNo ratings yet
- Therapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticDocument8 pagesTherapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticNITACORDEIRONo ratings yet
- ABC of Clinical Electrocardiography Myocardial IschaemiaDocument6 pagesABC of Clinical Electrocardiography Myocardial IschaemiaShri Mahalaxmi HarishNo ratings yet
- Neonatal and Pediatric Guidelines Arrhythmia ManagementDocument16 pagesNeonatal and Pediatric Guidelines Arrhythmia ManagementAkhmad HidayatNo ratings yet
- Hollamby Mitchell s5001226 Case 1 DtgaDocument13 pagesHollamby Mitchell s5001226 Case 1 Dtgaapi-299009880No ratings yet
- Cardiac ArrhythmiasDocument5 pagesCardiac Arrhythmiastere glezNo ratings yet
- VT SVT AvrDocument3 pagesVT SVT AvragneselimNo ratings yet
- Electrocardiographic and Echocardiographic Changes in Patients With Thyreotoxic CardiopathyDocument4 pagesElectrocardiographic and Echocardiographic Changes in Patients With Thyreotoxic CardiopathySilvia MudrencoNo ratings yet
- Establishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratoryDocument15 pagesEstablishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratorySamuelNo ratings yet
- Electrocardiographic Changes and Intracranial Pathology: Geraldine Syverud, Crna, BSNDocument4 pagesElectrocardiographic Changes and Intracranial Pathology: Geraldine Syverud, Crna, BSNchuck55No ratings yet
- The Tilt Table Test Is Useful For The Diagnosis of Vasovagal Syncope and Should Not Be AbolishedDocument5 pagesThe Tilt Table Test Is Useful For The Diagnosis of Vasovagal Syncope and Should Not Be AbolishedririsNo ratings yet
- 1 s2.0 S0870255121005096 MainDocument3 pages1 s2.0 S0870255121005096 MainangelemanuelarmasNo ratings yet
- Ekg STDocument23 pagesEkg STisaNo ratings yet
- Applications and New InsightsDocument7 pagesApplications and New InsightsPaola CardenasNo ratings yet
- Articles Publishd in JournalsDocument9 pagesArticles Publishd in JournalsHeartHealthNo ratings yet
- Heart 2002 Menon 531 7Document8 pagesHeart 2002 Menon 531 7TriponiaNo ratings yet
- Ijmps - The Value of Holter Monitoring PDFDocument6 pagesIjmps - The Value of Holter Monitoring PDFAnonymous Y0wU6InINo ratings yet
- Memory T-Waves, A Rare Cause of T-Wave Inversion in The Emergency Department - PMCDocument7 pagesMemory T-Waves, A Rare Cause of T-Wave Inversion in The Emergency Department - PMCfiat.2dindaNo ratings yet
- Ecg ManfestationsDocument19 pagesEcg Manfestationsnaxo128No ratings yet
- Practice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaDocument28 pagesPractice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaRully SyahrizalNo ratings yet
- Electrocardiograph Changes in Acute Ischemic Cerebral StrokeDocument6 pagesElectrocardiograph Changes in Acute Ischemic Cerebral StrokeFebniNo ratings yet
- Clinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761Document10 pagesClinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761William LeeNo ratings yet
- Current Concepts in QT ProlongationDocument9 pagesCurrent Concepts in QT ProlongationSuresh KumarNo ratings yet
- Prevalence and Clinical Correlates of QT Prolongation in Patients With Hypertrophic CardiomyopathyDocument7 pagesPrevalence and Clinical Correlates of QT Prolongation in Patients With Hypertrophic CardiomyopathyNITACORDEIRONo ratings yet
- Lapkas VT RevisiDocument13 pagesLapkas VT RevisiRannyNo ratings yet
- Techniques of TIPS in The Treatment of Liver Cirrhosis Combined With Incompletely Occlusive Main Portal Vein ThrombosisDocument9 pagesTechniques of TIPS in The Treatment of Liver Cirrhosis Combined With Incompletely Occlusive Main Portal Vein ThrombosisLeon L GayaNo ratings yet
- Wilbert S. Aronow. Hypertension and Left Ventricular HypertrophyDocument1 pageWilbert S. Aronow. Hypertension and Left Ventricular Hypertrophykorejat unpadNo ratings yet
- Tachyarrhythmias and Defibrillation: Ricardo A. Samson, MD, Dianne L. Atkins, MDDocument21 pagesTachyarrhythmias and Defibrillation: Ricardo A. Samson, MD, Dianne L. Atkins, MDEmilio Emmanué Escobar CruzNo ratings yet
- 3.arrhythmias After CongenitaDocument6 pages3.arrhythmias After Congenitaganda gandaNo ratings yet
- Cerebrovascular Disease From JeffryDocument8 pagesCerebrovascular Disease From JeffryIdrianaNo ratings yet
- ContentServer AspDocument9 pagesContentServer Aspganda gandaNo ratings yet
- Transfusion Associated Circulatory Overload Taco Emma GoodhallDocument5 pagesTransfusion Associated Circulatory Overload Taco Emma GoodhallAthirah M.NoerNo ratings yet
- Basic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest RadiographyDocument7 pagesBasic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest Radiographyrowd1yNo ratings yet
