Professional Documents
Culture Documents
CPPP PP P PP PPPPPPP PP
CPPP PP P PP PPPPPPP PP
Uploaded by
angelieballesterosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CPPP PP P PP PPPPPPP PP
CPPP PP P PP PPPPPPP PP
Uploaded by
angelieballesterosCopyright:
Available Formats
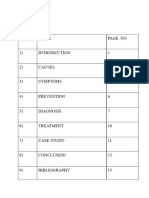
Meningitis
Meningitis is an inflammation of the lining around the brain and spinal cord caused by bacteria or viruses. Septic Meningitis is caused by bacteria like Streptococcus pneumonia and Neisseria meningitis. Haemohilus influenza was once a common cause of meningitis in children, but, because of vaccination, infection with this organism is now rare in developed countries. Aseptic Meningitis is caused by virus or secondary to lymphoma, leukemia, or human immunodeficiency virus.
Pathophysiology
Meningeal infections generally originates in one of two ways: through the bloodstream as a consequence of other infections or by direct spread, such as might occur after a traumatic injury to the facial bones or secondary to invasive procedures. N. meningitides concentrates in the nasopharynx and is transmitted by secretion or aerosol contamination. Once the causative organism enters the bloodstream, it crosses the blood-brain barrier and proliferates in the cerebrospinal fluid (CSF). The host immune response stimulates the release of cell wall fragments and lipopolysaccharides, facilitating inflammation of the subarachnoid and pia mater. Because the cranial vault contains little room for expansion, the inflammation may cause increased intracranial pressure (ICP). CSF circulates through the subarachnoid space, where inflammatory cellular materials from the affected meningeal tissue enter and accumulate.
Manifestations
*Headache *Stiff and painful neck *Positive Brudzinski s sign *Rashes *Disorientation *lethargy *coma *Brain stem herniation *Fever *Positive Kernig s sign *Photophobia *Skin lesions may develop *Memory impairment *unresponsiveness *Seizures
Diagnostic Procedures
Blood Tests are preformed for markers of inflammation (e.g. C-reactive protein, CBC), as well as blood culture Lumbar Puncture (LP, Spinal tap) is done by inserting a needle into the dural sac (a sac around the spinal cord) to collect cerebrospinal fluid or CSF).
It is contraindicated to patients with mass in the brain (tumor or abscess), and increase Intracranial pressure (ICP) as it may lead to brain herniation. CSF Analysis cloudy, increased pressure, WBCs and proteins high, glucose decreased, culture and gram stain are positive.
Medical Management
1. Early administration of an antibiotic that crosses the blood-brain barrier into the subarachnoid space in sufficient concentration to halt the multiplication of bacteria. y Vancomycin hydrochloride in the combination of cefalosporins is administered intravenously 2. Dexamethasone 15-29 minutes before first dose of antibiotic 3. Dehydration and shock are treated with fluid volume expanders 4. Phenytoin (Dilantin) for seizure 5. Administer osmotic diuretics, restricting fluids, draining CSF, controlling fever, maintaining systematic blood pressure and oxygenation, and reducing cellular metabolic demands for increase ICP.
Nursing Management
1. Neurologic status and vital signs are continually assessed. 2. Insertion of a cuffed endotracheal tube (or tracheotomy) and mechanical ventilation to maintain adequate tissue oxygenation. 3. Rapid IV fluid replacement may be prescribed, but care is taken to prevent fluid overload. 4. Reduce body temperature if the patient have a fever. 5. Protect the patient from injury secondary to seizure activity or altered LOC. 6. Monitor daily body weight; serum electrolytes; and urine volume, specific gravity, and osmolality, especially if syndrome of inappropriate antidiuretic hormone (SIADH) is suspected. 7. Preventing complications associated with immobility such as pressure ulcers and pneumonia. 8. Instituting infection control and precautions until 24 hours after initiation of antibiotic therapy (oral and nasal discharge is considered infectious).
