Professional Documents
Culture Documents
Fsurg 09 837545
Fsurg 09 837545
Uploaded by
juan uribeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fsurg 09 837545
Fsurg 09 837545
Uploaded by
juan uribeCopyright:
Available Formats
ORIGINAL RESEARCH
published: 04 April 2022
doi: 10.3389/fsurg.2022.837545
The Effect of the Intraoperative Blood
Loss and Intraoperative Blood
Transfusion on the Short-Term
Outcomes and Prognosis of
Colorectal Cancer: A Propensity
Score Matching Analysis
Bing Kang 1† , Xiao-Yu Liu 2† , Zi-Wei Li 2 , Chao Yuan 2 , Bin Zhang 2 , Zheng-Qiang Wei 2 and
Dong Peng 2*
1
Department of Clinical Nutrition, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China,
2
Department of Gastrointestinal Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
Edited by:
Annamaria Auricchio, Purpose: The purpose of the current study was to analyze the effect of intraoperative
University of Campania Luigi blood loss (IBL) and intraoperative blood transfusion (IBT) on the short-term outcomes
Vanvitelli, Italy
and prognosis for patients who underwent primary colorectal cancer (CRC) surgery.
Reviewed by:
Marcel André Schneider, Methods: We retrospectively collected the patients’ information from the database of a
University Hospital of teaching hospital from January 2011 to January 2020. IBL and IBT were collected and
Zürich, Switzerland
Christina A. Fleming, analyzed, and the propensity score matching (PSM) analysis was performed.
Centre Hospitalier Universitaire de
Results: A total of 4,250 patients with CRC were included in this study. There were
Bordeaux, France
1,911 patients in the larger IBL group and 2,339 patients in the smaller IBL group. As
*Correspondence:
Dong Peng for IBT, there were 82 patients in the IBT group and 4,168 patients in the non-IBT group.
carry_dong@126.com After 1:1 ratio PSM, there were 82 patients in the IBT group and 82 patients in the
† These authors share first authorship non-IBT group. The larger IBL group had longer operation time (p = 0.000 < 0.01),
longer post-operative hospital stay (p = 0.000 < 0.01), smaller retrieved lymph nodes (p
Specialty section:
= 0.000 < 0.01), and higher overall complication (p = 0.000 < 0.01) than the smaller IBL
This article was submitted to
Surgical Oncology, group. The IBT group had longer operation time (p = 0.000 < 0.01), longer hospital stay
a section of the journal (p = 0.016 < 0.05), and higher overall complications (p = 0.013 < 0.05) compared with
Frontiers in Surgery
the non-IBT group in terms of short-term outcomes. Larger IBL (p = 0.000, HR = 1.352,
Received: 16 December 2021
Accepted: 23 February 2022
95% CI = 1.142–1.601) and IBT (p = 0.044, HR = 1.487, 95% CI = 1.011–2.188) were
Published: 04 April 2022 independent predictive factors of overall survival (OS). Larger IBL (p = 0.000, HR = 1.338,
Citation: 95% CI = 1.150–1.558) was an independent predictor of disease-free survival (DFS);
Kang B, Liu X-Y, Li Z-W, Yuan C,
however, IBT (p = 0.179, HR = 1.300, 95% CI = 0.886–1.908) was not an independent
Zhang B, Wei Z-Q and Peng D (2022)
The Effect of the Intraoperative Blood predictor of DFS.
Loss and Intraoperative Blood
Transfusion on the Short-Term
Conclusion: Based on the short-term outcomes and prognosis of IBL and IBT, surgeons
Outcomes and Prognosis of should be cautious during the operation and more careful and proficient surgical skills
Colorectal Cancer: A Propensity are required for surgeons.
Score Matching Analysis.
Front. Surg. 9:837545. Keywords: colorectal cancer, intraoperative blood loss, surgery, prognosis, intraoperative blood
doi: 10.3389/fsurg.2022.837545 transfusion, outcomes
Frontiers in Surgery | www.frontiersin.org 1 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
INTRODUCTION Surgery Management
The CRC surgery was conducted according to the principle
Colorectal cancer (CRC) is one of the most common cancers of AJCC 8th Edition (16). Radical resection (total mesorectal
in the world, with an estimated 1.8 million new cases and excision/complete mesocolic excision) was performed, and the
861,000 deaths each year (1). The incidence of CRC is decreasing pathology confirmed R0 resection.
in western countries including the United States, Canada, and
Australia. However, an upward trend has been existing in China; Definitions
moreover, China is a country with the largest number of new The tumor node metastasis stage was diagnosed according to
cases and deaths of CRC every year in the world (2). At present, the AJCC 8th Edition (21). The complications were graded
radical surgical treatment of CRC is still the most important and according to the Clavien-Dindo classification (22), and major
decisive treatment (3–5). complications were defined as ≥ III classification complications.
Due to the popularity of laparoscopic surgery and the Overall survival (OS) was defined as the time from surgery to the
development of surgical equipment such as electrothermal last follow-up or death. Disease-free survival (DFS) was defined
bipolar activation devices and ultrasound systems, the average as the time from surgery to recurrence, death, or last follow-up.
intraoperative blood loss (IBL) has decreased (6, 7). However, IBL was defined as estimated blood loss during CRC surgery, and
IBL is still a matter of concern during the operation. Studies have IBL was divided into two groups including the larger IBL and
found that larger IBL might affect complications and prognosis the smaller IBL group. The cut-off value of IBL was the 75th
in gastrointestinal tumors (8–10). percentile of IBL (100 ml), larger IBL group was defined as IBL
Perioperative blood transfusion is another concern for ≥ 100 ml, smaller IBL group was defined as IBL < 100 ml. IBT
surgeons. However, the influence of perioperative blood was defined as patients who underwent blood transfusion during
transfusion on short-term outcomes and prognosis was CRC surgery, and they were divided into two groups including
inconsistent. Some studies reported that perioperative blood IBT group and non-IBT group.
transfusion could increase post-operative complications,
prolong hospital stay, and affect prognosis (11–13). However, Outcomes
other studies suggested that perioperative blood transfusion did The primary outcome was the prognosis including OS and DFS.
not affect prognosis (14, 15). The second outcome was the short-term outcomes including
The effect of IBL in patients with CRC is still controversial. operation time, retrieved lymph nodes, overall complications,
Some studies reported that larger IBL could increase major complications, and post-operative hospital stay.
complications and reduce prognosis (16–18). However, other
studies reported that IBL had no effect on complications and Data Collection
prognosis (19, 20). Furthermore, no previous studies reported The baseline information of patients with CRC was collected
the intraoperative blood transfusion (IBT) on the outcomes and retrospectively including sex, age, body mass index (BMI),
prognosis of patients with CRC. Thus, the purpose of the current smoking, drinking, hypertension, type 2 diabetes mellitus
study was to analyze the effect of IBL and IBT on the short-term (T2DM), tumor location, surgery history, surgical methods (open
outcomes and prognosis of patients who underwent primary surgery or laparoscopic surgery), and tumor stage. The short-
CRC surgery. term outcomes were collected through inpatient medical system.
The follow-up information was collected through out-patient
system and telephone interview.