- Tatalaksana Hyponatremia Pada Diuresis Post ObstruktifDocument4 pagesTatalaksana Hyponatremia Pada Diuresis Post ObstruktifGilberto ChafrinaNo ratings yet
- Jardine 2017Document27 pagesJardine 2017Ismi Prasastawati KurniawanNo ratings yet
- Wolsey SlidesCarnivalDocument25 pagesWolsey SlidesCarnivalRaudha JanahNo ratings yet
- Stress-Related Cardiomyopathy or Tako-Tsubo Syndrome: Current ConceptsDocument6 pagesStress-Related Cardiomyopathy or Tako-Tsubo Syndrome: Current ConceptslivroinglesNo ratings yet
- Diagnosis and Management of Splanchnic Ischemia: Ioannis E Koutroubakis, MD, PHD, Assistant Professor of MedicineDocument12 pagesDiagnosis and Management of Splanchnic Ischemia: Ioannis E Koutroubakis, MD, PHD, Assistant Professor of MedicineIgorCotagaNo ratings yet
- Detection AFDocument5 pagesDetection AFDhinny Heksa MarchiaNo ratings yet
- Drug-Induced QT Interval ProlongationDocument13 pagesDrug-Induced QT Interval ProlongationgeoaislaNo ratings yet
- How To Diagnose The Cause of Sudden Cardiac ArrestDocument7 pagesHow To Diagnose The Cause of Sudden Cardiac ArrestTaufik Muhammad JrNo ratings yet
- Paroxysmal Supraventricular TachycardiaDocument3 pagesParoxysmal Supraventricular TachycardiaIqbal Juher MNo ratings yet
- ECG HRV Assignment 19334107Document18 pagesECG HRV Assignment 19334107katehughes332No ratings yet
- Assessment of Pulse Transit Time To Indicate Cardiovascular Changes During Obstetric Spinal AnaesthesiaDocument6 pagesAssessment of Pulse Transit Time To Indicate Cardiovascular Changes During Obstetric Spinal AnaesthesiaprabuNo ratings yet
- Rashid 2021Document10 pagesRashid 2021Carmen Cuadros BeigesNo ratings yet
- Stroke 1982 Myers 838 42Document6 pagesStroke 1982 Myers 838 42Widyawan SyahputraNo ratings yet
- Estenosis Aortica 2016 Aafp 2016Document8 pagesEstenosis Aortica 2016 Aafp 2016Antonio MoncadaNo ratings yet
- ECG Frequency Changes inDocument13 pagesECG Frequency Changes inArief KamilNo ratings yet
- Additional Idea For Litrature (Repaired)Document17 pagesAdditional Idea For Litrature (Repaired)Abrsham AyeleNo ratings yet
- Aortic StenosisDocument11 pagesAortic StenosisIra Anuddin100% (1)
- Electrocardiograma en TóxicologiaDocument19 pagesElectrocardiograma en TóxicologiaLaura GNo ratings yet
- The Perindopril in Elderly PeopleDocument8 pagesThe Perindopril in Elderly PeopleluchititaNo ratings yet
- Coronary Vasomotion AbnormalitiesFrom EverandCoronary Vasomotion AbnormalitiesHiroaki ShimokawaNo ratings yet
- Cardiac Arrest After Cardiac Surgery: An Evidence-Based Resuscitation ProtocolDocument12 pagesCardiac Arrest After Cardiac Surgery: An Evidence-Based Resuscitation ProtocoljoseNo ratings yet
- Hemodynamics E-ConDocument1 pageHemodynamics E-ConpjebinkNo ratings yet
- SuciDocument12 pagesSucisuciNo ratings yet
- Timing of Revascularization in Patients With Transient ST Segment Elevation Myocardial Infarction A Randomized Clinical TrialDocument9 pagesTiming of Revascularization in Patients With Transient ST Segment Elevation Myocardial Infarction A Randomized Clinical TrialWelly WijayaNo ratings yet
- NCM118 TransesDocument11 pagesNCM118 TransesAlejandro Saclolo, IIINo ratings yet
- CT and MR in Cardiology 1St Edition Suhny Abbara Full Chapter PDFDocument69 pagesCT and MR in Cardiology 1St Edition Suhny Abbara Full Chapter PDFflayizouina100% (6)
- Assessment of Heart & Neck VesselsDocument4 pagesAssessment of Heart & Neck VesselsCardio GodNo ratings yet
- Acls Pretest Answer Key: Rhythm Identification (Part I)Document3 pagesAcls Pretest Answer Key: Rhythm Identification (Part I)aditNo ratings yet
- Atrial Fibrillation TDDocument6 pagesAtrial Fibrillation TDapi-594366475No ratings yet
- EKG Card 2Document2 pagesEKG Card 2mulyadiNo ratings yet
- CH17 Cardiac Surgery in The Adult 5th Edition 2018Document26 pagesCH17 Cardiac Surgery in The Adult 5th Edition 2018ChengShiun ShiueNo ratings yet
- PostsDocument6 pagesPostsQusaiBadrNo ratings yet
- Non St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyDocument4 pagesNon St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyKEn PilapilNo ratings yet
- Cardiomyopathies: Cardiomyopathy Is A Heart Muscle Disease Associated With CardiacDocument10 pagesCardiomyopathies: Cardiomyopathy Is A Heart Muscle Disease Associated With Cardiacmerin sunilNo ratings yet
- Government Service Insurance System, Petitioner, vs. ASTRID V. CORRALES, RespondentDocument20 pagesGovernment Service Insurance System, Petitioner, vs. ASTRID V. CORRALES, RespondentMaryland AlajasNo ratings yet