Treatment
Initial treatment Meningitis is potentially life-threatening and has a high mortality rate if untreated; delay in treatment has been associated with a poorer outcome. Thus treatment with wide-spectrum antibiotics should not be delayed while confirmatory tests are being conducted. If meningococcal disease is suspected in primary care, guidelines recommend that benzylpenicillin be administered before transfer to hospital. Intravenous fluids should be administered if hypotension (low blood pressure) or shock are present. Given that meningitis can cause a number of early severe complications, regular medical review is
recommended to identify these complications early, as well as admission to an intensive care unit if deemed necessary. Mechanical ventilation may be needed if the level of consciousness is very low, or if there is evidence of respiratory failure. If there are signs of raised intracranial pressure, measures to monitor the pressure may be taken; this would allow the optimization of the cerebral perfusion pressure and various treatments to decrease the intracranial pressure with medication (e.g. mannitol). Seizures are treated with anticonvulsants. Hydrocephalus (obstructed flow of CSF) may require insertion of a temporary or long-term drainage device, such as a cerebral shunt. Bacterial Miningitis Antibiotics Structural formula of ceftriaxone, one of the third-generation cefalosporin antibiotics recommended for the initial treatment of bacterial meningitis. Empiric antibiotics (treatment without exact diagnosis) must be started immediately, even before the results of the lumbar puncture and CSF analysis are known. The choice of initial treatment depends largely on the kind of bacteria that cause meningitis in a particular place. Empirical therapy may be chosen on the basis of the age of the patient, whether the infection was preceded by head injury, whether the patient has undergone neurosurgery and whether or not a cerebral shunt is present. Once the Gram stain results become available, and the broad type of bacterial cause is known, it may be possible to change the antibiotics to those likely to deal with the presumed group of pathogens. The results of the CSF culture generally take longer to become available (24 48 hours). Once they do, empiric therapy may be switched to specific antibiotic therapy targeted to the specific causative organism and its sensitivities to antibiotics. For an antibiotic to be effective in meningitis, it must not only be active against the pathogenic bacterium, but also reach the meninges in adequate quantities; some antibiotics have inadequate penetrance and therefore have little use in meningitis. Most of the antibiotics used in meningitis have not been tested directly on meningitis patients in clinical trials. Rather, the relevant knowledge has mostly derived from laboratory studies in rabbits. Steroids Adjuvant treatment with corticosteroids (usually dexamethasone) has been shown in some studies to reduce rates of mortality, severe hearing loss and neurological damage in adolescents and adults from high income countries which have low rates of HIV. The likely mechanism is suppression of overactive inflammation. Viral meningitis Viral meningitis typically requires supportive therapy only; most viruses responsible for causing meningitis are not amenable to specific treatment. Viral meningitis tends to run a more benign course than bacterial meningitis. Herpes simplex virus and varicella zoster virus may respond to treatment with antiviral drugs such as aciclovir, but there are no clinical trials that have specifically addressed whether this treatment is effective. Mild cases of viral meningitis can be treated at home with conservative measures such as fluid, bed rest, and analgesics