MATERIALS AND METHODS
Propensity Score Matching
We retrospectively collected the patients’ information from
Propensity score matching (PSM) is a method that could
database of a teaching hospital. The database included patients
minimize the bias of baseline information (23, 24). In this study,
who underwent primary CRC surgery from Jan 2011 to Jan
we compared the short-term outcomes and prognosis of IBT
2020. This study was conducted in accordance with the World
on patients with CRC using PSM. Nearest neighbor matching
Medical Association Declaration of Helsinki. Ethical approval
was performed without replacement at a 1:1 ratio and a caliper
from the institutional review board of the First Affiliated Hospital
width with a 0.01 standard deviation was specified. The matched
of Chongqing Medical University was obtained (2021-540). All
baseline information was as follows: age, sex, BMI, smoking,
patients signed the informed consent.
drinking, hypertension, T2DM, tumor location, and tumor stage.
Patients Selection Statistical Analysis
We included patients who underwent primary CRC surgery in a Continuous variables are expressed as the mean ± standard
single teaching hospital (n = 5,473). The exclusion criteria were deviation (SD) and independent-sample t-test was analyzed.
as follows: 1, incomplete medical records (n = 323); 2, non- Frequency variables are expressed as n (%) and Chi-square test
R0 resection (n = 25); and 3, stage IV CRC (n = 875). Finally, or Fisher’s exact test was used. Pearson’s correlation coefficients
a total of 4,250 patients with CRC were included in this study were used to analyze the correlation between IBL and clinical
(Figure 1). characteristics (age, BMI, retrieved lymph nodes, operation time,
Frontiers in Surgery | www.frontiersin.org 2 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
FIGURE 1 | Flow chart of patient selection. IBL, intraoperative blood loss; IBT, intraoperative blood transfusion.
and post-operative hospital stay). The Kaplan–Meier curve was Baseline Characteristics of IBL
conducted to compare the difference between the larger IBL There were 1,911 patients in the larger IBL group and 2,339
group and the smaller IBL group, and between the IBT group patients in the smaller IBL group. The larger IBL group had more
and the non-IBT group. Cox regression analyses were performed men (p = 0.000 < 0.01), higher smoking (p = 0.000 < 0.01),
to identify independent predictive factors for OS and DFS. Data higher drinking (p = 0.038 < 0.05), and more open surgery (p
were analyzed using SPSS (version 22.0) statistical software. A = 0.004 < 0.01) than the smaller IBL group (Table 2).
bilateral p < 0.05 was considered statistically significant.
Short-Term Outcomes of IBL
RESULTS The short-term outcomes were calculated between the larger IBL
group and the smaller IBL group. In this study, the larger IBL
Patients group had a longer operation time (p = 0.000 < 0.01), longer
A total of 4,250 patients with CRC were included in this study. post-operative hospital stay (p = 0.000 < 0.01), smaller retrieved
There were 1,911 patients in the larger IBL group and 2,339 lymph nodes (p = 0.000 < 0.01), and higher overall complication
patients in the smaller IBL group. As for IBT, there were 82 (p = 0.000 < 0.01) than the smaller IBL group (Table 3).
patients in the IBT group and 4,168 patients in the non-IBT
group. After 1:1 ratio PSM, there were 82 patients in the IBT Correlation of IBL and Clinical
group and 82 patients in the non-IBT group. The inclusion and Characteristics
exclusion criteria, and patients with CRC before and after PSM Correlation of IBL and clinical characteristics were analyzed.
are shown in Figure 1. Retrieved lymph nodes (r = −0.110, p = 0.000 < 0.01), operation
time (r = 0.369, p = 0.000 < 0.01), and post-operative stay (r =
Clinical Characteristics of Patients With 0.188, p = 0.000 < 0.01) were significantly correlated with IBL
CRC (Table 4).
The clinical information and surgery outcomes are summarized
in Table 1. There were 2,496 (58.7%) men and 1,754 (41.3%) Baseline Characteristics of IBT
women. The average IBL was 100.4 ± 125.7 ml and 82 (1.9%) The baseline characteristics were compared between the IBT
patients underwent IBT. group and the non-IBT group. The IBT group had older age (p
Frontiers in Surgery | www.frontiersin.org 3 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
TABLE 1 | Clinical characteristics of CRC patients. TABLE 2 | Baseline characteristics of between larger IBL group and smaller IBL
group.
Characteristics No. 4250
Characteristics Larger IBL (1,911) Smaller IBL (2,339) P-value
Age (mean ± SD), year 62.9 ± 12.1
Sex Age (year) 62.6 ± 11.9 63.9 ± 12.5 0.135
Male 2,496 (58.7%) Sex 0.000*
Female 1,754 (41.3%) Male 1,200 (62.8%) 1,296 (55.4%)
BMI (mean ± SD), kg/m 2
22.7 ± 3.2 Female 711 (37.2%) 1,043 (44.6%)
Smoking 1,607 (37.8%) BMI (kg/m2 ) 22.8 ± 3.3 22.6 ± 3.2 0.116
Drinking 1,301 (30.6%) T2DM 283 (14.8%) 238 (10.2%) 0.726
Hypertension 1,108 (26.1%) Smoking 789 (41.3%) 818 (35.0%) 0.000*
T2DM 521 (12.3%) Drinking 616 (32.2%) 685 (29.3%) 0.038*
Surgery history 995 (23.4%) Hypertension 488 (25.5%) 620 (26.5%) 0.473
Laparoscopic surgery 3,608 (84.9%) Surgery history 468 (24.5%) 527 (22.5%) 0.134
Tumor location Open surgery 479 (25.1%) 163 (7.0%) 0.000*
Colon 2,308 (54.3%) Tumor location 0.092
Rectum 1,942 (45.7%) Colon 855 (44.7%) 1,107 (47.3%)
TNM stage Rectum 1,056 (55.3%) 1,232 (52.7%)
I 850 (20.0%) Tumor stage 0.133
II 1,832 (43.1%) I 362 (18.9%) 488 (20.9%)
III 1,568 (36.9%) II 853 (44.6%) 979 (41.9%)
IBL, ml 100.4 ± 125.7 III 696 (36.5%) 872 (37.2%)
IBT 82 (1.9%) Variables are expressed as the mean ± SD, n (%), *P < 0.05.
Retrieved lymph nodes 14.7 ± 7.5 T2DM, type 2 diabetes mellitus; BMI, body mass index; IBL, intraoperative blood loss.
Operation time, min 222.8 ± 76.3
Post-operative hospital stay, day 11.4 ± 8.8
Overall complications 927 (21.8%) TABLE 3 | Outcomes between larger IBL group and smaller IBL group.
Major complications 99 (2.3%) Characteristics Larger IBL (1,911) Smaller IBL (2,339) P-value
Variables are expressed as the mean ± SD, n (%), *P < 0.05.
T2DM, type 2 diabetes mellitus; BMI, body mass index; IBL, intraoperative blood loss; Operation time (min) 256.1 ± 80.9 196.2 ± 60.5 0.000*
IBT, intraoperative blood transfusion. Retrieved lymph nodes 13.5 ± 7.4 15.7 ± 7.5 0.000*
Post-operative hospital 13.3 ± 10.4 9.8 ± 6.8 0.000*
stay (day)
= 0.004 < 0.01), lower BMI (p = 0.001 < 0.01), lower portion Overall complications 538 (28.2%) 389 (16.6%) 0.000*
of rectal cancer (p = 0.003 < 0.01), and lower portion of stage Major complications 53 (2.8%) 46 (2.0%) 0.083
I CRC (p = 0.013 < 0.05) than the non-IBT group before PSM.
