Professional Documents
Culture Documents
Exercise 4 - Respiratory Disorder
Exercise 4 - Respiratory Disorder
Uploaded by
Freya AvellanoCopyright:
Available Formats
You might also like
- The OCD Workbook - Your Guide To Breaking Free From Obsessive-Compulsive Disorder (PDFDrive)Document378 pagesThe OCD Workbook - Your Guide To Breaking Free From Obsessive-Compulsive Disorder (PDFDrive)MrRamm100% (11)
- Case 16 QuestionsDocument10 pagesCase 16 Questionsapi-532124328No ratings yet
- Module 1 Organic MedicinalsDocument7 pagesModule 1 Organic MedicinalsMARIA FREDIJEAN CARIÑONo ratings yet
- Informatics For Modular StudentsDocument7 pagesInformatics For Modular StudentsKeziah VenturaNo ratings yet
- Sample Internship Training Plan TemplateDocument127 pagesSample Internship Training Plan TemplatenadivataniaNo ratings yet
- M2 - Lesson 1 - Preparation of Standard Patient ScriptingDocument22 pagesM2 - Lesson 1 - Preparation of Standard Patient ScriptingElleason Joshua G. FranciscoNo ratings yet
- Bioavailability PK Practice Problems 2013Document2 pagesBioavailability PK Practice Problems 2013Linh PhamNo ratings yet
- Developing A Pharmaceutical Care PlanDocument2 pagesDeveloping A Pharmaceutical Care PlanRiga 'Azoe' AlrianiNo ratings yet
- Quali/Quanti FlashcardsDocument3 pagesQuali/Quanti FlashcardsKrisha Bernadette TillamanNo ratings yet
- Pharm Care 4 Chapter 1Document25 pagesPharm Care 4 Chapter 1MaraNagaSambarani100% (1)
- ManufacturingDocument11 pagesManufacturingKitkat CasacopNo ratings yet
- Exercises 8-10 (By Dr. N. Tubon) PDFDocument25 pagesExercises 8-10 (By Dr. N. Tubon) PDFLoren100% (1)
- Pharmaceutical Analysis - IiDocument12 pagesPharmaceutical Analysis - IiMae Quenie Abadingo TiroNo ratings yet
- Ficus Minahassae - Full Plant ReviewDocument11 pagesFicus Minahassae - Full Plant ReviewDanielQuasiPokuAmoahNo ratings yet
- RG4 1Document25 pagesRG4 1alien18 patsayyNo ratings yet
- St. Paul University PhilippinesDocument9 pagesSt. Paul University PhilippinesAshley DayagNo ratings yet
- Physicochemical IncompatibilitiesDocument20 pagesPhysicochemical Incompatibilitiesvicbart11No ratings yet
- List For Bcs ClassificationDocument3 pagesList For Bcs Classificationthemba67% (3)
- PH Chem 1Document10 pagesPH Chem 1Starlyn Jonalee Amarillo Alger50% (2)
- MIMSDocument3 pagesMIMSLheiDanielMariellMonteroNo ratings yet
- Manual - PrescriptionDocument5 pagesManual - PrescriptionRyan Glenn SoguilonNo ratings yet
- B Pharmaceutical ChemistryDocument29 pagesB Pharmaceutical ChemistryZllison Mae Teodoro MangabatNo ratings yet
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesNez TraehNo ratings yet
- Social and Administrative PharmacyDocument5 pagesSocial and Administrative PharmacyGrace Marino100% (1)
- Communications Chapter 1 (Lecture 1)Document20 pagesCommunications Chapter 1 (Lecture 1)yousername100% (1)
- Pharmaceutical Dosage Forms, Drug Delivery Systems and Medical Devices Pharm 201L Name:Tallod, Emerson John L. Group:11 Year/Section:Q2A Final RatingDocument7 pagesPharmaceutical Dosage Forms, Drug Delivery Systems and Medical Devices Pharm 201L Name:Tallod, Emerson John L. Group:11 Year/Section:Q2A Final RatingJames AzurinNo ratings yet
- Patient Medication ProfileDocument4 pagesPatient Medication ProfileLaura HernandezNo ratings yet
- UNIT 1 Computer 23 PDFDocument7 pagesUNIT 1 Computer 23 PDFHayna RoseNo ratings yet
- Phytochemical Screening, Antimicrobial and Cytotoxicity Properties ofDocument48 pagesPhytochemical Screening, Antimicrobial and Cytotoxicity Properties ofRyan HermosoNo ratings yet
- Philippine Association of Colleges of Pharmacy Pharmaceutical Dosage Forms QuestionDocument8 pagesPhilippine Association of Colleges of Pharmacy Pharmaceutical Dosage Forms QuestionEunice SofiaNo ratings yet
- SP GR Phy Phar Lab IntroDocument3 pagesSP GR Phy Phar Lab IntroAileen Delos SantosNo ratings yet
- PharCare NotesDocument9 pagesPharCare NotesJesza IgnacioNo ratings yet
- Toxicology Course Outline - CompletedDocument4 pagesToxicology Course Outline - Completedtpetronellah mandishona100% (1)