- CHAPTER 11: The History and Physical Examination: An Evidence Based ApproachDocument5 pagesCHAPTER 11: The History and Physical Examination: An Evidence Based ApproachReda SoNo ratings yet
- Del Nido Cardioplegia - What Is The Current Evidence?: Review PaperDocument5 pagesDel Nido Cardioplegia - What Is The Current Evidence?: Review PapermahNo ratings yet
- Electrocar Diogram: College of Nursing Madurai Medical College, Madurai-20 Procedure Demonstration OnDocument19 pagesElectrocar Diogram: College of Nursing Madurai Medical College, Madurai-20 Procedure Demonstration OnValarmathi100% (1)
- Catheter Reprocessing SystemDocument16 pagesCatheter Reprocessing Systemsutan IskandarsyahNo ratings yet
- Dissertationen Online Uni Bonn MedizinDocument8 pagesDissertationen Online Uni Bonn MedizinHelpWithWritingAPaperUK100% (1)
- Bio Essay CardioDocument3 pagesBio Essay CardiopadmaszNo ratings yet
- ECG Definition: - PurposeDocument2 pagesECG Definition: - PurposeJustine Karl Pablico100% (1)
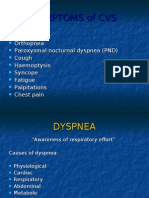
- Symptoms of CvsDocument25 pagesSymptoms of CvsstudymedicNo ratings yet
- Board 14 Desember 2014 Kumpulan FinalDocument73 pagesBoard 14 Desember 2014 Kumpulan FinalAnonymous XHguqDfWR0% (1)
- Pediatric Specialists - Managing The Medical MazeDocument4 pagesPediatric Specialists - Managing The Medical MazePathways AwarenessNo ratings yet
- Risk Factor For Atrial FibrilationDocument19 pagesRisk Factor For Atrial FibrilationDanny Soegianto IINo ratings yet
- CT and MR in Cardiology 1St Edition Suhny Abbara Full ChapterDocument67 pagesCT and MR in Cardiology 1St Edition Suhny Abbara Full Chapterelizabeth.dew603100% (9)
- Programbook IsicamDocument36 pagesProgrambook Isicamadi bestaraNo ratings yet
- Disusun Oleh NS Irvantri Aji Jaya - M.Kep. SP - Kep.M.BDocument26 pagesDisusun Oleh NS Irvantri Aji Jaya - M.Kep. SP - Kep.M.Bsangid yahyaNo ratings yet
Article 1
Article 1
Uploaded by
Fakhar Mahmood ShahidOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Article 1
Article 1
Uploaded by
Fakhar Mahmood ShahidCopyright:
Available Formats
Neth Heart J (2011) 19:3134 DOI 10.
1007/s12471-010-0049-1
REVIEW ARTICLE
ECG Changes in Subarachnoid Haemorrhage: A Synopsis
S. Chatterjee
Published online: 16 December 2010 # Springer Media/Bohn Stafleu van Loghum 2010
Abstract Subarachnoid haemorrhage (SAH) is a neurological emergency with high mortality rates. It is mainly caused by rupture of an aneurysm (congenital/infectious/ traumatic) or rupture of an arteriovenous malformation. Electrocardiograms (ECGs) done in patients with SAH have shown morphological changes as well as arrhythmias. Subarachnoid haemorrhage (SAH) patients have often been misdiagnosed to have cardiac abnormalities based on their ECGs when in many of those instances the ECG change had been the result of the SAH itself. They have led to unnecessary and wasteful investigations and therapies in many occasions. Hence the current article is an effort at consolidating the information available in an attempt to avoid possible errors in diagnosis by house staff and internists. There are two mechanisms that might mediate ECG changes in patients with SAH, i.e. autonomic neural stimulation from the hypothalamus or elevated levels of circulating catecholamine. Hypothalamic stimulation may cause ECG changes without associated myocardial damage whereas elevated catecholamine levels have been correlated with QT-interval prolongation and myocardial damage. Keywords Subarachnoid haemorrhage . Electrocardiogram . Arrhythmias
Significance of ECG Changes Seen in SAH Subarachnoid haemorrhage (SAH) has long been known to be associated with electrocardiogram (ECG) changes [1]. However, the aetiology, pathophysiology and prognosis of underlying cardiac abnormalities remain unexplained to a large extent. Hypothalamic stimulations [2] and autonomic dysfunctions have been linked but not conclusively proven to be causative. These considerations may influence therapeutic interventions as infusions of large volumes of fluids or administrations of vasopressors may prove detrimental in patients with a compromised heart [3]. ECG changes in SAH commonly reflect ischaemic heart disease and have been known to present with ST-segment elevation and T-wave inversion [4]. Therapeutic thrombolytic therapy and anticoagulation as well as withholding of life-saving neurosurgery in such cases may well endanger the life of the patient concerned [4, 5]. SAH has been associated with malignant ventricular arrhythmias, including ventricular tachycardia, torsades de pointes, and ventricular fibrillation, particularly if the corrected QT (QTc) interval is prolonged, often leading to compromise in a haemodynamically unstable patient [6, 7].