Variables are expressed as the mean ± SD, n (%), *P < 0.05.
After 1:1 ratio PSM, there was no significant difference between
the two groups (p > 0.05) (Table 5).
TABLE 4 | Correlation of IBL and clinical characteristics.
Short-Term Outcomes of IBT
The IBL of the IBT group was 376.6 ± 327.2 ml, which was larger IBL, ml
than 95.0 ± 111.8 ml of the non-IBT group before PSM. After 1:1 Correlation P
ratio PSM, the IBL of the IBT group was 376.6 ± 327.2 ml, which
was larger than 86.8 ± 74.7 ml of the non-IBT group. Age, year 0.020 0.191
Before 1:1 ratio PSM, the IBT group had longer operation time BMI, kg/m2 0.023 0.132
(p = 0.000 < 0.01), longer hospital stay (p = 0.000 < 0.01), and Retrieved lymph nodes −0.110 0.000*
higher overall complications (p = 0.000 < 0.01) compared with Operation time, min 0.369 0.000*
the non-IBT group. Post-operative hospital stay, day 0.188 0.000*
After 1:1 ratio PSM, the IBT group had longer operation time
*P < 0.05.
(p = 0.000 < 0.01), longer hospital stay (p = 0.016 < 0.05), and BMI, body mass index; IBL, intraoperative blood loss.
higher overall complications (p = 0.013 < 0.05) compared with
the non-IBT group (Table 6).
(p = 0.000, HR = 1.947, 95% CI = 1.648–2.302), advanced tumor
Prognosis stage (p = 0.000, HR = 2.098, 95% CI=1.853–2.377), larger IBL
The median follow-up time was 37 (1–114) months. We (p = 0.000, HR = 1.352, 95% CI = 1.142–1.601), IBT (p =
conducted univariate and multivariate analysis of OS; older age 0.044, HR = 1.487, 95% CI = 1.011–2.188), overall complications
Frontiers in Surgery | www.frontiersin.org 4 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
TABLE 5 | Baseline characteristics before and after PSM.
Characteristics Before PSM After PSM
IBT (82) Non-IBT (4,168) P-value IBT (82) Non-IBT (82) P-value
Age (year) 66.8 ± 14.9 62.8 ± 12.1 0.004* 66.8 ± 14.9 65.3 ± 10.5 0.463
Sex 0.625 0.875
Male 46 (56.1%) 2,450 (58.8%) 46 (56.1%) 47 (57.3%)
Female 36 (43.9%) 1,718 (41.2%) 36 (43.9%) 35 (42.7%)
BMI (kg/m2 ) 21.6 ± 3.1 22.8 ± 3.2 0.001* 21.6 ± 3.1 21.6 ± 3.2 0.986
Smoking 29 (35.4%) 1,578 (37.9%) 0.645 29 (35.4%) 31 (37.8%) 0.746
Drinking 23 (28.0%) 1,278 (30.7%) 0.611 23 (28.0%) 23 (28.0%) 1.000
Hypertension 20 (24.4%) 1,088 (26.1%) 0.726 20 (24.4%) 16 (19.5%) 0.450
T2DM 14 (17.1%) 507 (12.2%) 0.179 14 (17.1%) 15 (18.3%) 0.838
Tumor location 0.003* 0.268
Colon 51 (62.2%) 2,257 (54.2%) 51 (62.2%) 44 (53.7%)
Rectum 31 (37.8%) 1,911 (45.8%) 31 (37.8%) 38 (46.3%)
Tumor stage 0.013* 0.618
I 7 (8.5%) 843 (20.2%) 7 (8.5%) 10 (12.2%)
II 35 (42.7%) 1,797 (43.1%) 35 (42.7%) 30 (36.6%)
III 40 (48.8%) 1,528 (36.7%) 40 (48.8%) 42 (51.2%)
Variables are expressed as the mean ± SD, n (%), *P < 0.05.
T2DM, type 2 diabetes mellitus; BMI, body mass index; PSM, propensity score matching; IBT, intraoperative blood transfusion.
TABLE 6 | Short-term outcomes before and after PSM.
Characteristics Before PSM After PSM
IBT (82) Non-IBT (4,168) P-value IBT (82) Non-IBT (82) P-value
IBL (ml) 376.6 ± 327.2 95.0 ± 111.8 0.000* 376.6 ± 327.2 86.8 ± 74.7 0.000*
Operation time (min) 279.5 ± 91.7 221.7 ± 75.5 0.000* 279.5 ± 91.7 212.5 ± 72.7 0.000*
Retrieved lymph nodes 14.0 ± 7.3 14.7 ± 7.5 0.375 14.0 ± 7.3 15.3 ± 6.6 0.238
Post-operative hospital stay (day) 15.2 ± 9.2 11.3 ± 8.8 0.000* 15.2 ± 9.2 11.7 ± 9.3 0.016*
Overall complications 35 (42.7%) 892 (21.4%) 0.000* 35 (42.7%) 20 (24.4%) 0.013*
Major complications 2 (2.4%) 97 (2.3%) 0.717 2 (2.4%) 3 (3.7%) 1.000
Variables are expressed as the mean ± SD, n (%), *P <0.05.
PSM, propensity score matching; IBT, intraoperative blood transfusion.
(p = 0.000, HR = 1.439, 95% CI = 1.201–1.723) and major had worse OS and DFS before and after PSM than the non-IBT
complications (p = 0.000, HR = 2.431, 95% CI = 1.708–3.459) group (p < 0.05) (Figure 3).
were independent predictors of OS (Table 7).
In terms of DFS, older age (p = 0.000, HR = 1.718, 95% CI DISCUSSION
= 1.480–1.994), advanced tumor stage (p = 0.000, HR = 2.061,
95% CI = 1.841–2.307), overall complications (p = 0.001, HR In this study, there were 1,911 patients in the larger IBL group
= 1.344, 95% CI = 1.137–1.588), larger IBL (p = 0.000, HR = and 2,339 patients in the smaller IBL group. As for IBT, after 1:1
1.338, 95% CI = 1.150–1.558), and major complications (p = ratio PSM, there were 82 patients in the IBT group and 82 patients
0.000, HR = 2.187, 95% CI = 1.549–3.087) were independent in the non-IBT group. The larger IBL group had longer operation
predictors. However, IBT (p = 0.179, HR = 1.300, 95% CI time, longer post-operative hospital stay, smaller retrieved lymph
= 0.886–1.908) was not an independent predictor of DFS nodes, and higher overall complication than the smaller IBL
(Table 8). group. The IBT group had longer operation time, longer hospital
Furthermore, the Kaplan–Meier curve was conducted to stays, and higher overall complications compared with the non-
compare the difference between the larger IBL group and the IBT group in terms of short-term outcomes. Larger IBL and IBT
smaller IBL group, and between the IBT group and the non-IBT were independent predictive factors of OS.
group. The larger IBL group had worse OS and DFS than the The amount of IBL could reflect the difficulty of surgery. There
smaller IBL group (p < 0.01) (Figure 2). Moreover, the IBT group was a controversy of prognosis regarding IBL for patients with
Frontiers in Surgery | www.frontiersin.org 5 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
TABLE 7 | Univariate and multivariate analysis of overall survival. TABLE 8 | Univariate and multivariate analysis of disease-free survival.
