Professional Documents
Culture Documents
Metabolic Syndrome: A Psychiatric Outlook
Metabolic Syndrome: A Psychiatric Outlook
Uploaded by
JAVED ATHER SIDDIQUIOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metabolic Syndrome: A Psychiatric Outlook
Metabolic Syndrome: A Psychiatric Outlook
Uploaded by
JAVED ATHER SIDDIQUICopyright:
Available Formats
REVIEW
Psychosomatic Medicine Research 2023;5(1):1. https://doi.org/10.53388/PSMR2023001
Metabolic syndrome: a psychiatric outlook
Javed Ather Siddiqui1, 3*, Shazia Farheen Qureshi2, 3, Ibrahim Mohammed Alghamdi3, Hani Matrok Alotaibi3
1
Department of Psychiatry, Seth Gordhandas Sunderdas Medical College and the King Edward Memorial Hospital, Mumbai 400012, India. 2Department of
Psychiatry, College of Physicians and Surgeons of Bombay, Mumbai 400012, India. 3Department of Psychiatry, Mental Health Hospital, Taif 21944, Saudi Arabia.
*
Corresponding to: Javed Ather Siddiqui, Department of Psychiatry, Seth Gordhandas Sunderdas Medical College and the King Edward Memorial Hospital,
Acharya Donde Street, Parel, Mumbai 400012, India. E-mail: javedsiddiqui2000@gmail.com.
Author contributions Abstract
Javed Ather Siddiqui and Shazia Farheen Qureshi contributed A metabolic syndrome is a cluster of clinical signs that are risk factors for the development
to the acquisition data and manuscript writing. Ibrahim of type 2 diabetes mellitus, and cardiovascular disease. This cluster includes obesity,
Mohammed Alghamdi and Hani Matrok Alotaibi assisted with elevated blood sugar, high blood pressure, and high cholesterol. Atypical antipsychotics that
data acquisition and revised the manuscript. are associated with a group of signs and symptoms have resulted in an increased focus on
Competing interests this syndrome.
The authors declare no conflicts of interest. This review included accessible literature, such as review articles and original research
Acknowledgments articles. It provides useful guidelines for psychiatrists and gives them psycho-education so
This research received no specific grant from any funding that they can identify and monitor patients who may have the syndrome and properly
agency in the public, commercial, or not-for-profit sectors. manage it.
Abbreviations
Met-S, metabolic syndrome; HPA, hypothalamic –pituitary – Keywords: metabolic syndrome; psychotropic medications; obesity
adrenal; GLP-1, glucagon-like peptide-1; GIP,
glucose-dependent insulinotropic peptide.
Citation
Siddiqui JA, Qureshi SF, Alghamdi IM, Alotaibi HM. Metabolic
syndrome: a psychiatric outlook. Psychosom Med Res.
2023;5(1):1. doi: 10.53388/PSMR2023001.
Executive editor: Peng-Xiao Wang.
Received: 02 December 2022; Accepted: 18 January 2023;
Available online: 14 February 2023.
© 2023 By Author(s). Published by TMR Publishing Group
Limited. This is an open access article under the CC-BY license.
(https://creativecommons.org/licenses/by/4.0/)
Submit a manuscript: https://www.tmrjournals.com/psmr 1
REVIEW
Psychosomatic Medicine Research 2023;5(1):1. https://doi.org/10.53388/PSMR2023001
Introduction According to this process, weight gain occurs when people consume
more food while blocking the satiety signal, which causes insulin
The metabolic syndrome (Met-S) is a group of disorders that increases resistance, hyperlipidemia, and the development of the metabolic
the risk of heart disease, type 2 diabetes mellitus, and stroke. Excess syndrome [12].
body fat around the waist, high blood pressure, high blood sugar, and
abnormal cholesterol or triglyceride levels are all symptoms of this Risk factors for metabolic syndrome in psychiatric disorder
syndrome [1]. Although psychotropic medicines are one of the risk In psychiatric patients, metabolic syndrome has a variety of causes
factors for the development of metabolic syndrome, the specific and risk factors. Psychotropic medicines, including second-generation
etiology of antipsychotic-induced metabolic disturbances remains or atypical antipsychotics, as well as mood stabilizers, are known risk
uncertain. When prescribing antipsychotics, doctors do not screen for factors. Excessive smoking, excessive alcohol intake, a lack of physical
or treat metabolic syndrome, and the majority of psychiatrists do not activity, poor sleep hygiene, and unhealthy food habits may all lead to
believe that they should be the ones to address cardio-metabolic Met-S [13]. Met-S also gives out biological variables, including
abnormalities. Despite the fact that diagnostic criteria differ, the hypothalamic–pituitary–adrenal (HPA) axis dysfunction and insulin
condition is defined by visceral obesity, and impaired insulin resistance. Another genetic risk factor is the presence of specific genes
metabolism. A patient has Met-S if they have at least three of the linked to a metabolic propensity, as well as polymorphisms in the
following conditions as part of the adult treatment program (ATT 3): leptin and melanocortin pathways, which contribute to heterogeneity
hypertension, abdominal obesity as measured by 102 centimeters (38 in antipsychotic-induced weight gain. There are also hormonal
inches) for men and 88 centimeters (34 inches) for women. In men, abnormalities related to cortisol and leptin levels that contribute to
triglyceride levels must be greater than 150 milligrams per deciliter the condition.
and lower than 59 milligrams per deciliter in women, and fasting Psychiatric disorders are associated with metabolic syndrome not
glucose levels must exceed 110 milligrams per deciliter. only because of psychotropic drugs, but also because of genetic
polymorphisms, inflammation, endocrinopathies, and unhealthy
Psychotropic medications and the metabolic syndrome lifestyles. A number of risk factors contribute to metabolic syndrome
in chronic psychiatric illness, such as genetics, excessive alcohol
The relationship between psychotropic medications and the consumption, food imbalance and poor eating habits, sedentary
metabolic syndrome lifestyles, hormonal imbalances affecting cortisol and leptin, sedentary
Antipsychotics of the newer generation, notably the second generation lifestyles, and second-generation antipsychotics that may have side
(atypical antipsychotics), are frequently linked to an elevated risk of effects [14].
