Professional Documents
Culture Documents
Photodynamic Therapy: Re Entry in The Treatment of Chronic Periodontitis: A Clinical Study
Photodynamic Therapy: Re Entry in The Treatment of Chronic Periodontitis: A Clinical Study
Uploaded by
salman khawarOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Photodynamic Therapy: Re Entry in The Treatment of Chronic Periodontitis: A Clinical Study
Photodynamic Therapy: Re Entry in The Treatment of Chronic Periodontitis: A Clinical Study
Uploaded by
salman khawarCopyright:
Available Formats
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.
134]
Original Article
Photodynamic Therapy: Re‑entry in the Treatment of Chronic
Periodontitis: A Clinical Study
A. Suchetha, Latha Govindappa, N. Sapna, S. M. Apoorva, B. M. Darshan, Salman Khawar
Department of Background: Periodontitis is an inflammatory disease of multifactorial origin
Abstract
Periodontology, DAPM RV
Dental College, Bengaluru,
affecting the supporting tissues of the periodontium. Photodynamic therapy (PDT)
Karnataka, India involves the photosensitizer dye and a light source to induce reactive oxygen
species (singlet oxygen) and causes destruction of microorganisms. Aim: The
aim of this study was to compare the efficacy of PDT with scaling and root
planing (SRP) and also to compare the efficacy of two different concentrations
of photosensitizer (methylene blue 0.005% and 0.01%) in the treatment of
chronic periodontitis. Materials and Methodology: Forty‑five patients affected
by moderate‑to‑severe chronic periodontitis were included in the study and were
divided into three groups. The clinical parameters, plaque index (PI), gingival
index (GI), and probing pocket depth were recorded at baseline, 1 month, and
3 months of time interval. After SRP, PDT was performed using methylene blue
dye (0.005% and 0.01%) and diode laser with 665 nm wavelength for 60 s.
Results: At 1 and 3 months after treatment, there were no statistically significant
differences between the groups with regard to reduction in PI, GI, and probing
pocket depth in all the three groups (P > 0.05). Conclusion: The additional
application of a single episode of PDT to SRP failed to result in an additional
improvement in terms of reduction in plaque score, GI score, and pocket probing
depth.
Keywords: Gingival index, periodontitis, photodynamic therapy, plaque index,
pocket probing depth, scaling and root planing
Clinical Relevance to Interdisciplinary Dentistry
• Photodynamic therapy (PDT) which can be used in the treatment of periodontitis
• PDT can be treated in the treatment of peri‑implantitis
• PDT can also be used in the disinfection of root canals.
Introduction it has some limitations and even with therapy, some
patients still have attachment loss probably due to the
P eriodontitis is an inflammatory disease, which
is characterized by the presence of gingival
inflammation, periodontal pocket formation, loss of
persistence of periodontal pathogens and subsequent
recolonization of the subgingival area, which pose
connective tissue and alveolar bone of the teeth that a challenge for the patient and the therapist in plaque
results from the extent of subgingival inflammation control.[3] Thus, the advent of other options to improve
induced by bacteria in the biofilm.[1] The main objective the effectiveness of periodontal therapy is needed due to
of periodontal therapy is to eliminate deposits of bacteria
Address for correspondence: Dr. Latha Govindappa,
and bacterial niches by removing the supragingival #45/1, 1st Main, 4th Cross, Chocolate Factory Road, Tavarekere,
and subgingival biofilms.[2] Although mechanical BTM 1st Stage, Bangalore - 560 029, Karnataka, India.
instrumentation is still regarded as important modality E‑mail: lathagldc@gmail.com
which forms the gold standard of periodontal therapy, This is an open access article distributed under the terms of the Creative Commons
Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak,
Access this article online and build upon the work non‑commercially, as long as the author is credited and the new
Quick Response Code: creations are licensed under the identical terms.