- Perspective in Pharmacy ReviewerDocument4 pagesPerspective in Pharmacy ReviewerRosemarie OngNo ratings yet
- Code of Ethics For PharmacistsDocument9 pagesCode of Ethics For PharmacistsRadowan AhmadNo ratings yet
- PHA619 LEC 1st ShiftDocument35 pagesPHA619 LEC 1st ShiftrenNo ratings yet
- Members List of Duties: Worksheet No. 2 Acetone ObjectiveDocument6 pagesMembers List of Duties: Worksheet No. 2 Acetone Objectivenica velanoNo ratings yet
- Pharmaceutical Dosage Froms and Drug Delivery SystemsDocument14 pagesPharmaceutical Dosage Froms and Drug Delivery SystemsChantelle MeaNo ratings yet
- Tramadol Hydrochloride/paracetamol 37.5 mg/325 MG Film-Coated TabletsDocument2 pagesTramadol Hydrochloride/paracetamol 37.5 mg/325 MG Film-Coated Tabletspbalakrishnan100% (1)
- Lab Activity PcolDocument15 pagesLab Activity PcolHannah VueltaNo ratings yet
- Studi KasusDocument3 pagesStudi KasusJulian FelixNo ratings yet
- Preparation OintmentDocument1 pagePreparation OintmentLyanlie MinamotoNo ratings yet
- Preparation No. "20" "NF Mouthwash" A. Wrap-Up Guide QuestionsDocument5 pagesPreparation No. "20" "NF Mouthwash" A. Wrap-Up Guide QuestionsMEDELYN KEITH ESTANISLAO100% (1)
- Jurnal 7 Stars PharmacistDocument3 pagesJurnal 7 Stars PharmacistmrabdulmanafNo ratings yet
- Effervescent GranulesDocument6 pagesEffervescent GranulesVarinder KumarNo ratings yet
- EDPMS User Manual GuideDocument34 pagesEDPMS User Manual GuideColleen Ariel SandovalNo ratings yet
- B. Informatics (Slides 1-66)Document7 pagesB. Informatics (Slides 1-66)Chrissy LayugNo ratings yet
- Preparation No. "17" "Liquid Petrolatum Emulsion" A. Wrap-Up Guide QuestionsDocument5 pagesPreparation No. "17" "Liquid Petrolatum Emulsion" A. Wrap-Up Guide QuestionsMEDELYN KEITH ESTANISLAONo ratings yet
- Tele PharmacyDocument19 pagesTele PharmacyFrance100% (1)
- In Komp A Tibi LitasDocument54 pagesIn Komp A Tibi LitasHifi Rizki.RNo ratings yet
- Prep 24 - Captropil SuspensionDocument3 pagesPrep 24 - Captropil SuspensionThe Dededo NativeNo ratings yet
- Unit 1: Introduction: Intended Learning OutcomesDocument7 pagesUnit 1: Introduction: Intended Learning Outcomesalibel caballeroNo ratings yet
- Disp. 1 Lab ManualDocument8 pagesDisp. 1 Lab ManualJaceNo ratings yet
- Therapeutic Drug Monitoring 7-1-20Document27 pagesTherapeutic Drug Monitoring 7-1-20mofadhilNo ratings yet
- IncompatibilityDocument8 pagesIncompatibilitypoonamNo ratings yet
- Unit IV. Solid Modified Release Dosage FormsDocument24 pagesUnit IV. Solid Modified Release Dosage FormsMary-Ann Valencia SapnuNo ratings yet
- Chapter 9: Solid Oral Modified-Release Dosage Forms and Drug Delivery SystemsDocument26 pagesChapter 9: Solid Oral Modified-Release Dosage Forms and Drug Delivery SystemsAlecza Mae Savella100% (1)
- Statement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistDocument5 pagesStatement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistAprilia R. Permatasari0% (1)
- Solution, Solubility and Factors Affecting SolubilityDocument6 pagesSolution, Solubility and Factors Affecting Solubilityshehryar khanNo ratings yet
- Learning ObjectivesDocument3 pagesLearning ObjectivesYosep BeNo ratings yet
- Module For Students: Urinary SystemDocument10 pagesModule For Students: Urinary Systemasus kuningNo ratings yet
- PCOS311 Cosmetic Product Notification 1Document18 pagesPCOS311 Cosmetic Product Notification 1Freya AvellanoNo ratings yet
- Postlab Phenol and ChloroformDocument25 pagesPostlab Phenol and ChloroformFreya AvellanoNo ratings yet
- PHCT311 Prelim ManualDocument23 pagesPHCT311 Prelim ManualFreya AvellanoNo ratings yet
- Exercise 7 Mineral Oil EmulsionDocument3 pagesExercise 7 Mineral Oil EmulsionFreya AvellanoNo ratings yet
- Guidelines For Case ReportDocument2 pagesGuidelines For Case ReportFreya AvellanoNo ratings yet
- Exercise 5 Ferrous Sulfate SyrupDocument3 pagesExercise 5 Ferrous Sulfate SyrupFreya AvellanoNo ratings yet
- BuratDocument5 pagesBuratFreya AvellanoNo ratings yet