Implications
Electronic supplementary material The online version of this article (doi:10.1007/s12471-010-0049-1) contains supplementary material, which is available to authorised users. S. Chatterjee (*) Department of Internal Medicine, Maimonides Medical Center, Apt C11, 864 49th Street, Brooklyn, NY 11220, USA e-mail: saurav.sphs@gmail.com
Documented ECG abnormalities in a patient with SAH who has brain death mean the heart is not accepted as a donor organ because of the possibility of cardiac abnormalities. Greater knowledge about the pathophysiology and management of ECG changes in SAH may make heart donations possible in these cases [8]. Also in
32 Table 1 Morphological changes in ECG in SAH ECG changes High R waves ST depression T-wave abnormalities Large U waves Prolonged QTc Percentages (%) 19 15 32 47 23
Neth Heart J (2011) 19:3134
Morphological ECG Changes In SAH, ST-T wave changes such as associated with myocardial infarction seem to be predominant (Table 1). Other changes seen commonly include presence of a U wave, a Q wave, prolonged QTc intervals and large, flattened or notched T waves [15]. In the largest study [16] to date, a single preoperative 12-lead ECG from each of the 406 patients with SAH was examined. ECG findings included high-amplitude R waves in 19% of subjects, ST depression in 15%, T-wave abnormalities in 32%, U waves greater than 1 mm in amplitude in 47%, and prolonged QTc interval (>440 ms) in 23%. Most of these seem to point to a repolarisation abnormality in SAH patients. Abnormalities involving atrial depolarisation, particularly peaked P waves (>2.5 mm in amplitude) and short PR intervals (<100 ms), have also been reported (Fig. 1) [17, 18].
such a situation it is essential that a proper history is elicited and a thorough physical examination is conducted to rule out SAH and the threshold for ordering diagnostic cerebral imaging should be very low in these instances for thombolysis and anticoagulation may have catastrophic consequences in such patients.
Prevalence of ECG Abnormalities in SAH Rhythm Abnormalities The reported prevalence of ECG changes in patients with SAH ranges from 27% to 100% [3, 812]. Such wide variation may be due to differences in study design, investigators definitions of ECG abnormalities, or the methods used to evaluate ECG changes. Admissions with neurological diagnoses often do not have routine ECGs. Thus, there always remains a possibility of selection bias leading to greater inclusion of subjects who have had cardiac events during their hospitalisation, if ECG tracings are used as inclusion criteria. Also, baseline ECGs were unavailable in many cases making it impossible to differentiate between preexisting changes and de novo events associated with an episode of SAH. Promptness of ECG data collection may influence conclusions. Brouwers et al. [9] found that during the first 72 h after SAH, ECG changes were the most pronounced. Di Pasquale et al. [10] found that 90% of patients had ECG abnormalities within the first 48 h following SAH, suggesting that studies in which surveillance is started later in the course of illness may miss significant data [8]. Due to paucity of follow-up data, the chronological progression of the changes remains unclear. ST elevations seem to resolve while T wave inversions appear to persist even for months/years [13, 14]. Commonly detected rhythm disturbances in SAH include sinus bradycardia and sinus tachycardia, wandering atrial pacemaker and atrial fibrillation and have been detected in two studies [19, 20]. Premature atrial, junctional and ventricular complexes, ventricular tachycardia and atrioventricular block have also been detected occasionally [21]. Holter monitoring of patients in recent times has led to greater detection and reporting rates of arrhythmias in SAH patients. In the largest study to date in which Holter technology was used, Di Pasquale et al. [10] first obtained a 12-lead ECG at the time of admission from a sample of 120 patients with SAH. Holter monitoring was started on the same day, and a total of 107 adequate Holter recordings were obtained. Cardiac arrhythmias were detected in
ST-T changes in SAH
50% 45% 40% 35% 30% 25% 20% 15% 10% 5% 0%
es av es es si on av al iti es W w rm pr
Series1
de
no
ig h
ab
Bi g
ST
Hypothalamic stimulation as well as autonomic dysregulations have been implicated as causative for the ECG changes in SAH without corroborative conclusive evidence.
Fig. 1 ST-T changes in subarachnoid haemorrhage
av
Pr
ol
on
ge
Possible Mechanisms of the ECG Changes in SAH
Tc
Neth Heart J (2011) 19:3134
33
96 (90%) of the 107 patients. Premature ventricular complexes, including multiform premature ventricular complexes, couplets or triplets, and R-on-T phenomenon, were detected in 49 patients (46%). Five of the patients with frequent premature ventricular complexes also had nonsustained ventricular tachycardia (defined as three or more consecutive premature ventricular complexes). Torsades de pointes occurred in four patients and progressed to ventricular fibrillation and asystole in one of the four. Holter monitoring was repeated in 48 h for all patients with malignant ventricular arrhythmias, but no further similar arrhythmias were recorded. Of the 107 patients, 39 (36%) had supraventricular arrhythmias, including premature supraventricular complexes, nonsustained supraventricular tachycardia, and atrial fibrillation. Thirty-two patients (30%) had sinus tachycardia (heart rate >120/min), 32 (30%) had sinus arrhythmia, 42 (39%) had sinus bradycardia (heart rate <50/min) and 23 (21%) had sinoatrial blocks. Ventricular premature complexes in 49, nonsustained ventricular tachycardia in five, supraventricular premature complexes in 29, paroxysmal supraventricular tachycardia or atrial fibrillation in nine, sinoatrial block and arrest in 29, second-degree atrioventricular block in one, atrioventricular dissociation in four and idioventricular rhythm in two. Life-threatening ventricular arrhythmias (torsades de pointes type ventricular tachycardia) occurred in four patients, degenerating into either ventricular flutter or fibrillation in two. ST-segment changes suggestive of acute transitory myocardial ischaemia were found in eight patients (1.5 mm or more of ST depression in seven patients and 1.5 mm or more of ST elevation in one patient). In their attempt at correlating arrhythmias with time elapsed since SAH, Di Pasquale et al. [10] found that both frequency and severity of arrhythmias were higher in the 62 subjects studied within 48 h of SAH. However, all patients with malignant ventricular arrhythmias had a much longer QTc interval (59052 ms) and serum levels of potassium less than 3.5 mmol/l. The study by Di Pasquale et al. found no correlation between clinical condition, site of aneurysm, extent of intracranial haemorrhage, age or preexisting heart disease and the frequency and severity of arrhythmias [8, 10].