metabolic syndrome, which is a major risk factor for cardiovascular
disease [2, 3]. Premature death is more common in psychiatric Antipsychotics
patients than in the general population. Psychiatric patients are Weight gain, insulin resistance, dyslipidemia, impaired glucose
typically associated with a higher risk of metabolic syndrome (Met-S), tolerance, or type 2 diabetes, and hypertension are all common side
a group of symptoms associated with cardiovascular risk factors such effects of second-generation antipsychotics. Ultimately, metabolic
as dyslipidemia, abdominal obesity, hypertension, and hyperglycemia. syndrome results from metabolic dysfunction. As antipsychotics may
Motivational interviewing can be useful to psychiatrists in lowering cause weight gain, they are not recommended as substitutes for
the risk of metabolic syndrome in patients. Other non-pharmacologic placebos. No antipsychotic can be considered fully weight-neutral
therapies can help control the deadly symptoms of Met-S. The goals of when compared to a placebo [15-17]. Second-generation
these interventions are to enhance physical activity, sleep, stress antipsychotics like clozapine and olanzapine have metabolic side
management, and nutritional supplementation. The most effective effects like diabetes and dyslipidemia, which, if not treated properly,
interventions are increased consumption of fruits, vegetables, and can lead to dangerous consequences [18]. According to the
whole grains; increased physical activity; improved sleep; and the use researchers, second-generation antipsychotics like clozapine, and
of fish oil. The risk of Met-S is elevated among all types of mental olanzapine, have the greatest potential to cause weight gain. Among
illnesses, including major depressive disorder, bipolar disorder, other antipsychotics such as quetiapine, risperidone, paliperidone, and
schizophrenia, anxiety disorder, attention-deficit hyperactivity iloperidone, there is a moderate risk of weight gain. Weight gain is
disorder, and posttraumatic stress disorder [4]. Around 20 to 25 decreased or nonexistent with aripiprazole, amisulpride, ziprasidone,
percent of the global population suffers from metabolic syndrome. asenapine, and lurasidone. Antipsychotics can cause weight gain
According to a research meta-analysis, Met-S's prevalence is 58 through a variety of mechanisms. A number of receptors, including
percent greater in mental patients than the general population [4]. In 5-HT2C, H1, and D2, are involved in the selective antagonistic action
schizophrenia patients, the prevalence of metabolic syndrome ranges of antipsychotics. The antagonism of serotonin 5-HT2C receptors
from 22.2 to 60 percent [5]. There are high incidences of type 2 increases insulin resistance and decreases glucose absorption by
diabetes mellitus seen in schizophrenia patients, ranging from 19 to skeletal muscles, increasing the risk of diabetes mellitus, whereas
30 percent, implying a hereditary link between both illnesses [6]. The histamine agonists prevent weight gain [19]. Antipsychotics also have
study found that people with bipolar mood disorder had a metabolic an anti-histaminergic effect, which means they compete with
syndrome frequency of around 30% [7]. Another study found that 36 histamine for binding sites on H1 receptors, resulting in sedation and a
percent of depression patients had metabolic syndrome, which is decrease in metabolism. Weight gain can be caused by a blockage of
associated with major depression [8]. There are specific metabolic adrenergic 1, serotonergic 5HT2 and 5-HT2C transmission, as well as
syndrome traits associated with individuals suffering from histaminergic H1 transmission of neuropeptides such as leptin and
posttraumatic stress disorder [9]. ghrelin [20].
Certain psychotropics, such as atypical antipsychotics, may raise the Researchers have interpreted that olanzapine, and clozapine
risk of Met-S by increasing weight gain or causing changes in lipid or enhance the risk of diabetes mellitus through both direct and indirect
glucose metabolism. Despite the fact that several psychiatric mechanisms, such as increasing peripheral insulin resistance and
medicines cause an increase in serum lipid levels, the researchers were promoting weight gain. Different antipsychotics are likely to produce
unable to establish a direct link between antipsychotics and hyperglycemia in a variety of ways. As an example, olanzapine is
dyslipidemia. It states that both dyslipidemia and insulin resistance linked to a 37 percent higher risk of diabetes mellitus than risperidone
are predominantly connected with mental illness [10]. Psychiatric [21]. An additional antipsychotic, clozapine, causes insulin resistance
patients in these situations require good physical education, proper due to increased levels of TNF-cytokines produced by adipocytes. In
nutrition, physical activity, and more advanced cognitive-behavioral fact, it can be used to predict obesity when certain antipsychotics are
therapy [11]. The pharmacodynamics of weight gain and insulin taken. If we focus on a single drug, olanzapine has a high propensity
resistance in psychotropics are discussed at the receptor level. to derange metabolic parameters in patients with schizophrenia. It is
Submit a manuscript: https://www.tmrjournals.com/psmr 2
REVIEW
Psychosomatic Medicine Research 2023;5(1):1. https://doi.org/10.53388/PSMR2023001
recommended that olanzapine be monitored closely and that lifestyle critical factor. It improves drug adherence as well as relapse
modifications are made in order to prevent adverse metabolic effects. prevention. Some advice for preventing clusters of Met S symptoms
According to NCEP ATP III criteria, the prevalence of Met-S before includes the correct selection of an atypical antipsychotic, counseling
initiation of olanzapine was 15.4%, and it increased to 56.9% after for behavioral or lifestyle management, early initialization, and
one year [22]. A study on drug-naive individuals found that 3.8% of preventive pharmaceutical control of risk factors. If psychiatric
participants had Met-S before initiation of Olanzapine [23]. patients suffer metabolic side effects when taking an atypical
Researchers also compared the increase to CATIE's phase 1 trial, in antipsychotic, they can switch to a low-risk atypical antipsychotic.
