Professional Documents
Culture Documents
Protective Effectiveness of Previous SARS-CoV-2 Infection and Hybrid Immunity
Protective Effectiveness of Previous SARS-CoV-2 Infection and Hybrid Immunity
Uploaded by
CTV CalgaryOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Protective Effectiveness of Previous SARS-CoV-2 Infection and Hybrid Immunity
Protective Effectiveness of Previous SARS-CoV-2 Infection and Hybrid Immunity
Uploaded by
CTV CalgaryCopyright:
Available Formats
Articles
Protective effectiveness of previous SARS-CoV-2 infection
and hybrid immunity against the omicron variant and severe
disease: a systematic review and meta-regression
Niklas Bobrovitz, Harriet Ware, Xiaomeng Ma, Zihan Li, Reza Hosseini, Christian Cao, Anabel Selemon, Mairead Whelan, Zahra Premji,
Hanane Issa, Brianna Cheng, Laith J Abu Raddad, David L Buckeridge, Maria D Van Kerkhove, Vanessa Piechotta, Melissa M Higdon,
Annelies Wilder-Smith, Isabel Bergeri, Daniel R Feikin, Rahul K Arora*, Minal K Patel*, Lorenzo Subissi*
Summary
Background The global surge in the omicron (B.1.1.529) variant has resulted in many individuals with hybrid Lancet Infect Dis 2023
immunity (immunity developed through a combination of SARS-CoV-2 infection and vaccination). We aimed to Published Online
systematically review the magnitude and duration of the protective effectiveness of previous SARS-CoV-2 infection January 18, 2023
https://doi.org/10.1016/
and hybrid immunity against infection and severe disease caused by the omicron variant.
S1473-3099(22)00801-5
See Online/Comment
Methods For this systematic review and meta-regression, we searched for cohort, cross-sectional, and case–control https://doi.org/10.1016/
studies in MEDLINE, Embase, Web of Science, ClinicalTrials.gov, the Cochrane Central Register of Controlled Trials, S1473-3099(22)00880-5
the WHO COVID-19 database, and Europe PubMed Central from Jan 1, 2020, to June 1, 2022, using keywords related *Contributed equally
to SARS-CoV-2, reinfection, protective effectiveness, previous infection, presence of antibodies, and hybrid immunity. Temerty Faculty of Medicine
The main outcomes were the protective effectiveness against reinfection and against hospital admission or severe (N Bobrovitz DPhil, C Cao,
disease of hybrid immunity, hybrid immunity relative to previous infection alone, hybrid immunity relative to B Cheng MSc) and Institute of
Health Policy Management and
previous vaccination alone, and hybrid immunity relative to hybrid immunity with fewer vaccine doses. Risk of bias Evaluation (X Ma MSc),
was assessed with the Risk of Bias In Non-Randomized Studies of Interventions Tool. We used log-odds random- University of Toronto, Toronto,
effects meta-regression to estimate the magnitude of protection at 1-month intervals. This study was registered with ON, Canada; Department of
PROSPERO (CRD42022318605). Critical Care Medicine
(N Bobrovitz), Centre for Health
Informatics, Cumming School
Findings 11 studies reporting the protective effectiveness of previous SARS-CoV-2 infection and 15 studies reporting of Medicine (N Bobrovitz,
the protective effectiveness of hybrid immunity were included. For previous infection, there were 97 estimates H Ware MSc, Z Li BASc,
(27 with a moderate risk of bias and 70 with a serious risk of bias). The effectiveness of previous infection against R Hosseini MD, C Cao,
A Selemon, M Whelan MSc,
hospital admission or severe disease was 74·6% (95% CI 63·1–83·5) at 12 months. The effectiveness of previous R K Arora BHSc), University of
infection against reinfection waned to 24·7% (95% CI 16·4–35·5) at 12 months. For hybrid immunity, there were Calgary, Calgary, AB, Canada;
153 estimates (78 with a moderate risk of bias and 75 with a serious risk of bias). The effectiveness of hybrid immunity Department of Bioengineering,
against hospital admission or severe disease was 97·4% (95% CI 91·4–99·2) at 12 months with primary series University of California,
Berkeley, CA, USA, (Z Li); School
vaccination and 95·3% (81·9–98·9) at 6 months with the first booster vaccination after the most recent infection or of Population and Public
vaccination. Against reinfection, the effectiveness of hybrid immunity following primary series vaccination waned to Health, University of British
41·8% (95% CI 31·5–52·8) at 12 months, while the effectiveness of hybrid immunity following first booster Columbia, Vancouver, BC,
vaccination waned to 46·5% (36·0–57·3) at 6 months. Canada (R Hosseini); Libraries,
University of Victoria, Victoria,
BC, Canada (Z Premji PhD);
Interpretation All estimates of protection waned within months against reinfection but remained high and sustained Institute of Health Informatics,
for hospital admission or severe disease. Individuals with hybrid immunity had the highest magnitude and durability University College London,
London, UK (H Issa MSc);
of protection, and as a result might be able to extend the period before booster vaccinations are needed compared to
Infectious Disease
individuals who have never been infected. Epidemiology Group, Weill
Cornell Medicine–Qatar, Cornell
Funding WHO COVID-19 Solidarity Response Fund and the Coalition for Epidemic Preparedness Innovations. University, Doha, Qatar
(Prof L J Abu Raddad PhD);
Department of Epidemiology
Copyright © 2023 World Health Organization; licensee Elsevier. This is an Open Access article published under the and Biostatistics, School of
CC BY 3.0 IGO license which permits unrestricted use, distribution, and reproduction in any medium, provided the Population and Global Health,
original work is properly cited. In any use of this article, there should be no suggestion that WHO endorses any McGill University, Montreal,
QC, Canada
specific organisation, products or services. The use of the WHO logo is not permitted. This notice should be preserved
(Prof D L Buckeridge PhD);
along with the article’s original URL. Health Emergencies
Programme, World Health
Introduction However, estimating the magnitude and durability of this Organization, Geneva,
Switzerland
Restricting the spread of SARS-CoV-2 infection and protection in the population has become a challenge
(M D Van Kerkhove PhD,
preventing severe COVID-19 remains a priority at the because of the surge in the omicron (B.1.1.529) variant, I Bergeri PharmD, L Subissi PhD);
global scale. Immunological protection from SARS-CoV-2 which has resulted in many individuals with hybrid Department of Infectious
can be induced from previous infection or vaccination.1,2 immunity (immunity developed through a combination Disease Epidemiology,
www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5 1
Articles
Robert Koch Institute, Berlin,
Germany (V Piechotta PhD); Research in context
International Vaccine Access
Center, Department of Evidence before this study protection in projections to 12 months after primary series
International Health, John The global emergence and rapid spread of the omicron hybrid immunity and 6 months after booster vaccination
Hopkins Bloomberg School of (B.1.1.529) variant of SARS-CoV-2 and its subvariants, hybrid immunity.
Public Health, Johns Hopkins
characterised by its ability to escape immunity, has required
University, Baltimore, MD, USA Implications of all the available evidence
(M M Higdon MPH); scientists and policy makers to reassess population protection
These results provide information that can be used to tailor
Department of Immunizations, against SARS-CoV-2 infection and severe disease due to the
Vaccines and Biologicals, World guidance on the number and timing of SARS-CoV-2
omicron variant. We searched MEDLINE (Ovid), Embase (Ovid),
Health Organization, Geneva, vaccinations. At the public health level, these findings can be
Web of Science (Core Collection), ClinicalTrials.gov, the
Switzerland combined with data on local infection prevalence, vaccination
(Prof A Wilder-Smith MD, Cochrane Central Register of Controlled Trials (Ovid), the WHO
rates, and their timing. In settings with high seroprevalence,
D R Feikin MD, M K Patel MD); COVID-19 database, and Europe PubMed Central (limited to
Heidelberg Institute of Global scarce resources, and competing health priorities, evidence
preprints) from Jan 1, 2020, to June 1, 2022, with keywords
Health, University of suggests that it is reasonable to focus on achieving high
related to SARS-CoV-2, reinfection, protective effectiveness,
Heidelberg, Germany coverage rates with primary series vaccination among
(Prof A Wilder-Smith); Institute previous infection, presence of antibodies, and hybrid
individuals who are at higher risk of poor outcomes, as this will
of Biomedical Engineering, immunity. We found a few systematic reviews that
University of Oxford, Oxford, provide a high level of protection against severe disease for at
incorporated data on the omicron variant, but none that
UK (R K Arora) least 1 year among those with previous infection. Furthermore,
examined protection against the omicron variant conferred by
Correspondence to: given the waning protection for both infection-induced and
hybrid immunity (ie, immunity gained from the combination
Dr Niklas Bobrovitz, Temerty vaccine-induced immunity against SARS-CoV-2 infection or
Faculty of Medicine, University of of vaccination and previous infection), which is now
reinfection, wider vaccination among populations (eg, mass
Toronto, Toronto, ON M5S 1A8, widespread globally. One review reported the duration and
Canada vaccination) could be timed for rollout before periods of
magnitude of protection from previous infection over time;
niklas.bobrovitz@mail. expected increased incidence, such as the winter season. At the
however, to the best of our knowledge, no study has
utoronto.ca individual level, these results can be combined with knowledge
systematically compared the magnitude and duration of
of a person’s infection and vaccination history. A 6-month
protection from vaccination, previous infection, and hybrid
delay in a booster dose might be justified after the last infection
immunity. A large study in Qatar reported that protection from
or vaccination for individuals with a known history of previous
infection or hybrid immunity against the omicron variant
infection and full primary series vaccination. Further follow-up
wanes to low levels at 15 months but is relatively stable against
data on the protective effectiveness of hybrid immunity against
severe disease.
hospital admission or severe disease for all vaccines are needed
Added value of this study to clarify how much waning of protection might occur with a
Previous SARS-CoV-2 infection and hybrid immunity both longer duration since the last infection or vaccination.