arrhythmias warrants a close monitoring of the ECG in these patients. A recent study has found that arrhythmias are associated with an increased risk of cardiovascular comorbidity, prolonged hospital stay and poor outcome or death after SAH, after adjusting for other predictors of poor outcome [22]. Although no correlation was found between the frequency and severity of cardiac arrhythmias and the neurological condition, the site and extent of intracranial blood on computed tomography scan, or the location of ruptured malformation, the extremely high incidence of cardiac arrhythmias, sometimes serious, in the acute period after subarachnoid haemorrhage and the absence of clinical and radiological predictors make systematic continuous ECG monitoring compulsory to improve the overall results of subarachnoid haemorrhage, irrespective of early or delayed surgical treatment. If kept in mind, the ECG changes as enumerated might be beneficial when an SAH patient is evaluated for an abnormal ECG.
References
1. Goldstein DS. The electrocardiogram in stroke: relationship to pathophysiological type and comparison with prior tracings. Stroke. 1979;10(3):2539. 2. Weinberg SJ, Fuster JM. Electrocardiographic changes produced by localized hypothalamic stimulations. Ann Intern Med. 1960;53:33241. 3. Zaroff JG, Rordorf GA, Newell BA, Ogilvy CS, Levinson JR. Cardiac outcome in patients with subarachnoid hemorrhage and electrocardiographic abnormalities. Neurosurgery. 1999;44:34 40. 4. Beard EF, Robertson JW, Robertson RCL. Spontaneous subarachnoid hemorrhage simulating acute myocardial infarction. Am Heart J. 1959;58:7559. 5. Cropp GJ, Manning GW. Electrocardiographic changes simulating myocardial ischemia and infarction associated with spontaneous intracranial hemorrhage. Circulation. 1960;22:2538. 6. Carruth JE, Silverman ME. Torsade de pointe atypical ventricular tachycardia complicating subarachnoid hemorrhage. Chest. 1980;78:8868. 7. Cruickshank JM, Neil-Dwyer G, Brice J. Electrocardiographic changes and their prognostic significance in subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry. 1974;37:7559. 8. Sommargren CE. Electrocardiographic abnormalities in patients with subarachnoid hemorrhage. Am J Critical Care. 2002;11:48 56. 9. Brouwers PJ, Wijdicks EF, Hasan D, et al. Serial electrocardiographic recording in aneurysmal subarachnoid hemorrhage. Stroke. 1989;20:11627. 10. Di Pasquale G, Pinelli G, Andreoli A, Manini G, Grazi P, Tognetti F. Holter detection of cardiac arrhythmias in intracranial subarachnoid hemorrhage. Am J Cardiol. 1987;59:596600. 11. Kreus KE, Kamila SJ, Takala JR. Electrocardiographic changes in cerebrovascular accidents. Acta Med Scand. 1969;185:327 34. 12. Solenski NJ, Haley Jr EC, Kassell NF, et al. Medical complications of aneurysmal subarachnoid hemorrhage: a
Summary The morphological ECG changes most frequently encountered in a subject with SAH are U waves, T-wave abnormalities, R-wave abnormalities and non-specific ST-T changes. The predominant rhythm abnormalities seem to be relatively benign sinus tachycardias and bradycardias. However, the possibility of development of supraventricular arrhythmias, sinoatrial blocks and arrests, and life-threatening ventricular
34 report of the multicenter, cooperative aneurysm study. Crit Care Med. 1995;23:100717. Kuroiwa T, Morita H, Tanabe H, Ohta T. Significance of ST segment elevation in electrocardiograms in patients with ruptured cerebral aneurysms. Acta Neurochir (Wien). 1995;133:1416. Shuster S. The electrocardiogram in subarachnoid hemorrhage. Br Heart J. 1960;22:31620. Arruda WO, de Lacerda Jr FS. Electrocardiographic findings in acute cerebrovascular hemorrhage: a prospective study of 70 patients. Arq Neuropsiquiatr. 1992;50:26974. Rudehill A, Olsson GL, Sundqvist K, Gordon E. ECG abnormalities in patients with subarachnoid haemorrhage and intracranial tumours. J Neurol Neurosurg Psychiatry. 1987;50:137581. de Sweit J. Changes simulating hypothermia in the electrocardiogram in subarachnoid hemorrhage. J Electrocardiol. 1972;5:935.