You might also like
- nsg444 Jessica Evans Personal StatementDocument3 pagesnsg444 Jessica Evans Personal Statementapi-439893609No ratings yet
- NBME 7 KeyDocument6 pagesNBME 7 KeyQaim ShahNo ratings yet
- TB MeningitisDocument18 pagesTB Meningitisjesa34No ratings yet
- Eye Acupuncture PDFDocument8 pagesEye Acupuncture PDFLiv100% (3)
- 67 Success StoriesDocument72 pages67 Success StoriesPoorna Kalandhar100% (1)
- Meningitis &encephalitisDocument9 pagesMeningitis &encephalitisSnIP StandredNo ratings yet
- Meningitis PresentationDocument41 pagesMeningitis PresentationO'Mark AndrewsNo ratings yet
- Meningitis and Dementia: Dr. Lubna DwerijDocument52 pagesMeningitis and Dementia: Dr. Lubna DwerijNoor MajaliNo ratings yet
- Meningitis: N Meningitidis Are Gram-Negative, Kidney Bean-Shaped Organisms and Frequently AreDocument7 pagesMeningitis: N Meningitidis Are Gram-Negative, Kidney Bean-Shaped Organisms and Frequently AreKhryss Paula BaldonadoNo ratings yet
- Signs and Symptoms: Clinical PresentationDocument11 pagesSigns and Symptoms: Clinical PresentationGaluh NurfadillahNo ratings yet
- BffsDocument60 pagesBffsdrewantaNo ratings yet
- ENLS Meningitis and Encephalitis ProtocolDocument20 pagesENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNo ratings yet
- Bacterial Meningitis in AdultsDocument55 pagesBacterial Meningitis in AdultsfjnaressiNo ratings yet
- Research Paper Bacterial MeningitisDocument4 pagesResearch Paper Bacterial Meningitisafeebovus100% (1)
- Bacterial MeningitisDocument5 pagesBacterial Meningitisjamesignacio787No ratings yet
- Blank 10Document7 pagesBlank 10Leomer Calderon jr.No ratings yet
- Bacterial Meningitis Patho PaperDocument5 pagesBacterial Meningitis Patho PaperJessica BrayNo ratings yet
- Bacterial Meningitis in ChildrenDocument10 pagesBacterial Meningitis in ChildrenAnny AryanyNo ratings yet
- Cns InfectionsDocument56 pagesCns InfectionsDinaNo ratings yet
- Acute Bacterial MeningitisDocument15 pagesAcute Bacterial MeningitisOana StefanNo ratings yet
- Research Paper On Bacterial MeningitisDocument8 pagesResearch Paper On Bacterial Meningitisvvgnzdbkf100% (1)
- AcuteDocument11 pagesAcutenunu ahmedNo ratings yet
- Bacterial Meningitis: Etiology and PathophysiologyDocument9 pagesBacterial Meningitis: Etiology and PathophysiologyIndra Dwi VerawatiNo ratings yet
- Meningitis: By-Dr Nimco A. MDDocument31 pagesMeningitis: By-Dr Nimco A. MDgibreilNo ratings yet
- Investigatory Project On MeningitisDocument15 pagesInvestigatory Project On MeningitisMaanya PrithianiNo ratings yet
- Bacterial Meningitis ThesisDocument8 pagesBacterial Meningitis ThesisRick Vogel100% (2)
- Definition-: Neisseria Meningitidis Invading The Subarachnoid Space of The BrainDocument12 pagesDefinition-: Neisseria Meningitidis Invading The Subarachnoid Space of The BrainAmit MartinNo ratings yet
- Neurological Infections: By, Mr. Anish Ghosh M.Sc. Nursing 2 YearDocument57 pagesNeurological Infections: By, Mr. Anish Ghosh M.Sc. Nursing 2 YearAnish GhoshNo ratings yet
- Viral MeningitisDocument19 pagesViral MeningitisUneebNo ratings yet
- Chapter 22Document7 pagesChapter 22Lyra Ortega OliquinoNo ratings yet
