Professional Documents
Culture Documents
Day 4 Lecture - GI and Nutrition
Day 4 Lecture - GI and Nutrition
Uploaded by
Remej Silutgam0 ratings0% found this document useful (0 votes)
63 views113 pagesAn ERCP (endoscopic retrograde cholangiopancreatography) uses an endoscope to visualize the biliary and pancreatic ducts. It can be used to identify stones, strictures, cysts, or tumors. The endoscope is inserted and dye is injected to outline the ducts. Risks include perforation, infection, pancreatitis, or aspiration. It is contraindicated in patients who are uncooperative, have had upper GI surgery, have esophageal diverticula, or acute pancreatitis.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAn ERCP (endoscopic retrograde cholangiopancreatography) uses an endoscope to visualize the biliary and pancreatic ducts. It can be used to identify stones, strictures, cysts, or tumors. The endoscope is inserted and dye is injected to outline the ducts. Risks include perforation, infection, pancreatitis, or aspiration. It is contraindicated in patients who are uncooperative, have had upper GI surgery, have esophageal diverticula, or acute pancreatitis.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
63 views113 pagesDay 4 Lecture - GI and Nutrition
Day 4 Lecture - GI and Nutrition
Uploaded by
Remej SilutgamAn ERCP (endoscopic retrograde cholangiopancreatography) uses an endoscope to visualize the biliary and pancreatic ducts. It can be used to identify stones, strictures, cysts, or tumors. The endoscope is inserted and dye is injected to outline the ducts. Risks include perforation, infection, pancreatitis, or aspiration. It is contraindicated in patients who are uncooperative, have had upper GI surgery, have esophageal diverticula, or acute pancreatitis.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 113
▪ Is the direct visualization of the GI system by means of
a lighted, flexible tube.
▪ It is more accurate than radiologic examination
because sources of bleeding, surface lesions, or
healing tissues can be directly observed.
▪ Upper GI tract endoscopy includes esophagoscopy,
gastroscopy and esophagogastroduodenoscopy.
▪ Written consent should be obtain prior to the
procedure.
▪ An esophagogastroduodenoscopy (also called
EGD or upper endoscopy) is a procedure that
allows the doctor to examine the inside of the
esophagus, stomach, and duodenum.
▪ A thin, flexible, lighted tube, called an endoscope,
is guided into the mouth and throat, then into the
esophagus, stomach, and duodenum.
▪ Other names: Upper gastrointestinal [UGI]
endoscopy, Gastroscopy)
▪ Acute or chronic GI bleeding
▪ Pernicious anemia
▪ Esophageal injury, masses, strictures
▪ Dysphagia
▪ Substernal pain
▪ Epigastric discomfort
▪ Inflammatory bowel disease
▪ Conscious sedation with sedative, opioid
(narcotics) or tranquilizers may be given before or
during the procedure
▪ Anticholinergic (AtSO4) medications may be given
to decrease oropharyngeal secretions and prevent
reflex bradycardia.
▪ When client is sedated, a local anesthetic is sprayed
on the posterior pharynx to ease discomfort and
prevent gagging (depress gag reflex) during
insertion of endoscope.
▪ Instruction: Do not swallow saliva.
▪ Left lateral decubitus (sims lateral) position – to allow
saliva to drain from side of the mouth and reduce risk of
aspiration.
▪ Flexible fiberoptic tube – passed orally into the
esophagus, stomach, pylorus and duodenum. Some
endoscopes are equipped with a camera that allows to
obtain color photographs.
▪ If cancer is suspected, cells or tissue can be collected for
cytologic exam.
▪ Small, single polyps may be removed.
▪ With upper GI endoscopy, one can also visualize and
perform a biopsy of tissue in most of the small intestinal
tract. This procedure is referred to as enteroscopy.
▪ Abnormalities of the small intestine such as
arteriovenous (AV) malformations, tumors,
enteropathies (e.g., celiac disease), and ulcerations
can be diagnosed with enteroscopy.
▪ Monitor for cardiac and respiratory complications
▪ Assess the client’s heart rate, blood pressure, respiratory
rate and pulse oximetry frequently.
▪ Specific antagonists to benzodiazepines and opioids
should be available for emergency reversal of drug
effects. (ex. Flumanzil, Naltexone, Naloxone)
▪ Upper GI endoscopy should not be performed in clients
with severe cardiovascular disease.
▪ Obtain signed written consent
▪ If client is going home within 24 hours after the
procedure, someone should be available to drive.
▪ For clients with history of cardiac valve disease or
replacement, antibiotic prophylaxis may be required.
▪ NPO for 8 to 12 hours – to prevent aspiration of stomach
contents to the lungs
▪ Assess oral cavity and report any loose teeth or lesions to
the gastroenterologists
▪ Remove dentures and any removable bridges.
▪ Client my experience discomfort, nausea or pressure.
Tell the client to breathe through the nose during the
procedure.
▪ Explain that the room will be cool and dark and pt will
not be able to talk while the endoscope is in place.
▪ For capsule endoscopy, instruct the patient to return to
the physician’s office in 6 to 10 hours to return the
recording device and have all recording wires removed.
▪ For capsule endoscopy, instruct the patient that he or she
can continue regular activities throughout the
examination and will not feel any sensations resulting
from the capsule’s passage.
▪ Place patient in Sims position (side lying) – until
sedation and local anesthesia wear off. To prevent
aspiration.
▪ Withhold fluids and solids (NPO) for 2 – 4 hours until the
gag reflex returns. Test for return of gag reflex by
stroking the back of the throat with a tongue blade.
▪ Once gag returns the doctor may order anesthetic
throat lozenges or normal saline gargles to ease throat
irritation or hoarseness.
▪ Monitor for bradycardia or other dysrhythmias – result of
sedatives or anesthesia
▪ Assess for signs for esophageal or gastric perforation
▪ Esophageal perforation – may cause crepitus (crackling) in
the neck (from air leakage), fever, bleeding, or pain. Neck
and throat pain, aggravated by swallowing or moving, may
also occur.
▪ Midesophageal perforation results in referred substernal or
epigastric pain.