Risk factors Univariate analysis Multivariate analysis Risk factors Univariate analysis Multivariate analysis
HR (95% CI) P-value HR (95% CI) P-value HR (95% CI) P-value HR (95% CI) P-value
Age (>/≤64, 2.141 (1.817–2.522) 0.000* 1.947 (1.648–2.302) 0.000* Age (>/≤64, 1.852 (1.598–2.146) 0.000* 1.718 (1.480–1.994) 0.000*
years) years)
Sex (female/male) 0.897 (0.763–1.055) 0.188 Sex (female/male) 0.902 (0.778–1.046) 0.172
BMI (>/≤22.6) 0.793 (0.675–0.930) 0.004* 0.873 (0.743–1.027) 0.101 BMI (>/≤22.6) 0.854 (0.739–0.988) 0.034* 0.930 (0.804–1.077) 0.332
Hypertension 1.047 (0.874–1.255) 0.618 Hypertension 1.038 (0.880–1.224) 0.659
(yes/no) (yes/no)
T2DM (yes/no) 1.267 (1.005–1.598) 0.045* 1.067 (0.843–1.349) 0.591 T2DM (yes/no) 1.136 (0.914–1.412) 0.252
Tumor site (colon/ 1.160 (0.990–1.359) 0.067 Tumor site (colon/ 1.085 (0.939–1.254) 0.268
rectum) rectum)
Tumor stage (III/II/I) 2.073 (1.831–2.346) 0.000* 2.098 (1.853–2.377) 0.000* Tumor stage (III/II/I) 2.039 (1.823–2.282) 0.000* 2.061 (1.841–2.307) 0.000*
Smoking (yes/no) 1.075 (0.914–1.264) 0.382 Smoking (yes/no) 1.085 (0.936–1.257) 0.279
Drinking (yes/no) 1.040 (0.876–1.234) 0.654 Drinking (yes/no) 1.036 (0.886–1.211) 0.661
IBL (larger/smaller) 1.465 (1.242–1.727) 0.000* 1.352 (1.142–1.601) 0.000* IBL (larger/smaller) 1.415 (1.220–1.642) 0.000* 1.338 (1.150–1.558) 0.000*
IBT (yes/no) 2.107 (1.442–3.080) 0.000* 1.487 (1.011–2.188) 0.044* IBT (yes/no) 1.802 (1.235–2.630) 0.002* 1.300 (0.886–1.908) 0.179
Overall 1.817 (1.539–2.146) 0.000* 1.439 (1.201–1.723) 0.000* Overall 1.647 (1.411–1.923) 0.000* 1.344 (1.137–1.588) 0.001*
complications complications
(yes/no) (yes/no)
Major 2.991 (2.154–4.154) 0.000* 2.431 (1.708–3.459) 0.000* Major 2.561 (1.855–3.536) 0.000* 2.187 (1.549–3.087) 0.000*
complications complications
(yes/no) (yes/no)
*P < 0.05. *P < 0.05.
HR, hazard ratio; CI, confidence interval; BMI, body mass index; T2DM, type 2 diabetes HR, hazard ratio; CI, confidence interval; BMI, body mass index; T2DM, type 2 diabetes
mellitus; IBL, intraoperative blood loss; IBT, intraoperative blood transfusion. mellitus; IBL, intraoperative blood loss; IBT, intraoperative blood transfusion.
CRC (16–20, 25–27). Egenvall et al. reported that larger IBL might be affected by larger IBL and IBT, which resulted in
increases the risk of later surgery for small bowel obstruction prolonged hospital stay. Therefore, surgeons should try to ensure
caused by tumor recurrence and surgical complications, but OS the accuracy of the operation to avoid larger IBL or IBT.
was not affected (20). Another study also reported IBL was not In this study, larger IBL was an independent predictive
associated with increased median length of hospital stay nor factor of OS and DFS. The mechanism might be as follows:
did it increase the 30-day readmission rate (19). However, other the animal experiments show that the activity or cytotoxicity
studies reported that larger IBL was associated with increased of natural killer cells was reduced after blood loss, and the
complications or poor prognosis (16–18). Therefore, it was degree of reduction was related to the amount of blood
necessary to analyze the effect of IBL on the short-term outcomes loss (28, 29). IBL might increase the risk of tumor spread
and prognosis of patients who underwent primary CRC surgery. through blood during CRC surgery, which might lead to
However, the cut-off value of IBL was inconsistent in previous early recurrence and poor prognosis (30). In addition, larger
studies. We concluded the baseline information, cut-off value of IBL could lead to insufficient tissue perfusion and insufficient
IBL, and outcomes of previous studies in Table 9. The cut-off oxygenation (18). These events inhibited mitogen-induced
value of IBL was 50 ml, 100 ml, 200 ml, 250 ml, 450 ml, 800 ml, lymphocyte proliferation and the production of interleukin-2
and 1,400 ml (16–20, 25–27). In this study, the cut-off value of (31, 32), thus hindering anti-tumor immunity and upregulating
IBL was the 75th percentile of IBL (100 ml), which was according vascular endothelial growth factor, which accelerated tumor
to a previous study (16). angiogenesis (33, 34). Moreover, hypoxia could promote
Perioperative blood transfusion might affect the genome instability and lead to various genetic changes, which
complications, hospital stay, short-term death, and prognosis resulted in more aggressive phenotypes of residual tumor
(11–15). However, no previous studies analyzed the effect of cells (35).
IBT on the short-term outcomes or prognosis. In this study, we Intraoperative blood transfusion was also an independent
analyzed IBT on the outcomes of CRC surgery; furthermore, predictive factor of OS. The potential hypothesis was that
PSM was conducted to minimize the bias of baseline information IBT might cause immune disturbances through transfused
and the results would be more robust after PSM. leukocytes, including changes in circulating lymphocytes, B cell
In terms of short-term outcomes, we found that larger IBL and function, suppressor T cell ratios, and helper T cells (12, 36).
IBT prolonged operation time and hospital stay, and increased Another possible interpretation was that the need for IBT was
complications. The prolonged hospital stay might be due to post- a marker for sicker patients who were more likely to have worse
operative complications, and the recovery of intestinal peristalsis prognosis than non-IBT patients (37).
Frontiers in Surgery | www.frontiersin.org 6 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
FIGURE 2 | Prognosis of IBL on patients with CRC. (A) OS; (B) DFS. OS, overall survival; DFS, disease-free survival; IBL, intraoperative blood loss; CRC,
colorectal cancer.
FIGURE 3 | Prognosis of IBT on patients with CRC before and after PSM. (A) OS before PSM; (B) DFS before PSM; (C) OS after PSM; (D) DFS before PSM. OS,
overall survival; DFS, disease-free survival; PSM, propensity score matching; IBL, intraoperative blood transfusion; CRC, colorectal cancer.
Frontiers in Surgery | www.frontiersin.org 7 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
TABLE 9 | Previous studies reporting the IBL on the outcomes of CRC patients.
References Country Sample size Cut-off IBL Patients Outcomes
Okamura (16) Japan 1,554 200 ml Stage I/III CRC IBL is associated with postoperative morbidity and survival in very
elderly CRC patients.
Tamagawa (17) Japan 1,597 200 ml Stage II/III CRC IBL was associated with significant differences in the OS and DFS of
patients with stage II/III CRC patients.