which the metabolic prevalence grew from 34.8% to 43.9% after three Pharmacological management of the various components of metabolic
months in patients taking olanzapine [24]. syndrome, such as weight gain, diabetes mellitus or hyperglycemia,
hypertension, and dyslipidemia, is followed by an evaluation of all
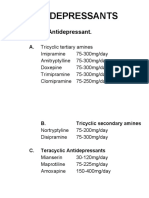
Antidepressants other drugs and substance use histories that may contribute to
According to researchers, antidepressants rarely cause metabolic metabolic syndrome. The psychiatrist should assess all metabolic
syndrome. The metabolic syndrome is more common with older parameters before beginning any intervention in order to prevent or
antidepressants like tricyclics, and it is uncommon with newer classes correct metabolic side effects from atypical antipsychotics. It is best to
of antidepressants. Insulin resistance and hypertriglyceridemia are use weight loss medications as a last resort after attempting to change
side effects of tricyclic antidepressants. The weight gain associated one's lifestyle through behavioral programs. Dieticians and weight
with tricyclics, such as amitriptyline and doxepin, has been management specialists can provide further details about diet and
documented [25]. Paykel coined the phrase "carbohydrate hunger" to exercise. Patients should also have access to holistic well-being
characterize the increased appetite seen in individuals taking tricyclic programs; enrolling patients in weight-loss support groups may
antidepressants. Distinct effects of tricyclic to noradrenergic, encourage them to stay healthy. The use of cognitive behavioral
histaminergic, it is also discovered that amitriptyline has a powerful therapy can help people eliminate negative health-related thoughts
anti-histaminergic action, and that doxepin is to blame for the weight and behaviors. The most successful technique was determined to be a
gain. Serotonin- specific reuptake inhibitors, on the other hand, due to cognitive behavioral approach combined with psychoeducation [34].
their selective action on the rise in serotonin transportation, do not These psychotherapeutic approaches are more effective than
induce a large gain in body weight. However, it can be reduced by weight-loss drugs in psychiatric patients for weight loss and diabetes
decreasing hunger. The use of antidepressants that increase body prevention, especially when used consistently throughout the
weight, such as amitriptyline, paroxetine, and mirtazapine, is not treatment program [35].
associated with a hormone like leptin. In contrast, amitriptyline and
mirtazapine raise TNF- levels, which are absent with TNF-friendly Pharmacological intervention
fluoxetine, paroxetine, and venlafaxine [25]. In patients with type 2 The main goal of pharmacological management of the metabolic
diabetes, antidepressants like fluoxetine increase insulin action. The syndrome is to treat the specific components of the syndrome, such as
risk of metabolic syndrome with serotonin-selective reuptake hypertension, dyslipidemia, and increased blood sugar.
inhibitors is very low. Antihypertensive and cholesterol-lowering medications, as well as
The link between depressive disorder and metabolic syndrome is anti-diabetic medications, can reduce the risk of cardiovascular
complicated, and numerous factors play a role. To begin with, people disease with a potentially fatal outcome. A variety of medications
with depression are less likely to adhere to dietary restrictions and are have been effective in reducing excessive weight gain caused by
more likely to be physically inactive. As a result, these patients are second generation antipsychotics, sodium valproate, ephedrine, a beta
more likely to engage in unhealthy behaviors such as smoking and adrenergic agonist combined with caffeine; orlistat, a lipase inhibitor
alcohol consumption. Obesity and insulin resistance are the results of that reduces fat reabsorption in the bowels; naloxone, an opioid
this sort of patient behavior [26, 27]. Secondly, stimulation of the antagonist that inhibits hunger; and metformin, an oral anti-diabetic
HPA axis raises plasma cortisol levels, resulting in pseudo-Cushing's drug that reduces excess weight gain caused by atypical
syndrome and other metabolic syndrome symptoms [28]. Finally, antipsychotics. An analysis of 32 randomized controlled trials on
insulin and leptin levels have increased. This can lead to an increase in pharmacological interventions for weight loss in
circulating catecholamines poor glucose metabolism, blood pressure antipsychotic-induced weight included metformin, d-fenfluramine,
regulation, and belly fat buildup, all of which can activate the sibutramine, topiramate, reboxetine, amantadine, nizatidine, orlistat,
sympathetic nervous system. [29]. Fourth, elevated levels of metformin plus sibutramine, famotidine, dextroamphetamine,
pro-inflammatory cytokines [30] and leptin [31] have been linked to fluoxetine, and rosiglitazone. Endogenous incretins such as
depressive disorder in patients with metabolic syndrome. In addition, glucagon-like peptide-1 (GLP-1), and glucose-dependent
dysfunction of the vascular endothelium can contribute to depression insulinotropic peptide (GIP) influence insulin secretion and have been
[32]. employed in the treatment of metabolic syndrome [36]. Bariatric
surgery is one of the surgical interventions that is indicated for
Mood stabilizer significantly obese people [37].
The metabolic syndrome has been linked to mood stabilizers, Conclusion
particularly lithium and sodium valproate. Others, such as sodium
valproate, can cause weight gain by increasing the level of circulating In psychiatric patients, metabolic syndrome is a serious yet
leptin. The impact is comparable to valproate when combined with under-recognized illness. Before beginning treatment with these
carbamazepine, although gabapentin and lamotrigine have no effect atypical antipsychotics, doctors should consider the possibility of
on body weight while topiramate does. According to researchers, the potential therapeutic benefits against the metabolic side effects. We
effects of lithium on glucose metabolism are inconsistent, if not also urge that practitioners give psychoeducation about the metabolic
contradictory. They claim that it improves glucose metabolism in hazards of second-generation antipsychotics to the patients and their
certain cases and reduces tolerance to glucose in others [33]. families. Researchers must develop psychotropic drugs that are less
likely to cause metabolic syndrome and assess the efficacy and safety
Management of pharmacological agents such as metformin and GLP-1 agonists on
the syndrome.