provided greater and more sustained protection against the Producing estimates of protection for vaccines targeting new
omicron variant than vaccination alone. Individuals with hybrid variants will be crucial for COVID-19 vaccination policy and
immunity had the highest magnitude and durability of decision-making bodies. Policy makers considering the use and
protection against all outcomes; protection against severe timing of vaccinations could include the local extent of past
disease remained higher than 95% until the end of available infection, the protection conferred by previous infection or
follow-up at 11 months after hybrid immunity with primary hybrid immunity, and the duration of this protection as key
series vaccination and 4 months after hybrid immunity with considerations to inform their decision making.
booster vaccination, and was sustained at these high levels of
of SARS-CoV-2 infection and vaccination), varying rates vaccinated (ie, the effectiveness of hybrid immunity). A
and timings of past infection and vaccination, multiple systematic review has estimated the durability of
types of vaccination and numbers of doses, and variants of protection conferred by previous infection.7 However,
concern that can escape pre-existing immunity.3,4 no systematic review has, to the best of our knowledge,
Systematic reviews of SARS-CoV-2 vaccine effec estimated the durability of protection conferred by
tiveness studies have provided clarity on the durability hybrid immunity or compared the durability of the
of protection for different variants of concern.5,6 These different types of protection.
studies have compared protection among vaccinated We aimed to systematically review the evidence for the
individuals to that in unvaccinated individuals and magnitude and duration of the effectiveness of previous
compared protection between different numbers of infection and hybrid immunity against multiple clinical
doses. However, there are gaps in the literature on the outcomes of SARS-CoV-2 infection caused by the
magnitude and duration of protection conferred by omicron variant. We also aimed to examine the
previous infection, both among individuals who have comparative protection of hybrid immunity relative to
not been vaccinated (ie, the effectiveness of previous previous infection only, vaccination only, and hybrid
infection alone) and among individuals who have been immunity with fewer vaccine doses.
2 www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5
Articles
Methods systematic review6 used similar inclusion and exclusion
Search strategy and selection criteria criteria to our analysis. We applied our meta-regression
This systematic review and meta-regression was registered model to the dataset to project the trends of waning
with PROSPERO (CRD42022318605), conducted in vaccine effectiveness, in parallel with trends for previous
alignment with the Cochrane Handbook for Systematic infection and hybrid immunity generated from data
Reviews of Interventions,8 and reported according to the procured in our systematic review (appendix pp 12–13).
Preferred Reporting Items for Systematic Reviews and
Meta-Analyses (PRISMA) guidelines (appendix pp 2–4).9 Data analysis See Online for appendix
We searched MEDLINE (Ovid), Embase (Ovid), Web of Summary data were extracted from published reports by
Science (Core Collection), ClinicalTrials.gov, the one reviewer and verified by a second reviewer (NB, XM,
Cochrane Central Register of Controlled Trials (Ovid), ZL, RH, CC, and AS). We extracted data for each outcome
WHO COVID-19 database, and Europe PubMed Central (infection [asymptomatic or symptomatic disease],
(limited to preprints) from Jan 1, 2020, to June 1, 2022 hospital admission, or severe disease [a combination of
(appendix pp 5–9). The search strategy comprised the WHO definitions of severe, critical, or fatal
three keyword concepts: SARS-CoV-2; reinfection and COVID-19]),11 stratifying by age, sex, vaccine type, the
protective effectiveness; and previous infection, presence variant of concern causing the index infection, and the
of antibodies, and hybrid immunity. We also sought severity of the index infection (appendix pp 10–13). Few
article recommendations from authors of previous studies reported ethnicity data, so we were unable to
vaccine effectiveness studies and WHO Solidarity II analyse the impact of ethnicity on our study outcomes.
network investigators. Risk of bias was assessed with the Risk of Bias In Non-
Screening was done in Covidence software with titles Randomized Studies of Interventions (ROBINS-I) Tool.12
and abstracts and full-text manuscripts. Two reviewers Two reviewers (NB and VP) independently completed the
independently screened studies (NB, XM, ZL, RH, CC, assessments for each reported outcome. Conflicts were
AS, HI, BC). Conflicts were resolved by a third reviewer resolved by discussion and consensus among the two
(NB, XM). authors.
Detailed inclusion and exclusion criteria are reported in Five effect measures of protection were calculated on
the appendix (pp 10–12). We included studies examining the basis of different comparisons of immune status: the
protection against reinfection with the omicron variant, protective effectiveness of previous infection (defined as
in which the exposure group was people with previous previous infection vs immune naive); the protective
infection with any SARS-CoV-2 variant or hybrid effectiveness of hybrid immunity (defined as hybrid
immunity and the control group was immune-naive immunity vs immune naive); the comparative protective
individuals, previously infected individuals, or previously effectiveness of hybrid immunity relative to previous
vaccinated individuals. Infection due to the omicron infection alone (defined as hybrid immunity vs infection);
variant was determined by genomic sequencing or the comparative protective effectiveness of hybrid
inferred on the basis of time periods when the variants immunity relative to previous vaccination alone (defined
were predominant according to the GISAID (Global as hybrid immunity vs previous vaccination); and the
Initiative on Sharing Avian Influenza Data) EpiFlu comparative protective effectiveness of hybrid immunity For more on the GISAID EpiFlu
database. Studies were excluded if they did not report relative to hybrid immunity with fewer vaccine doses database see https://www.
re3data.org/repository/
evidence of previously confirmed SARS-CoV-2 cases or (defined as hybrid immunity with more vaccine doses vs
r3d100010126
did not report the period of time between the index hybrid immunity with fewer vaccine doses). The
infection and reinfection. immunity comparisons, effect measures, and their
epidemiological importance are described in the appendix
Outcome definition and comparison groups (p 13). The primary outcomes were the abovementioned
SARS-CoV-2 reinfection was defined as a possible, five measures of protection against hospital admission
probable, or confirmed reinfection case according to due to COVID-19 or severe disease at discrete timepoints.
adapted WHO definitions (appendix p 10).10 Partial The secondary outcomes were the same five measures of
primary series and full primary series vaccination were protection against infection with the omicron variant at
defined according to the original clinical trials of the discrete timepoints. For previous infection, we used
respective COVID-19 vaccines. First booster vaccination estimates starting from 2 months after the primary
included individuals at least 7 days from receipt of the infection, reflecting the length of time required for a
first booster dose. possible reinfection. For hybrid immunity, we used
Estimates of vaccine effectiveness (ie, vaccinated vs estimates starting from 2 months after the primary
unvaccinated) against the omicron variant were obtained infection or at least 7 days after the most recent vaccination
from the dataset of a systematic review and meta- (the cutoff threshold varied by vaccine according to the
regression involving 19 studies of both primary series original clinical trials; appendix pp 10–11).
and booster vaccination (of which 18 were primary series Using the log-odds meta-regression model, we
studies and 12 were first booster studies).6 This previous generated estimates of effectiveness in successive months
www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5 3
Articles
as well as percentage-point changes in effectiveness from
7133 articles from electronic databases
3 to 6 months and from 3 to 12 months, with 95% bootstrap
1398 MEDLINE CIs for the changes calculated using 1000 bootstrap
1642 Embase samples. For the protective effectiveness of hybrid
1729 Web of Science
12 ClinicalTrials.gov immunity we predicted estimates 1 month and 2 months
56 Cochrane Central Register of Controlled Trials beyond final follow-up times, yielding estimates of
1252 WHO COVID-19 NVOC database
1044 Europe PubMed Central (preprints) protection at 12 months for hybrid immunity with primary
series vaccination and 6 months for hybrid immunity with
booster vaccination. For a given outcome measure, if
130 articles from additional searching there were insufficient data for meta-regression over time
72 expert recommendations
58 updated versions of preprint then estimates were pooled via meta-analysis (same log-
articles odds model with no time covariate).13 These estimates
represented an average of the timepoints reported in
7263 articles captured
different studies. Modelling details are reported in the
appendix (p 12).
Two sensitivity analyses were done: one analysis focused
2995 duplicate articles removed on severe disease and excluded all-cause hospital
admission and the other excluded estimates with a serious
4268 titles and abstracts screened
risk of bias. There were insufficient data to report results
stratified by age, sex, severity of the index infection, and
the omicron subvariant causing reinfection.
3373 articles that did not report on the protection conferred by Data were analysed with R statistical software
previous SARS-CoV-2 infection or hybrid immunity
excluded (version 4.1.2).14
Role of the funding source
895 full-text articles screened*
The funders had no role in study design, data collection,
data analysis, data interpretation, or the writing of the
571 full-text articles excluded report.
194 wrong study design (eg, protocol, case report, case
series, systematic review)
171 no relevant comparison group Results
14 abstract only (no full text) 4268 article titles and abstracts were screened and
10 reinfection defined as <60 days between infections 895 underwent full-text review (figure 1). 16 unique
9 did not report on SARS-CoV-2
8 non-English language articles reporting data for 26 studies were included in
6 did not report time period between last immunological the analysis.15–30 Seven articles reported data for two or
challenge and reinfection
6 ineligible confirmatory test for reinfection more studies (at least one previous infection study and
152 duplicate articles at least one hybrid immunity study), defined by multiple
1 retracted article
sets of participant inclusion and exclusion criteria or
popu lations that resulted in unique non-pooled
estimates of protection for each population. 11 studies
146 full-text articles on previous 178 full-text articles on hybrid immunity reported on previous infection and 15 reported on
infection screened for inclusion screened for inclusion hybrid immunity; seven reported on both. A summary
of the characteristics of included studies is shown in
136 full-text articles excluded 166 full-text articles excluded
table 1. Individual study characteristics are reported in
80 reinfection with pre-omicron 123 no relevant comparator the appendix (pp 14–37). For previous infection there
variant group were 97 estimates: 27 with a moderate risk of bias and
21 superseded by an updated 22 superseded by an updated
version of the article or version of the article or
updated cohort data updated cohort data
21 no relevant comparator group 12 wrong study design
8 reinfection defined as 6 timeframe between
<60 days between infections infections not reported Figure 1: Study selection
6 timeframe between 1 reinfection defined as *There were two rounds of full-text screening. Studies not meeting general
infections not reported <60 days between infections inclusion criteria were excluded in the first round. In the second round, articles
1 number of vaccines unclear
were screened with criteria specific to the types of exposures and comparators
1 ineligible vaccine
being reported (ie, previous infection and hybrid immunity). †There were
16 unique articles: nine articles reported on one study, five articles reported on
two studies (one on previous infection and one on hybrid immunity), one article
10 included articles that reported results 12 included articles that reported results reported on three studies (one on previous infection and two on hybrid
for 11 studies on the protection for 15 studies on the protection immunity), and one article reported on four studies (two on previous infection
conferred by previous infection*† conferred by hybrid immunity*†
and two on hybrid immunity). Seven articles reported data for previous
infection and hybrid immunity.