▪ Distal esophageal perforation results in shoulder pain,
dyspnea or manifestations similar to those of perforated
ulcers.
▪ If you suspect perforation, an x-ray study should be
obtained to confirm the presence of free air.
▪ For capsule endoscopy, instruct the patient that there is
no need to retrieve the capsule or camera from the stool.
▪ Or also known as wireless capsule endoscopy
▪ uses a capsule containing a miniature camera that records
images of the entire digestive tract, particularly the small
intestine
▪ The most common reason for doing capsule endoscopy is
to search for a cause of bleeding from the small
intestine. It may also be useful for detecting polyps,
inflammatory bowel disease (Crohn disease) ulcers,
and tumors of the small intestine.
▪ With fiberoptic colonoscopy, the entire colon from
anus to cecum (and often a portion of terminal ileum)
can be examined in most patients.
▪ Anoscopy refers to examination of the anus;
▪ Proctoscopy to examination of the anus and rectum;
and
▪ Sigmoidoscopy to examination of the anus, rectum,
and sigmoid colon. Sigmoidoscopy can be performed
with a rigid (≤ 25 cm from the anus) or flexible (≤ 60
cm from the anus) sigmoidoscope.
▪ Colonoscopies are performed by a physician trained
in GI endoscopy in approximately 30 to 60 minutes.
the patient is sedated, he or she experiences very
little discomfort and may not have recall of the
procedure.
▪ Sigmoidoscopies are performed in about 20 minutes.
Sedation is not required. Patients may feel discomfort
and the urge to defecate as the scope is inserted.
▪ Is the visual examination of the lining of the entire colon
with a flexible fiberoptic endoscope.
▪ It is indicated for clients with history of constipation
and diarrhea, persistent rectal bleeding, or lower
abdominal pain when results of proctosigmoidoscopy
and a barium enema are negative or inconclusive.
▪ Use to screen clients at high risk for colon cancer.
▪ Colonoscopy every 10 years is recommended for
persons 50 years of age or older at average risk for
colorectal cancer.
▪ Sedation and placed pt on the left side, knees
flexed.
▪ After the colonoscope is inserted through the anus, a
small amount of air is insufflated to locate the bowel
lumen
▪ The scope is advanced through the rectum into the
sigmoid colon under the direct visualization.
▪ When instrument reaches the descending sigmoid
junction, the client may be assisted to the supine
position to aid the scope’s advance past the splenic
flexure.
▪ After scope has passed the splenic flexure, it is
advanced through the transverse colon and past the
hepatic flexure in the ascending colon and cecum.
▪ Abdominal palpation or fluoroscopy may help to
guide the colonoscope through the large intestine.
▪ Observe the client closely for manifestations of bowel
perforation (malaise, rectal bleeding, abdominal pain,
and distention, fever and mucopurulent drainage)
▪ Monitor vital signs as order until they are stable. (note
for vasovagal response, e.g. bradycardia,
hypotension)
▪ Assess for signs and symptoms of perforation.
▪ Observe the client closely for manifestations of bowel
perforation (malaise, rectal bleeding, abdominal pain,
and distention, fever and mucopurulent drainage)
▪ Monitor vital signs as order until they are stable. (note
for vasovagal response, e.g. bradycardia,
hypotension)
▪ Assess for signs and symptoms of perforation.
▪ A double-balloon enteroscopy, also known as a push-
and-pull endoscopy, is an endoscopic technique used
to visualize the entire gastrointestinal tract. It is
used to help in the diagnosis of a variety of digestive
disorders.
▪ The overtube balloon is then deployed, and the
enteroscope balloon is deflated. The process
continues until the entire small bowel is visible. The
procedure typically takes about two hours.
▪ Give detailed preparation instructions.
▪ Double balloon enteroscopy may be done anterograde
(through the mouth) or retrograde (through the anus).
▪ Preparation may also include stopping certain
medications like blood thinners, diabetes medications
or iron supplements.
▪ UGI: through esophagus, LGI: through anus
▪ When done through the mouth it requires a period of
being on a liquid diet and then fasting.
▪ When done through the anus it requires drinking a
bowel cleanser to completely evacuate the bowels –
just like for a colonoscopy.
▪ Uses fiberoptic endoscope that provides
radiographic visualization of the biliary and
pancreatic ducts
▪ This is especially useful in patients with jaundice.
▪ Stones, benign strictures, cysts, ampullary stenosis,
anatomic variations, and malignant tumors can be
identified.
▪ • Patients who are uncooperative. Cannulation of the
ampulla of Vater requires that the patient lie very still.
▪ • Patients whose ampulla of Vater is not accessible
endoscopically because of previous upper
gastrointestinal (GI) surgery
▪ • Patients with esophageal diverticula. The scope can
fall into a diverticulum and perforate its wall.
▪ • Patients with known acute pancreatitis
▪ Perforation of the esophagus, stomach, or duodenum
▪ Gram-negative sepsis. This results from introducing
bacteria through the biliary system and into the
blood.
▪ Pancreatitis resulting from pressure of the dye
injection
▪ Aspiration of gastric contents into the lungs
▪ Respiratory arrest as a result of oversedation
▪ Explain the procedure to the patient. See p. xviii for
radiation exposure and risks.
▪ Obtain informed consent from the patient.
▪ Inform the patient that breathing will not be
compromised by the insertion of the endoscope.
▪ Keep the patient NPO as of midnight the day of the
test.
▪ Administer appropriate premedication if ordered.
▪ Note the following procedural steps:
▪ 1. A flat plate of the abdomen is taken to ensure that any
barium from previous studies will not obscure
visualization of the bile duct.
▪ 2. The patient is positioned supine or on the left side.
▪ 3. The patient is usually sedated with a narcotic and a
sedative–hypnotic.
▪ 4. The pharynx is sprayed with a local anesthetic to
inactivate the gag reflex and to lessen the discomfort.
▪ 5. A fiberoptic duodenoscope is inserted through the oral
pharynx and passed through the esophagus and stomach
and then into the duodenum
▪ Glucagon is often administered intravenously to
minimize the spasm of the duodenum and to improve
visualization of the ampulla of Vater.