Non-pharmacological intervention
In patients with metabolic syndrome, psychiatrists must support good References
lifestyle behaviors and suitable dieting habits. The patient must be
informed about their psychiatric disease, and medications, which is a 1. De Hert M, Cohen D, Bobes J, et al. Physical illness in patients
Submit a manuscript: https://www.tmrjournals.com/psmr 3
REVIEW
Psychosomatic Medicine Research 2023;5(1):1. https://doi.org/10.53388/PSMR2023001
with severe mental disorders. II. Barriers to care, monitoring treatment. J Psychopharmacol 2017;31(11):1430–1436.
and treatment guidelines, plus recommendations at the system http://doi.org/10.1177/0269881117722987
and individual level. World Psychiatry 2011;10(2):138–151. 18. Siddiqui J, Qureshi S, Ahmed Shawosh Y. Clozapine-induced
http://doi.org/10.1002/j.2051-5545.2011.tb00036.x massive hematemesis: a rare case report. Ann Indian Psychiatry
2. De Hert MA, van Winkel R, Van Eyck D, et al. Prevalence of the 2019;3(2):171.
metabolic syndrome in patients with schizophrenia treated with http://doi.org/10.4103/aip.aip_8_19
antipsychotic medication. Schizophr Res 2006;83(1):87–93. 19. McIntyre RS, Mancini DA, Basile VS. Mechanisms of
http://doi.org/10.1016/j.schres.2005.12.855 antipsychotics-induced weight gain. J Clin Psychiatry
3. American Diabetes Association, American Psychiatric 2001;62:23–29.
Association, American Association of Clinical Endocrinologists, https://pubmed.ncbi.nlm.nih.gov/11603882/
et al. Consensus development conference on antipsychotic drugs 20. Lindenmayer JP, Nathan AM, Smith RC. Hyperglicemia
and obesity and diabetes. Diabetes care 2004;27(2):596–601. associated with the use of atypical antipsychotics. J Clin
http://doi.org/10.2337/diacare.27.2.596 Psychiatry 2001;23:30–38.
4. Vancampfort D, Stubbs B, Mitchell AJ, et al. Risk of metabolic https://pubmed.ncbi.nlm.nih.gov/11603883/
syndrome and its components in people with schizophrenia and 21. Henderson DC. Schizophrenia and commorbid metabolic
related psychotic disorders, bipolar disorder and major disorders. J Clin Psychiatry 2005;6:11–20.
depressive disorder: a systematic review and meta-analysis. https://pubmed.ncbi.nlm.nih.gov/16107179/
World Psychiatry 2015;14(3):339–347. 22. Samyukta K, Shivson D, Kantipudi SJ. Effect of Olanzapine on
http://doi.org/10.1002/wps.20252 metabolic syndrome- a one year follow-up study. J Clin
5. Meyer J, Koro CE, L’Italien GJ. The metabolic syndrome and Diagnostic Res 2020;14(6):VC01–VC04.
schizophrenia: a review. Int Rev Psychiatry 2005;17(3):173–180. http://doi.org/10.7860/JCDR/2020/44521.13773
http://doi.org/10.1080/09540260500071798 23. Padmavati R, McCreadie RG, Tirupati S. Low prevalence of
6. Thakore JH. Metabolic syndrome and schizophrenia. Br J obesity and metabolic syndrome in never-treated chronic
Psychiatry 2005;186(6):455–456. schizophrenia. Schizophr Res 2010;121(1–3):199–202.
http://doi.org/10.1192/bjp.186.6.455 http://doi.org/10.1016/j.schres.2010.05.010
7. Fagiolini A, Frank E, Scott JA, Turkin S, Kupfer DJ. Metabolic 24. Meyer JM, Davis VG, Goff DC, et al. Change in metabolic
syndrome in bipolar disorder: findings from the Bipolar syndrome parameters with antipsychotic treatment in the
Disorder Center for Pennsylvanians. Bipolar Disord CATIE schizophrenia trial: prospective data from phase 1.
2005;7(5):424–430. Schizophr Res 2008;101(1–3):273–386.
http://doi.org/10.1111/j.1399-5618.2005.00234.x http://doi.org/10.1016/j.schres.2007.12.487
8. Heiskanen TH, Niskanen LK, Hintikka JJ, et al. Metabolic 25. Chokka P, Tancer M, Yeragani VK. Metabolic syndrome:
syndrome and depression: a cross-sectional analysis. J Clin relevance to antidepressant treatment. J Psychiatry Neurosci
Psychiatry 2006;67(9):1422–1427. 2006;31(6):414.
http://doi.org/10.4088/JCP.v67n0913 https://pubmed.ncbi.nlm.nih.gov/17136222/
9. Vieweg WVR, Julius DA, Fernandez A, Tassone DM, Narla SN, 26. Attvall S, Fowelin J, Lager I, Schenck H, Smith U. Smoking
Pandurangi AK. Posttraumatic stress disorder in male military induces insulin resistance-a potential link with the insulin
veterans with comorbid overweight and obesity. Prim Care resistance syndrome. J Intern Med 1993;233(4):327–332.