4 www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5
Articles
70 with a serious risk of bias. For hybrid immunity there 11 studies comprising a median of 294 900
were 153 estimates: 78 with a moderate risk of bias and (IQR 83 251–1 142 605) participants reported the protective
75 with a serious risk of bias. The most common reason effectiveness of previous infection (appendix pp 14–17). Of
for an increased risk of bias was incomplete adjustment these 11 studies, six reported on protection against hospital
for confounding factors (eg, testing frequency, comor admission or severe disease, ten reported on protection
bidity, or calendar time) and not reporting an a-priori against reinfection, and six reported protection against
protocol to enable ruling out reporting bias (appendix both, with the longest follow-up at 15 months (table 2,
pp 38–42). figure 2). The effectiveness of previous infection against
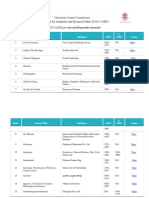
Studies focusing Studies focusing on hybrid immunity
on previous
infection
Previous infection Hybrid immunity Hybrid immunity Hybrid immunity Hybrid Summary of all
vs immune naive* vs immune naive* vs previous vs hybrid immunity vs hybrid immunity
(n=11) (n=9) infection* (n=7) immunity with vaccination* studies (n=15)
fewer vaccine (n=1)
doses* (n=4)
Study design
Cohort 2 (18%) 0 (0%) 2 (29%) 1 (25%) 1 (100%) 3 (20%)
Cross-sectional 1 (9%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%)
Test-negative design case–control 8 (73%) 7 (78%) 4 (57%) 2 (50%) 0 (40%) 9 (60%)
Traditional case–control 0 (0%) 2 (22%) 1 (14%) 1 (25%) 0 (0%) 3 (20%)
Total sample size 294 900 317 110 130 073 75 643 38 130 073
(83 251–1 142 605) (50 576–696 439) (14 625–470 984) (17 919–271 664) (14 625–335 882)
Study population
General population 11 (100%) 9 (100%) 6 (86%) 3 (75%) 1 (100%) 14 (93%)
Health-care workers 0 (0%) 0 (0%) 1 (14%) 1 (25%) 0 (0%) 1 (7%)
WHO region
African region 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%)
Region of the Americas 4 (36%) 3 (33%) 5 (71%) 3 (75%) 0 (0%) 6 (40%)
Eastern Mediterranean region 2 (18%) 2 (22%) 0 (0%) 0 (0%) 0 (0%) 2 (13%)
European region 5 (45%) 4 (44%) 2 (29%) 1 (25%) 1 (100%) 7 (47%)
South-East Asia region 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%)
Western Pacific region 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%) 0 (0%)
Reported the sequence of index infection and vaccination ·· 4 (44%) 5 (71%) 3 (75%) 1 (100%) 9 (60%)
Reported omicron (B.1.1.529) subvariants 4 (36%) 5 (56%) 1 (14%) 1 (25%) 0 (0%) 6 (40%)
Primary infection dominant variant
Alpha (B.1.1.7) 1 (9%) 1 (11%) 0 (0%) 0 (0%) 0 (0%) 1 (7%)
Delta (B.1.617.2) 3 (27%) 4 (44%) 0 (0%) 0 (0%) 0 (0%) 4 (27%)
Mixed variant 9 (82%) 7 (78%) 7 (100%) 4 (100%) 1 (100%) 13 (87%)
Primary series vaccination for hybrid immunity† ·· 9 5 3 ·· 12
Inactivated: CoronaVac (Sinovac) ·· 1 (11%) 1 (14%) 0 (0%) ·· 1 (7%)
mRNA: BNT162b2 (Pfizer–BioNTech) ·· 1 (11%) 1 (14%) 0 (0%) ·· 2 (13%)
mRNA: mRNA-1273 (Moderna) ·· 1 (11%) 0 (0%) 0 (0%) ·· 1 (7%)
mRNA: BNT162b2 (Pfizer–BioNTech) plus mRNA-1273 (Moderna) ·· 2 (22%) 3 (43%) 3 (100%) ·· 5 (33%)
NRVV: Vaxzevria (Oxford–AstraZeneca) ·· 1 (11%) 1 (14%) 0 (0%) ·· 1 (7%)
NRVV: Ad26.COV2.S (Janssen) ·· 1 (11%) 1 (14%) 0 (0%) ·· 1 (7%)
Mixed (inactivated plus NRVV plus mRNA)‡ ·· 5 (56%) 4 (57%) 0 (0%) ·· 8 (53%)
First booster vaccination for hybrid immunity† ·· 7 5 4 1 12
Inactivated: CoronaVac (Sinovac) ·· 1 (11%) 1 (14%) 0 (0%) 0 (0%) 1 (7%)
mRNA: BNT162b2 (Pfizer–BioNTech) ·· 2 (22%) 1 (14%) 0 (0%) 0 (0%) 3 (20%)
mRNA: BNT162b2 (Pfizer–BioNTech) plus mRNA-1273 (Moderna) ·· 2 (22%) 3 (43%) 3 (75%) 1 (100%) 7 (470%)
NRVV: Vaxzevria (Oxford–AstraZeneca) ·· 1 (11%) 1 (14%) 0 (0%) 0 (0%) 1 (7%)
NRVV: Ad26.COV2.S (Janssen) ·· 1 (11%) 1 (14%) 0 (0%) 0 (0%) 1 (7%)
Mixed (inactivated plus NRVV plus mRNA)‡ ·· 2 (22%) 1 (14%) 1 (25%) 0 (0%) 3 (20%)
(Table 1 continues on next page)
www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5 5
Articles
Studies focusing Studies focusing on hybrid immunity
on previous
infection
Previous infection Hybrid immunity Hybrid immunity Hybrid immunity Hybrid Summary of all
vs immune naive* vs immune naive* vs previous vs hybrid immunity vs hybrid immunity
(n=11) (n=9) infection* (n=7) immunity with vaccination* studies (n=15)
fewer vaccine (n=1)
doses* (n=4)
(Continued from previous page)
Type of reinfection§
Confirmed 3 (27%) 3 (33%) 0 (0%) 0 (0%) 0 (0%) 3 (20%)
Probable 6 (55%) 6 (67%) 7 (100%) 4 (100%) 0 (0%) 11 (73%)
Possible 2 (18%) 0 (0%) 0 (0%) 0 (0%) 1 (100%) 1 (7%)
Reinfection severity¶
Any reinfection 10 (91%) 8 (89%) 6 (86%) 4 (100%) 1 (100%) 13 (87%)
Severe disease (includes hospital admission) 7 (64%) 6 (67%) 3 (43%) 1 (25%) 0 (0%) 7 (47%)
Severe disease (as per WHO definition) 4 (36%) 4 (44%) 0 (0%) 0 (0%) 0 (0%) 4 (27%)
Adjustment of primary estimate
None 2 (18%) 1 (11%) 2 (29%) 1 (25%) 1 (100%) 2 (13%)
Population characteristics only 3 (27%) 0 (0%) 1 (14%) 0 (0%) 0 (0%) 1 (7%)
Time only 0 (0%) 0 (0%) 1 (14%) 1 (25%) 0 (0%) 1 (7%)
Population and time 6 (55%) 8 (89%) 3 (43%) 2 (50%) 0 (0%) 11 (73%)
Data are n (%) or median (IQR). NRVV=non-replicating viral vector. *Seven studies reported results on both the protection conferred by previous infection and hybrid immunity. Hybrid immunity studies can be
included in more than one column where they report multiple effect measures. †Percentages in the columns summarising hybrid immunity studies can add up to more than 100% where studies report multiple
vaccine types. ‡The mixed vaccination category included the following types of vaccines: inactivated (BBIBP-CorV [Sinopharm]); non-replicating viral vector (Vaxzevria [Oxford–AstraZeneca], Ad26.COV2.S
[Janssen], and Sputnik-V [Gamaleja]); and mRNA (BNT162b2 [Pfizer–BioNTech] and mRNA-1273 [Moderna]). §SARS-CoV-2 reinfection was defined as a possible, probable, or confirmed reinfection case
according to adapted WHO definitions.11 ¶Percentages can add up to more than 100% where studies report multiple levels of reinfection severity.
Table 1: Study characteristics
hospital admission or severe disease was 82·5% (95% CI immunity (with primary series vaccination) against
71·8 to 89·7) at 3 months; this was stable over time, hospital admission or severe disease was 96·0% (95% CI
reaching 74·6% (63·1 to 83·5) at 12 months (percentage 89·0 to 98·6) at 3 months and remained stable at 97·4%
point change –7·8% [95% CI –20·9 to 12·1]) and 71·6% (91·4 to 99·2) in projections at 12 months (percentage
(57·1 to 82·6) at 15 months (percentage point change point change 1·3% [95% CI –4·3 to 7·4]). The effectiveness
–10·9% [–29·4 to 12·7]). The effectiveness of previous of hybrid immunity (with primary series vaccination)
infection against reinfection was 65·2% (95% CI against reinfection was 69·0% (95% CI 58·9 to 77·5) at
52·9 to 75·9) at 3 months, dropping to 24·7% (16·4 to 35·5) 3 months, dropping to 41·8% (31·5 to 52·8) at 12 months
at 12 months (percentage point change –40·5% [95% CI (percentage point change –27·2% [95% CI –6·4 to –53·2]).