Jiang (18) China 139 250 ml CRLM IBL during CRLM resection is an independent predictor of long term
survival and tumor recurrence.
Saleh (19) United Kingdom 65 50 ml, 150 ml CRC IBL was not associated with increased median length of stay nor did
it increase the 30 day re-admission rate.
Egenvall (20) Sweden 1,843 450 ml, 800 ml, 1400 ml RC Major blood loss during surgery for RC increases the risk of later
surgery for small bowel obstruction caused by tumor recurrence and
surgical complications, but overall survival is not affected.
Shibutani (25) Japan 277 100 ml Stage II/III CRC IBL was associated with poor long-term survival.
Mörner (26) Sweden 3,554 250 ml CC IBL during surgery for colon cancer is an independent risk factor for
later surgery for small bowel obstruction caused by tumor
recurrence.
Mörner (27) Sweden 3,062 250 ml CC IBL during surgery for colon cancer is a factor that influences
long-term survival.
CRC, colorectal cancer; IBL, intraoperative blood loss; CC, colon cancer; OS, overall survival; DFS, disease-free survival; CRLM, colorectal cancer liver metastasis; RC, rectal cancer.
There were some limitations in this study. First, this was a of Chongqing Medical University. The patients/participants
single-center retrospective study, which might cause selection provided their written informed consent to participate in
bias; second, the follow-up time was relatively short and long- this study.
term follow-up is needed in the future; third, the information of
classification and differentiation of tumors was lacking; fourth,
the preoperative hemoglobin, the kind and volume of transfusion
AUTHOR CONTRIBUTIONS
were lacking as well. Therefore, larger sample size with detailed DP and BK contributed to the conception and design of the study
information and long-term follow-up should be conducted in the and wrote the first draft of the manuscript. BK organized the
following experiments. database. DP performed the statistical analysis. X-YL, Z-WL, CY,
In conclusion, larger IBL and IBT were associated with BZ, and Z-QW wrote sections of the manuscript. All authors
longer operation time, longer hospital stay, higher overall contributed to manuscript revision, read, and approved the
complications, and poorer OS. Based on the short-term outcomes submitted version.
and prognosis of IBL and IBT, surgeons should be cautious and
more careful during the operation, and they require proficient
surgical skills. FUNDING
This study was supported by Chongqing Key Diseases Research
DATA AVAILABILITY STATEMENT and Application Demonstration Program (Colorectal Cancer
The datasets used and analyzed during the current study are Prevention and Treatment Technology Research and Application
available from the corresponding author on reasonable request. Demonstration [No. 2019ZX003]).
ETHICS STATEMENT ACKNOWLEDGMENTS
The studies involving human participants were reviewed and The authors are grateful to Xun Lei for the substantial work in
approved by the Ethics Committee of the First Affiliated Hospital the statistical methods and Peng Hong for English editing.
REFERENCES Support Care Cancer. (2021) 30:2349–57. doi: 10.1007/s00520-021-0
6638-3
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer 3. Cheng YX, Tao W, Zhang H, Peng D, Wei ZQ. Does liver cirrhosis
statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide affect the surgical outcome of primary colorectal cancer surgery? a meta-
for 36 cancers in 185 countries. CA Cancer J Clin. (2018) 68:394–424. analysis. World J Surg Oncol. (2021) 19:167. doi: 10.1186/s12957-021-0
doi: 10.3322/caac.21492 2267-6
2. Zhang Y, Zhu M, Wu X, Meng Y, Pu F, Zhang M. Factors associated 4. Ma Y, Shi L, Lu P, Yao S, Xu H, Hu J, et al. Creation of a novel nomogram based
with returning to work and work ability of colorectal cancer survivors. on the direct bilirubin-to-indirect bilirubin ratio and lactate dehydrogenase
Frontiers in Surgery | www.frontiersin.org 8 April 2022 | Volume 9 | Article 837545
Kang et al. Effect of IBL on CRC
levels in resectable colorectal cancer. Front Mol Biosci. (2021) 8:751506. complications: five-year experience. Ann Surg. (2009) 250:187–96.
doi: 10.3389/fmolb.2021.751506 doi: 10.1097/SLA.0b013e3181b13ca2
5. Peng D, Cheng YX, Cheng Y. Improved overall survival of colorectal 23. Rubin DB, Thomas N. Matching using estimated propensity scores: relating
cancer under multidisciplinary team: a meta-analysis. Biomed Res Int. (2021) theory to practice. Biometrics. (1996) 52:249–64. doi: 10.2307/2533160
2021:5541613. doi: 10.1155/2021/5541613 24. Lonjon G, Boutron I, Trinquart L, Ahmad N, Aim F, Nizard R,
6. Son IT, Kim JY, Kim MJ, Kim BC, Kang BM, Kim JW. Clinical and et al. Comparison of treatment effect estimates from prospective
oncologic outcomes of laparoscopic versus open surgery in elderly patients nonrandomized studies with propensity score analysis and randomized
with colorectal cancer: a retrospective multicenter study. Int J Clin Oncol. controlled trials of surgical procedures. Ann Surg. (2014) 259:18–25.
(2021) 26:2237–45. doi: 10.1007/s10147-021-02009-4 doi: 10.1097/SLA.0000000000000256
7. Bizzoca C, Zupo R, Aquilino F, Castellana F, Fiore F, Sardone R, et al. 25. Shibutani M, Maeda K, Kashiwagi S, Hirakawa K, Ohira M. The
Video-laparoscopic versus open surgery in obese patients with colorectal impact of intraoperative blood loss on the survival after laparoscopic
cancer: a propensity score matching study. Cancers. (2021) 13:1844. surgery for colorectal cancer. Anticancer Res. (2021) 41:4529–34.
doi: 10.3390/cancers13081844 doi: 10.21873/anticanres.15264
8. Mizuno A, Kanda M, Kobayashi D, Tanaka C, Iwata N, Yamada S, et al. 26. Mörner M, Gunnarsson U, Jestin P, Egenvall M. Volume of blood loss
Adverse effects of intraoperative blood loss on long-term outcomes after during surgery for colon cancer is a risk determinant for future small bowel
curative gastrectomy of patients with stage II/III gastric cancer. Dig Surg. obstruction caused by recurrence–a population-based epidemiological study.
(2016) 33:121–8. doi: 10.1159/000443219 Langenbecks Arch Surg. (2015) 400:599–607. doi: 10.1007/s00423-015-1317-8
9. Liang YX, Guo HH, Deng JY, Wang BG, Ding XW, Wang XN, et al. Impact of 27. Mörner ME, Gunnarsson U, Jestin P, Svanfeldt M. The importance of blood
intraoperative blood loss on survival after curative resection for gastric cancer. loss during colon cancer surgery for long-term survival: an epidemiological
World J Gastroenterol. (2013) 19:5542–50. doi: 10.3748/wjg.v19.i33.5542 study based on a population based register. Ann Surg. (2012) 255:1126–8.