- First Aid in The LaboratoryDocument1 pageFirst Aid in The LaboratoryFreya AvellanoNo ratings yet
- Document 14Document1 pageDocument 14Freya AvellanoNo ratings yet
- 22 Imobilisasi Pada Usia LanjutDocument34 pages22 Imobilisasi Pada Usia LanjutGian KalalembangNo ratings yet
- Accounting Information Systems 5th Edition Parkes Solutions ManualDocument36 pagesAccounting Information Systems 5th Edition Parkes Solutions Manualnubilegoggler.i8cm100% (18)
- AviPro News Issue 4Document8 pagesAviPro News Issue 4Bryan NicollNo ratings yet
- Safety and Immunogenicity of A Heterologous Boost With A Recombinant VaccineDocument35 pagesSafety and Immunogenicity of A Heterologous Boost With A Recombinant VaccineAristegui NoticiasNo ratings yet
- Erectile Function After Partial Penectomy For Penile CancerDocument8 pagesErectile Function After Partial Penectomy For Penile CancerTai rascunhos TaiNo ratings yet
- Paediatric Protocols Kenya PDFDocument35 pagesPaediatric Protocols Kenya PDFMusab Ahmed HirshiNo ratings yet
- Jurnal Ilmiah Simantek ISSN. 2550-0414 Vol. 5 No. 1 Februari 2021Document5 pagesJurnal Ilmiah Simantek ISSN. 2550-0414 Vol. 5 No. 1 Februari 2021Muhamad IhsanNo ratings yet
- Medical Surgical Nursing - Responses To Altered Tissue PerfusionDocument23 pagesMedical Surgical Nursing - Responses To Altered Tissue PerfusionLouise NicoleNo ratings yet
- Pancha KarmaDocument54 pagesPancha KarmamasdfgNo ratings yet
- Wa0016.Document176 pagesWa0016.Sreeja ReddyNo ratings yet
- Reviews: Testing at Scale During The COVID-19 PandemicDocument12 pagesReviews: Testing at Scale During The COVID-19 PandemicAdrija SinghNo ratings yet
- GSEE CBA Admission Records and Pre-Reg FormDocument6 pagesGSEE CBA Admission Records and Pre-Reg FormKathe Marren Sicat DuquesaNo ratings yet
- Vitamin D and Skin Diseases - A ReviewDocument12 pagesVitamin D and Skin Diseases - A ReviewMai Anh NguyễnNo ratings yet
- Sas 7-9Document7 pagesSas 7-9Jilkiah Mae Alfoja CampomanesNo ratings yet
- Project 3 Visual MappingDocument1 pageProject 3 Visual Mappingapi-593346566No ratings yet
- Truth and Healing Commission On Indian Boarding School Policies in The United States ActDocument37 pagesTruth and Healing Commission On Indian Boarding School Policies in The United States Actjen_benderyNo ratings yet
- TiroideDocument10 pagesTiroideRosália CoutadaNo ratings yet
- Test Bank For Emergency Care Emt 13th EditionDocument30 pagesTest Bank For Emergency Care Emt 13th EditionCharles Pando100% (40)
- Study of Risk Incidence and Mortality Associated WDocument8 pagesStudy of Risk Incidence and Mortality Associated WYulian 53No ratings yet
- Issue Brief: Re-Examining Hunger in The USDocument16 pagesIssue Brief: Re-Examining Hunger in The USAnnelise McGowanNo ratings yet
- Case of TuberculosisDocument5 pagesCase of TuberculosisSheryhan Tahir BayleNo ratings yet
- TOPIC 3.A Bag TechniqueDocument38 pagesTOPIC 3.A Bag TechniqueJayrelle D. Safran100% (1)
- Aadya Mishra - Horoscope AnalysisDocument11 pagesAadya Mishra - Horoscope Analysisastrologylover BanglaNo ratings yet
- Ok 936860629 Ok 11 Yds Mart 2019Document25 pagesOk 936860629 Ok 11 Yds Mart 2019gizemcetinNo ratings yet
- 9201 Mark Scheme Paper2 International Gcse Biology Jun22Document21 pages9201 Mark Scheme Paper2 International Gcse Biology Jun22asdf0% (1)
- Diode Laser T8 ProDocument32 pagesDiode Laser T8 ProAmine ManouNo ratings yet
- 8th Grade Vocabulary ListDocument1 page8th Grade Vocabulary ListsabrinaNo ratings yet
- Neurobiological Basis of PsychologyDocument62 pagesNeurobiological Basis of PsychologyJovelyn Morales JosolNo ratings yet
Exercise 4 - Respiratory Disorder
Exercise 4 - Respiratory Disorder
Uploaded by
Freya AvellanoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Exercise 4 - Respiratory Disorder
Exercise 4 - Respiratory Disorder
Uploaded by
Freya AvellanoCopyright:
Available Formats
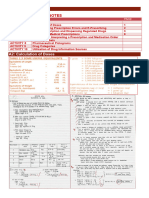
College of Pharmacy
CLINICAL PHARMACY LABORATORY
Group # Year and Section:
Name of Group Members Task Assignment:
(in alphabetical order, Last Name, First Name, M.I.)