Companion J Clin Psychiatry 2006;8(1):25–31. http://doi.org/10.1111/j.1365-2796.1993.tb00680.x
http://doi.org/10.4088/PCC.v08n0104 27. Jelski W, Szmitkowski M. Effect of ethanol on metabolic
10. Muldoon MF, Mackey RH, Korytkowski MT, Flory JD, Pollock syndrome. Pol Arch Intern Med 2007;117(7):306–311.
BG, Manuck SB. The metabolic syndrome is associated with http://doi.org/10.20452/pamw.164
reduced central serotonergic responsivity in healthy community 28. Björntorp P, Rosmond R. The metabolic syndrome — a
volunteers. J Clin Endocrinol Metab 2006;91(2):718–721. neuroendocrine disorder? Br J Nutr 2000;83(S1):S49–S57.
http://doi.org/10.1210/jc.2005-1654 http://doi.org/10.1017/S0007114500000957
11. Aronne LJ. Epidemiology, morbidity and treatment of 29. Musselman DL, Evans DL, Nemeroff CB. The relationship of
overweight and obesity. J Clin Psychiatry 2001;62:13–22. depression to cardiovascular disease. Arch Gen Psychiatry
https://pubmed.ncbi.nlm.nih.gov/11603881/ 1998;55(7):580.
12. McIntyre RS, Mancini DA, Basile VS. Mechanisms of http://doi.org/10.1001/archpsyc.55.7.580
antipsychotics-induced weight gain. J Clin Psychiatry 30. Howren MB, Lamkin DM, Suls J. Associations of depression with
2001;62:23–29. c-reactive Protein, IL-1, and IL-6: a meta-analysis. Psychosom
https://pubmed.ncbi.nlm.nih.gov/11603882/ Med 2009;71(2):171–186.
13. Connolly M, Kelly C. Lifestyle and physical health in http://doi.org/10.1097/PSY.0b013e3181907c1b
schizophrenia. Adv psychiatr treat 2005;11(2):125–132. 31. Patel SB, Reams GP, Spear RM, Freeman RH, Villarreal D.
http://doi.org/10.1192/apt.11.2.125 Leptin: linking obesity, the metabolic syndrome, and
14. Ho CSH, Zhang MWB, Mak A, Ho RCM. Metabolic syndrome in cardiovascular disease. Current Science Inc 2008;10(2):131–137.
psychiatry: advances in understanding and management. Adv http://doi.org/10.1007/s11906-008-0025-y
psychiatr treat 2014;20(2):101–112. 32. Bench CJ, Friston KJ, Brown RG, Scott LC, Frackowiak RSJ,
http://doi.org/10.1192/apt.bp.113.011619 Dolan RJ. The anatomy of melancholia – focal abnormalities of
15. Bak M, Fransen A, Janssen J, van Os J, Drukker M. Almost all cerebral blood flow in major depression. Psychol Med
antipsychotics result in weight gain: a meta-analysis. PLoS One 1992;22(3):607–615.
2014;9(4):e94112. http://doi.org/10.1017/S003329170003806X
http://doi.org/10.1371/journal.pone.0094112 33. Chang HH, Chou CH, Chen PS, et al. High prevalence of
16. Correll CU, Detraux J, Lepeleire JD, Hert MD. Effects of metabolic disturbances in patients with bipolar disorder in
antipsychotics, antidepressants and mood stabilizers on risk for Taiwan. J Affect Disord 2009;117(1–2):124–129.
physical diseases in people with schizophrenia, depression and http://doi.org/10.1016/j.jad.2008.12.018
bipolar disorder. World Psychiatry 2015;14(2):119–136. 34. Weber M, Wyne K. A cognitive/behavioral group intervention
http://doi.org/10.1002/wps.20204 for weight loss in patients treated with atypical antipsychotics.
17. Reynolds GP, McGowan OO. Mechanisms underlying metabolic Schizophr Res 2006;83(1):95–101.
disturbances associated with psychosis and antipsychotic drug http://doi.org/10.1016/j.schres.2006.01.008
Submit a manuscript: https://www.tmrjournals.com/psmr 4
REVIEW
Psychosomatic Medicine Research 2023;5(1):1. https://doi.org/10.53388/PSMR2023001
35. De Hert M, Schreurs V, Vancampfort D, Van Winkel R. 2011;124(1):S3–S18.
Metabolic syndrome in people with schizophrenia: a review. http://doi.org/10.1016/j.amjmed.2010.11.002
World Psychiatry 2009;8(1):15–22. 37. Blackburn GL, Hutter MM, Harvey AM, et al. Expert panel on
http://doi.org/10.1002/j.2051-5545.2009.tb00199.x weight loss surgery: executive report update. Obesity