Website:
www.jidonline.com For reprints contact: reprints@medknow.com
How to cite this article: Suchetha A, Govindappa L, Sapna N, Apoorva SM,
DOI: Darshan BM, Khawar S. Photodynamic therapy: Re-entry in the
10.4103/jid.jid_74_16 treatment of chronic periodontitis: A clinical study. J Interdiscip
Dentistry 2017;7:15-22.
© 2017 Journal of Interdisciplinary Dentistry | Published by Wolters Kluwer ‑ Medknow 15
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.134]
Suchetha, et al.: Photodynamic therapy in the management of chronic periodontitis
limited access to furcation areas, concavities, grooves, the efficacy of PDT in the nonsurgical treatment of
distal sites of molars, and deep pockets found during chronic periodontitis with SRP and to compare the
conventional periodontal therapy.[4] The increase in efficacy of two different concentrations of methylene
bacterial resistance due to the use of systemic antibiotics blue (0.005% and 0.01%) photosensitizer.
could also justify the appearance of other adjuvants for
established periodontal treatment.[5,6] Materials and Methodology
Recent advances in technology have led to a constant A total of 45 patients having chronic
drive to develop novel approaches for the treatment of periodontitis (based on the 1999 Classification of
periodontal diseases. Photodynamic therapy (PDT) is Periodontal Diseases and Conditions) were selected from
also known as photoradiation therapy, phototherapy, or the outpatients visiting the Department of Periodontology,
photochemotherapy.[7] DAPM RV Dental College, Bengaluru. The ethical
clearance for the study was obtained from the Ethical
Phototherapy began in ancient Greece, Egypt, and Committee and review board of the institution. This
India and was disappeared for decades. The use of clinical study was conducted from October 2014 to April
contemporary PDT was first reported by Danish 2015. The patients of both sexes aged between 30 and
Physician, Niels Finsen. He successfully demonstrated 65 years, with a minimum of six teeth having periodontal
PDT by employing heat‑filtered light from carbon pocket depth of ≥5 mm and with no systemic conditions
arc lamp (The Finsen Lamp) in the treatment of lupus that would contraindicate routine periodontal procedures,
vulgaris. PDT was introduced in medical therapy in were included in the study. Patients with the following
the year 1904 as the light‑induced inactivation of cells, criteria were excluded from the study: patients who have
microorganisms, or molecules and is based on the received periodontal therapy within the past 6 months,
principle that a photosensitizer (i.e., a photoactivatable pregnant and lactating patients, patients who have taken
substance) binds to the target cells and can be activated antibiotics within 6 months period preceding study, teeth
by light of a suitable wavelength in the presence of exhibiting Class II and Class III mobility, smokers,
oxygen.[8] acute oral infections, and patients with known allergy to
PDT is an oxygen‑dependent photochemical reaction methylene blue dye. All participants signed the informed
that occurs upon exposure to a particular wavelength consent form after being informed about the treatment
of light in the presence of a suitable photosensitizer protocol.
dye. The various photosensitizer dyes were used Participants were divided into three groups as follows:
including (a) tricyclic dyes with different mesoatoms, • Group I (n = 15): Those to be treated with scaling
for example, acridine orange, proflavine, riboflavin, and root planning (SRP) only
methylene blue, toluidine blue, fluorescein, and • Group II (n = 15): Those to be treated with
erythrosine, (b) tetrapyrroles, for example, porphyrins, SRP + PDT (0.005% methylene blue) for the
derivatives, chlorophyll, phylloerythrin, and treatment of chronic periodontitis
phthalocyanines, and (c) furocoumarins, for example, • Group III (n = 15): Those to be treated with
psoralen and its methoxy derivatives, xanthotoxin, and SRP + PDT (0.01% methylene blue) for the treatment
bergapten. of chronic periodontitis.