1.
2.
3.
4.
Exercise No. 04
Title Respiratory Disorder (Chronic Obstructive Pulmonary Disease)
Instruction This exercise will be a group activity. In answering, use Arial for the font type with a font
size of 10. Save your file in pdf format with a file name (Group#_PHCPLab_E4) before
uploading it to canvas. Only one member of the group will upload the file but make sure that
everyone participated.
Objective:
After completing this case study, the reader should be able to:
1. Recognize modifiable and nonmodifiable risk factors for the development of COPD.
2. Interpret spirometry readings to evaluate and appropriately stage the severity of COPD for an individual patient.
3. Identify the importance of nonpharmacologic therapy in patients with COPD.
4. Develop an appropriate medication regimen for a patient with COPD based on disease severity.
5. Evaluate the role of inhaled and/or oral corticosteroids in the management of COPD.
6. Educate patients on using inhaled medications properly and determine which patients may benefit from spacers
and/or holding chambers.
Materials: textbook, medical dictionary, clinical laboratory books
Procedure:
1. Read and analyze the given case.
2. Prepare a patient therapeutic care plan.
3. Answer the questions at the end of the activity
Subjective
Chief Complaint: “Why can’t I just take prednisone every day? It always works when I get admitted to the hospital.”
HPI: Thomas Jones is a 66-year-old man with COPD presenting to the family medicine clinic today for a 1-month follow-
up appointment from his last hospital admission for an acute exacerbation of COPD. This last COPD exacerbation is the
second hospital admission in the last 6 months related to TJ’s COPD instability. After TJ’s hospitalization, his discharge
COPD regimen was changed to include tiotropium, 1 inhalation daily in addition to salmeterol 50 mcg, 1 inhalation Q 12
h, and an albuterol MDI as needed. TJ had pulmonary function tests (PFTs) while he was in the hospital 1 month ago but
has yet to have them reassessed after the change in his COPD regimen. He wants to start taking prednisone every day
because he believes this would prevent him from being readmitted to the hospital. The patient states that his respiratory
symptoms are better than when he was admitted 1 month ago, but he still has shortness of breath every day and a
decreased exercise capacity (e.g., he becomes very short of breath after walking a couple of blocks). He states that he
is adherent to the new medication regimen that was changed on discharge from the hospital. No other medications were
changed at that time that he can recall. His daughter, who is at the appointment today, states that she makes sure he
uses his inhalers but often wonders if he is using them correctly because he still has daily symptoms.
PMH: COPD × 12 years, GERD × 5 years, HTN × 20 years, CAD (MI 5 years ago)
CLINICAL PHARMACY LABORATORY
FH: Mother died from emphysema 4 years ago at the age of 82. Father has a history of coronary artery disease.
SH: He lives with his daughter and her family. His wife died 10 years ago from breast cancer. He has a 35-pack-year
history of smoking. He quit smoking approximately 3 months ago but has had occasional relapses. He states he has not
smoked for approximately a week. He drinks one to two beers every evening.