–51·9 to –33·9]) and 15·5% (9·9 to 23·6) at 15 months Of the seven studies that evaluated the protection
(percentage point change –49·7% [–42·2 to –62·8]). conferred by hybrid immunity with the first booster
Nine studies, involving a median of 317 110 vaccination over time, four reported on protection against
(IQR 50 576–696 439) participants, reported the protective hospital admission or severe disease, six reported on
effectiveness of hybrid immunity compared to immune- protection against reinfection, and three reported on
naive individuals, all of which reported on infection in protection against both, with the longest follow-up of
combination with primary series vaccination. Seven 4 months (table 2, figure 2). The effectiveness of hybrid
studies, involving a median of 317 110 (IQR 172 738–807 329) immunity with the first booster vaccination against
participants, reported on the protective effectiveness of hospital admission or severe disease was 97·2% (95% CI
previous infection in combination with the first booster 90·0 to 99·3) at 3 months and remained stable at 95·3%
vaccination. (81·9 to 98·9) in projections at 6 months (percentage
Of the nine studies that evaluated the protection point change –1·8 [95% CI –10·3 to 0·77]). The
conferred by hybrid immunity with primary series effectiveness of hybrid immunity with the first booster
vaccination over time, five reported on protection against against reinfection was 68·6% (95% CI 58·8 to 76·9) at
hospital admission or severe disease, seven reported on 3 months, dropping to 46·5% (36·0 to 57·3) at 6 months
protection against reinfection, and three reported (percentage point change –22·0 [95% C I–4·3 to –38·8]).
protection against both, with the longest follow-up at Seven studies, involving a median of 130 073
11 months (table 2, figure 2). The effectiveness of hybrid (IQR 14 625–470 984) participants, reported the comparative
6 www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5
Articles
Number Number Month 1* Month 2† Month 3 Month 4 Month 6 Month 9 Month 12 Month 15 Percentage Percentage
of of point point change
studies estimates change in in
protection, protection,
3–6 months 3–12 months
(95% CI)‡ (95% CI)‡
Previous infection
Hospital 6 16 NA 83·2% (72·1 82·5% (71·8 81·7% (71·4 80·1% (70·3 77·5% (67·5 74·6% (63·1 71·6% (57·1 –2·4 (–5·1 –7·8 (–20·9
admission or to 90·5) to 89·7) to 88·9) to 87·2) to 85·1) to 83·5) to 82·6) to 4·7) to 12·1)
severe disease
Any 10 64 NA 69·5% (57·6 65·2% (52·9 60·7% (48 51·2% (38·6 37·0% (26 24·7% (16·4 15·5% (9·9 –14·0 (–12·0 –40·5 (–33·9
infection§ to 79·2) to 75·9) to 72·1) to 63·7) to 49·6) to 35·5) to 23·6) to –18·2) to –51·9)
Hybrid immunity (primary series vaccination)
Hospital 5 23 95·7% (88·0 95·9% (88·5 96·0% (89·0 96·2% (89·4 96·5% (90·2 97·0% (90·9 97·4% (91·4 NA 0·50 (–2·2 1·3 (–4·3 to
admission or to 98·5) to 98·6) to 98·6) to 98·7) to 98·8) to 99) to 99·2)¶ to 2·1) 7·4)
severe disease
Any infection 7 55 74·1% (64·8 71·6% (61·9 69·0% (58·9 66·2% (55·8 60·4% (49·6 51·1% (40·2 41·8% (31·5 NA –8·6 (–1·7 –27·2 (–6·4 to
to 81·6) to 79·6) to 77·5) to 75·3) to 70·3) to 61·9) to 52·8)¶ to –17·2) –53·2)
Hybrid immunity (first booster vaccination)
Hospital 4 17 98·0% (92·9 97·6% (91·6 97·2% (90·0 96·7% (87·9 95·3% (81·9 NA NA NA –1·8 (–10·3 NA
admission or to 99·5) to 99·4) to 99·3) to 99·1) to 98·9)¶ to 0·77)
severe disease
Any infection 6 24 80·1% (72·5 74·8 (66·0 68·6% (58·8 61·6% (51·2 46·5% (36·0 NA NA NA –22·0 (–4·3 NA
to 86) to 81·9) to 76·9) to 71·1) to 57·3)¶ to –38·8)
This table displays the point estimates and 95% CIs of protection shown in figure 2. This analysis used a log-odds meta-regression model. NA=not available (ie, insufficient data for model extrapolation).
*Month 1 data were for individuals with hybrid immunity whose last immunological challenge was vaccination and thus were eligible for reinfection within a shorter timeframe than people who most recently
had previous infection (2 months minimum for probable reinfection). †Month 2 data represent the minimum time period for reinfection among individuals with previous infection (ie, possible reinfection).
‡95% CIs calculated with the bootstrap method. Percentage point changes over time are reported from 3 months as this represents probable and confirmed reinfections. §Any infections comprised mild
infections, symptomatic infections, and asymptomatic infections. ¶Model predictions beyond the range of the available data. Previous infection data are available for predictions for 2–16 months; hybrid
immunity data were available for predictions for 1–11 months. Data were extrapolated to a maximum of 3 months beyond the final follow-up date.
Table 2: Protection conferred by previous infection and hybrid immunity compared to immune-naive individuals
A Previous infection B Hybrid immunity (primary series vaccine) C Hybrid immunity (booster)
Hospital admission or severe disease Hospital admission or severe disease Hospital admission or severe disease
100
75
Protection (%)
50
25
Any infection Any infection Any infection
100
75
Protection (%)
50
25
0
0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16
Time since previous infection (months) Time since last vaccination or infection (months) Time since last vaccination or infection (months)
Figure 2: Protection against omicron variant conferred by previous infection or hybrid immunity compared to immune-naive individuals over time
This analysis uses a log-odds meta-regression model. Points of the same color represent estimates from the same study. The diameter of the circles varies with the sample size of the study. Dotted lines
represent 95% CIs. Solid black lines represent point estimates.
www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5 7
Articles
Exposure Comparator Number Number of Pooled relative
of studies estimates protection (95% CI)
Hybrid immunity vs previous infection
Hospital admission or severe disease Previous infection plus partial primary series Previous infection 2 3 28·9% (14·4–49·6)
vaccine
Any infection Previous infection plus partial primary series Previous infection 2 2 59·0% (51·5–66·1)
vaccine
Hospital admission or severe disease Previous infection plus full primary series Previous infection 3 4 57·7% (28·6–82·2)
Any infection Previous infection plus full primary series Previous infection 4 5 46·1% (30·6–62·4)
Hospital admission or severe disease Previous infection plus first booster dose Previous infection 3 3 80·1% (48·6–94·5)
Any infection Previous infection plus first booster dose Previous infection 4 5 46·5% (24·6–69·9)
Hybrid immunity vs vaccination
Any infection Previous infection plus first booster dose First booster dose 1 1 88·9% (29·5–98·2)
Hybrid immunity vs hybrid immunity with fewer vaccine doses
Hospital admission or severe disease Previous infection plus full primary series Previous infection plus partial primary series vaccine 1 2 49·6% (19·9–79·7)
Any infection Previous infection plus full primary series Previous infection plus partial primary series vaccine 1 1 16·3% (11·1–21·2)
Hospital admission or severe disease Previous infection plus first booster dose Previous infection plus partial primary series vaccine 1 1 67·1% (21·1–86·3)
Any infection Previous infection plus first booster dose Previous infection plus partial primary series vaccine 2 2 5·8% (0·2–65·2)
Hospital admission or severe disease Previous infection plus first booster dose Previous infection plus full primary series 1 2 37·0% (6·2–83·9)
Any infection Previous infection plus first booster dose Previous infection plus full primary series 3 3 40·8% (22·0–62·7)
There were insufficient data available for a sensitivity analysis.
Table 3: Comparative protective effectiveness of hybrid immunity relative to previous infection, vaccination, and hybrid immunity with fewer vaccine doses
protective effectiveness of hybrid immunity relative to conferred significant gains in protection against both
individuals with previous infection only, of which five hospital admission or severe disease and reinfection;
reported on hybrid immunity with primary series however, data were scarce for some comparisons (table 3).
vaccination, and five reported on hybrid immunity with One cohort study of 38 older adults (aged 71–101 years)
the first booster vaccination (appendix pp 18–37). Of these done in France19 reported the comparative protective
seven studies, one reported protection against hospital effectiveness of hybrid immunity with the first booster
admission or severe disease, four reported protection vaccination series relative to the first booster vacci
against reinfection, and two reported protection against nation only with the BNT162b2 (Pfizer–BioNTech) or
both, with the longest follow-up of 11 months (appendix mRNA-1273 (Moderna) vaccines. After 90 days since the
pp 18–37). Data were insufficient for meta-regression; last immunological challenge, the estimate of protection
however, the meta-analysis showed that hybrid immunity against reinfection with the omicron variant was 88·9%
conferred a significant gain in protection compared to (95% CI 29·5–98·2), indicating that hybrid immunity in
previous infection alone, including with partial primary combination with the first booster vaccination conferred
series (28·9% [95% CI 14·4–49·6] against hospital a significant gain in protection compared to first booster
admission or severe disease [two studies] and 59·0% vaccination alone (appendix p 25).