10. Kamei T, Kitayama J, Yamashita H, Nagawa H. Intraoperative blood doi: 10.1097/SLA.0b013e3182512df0
loss is a critical risk factor for peritoneal recurrence after curative 28. Angele MK, Faist E. Clinical review: immunodepression in the surgical
resection of advanced gastric cancer. World J Surg. (2009) 33:1240–6. patient and increased susceptibility to infection. Crit Care. (2002) 6:298–305.
doi: 10.1007/s00268-009-9979-4 doi: 10.1186/cc1514
11. McSorley ST, Tham A, Dolan RD, Steele CW, Ramsingh J, Roxburgh C, 29. Hoynck van Papendrecht MA, Busch OR, Jeekel J, Marquet RL. The influence
et al. Perioperative blood transfusion is associated with postoperative systemic of blood loss on tumour growth: effect and mechanism in an experimental
inflammatory response and poorer outcomes following surgery for colorectal model. Neth J Surg. (1991) 43:85–8.
cancer. Ann Surg Oncol. (2020) 27:833–43. doi: 10.1245/s10434-019-0 30. Katz SC, Shia J, Liau KH, Gonen M, Ruo L. Operative blood loss independently
7984-7 predicts recurrence and survival after resection of hepatocellular carcinoma.
12. Wu HL, Tai YH, Lin SP, Chan MY, Chen HH, Chang KY. The impact of Ann Surg. (2009) 249:617–23. doi: 10.1097/SLA.0b013e31819ed22f
blood transfusion on recurrence and mortality following colorectal cancer 31. Abraham E, Chang YH. Effects of hemorrhage on inflammatory response.
resection: a propensity score analysis of 4,030 patients. Sci Rep. (2018) 8:13345. Arch Surg. (1984) 119:1154–7. doi: 10.1001/archsurg.1984.01390220040009
doi: 10.1038/s41598-018-31662-5 32. Abraham E, Lee RJ, Chang YH. The role of interleukin 2 in hemorrhage-
13. Skånberg J, Lundholm K, Haglind E. Effects of blood transfusion with induced abnormalities of lymphocyte proliferation. Circ Shock. (1986) 18:205–
leucocyte depletion on length of hospital stay, respiratory assistance and 13.
survival after curative surgery for colorectal cancer. Acta Oncol. (2007) 33. Leo C, Giaccia AJ, Denko NC. The hypoxic tumor microenvironment
46:1123–30. doi: 10.1080/02841860701441830 and gene expression. Semin Radiat Oncol. (2004) 14:207–14.
14. Nanji S, Mir ZM, Karim S, Brennan KE, Patel SV, Merchant SJ, et al. doi: 10.1016/j.semradonc.2004.04.007
Perioperative blood transfusion and resection of colorectal cancer liver 34. Shibutani M, Nakao S, Maeda K, Nagahara H, Fukuoka T. Inflammation
metastases: outcomes in routine clinical practice. HPB. (2021) 23:404–12. caused by surgical stress has a negative impact on the long-term survival
doi: 10.1016/j.hpb.2020.06.014 outcomes in patients with colorectal cancer. Anticancer Res. (2020) 40:3535–
15. Qiu L, Wang DR, Zhang XY, Gao S, Li XX, Sun GP, et al. Impact 42. doi: 10.21873/anticanres.14342
of perioperative blood transfusion on immune function and prognosis 35. Reynolds TY, Rockwell S, Glazer PM. Genetic instability induced by the tumor
in colorectal cancer patients. Transfus Apher Sci. (2016) 54:235–41. microenvironment. Cancer Res. (1996) 56:5754–7.
doi: 10.1016/j.transci.2015.07.004 36. Weber RS, Jabbour N, Martin RC 2nd. Anemia and transfusions in
16. Okamura R, Hida K, Hasegawa S, Sakai Y, Hamada M, Yasui M, et al. Impact patients undergoing surgery for cancer. Ann Surg Oncol. (2008) 15:34–45.
of intraoperative blood loss on morbidity and survival after radical surgery for doi: 10.1245/s10434-007-9502-9
colorectal cancer patients aged 80 years or older. Int J Colorectal Dis. (2016) 37. Tachibana M, Tabara H, Kotoh T, Kinugasa S, Dhar DK, Hishikawa
31:327–34. doi: 10.1007/s00384-015-2405-5 Y, et al. Prognostic significance of perioperative blood transfusions in
17. Tamagawa H, Numata M, Aoyama T, Kazama K, Atsumi Y, Iguchi K, et al. resectable thoracic esophageal cancer. Am J Gastroenterol. (1999) 94:757–65.
Impact of intraoperative blood loss on the survival of patients with stage II/III doi: 10.1111/j.1572-0241.1999.00948.x
colorectal cancer: a multicenter retrospective study. in vivo. (2021) 35:3483–8.
doi: 10.21873/invivo.12649 Conflict of Interest: The authors declare that the research was conducted in the
18. Jiang W, Fang YJ, Wu XJ, Wang FL, Lu ZH, Zhang RX, et al. absence of any commercial or financial relationships that could be construed as a
Intraoperative blood loss independently predicts survival and recurrence after potential conflict of interest.
resection of colorectal cancer liver metastasis. PLoS ONE. (2013) 8:e76125.
doi: 10.1371/journal.pone.0076125 Publisher’s Note: All claims expressed in this article are solely those of the authors
19. Saleh A, Ihedioha U, Babu B, Evans J, Kang P. Is estimated intra- and do not necessarily represent those of their affiliated organizations, or those of
operative blood loss a reliable predictor of surgical outcomes in
the publisher, the editors and the reviewers. Any product that may be evaluated in
laparoscopic colorectal cancer surgery? Scott Med J. (2016) 61:167–70.
this article, or claim that may be made by its manufacturer, is not guaranteed or
doi: 10.1177/0036933015597174
20. Egenvall M, Mörner M, Påhlman L, Gunnarsson U. Degree of blood loss endorsed by the publisher.
during surgery for rectal cancer: a population-based epidemiologic study Copyright © 2022 Kang, Liu, Li, Yuan, Zhang, Wei and Peng. This is an open-access
of surgical complications and survival. Colorectal Dis. (2014) 16:696–702. article distributed under the terms of the Creative Commons Attribution License (CC
doi: 10.1111/codi.12630 BY). The use, distribution or reproduction in other forums is permitted, provided
21. Weiser MR. AJCC 8th edition: colorectal cancer. Ann Surg Oncol. (2018) the original author(s) and the copyright owner(s) are credited and that the original
25:1454–5. doi: 10.1245/s10434-018-6462-1 publication in this journal is cited, in accordance with accepted academic practice.
22. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, No use, distribution or reproduction is permitted which does not comply with these
Schulick PD, et al. The Clavien-Dindo classification of surgical terms.