Meds: Metoprolol tartrate 50 mg PO BID, Salmeterol (Serevent Diskus) 1 inhalation (50 mcg) BID, Tiotropium (Spiriva) 1
capsule (18 mcg) inhaled once daily, Lisinopril 20 mg PO once daily, Esomeprazole (Nexium) 20 mg PO once daily,
Albuterol MDI 1–2 puffs Q 6 h PRN, Aspirin 81 mg PO once daily
ROS: (+) Shortness of breath with chronic nonproductive cough; (+) fatigue; (+) exercise intolerance
Objective
PHYSICAL EXAMINATION
• Gen: WDWN man appearing in mild respiratory distress after walking to the end of the hall to reach the exam
room
• VS: BP 138/88, P 85, RR 26, T 37.5°C; Wt 95 kg, Ht 5'11''
• Skin: Warm, dry; no rashes
• HEENT: Normocephalic; PERRLA, EOMI; normal sclerae; mucous membranes are moist; TMs intact;
oropharynx clear
• Neck/Lymph Nodes: Supple without lymphadenopathy
• Lungs: Tachypnea with prolonged expiration; decreased breath sounds; no rales, rhonchi, or crackles
• CV: RRR without murmur; normal S1 and S2
• Abd: Soft, NT/ND; (+) bowel sounds; no organomegaly
• Genit/Rect: No back or flank tenderness; normal male genitalia
• MS/Ext: No clubbing, cyanosis, or edema; pulses 2+ throughout
• Neuro: A & O × 3; CN II–XII intact; DTR 2+; normal mood and affect
LABORATORY EXAMINATION
Pulmonary Function Tests (during Hospital Admission 1 Month Ago):
• Prebronchodilator FEV1 = 1.1 L (predicted is 3.1 L)
• Prebronchodilator FVC = 3.2 L
• Postbronchodilator FEV1 = 1.6 L
Pulmonary Function Tests (during Clinic Visit Today):
• Prebronchodilator FEV1 = 1.3 L (predicted is 3.1 L)
• Prebronchodilator FVC = 3.2 L
• Postbronchodilator FEV1 = 1.47 L
CLINICAL PHARMACY LABORATORY
A. CASE ANALYSIS:
Complete the patient therapeutic care plan record below:
PATIENT THERAPEUTIC CARE PLAN RECORD
PATIENT DEMOGRAPHICS
Name: Age: Sex:
Birthday: Weight: Height:
Race: BMI:
MEDICAL INFORMATION
Chief Complaint:
HPI:
PMH:
Allergies:
Family History:
Social History: Tobacco use: ___Yes ___ No Caffeine use
If yes, how many sticks per day? ( ) Tobacco use: ___Yes ___ No
If yes, how many cups a day? ( )
Alcohol use: ___Yes ___ No Recreational Drug: ___Yes ___ No
If yes, how often? ( ) If yes, enumerate:
Others:
ROS:
PHYSICAL EXAMINATION
Vital Signs BP: ______ PR: _____
Temp: _____ RR: _____
Others:
CLINICAL PHARMACY LABORATORY
MEDICATION RECORD
Drug Name Indication Dosage Strength Dosage Regimen
LABORATORY EXAMINATION RESULTS
Test Result Normal Values Interpretation
ASSESSMENT OF THE MEDICAL CONDITION OF THE PATIENT:
a. What subjective and objective information indicates the presence of COPD in this patient?
b. What is the patient's COPD severity based on the subjective and objective information available?
CLINICAL PHARMACY LABORATORY
ASSESSMENT OF DRUG-RELATED PROBLEMS:
a. Create a list of the patient’s drug therapy problems and prioritize them. Include an assessment of medication appropriateness,
effectiveness, safety, and patient adherence. Discuss also whether there is an adverse effects and drug interactions.
PLAN
a. Therapeutic Interventions:
What are the goals of pharmacotherapy and nondrug therapy in this case?
Pharmacologic Interventions: Non-pharmacologic interventions:
b. Patient Education and Counseling:
What information should be provided to the patient to enhance adherence, ensure successful therapy, and minimize adverse effects?
c. Follow-up plan:
What clinical and laboratory parameters should be used to evaluate the therapy for the achievement of the desired therapeutic outcome
and to detect and prevent adverse effects?
CLINICAL PHARMACY LABORATORY
B. RELATED QUESTIONS:
1. Discuss what is COPD and its pathophysiology.
REFERENCES:
(Type your reference here in APA format)
2. Discuss the role of inhaled and/or oral corticosteroids in the management of COPD.
REFERENCES:
(Type your reference here in APA format)