Neth Heart J (2011) 19:3134 18. Syverud G. Electrocardiographic changes and intracranial pathology. AANA J. 1991;59:22932. 19. Eisalo A, Persalo J, Halonen PI. Electrocardiographic abnormalities and some laboratory findings in patients with subarachnoid haemorrhage. Br Heart J. 1972;34:21726. 20. Cruickshank JM, Neil-Dwyer G, Stott AW. Possible role of catecholamines, corticosteroids, and potassium in production of electrocardiographic abnormalities associated with subarachnoid haemorrhage. Br Heart J. 1974;36:697706. 21. Estaol BV, Badui ED, Cesarman E, et al. Cardiac arrhythmias associated with subarachnoid hemorrhage: prospective study. Neurosurgery. 1979;5:67580. 22. Frontera JA, Parra A, Shimbo D, et al. Cardiac arrhythmias after subarachnoid hemorrhage: risk factors and impact on outcome. Cerebrovasc Dis. 2008;26:718.
13.
14. 15.
16.
17.
You might also like
- Digoxin: Mechanism of ActionDocument4 pagesDigoxin: Mechanism of ActionahmedNo ratings yet
- Assessment of Palpitation Complaints Benign Paroxysmal Positional VertigoDocument6 pagesAssessment of Palpitation Complaints Benign Paroxysmal Positional VertigoHappy PramandaNo ratings yet
- T Wave Alternans For Ventricular Arrhythmia Risk StratificationDocument5 pagesT Wave Alternans For Ventricular Arrhythmia Risk StratificationSalim VelaniNo ratings yet
- Effect of Nocturnal Oxygen Therapy On Electrocardiographic Changes Among Patients With Congestive Heart FailureDocument3 pagesEffect of Nocturnal Oxygen Therapy On Electrocardiographic Changes Among Patients With Congestive Heart FailureNurAfifahNo ratings yet
- Lapkas Pediatrik NLDocument31 pagesLapkas Pediatrik NLHannaTashiaClaudiaNo ratings yet
- AV Bloc Induces TDPDocument13 pagesAV Bloc Induces TDPMirza AlfiansyahNo ratings yet
- In-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisDocument15 pagesIn-Hospital Arrhythmia Development and Outcomes in Pediatric Patients With Acute MyocarditisAnonymous OU6w8lX9No ratings yet
- Journal of Nursing: Basic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest RadiographyDocument8 pagesJournal of Nursing: Basic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest RadiographyNiala AlmarioNo ratings yet
- SVT Mayo 2008Document12 pagesSVT Mayo 2008muhanasNo ratings yet
- Therapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticDocument8 pagesTherapeutic Implications: Short QT Syndrome: Clinical Findings and DiagnosticNITACORDEIRONo ratings yet
- ABC of Clinical Electrocardiography Myocardial IschaemiaDocument6 pagesABC of Clinical Electrocardiography Myocardial IschaemiaShri Mahalaxmi HarishNo ratings yet
- Neonatal and Pediatric Guidelines Arrhythmia ManagementDocument16 pagesNeonatal and Pediatric Guidelines Arrhythmia ManagementAkhmad HidayatNo ratings yet
- Hollamby Mitchell s5001226 Case 1 DtgaDocument13 pagesHollamby Mitchell s5001226 Case 1 Dtgaapi-299009880No ratings yet
- Cardiac ArrhythmiasDocument5 pagesCardiac Arrhythmiastere glezNo ratings yet
- VT SVT AvrDocument3 pagesVT SVT AvragneselimNo ratings yet
- Electrocardiographic and Echocardiographic Changes in Patients With Thyreotoxic CardiopathyDocument4 pagesElectrocardiographic and Echocardiographic Changes in Patients With Thyreotoxic CardiopathySilvia MudrencoNo ratings yet
- Establishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratoryDocument15 pagesEstablishing The Mechanism of Supraventricular Tachycardia in The Electrophysiology LaboratorySamuelNo ratings yet
- Electrocardiographic Changes and Intracranial Pathology: Geraldine Syverud, Crna, BSNDocument4 pagesElectrocardiographic Changes and Intracranial Pathology: Geraldine Syverud, Crna, BSNchuck55No ratings yet
- The Tilt Table Test Is Useful For The Diagnosis of Vasovagal Syncope and Should Not Be AbolishedDocument5 pagesThe Tilt Table Test Is Useful For The Diagnosis of Vasovagal Syncope and Should Not Be AbolishedririsNo ratings yet
- 1 s2.0 S0870255121005096 MainDocument3 pages1 s2.0 S0870255121005096 MainangelemanuelarmasNo ratings yet
- Ekg STDocument23 pagesEkg STisaNo ratings yet
- Applications and New InsightsDocument7 pagesApplications and New InsightsPaola CardenasNo ratings yet
- Articles Publishd in JournalsDocument9 pagesArticles Publishd in JournalsHeartHealthNo ratings yet
- Heart 2002 Menon 531 7Document8 pagesHeart 2002 Menon 531 7TriponiaNo ratings yet
- Ijmps - The Value of Holter Monitoring PDFDocument6 pagesIjmps - The Value of Holter Monitoring PDFAnonymous Y0wU6InINo ratings yet