The various light sources were utilized including lasers of All the patients were subjected to a full‑mouth periodontal
different wavelengths and nonlaser light sources such as examination at six sites per tooth (excluding the third
light emitting diodes. The photochemical reaction results molar). After oral hygiene instructions, all patients
in generation of cytotoxic species such as superoxide, received full‑mouth SRP under local anesthesia using both
hydroxyl radicals, hydrogen peroxide, and singlet oxygen. hand instruments and ultrasonic device. The following
Among these, reactive oxygen species (singlet oxygen) clinical parameters such as plaque index (PI) (Silness and
plays a major role in microbial destruction as it can Loe 1964), gingival index (GI) (Loe and Silness 1963),
interact with a large number of biological substrates and pocket probing depth (PPD) (using UNC 15 Probe)
inducing oxidative damage to the cell membrane and cell were recorded at baseline, 1 month, and 3 months. In
wall of bacteria, fungi, and viruses. Group II and III participants after thorough SRP, safety
goggles were provided to the patient, operator, and the
Various studies have used different concentrations of
assistant to prevent damage to the eyes by laser.
photosensitizer dye (0.01% or 0.005%), so the present
study was conducted to determine any variations in the Using a blunt needle, the methylene blue photosensitizer
outcome of different concentrations applied in the PDT solution with a concentration of 0.005% and 0.01%,
procedure. The present study was aimed at evaluating respectively, was applied to the base of the pocket, starting
16 Journal of Interdisciplinary Dentistry ¦ Volume 7 ¦ Issue 1 ¦ January-April 2017
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.134]
Suchetha, et al.: Photodynamic therapy in the management of chronic periodontitis
from the apical end of the pocket moving coronally to respectively, in Group I; 6.29 ± 1.08, 5.88 ± 1.35, and
avoid entrapment of air bubbles. Three minutes later, 5.05 ± 1.05, respectively, in Group II; and 6.40 ± 0.98,
all pockets were thoroughly rinsed with sterile saline to 5.65 ± 1.25, and 5.00 ± 1.02, respectively, in
remove the excessive photosensitizer. Immediately after Group III. The mean PPD was found to be statistically
rinsing, the diode laser (Sirona) with 660 nm wavelength significant among all the groups between all the time
and 1 mW of output equipped with a fiber optic probe intervals (P < 0.05); however, on intergroup comparison,
tip was placed at the depth of the pocket and moved the mean PPD was found to be statistically significant
circumferentially in sweeping motion around the teeth among all the groups (P ˃ 0.05). The result of PPD is
for 1 min as shown in Figures 1-4. Patients were recalled shown in Tables 5, 6 and Graphs 4‑6. On intergroup
after 1 month and 3 months posttherapy and all the comparison, the results of the study were statistically
clinical parameters were recorded. Statistical analysis was insignificant (P ˃ 0.05) [Tables 2, 4, 6 and Graphs 4‑6].
carried out by one‑way analysis of variance (ANOVA).
Discussion
Results Periodontitis being multifactorial in etiology results in
The mean PI scores at baseline, 1 month, and 3 months loss of supporting tissues of the periodontium and also
were 2.58 ± 0.20, 1.25 ± 0.15, and 1.08 ± 0.08, presents with therapeutic difficulties. Microbial plaque
respectively, in Group I; 2.37 ± 0.22, 1.19 ± 0.14, and accumulation is considered to be one of the main factors
1.04 ± 0.07 in Group II; and 2.31 ± 0.15, 1.15 ± 0.15, of this disease as bacteria have the ability to grow in
and 1.05 ± 0.07, respectively, in Group III. The mean biofilms and are beyond the reach of antimicrobial
PI was found to be statistically significant among all the chemical agents. In addition, the anatomical complexity
groups between all the time intervals (P < 0.05). The of tooth roots causes them to be predisposed to the
results of PI are shown in Tables 1, 2 and Graphs 1, 4‑6. development of many niches for bacterial deposits,
The mean GI scores at baseline, 1 month, and 3 months making eradication of periodontopathogens more difficult
were 2.30 ± 0.23, 1.18 ± 0.13, and 1.05 ± 0.05, both mechanically and chemically.