CLINICAL PHARMACY LABORATORY
3. What is spirometry? Discuss the process of interpreting FEV1/FVC results.
REFERENCES:
(Type your reference here in APA format)
4. Describe the relationship between α1-antitrypsin deficiency and the development of emphysema
REFERENCES:
(Type your reference here in APA format)
CLINICAL PHARMACY LABORATORY
You might also like
- The OCD Workbook - Your Guide To Breaking Free From Obsessive-Compulsive Disorder (PDFDrive)Document378 pagesThe OCD Workbook - Your Guide To Breaking Free From Obsessive-Compulsive Disorder (PDFDrive)MrRamm100% (11)
- Case 16 QuestionsDocument10 pagesCase 16 Questionsapi-532124328No ratings yet
- Module 1 Organic MedicinalsDocument7 pagesModule 1 Organic MedicinalsMARIA FREDIJEAN CARIÑONo ratings yet
- Informatics For Modular StudentsDocument7 pagesInformatics For Modular StudentsKeziah VenturaNo ratings yet
- Sample Internship Training Plan TemplateDocument127 pagesSample Internship Training Plan TemplatenadivataniaNo ratings yet
- M2 - Lesson 1 - Preparation of Standard Patient ScriptingDocument22 pagesM2 - Lesson 1 - Preparation of Standard Patient ScriptingElleason Joshua G. FranciscoNo ratings yet
- Bioavailability PK Practice Problems 2013Document2 pagesBioavailability PK Practice Problems 2013Linh PhamNo ratings yet
- Developing A Pharmaceutical Care PlanDocument2 pagesDeveloping A Pharmaceutical Care PlanRiga 'Azoe' AlrianiNo ratings yet
- Quali/Quanti FlashcardsDocument3 pagesQuali/Quanti FlashcardsKrisha Bernadette TillamanNo ratings yet
- Pharm Care 4 Chapter 1Document25 pagesPharm Care 4 Chapter 1MaraNagaSambarani100% (1)
- ManufacturingDocument11 pagesManufacturingKitkat CasacopNo ratings yet
- Exercises 8-10 (By Dr. N. Tubon) PDFDocument25 pagesExercises 8-10 (By Dr. N. Tubon) PDFLoren100% (1)
- Pharmaceutical Analysis - IiDocument12 pagesPharmaceutical Analysis - IiMae Quenie Abadingo TiroNo ratings yet
- Ficus Minahassae - Full Plant ReviewDocument11 pagesFicus Minahassae - Full Plant ReviewDanielQuasiPokuAmoahNo ratings yet
- RG4 1Document25 pagesRG4 1alien18 patsayyNo ratings yet
- St. Paul University PhilippinesDocument9 pagesSt. Paul University PhilippinesAshley DayagNo ratings yet
- Physicochemical IncompatibilitiesDocument20 pagesPhysicochemical Incompatibilitiesvicbart11No ratings yet
- List For Bcs ClassificationDocument3 pagesList For Bcs Classificationthemba67% (3)
- PH Chem 1Document10 pagesPH Chem 1Starlyn Jonalee Amarillo Alger50% (2)
- MIMSDocument3 pagesMIMSLheiDanielMariellMonteroNo ratings yet
- Manual - PrescriptionDocument5 pagesManual - PrescriptionRyan Glenn SoguilonNo ratings yet
- B Pharmaceutical ChemistryDocument29 pagesB Pharmaceutical ChemistryZllison Mae Teodoro MangabatNo ratings yet
- (Dispensing 1 Laboratory) Review NotesDocument12 pages(Dispensing 1 Laboratory) Review NotesNez TraehNo ratings yet
- Social and Administrative PharmacyDocument5 pagesSocial and Administrative PharmacyGrace Marino100% (1)
- Communications Chapter 1 (Lecture 1)Document20 pagesCommunications Chapter 1 (Lecture 1)yousername100% (1)
- Pharmaceutical Dosage Forms, Drug Delivery Systems and Medical Devices Pharm 201L Name:Tallod, Emerson John L. Group:11 Year/Section:Q2A Final RatingDocument7 pagesPharmaceutical Dosage Forms, Drug Delivery Systems and Medical Devices Pharm 201L Name:Tallod, Emerson John L. Group:11 Year/Section:Q2A Final RatingJames AzurinNo ratings yet
- Patient Medication ProfileDocument4 pagesPatient Medication ProfileLaura HernandezNo ratings yet
- UNIT 1 Computer 23 PDFDocument7 pagesUNIT 1 Computer 23 PDFHayna RoseNo ratings yet
- Phytochemical Screening, Antimicrobial and Cytotoxicity Properties ofDocument48 pagesPhytochemical Screening, Antimicrobial and Cytotoxicity Properties ofRyan HermosoNo ratings yet
- Philippine Association of Colleges of Pharmacy Pharmaceutical Dosage Forms QuestionDocument8 pagesPhilippine Association of Colleges of Pharmacy Pharmaceutical Dosage Forms QuestionEunice SofiaNo ratings yet