▪ 7. Through the accessory lumen within the scope, a
small catheter is passed through the ampulla of Vater
and into the common bile or pancreatic ducts.
▪ 8. Radiographic dye is injected, and x-ray images are
taken.
▪ Glucagon is often administered intravenously to
minimize the spasm of the duodenum and to improve
visualization of the ampulla of Vater.
▪ 7. Through the accessory lumen within the scope, a
small catheter is passed through the ampulla of Vater
and into the common bile or pancreatic ducts.
▪ 8. Radiographic dye is injected, and x-ray images are
taken.
▪ Note that the test usually takes approximately 1 hour
and is performed by a physician trained in endoscopy.
The x-ray images are interpreted by a radiologist.
▪ Tell the patient that no discomfort is associated with
the dye injection but that minimal gagging may occur
during the initial introduction of the scope into the oral
pharynx.
▪ Do not allow the patient to eat or drink until the gag
reflex returns. Encourage light eating for the next 12 to
24 hours.
▪ Observe the patient closely for development of
abdominal pain, nausea, and vomiting. This may herald
the onset of ERCP-induced pancreatitis or
gastroduodenal perforation.
▪ Observe safety precautions until the effects of the
sedatives have worn off.
▪ Monitor the patient for signs of respiratory depression.
▪ Medication (e.g., naloxone) should be available to
counteract serious respiratory depression.
▪ Assess the patient for signs and symptoms of
septicemia, which may indicate the onset of ERCP-
induced cholangitis.
▪ Inform the patient that he or she may be hoarse and
have a sore throat for several days. Drinking cool fluids
and gargling will help relieve some of this soreness.
▪ Instruct the patient to notify the physician immediately
of fever or shaking chills. This may indicate possible
cholangitis.
▪ a minimally invasive procedure to assess diseases of
the digestive (gastrointestinal) tract and other nearby
organs and tissues. Endoscopic ultrasound combines
the use of a thin, flexible tube (endoscope) inserted
into the gastrointestinal tract and a device that uses
sound waves to create images (ultrasound).
▪ An endoscopic tube may also have a small needle to
remove fluid or tissue samples (biopsy) for
examination in a lab. This procedure is called EUS-
guided fine-needle aspiration or EUS-guided fine-
needle biopsy.
▪ Internal organs or nearby structures can also be
visualized, including the following:
▪ Lungs
▪ Lymph nodes in the center of the chest
▪ Liver
▪ Gall bladder
▪ Bile ducts
▪ Pancreas
▪ Assess damage to tissues due to inflammation or disease
▪ Determine whether cancer is present or has spread to
lymph nodes
▪ Assess how much a cancerous (malignant) tumor invades
tissues
▪ Determine how advanced cancer is
▪ Provide more-detailed information about lesions
identified with other imaging technologies
▪ Extract fluid or tissue for diagnostic testing
▪ Drain fluids from cysts
▪ Deliver therapies to a targeted region, such as a malignant
tumor
▪ Bleeding
▪ Infection
▪ Tearing (perforation) of an organ wall
▪ Pancreatitis, if fine-needle aspiration of the pancreas is
done
▪ Fasting. (6 hrs) before the test to ensure your stomach is
empty.
▪ Colon cleansing. A colon cleansing solution or to follow a
liquid diet and use a laxative before the procedure.
▪ Medication. Tell your doctor about all prescription and
nonprescription medications you take, as well as herbal
remedies and dietary supplements.
▪ Travel. Medication to help you relax or sleep (sedative) or
anesthesia can impair your coordination and judgment
after the procedure. Arrange for someone to drive you
home and stay with you the rest of the day.
▪ Fasting. (6 hrs) before the test to ensure your stomach is
empty.
▪ Colon cleansing. A colon cleansing solution or to follow a
liquid diet and use a laxative before the procedure.
▪ Medication. Tell your doctor about all prescription and
nonprescription medications you take, as well as herbal
remedies and dietary supplements.
▪ Travel. Medication to help you relax or sleep (sedative) or
anesthesia can impair your coordination and judgment
after the procedure. Arrange for someone to drive you
home and stay with you the rest of the day.
▪ safe, simple, and valuable method of diagnosing
pathologic liver conditions. For this study, a specially
designed needle is inserted through the abdominal
wall and into the liver.
▪ A piece of liver tissue is removed for microscopic
examination. Percutaneous liver biopsy is used in the
diagnosis of various liver disorders (e.g., cirrhosis,
hepatitis, drug reaction, granuloma, and tumor).
▪ Biopsy is indicated for the following:
▪ Patients with unexplained hepatomegaly
▪ Patients with persistently elevated liver enzymes
▪ Patients with suspected primary or metastatic tumor
▪ Patients with unexplained jaundice
▪ Patients with suspected hepatitis
▪ Patients with suspected infiltrative diseases
▪ The biopsy may be performed by a blind stick or
directed with the use of computed tomography (CT),
magnetic resonance imaging (MRI), or ultrasound.
▪ Explain the procedure to the patient. Many patients are
apprehensive about it.
▪ Obtain informed consent.
▪ Ensure that all coagulation tests are normal.
▪ Instruct the patient to keep NPO after midnight on the
day of the test.
▪ Administer any sedative medications as ordered.
▪ 1. The patient is placed in the supine or left lateral
position.
▪ 2. The skin area used for puncture is anesthetized locally.
▪ 3. The patient is asked to exhale and hold the exhalation.
This causes the liver to descend and reduces the
possibility of a pneumothorax.
▪ 4. During the patient’s sustained exhalation, the physician
rapidly introduces the biopsy needle into the liver and
obtains liver tissue. Occasionally, the biopsy needle is
inserted under CT guidance. This is especially useful
when tissue from a specific area of the liver is needed.
▪ 5. The needle is withdrawn from the liver.
▪ Note that this test is performed by a physician in
approximately 15 minutes.
▪ Inform the patient that he or she may have minor
discomfort during injection of the local anesthetic and
needle insertion.
▪ Place the tissue sample into a specimen bottle
containing formalin and send it to the pathology
department.
▪ Apply a small dressing over the needle insertion site.