Frontiers in Surgery | www.frontiersin.org 9 April 2022 | Volume 9 | Article 837545
You might also like
- The Four Functions of ForceDocument5 pagesThe Four Functions of ForceDeywisson Ronaldo De SouzaNo ratings yet
- NCP (PEDIA Tonsillitis)Document2 pagesNCP (PEDIA Tonsillitis)Athena Kabigting64% (14)
- FormISR 1 Register Change PAN & KYC DetailsDocument2 pagesFormISR 1 Register Change PAN & KYC DetailsMd AlamgirNo ratings yet
- Ümumġ Sinaq Ġmtahani 4: Adı: Soyadı: ĠV SeriyaDocument9 pagesÜmumġ Sinaq Ġmtahani 4: Adı: Soyadı: ĠV SeriyaNigar MemmedovaNo ratings yet
- History: Important DaysDocument3 pagesHistory: Important DaysVARATHAPANDIAN GNo ratings yet
- B-Administrative PerformanceDocument7 pagesB-Administrative PerformanceJanine Marie BalladaresNo ratings yet
- J Thorsurg 2018 09 002Document17 pagesJ Thorsurg 2018 09 002zarathosNo ratings yet
- Perceptual DisordersDocument40 pagesPerceptual Disordersisos.mporei.vevaios.0% (1)
- Placement Brochure PDFDocument52 pagesPlacement Brochure PDF中华人民共和国Xi JinpingNo ratings yet
- Wi Resume-ApplicationDocument2 pagesWi Resume-ApplicationRichverr LovelyNo ratings yet
- Experiment With Truths-FinalsDocument71 pagesExperiment With Truths-FinalsShaurya JenaNo ratings yet
- National COVID-19 TERTIARY BURSARY CONFIRMATION LETTERDocument6 pagesNational COVID-19 TERTIARY BURSARY CONFIRMATION LETTERmoshibudi georginaNo ratings yet
- Outdoor Weekend Opens This Friday: Tri-City TimesDocument26 pagesOutdoor Weekend Opens This Friday: Tri-City TimesWoodsNo ratings yet
- A New Kinetic Model For Pyrolysis of Athabasca BitumenDocument13 pagesA New Kinetic Model For Pyrolysis of Athabasca BitumenMejbahul SarkerNo ratings yet
- Uptake of Long Acting Reversible Contraceptives Among Post Abortion Clients in Sargodha, PakistanOriginal ArticleDocument13 pagesUptake of Long Acting Reversible Contraceptives Among Post Abortion Clients in Sargodha, PakistanOriginal ArticleSaadiaNo ratings yet
- Insurer Market PowerDocument7 pagesInsurer Market PowerTom BiusoNo ratings yet
- Project Report On Retail BankingDocument42 pagesProject Report On Retail Bankingprasad alahitNo ratings yet
- (Chapter-3) Simranjeet KaurDocument13 pages(Chapter-3) Simranjeet KaurBest Hindi Poetry And Hindi Songs100% (1)
- Standard and Non Standard Lexicon in Aviation EnglishDocument1 pageStandard and Non Standard Lexicon in Aviation EnglishRamsey FerrerNo ratings yet
- Utilization of Primary Health Care Services in Rural and Urban Areas in ShirazDocument10 pagesUtilization of Primary Health Care Services in Rural and Urban Areas in ShirazNamarig IzzaldinNo ratings yet
- 10 1016j Teln 2018 12 005Document6 pages10 1016j Teln 2018 12 005Ma. Ferimi Gleam BajadoNo ratings yet
- RhineyandCruseCh 4Document24 pagesRhineyandCruseCh 4Rodriguez RochaNo ratings yet
- Frontiers - Rheumatic Heart Valve Disease Pathophysiology and Underlying MechanismsDocument33 pagesFrontiers - Rheumatic Heart Valve Disease Pathophysiology and Underlying MechanismsJAHNELLA XYRINE PERITONo ratings yet
- July 18,2017Document3 pagesJuly 18,2017April Joy Lascuña - CailoNo ratings yet
- SodapdfDocument747 pagesSodapdfMaybelyn Rivera PagkatotohanNo ratings yet
- Beale EleanorDocument59 pagesBeale EleanorIzzati AzmanNo ratings yet
- IB Security Assistant Exam Syllabus 2022Document6 pagesIB Security Assistant Exam Syllabus 2022Mundhe SameerNo ratings yet
- Accounting and Finance Final Project PDFDocument30 pagesAccounting and Finance Final Project PDFNarmeen HasanNo ratings yet
- 1005 Aisc G1a W Shape in Strong Axis ShearDocument3 pages1005 Aisc G1a W Shape in Strong Axis ShearAaron EasleyNo ratings yet
- Practical Research 2Document8 pagesPractical Research 2Tracy SalazarNo ratings yet
- US9284314Document28 pagesUS9284314Hien nguyenNo ratings yet
- Ead A 1:: (I EtsaDocument12 pagesEad A 1:: (I EtsaEsteban LVNo ratings yet
- Day 4 Organizational StructureDocument36 pagesDay 4 Organizational StructurePhan Thu Trang K60BFNo ratings yet
- AStudyonAnalysisofStockPricesofSelectedIndustries-research GateDocument51 pagesAStudyonAnalysisofStockPricesofSelectedIndustries-research GateAvicena Ilham GhifarieNo ratings yet
- PILLARDocument7 pagesPILLARLorelyn de la TorreNo ratings yet
- Pyhsics ch-6 MCQDocument22 pagesPyhsics ch-6 MCQVlogger lifeNo ratings yet
- A Novel Lattice Structure For SL Investment Casting PatternsDocument10 pagesA Novel Lattice Structure For SL Investment Casting PatternsNicola MerzagoraNo ratings yet
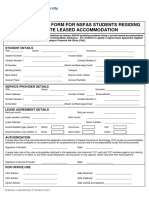
- NSFAS-Leased-applicationForm 2Document3 pagesNSFAS-Leased-applicationForm 2Alex SanchezNo ratings yet
- Deep RL For BiologyDocument33 pagesDeep RL For BiologyMarcello BarylliNo ratings yet
- Jurnal Kepimpinan Pendidikan - : Key Performance Indicators Tugas, Ganjaran Dan Prestasi KerjaDocument23 pagesJurnal Kepimpinan Pendidikan - : Key Performance Indicators Tugas, Ganjaran Dan Prestasi Kerjamohanneswaran ramasamyNo ratings yet
- The Chinese Economy Infra Driven ReboundDocument8 pagesThe Chinese Economy Infra Driven ReboundAruNo ratings yet
- Noncontingent ReinforcementDocument2 pagesNoncontingent ReinforcementAnna KrauzeNo ratings yet
- ziz/ /siz/ /ziz/ /ziz/ /S/ /S/ /K/ /S/: Practice Test 5 Time Allotted: 60 MinDocument3 pagesziz/ /siz/ /ziz/ /ziz/ /S/ /S/ /K/ /S/: Practice Test 5 Time Allotted: 60 MinMôn MônNo ratings yet
- Aavas Q4FY21 ResultsDocument16 pagesAavas Q4FY21 ResultsdarshanmaldeNo ratings yet
- Research Paper Reconstructing Forest Ecosystem On Mined Outlands RevDocument17 pagesResearch Paper Reconstructing Forest Ecosystem On Mined Outlands RevLeo DoeNo ratings yet
- Prospects and Potential of Tourism in Chinta Valley, Bhaderwah, Doda, Jammu and KahmirDocument6 pagesProspects and Potential of Tourism in Chinta Valley, Bhaderwah, Doda, Jammu and KahmirEditor IJTSRDNo ratings yet
- 2k21 A13 61 Chem Exp1Document7 pages2k21 A13 61 Chem Exp1Aryan KapurNo ratings yet
- Karim 2020Document15 pagesKarim 2020Astri SuyataNo ratings yet
- Transition Plan - Plan A and Plan BDocument10 pagesTransition Plan - Plan A and Plan Bapi-631400099No ratings yet