- SP GR Phy Phar Lab IntroDocument3 pagesSP GR Phy Phar Lab IntroAileen Delos SantosNo ratings yet
- PharCare NotesDocument9 pagesPharCare NotesJesza IgnacioNo ratings yet
- Toxicology Course Outline - CompletedDocument4 pagesToxicology Course Outline - Completedtpetronellah mandishona100% (1)
- Perspective in Pharmacy ReviewerDocument4 pagesPerspective in Pharmacy ReviewerRosemarie OngNo ratings yet
- Code of Ethics For PharmacistsDocument9 pagesCode of Ethics For PharmacistsRadowan AhmadNo ratings yet
- PHA619 LEC 1st ShiftDocument35 pagesPHA619 LEC 1st ShiftrenNo ratings yet
- Members List of Duties: Worksheet No. 2 Acetone ObjectiveDocument6 pagesMembers List of Duties: Worksheet No. 2 Acetone Objectivenica velanoNo ratings yet
- Pharmaceutical Dosage Froms and Drug Delivery SystemsDocument14 pagesPharmaceutical Dosage Froms and Drug Delivery SystemsChantelle MeaNo ratings yet
- Tramadol Hydrochloride/paracetamol 37.5 mg/325 MG Film-Coated TabletsDocument2 pagesTramadol Hydrochloride/paracetamol 37.5 mg/325 MG Film-Coated Tabletspbalakrishnan100% (1)
- Lab Activity PcolDocument15 pagesLab Activity PcolHannah VueltaNo ratings yet
- Studi KasusDocument3 pagesStudi KasusJulian FelixNo ratings yet
- Preparation OintmentDocument1 pagePreparation OintmentLyanlie MinamotoNo ratings yet
- Preparation No. "20" "NF Mouthwash" A. Wrap-Up Guide QuestionsDocument5 pagesPreparation No. "20" "NF Mouthwash" A. Wrap-Up Guide QuestionsMEDELYN KEITH ESTANISLAO100% (1)
- Jurnal 7 Stars PharmacistDocument3 pagesJurnal 7 Stars PharmacistmrabdulmanafNo ratings yet
- Effervescent GranulesDocument6 pagesEffervescent GranulesVarinder KumarNo ratings yet
- EDPMS User Manual GuideDocument34 pagesEDPMS User Manual GuideColleen Ariel SandovalNo ratings yet
- B. Informatics (Slides 1-66)Document7 pagesB. Informatics (Slides 1-66)Chrissy LayugNo ratings yet
- Preparation No. "17" "Liquid Petrolatum Emulsion" A. Wrap-Up Guide QuestionsDocument5 pagesPreparation No. "17" "Liquid Petrolatum Emulsion" A. Wrap-Up Guide QuestionsMEDELYN KEITH ESTANISLAONo ratings yet
- Tele PharmacyDocument19 pagesTele PharmacyFrance100% (1)
- In Komp A Tibi LitasDocument54 pagesIn Komp A Tibi LitasHifi Rizki.RNo ratings yet
- Prep 24 - Captropil SuspensionDocument3 pagesPrep 24 - Captropil SuspensionThe Dededo NativeNo ratings yet
- Unit 1: Introduction: Intended Learning OutcomesDocument7 pagesUnit 1: Introduction: Intended Learning Outcomesalibel caballeroNo ratings yet
- Disp. 1 Lab ManualDocument8 pagesDisp. 1 Lab ManualJaceNo ratings yet
- Therapeutic Drug Monitoring 7-1-20Document27 pagesTherapeutic Drug Monitoring 7-1-20mofadhilNo ratings yet
- IncompatibilityDocument8 pagesIncompatibilitypoonamNo ratings yet
- Unit IV. Solid Modified Release Dosage FormsDocument24 pagesUnit IV. Solid Modified Release Dosage FormsMary-Ann Valencia SapnuNo ratings yet
- Chapter 9: Solid Oral Modified-Release Dosage Forms and Drug Delivery SystemsDocument26 pagesChapter 9: Solid Oral Modified-Release Dosage Forms and Drug Delivery SystemsAlecza Mae Savella100% (1)
- Statement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistDocument5 pagesStatement of Principle Self-Care Including Self-Medication - The Professional Role of The PharmacistAprilia R. Permatasari0% (1)
- Solution, Solubility and Factors Affecting SolubilityDocument6 pagesSolution, Solubility and Factors Affecting Solubilityshehryar khanNo ratings yet
- Learning ObjectivesDocument3 pagesLearning ObjectivesYosep BeNo ratings yet
- Module For Students: Urinary SystemDocument10 pagesModule For Students: Urinary Systemasus kuningNo ratings yet
- PCOS311 Cosmetic Product Notification 1Document18 pagesPCOS311 Cosmetic Product Notification 1Freya AvellanoNo ratings yet
- Postlab Phenol and ChloroformDocument25 pagesPostlab Phenol and ChloroformFreya AvellanoNo ratings yet
- PHCT311 Prelim ManualDocument23 pagesPHCT311 Prelim ManualFreya AvellanoNo ratings yet