- Memory T-Waves, A Rare Cause of T-Wave Inversion in The Emergency Department - PMCDocument7 pagesMemory T-Waves, A Rare Cause of T-Wave Inversion in The Emergency Department - PMCfiat.2dindaNo ratings yet
- Ecg ManfestationsDocument19 pagesEcg Manfestationsnaxo128No ratings yet
- Practice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaDocument28 pagesPractice Essentials: Essential Updates: Distinguishing Between Left-And Right-Sided Atrial TachycardiaRully SyahrizalNo ratings yet
- Electrocardiograph Changes in Acute Ischemic Cerebral StrokeDocument6 pagesElectrocardiograph Changes in Acute Ischemic Cerebral StrokeFebniNo ratings yet
- Clinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761Document10 pagesClinical Features and Outcomes of Takotsubo Stress Cardiomyopathy NEJMoa1406761William LeeNo ratings yet
- Current Concepts in QT ProlongationDocument9 pagesCurrent Concepts in QT ProlongationSuresh KumarNo ratings yet
- Prevalence and Clinical Correlates of QT Prolongation in Patients With Hypertrophic CardiomyopathyDocument7 pagesPrevalence and Clinical Correlates of QT Prolongation in Patients With Hypertrophic CardiomyopathyNITACORDEIRONo ratings yet
- Lapkas VT RevisiDocument13 pagesLapkas VT RevisiRannyNo ratings yet
- Techniques of TIPS in The Treatment of Liver Cirrhosis Combined With Incompletely Occlusive Main Portal Vein ThrombosisDocument9 pagesTechniques of TIPS in The Treatment of Liver Cirrhosis Combined With Incompletely Occlusive Main Portal Vein ThrombosisLeon L GayaNo ratings yet
- Wilbert S. Aronow. Hypertension and Left Ventricular HypertrophyDocument1 pageWilbert S. Aronow. Hypertension and Left Ventricular Hypertrophykorejat unpadNo ratings yet
- Tachyarrhythmias and Defibrillation: Ricardo A. Samson, MD, Dianne L. Atkins, MDDocument21 pagesTachyarrhythmias and Defibrillation: Ricardo A. Samson, MD, Dianne L. Atkins, MDEmilio Emmanué Escobar CruzNo ratings yet
- 3.arrhythmias After CongenitaDocument6 pages3.arrhythmias After Congenitaganda gandaNo ratings yet
- Cerebrovascular Disease From JeffryDocument8 pagesCerebrovascular Disease From JeffryIdrianaNo ratings yet
- ContentServer AspDocument9 pagesContentServer Aspganda gandaNo ratings yet
- Transfusion Associated Circulatory Overload Taco Emma GoodhallDocument5 pagesTransfusion Associated Circulatory Overload Taco Emma GoodhallAthirah M.NoerNo ratings yet
- Basic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest RadiographyDocument7 pagesBasic Cardiac Assessments: Physical Examination, Electrocardiography, and Chest Radiographyrowd1yNo ratings yet
- Tatalaksana Hyponatremia Pada Diuresis Post ObstruktifDocument4 pagesTatalaksana Hyponatremia Pada Diuresis Post ObstruktifGilberto ChafrinaNo ratings yet
- Jardine 2017Document27 pagesJardine 2017Ismi Prasastawati KurniawanNo ratings yet
- Wolsey SlidesCarnivalDocument25 pagesWolsey SlidesCarnivalRaudha JanahNo ratings yet
- Stress-Related Cardiomyopathy or Tako-Tsubo Syndrome: Current ConceptsDocument6 pagesStress-Related Cardiomyopathy or Tako-Tsubo Syndrome: Current ConceptslivroinglesNo ratings yet
- Diagnosis and Management of Splanchnic Ischemia: Ioannis E Koutroubakis, MD, PHD, Assistant Professor of MedicineDocument12 pagesDiagnosis and Management of Splanchnic Ischemia: Ioannis E Koutroubakis, MD, PHD, Assistant Professor of MedicineIgorCotagaNo ratings yet
- Detection AFDocument5 pagesDetection AFDhinny Heksa MarchiaNo ratings yet
- Drug-Induced QT Interval ProlongationDocument13 pagesDrug-Induced QT Interval ProlongationgeoaislaNo ratings yet
- How To Diagnose The Cause of Sudden Cardiac ArrestDocument7 pagesHow To Diagnose The Cause of Sudden Cardiac ArrestTaufik Muhammad JrNo ratings yet
- Paroxysmal Supraventricular TachycardiaDocument3 pagesParoxysmal Supraventricular TachycardiaIqbal Juher MNo ratings yet
- ECG HRV Assignment 19334107Document18 pagesECG HRV Assignment 19334107katehughes332No ratings yet
- Assessment of Pulse Transit Time To Indicate Cardiovascular Changes During Obstetric Spinal AnaesthesiaDocument6 pagesAssessment of Pulse Transit Time To Indicate Cardiovascular Changes During Obstetric Spinal AnaesthesiaprabuNo ratings yet
- Rashid 2021Document10 pagesRashid 2021Carmen Cuadros BeigesNo ratings yet
- Stroke 1982 Myers 838 42Document6 pagesStroke 1982 Myers 838 42Widyawan SyahputraNo ratings yet
- Estenosis Aortica 2016 Aafp 2016Document8 pagesEstenosis Aortica 2016 Aafp 2016Antonio MoncadaNo ratings yet