respectively, in Group I; 2.37 ± 0.18, 1.15 ± 0.13, and Furthermore, some periodontopathogens
1.07 ± 0.08, respectively, in Group II; and 2.26 ± 0.20, (e.g., Aggregatibacter actinomycetemcomitans and
1.22 ± 0.12, and 1.06 ± 0.08, respectively, in Group III. Porphyromonas gingivalis) can penetrate into and
The mean GI was found to be statistically significant persist in epithelial cells of the periodontal pockets and
among all the groups between all the time the gingiva, thus avoiding the efficacy of conventional
intervals (P < 0.05). The result of GI is shown in antimicrobial drugs. In addition, the systemic
Tables 3, 4 and Graphs 2, 4‑6.
The mean PPD scores at baseline, 1 month, and
3 months were 6.69 ± 1.07, 5.59 ± 1.23, and 5.53 ± 1.33,
Figure 2: Application of methylene blue and saline irrigation to remove
the excess dye
Figure 1: Preoperative pocket probing depth
Figure 3: Laser activation of methylene blue dye (photosensitizer) Figure 4: Three months of posttreatment probing photos
Journal of Interdisciplinary Dentistry ¦ Volume 7 ¦ Issue 1 ¦ January-April 2017 17
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.134]
Suchetha, et al.: Photodynamic therapy in the management of chronic periodontitis
antibiotic therapy is limited by the minimum inhibitory laser light (Sirona) with the wavelength of 660 nm was
concentration of the drug, which is difficult to achieve used at 1 mW of energy. The depth of penetration of
in gingival crevicular fluid and scarcely possible in laser light is ranging from 0.5 mm to 1.5 mm.
bacterial biofilms. Moreover, there is also a problem
In the present study, all the precautions were followed
of increasing bacterial resistance developing for the
to prevent the laser‑associated damages to the patient as
systemic antibiotics.[9‑12]
well as to the operator. The clinical parameters observed
Conventional treatment such as SRP does not completely are PI, GI, and PPD.[25] Data obtained by the study were
eliminate periodontal pathogens, especially in deep analyzed by using ANOVA followed by Bonferroni
periodontal pockets. Moreover, it does not prevent this post hoc analysis.
microorganism from penetrating into periodontal tissue.
The results obtained from this study showed that the
In addition, this predisposes the periodontal pockets to
mean PI scores at baseline, 1 month, and 3 months in
recolonization and recurrence of the disease.[13‑17]
Group I were 2.58 ± 0.20, 1.25 ± 0.15, and 1.08 ± 0.08,
PDT was discovered in the beginning of the 20th century respectively. In Group II, the mean PI scores at baseline,
and then implemented in medicine. It consists of 1 month, and 3 months were 2.37 ± 0.22, 1.19 ± 0.14,
three elements: harmless visible light, a nontoxic and 1.04 ± 0.07, respectively. In Group III, the mean
photosensitizer, and oxygen. It is based on the principle PI scores at baseline, 1 month, and 3 months were
that the photosensitizer (or photoactivatable substance) 2.31 ± 0.15, 1.15 ± 0.15, and 1.05 ± 0.07, respectively.
binds to the targeted cells and then can be activated by The mean PI was found to be statistically significant at
light of the appropriate wavelength in the presence of baseline (P < 0.05) between Group I and Group II but
oxygen. This results in the generation of singlet oxygen was statistically insignificant at 1 month and 3 months of
and free radicals, which are toxic to certain cells and time intervals (P ˃ 0.05) and was statistically insignificant
bacteria.[2,18‑21] at all‑time intervals in Group III (P ˃ 0.05). However,
when compared between Group II and Group III,
The mechanism of the action of antibacterial
Group II showed more reduction in PI scores at 1 month
PDT (aPDT) is that initially, a photosensitizer at ground
and 3 months of time interval comparatively. The results
state is activated to a highly energized triplet state by
obtained in the present study in plaque reduction scores
irradiation with the light of a certain wavelength. The
were in agreement with the studies conducted by Ge
excited photosensitizer has a longer lifetime, which
et al. and Berakdar et al.[25,26] In the present study, there
results in interactions with the surrounding molecules,
was no statistically significant reduction in plaque scores
and it is generally assumed that at the triplet state, the
observed.