- Exercise 7 Mineral Oil EmulsionDocument3 pagesExercise 7 Mineral Oil EmulsionFreya AvellanoNo ratings yet
- Guidelines For Case ReportDocument2 pagesGuidelines For Case ReportFreya AvellanoNo ratings yet
- Exercise 5 Ferrous Sulfate SyrupDocument3 pagesExercise 5 Ferrous Sulfate SyrupFreya AvellanoNo ratings yet
- BuratDocument5 pagesBuratFreya AvellanoNo ratings yet
- First Aid in The LaboratoryDocument1 pageFirst Aid in The LaboratoryFreya AvellanoNo ratings yet
- Document 14Document1 pageDocument 14Freya AvellanoNo ratings yet
- 22 Imobilisasi Pada Usia LanjutDocument34 pages22 Imobilisasi Pada Usia LanjutGian KalalembangNo ratings yet
- Accounting Information Systems 5th Edition Parkes Solutions ManualDocument36 pagesAccounting Information Systems 5th Edition Parkes Solutions Manualnubilegoggler.i8cm100% (18)
- AviPro News Issue 4Document8 pagesAviPro News Issue 4Bryan NicollNo ratings yet
- Safety and Immunogenicity of A Heterologous Boost With A Recombinant VaccineDocument35 pagesSafety and Immunogenicity of A Heterologous Boost With A Recombinant VaccineAristegui NoticiasNo ratings yet
- Erectile Function After Partial Penectomy For Penile CancerDocument8 pagesErectile Function After Partial Penectomy For Penile CancerTai rascunhos TaiNo ratings yet
- Paediatric Protocols Kenya PDFDocument35 pagesPaediatric Protocols Kenya PDFMusab Ahmed HirshiNo ratings yet
- Jurnal Ilmiah Simantek ISSN. 2550-0414 Vol. 5 No. 1 Februari 2021Document5 pagesJurnal Ilmiah Simantek ISSN. 2550-0414 Vol. 5 No. 1 Februari 2021Muhamad IhsanNo ratings yet
- Medical Surgical Nursing - Responses To Altered Tissue PerfusionDocument23 pagesMedical Surgical Nursing - Responses To Altered Tissue PerfusionLouise NicoleNo ratings yet
- Pancha KarmaDocument54 pagesPancha KarmamasdfgNo ratings yet
- Wa0016.Document176 pagesWa0016.Sreeja ReddyNo ratings yet
- Reviews: Testing at Scale During The COVID-19 PandemicDocument12 pagesReviews: Testing at Scale During The COVID-19 PandemicAdrija SinghNo ratings yet
- GSEE CBA Admission Records and Pre-Reg FormDocument6 pagesGSEE CBA Admission Records and Pre-Reg FormKathe Marren Sicat DuquesaNo ratings yet
- Vitamin D and Skin Diseases - A ReviewDocument12 pagesVitamin D and Skin Diseases - A ReviewMai Anh NguyễnNo ratings yet
- Sas 7-9Document7 pagesSas 7-9Jilkiah Mae Alfoja CampomanesNo ratings yet
- Project 3 Visual MappingDocument1 pageProject 3 Visual Mappingapi-593346566No ratings yet
- Truth and Healing Commission On Indian Boarding School Policies in The United States ActDocument37 pagesTruth and Healing Commission On Indian Boarding School Policies in The United States Actjen_benderyNo ratings yet
- TiroideDocument10 pagesTiroideRosália CoutadaNo ratings yet
- Test Bank For Emergency Care Emt 13th EditionDocument30 pagesTest Bank For Emergency Care Emt 13th EditionCharles Pando100% (40)
- Study of Risk Incidence and Mortality Associated WDocument8 pagesStudy of Risk Incidence and Mortality Associated WYulian 53No ratings yet
- Issue Brief: Re-Examining Hunger in The USDocument16 pagesIssue Brief: Re-Examining Hunger in The USAnnelise McGowanNo ratings yet
- Case of TuberculosisDocument5 pagesCase of TuberculosisSheryhan Tahir BayleNo ratings yet
- TOPIC 3.A Bag TechniqueDocument38 pagesTOPIC 3.A Bag TechniqueJayrelle D. Safran100% (1)
- Aadya Mishra - Horoscope AnalysisDocument11 pagesAadya Mishra - Horoscope Analysisastrologylover BanglaNo ratings yet
- Ok 936860629 Ok 11 Yds Mart 2019Document25 pagesOk 936860629 Ok 11 Yds Mart 2019gizemcetinNo ratings yet
- 9201 Mark Scheme Paper2 International Gcse Biology Jun22Document21 pages9201 Mark Scheme Paper2 International Gcse Biology Jun22asdf0% (1)
- Diode Laser T8 ProDocument32 pagesDiode Laser T8 ProAmine ManouNo ratings yet
- 8th Grade Vocabulary ListDocument1 page8th Grade Vocabulary ListsabrinaNo ratings yet
- Neurobiological Basis of PsychologyDocument62 pagesNeurobiological Basis of PsychologyJovelyn Morales JosolNo ratings yet