Professional Documents
Culture Documents
Assessment
Assessment
Uploaded by
Wajiha Esmula TiuOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessment
Assessment
Uploaded by
Wajiha Esmula TiuCopyright:
Available Formats
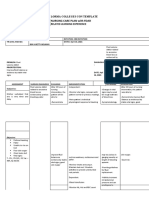
ASSESSMENT Subjective Cues: >Patient states, I am very thirsty.
Objective Cues: > excessive thirst > dry oral mucous membranes > increased heart rate (HR= 140) > decreased BP (BP= 80/57) > increased body temperature (T= 38) > severe polyuria (>7L/day) > urine specific gravity= 1.001 > decreased skin turgor > weakness > irritability
DIAGNOSIS Deficient Fluid Volume related to nausea, vomiting, and diarrhea as evidenced by decreased urine output, increased urine concentration, weakness, fever, decreased skin/tongue turgor, dry mucous membranes, increased pulse rate, and decreased blood pressure
INFERENCE Fluid imbalance can arise due to hypovolemia, normovolemia with maldistribution of fluid, and hypervolemia. Trauma is among the most frequent causes of hypovolemia, with its often profuse attendant blood loss. Another common cause is dehydration, which primarily entails loss of plasma rather than whole blood. The consequences of hypovolemia include reduction in circulating
PLANNING Within 8 hours, patient will maintain adequate fluid volume as evidenced by: > vital signs within N range for age > urine output of 5080ml/hr > urine specific gravity between 1.004 and 1.030 > moist mucous membranes > good skin turgor > patient verbalizing that thirst is no longer excessive
INTERVENTION y Monitor for the existence of factors causing deficient fluid volume (e.g., gastrointestinal losses, difficulty maintaining oral intake, fever, uncontrolled type IIdiabetes mellitus, diuretic therapy).
RATIONALE y Early identification of risk factors and early intervention can decrease the occurrence and severity of complications from deficient fluid volume.
Watch for early signs of hypovolemia, including weakness, muscle cramps, and postural hypotension.
Late signs include oliguria; abdominal or chest pain; cyanosis; cold, clammy skin; and confusion.
EVALUATION Goal met. Patient maintained adequate fluid volume as evidenced by N vital signs, adequate urinary output with normal specific gravity, moist mucous membranes, good skin turgor, and patient s verbalization that thirst is not excessive.
Watch trends in output for 3 days; include all routes of intake and output and
Monitoring for trends for 2 to 3 days gives a more valid picture of the
blood volume, lower venous return and, in profound cases, arterial hypotension. Myocardial failure may result from increased myocardial oxygen demand in conjunction with reduced tissue perfusion.
note color and specific gravity of urine.
client's hydration status than monitoring for a shorter period. Darkcolored urine with increasing specific gravity reflects increased urine concentration.
Monitor daily weight for sudden decreases, especially in the presence of decreasing urine output or active fluid loss. Weigh client on same scale with same type of clothing at same time of day, preferably before breakfast.
Body weight changes reflect changes in body fluid volume. A 1pound weight loss reflects a fluid loss of about 500 cc.