generation of cytotoxic species occurs. The triplet‑state
photosensitizer reacts with biomolecules using two The results obtained in this study showed that the
different pathways (two types of reactions).[22] mean GI scores at baseline, 1 month, and 3 months in
Group I were 2.30 ± 0.23, 1.25 ± 0.15, and 1.08 ± 0.08,
Antimicrobial photosensitizers such as porphyrins,
respectively. In Group II, the mean PI scores at baseline,
phthalocyanines, and phenothiazines (e.g., methylene blue
1 month, and 3 months were 2.37 ± 0.22, 1.19 ± 0.14, and
and toluidine blue O) have been reported to penetrate
1.04 ± 0.07, respectively. In Group III, the mean GI scores
into Gram‑positive and Gram‑negative bacteria. The
at baseline, 1 month, and 3 months were 2.31 ± 0.15,
positive charge seems to promote the binding of the
1.15 ± 0.15, and 1.05 ± 0.07, respectively. The mean
photosensitizer to the Gram‑negative bacterial membrane
GI index score was found to be statistically significant
and leads to its localized damage, resulting in an
at baseline (P < 0.05) in Group I and Group II but was
increase in its permeability. Hence, toluidine blue O and
statistically insignificant at 1 month and 3 months of time
methylene blue are commonly used in aPDT.[23,24] Various
intervals (P ˃ 0.05) and was statistically insignificant at
studies have been conducted previously using different
all‑time intervals in Group III (P ˃ 0.05). However, when
concentrations of methylene blue, but there were no
compared between Group II and Group III, Group III
studies conducted to compare both concentrations.[25,26]
showed more reduction in GI scores at 1 month and
Hence, the present study was planned to evaluate the 3 months of time interval. The results obtained from this
efficacy of PDT with SRP, and also we compared the study were in agreement with the study conducted by
efficacy of two different concentrations of methylene de Oliveira et al.[27,28] In the present study, there was no
blue photosensitizer in PDT. statistically significant reduction in GI scores observed.
The methylene blue photosensitizer gets activated at a The results obtained from this study showed that the
wavelength of 660 nm to 720 nm of laser light which is mean PPD scores at baseline, 1 month, and 3 months in
in the red zone of light spectrum. In the present study, Group I were 6.69 ± 1.08, 5.88 ± 1.35, and 5.53 ± 1.33,
18 Journal of Interdisciplinary Dentistry ¦ Volume 7 ¦ Issue 1 ¦ January-April 2017
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.134]
Suchetha, et al.: Photodynamic therapy in the management of chronic periodontitis
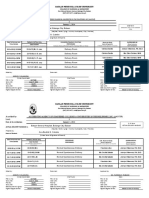
Table 1: Intragroup comparison of plaque index
Parameter Study group Time n Mean±SD Greenhouse‑Geisser Difference P
F P
Plaque index SRP Baseline 15 2.58±0.20 1 versus 2 768.493 <0.001* <0.001*
1 month 15 1.25±0.15 1 versus 3 <0.001*
2 months 15 1.08±0.08 2 versus 3 0.003*
SRP + PDT (0.005% MB) Baseline 15 2.37±0.22 394.535 <0.001* 1 versus 2 <0.001*