- Meningitis in Adults: Diagnosis and Management: PembimbingDocument45 pagesMeningitis in Adults: Diagnosis and Management: PembimbingNeny Mathilda UniplaitaNo ratings yet
- Meningitis - Practice Essentials, Background, PathophysiologyDocument26 pagesMeningitis - Practice Essentials, Background, PathophysiologydilaNo ratings yet
- Infectious and Inflammatory Diseases of Brain and Spinal CordDocument50 pagesInfectious and Inflammatory Diseases of Brain and Spinal CordKeerthana BNo ratings yet
- MeningitisDocument64 pagesMeningitisubafran92No ratings yet
- Therapy LV CNS 4th Year KirubelDocument156 pagesTherapy LV CNS 4th Year Kirubelpblinder1319No ratings yet
- Types of MeningitisDocument6 pagesTypes of MeningitisARISNo ratings yet
- 2_5217623676744122824Document7 pages2_5217623676744122824am55eer55No ratings yet
- Neurological InfectionsDocument21 pagesNeurological Infectionsfortuneholiness11No ratings yet
- MeningitisDocument42 pagesMeningitisRajesh YadavNo ratings yet
- Spinal MeningitisDocument7 pagesSpinal Meningitisapi-282958026No ratings yet
- EncephalitisDocument37 pagesEncephalitisPRADEEPNo ratings yet
- Meningitis and Encephalitis: Samantha Noll June 11, 2015Document45 pagesMeningitis and Encephalitis: Samantha Noll June 11, 2015galihNo ratings yet
- Meningitis, AAFPDocument8 pagesMeningitis, AAFPCarlos Danilo Noroña CNo ratings yet
- MeningitisDocument3 pagesMeningitisAMOS MELINo ratings yet
- Meningo Encephalitis DiscussionDocument28 pagesMeningo Encephalitis DiscussionVindu WadhwaniNo ratings yet
- College of Nursing Berhampur: Subject-Medical Surgical Nursing Topic-MeningitisDocument9 pagesCollege of Nursing Berhampur: Subject-Medical Surgical Nursing Topic-MeningitisAmlan jyoti thanapati100% (1)
- Meningitis: Author InformationDocument10 pagesMeningitis: Author Informationakbar011512No ratings yet
- Neuroinfección Rosen's Emergency Medicine - Concepts and Clinical Practice 10th Edition 2022Document13 pagesNeuroinfección Rosen's Emergency Medicine - Concepts and Clinical Practice 10th Edition 2022fyqmk4q8pkNo ratings yet
- 1-Rheumatic Heart Disease and EndocarditisDocument69 pages1-Rheumatic Heart Disease and EndocarditisHamzehNo ratings yet
- Management of MenengitesDocument8 pagesManagement of Menengiteskhaled alsulaimNo ratings yet
- Presentation On MeningitisDocument51 pagesPresentation On Meningitissushma shresthaNo ratings yet
- Meningitis 1 Meningitis Katie, Elizabeth, Alison LVN #11Document4 pagesMeningitis 1 Meningitis Katie, Elizabeth, Alison LVN #11kt16roxNo ratings yet
- 2020 11 20 CNS Infections MitsiasDocument75 pages2020 11 20 CNS Infections MitsiasΖέτα ΤσίρκαNo ratings yet
- Referat SepsisDocument18 pagesReferat SepsisImelva GirsangNo ratings yet
- Meningitis IN PDF PEDIATRICDocument14 pagesMeningitis IN PDF PEDIATRICCruz Roelia Ruiz SanchezNo ratings yet
- Signs and SymptomsDocument33 pagesSigns and SymptomsGaluh NurfadillahNo ratings yet
- Infection of CNSDocument6 pagesInfection of CNSsagessenguegangNo ratings yet
- Nyarang'o Dennis Level IIIDocument29 pagesNyarang'o Dennis Level IIIBryan AmataNo ratings yet
- Bacterial Meningitis in The Neonate - Neurologic Complications - UpToDateDocument9 pagesBacterial Meningitis in The Neonate - Neurologic Complications - UpToDateAngélica PedrazaNo ratings yet
- Central Nervous System InfectionsDocument33 pagesCentral Nervous System InfectionsJENSEL CLOUIE C. REGLOSNo ratings yet
- Session 39 MeningitisDocument25 pagesSession 39 MeningitisJohn MoshaNo ratings yet