▪ Place the patient on his or her right side for
approximately 1 to 2 hours. In this position, the liver
capsule is compressed against the chest wall, thereby
decreasing the risk of hemorrhage or bile leak.
▪ Assess the patient’s vital signs frequently for evidence
of hemorrhage and peritonitis.
▪ Evaluate the rate, rhythm, and depth of respirations.
Report chest pain and signs of dyspnea, cyanosis, and
restlessness, which may be indicative of
pneumothorax.
▪ Tell the patient to avoid coughing or straining, which
may cause increased intraabdominal pressure.
▪ also known as a diagnostic laparoscopy, is a surgical
diagnostic procedure used to examine the organs
inside the abdomen, as well as other closed spaces,
such as the knees. It’s a low risk, minimally invasive
procedure that requires only small incisions.
▪ When an abdominal laparoscopy is performed, a
doctor uses an instrument called a laparoscope to
look at the abdominal organs.
▪ A laparoscope is a long, thin tube with a high intensity
light and a high resolution camera at the front. The
instrument is inserted through an incision in the
abdominal wall. As it moves along, the camera sends
images to a video monitor.
▪ A laparoscopy allows your doctor to see inside your
body in real time, without having to make large
incisions. Your doctor can also obtain biopsy samples
during this procedure, as well as also perform surgery.
▪ Inform physician about any prescription or over-the-
counter medications you’re taking.
▪ Physician may change the dose of any medications that
could affect the outcome of a laparoscopy. These drugs
include:
▪ anticoagulants, such as blood thinners
▪ nonsteroidal anti-inflammatory drugs (NSAIDs), including
aspirin (Bufferin) or ibuprofen (Advil, Motrin IB)
▪ other medications that affect blood clotting
▪ herbal or dietary supplements
▪ vitamin K
▪ NPO 8 hours before a laparoscopy.
▪ Developed by George Papanicolaou, a study of
cells that have sloughed off from a tissue.
▪ Performed to distinguish benign from malignant
lesions.
▪ Detect malignant cells
▪ Malignant cells exfoliate more readily than normal
cells.
▪ Specific areas of the GI tract are lavaged, and cells
are collected and sent to the laboratory for analysis.
▪ Cells of the esophagus, stomach, small intestine and
colon can be examined.
▪ Stomach contents are examined for the presence of
Helicobacter pylori, a bacterium that can cause
gastritis and peptic ulcer disease.
▪ UGI: NGT Insertion, LGI: Laxative/Enema
▪ In this procedure, a nasogastric tube is placed
and cells are obtained by saline lavage through
the tube (proctoscope).
▪ Explain the procedure to the client and, if required,
obtain written consent.
▪ NPO before the procedure
▪ Afterward, the client rests and may resume
eating/diet.
▪ Is performed to measure secretions of
hydrochloric acid (HCl) and pepsin in the
stomach.
▪ Analysis of gastric contents can aid in the diagnosis
of duodenal ulcer, Zollinger-Ellison syndrome,
gastric carcinoma and pernicious anemia.
▪ Gastric analysis consists of (1) the basal cell
secretion test and (2) the gastric acid
stimulation test.
▪ Basal cell secretion test:
▪ A nasogastric tube is inserted and attached to the
suction. Stomach contents are collected every 15
minutes for 1 hour.
▪ Label specimens carefully with time, volume and
client identification.
▪ The specimens are analyzed. If abnormal gastric
secretion is suggested, a gastric acid stimulation
test is performed.
▪ Gastric acid stimulation test
▪ The test measures the amount of gastric acid for 1 hour after
subcutaneous injection of a drug that stimulate its secretion
(pentagastrin and betazole).
▪ If results are abnormal, radiographic studies or endoscopy
may be done to determine the cause.
▪ A markedly increased level of gastric secretion may
indicate Zollinger-Ellison syndrome, whereas a
moderately increased level suggests a duodenal ulcer.
▪ Decreased levels of gastric secretion may indicate gastric
ulcer or carcinoma.
▪ NPO for 12 hours before the test.
▪ Insert a nasogastric tube, and remove any contents
left in the stomach.
▪ Do not administer drugs that interfere with gastric
acid levels, such as cholinergics, histamine
blockers or antacids.
▪ If client requires, coronary vasodilator therapy,
change the oral form to an ointment or sublingual
preparation during the procedure.
▪ If the nasogastric is left in place, attach it to low
intermittent suction.
▪ Record the amount and color of the drainage.
▪ Also known as the Bernstein Test
▪ Determines whether a client’s chest pain is related
to acid perfusion across the esophageal mucosa.
▪ A nasogastric tube is inserted and gastric contents are
aspirated.
▪ NSS (0.9%) and 0.1% HCL are alternately instilled into
the lower esophagus.
▪ If the client does not experience pain, the test is
considered normal.
▪ If pain occurs, normal saline is administered until pain
ceases. To ensure that the pain is cause by acid
perfusion, 0.1% HCl is readministered.
▪ After the test, the nasogastric tube is withdrawn.
▪ Keep the client NPO the night before the test.
▪ Instruction about the procedure includes preparing
the client for insertion of the nasogastric tube
▪ After the procedure the client may receive an
antacid.
▪ Is used to assess esophageal motor function and
can be used to assess and diagnose dysphagia,
esophageal reflux, spasm, motility disorders
and hiatal hernia.
▪ A special enteric tube with fused small-caliber
catheter is inserted into the esophagus.
▪ The tube is designed to measure simultaneous
pressures of the esophagus and lower esophageal
sphincter by infusion of water into the catheters.
▪ The client is asked to swallow small amounts of
water, and the esophageal pressures are recorded
during the muscular relaxation and contraction.
▪ Instruct the client about the procedure and maintain
the client in an NPO status – 6 to 8 hours before the
procedure.
▪ The test takes about 15 – 20 minutes.
▪ After the test , remove the enteric tube.
▪ The physician may recommend medications or diet
alterations based on the results.
▪ Is used to distinguish chest pain caused by gastric
acid reflux from chest pain caused by angina or
myocardial infarction.