36. Nauck MA. Incretin-based therapies for type 2 diabetes mellitus: 2009;17(5):842–862.
properties, functions, and clinical implications. Am J Med http://doi.org/10.1038/oby.2008.578
Submit a manuscript: https://www.tmrjournals.com/psmr 5
You might also like
- Handbook For Advanced Teaching - Fundamentals of HomeopathyDocument137 pagesHandbook For Advanced Teaching - Fundamentals of HomeopathySuharikaNo ratings yet
- Nosodes Sarcodes HomeopathyDocument35 pagesNosodes Sarcodes HomeopathydrdivishNo ratings yet
- Homeopathy Answer KeyDocument16 pagesHomeopathy Answer Keyokta yuliawatiNo ratings yet
- MaanDocument6 pagesMaanIon BogdanNo ratings yet
- FBCA Biomarkers and ConditionsDocument8 pagesFBCA Biomarkers and Conditionsmet50% (2)
- Chapter 13 Quiz For Health Psychology 328 McgillDocument3 pagesChapter 13 Quiz For Health Psychology 328 McgillOlivia CoutoNo ratings yet
- (Simpo 2 Dr. Sally) - Sindrom MetabolikDocument57 pages(Simpo 2 Dr. Sally) - Sindrom MetabolikYosefin RatnaningtyasNo ratings yet
- 2.mood Disorder TreatmentDocument56 pages2.mood Disorder TreatmentREDEEM NNo ratings yet
- Depressive DisorderDocument59 pagesDepressive DisorderJoshua RingorNo ratings yet
- Steven Johnson SyndromeDocument70 pagesSteven Johnson SyndromeAiram P NatingaNo ratings yet
- Barbiturate Benzodiazepine PoisoningDocument23 pagesBarbiturate Benzodiazepine PoisoningRoman MamunNo ratings yet
- Schizophrenia PPT FinalDocument34 pagesSchizophrenia PPT FinalitishreeNo ratings yet
- Theories of Disease CausationDocument16 pagesTheories of Disease CausationkenmanikeseNo ratings yet
- Done by: فآكلا ماسح هنبابع دامع حدحداب رمع جارس ديجملا دبع ةلزغ وبا داهجDocument23 pagesDone by: فآكلا ماسح هنبابع دامع حدحداب رمع جارس ديجملا دبع ةلزغ وبا داهجRashedNo ratings yet
- EndometriosisDocument4 pagesEndometriosislokesh_arya1No ratings yet
- Hpathy Psoriasis in A Man of 38Document20 pagesHpathy Psoriasis in A Man of 38Muhammad ArshadNo ratings yet
- Schizophrenia and Other Psychoses: Psychosis - Is A Disruptive Mental State inDocument7 pagesSchizophrenia and Other Psychoses: Psychosis - Is A Disruptive Mental State inDhen MarcNo ratings yet
- Antidepressants: I. Cyclic AntidepressantDocument17 pagesAntidepressants: I. Cyclic AntidepressantVaibhav KrishnaNo ratings yet
- Mood Stablizing AgentsDocument15 pagesMood Stablizing AgentsDhAiRyA ArOrANo ratings yet
- Psycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsDocument29 pagesPsycho-Pharmacotherapy: Major Tranquilizers, D2 - Receptor Blockers and Anti - Schizophrenic DrugsPoonam RanaNo ratings yet
- Dual Diagnosis - Clinical and Therapeutic Aspects (Maremmani 03)Document92 pagesDual Diagnosis - Clinical and Therapeutic Aspects (Maremmani 03)antonelloveltriNo ratings yet
- Improve Your Self Esteem With HomeopathyDocument2 pagesImprove Your Self Esteem With HomeopathyrbsNo ratings yet
- APA - DSM5 - Severity Measure For Panic Disorder Adult PDFDocument3 pagesAPA - DSM5 - Severity Measure For Panic Disorder Adult PDFMelissandreNo ratings yet
- PSYCHOPHARMACOLOGYDocument2 pagesPSYCHOPHARMACOLOGYJulia Rae Delos SantosNo ratings yet
- Hypertension Clinical Study PDFDocument42 pagesHypertension Clinical Study PDFsertti23No ratings yet
- Susceptibility 3rd Yr 2 (1) (Read-Only)Document21 pagesSusceptibility 3rd Yr 2 (1) (Read-Only)sai krishnaNo ratings yet
- Miasmatic Prescribing Softcover Subrata Kumar Banerjea.06424 1Document12 pagesMiasmatic Prescribing Softcover Subrata Kumar Banerjea.06424 1Clangames 4No ratings yet
- Mood Disorders: Slides & Handouts by Karen Clay Rhines, Ph.D. Northampton Community CollegeDocument81 pagesMood Disorders: Slides & Handouts by Karen Clay Rhines, Ph.D. Northampton Community CollegeumerfarooqNo ratings yet
- "Monograph Eating Disorders": StudentDocument12 pages"Monograph Eating Disorders": StudentTeffy NeyraNo ratings yet
- Fire FlyDocument10 pagesFire FlyMuralidaran SelvarajNo ratings yet
- Schizophrenia and HomeopathyDocument5 pagesSchizophrenia and HomeopathyDr. Nur-E-Alam Rasel100% (1)
- Presented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Document17 pagesPresented By:-11081506 (Ridhi) 11081524 (Khushboo) 11081560 (Shiny) 11081542 (Sakshi)Akanksha KapoorNo ratings yet
- Antisocial Personality Disorder and HomeopathyDocument2 pagesAntisocial Personality Disorder and HomeopathyAnonymous dpxYTENo ratings yet
- Sedative-Hypnotics (SeH) and AnxiolyticsDocument101 pagesSedative-Hypnotics (SeH) and Anxiolyticsmatchees-gone rogueNo ratings yet
- Case StudyDocument15 pagesCase Studyapi-589548099No ratings yet
- Group Study MedicineDocument8 pagesGroup Study MedicineRavi ChandarNo ratings yet
- Anxiety Disorder PDFDocument14 pagesAnxiety Disorder PDFTalal 197No ratings yet
- Most Question That The "Psychiatrist" Would Ask?Document1 pageMost Question That The "Psychiatrist" Would Ask?Chayantorn NimmanwathanaNo ratings yet
- Psychiatric Emergency PresentationDocument61 pagesPsychiatric Emergency PresentationValantino RamosNo ratings yet
- Lithium ToxicityDocument28 pagesLithium ToxicityReejan PaudelNo ratings yet