- Brain Abscess PDFDocument28 pagesBrain Abscess PDFdoctordilafrozaNo ratings yet
- Therapeutics in Aquaculture (AAH 301 1+1)Document25 pagesTherapeutics in Aquaculture (AAH 301 1+1)RISHIKANo ratings yet
- Bonifacio V. Romero High School Tle Beauty Care 9 1st Quarter Examination S.Y. 2018-2019Document6 pagesBonifacio V. Romero High School Tle Beauty Care 9 1st Quarter Examination S.Y. 2018-2019Virginia Saavedra100% (1)
- Non-Pharmacologic Pain Management in OrthodonticsDocument21 pagesNon-Pharmacologic Pain Management in OrthodonticsDr. Kanak100% (1)
- Exam ANS Pharmacology Report Inter2023 1 PRVDocument8 pagesExam ANS Pharmacology Report Inter2023 1 PRVtestingNo ratings yet
- ANSWER KEY ĐỀ ĐỀ XUẤT CHL - QN lớp 10Document6 pagesANSWER KEY ĐỀ ĐỀ XUẤT CHL - QN lớp 10caothanhquang27No ratings yet
- Histologi Saluran Nafas Dan ParuDocument28 pagesHistologi Saluran Nafas Dan ParuDhimasAjiZuandaNo ratings yet
- HTB-14 Product Sheet - U-87 MGDocument6 pagesHTB-14 Product Sheet - U-87 MGBiopharma GuruNo ratings yet
- Ssa 827Document2 pagesSsa 827joshud7264100% (3)
- Pharma Supply ChainDocument63 pagesPharma Supply ChainVijay KumarNo ratings yet
- Price List Khusus PharosDocument4 pagesPrice List Khusus Pharoshendra.susanto.mailNo ratings yet
- Claims - Evidence - Reasoning (C-E-R) Writing Graphic Organizer / 7thDocument4 pagesClaims - Evidence - Reasoning (C-E-R) Writing Graphic Organizer / 7thToot ScootNo ratings yet
- Injuries Around Leg: DR Abhishek Pathak Asst. Prof Deptt of Orthopaedics & Traumatology Gandhi Medical College BhopalDocument43 pagesInjuries Around Leg: DR Abhishek Pathak Asst. Prof Deptt of Orthopaedics & Traumatology Gandhi Medical College BhopaldrabhishekorthoNo ratings yet
- List of Empanelled HCOs - Hyderabad (July 2021)Document11 pagesList of Empanelled HCOs - Hyderabad (July 2021)Venu MadhavNo ratings yet
- Genius Case StudyDocument10 pagesGenius Case StudychengadNo ratings yet
- Study On The Transformation Codes StuffDocument2 pagesStudy On The Transformation Codes StuffManojkumar NairNo ratings yet
- Management of Acute Pelvic Inflammatory Disease: DR .Ashraf Fouda Ob/Gyn. ConsultantDocument75 pagesManagement of Acute Pelvic Inflammatory Disease: DR .Ashraf Fouda Ob/Gyn. ConsultantdrdivishNo ratings yet
- Hematology ReviewDocument4 pagesHematology ReviewAlfred ChowNo ratings yet
- Azimor - 250 TabletsDocument1 pageAzimor - 250 TabletsRakesh PalNo ratings yet
- 1898 Mahamari, or The Plague, in British Garhwal and Kumaun by Hutcheson S PDFDocument15 pages1898 Mahamari, or The Plague, in British Garhwal and Kumaun by Hutcheson S PDFguangxidogNo ratings yet
- Eye Eye: Visit For More The Ultimate Online Montessori Resource !Document21 pagesEye Eye: Visit For More The Ultimate Online Montessori Resource !uncorreopararegistroNo ratings yet
- Antioxidants and Their Charecterization: September 2011Document4 pagesAntioxidants and Their Charecterization: September 2011SofhiaZahraNo ratings yet
- The CO2 Absorber Based On LiOHDocument4 pagesThe CO2 Absorber Based On LiOHKariveli TharavaduNo ratings yet
- Review of ApplicationDocument6 pagesReview of ApplicationPrabath ChinthakaNo ratings yet
- Dekra Leading Indicator For SIFDocument15 pagesDekra Leading Indicator For SIFsdurga1100% (2)
- Flowchart - Medical Pathways 2014Document2 pagesFlowchart - Medical Pathways 2014Hillaryy K JongNo ratings yet
- Pharmacokinetic Models MultiDocument79 pagesPharmacokinetic Models Multiuday sainiNo ratings yet