- ECG Frequency Changes inDocument13 pagesECG Frequency Changes inArief KamilNo ratings yet
- Additional Idea For Litrature (Repaired)Document17 pagesAdditional Idea For Litrature (Repaired)Abrsham AyeleNo ratings yet
- Aortic StenosisDocument11 pagesAortic StenosisIra Anuddin100% (1)
- Electrocardiograma en TóxicologiaDocument19 pagesElectrocardiograma en TóxicologiaLaura GNo ratings yet
- The Perindopril in Elderly PeopleDocument8 pagesThe Perindopril in Elderly PeopleluchititaNo ratings yet
- Coronary Vasomotion AbnormalitiesFrom EverandCoronary Vasomotion AbnormalitiesHiroaki ShimokawaNo ratings yet
- Cardiac Arrest After Cardiac Surgery: An Evidence-Based Resuscitation ProtocolDocument12 pagesCardiac Arrest After Cardiac Surgery: An Evidence-Based Resuscitation ProtocoljoseNo ratings yet
- Hemodynamics E-ConDocument1 pageHemodynamics E-ConpjebinkNo ratings yet
- SuciDocument12 pagesSucisuciNo ratings yet
- Timing of Revascularization in Patients With Transient ST Segment Elevation Myocardial Infarction A Randomized Clinical TrialDocument9 pagesTiming of Revascularization in Patients With Transient ST Segment Elevation Myocardial Infarction A Randomized Clinical TrialWelly WijayaNo ratings yet
- NCM118 TransesDocument11 pagesNCM118 TransesAlejandro Saclolo, IIINo ratings yet
- CT and MR in Cardiology 1St Edition Suhny Abbara Full Chapter PDFDocument69 pagesCT and MR in Cardiology 1St Edition Suhny Abbara Full Chapter PDFflayizouina100% (6)
- Assessment of Heart & Neck VesselsDocument4 pagesAssessment of Heart & Neck VesselsCardio GodNo ratings yet
- Acls Pretest Answer Key: Rhythm Identification (Part I)Document3 pagesAcls Pretest Answer Key: Rhythm Identification (Part I)aditNo ratings yet
- Atrial Fibrillation TDDocument6 pagesAtrial Fibrillation TDapi-594366475No ratings yet
- EKG Card 2Document2 pagesEKG Card 2mulyadiNo ratings yet
- CH17 Cardiac Surgery in The Adult 5th Edition 2018Document26 pagesCH17 Cardiac Surgery in The Adult 5th Edition 2018ChengShiun ShiueNo ratings yet
- PostsDocument6 pagesPostsQusaiBadrNo ratings yet
- Non St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyDocument4 pagesNon St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyKEn PilapilNo ratings yet
- Cardiomyopathies: Cardiomyopathy Is A Heart Muscle Disease Associated With CardiacDocument10 pagesCardiomyopathies: Cardiomyopathy Is A Heart Muscle Disease Associated With Cardiacmerin sunilNo ratings yet
- Government Service Insurance System, Petitioner, vs. ASTRID V. CORRALES, RespondentDocument20 pagesGovernment Service Insurance System, Petitioner, vs. ASTRID V. CORRALES, RespondentMaryland AlajasNo ratings yet
- CHAPTER 11: The History and Physical Examination: An Evidence Based ApproachDocument5 pagesCHAPTER 11: The History and Physical Examination: An Evidence Based ApproachReda SoNo ratings yet
- Del Nido Cardioplegia - What Is The Current Evidence?: Review PaperDocument5 pagesDel Nido Cardioplegia - What Is The Current Evidence?: Review PapermahNo ratings yet
- Electrocar Diogram: College of Nursing Madurai Medical College, Madurai-20 Procedure Demonstration OnDocument19 pagesElectrocar Diogram: College of Nursing Madurai Medical College, Madurai-20 Procedure Demonstration OnValarmathi100% (1)
- Catheter Reprocessing SystemDocument16 pagesCatheter Reprocessing Systemsutan IskandarsyahNo ratings yet
- Dissertationen Online Uni Bonn MedizinDocument8 pagesDissertationen Online Uni Bonn MedizinHelpWithWritingAPaperUK100% (1)
- Bio Essay CardioDocument3 pagesBio Essay CardiopadmaszNo ratings yet
- ECG Definition: - PurposeDocument2 pagesECG Definition: - PurposeJustine Karl Pablico100% (1)
- Symptoms of CvsDocument25 pagesSymptoms of CvsstudymedicNo ratings yet
- Board 14 Desember 2014 Kumpulan FinalDocument73 pagesBoard 14 Desember 2014 Kumpulan FinalAnonymous XHguqDfWR0% (1)
- Pediatric Specialists - Managing The Medical MazeDocument4 pagesPediatric Specialists - Managing The Medical MazePathways AwarenessNo ratings yet
- Risk Factor For Atrial FibrilationDocument19 pagesRisk Factor For Atrial FibrilationDanny Soegianto IINo ratings yet
- CT and MR in Cardiology 1St Edition Suhny Abbara Full ChapterDocument67 pagesCT and MR in Cardiology 1St Edition Suhny Abbara Full Chapterelizabeth.dew603100% (9)
- Programbook IsicamDocument36 pagesProgrambook Isicamadi bestaraNo ratings yet
- Disusun Oleh NS Irvantri Aji Jaya - M.Kep. SP - Kep.M.BDocument26 pagesDisusun Oleh NS Irvantri Aji Jaya - M.Kep. SP - Kep.M.Bsangid yahyaNo ratings yet