- Pheochromocytoma and HomoeopathyDocument13 pagesPheochromocytoma and HomoeopathyDr. Rajneesh Kumar Sharma MD HomNo ratings yet
- DeliriumDocument27 pagesDeliriumBushra EjazNo ratings yet
- Eatiing DisordersDocument69 pagesEatiing DisordersMasa MasaNo ratings yet
- Case StudyDocument12 pagesCase Studyapi-663568963No ratings yet
- DipressionDocument8 pagesDipressionImtiaz Hussain100% (1)
- Homeopathic Medicines For Delusions - DrHomeo HomeopathyDocument1 pageHomeopathic Medicines For Delusions - DrHomeo HomeopathyNancyNo ratings yet
- New Post Grad ProgramDocument8 pagesNew Post Grad ProgramPradeep KumarNo ratings yet
- Tension Headaches: What Is A Tension Headache? HighlightsDocument9 pagesTension Headaches: What Is A Tension Headache? HighlightsIndryNo ratings yet
- Behaviors: How To Respond When Dementia Causes Unpredictable BehaviorsDocument12 pagesBehaviors: How To Respond When Dementia Causes Unpredictable BehaviorsJohn GurungNo ratings yet
- Clinical Trial of Homoeopathic Preparations of Amyleum Nitrosum, Azathioprine Cocainum Muriaticum and Cyclosporine in HIV DiseaseDocument34 pagesClinical Trial of Homoeopathic Preparations of Amyleum Nitrosum, Azathioprine Cocainum Muriaticum and Cyclosporine in HIV DiseaseDr Dushyant Kamal DhariNo ratings yet
- Duration of Protection - VaccinesDocument10 pagesDuration of Protection - VaccinesM.DalaniNo ratings yet
- Antipsychotic DrugsDocument47 pagesAntipsychotic DrugsIkram UddinNo ratings yet
- Benzodiazepines For Anxiety Disorders Maximising The Benefits and Minimising The RisksDocument9 pagesBenzodiazepines For Anxiety Disorders Maximising The Benefits and Minimising The RisksJordanNo ratings yet
- Homoeopathy and Psychiatry: Editorial For The Month of November 2007 Psycho-Somatic Illnesses and HomoeopathyDocument5 pagesHomoeopathy and Psychiatry: Editorial For The Month of November 2007 Psycho-Somatic Illnesses and HomoeopathycgarciNo ratings yet
- RUH Vol 9 10 Issue 1Document63 pagesRUH Vol 9 10 Issue 1Saurav Arora100% (1)
- Anxiety Disorders: Samantha Meltzer-Brody, M.D., M.P.H. Assistant Professor UNC Department of PsychiatryDocument62 pagesAnxiety Disorders: Samantha Meltzer-Brody, M.D., M.P.H. Assistant Professor UNC Department of PsychiatryPRHSTNo ratings yet
- 3 Schizophrenia AssessmentDocument36 pages3 Schizophrenia AssessmentArvindhanNo ratings yet
- The Psychiatric Review of Symptoms - A Screening Tool For Family Physicians - American Family PhysicianDocument7 pagesThe Psychiatric Review of Symptoms - A Screening Tool For Family Physicians - American Family PhysicianTimothy TurscakNo ratings yet
- Schizophrenia: Signs and SymptomsDocument38 pagesSchizophrenia: Signs and SymptomsRatu Nurul Fadhilah100% (1)
- The Precise Neurological ExamDocument30 pagesThe Precise Neurological ExamZīshān FārūqNo ratings yet
- Affective Disorders: Dr. Zeina Adnan Family Medicine SpecialistDocument31 pagesAffective Disorders: Dr. Zeina Adnan Family Medicine SpecialistLamyaa Ali HasanNo ratings yet
- Terminology of PsychiatryDocument6 pagesTerminology of PsychiatryHassan.shehri100% (1)
- J Yogaratnam 2013 Asia Piola PDFDocument8 pagesJ Yogaratnam 2013 Asia Piola PDFCamila RosenNo ratings yet
- Prevalence of Metabolic Syndrome Among Patients With Schizophrenia From Long Care Unit in Forensic Psychiatry Program: An Observational StudyDocument6 pagesPrevalence of Metabolic Syndrome Among Patients With Schizophrenia From Long Care Unit in Forensic Psychiatry Program: An Observational StudyJAVED ATHER SIDDIQUINo ratings yet
- The Association Between Hyponatremia and Psychotropic: An Observational Study in Chronic Forensic Rehabilitation Ward at Mental Health Hospital, Taif, Saudi ArabiaDocument5 pagesThe Association Between Hyponatremia and Psychotropic: An Observational Study in Chronic Forensic Rehabilitation Ward at Mental Health Hospital, Taif, Saudi ArabiaJAVED ATHER SIDDIQUINo ratings yet
- Dress Syndrome Asserious Skin Hypersensitivity Reactions Associated With Olanzapine: Case ReportDocument4 pagesDress Syndrome Asserious Skin Hypersensitivity Reactions Associated With Olanzapine: Case ReportJAVED ATHER SIDDIQUINo ratings yet
- Imaginary Love Stories Related To Substance Use Disorder: A Case ReportDocument3 pagesImaginary Love Stories Related To Substance Use Disorder: A Case ReportJAVED ATHER SIDDIQUINo ratings yet
- The Phenomenology, Socio-Demographic, and Clinical Profile of Substance Abusers Admitted To Drug De-Addiction Unit at Eradah and Mental Health Hospital, Taif, Saudi ArabiDocument5 pagesThe Phenomenology, Socio-Demographic, and Clinical Profile of Substance Abusers Admitted To Drug De-Addiction Unit at Eradah and Mental Health Hospital, Taif, Saudi ArabiJAVED ATHER SIDDIQUINo ratings yet
- Onychophagia: A Synopsis of Nail Biting and Its ManagementDocument4 pagesOnychophagia: A Synopsis of Nail Biting and Its ManagementJAVED ATHER SIDDIQUINo ratings yet