▪ Location of the lower esophageal sphincter (LES)
is determined by esophageal manometry and a
nasoenteric tube with a pH sensor is inserted 5 cm
above the LES.
▪ The enteric tube is secured to the client’s face and
attached to a battery-operated recorder.
▪ The client is then instructed to push a button on the
recorded at the start and end of specific activities,
such as eating, sleeping, and smoking.
▪ Tell the client to note when chest pain or
indigestion starts and ends.
▪ Because the location of the LES must be
determined, inform the client that esophageal
manometry may be performed first after which a
second enteric tube may be placed for pH
monitoring.
▪ You may need to stop giving the client drugs that
affect the GI tract (H2 histamine blockers and
motility drugs) before the procedure.
▪ Instruct the client about the importance of
recording activities and manifestations.
▪ The tube must remain securely taped.
▪ Tell the client to avoid bumping or pulling the tube
when dressing or during face washing.
▪ After the procedure remove the tube and advise the
client that normal activities may be resumed.
▪ Iron deficiency anemia is the most common cause
of anemia.
▪ Normal hematologic function requires adequate
intake, absorption, use and storage of nutrients,
such as protein, vitamin B12, and copper.
▪ Assessment of red blood cell function and iron
stores is crucial to nutritional assessment.
▪ Are important for maintain intravascular oncotic
pressure and as carrier molecules.
▪ Serum proteins include:
❖Albumin
❖Prealbumin
❖Retinol-binding protein
❖Transferrin
▪ Requires venous blood sample in a fasting or
nonfasting state.
▪ Serum protein with long half lives (albumin) tend to
be the global indicators of nutritional status and
serum proteins with shorter half-lives (prealbumin
and transferrin) suggest acute changes in
nutritional status.
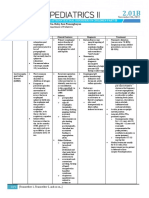
Protein Normal range Half-life Effect of associated conditions
Albumin 3.5 – 5 g/dl 14-20 days Increased with dehydration
Decreased with malnutrition,
overhydration, trauma, protein loss,
liver disease
Prealbumin 20 – 40 mg/dl 3-5 days Increased with nutrition intake and
renal failure
Decreased with poor dietary intake
Retinol- 3 – 6 mg/L 8-12 hours Decreased with overhydration, liver
binding distress, zinc and vitamin A deficit
protein
Transferrin 200-400 mg/dl 8-10 hours Increased with pregnancy, iron
deficiency
Decreased with chronic infection,
cirrhosis
▪ Immune function and nutritional status are closely
related.
▪ Total lymphocyte count (TLC), an indicator of immune
function, provides a gross measure of nutritional status.
▪ To determine TLC, obtain a white blood cell (WBC)
count with differential from the venous blood sample.
▪ Next, multiple the percentage of lymphocytes by the
total WBC count.
▪ Ex: a client with WBC count of 7000/mm³ and 30%
lymphocytes has a TLC of 2100/ mm³
▪TLCs less than 1800/mm³ suggest malnutrition
▪ Because TLC is a gross indicator of immune
function and nutritional states, normally nourished
clients may have a low TLC after a chemotherapy.
▪ Alternatively, an elevated TLC may be found in
malnourished clients with sepsis.
▪ D-Xylose a monosaccharide, is absorbed in the
small intestine and is used to assess/diagnose
malabsorption.
▪ NPO for 10 – 12 hours before the test
▪ Blood sample and first voided morning urine
specimen are collected.
▪ After oral administration of a known quantity of D-
xylose mixed in water, blood and urine levels of
D-xylose are measured.
▪Blood is drawn 2 hours after D-xylose is
given and all urine is collected for a specified
time.
▪Instruct client to remain in bed during the
test because activity alters results.
▪Decreased values of absorbed D-xylose in
blood and urine indicate possible
malabsorption in the small intestine.
▪a measure of one’s anabolic or catabolic state.
▪To determine nitrogen balance,
simultaneously record the amount and type of
food consumed in a 24-hour period and
obtain a 24-hour urine collection.
▪The start and stop time for the food intake
record and the 24 hour urine collection must
be the same.
▪Instruct the client about the procedure and
the importance of recording all food intake
and saving all urine for 24 hours.
▪The 24-hour urine collection begins with
discarding the first voided specimen, then
collecting all urine for the next 24 hours in an
iced, preservative-free container.
▪ After completing the 24-hour urine collection,
send the urine to the laboratory for measurement
of the urine urea nitrogen (UUN).
▪ Urine creatinine, sodium and potassium may be
measured to determine the adequacy of the urine
collection.
▪ Collection registered dietitian to calculate 24-hour
protein intake
▪ If the client received tube feedings or parenteral
nutrition during the 24-hout test period, the
amount of protein from these sources must be
included in the calculation.
▪ Protein is approximately 16% nitrogen.
▪ To determine the amount of nitrogen consumed
over the 24 hours, multiply the amount of protein
consumed (in grams) by 0.16.
▪ UUN is the major source of nitrogen excretion.
▪ Subtract the UUN (in grams) from the amount of
nitrogen consumed.
▪ Because nitrogen is also lost through the skin, stool
and the GI tract, subtract a correction factor of 3 from
the nitrogen consumed.
▪ Nitrogen balance = (nitrogen consumed [in grams]
– UUN [in grams] – 3
▪ Normal nitrogen balance is positive and ranges from
4 – 6 g. negative nitrogen balance suggests a
catabolic state indicating more protein is broken
down than is consumed.
▪ UUN is the major source of nitrogen excretion.
▪ Subtract the UUN (in grams) from the amount of
nitrogen consumed.
▪ Because nitrogen is also lost through the skin, stool
and the GI tract, subtract a correction factor of 3 from
the nitrogen consumed.
▪ Nitrogen balance = (nitrogen consumed [in grams]
– UUN [in grams] – 3
▪ Normal nitrogen balance is positive and ranges from
4 – 6 g. negative nitrogen balance suggests a
catabolic state indicating more protein is broken
down than is consumed.
▪Is a glycoprotein secreted on the glycocalyx
surface of cells lining the GI tract and is
normally produced during the first or second
trimester of fetal life.