[51·5–66·1] against reinfection [two studies]); full primary The appendix includes the subgroup analyses and
series (57·7% [28·6–82·2] against hospital admission or summaries of results for studies reporting data by age
severe disease [three studies] and 46·1% [30·6–62·4] (pp 43–44), vaccine type (p 45), and index variant (p 46).
against reinfection [ four studies]), and the first booster Sensitivity analyses excluding estimates with a serious
vaccination (80·1% [48·6–94·5] against hospital admission risk of bias and excluding hospital admission from the
or severe disease [three studies] and 46·5% [24·6–69·9%] severe disease outcome showed similar findings as the
against reinfection [ four studies]; table 3). main analyses (appendix pp 47–49). Definitions of severe
Four studies, involving a median of 75 643 disease used in each study are reported in the appendix
(IQR 17 919–271 664) participants, reported the com (p 51).
parative protective effectiveness of hybrid immunity with Meta-regression showed that against hospital
more vaccine doses relative to individuals with hybrid admission or severe disease at 6 months, hybrid
immunity with fewer vaccine doses. Of these four immunity with the first booster vaccination (95·3%
studies, three reported protection against reinfection and [95% CI 81·9–98·9]) or hybrid immunity with the
one reported protection against both reinfection and primary series (96·5% [90·2–98·8]) provided significantly
hospital admission or severe disease, with the longest greater protection than previous infection alone (80·1%
follow-up of 3 months (appendix pp 18–37). In general, [70·3–87·2]), the first booster vaccination alone (76·7%
hybrid immunity with a greater number of vaccinations [72·5–80·4]), or the primary series alone (64·6%
8 www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5
Articles
[54·5–73·6]; figure 3; appendix p 52). Against reinfection Primary series First booster dose Infection plus primary series
at 6 months, there was a similar protection conferred by Infection plus first booster dose Previous infection
hybrid immunity with the first booster vaccination Hospital admission or severe disease Any infection
(46·5% [95% CI 36·0–57·3]), hybrid immunity with the 100
primary series (60·4% [49·6–70·3]), and previous
infection alone (51·2% [38·6–63·7]), with all three types 75
Protection (%)
of immunity conferring significantly greater protection
50
than primary series vaccination alone (15·1% [11·3–19·8])
or first booster vaccination alone (24·8% [18·5–32·5];
25
figure 3; appendix p 52).
0
Discussion 0 1 2 3 4 5 6 7 8 0 1 2 3 4 5 6 7 8
Time since last vaccination or infection (months) Time since last vaccination or infection (months)
This systematic review and meta-regression found that
both previous infection alone and previous infection Figure 3: Protection against omicron variant conferred by the primary series vaccine, first booster vaccine,
combined with previous vaccination (ie, hybrid immunity) previous infection, and hybrid immunity compared to immune-naive individuals over time
conferred rapidly waning protection against SARS-CoV-2 The shaded areas denote 95% CIs. Vaccine effectiveness data were procured from a separate systematic review.
infection with the omicron variant, but high and sustained
protection against hospital admission or severe disease or who has had a breakthrough infection after initiation
due to the omicron variant. Previous infection was found of the primary series compared to a previously
to provide higher protection against reinfection and more uninfected individual. Our findings are in line with a
sustained protection against hospital admission or severe recent study that reported a higher quality and
disease than vaccination alone. However, individuals with magnitude of immune responses (antibodies and
hybrid immunity had the highest magnitude and B cells) with a longer interval between infection and
durability of protection against all outcomes, emphasising booster vaccination (>180 days).36 It might therefore be
the importance of providing vaccination to previously reasonable for individuals with a previous infection and
infected individuals. full primary series vaccination to delay subsequent doses
Another systematic review similarly reported rapid of vaccination by 6 months, while still maintaining high
waning of protection against infection with the omicron levels of protection against severe disease.
variant, but was unable to infer protection against severe On a population level, the optimal number of vaccine
disease over time and did not examine hybrid immunity.7 doses and the inter-dose interval might differ in settings
Previous studies have similarly reported that previous with various degrees of vaccine-induced versus infection-
infection confers more durable protection than induced immunity. However, well designed serosurveys
vaccination.31 This pattern might be explained by natural are required for estimating infection-induced sero
infection invoking a more diverse immune response to prevalence rates and reliable estimates can only be
multiple antigenic sites on the virus compared to the generated in countries where inactivated vaccines were
immunity developed through vaccines that target only not used. Considering this caveat, basing national
spike antigens. vaccination policies on infection-induced seroprevalence
Protection from previous infection should not detract rates could be challenging in many settings.
from the need for vaccination. Infection-induced protec In countries where only S-protein antigen vaccines were
tion against reinfection wanes rapidly, and vaccination used, it might be possible to classify individuals as
increases durability. Furthermore, there are serious risks previously infected with an anti-N antibody test and use
associated with infection. These include the risks of this to modify recommendations for boosters. However,
hospital admission, ICU admission and mechanical this approach might not be reasonable for high-risk
ventilation, and death; they also include the risk of groups, including older people and immunocompromised
developing post-COVID-19 complications. Additionally, individuals, since our data were not stratified by patient
those who recover from severe COVID-19 have a demographics. Caution is also required as programmatic
higher risk of cardiovascular complications, neurological vaccine rollout should be as simple as possible; modifying
complications, dementia, diabetes, and chronic respiratory the number of vaccines and intervals by infection-induced
problems.32,33 Vaccination is therefore a safe intervention to seroprevalence rates could complicate vaccine programmes
avert severe disease outcomes and to reduce post- and thus hamper vaccine uptake. Further more, pre-
COVID-19 complications.34 Reassuringly, vaccination after vaccination screening for past infections is not
natural infection is not thought to be associated with an recommended by WHO,37 similar to other mass vaccination
increased risk of reactogenicity or other safety concerns.35 programmes (eg, measles) where past infections are not a
At the individual level, our results show that the need reason to exclude individuals from vaccination or delay
for, and optimal timing of, the primary vaccination vaccination. Additionally, there might still be benefit in
series and booster dose might be different in an providing boosters before periods with expected increased
individual who has previously had SARS-CoV-2 infection incidence, such as the winter season, to individuals whose
www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5 9
Articles
last immunological challenge is unknown. In fact, this the same method that was used for the data on previous
scenario is common as the prevalence of infection has infection and hybrid immunity. Sixth, we were only able
been largely underestimated in most settings throughout to examine protection conferred by pre-omicron SARS-
the pandemic.3 CoV-2 variants (ie, the index virus through to the delta
Our systematic review had several potential limitations. [B.1.617.2] variant). Future evidence synthesis will be
First, the patterns of declining protection observed in needed to ascertain the protection conferred by the
this study might be explained by waning immunity; omicron variant against reinfection.
however, these results could also be in part attributable Our findings make clear the substantial durability of
to unmeasured biases. The observational studies we hybrid immunity and could help inform the timing and
included assumed that all individuals had the same prioritisation of vaccination programmes in populations
risk of exposure. However, differential depletion of with high rates of past infection. Further follow-up is
susceptibles bias could have occurred, where, when the needed to assess the protective effectiveness of hybrid
vaccine is effective, people who are infected are more immunity against hospital admission or severe disease,
likely to be unvaccinated than vaccinated, thus reducing the two outcomes that drive most COVID-19 policy
the proportion of susceptible individuals in the decisions, to clarify how much waning of protection
unvaccinated group and creating the appearance of might occur over a longer duration, especially if new
waning.38 Exposure could also differ between groups, as variants of concern emerge. More precise quantification
in the case of individuals who are unvaccinated because of the duration of this protection will help inform the
they are severely immunocompromised, and thus necessity and timing of future booster vaccinations.
also have a greater risk of infection. The likelihood of Policy makers can use these findings to project
measuring an outcome could also differ between groups population protection from local vaccination and
(eg, individuals with no previously reported infection seroprevalence rates, helping to inform the use and
who might not have had access to testing). Individual timing of COVID-19 vaccination as an important public
studies adjusted for some of these factors (eg, calendar health tool.
time, age, comorbidities, and testing frequency) and Contributors
these adjustments were considered in the risk of bias NB, LAR, DLB, IB, RKA, AWS, DF, MKP, LS, and MDVK were
assessment; however, not all studies reported these responsible for conceptualisation of the study. NB, ZL, ZP, HI, BC,
MMH, RKA, DF, MKP, and LS were responsible for data curation.
adjustments. Second, our analysis did not incorporate NB, ZL, HW, XM, LAR, RKA, DF, MKP, and LS were responsible for
the sequence of and timing between vaccination and formal analysis. NB, RKA, MDVK, and IB were responsible for
previous infection for hybrid immunity. Nine studies acquisition of funding. NB, ZL, HW, XM, ZP, LAR, VP, MMH, RKA,
reported information on the sequence of immunological AWS, DF, MKP, and LS were responsible for the methodology.
NB, MW, DLB, RKA, AWS, IB, DF, MKP, and LS were responsible for
challenges; however, the data were spread across different project administration. NB, RKA, MDVK, IB, and LS were responsible
types of exposures (eg, hybrid immunity with different for resources. NB, LAR, DLB, IB, MMH, MDVK, RKA, AWS, IB, DF,
numbers of vaccine doses) and sequence permutations. MKP, and LS were responsible for supervision of the study. NB, ZL,
Data from studies measuring neutralising antibodies XM, RH, CC, AS, and VP were responsible for validation of the data.
NB, HW, XM, and LAR were responsible for visualisation of the data.
suggest that the sequence and timing of immunological NB, HW, ZP, XM, RKA, and LS were responsible for writing the
challenges could interact with the level of protection original draft of the manuscript. All authors were responsible for
conferred,36,39 but further studies with linked individual- review and editing of the manuscript. All authors debated, discussed,
level data are needed. Third, data were scarce for some edited, and approved the final version of the manuscript. NB, HW, XM,
and ZL had full access to the full data in the study and verified all the
analyses, which implies the need for caution in data. All authors had final responsibility for the decision to submit the
interpretation of results, particularly for estimates of the manuscript for publication. The authors alone are responsible for the
comparative protective effectiveness of hybrid immunity views expressed in this publication and they do not necessarily
relative to vaccination, estimates by vaccination type, and represent the decisions, policy, or views of WHO or the Coalition for
Epidemic Preparedness Innovations (CEPI).
estimates by the variant causing the primary infection.