- Perceived Awareness of Clozapine Associated With Socio - Demographic Status, Clinical, and Side Effect Profile Among Patients From Mental Health Hospital, Taif, Saudi ArabiaDocument8 pagesPerceived Awareness of Clozapine Associated With Socio - Demographic Status, Clinical, and Side Effect Profile Among Patients From Mental Health Hospital, Taif, Saudi ArabiaJAVED ATHER SIDDIQUINo ratings yet
- Risperidone-Induced Premature Ventricular Complexes in Psychosis: A Case ReportDocument4 pagesRisperidone-Induced Premature Ventricular Complexes in Psychosis: A Case ReportJAVED ATHER SIDDIQUINo ratings yet
- Factitious Disorder - Patient Pretending To Long Stay at The HospitalDocument3 pagesFactitious Disorder - Patient Pretending To Long Stay at The HospitalJAVED ATHER SIDDIQUINo ratings yet
- Hyponatremia & Water Intoxication With Carbamazepine: A Rare Case ReportDocument3 pagesHyponatremia & Water Intoxication With Carbamazepine: A Rare Case ReportJAVED ATHER SIDDIQUINo ratings yet
- Left Temporal Lobe Arachnoid Cyst Presenting With Symptoms of PsychosisDocument4 pagesLeft Temporal Lobe Arachnoid Cyst Presenting With Symptoms of PsychosisJAVED ATHER SIDDIQUINo ratings yet
- Interictal Psychosis - A Case of Psychosis of EpilepsyDocument3 pagesInterictal Psychosis - A Case of Psychosis of EpilepsyJAVED ATHER SIDDIQUINo ratings yet
- Psychotropic-Induced Hyponatremia: A ReviewDocument9 pagesPsychotropic-Induced Hyponatremia: A ReviewJAVED ATHER SIDDIQUINo ratings yet
- Metabolic Syndrome GuidelinesDocument3 pagesMetabolic Syndrome GuidelinesCrhistian Celis OlaveNo ratings yet
- Obesity and Type 2 DiabetesDocument18 pagesObesity and Type 2 DiabetespritaultimardianNo ratings yet
- The Fructose-Copper Connection - Added Sugars Induce Fatty Liver and Insulin Resistance Via Copper DeficiencyDocument3 pagesThe Fructose-Copper Connection - Added Sugars Induce Fatty Liver and Insulin Resistance Via Copper DeficiencyNvo SpektarNo ratings yet
- Metabolic SyndromDocument11 pagesMetabolic SyndromAshaNo ratings yet
- Smoking and DiabetesDocument5 pagesSmoking and DiabetesgiannidietNo ratings yet
- Cactus (Opuntia Ficus-Indica) : A Review On Its Antioxidants Properties and Potential Pharmacological Use in Chronic DiseasesDocument9 pagesCactus (Opuntia Ficus-Indica) : A Review On Its Antioxidants Properties and Potential Pharmacological Use in Chronic DiseasesAidNo ratings yet
- The 8 Second Secret The Scientifically Proven Method For Lasting WeightlossDocument204 pagesThe 8 Second Secret The Scientifically Proven Method For Lasting WeightlossGlen HutchinsonNo ratings yet
- Menopause Related Symptoms and Their Correlates: A Community Based Cross Sectional Study in Kollam District, KeralaDocument129 pagesMenopause Related Symptoms and Their Correlates: A Community Based Cross Sectional Study in Kollam District, Keraladhaya georgeNo ratings yet
- Storgard Channing WP1Document6 pagesStorgard Channing WP1Channing StorgardNo ratings yet
- ?overview of Secondary Prevention of Ischemic Stroke - UpToDateDocument40 pages?overview of Secondary Prevention of Ischemic Stroke - UpToDateJorgeNo ratings yet
- 2074WJMH - WJMH 41 E26Document19 pages2074WJMH - WJMH 41 E26Murillo Pyaia Alves PaixãoNo ratings yet
- Obesity TreatmentDocument170 pagesObesity Treatmentojobi joeNo ratings yet
- Aha 2018 Cir.0000000000000558 PDFDocument426 pagesAha 2018 Cir.0000000000000558 PDFDesy YardinaNo ratings yet
- Insulin ResistanceDocument48 pagesInsulin ResistanceLavina JainNo ratings yet
- Thyroid Function and The Metabolic Syndrome in Older Persons: A Population-Based StudyDocument7 pagesThyroid Function and The Metabolic Syndrome in Older Persons: A Population-Based StudyAlifia RahmaNo ratings yet
- Blaylock Hypertension 13Document16 pagesBlaylock Hypertension 13mohanp71No ratings yet
- Pathophysiology, Diagnosis, and Management of Dyslipidemia: Gerald T. Gau, MD, and R. Scott Wright, MD, FACC, FAHA, FESCDocument42 pagesPathophysiology, Diagnosis, and Management of Dyslipidemia: Gerald T. Gau, MD, and R. Scott Wright, MD, FACC, FAHA, FESCCalvin LitraNo ratings yet
- Physiology of DiabetesDocument52 pagesPhysiology of DiabetesPhysiology by Dr RaghuveerNo ratings yet
- Aggoun 2007Document7 pagesAggoun 2007Messias FilhoNo ratings yet
- Peripheral Arterial DiseaseDocument161 pagesPeripheral Arterial Diseasec406400No ratings yet
- Lexington Medical Center Heart Health InsertDocument12 pagesLexington Medical Center Heart Health InsertLexington Medical CenterNo ratings yet
- 127 FullDocument9 pages127 FullCho HyumiNo ratings yet
- Acanthosis NigricansDocument32 pagesAcanthosis NigricansZeliha TürksavulNo ratings yet
- Nutrients 11 00655Document20 pagesNutrients 11 00655Ibtidau NiamilahNo ratings yet
- Pcos RRL 2Document71 pagesPcos RRL 2Rosher Deliman JanoyanNo ratings yet
- Causes of ObesityDocument3 pagesCauses of ObesityKaren Chambre100% (1)
- Fasting Insulin Levels Independently Associates With Coronary Heart Diseade in Non-Diabetic Turkish Men and WomenDocument9 pagesFasting Insulin Levels Independently Associates With Coronary Heart Diseade in Non-Diabetic Turkish Men and WomenJanne AraújoNo ratings yet