▪High CEA levels are characteristics of various
malignant conditions such as cancer of the
colon, lung, or breast and of certain
nonmalignant conditions such as liver disease,
cirrhosis, alcoholic pancreatitis, heavy
smoking and IBD.
▪ Often called a tumor marker, CEA is used to
monitor the effectiveness of colorectal cancer
therapy.
▪ Serum levels usually return to normal within 6
weeks if cancer treatment is successful.
▪ Perform venipuncture and collect the sample in 7-
ml red-topped tube. Handle the sample gently to
prevent hemolysis which may alter the results.
▪ No heparin for 2 days.
▪ No post procedure care.
▪Fecal content is an indicator of the absorptive
capacity of the gut.
▪It aids in the evaluation of digestive efficiency
and the integrity of the stomach and
intestines.
▪Analysis begins with gross examination of
stool color, consistency, odor, and other
characteristics and concludes with
microscopic, chemical or bacterial analysis.
▪ Blood in the stool – result from hemorrhoids,
partial obstruction
▪ Black tarry stool – result from upper GI bleeding.
▪ Large, bulky, foul smelling stool that floats – may
indicate malabsorption
▪ Diarrhea – is a result of too rapid transit of food in
the GI tract, often caused by viral infection.
▪ Mucus or pus in the stool – result from rectal
abscess or ulcerative colitis
▪ Most frequently performed screening test for
colorectal cancer and is the only test demonstrate.
▪ Detect GI Bleeding
▪ It is based on the change in the color of a guaiac-
based colorless dye to blue caused by the
peroxidase activity of hemoglobin.
▪ It can be performed immediately after the rectal
examination or on stool specimens collected over
3 days. (3 consecutive days)
▪Two samples from each of the consecutive
stools are tested to avoid false-positives.
▪A wooded applicator is used to apply stool to
one side of the guaiac-treated paper.
▪Developing solution is applied, and result is
immediately noted.
▪Blue indicates a positive reaction.
▪Increase fiber diet 48 – 72 hours.
▪ No rare meat and peroxidase-rich foods such as
raw fruits and vegetables for 3 days before test.
▪ Withhold Aspirin, NSAIDs, may increased GI
bleeding.
▪ No read meats, poultry, fish, turnips, horseradish
▪ Withhold for 48hrs: iron, steroids, indomethacin,
colchicine
▪ Iron causes blackish/greenish discoloration of stool
▪ Steroids, indomethacin and colchicine may cause GI
irritation thereby bleeding.
▪Detect intestinal infection caused by several
types of parasites and their ova (eggs).
▪Wear gloves and collect the stool specimen
directly in the container. Note the date and
time of the collection, the consistency of the
specimen, pertinent dietary history and
recent or current antimicrobial therapy.
▪Send specimen to laboratory within 30
minutes of passage or refrigerate if it will bot
be examined immediately.
▪Instruct client to avoid treatments with castor
oil or mineral oil, bismuth, magnesium or
antidiarrheal compounds, barium enemas,
and antibiotics for 7-10 days before the test.
▪Three specimens should be tested by
collection of stool every other day or every
third day.
▪There is no post procedure care.
▪ Bacteriologic examination of the stool identifies
pathogens that may cause overt GI disease.
▪ A sensitivity test may follow isolation of pathogen.
▪ A stool specimen is collected on 3 consecutive days.
▪ Wear gloves and collect the specimen directly in the
container.
▪ Stool may also be collected by means of a rectal swab
inserted past the anal sphincter, rotated gently and
withdrawn.
▪ Place the swab (cotton tipped applicator) in the
appropriate container (sterile test tube), and
send it immediately to the laboratory.
▪ Note the dietary history, recent antimicrobial
therapy and any recent travel that might indicate
endemic infection or infestation.
▪ There is no post procedure care.
▪ Dietary lipids, emulsified by bile, are almost
completely absorbed in the small intestine, provided
biliary and pancreatic secretions are adequate;
however, both digestive and absorptive disorders
may cause steatorrhea (excessive secretions of fecal
lipids)
▪ A quantitative test performed on stool collected over
72-hour period confirms the presence of steatorrhea.
▪ Collect the stool in a non-wax container and keep it
refrigerated.
▪ Instruct the client to abstain from alcohol and to
consume a high-fat diet (100 g) daily for 3 days
before the test and during the collection period.
Drugs that may affect test results, such as
mineral oil, potassium chloride, and neomycin,
should be withheld.
▪ There is no post procedure care.