Declaration of interests
Scarce data also precluded stratified analyses by age, sex,
NB, HW, XM, ZL, RH, CC, AS, MW, BC, and RKA report grants
ethnicity, severity of primary infection, and protection unrelated to the present work from the WHO Health Emergencies
against the distinct omicron subvariants. Stratifications Program, the Public Health Agency of Canada through Canada’s
by participant demographic characteristics were often COVID-19 Immunity Task Force (grant 2021-HQ-000056), the
Robert Koch Institute, and the Canadian Medical Association Joule
omitted by researchers and should be consistently
Innovation Fund. HI reports contracts unrelated to the present work
reported. Fourth, in the 11 studies reporting data based from WHO. MMH reports contracts unrelated to the present work from
on multiple vaccines, the relative proportions of WHO, Pfizer, and the Bill & Melinda Gates Foundation. VP is an unpaid
individuals vaccinated by each product was unclear, governing board member and Royal Trustee at Cochrane. RKA reports
consulting fees unrelated to the present work from the Bill &
complicating our ability to generate estimates specific to
Melinda Gates Foundation Strategic Investment Fund, Health Canada,
vaccine brands. Fifth, the vaccine effectiveness data were and Flagship Pioneering, and stock in Alethea Medical that is unrelated
procured from a separate systematic review. However, to the present work. MDVK, IB, DF, and LS are employed by WHO.
the inclusion and exclusion criteria were similar to our MMH has contracts with WHO, CEPI, and the Asian Development
Bank to gather data on COVID-19 vaccine efficacy, effectiveness, and
study. Furthermore, we re-analysed the raw data using
10 www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5
Articles
safety from published studies, and reports unrelated grants from Pfizer 18 Björk J, Bonander C, Moghaddassi M, et al. COVID-19 vaccine
and the Bill & Melinda Gates Foundation. AW-S and MKP consult on effectiveness against severe disease from SARS-CoV-2 Omicron
COVID-19 research and policy for WHO. BA.1 and BA.2 subvariants - surveillance results from southern
Sweden, December 2021 to March 2022. Euro Surveill 2022;
Data sharing 27: 2200322.
The statistical code for our main model is available online on GitHub. 19 Bruel T, Pinaud L, Tondeur L, et al. Neutralising antibody responses For the statistical code see
Data extracted from published articles and used in our analysis will be to SARS-CoV-2 omicron among elderly nursing home residents https://github.com/serotracker/
made available upon request via email to the corresponding author. Data following a booster dose of BNT162b2 vaccine: a community-based, protective-effectiveness
provided to us directly by authors of the included studies will not be prospective, longitudinal cohort study. EClinicalMedicine 2022;
shared unless the investigators requesting data obtain permission from 51: 101576.
the original study authors. 20 Carazo S, Skowronski DM, Brisson M, et al. Protection against
omicron (B.1.1.529) BA.2 reinfection conferred by primary omicron
Acknowledgments BA.1 or pre-omicron SARS-CoV-2 infection among health-care
We thank the authors of the included studies who responded to our data workers with and without mRNA vaccination: a test-negative case-
requests and provided aggregate data for use in analysis. We also thank control study. Lancet Infect Dis 2022; published online Sept 21.
the WHO COVID-19 Solidarity Response Fund and CEPI for their https://10.1016/S1473-3099(22)00578-3.
funding support. 21 Cerqueira-Silva T, de Araujo Oliveira V, Paixão ES, et al. Vaccination
plus previous infection: protection during the omicron wave in
References
Brazil. Lancet Infect Dis 2022; 22: 945–46.
1 Jeffery-Smith A, Rowland TAJ, Patel M, et al. Reinfection with new
variants of SARS-CoV-2 after natural infection: a prospective 22 Chin ET, Leidner D, Lamson L, et al. Protection against omicron
observational cohort in 13 care homes in England. conferred by mRNA primary vaccine series, boosters, and prior
Lancet Healthy Longev 2021; 2: e811–19. infection. medRxiv 2022; published online May 27. https://doi.
org/10.1101/2022.05.26.22275639 (preprint).
2 Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the
BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 2020; 383: 2603–15. 23 Lind ML, Robertson AJ, Silva J, et al. Effectiveness of primary and
booster COVID-19 mRNA vaccination against omicron variant
3 Bergeri I, Whelan MG, Ware H, et al. Global SARS-CoV-2
SARS-CoV-2 infection in people with a prior SARS-CoV-2 infection.
seroprevalence from January 2020 to April 2022: a systematic review
medRxiv 2022; published online April 25. https://doi.
and meta-analysis of standardized population-based studies.
org/10.1101/2022.04.19.22274056 (preprint).
PLoS Med 2022; 19: e1004107.
24 Medić S, Anastassopoulou C, Lozanov-Crvenković Z, et al. Risk and
4 Sallam M. COVID-19 vaccine hesitancy worldwide: a concise
severity of SARS-CoV-2 reinfections during 2020-2022 in Vojvodina,
systematic review of vaccine acceptance rates. Vaccines 2021; 9: 160.
Serbia: a population-level observational study. Lancet Reg Health Eur
5 Feikin DR, Higdon MM, Abu-Raddad LJ, et al. Duration of 2022; 20: 100453.
effectiveness of vaccines against SARS-CoV-2 infection and
25 Michlmayr D, Hansen CH, Gubbels SM, et al. Observed
COVID-19 disease: results of a systematic review and meta-
protection against SARS-CoV-2 reinfection following a primary
regression. Lancet 2022; 399: 924–44.
infection: a Danish cohort study among unvaccinated using
6 Higdon MM, Baidya A, Walter KK, et al. Duration of effectiveness two years of nationwide PCR-test data. Lancet Reg Health Eur
of vaccination against COVID-19 caused by the omicron variant. 2022; 20: 100452.
Lancet Infect Dis 2022; 22: 1114–16.
26 Nielsen KF, Moustsen-Helms IR, Schelde AB, et al. Vaccine
7 COVID-19 Forecasting Team. Lim SS. Past SARS-CoV-2 infection effectiveness against SARS-CoV-2 reinfection during periods of
protection against reinfection: a systematic review and meta- alpha (B.1.1.7), delta (B.1.617.2) or omicron (B.1.1.529) dominance:
analysis. SSRN 2022; published online July 6. https://papers.ssrn. a Danish nationwide study. medRxiv 2022; published online June 1.
com/abstract=4155225 (preprint). https://doi.org/10.1101/2022.06.01.22275858 (preprint).
8 Higgins J, Thomas J, Chandler J, et al. Cochrane Handbook for 27 Nyberg T, Ferguson NM, Nash SG, et al. Comparative analysis of
Systematic Reviews of Interventions. Version 6.3 (updated the risks of hospitalisation and death associated with SARS-CoV-2
February 2022). https://training.cochrane.org/handbook (accessed omicron (B.1.1.529) and delta (B.1.617.2) variants in England:
Sept 2, 2022). a cohort study. Lancet 2022; 399: 1303–12.
9 Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 28 Plumb ID, Feldstein LR, Barkley E, et al. Effectiveness of COVID-19
statement: an updated guideline for reporting systematic reviews. mRNA vaccination in preventing COVID-19-associated
PLoS Med 2021; 18: e1003583. hospitalization among adults with previous SARS-CoV-2 infection -
10 WHO. WHO COVID-19 case definition - updated in public health United States, June 2021–February 2022.
surveillance for COVID-19. July 22, 2022. https://www.who.int/ MMWR Morb Mortal Wkly Rep 2022; 71: 549–55.
publications-detail-redirect/WHO-2019-nCoV-Surveillance_Case_ 29 Shrestha NK, Shrestha P, Burke PC, Nowacki AS, Terpeluk P,
Definition-2022.1 (accessed Sept 2, 2022). Gordon SM. Coronavirus disease 2019 vaccine boosting in
11 WHO. Living guidance for clinical management of COVID-19. previously infected or vaccinated individuals (COVID-19).
Nov 23, 2021. https://apps.who.int/iris/bitstream/handle/10665/ Clin Infect Dis 2022; published online April 27. https://doi.
349321/WHO-2019-nCoV-clinical-2021.2-eng.pdf (accessed org/10.1093/cid/ciac327.
Nov 30, 2022). 30 Šmíd M, Berec L, Přibylová L, et al. Protection by vaccines and
12 Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for previous infection against the omicron variant of severe acute
assessing risk of bias in non-randomised studies of interventions. respiratory syndrome coronavirus 2. J Infect Dis 2022;
BMJ 2016; 355: i4919. 226: 1385–90.
13 Musekiwa A, Manda SOM, Mwambi HG, Chen DG. Meta-analysis 31 Gazit S, Shlezinger R, Perez G, et al. Severe acute respiratory
of effect sizes reported at multiple time points using general linear syndrome coronavirus 2 (SARS-CoV-2) naturally acquired immunity
mixed model. PLoS One 2016; 11: e0164898. versus vaccine-induced immunity, reinfections versus breakthrough
14 Berkey CS, Hoaglin DC, Antczak-Bouckoms A, Mosteller F, infections: a retrospective cohort study. Clin Infect Dis 2022;
Colditz GA. Meta-analysis of multiple outcomes by regression with 75: e545–51.
random effects. Stat Med 1998; 17: 2537–50. 32 Kompaniyets L, Pennington AF, Goodman AB, et al. Underlying
15 Altarawneh HN, Chemaitelly H, Ayoub HH, et al. Effects of medical conditions and severe illness among 540,667 adults
previous infection and vaccination on symptomatic omicron hospitalized with COVID-19, March 2020–March 2021.
infections. N Engl J Med 2022; 387: 21–34. Prev Chronic Dis 2021; 18: E66.
16 Altarawneh HN, Chemaitelly H, Hasan MR, et al. Protection 33 Xu E, Xie Y, Al-Aly Z. Long-term neurologic outcomes of COVID-19.
against the omicron variant from previous SARS-CoV-2 infection. Nat Med 2022; 28: 2406–15.
N Engl J Med 2022; 386: 1288–90. 34 Notarte KI, Catahay JA, Velasco JV, et al. Impact of COVID-19
17 Andeweg SP, de Gier B, Eggink D, et al. Protection of COVID-19 vaccination on the risk of developing long-COVID and on existing
vaccination and previous infection against Omicron BA.1, BA.2 and long-COVID symptoms: a systematic review. EClinicalMedicine
Delta SARS-CoV-2 infections. Nat Commun 2022; 13: 4738. 2022; 53: 101624.
www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5 11
Articles
35 Bardenheier BH, Gravenstein S, Blackman C, et al. Adverse events 38 Ray GT, Lewis N, Klein NP, Daley MF, Lipsitch M, Fireman B.
following one dose of mRNA COVID-19 vaccination among US Depletion-of-susceptibles bias in analyses of intra-season waning
nursing home residents with and without a previous SARS-CoV-2 of influenza vaccine effectiveness. Clin Infect Dis 2020;
infection. J Am Med Dir Assoc 2021; 22: 2228–32. 70: 1484–86.