You might also like
- Sickle Cell Anemia Nursing Care PlanDocument6 pagesSickle Cell Anemia Nursing Care PlanArisa Vijungco100% (4)
- Post Partum Hemorrhage Nursing Care PlanDocument2 pagesPost Partum Hemorrhage Nursing Care PlanCyrus De Asis82% (34)
- Nursing Diagnosis and Nursing Interventions For Dengue Hemorrhagic FeverDocument2 pagesNursing Diagnosis and Nursing Interventions For Dengue Hemorrhagic FeverThirdy Aquino82% (28)
- Nursing Care Plan For Acute Gastrointestinal HemorrhageDocument2 pagesNursing Care Plan For Acute Gastrointestinal HemorrhageCyrus De Asis92% (25)
- NCP For DehydrationDocument3 pagesNCP For Dehydrationpeter_degamo200025% (4)
- NCP Format 3 (CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy)Document4 pagesNCP Format 3 (CKD Chronic Kidney Disease DM Diabetes Mellitus Nephropathy)John Christopher Celestino100% (10)
- Assignment 2 Buffers and Isotonic SolutionsDocument3 pagesAssignment 2 Buffers and Isotonic SolutionsArlac AsocseNo ratings yet
- SAMPLE NCP For Diabetes InsipidusDocument3 pagesSAMPLE NCP For Diabetes InsipidusClancy Anne Garcia Naval50% (2)
- Decreased Cardiac OutputDocument9 pagesDecreased Cardiac OutputChinita Sangbaan75% (4)
- Gordon's 11 Functional Health PatternsDocument1 pageGordon's 11 Functional Health PatternsTracy100% (37)
- Student Guide: Unit 2: Brain Maintenance Lesson 2Document3 pagesStudent Guide: Unit 2: Brain Maintenance Lesson 2ria wu0% (1)
- Fluid Volume DeficitDocument12 pagesFluid Volume DeficitKersee GailNo ratings yet
- Fluid Deficit RevisedDocument6 pagesFluid Deficit RevisedShaira SariaNo ratings yet
- Fluids Electrolytes Group 1 CompilationDocument41 pagesFluids Electrolytes Group 1 CompilationShaira SariaNo ratings yet
- Fluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsDocument17 pagesFluid Volume Deficit (Dehydration) Nursing Care Plan - NurseslabsA.No ratings yet
- Nursing Care Plans With Nursing DiagnosisDocument6 pagesNursing Care Plans With Nursing DiagnosisLalaine RomeroNo ratings yet
- Signs and Symptoms Vital SignsDocument3 pagesSigns and Symptoms Vital SignsCris CandoNo ratings yet
- Cues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationDocument3 pagesCues Nursing Diagnosis Goal Nursing Interventions Rationale EvaluationVher SisonNo ratings yet
- Nursing DiagnosisDocument4 pagesNursing DiagnosisMavy AndresNo ratings yet
- Hypovolemic Shock 09Document58 pagesHypovolemic Shock 09Joanne Bernadette Aguilar100% (2)
- Fluid Imbalance (NCP)Document9 pagesFluid Imbalance (NCP)Putry RainismNo ratings yet
- Water Excess SyndromeDocument5 pagesWater Excess SyndromeQueenie Velasquez Reinoso JacksonNo ratings yet
- Nursing Diagnosis Fluid ExcessDocument8 pagesNursing Diagnosis Fluid ExcessLuthfiy IrfanasruddinNo ratings yet
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- Cardiovascular System Diseases Part 2Document9 pagesCardiovascular System Diseases Part 2Prince Rener Velasco PeraNo ratings yet
- KMB Diabetes InsipidusDocument24 pagesKMB Diabetes InsipidusNur Rofikoh Bil Karomah100% (1)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Chief Complaint: IndependentDocument4 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective: Chief Complaint: IndependentTed Cipriano VistaNo ratings yet
- NCP 3 DEFICIT IN FLUID VOLUMEDocument2 pagesNCP 3 DEFICIT IN FLUID VOLUMEGenEsis CarandangNo ratings yet
- Hypovolemic ShockDocument12 pagesHypovolemic ShockHassanal DimaporoNo ratings yet
- Approach To Patient With Generalized Body OedemaDocument7 pagesApproach To Patient With Generalized Body OedemaAbdulJabar RiadhNo ratings yet
- Pleno Minggu 2 Blok 3.4Document84 pagesPleno Minggu 2 Blok 3.4Devi Yunita PurbaNo ratings yet