You might also like
- Diagon SticDocument79 pagesDiagon SticRamyaNo ratings yet
- Textbook Of: Ear, Nose, Throat SurgeryDocument23 pagesTextbook Of: Ear, Nose, Throat SurgeryOliver Scissors50% (2)
- Mksap18 PDFDocument2,355 pagesMksap18 PDFsepan abdullah100% (2)
- EsophagogastroduodenosDocument34 pagesEsophagogastroduodenosAngela Beatriz Dela Vega100% (1)
- Endoscopy: (Esophago-Gastro-Duodenoscopy)Document13 pagesEndoscopy: (Esophago-Gastro-Duodenoscopy)Renaa PujiiNo ratings yet
- GI Diagnostic TestsDocument7 pagesGI Diagnostic TestspatzieNo ratings yet
- Penyiasatan Sistem Alimentry INSANDocument30 pagesPenyiasatan Sistem Alimentry INSANSaha DirllahNo ratings yet
- Ii. Diagnostic TestDocument93 pagesIi. Diagnostic TestFarisa Jane BanggoNo ratings yet
- Barium EnemaDocument5 pagesBarium EnemaarturogarcesjrNo ratings yet
- Indikasi Endoskopi Saluran Cerna Atas Dan Persiapan PasienDocument38 pagesIndikasi Endoskopi Saluran Cerna Atas Dan Persiapan PasienChristopher KusumajayaNo ratings yet
- Diagnostic Procedures ERCPetcDocument46 pagesDiagnostic Procedures ERCPetcMae Arra Lecobu-anNo ratings yet
- Preparation of Patient Prior Upper and Lower GiDocument40 pagesPreparation of Patient Prior Upper and Lower Gishyaka jean claudeNo ratings yet
- EsophagogastroduodenosDocument6 pagesEsophagogastroduodenosdrnareshkumar3281No ratings yet
- Endoscopy, Barium MealDocument22 pagesEndoscopy, Barium Mealyudhisthir panthiNo ratings yet
- DysphagiaDocument4 pagesDysphagiaIqra FatemahNo ratings yet
- Day 3 Lecture - GI and NutritionDocument71 pagesDay 3 Lecture - GI and NutritionRemej SilutgamNo ratings yet
- CT Specialized ProceduresDocument41 pagesCT Specialized ProceduresJimmy MainaNo ratings yet
- Colonoscopy / Page ofDocument4 pagesColonoscopy / Page offallenangelleNo ratings yet
- Intestinal ObstructionDocument6 pagesIntestinal ObstructionAnton GabrielNo ratings yet
- MINOR SURGERY REPORT-editDocument20 pagesMINOR SURGERY REPORT-editNdor BariboloNo ratings yet
- Definition of The Disease: Risk FactorsDocument13 pagesDefinition of The Disease: Risk FactorsDivine Ballesteros Dela CruzNo ratings yet
- Contrast Radiology, Coronary AngioDocument44 pagesContrast Radiology, Coronary AngioManikandan KanagarajNo ratings yet
- Colonoscopy ProcedureDocument2 pagesColonoscopy ProcedureNick Arngel CorporalNo ratings yet
- ColonosDocument5 pagesColonosMa. Aira Jean PedroNo ratings yet
- Endoscopic Retrograde Cholangiopancreatography (Ercp) : Jinu Janet Varghese Group IV Year IIIDocument22 pagesEndoscopic Retrograde Cholangiopancreatography (Ercp) : Jinu Janet Varghese Group IV Year IIIManish DhapolaNo ratings yet
- Lecture-3 GIT RKDocument46 pagesLecture-3 GIT RKmuhammadameerhamza4786No ratings yet
- UGIS RadiologyDocument31 pagesUGIS RadiologyJulienne Sanchez-SalazarNo ratings yet
- Bowel Obstruction - ppt1Document30 pagesBowel Obstruction - ppt1Elfrida Aulia100% (1)
- Care With Git PTDocument16 pagesCare With Git PTHafidz Ma'rufNo ratings yet
- ColonosDocument20 pagesColonosCarl miguel LoretoNo ratings yet
- CholecystectomyDocument17 pagesCholecystectomyStephanie Joy EscalaNo ratings yet
- Cholecystectomy and Nursing Care PlanDocument8 pagesCholecystectomy and Nursing Care PlanLara GatbontonNo ratings yet
- NG Tube Lictures 2023Document22 pagesNG Tube Lictures 2023ALi NursingNo ratings yet
- NGT PresentationDocument23 pagesNGT PresentationniyigokNo ratings yet
- ColonosDocument22 pagesColonosJulienne Sanchez-Salazar100% (1)
- July 27, 2009 Exploratory Laparotomy and Transverse Loop Colostomy 1.Document8 pagesJuly 27, 2009 Exploratory Laparotomy and Transverse Loop Colostomy 1.MaRVNo ratings yet
- Sigmoidoscopy: Presented by Kriti Adhikari Roll No: 17Document38 pagesSigmoidoscopy: Presented by Kriti Adhikari Roll No: 17sushma shresthaNo ratings yet
- Nur 322 Gi DisordersDocument113 pagesNur 322 Gi DisordersLovelights ZamoraNo ratings yet
- What Is EndosDocument2 pagesWhat Is EndosSambit ClinicNo ratings yet
- Providing Special CareDocument23 pagesProviding Special CareJan LagriaNo ratings yet
- GASTROSTOMYDocument8 pagesGASTROSTOMYRio Gonzales100% (1)
- Malformations of OesophagusDocument24 pagesMalformations of OesophagusOwoupele Ak-Gabriel100% (1)
- Endoscopicretrograde Cholangiopancreatography (ERCP)Document21 pagesEndoscopicretrograde Cholangiopancreatography (ERCP)Suman PokhrelNo ratings yet
- Doc1 Obstractive JaundiceDocument7 pagesDoc1 Obstractive JaundiceZhy CaluzaNo ratings yet
- MSN AssignmentDocument43 pagesMSN AssignmentSupriya chhetryNo ratings yet
- Intussuscept ION: in The Paediatric PatientDocument30 pagesIntussuscept ION: in The Paediatric PatientSuneil R AlsNo ratings yet
- 116 Final ReviewDocument194 pages116 Final ReviewAlkiana SalardaNo ratings yet
- Readings On UgieDocument5 pagesReadings On UgieQueenie Gail Duarte RodrigoNo ratings yet
- Colonoscopy ProcedureDocument3 pagesColonoscopy Procedurejmarcos84No ratings yet
- LaparotomyDocument36 pagesLaparotomydenekeNo ratings yet
- Capsule Endoscopy (Wireless Endoscopy)Document19 pagesCapsule Endoscopy (Wireless Endoscopy)Pratik KulkarniNo ratings yet
- Gastro Esophageal Reflux Disease: (Case Study)Document7 pagesGastro Esophageal Reflux Disease: (Case Study)nj02No ratings yet
- Case Lâm SàngDocument39 pagesCase Lâm SàngHungNo ratings yet