36 Buckner CM, Kardava L, El Merhebi O, et al. Interval between prior 39 Jacobsen H, Cobos Jiménez V, Sitaras I, et al. Post-vaccination T cell
SARS-CoV-2 infection and booster vaccination impacts magnitude immunity to omicron. Front Immunol 2022; 13: 944713.
and quality of antibody and B cell responses. Cell 2022;
185: 4333–46.e14.
37 WHO. WHO SAGE roadmap for prioritizing use of COVID-19.
Jan 22, 2022. https://www.who.int/publications/i/item/WHO-2019-
nCoV-Vaccines-SAGE-Prioritization-2022.1 (accessed Nov 30, 2022).
12 www.thelancet.com/infection Published online January 18, 2023 https://doi.org/10.1016/S1473-3099(22)00801-5
You might also like
- 2023 03 17 Statement of ClaimDocument44 pages2023 03 17 Statement of ClaimCTV Calgary100% (1)
- Viewpoint: OnlineDocument4 pagesViewpoint: OnlineJoseph Adinolfi Jr.92% (12)
- Flower ShopDocument5 pagesFlower Shopndafuma71% (7)
- NEB mRNA Lisolation ManualDocument9 pagesNEB mRNA Lisolation Manual10sgNo ratings yet
- School Leadership - CompDocument35 pagesSchool Leadership - CompRaymund P. CruzNo ratings yet
- Dearborn 547Document3 pagesDearborn 547NuryNo ratings yet
- Sharp XLHF 203bDocument23 pagesSharp XLHF 203bJorge Sánchez RodríguezNo ratings yet
- Northern Peru Birding Route WebDocument1 pageNorthern Peru Birding Route WebRaul VillegasNo ratings yet
- CA Prospects ListDocument108 pagesCA Prospects ListJohn GroganNo ratings yet
- Thaer Abdulrahim QasirDocument45 pagesThaer Abdulrahim QasirOPL OJJJNo ratings yet
- Parking Permit FormDocument2 pagesParking Permit FormBrandon BriceNo ratings yet
- Birding in DeltaDocument2 pagesBirding in Deltaapi-269483056No ratings yet
- Coto de Caza Planning Advisory Committe (CPAC) Community Notice and ApplicationDocument5 pagesCoto de Caza Planning Advisory Committe (CPAC) Community Notice and Application"Buzz" AguirreNo ratings yet
- Olympic Booklet 8-7-2012Document13 pagesOlympic Booklet 8-7-2012vishwasvnNo ratings yet
- Housing Options For Adults With Autism - FINAL - 05-20-10Document88 pagesHousing Options For Adults With Autism - FINAL - 05-20-10aniko kollarNo ratings yet
- Reality TVDocument1 pageReality TVapi-508860665No ratings yet
- Lab GuidelinesDocument60 pagesLab GuidelinesTenaNo ratings yet
- Severe Pulmonary Arterial Hypertension - Stratification of Medical Therapies, Mechanical Support, and Lung TransplantationDocument11 pagesSevere Pulmonary Arterial Hypertension - Stratification of Medical Therapies, Mechanical Support, and Lung Transplantationjose lopeNo ratings yet
- PoliticDocument4 pagesPolitickhoa dangNo ratings yet
- Death Wish ListDocument6 pagesDeath Wish ListphilippatstonNo ratings yet
- TRABALHO Zika Virus Selectively Kills Aggressive Human Embryonal CNS Tumor Cells in Vitro and in Vivo - Cancer ResearchDocument20 pagesTRABALHO Zika Virus Selectively Kills Aggressive Human Embryonal CNS Tumor Cells in Vitro and in Vivo - Cancer ResearchAdonai AlvesNo ratings yet
- Jamainternal Sun 2021 Oi 210075 1643648297.88061Document10 pagesJamainternal Sun 2021 Oi 210075 1643648297.88061Leidy Nayerli Garcia RodriguezNo ratings yet
- Articles: BackgroundDocument9 pagesArticles: Backgroundgilang_8899No ratings yet
- Development of Novel Carrier(s) Mediated Tuberculosis Vaccine: More Than A Tour de ForceDocument17 pagesDevelopment of Novel Carrier(s) Mediated Tuberculosis Vaccine: More Than A Tour de ForceDrMuhamad Luthfi AsyharNo ratings yet
- Typhoid DeclineDocument13 pagesTyphoid Declinecalvinmagara1307No ratings yet
- Fourth Dose of BNT162b2 mRNA Covid-19 Vaccine in A Nationwide SettingDocument12 pagesFourth Dose of BNT162b2 mRNA Covid-19 Vaccine in A Nationwide SettinggersondcesgpNo ratings yet
- Long Term Effectiveness of COVID 19 Vaccines AgainDocument14 pagesLong Term Effectiveness of COVID 19 Vaccines Againsergio salazarNo ratings yet
- GhkmjgyfDocument12 pagesGhkmjgyfLucatntNo ratings yet
- MainDocument5 pagesMainFerdous HakimNo ratings yet
- Past SARS-CoV-2 Infection Protection Against Re-InfectionDocument10 pagesPast SARS-CoV-2 Infection Protection Against Re-InfectionRoel PlmrsNo ratings yet
- Piis258953702200061x PDFDocument11 pagesPiis258953702200061x PDFRong LiuNo ratings yet
- 1 s2.0 S0264410X23000348 MainDocument12 pages1 s2.0 S0264410X23000348 MainJose Luis Isazañ JoseNo ratings yet
- Human Challenge Studies To Accelerate Coronavirus Vaccine LicensureDocument5 pagesHuman Challenge Studies To Accelerate Coronavirus Vaccine LicensurePablo Segales BautistaNo ratings yet
- Vaccine Epidemiology Efficacy EffectivenessDocument5 pagesVaccine Epidemiology Efficacy EffectivenessCesar Augusto Hernandez GualdronNo ratings yet
- BNT162b2 mRNA Covid-19 Vaccine in A Nationwide Mass Vaccination SettingDocument12 pagesBNT162b2 mRNA Covid-19 Vaccine in A Nationwide Mass Vaccination SettingMushtofa KamalNo ratings yet
- Lancet CovidDocument17 pagesLancet CovidSergiu GutNo ratings yet
- Hepatitis B and The Need For A Booster DoseDocument8 pagesHepatitis B and The Need For A Booster DoseMekar PalupiNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundJoseph Adinolfi Jr.80% (5)
- Vaccine Technologies and Platforms For Infectious Diseases Current Progress, Challenges, and Opportunities-1Document31 pagesVaccine Technologies and Platforms For Infectious Diseases Current Progress, Challenges, and Opportunities-1anzueth lopezNo ratings yet
- Cost Utility of Vaccination Against COVID-19 in BrazilDocument8 pagesCost Utility of Vaccination Against COVID-19 in BrazilTatiana DutraNo ratings yet
- COVID-19 Vaccination of Patients With Chronic Immune-Mediated Inflammatory DiseaseDocument6 pagesCOVID-19 Vaccination of Patients With Chronic Immune-Mediated Inflammatory DiseaseSangeetha VijianNo ratings yet
- Sinovac JournalDocument10 pagesSinovac JournalGeulissa AddiniNo ratings yet
- Epid 1Document4 pagesEpid 1lakshanNo ratings yet
- Equivalency of Protection From Natural Immunity in COVID-19 Recovered Versus Fully Vaccinated Persons: A Systematic Review and Pooled AnalysisDocument30 pagesEquivalency of Protection From Natural Immunity in COVID-19 Recovered Versus Fully Vaccinated Persons: A Systematic Review and Pooled AnalysisPDFReadAndDevelopNo ratings yet
- Influence of A COVID-19 Vaccine's Effectiveness and Safety Profile On Vaccination AcceptanceDocument5 pagesInfluence of A COVID-19 Vaccine's Effectiveness and Safety Profile On Vaccination AcceptancencNo ratings yet
- 1 s2.0 S1473309922003450 MainDocument9 pages1 s2.0 S1473309922003450 Maincathylamont816No ratings yet
- Women Who Received Varicella Vaccine Versus Natural Infection Have Different Long-Term T Cell Immunity But Similar Antibody Levels 2020Document5 pagesWomen Who Received Varicella Vaccine Versus Natural Infection Have Different Long-Term T Cell Immunity But Similar Antibody Levels 2020Mohan PrasadNo ratings yet
- Community Acquired Pneumonia In+childrenDocument4 pagesCommunity Acquired Pneumonia In+childrendai shujuanNo ratings yet
- Fimmu 13 782198Document11 pagesFimmu 13 782198Suryati HusinNo ratings yet
- 1 s2.0 S0264410X21016157 MainDocument10 pages1 s2.0 S0264410X21016157 MainJavier Cabrera PérezNo ratings yet
- Multidrug-Resistant Bacterial Infections in U.S. Hospitalized Patients, 2012-2017Document11 pagesMultidrug-Resistant Bacterial Infections in U.S. Hospitalized Patients, 2012-2017sebastianNo ratings yet
- Immunità Naturale Vs Vaccini PDFDocument7 pagesImmunità Naturale Vs Vaccini PDFmakajeNo ratings yet
- COVID-19 Vaccination Efficacy and Safety Literature Review: ArticleDocument19 pagesCOVID-19 Vaccination Efficacy and Safety Literature Review: ArticlePromiseNo ratings yet
- Antibiotics 11 00022Document16 pagesAntibiotics 11 00022Putri RamadhaniNo ratings yet
- Published Leveraging Innovative Vaccines in Conquering Emerging Infectious DiseaseDocument36 pagesPublished Leveraging Innovative Vaccines in Conquering Emerging Infectious Diseaseঅসীম সীমান্তNo ratings yet
- Artikel VaksinDocument9 pagesArtikel VaksinrajyurafNo ratings yet
- Fmicb 15 1385834Document11 pagesFmicb 15 1385834An iNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundRey John MonjeNo ratings yet
- 1 s2.0 S1473309921004606 MainDocument13 pages1 s2.0 S1473309921004606 MainLOPEZ BARAJAS GABRIELNo ratings yet