- But He Hated The Taste of Water: Nursing Assessment RationaleDocument4 pagesBut He Hated The Taste of Water: Nursing Assessment RationaleJiv Rouziell DoroteoNo ratings yet
- Hypovolemic Shock Nursing Care Management and Study GuideDocument1 pageHypovolemic Shock Nursing Care Management and Study GuideRoselyn VelascoNo ratings yet
- LP DHFDocument14 pagesLP DHFyustiNo ratings yet
- Assessment Diagnosis Scientific Explanation Goal Intervention Rationale Expected Outcome SubjectiveDocument4 pagesAssessment Diagnosis Scientific Explanation Goal Intervention Rationale Expected Outcome SubjectiveKeith MirasolNo ratings yet
- Nursing Care PlanDocument28 pagesNursing Care PlanChristine Karen Ang Suarez67% (3)
- Medical Surgical Fluid and Electrolytes FVD FVEDocument7 pagesMedical Surgical Fluid and Electrolytes FVD FVEMichaelaKatrinaTrinidadNo ratings yet
- C C C C C C C C C C C C C C C C C C C C C C C C C C C C C C C CDocument5 pagesC C C C C C C C C C C C C C C C C C C C C C C C C C C C C C C CMichaela ArellanoNo ratings yet
- NCP CKD From CaneDocument74 pagesNCP CKD From CaneSheela Khrystyn LeeNo ratings yet
- Acute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CDocument29 pagesAcute Glomerulonep Hritis: By: Edelrose D. Lapitan BSN Iii-CEdelrose Lapitan100% (1)
- Fluid Volume ExcessDocument4 pagesFluid Volume ExcessChristine Quirona100% (1)
- Assessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationDocument6 pagesAssessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationRoMarie AbainzaNo ratings yet
- Dapus 3Document7 pagesDapus 3Dhea NadhilaNo ratings yet
- Acute Glomerulonephritis (Agn)Document42 pagesAcute Glomerulonephritis (Agn)Rowshon AraNo ratings yet
- HemodialysisDocument4 pagesHemodialysisJon Adam Bermudez SamatraNo ratings yet
- 1 Fluid Volume Excess Chronic Renal Failure Nursing Care PlansDocument3 pages1 Fluid Volume Excess Chronic Renal Failure Nursing Care PlansMichael Baylon DueñasNo ratings yet
- Excess Fluid Volume HypervolemiaDocument7 pagesExcess Fluid Volume HypervolemiaLuthfiy IrfanasruddinNo ratings yet
- Deficient Fluid VolumeDocument1 pageDeficient Fluid VolumeSheila ErpeloNo ratings yet
- There Are Two Main Types of GastritisDocument11 pagesThere Are Two Main Types of GastritisMike Faustino SolangonNo ratings yet
- NCP LatestDocument6 pagesNCP LatestThirdy AquinoNo ratings yet
- Fluid Volume Deficit Nursing ManagementDocument5 pagesFluid Volume Deficit Nursing ManagementA.No ratings yet
- Assessment NSG Diagnosis Goal Intervention Implementation EvaluationDocument2 pagesAssessment NSG Diagnosis Goal Intervention Implementation EvaluationMichelle ErikaNo ratings yet
- Cues Nursing Diagnosis Rationale Goals and Objectives Intervention Rationale Evaluation IndependentDocument23 pagesCues Nursing Diagnosis Rationale Goals and Objectives Intervention Rationale Evaluation IndependentWendy EscalanteNo ratings yet
- 79 - Dengue and Dengue Shock SyndromeDocument5 pages79 - Dengue and Dengue Shock SyndromeCeejhay Lee0% (1)
- Hypovolemic Shock RosalDocument27 pagesHypovolemic Shock RosalBEA RADANo ratings yet
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- A Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisFrom EverandA Simple Guide to Blood in Stools, Related Diseases and Use in Disease DiagnosisRating: 3 out of 5 stars3/5 (1)
- Ascites, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandAscites, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- Fluid and Electrolytes for Nursing StudentsFrom EverandFluid and Electrolytes for Nursing StudentsRating: 5 out of 5 stars5/5 (12)
- JjjjokjhDocument4 pagesJjjjokjhWajiha Esmula TiuNo ratings yet
- Signifance of The Study (Version 2)Document2 pagesSignifance of The Study (Version 2)Wajiha Esmula TiuNo ratings yet