2 months 15 1.19±0.14 1 versus 3 <0.001*
3 months 15 1.04±0.07 2 versus 3 0.002*
SRP + PDT (0.01% MB) Baseline 15 2.31±0.15 437.912 <0.001* 1 versus 2 <0.001*
3 months 15 1.15±0.15 1 versus 3 <0.001*
4 months 15 1.05±0.07 2 versus 3 0.02*
1=Baseline, 2=1 month, 3=2 months. *Statistically significant. SRP=Scaling and root planing, PDT=Photodynamic therapy,
MB=Methylene blue, SD=Standard deviation
Table 2: Intergroup comparison of plaque index
Months Study groups n Mean±SD Minimum Maximum F P Difference P
Baseline SRP 15 2.58±0.20 2.07 2.86 8.396 0.001* 1 versus 2 0.02*
SRP + PDT (0.005%) 15 2.37±0.22 2.10 2.86 1 versus 3 0.001*
SRP + PDT (0.01%) 15 2.31±0.15 2.10 2.61 2 versus 3 1.00
1 month SRP 15 1.25±0.15 1.02 1.56 1.706 0.19 ‑ ‑
SRP + PDT (0.005%) 15 1.19±0.14 1.00 1.50 ‑ ‑
SRP + PDT (0.01%) 15 1.15±0.15 1.00 1.53 ‑ ‑
3 months SRP 15 1.08±0.08 1.00 1.22 1.404 0.26 ‑ ‑
SRP + PDT (0.005%) 15 1.04±0.07 1.00 1.22 ‑ ‑
SRP + PDT (0.01%) 15 1.05±0.07 1.00 1.22 ‑ ‑
*Statistically significant. SRP=Scaling and root planing, PDT=Photodynamic therapy, MB=Methylene blue, SD=Standard deviation
3.00 2.50
2.37
2.30
2.26
2.50 2.58
2.37 2.00
2.31
Mean Gingival Index
Mean Plaque Index
2.00
1.50
SRP SRP
1.50
SRP + PDT [0.005% MB] 1.18 SRP + PDT [0.005% MB]
1.25 1.15
1.00 1.22 1.05
1.19 SRP + PDT [0.01% MB] 1.06 SRP + PDT [0.01% MB]
1.00 1.15 1.08 1.07
1.05
1.04
0.50
0.50
0.00 0.00
BL 1 Month 2 Months BL 1 Month 2 Months
Graph 1: Intra group comparison of Plaque index (PI) Graph 2: Intra group comparison of Gingival index (GI)
respectively. In Group II, the mean PPD scores at with the study conducted by de Oliveira et al.[26,28] In
baseline, 1 month, and 3 months were 6.29 ± 1.07, the present study, there was no statistically significant
5.59 ± 1.23, and 5.05 ± 1.05, respectively. In Group III, reduction in probing pocket depth observed.
the mean PPD at baseline, 1 month, and 3 months were The results of the present study signify that the PDT
6.40 ± 0.98, 5.65 ± 1.25, and 5.00 ± 1.02, respectively. for the treatment of chronic periodontitis has similar
The mean PPD score was not found to be statistically outcome that of conventional therapy (SRP). In the
significant at all‑time intervals (P ˃ 0.05). However, present study, PDT did not show any added benefit over
when compared between Group II and Group III, SRP in the treatment of chronic periodontitis. In addition,
Group III showed more reduction in probing pocket depth there was no statistically significant difference in the two
at baseline and 1 month of time interval comparatively. concentrations of photosensitizer dye in the treatment
The results obtained from this study were in agreement outcome. Limitations of the study include small sample
Journal of Interdisciplinary Dentistry ¦ Volume 7 ¦ Issue 1 ¦ January-April 2017 19
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.134]
Suchetha, et al.: Photodynamic therapy in the management of chronic periodontitis