- Influence of A COVID-19 Vaccine's Effectiveness and Safety Profile On Vaccination AcceptanceDocument5 pagesInfluence of A COVID-19 Vaccine's Effectiveness and Safety Profile On Vaccination AcceptanceHafizh ShidqiNo ratings yet
- Nejmoa 2110475Document14 pagesNejmoa 2110475Luis Ricardo Vejar FelixNo ratings yet
- Ipt 4Document10 pagesIpt 4PPDS ANAK FK USUNo ratings yet
- 1 s2.0 S1473309922008118 MainDocument13 pages1 s2.0 S1473309922008118 MaindaniaNo ratings yet
- Conduct Hearing of Dr. Morgan OsborneDocument10 pagesConduct Hearing of Dr. Morgan OsborneCTV CalgaryNo ratings yet
- EMS Data On Unfilled ShiftsDocument1 pageEMS Data On Unfilled ShiftsCTV CalgaryNo ratings yet
- Allegations Involving Premier Danielle Smith May 17 2023Document17 pagesAllegations Involving Premier Danielle Smith May 17 2023edmontonjournalNo ratings yet
- Funding Breakdown For Operational Funding For Alberta Post-Secondary Schools, 2023Document2 pagesFunding Breakdown For Operational Funding For Alberta Post-Secondary Schools, 2023CTV CalgaryNo ratings yet
- Decriminalization: A Proposed Theory of Change For Improved Community Safety and Wellbeing OutcomesDocument32 pagesDecriminalization: A Proposed Theory of Change For Improved Community Safety and Wellbeing OutcomesCTV CalgaryNo ratings yet
- Letter To CBC - April 2, 2023Document3 pagesLetter To CBC - April 2, 2023CTV CalgaryNo ratings yet
- YYC Arena May 1 2023Document9 pagesYYC Arena May 1 2023CTV CalgaryNo ratings yet
- Angus Reid Premiers Approval RatingsDocument10 pagesAngus Reid Premiers Approval RatingsCTV CalgaryNo ratings yet
- ThinkHQ: Concerns About Crime On The Rise in CalgaryDocument15 pagesThinkHQ: Concerns About Crime On The Rise in CalgaryCTV CalgaryNo ratings yet
- Rail Transportation Safety Investigation Report R21C0070Document7 pagesRail Transportation Safety Investigation Report R21C0070CTV CalgaryNo ratings yet
- CM V Alberta 2022 ABKB 716 DecisionDocument28 pagesCM V Alberta 2022 ABKB 716 DecisionCTV CalgaryNo ratings yet
- Ot 1Document29 pagesOt 1CTV CalgaryNo ratings yet
- Stephens DecisionDocument9 pagesStephens DecisionCTV CalgaryNo ratings yet
- Calgary City Council 1-Year Report Card 2022Document17 pagesCalgary City Council 1-Year Report Card 2022CTV CalgaryNo ratings yet
- SGS FTIR Testing Report Calgary Coop BagsDocument5 pagesSGS FTIR Testing Report Calgary Coop BagsCTV CalgaryNo ratings yet
- Protection Status, Human Disturbance, Snow Cover and Trapping Drive Density of A Declining Wolverine Population in The Canadian Rocky MountainsDocument15 pagesProtection Status, Human Disturbance, Snow Cover and Trapping Drive Density of A Declining Wolverine Population in The Canadian Rocky MountainsCTV CalgaryNo ratings yet
- Fish Creek Provincial Park Coyote AttackDocument1 pageFish Creek Provincial Park Coyote AttackCTV CalgaryNo ratings yet
- Decision of The Hearing Tribunal of The College of Physicians & Surgeons of AlbertaDocument11 pagesDecision of The Hearing Tribunal of The College of Physicians & Surgeons of AlbertaCTV CalgaryNo ratings yet
- Alberta Securities Commission Decision Citation: Re Breitkreutz, 2019 ABASC 38 Date: 20190221Document24 pagesAlberta Securities Commission Decision Citation: Re Breitkreutz, 2019 ABASC 38 Date: 20190221CTV CalgaryNo ratings yet
- Jonathan Denis Contempt DecisionDocument10 pagesJonathan Denis Contempt DecisionCTV CalgaryNo ratings yet
- Judge Decision April 2022 Court Challenge Hinshaw QuestionsDocument7 pagesJudge Decision April 2022 Court Challenge Hinshaw QuestionsCTV CalgaryNo ratings yet
- AHS Closure Order For PurrTeaDocument9 pagesAHS Closure Order For PurrTeaCTV CalgaryNo ratings yet
- TBF Superintendent of Insurance Annual Report 2020Document36 pagesTBF Superintendent of Insurance Annual Report 2020CTV CalgaryNo ratings yet
- DBRS AlbertaDocument6 pagesDBRS AlbertaCTV CalgaryNo ratings yet
- 2021 SBOR Police Commission PresentationDocument19 pages2021 SBOR Police Commission PresentationCTV CalgaryNo ratings yet
- CPSA Hearing Tribunal Decision - Dr. Gaylord WardellDocument27 pagesCPSA Hearing Tribunal Decision - Dr. Gaylord WardellCTV CalgaryNo ratings yet
- CPSA Tribunal Finding For Dr. Peter IdahosaDocument23 pagesCPSA Tribunal Finding For Dr. Peter IdahosaCTV CalgaryNo ratings yet
- TRB V KWPB 2021 ABQB 997 Memorandum of DecisionDocument9 pagesTRB V KWPB 2021 ABQB 997 Memorandum of DecisionCTV CalgaryNo ratings yet
- ASIRT Investigation Into Calgary Police Officers Use of Force and Evidence at TrialDocument31 pagesASIRT Investigation Into Calgary Police Officers Use of Force and Evidence at TrialCTV Calgary100% (2)
- Indain Ethos and Business EthicsDocument40 pagesIndain Ethos and Business EthicsavdhutpatilkingNo ratings yet
- MAT 2101 Complex Variables, Laplace and Z Transform COURSE OUTLINE Fall 23-24Document7 pagesMAT 2101 Complex Variables, Laplace and Z Transform COURSE OUTLINE Fall 23-24jop23343No ratings yet
- JurnalDocument12 pagesJurnalsya viraNo ratings yet
- What Do You Know About ROSHNDocument5 pagesWhat Do You Know About ROSHNSARAHNo ratings yet
- Assessment of Financial Performance of Public Transportation The Case of Public Transportation EnterpriseDocument57 pagesAssessment of Financial Performance of Public Transportation The Case of Public Transportation EnterpriseFasilNo ratings yet
- CH 3Document12 pagesCH 3Lleuan Masong0% (1)
- Factors Affecting Female Consumer'S Online Buying BehaviorDocument21 pagesFactors Affecting Female Consumer'S Online Buying BehaviorAmruta VadnerkarNo ratings yet
- Diss Lesson 4 SocioDocument55 pagesDiss Lesson 4 Sociojocelyn de castroNo ratings yet
- Q4 Module 1-Distinguishing Technical Terms in ResearchDocument48 pagesQ4 Module 1-Distinguishing Technical Terms in ResearchJayr GiananNo ratings yet
- NITRA Technical CampusDocument27 pagesNITRA Technical CampusNitraNtcNo ratings yet
- What Is Computational Design?Document19 pagesWhat Is Computational Design?Douglas Lopes de SouzaNo ratings yet
- Flipped Classroom Lesson Plan TemplateDocument2 pagesFlipped Classroom Lesson Plan Templateapi-351598518No ratings yet
- Cosmetic Product Usage and Self Confidence of The Selected Grade 12 StudentsDocument12 pagesCosmetic Product Usage and Self Confidence of The Selected Grade 12 StudentsArci Oneles100% (3)
- My Dissertation Report On AirtelDocument35 pagesMy Dissertation Report On AirtelRohan Chakrabarti100% (1)
- A New Method For The Synthesis of Aliphatic Nitro Compounds1, 2Document5 pagesA New Method For The Synthesis of Aliphatic Nitro Compounds1, 2banjo01No ratings yet
- Project FormsDocument3 pagesProject FormsJagan RajNo ratings yet
- Quiz 3 (HRM 415, Sec - 1)Document2 pagesQuiz 3 (HRM 415, Sec - 1)Mohammad RoyelNo ratings yet
- COSTILLAS Raffy Tulfo in Action Viewership PDFDocument10 pagesCOSTILLAS Raffy Tulfo in Action Viewership PDFMay MayNo ratings yet
- Human Resource Management 4: Fundamentals ofDocument15 pagesHuman Resource Management 4: Fundamentals ofLoiweza AbagaNo ratings yet
- Research Proposal - Is Social Exclusion Worse For WomenDocument14 pagesResearch Proposal - Is Social Exclusion Worse For WomenKovcs EszterNo ratings yet
- Volume IDocument68 pagesVolume ICharleneKronstedtNo ratings yet
- Ansys DFR Mil HDBK 217Document8 pagesAnsys DFR Mil HDBK 217luze YuNo ratings yet
- Research DesignDocument4 pagesResearch DesignAbdul BasitNo ratings yet
- Arts and Humanities PDFDocument26 pagesArts and Humanities PDFAashiq GokulNo ratings yet
- Capstone Research Project Research Proposal Rubric: Most Two Perspectives That AreDocument3 pagesCapstone Research Project Research Proposal Rubric: Most Two Perspectives That AreAliah LingbawanNo ratings yet
- Rajiv Gandhi University of Health Sciences Karnataka, BangaloreDocument10 pagesRajiv Gandhi University of Health Sciences Karnataka, Bangaloreshivangi YaduvanshiNo ratings yet
- Call For Papers: Special Issue On The Contributions of Qualitative Methods To Intervention ResearchDocument1 pageCall For Papers: Special Issue On The Contributions of Qualitative Methods To Intervention ResearchJane GilgunNo ratings yet
- 2007ccj Research EssayDocument10 pages2007ccj Research EssayGeorgie FriedrichsNo ratings yet