- INTESTINAL OBSTRUCTION ShamxDocument11 pagesINTESTINAL OBSTRUCTION ShamxWilhelmo DiconNo ratings yet
- CHOLELITHIASISDocument27 pagesCHOLELITHIASISAlkiana SalardaNo ratings yet
- Cholecystitis Cholelithiasis PresentationDocument21 pagesCholecystitis Cholelithiasis PresentationPrincess Meinny JeanNo ratings yet
- Ulcerative ColitisDocument12 pagesUlcerative Colitisquidditch07No ratings yet
- Open Cholecystectomy: By: Santoyo, Sarah Jane R. BSN 3-B Group 6-Operating RoomDocument6 pagesOpen Cholecystectomy: By: Santoyo, Sarah Jane R. BSN 3-B Group 6-Operating RoomJullie Anne SantoyoNo ratings yet
- Barium SwallowDocument56 pagesBarium SwallowJulienne Sanchez-Salazar100% (1)
- Dysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandDysphagia, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 5 out of 5 stars5/5 (1)
- Diverticulitis Cure: The Ultimate Diverticulitis Diet: Diverticulitis Recipes: Your Ultimate Diverticulitis CookbookFrom EverandDiverticulitis Cure: The Ultimate Diverticulitis Diet: Diverticulitis Recipes: Your Ultimate Diverticulitis CookbookNo ratings yet
- Day 5 Lecture - GI and NutritionDocument65 pagesDay 5 Lecture - GI and NutritionRemej SilutgamNo ratings yet
- Day 3 Lecture - GI and NutritionDocument71 pagesDay 3 Lecture - GI and NutritionRemej SilutgamNo ratings yet
- Day 2 Lecture - GI and NutritionDocument58 pagesDay 2 Lecture - GI and NutritionRemej SilutgamNo ratings yet
- Handoversheet AnsoDocument15 pagesHandoversheet AnsoRemej SilutgamNo ratings yet
- Day 1 Lecture - GI and NutritionDocument46 pagesDay 1 Lecture - GI and NutritionRemej SilutgamNo ratings yet
- BARTHELDocument2 pagesBARTHELRemej SilutgamNo ratings yet
- Nutrition Risk Screening 2002 (NRS 2002)Document1 pageNutrition Risk Screening 2002 (NRS 2002)Remej SilutgamNo ratings yet
- DiarrheaDocument14 pagesDiarrheaRemej SilutgamNo ratings yet
- Midsayap Doctors Specialist Hospital, Inc.: Clinical Cover SheetDocument2 pagesMidsayap Doctors Specialist Hospital, Inc.: Clinical Cover SheetRemej SilutgamNo ratings yet
- Concepts of ComputerDocument81 pagesConcepts of ComputerRemej SilutgamNo ratings yet
- Year 6 - Science Keypoint NotesDocument8 pagesYear 6 - Science Keypoint Notesteddyen100% (1)
- Teeth and Tongue-: I. MouthDocument11 pagesTeeth and Tongue-: I. Moutharisu100% (1)
- Children Part I Continuation TABLEDocument5 pagesChildren Part I Continuation TABLEMaikka IlaganNo ratings yet
- NCM 116Document19 pagesNCM 116Gail Leslie HernandezNo ratings yet
- Carcinoma Oesophagus: Dr. S. Ranita DeviDocument46 pagesCarcinoma Oesophagus: Dr. S. Ranita DeviVivek AhanthemNo ratings yet
- Histology ReviewDocument66 pagesHistology Reviewsayeda.raza24No ratings yet
- Gerd Maam Weng MingoyDocument1 pageGerd Maam Weng MingoyMingoy, CarlosNo ratings yet
- Acid RefluxDocument6 pagesAcid RefluxAnu RNo ratings yet
- Digestive System and NutritionDocument6 pagesDigestive System and NutritionAthena HuynhNo ratings yet
- Clinical Surgery NotesDocument214 pagesClinical Surgery Notessarahsarahsarahsarah100% (6)
- Week 8 Pedia Pediatric GI DisturbancesDocument110 pagesWeek 8 Pedia Pediatric GI DisturbancesJaja ManezNo ratings yet
- Cat Dissection Guide NetDocument46 pagesCat Dissection Guide NetHazel Grace Bellen100% (3)
- Digestive System of FinfishesDocument38 pagesDigestive System of FinfishesUmme TasnimNo ratings yet
- Digestive System: Submitted By: Caimoso, Tricia Ann D. Quiambao, Aliyah Lourdes D. Bs Psychology 3-3Document9 pagesDigestive System: Submitted By: Caimoso, Tricia Ann D. Quiambao, Aliyah Lourdes D. Bs Psychology 3-3Tricia Ann CaimosoNo ratings yet
- Typhoid Fever - For PrintingDocument23 pagesTyphoid Fever - For PrintingAna Katrina CaberteNo ratings yet
- Upper Git Medical Nutrition Therapy 2Document32 pagesUpper Git Medical Nutrition Therapy 2KHALEEL SALEHNo ratings yet
- A Guide To Gastrointestinal Motility DisordersDocument113 pagesA Guide To Gastrointestinal Motility DisordersArlen ElisaNo ratings yet
- I. Common GI Presentations.: 1. The MouthDocument26 pagesI. Common GI Presentations.: 1. The MouthFarah FarahNo ratings yet
- Guidelines For Surgical Treatment of Gastroesophageal Reflux Disease GERDDocument48 pagesGuidelines For Surgical Treatment of Gastroesophageal Reflux Disease GERDMateo TamayoNo ratings yet
- Hiatal HerniaDocument2 pagesHiatal Hernianursegian13No ratings yet
- Pre Natal Care Book BasedDocument9 pagesPre Natal Care Book BasedAngelaTrinidadNo ratings yet
- Barium SwallowDocument24 pagesBarium SwallowFaria KhanNo ratings yet
- Care With Git PTDocument16 pagesCare With Git PTHafidz Ma'rufNo ratings yet
- Project Omoverhi - Low-Cost Neonatal IncubatorDocument128 pagesProject Omoverhi - Low-Cost Neonatal IncubatorAhmedSaadNo ratings yet
- 9 Digestive System Part 1Document14 pages9 Digestive System Part 1Fhayee Sulaik HaronNo ratings yet
- Final SURGERY PDF 4TH YR 7TH SEM SOLVED ON THE BASIS OF PREVIOUS YR PAPER AND BOOKS ANKIT AKELADocument25 pagesFinal SURGERY PDF 4TH YR 7TH SEM SOLVED ON THE BASIS OF PREVIOUS YR PAPER AND BOOKS ANKIT AKELAchai rinNo ratings yet
- L 8 Histology of The Esophagus & StomachDocument10 pagesL 8 Histology of The Esophagus & StomachBoody KhalilNo ratings yet
- Amboss - GITDocument16 pagesAmboss - GITAllysahNo ratings yet