size, included in the study, short duration of observation, have a beneficial effect on the nonsurgical management
and single application of PDT. of chronic periodontitis, PDT as an adjunct to SRP did
not have any added benefit over the conventional SRP
Conclusion alone. However, PDT showed similar clinical outcome as
The results obtained from the present study concludes that of SRP, and there was no difference in the clinical
that the conventional mechanical therapy and SRP alone outcome of two different concentrations of methylene
8.00
8.00
6.69
6.40
6.29
7.00
7.00
6.69 SRP
6.40 6.00
6.00 6.29 5.88 SRP + PDT [0.005% MB]
Mean PPD Scores
5.59 5.53 5.00 SRP + PDT [0.01% MB]
Mean Scores
5.00 5.65
5.00 SRP
5.05 4.00
4.00
SRP + PDT [0.005% MB]
2.58
2.37
2.37
2.31
2.30
3.00
2.26
3.00 SRP + PDT [0.01% MB]
2.00
2.00
1.00
1.00
0.00
0.00
PI GI PPD
BL 1 Month 2 Months
Graph 4: Inter-group comparison at baseline
Graph 3: Intra group comparison of Probing pocket depth (PPD)
5.53
7.00
6.00
5.05
5.00
5.88
5.65
5.59
6.00 5.00
SRP SRP
5.00 SRP + PDT [0.005% MB] SRP + PDT [0.005% MB]
4.00
SRP + PDT [0.01% MB] SRP + PDT [0.01% MB]
Mean Scores
Mean Scores
4.00
3.00
3.00
2.00
2.00
1.08
1.07
1.06
1.25
1.05
1.05
1.04
1.22
1.19
1.18
1.15
1.15
1.00 1.00
0.00 0.00
PI GI PPD PI GI PPD
Graph 5: Inter-group comparison at 1 month Graph 6: Inter-group comparison at 3 months
Table 3: Intragroup comparison of gingival index
Parameter Study group Time n Mean±SD Greenhouse‑Geisser Difference P
F P
Gingival index SRP Baseline 15 2.30±0.23 323.298 <0.001* 1 versus 2 <0.001*
1 month 15 1.18±0.13 1 versus 3 <0.001*
2 months 15 1.05±0.05 2 versus 3 0.007*
SRP + PDT (0.005% MB) Baseline 15 2.37±0.18 511.817 <0.001* 1 versus 2 <0.001*
2 months 15 1.15±0.13 1 versus 3 <0.001*
3 months 15 1.07±0.08 2 versus 3 0.08
SRP + PDT (0.01% MB) Baseline 15 2.26±0.20 316.447 <0.001* 1 versus 2 <0.001*
3 months 15 1.22±0.12 1 versus 3 <0.001*
4 months 15 1.06±0.08 2 versus 3 <0.001*
1=Baseline, 2=1 month, 3=2 months. *Statistically significant. SRP=Scaling and root planing, PDT=Photodynamic therapy, MB=Methylene
blue, SD=Standard deviation
20 Journal of Interdisciplinary Dentistry ¦ Volume 7 ¦ Issue 1 ¦ January-April 2017
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.134]
Suchetha, et al.: Photodynamic therapy in the management of chronic periodontitis
Table 4: Intergroup comparison of gingival index
Months Study groups N Mean±SD Minimum Maximum F P
Baseline SRP 15 2.30±0.23 2.00 2.65 1.010 0.37
SRP + PDT (0.005%) 15 2.37±0.18 2.10 2.76
SRP + PDT (0.01%) 15 2.26±0.20 2.00 2.57
1 month SRP 15 1.18±0.13 1.00 1.46 0.954 0.39
SRP + PDT (0.005%) 15 1.15±0.13 1.01 1.50
SRP + PDT (0.01%) 15 1.22±0.12 1.01 1.40
3 months SRP 15 1.05±0.05 1.00 1.20 0.108 0.90
SRP + PDT (0.005%) 15 1.07±0.08 1.00 1.22
SRP + PDT (0.01%) 15 1.06±0.08 1.00 1.24
SRP=Scaling and root planing, PDT=Photodynamic therapy, MB=Methylene blue, SD=Standard deviation
Table 5: Intragroup comparison of pocket probing depth