- Man Know Thyself PortDocument38 pagesMan Know Thyself Portkarin_86944598No ratings yet
- Booklist 01 May 2022Document70 pagesBooklist 01 May 2022januszNo ratings yet
- FILM330 Problems 2Document5 pagesFILM330 Problems 2Raisya febiyaneeeNo ratings yet
- Retail GroceriesDocument6 pagesRetail Groceriessharan shariNo ratings yet
- 1 s2.0 S014067362300020X MainDocument14 pages1 s2.0 S014067362300020X MainGERIATRIA 72No ratings yet
- Digital Economy and Sustainable Use of Resources A Case Study of Saudi ArabiaDocument9 pagesDigital Economy and Sustainable Use of Resources A Case Study of Saudi ArabiaInternational Journal of Advance Study and Research WorkNo ratings yet
- Jilla B. Alvarado P.E. 3 Answer SheetsDocument4 pagesJilla B. Alvarado P.E. 3 Answer SheetsWhencell Ann RomblonNo ratings yet
- 236178-Cataloge of The Pictures (1892) - TextDocument260 pages236178-Cataloge of The Pictures (1892) - Textacademo misirNo ratings yet
- Rbi Irac Norms Circular PDFDocument138 pagesRbi Irac Norms Circular PDFCA Nikhil BazariNo ratings yet
- LittleTybee50yrManagementPlan SignedDocument73 pagesLittleTybee50yrManagementPlan SignedMary LandersNo ratings yet
- Music1-Second QuarterDocument42 pagesMusic1-Second QuarterZairah Lyn SaysonNo ratings yet
- Wjgo 14 1199Document12 pagesWjgo 14 1199juan uribeNo ratings yet
- DCR 64 1471Document8 pagesDCR 64 1471juan uribeNo ratings yet
- Wjgo 14 1199Document12 pagesWjgo 14 1199juan uribeNo ratings yet
- In - Vivo 35 3483Document6 pagesIn - Vivo 35 3483juan uribeNo ratings yet
- Chronic Effects of High Intensity Functional Training On Motor Function: A Systematic Review With Multilevel Meta AnalysisDocument13 pagesChronic Effects of High Intensity Functional Training On Motor Function: A Systematic Review With Multilevel Meta Analysisjuan uribeNo ratings yet
- Fspor 04 1073223Document16 pagesFspor 04 1073223juan uribeNo ratings yet
- Usy 274Document9 pagesUsy 274juan uribeNo ratings yet
- An 8-Year Longitudinal Study of Overreaching in 114 Elite Female Chinese WrestlersDocument7 pagesAn 8-Year Longitudinal Study of Overreaching in 114 Elite Female Chinese Wrestlersjuan uribeNo ratings yet
- Ijms 23 15700Document12 pagesIjms 23 15700juan uribeNo ratings yet
- JBS 40 112086Document12 pagesJBS 40 112086juan uribeNo ratings yet
- JBS 39 109453Document9 pagesJBS 39 109453juan uribeNo ratings yet
- Full Chapter A Planet of Viruses Third Edition Zimmer PDFDocument53 pagesFull Chapter A Planet of Viruses Third Edition Zimmer PDFrichard.robison345100% (5)
- Effective Hemodynamic Monitoring 2Document10 pagesEffective Hemodynamic Monitoring 2Shirley castañedaNo ratings yet
- Achilles Tendinopathy What Runners Should Know FinitoDocument4 pagesAchilles Tendinopathy What Runners Should Know FinitoAdmirNo ratings yet
- Case Scenario Mohsen SaadDocument6 pagesCase Scenario Mohsen SaadIbrahim HemdanNo ratings yet
- Ahmed Project YSU (1) FINAL EDITION 2016 2017-1Document28 pagesAhmed Project YSU (1) FINAL EDITION 2016 2017-1Yakubu Adamu JajereNo ratings yet
- IELTS Reading Test 4: Section 1Document64 pagesIELTS Reading Test 4: Section 1rguy5866No ratings yet
- Major Case Study Presentation SlidesDocument51 pagesMajor Case Study Presentation Slidesapi-640180401No ratings yet
- Semi Detailed Lesson Plan Eed Tle 2Document7 pagesSemi Detailed Lesson Plan Eed Tle 2Lopez Rhen DaleNo ratings yet
- Helping Patient With WoundDocument3 pagesHelping Patient With WoundSevina Eka ChannelNo ratings yet
- Public Speaking TextDocument2 pagesPublic Speaking TextNUR HANANI BINTI YUSUFF KPM-GuruNo ratings yet
- A Systematic Review of Running-Related Musculoskeletal Injuries in RunnersDocument10 pagesA Systematic Review of Running-Related Musculoskeletal Injuries in RunnersInfo-qe QualityenergyNo ratings yet
- Chronic DiseaseDocument13 pagesChronic DiseaseDanielle MadeNo ratings yet
- A Study On Molecular Diagnosis of Theileria Species Infection by PCR Amplification in Sheep and Goats in Multan, PakistanDocument10 pagesA Study On Molecular Diagnosis of Theileria Species Infection by PCR Amplification in Sheep and Goats in Multan, PakistanAhmad RazaNo ratings yet
- Case Study 1Document28 pagesCase Study 1Sean Carl TubilNo ratings yet
- Shoulder Orthosis - DevadriDocument18 pagesShoulder Orthosis - DevadriDevadri DeyNo ratings yet
- Imci Introduction Danger Signs 2023Document61 pagesImci Introduction Danger Signs 2023Nathaniel NograNo ratings yet
- TheileriosisDocument10 pagesTheileriosisSomesh SharmaNo ratings yet
- The No. Most Ignored Disease: Thyroid Troubles Skyrocket As You AgeDocument16 pagesThe No. Most Ignored Disease: Thyroid Troubles Skyrocket As You AgeemagooNo ratings yet
- Clinical Versus Actuarial Judgment: Methods of Judgment and Means of ComparisonDocument19 pagesClinical Versus Actuarial Judgment: Methods of Judgment and Means of ComparisonanguschandlerNo ratings yet
- Oral Health in PregnancyDocument6 pagesOral Health in PregnancyTamara Al KautsarNo ratings yet
- Novartis: Strategic Alliance of NovartisDocument8 pagesNovartis: Strategic Alliance of NovartisHARSHIT KUMAR SRIVASTAVANo ratings yet
- NCP & Imci Case ManagementDocument6 pagesNCP & Imci Case ManagementElizabeth ZamoraNo ratings yet
- Flexible Contribution Tenure With 25 Years of Protection: HSBC Takaful Future SmartDocument6 pagesFlexible Contribution Tenure With 25 Years of Protection: HSBC Takaful Future SmartmiazainuddinNo ratings yet
- OSTEOMALACIADocument16 pagesOSTEOMALACIAlibrian_pallavi39420% (1)
- Dermatology QuestionsDocument3 pagesDermatology QuestionsMuziki Wa KiafrikaNo ratings yet
- Ergotherapy, The Occupational Therapy As An Aid To Return To Being by DoingDocument20 pagesErgotherapy, The Occupational Therapy As An Aid To Return To Being by DoingAnthony El HageNo ratings yet
- Elephant's Ear Sign PDFDocument3 pagesElephant's Ear Sign PDFana starcevicNo ratings yet
- Target Paper - Xi Zoology by Sir MuneebDocument3 pagesTarget Paper - Xi Zoology by Sir MuneebmahmadwasiNo ratings yet
- Compound RX Form PDFDocument1 pageCompound RX Form PDFGordon FagrasNo ratings yet