- AbstractDocument2 pagesAbstractWajiha Esmula TiuNo ratings yet
- Roles of The Circulating NurseDocument1 pageRoles of The Circulating NurseWajiha Esmula TiuNo ratings yet
- Đề thi vào 10 chuyên anh đáp án ĐỀ THI THỬ LẦNDocument8 pagesĐề thi vào 10 chuyên anh đáp án ĐỀ THI THỬ LẦNHồ Ngọc TrAnhNo ratings yet
- Heat Exhaustion: Widya Gladiantari - 1510211068 - Tutorial B1 - Blok MatraDocument8 pagesHeat Exhaustion: Widya Gladiantari - 1510211068 - Tutorial B1 - Blok MatraWidya GladiantariNo ratings yet
- Fluids and ElectrolytesDocument140 pagesFluids and ElectrolytesChe S. MDNo ratings yet
- PRNA 2009pocket Resource For Nutrition AssessmentDocument132 pagesPRNA 2009pocket Resource For Nutrition AssessmentjinkuocsulbNo ratings yet
- Inbound 7239638357502484983Document9 pagesInbound 7239638357502484983fedeliciojizelleNo ratings yet
- Water Physiology Essentiality, Metabolism, And.8Document6 pagesWater Physiology Essentiality, Metabolism, And.8Patricia ChirinosNo ratings yet
- NCP DiabetesDocument3 pagesNCP DiabetesKartika MilaningrumNo ratings yet
- Importance of Sports NutritionDocument63 pagesImportance of Sports NutritionAlexander ScottNo ratings yet
- Nursing Care PlanDocument28 pagesNursing Care PlanChristine Karen Ang Suarez67% (3)
- ACSM Position Stand - Exercise and Fluid Replacement - Medicine & Science in Sports & ExerciseDocument7 pagesACSM Position Stand - Exercise and Fluid Replacement - Medicine & Science in Sports & ExerciseDiógenes OliveiraNo ratings yet
- Presentation On Hydration PDFDocument17 pagesPresentation On Hydration PDFManuel CastroNo ratings yet
- Lab ResultsDocument3 pagesLab ResultsKristal Cyril PolzNo ratings yet
- Zollinger-Ellison SyndromeDocument9 pagesZollinger-Ellison SyndromeGLYDEL CORDERONo ratings yet
- Chemotherapy Information: Central Toronto Veterinary Referral Clinic Oncology Service Kevin Finora DVM, Diplomate ACVIMDocument5 pagesChemotherapy Information: Central Toronto Veterinary Referral Clinic Oncology Service Kevin Finora DVM, Diplomate ACVIMfrancesjadeNo ratings yet
- Preps 4-61Document57 pagesPreps 4-61fianaNo ratings yet
- Data Sheet Data Sheet: Gelafusal GelafusalDocument2 pagesData Sheet Data Sheet: Gelafusal Gelafusalfahri azwarNo ratings yet
- 16 Fluid Electrolytes and Acid-Base ImbalancesDocument29 pages16 Fluid Electrolytes and Acid-Base ImbalancesBea Bianca CruzNo ratings yet
- Kostelnik JAm Coll Nutr 2020 Urine ColorreviewDocument10 pagesKostelnik JAm Coll Nutr 2020 Urine ColorreviewNicole TenenbaumNo ratings yet
- Reading Diagnotic Pre-Test (Paper)Document10 pagesReading Diagnotic Pre-Test (Paper)Imam Mulya SetiadiNo ratings yet
- Acute Viral Gastroenteritis in Adults UpToDateDocument12 pagesAcute Viral Gastroenteritis in Adults UpToDateItzrael DíazNo ratings yet
- Fluid Electrolytes and Acid-Base BalanceDocument12 pagesFluid Electrolytes and Acid-Base BalanceHajra Al-Khuwaitem100% (1)
- CPG - Acute Infectious DiarrheaDocument52 pagesCPG - Acute Infectious DiarrheaJim Christian EllaserNo ratings yet
- F. NCP ProperDocument4 pagesF. NCP ProperAle SandraNo ratings yet
- Acute Diarrhea and Shock in The EDDocument5 pagesAcute Diarrhea and Shock in The EDmohamed fahmyNo ratings yet
- Pediatric Gastroenterology Algorithme PDFDocument118 pagesPediatric Gastroenterology Algorithme PDFJonathan Welch100% (1)
- PE 11 - MELC 5 Module 5 - Week8 For StudentDocument27 pagesPE 11 - MELC 5 Module 5 - Week8 For StudentEsmer Cabansag FelixNo ratings yet
- Nursing Care Plan With Fdar: Lorma Colleges Con Template Related Learning ExperienceDocument3 pagesNursing Care Plan With Fdar: Lorma Colleges Con Template Related Learning ExperienceMelinda Cariño BallonNo ratings yet
- 13 Areas of AssessmentDocument5 pages13 Areas of AssessmentPau-pau BasiNo ratings yet