Parameter Study group Time n Mean±SD Greenhouse‑Geisser Difference P
F P
Pocket probing depth SRP Baseline 15 6.69±1.08 24.640 <0.001*
1 versus 2 <0.001*
1 month 15 5.88±1.35 1 versus 3 <0.001*
2 months 15 5.53±1.33 2 versus 3 0.16
SRP + PDT (0.005% MB) Baseline 15 6.29±1.07 61.111 <0.001* 1 versus 2 <0.001*
2 months 15 5.59±1.23 1 versus 3 <0.001*
3 months 15 5.05±1.05 2 versus 3 0.001*
SRP + PDT (0.01% MB) Baseline 15 6.40±0.98 50.070 <0.001* 1 versus 2 <0.001*
3 months 15 5.65±1.25 1 versus 3 <0.001*
4 months 15 5.00±1.02 2 versus 3 0.002*
1=Baseline, 2=1 month, 3=2 months. *Statistically significant. SRP=Scaling and root planing, PDT=Photodynamic therapy, MB=Methylene
blue, SD=Standard deviation
Table 6: Intergroup comparison of pocket probing depth
Months Study groups N Mean±SD Minimum Maximum F P
Baseline SRP 15 6.69±1.08 5.00 8.50 0.606 0.55
SRP + PDT (0.005%) 15 6.29±1.07 5.00 8.20
SRP + PDT (0.01%) 15 6.40±0.98 5.00 8.20
1 month SRP 15 5.88±1.35 4.00 8.00 0.214 0.81
SRP + PDT (0.005%) 15 5.59±1.23 4.00 7.40
SRP + PDT (0.01%) 15 5.65±1.25 4.00 7.50
3 months SRP 15 5.53±1.33 3.00 7.50 1.007 0.37
SRP + PDT (0.005%) 15 5.05±1.05 4.00 7.00
SRP + PDT (0.01%) 15 5.00±1.02 4.00 7.00
SRP=Scaling and root planing, PDT=Photodynamic therapy, MB=Methylene blue, SD=Standard deviation
blue photosensitizer. PDT can be used as an adjunct root planing. J Clin Dent 2007;18:34‑8.
to SRP in the management of periodontitis. Further 2. Takasaki AA, Aoki A, Mizutani K, Schwarz F, Sculean A,
Wang CY, et al. Application of antimicrobial photodynamic
long‑term studies with large sample size are required to
therapy in periodontal and peri‑implant diseases. Periodontol
obtain predictable results. 2000 2009;51:109‑40.
Financial support and sponsorship 3. Del Peloso Ribeiro E, Bittencourt S, Sallum EA, Nociti FH
Jr., Gonçalves RB, Casati MZ. Periodontal debridement as a
Nil. therapeutic approach for severe chronic periodontitis: A clinical,
Conflicts of interest microbiological and immunological study. J Clin Periodontol
2008;35:789‑98.
There are no conflicts of interest. 4. Aoki A, Sasaki KM, Watanabe H, Ishikawa I. Lasers in
nonsurgical periodontal therapy. Periodontol 2000 2004;36:59‑97.
References 5. Ishikawa I, Aoki A, Takasaki AA, Mizutani K, Sasaki KM,
1. Andersen R, Loebel N, Hammond D, Wilson M. Treatment of Izumi Y. Application of lasers in periodontics: True innovation or
periodontal disease by photodisinfection compared to scaling and myth? Periodontol 2000 2009;50:90‑126.
Journal of Interdisciplinary Dentistry ¦ Volume 7 ¦ Issue 1 ¦ January-April 2017 21
[Downloaded free from http://www.jidonline.com on Friday, February 8, 2019, IP: 106.207.21.134]
Suchetha, et al.: Photodynamic therapy in the management of chronic periodontitis
6. Perussi JR. Photodynamic inactivation of microorganisms. New 18. Maisch T. Anti‑microbial photodynamic therapy: Useful in the
chwmistry 2007;30:988‑94. future? Lasers Med Sci 2007;22:83‑91.
7. Konopka K, Goslinski T. Photodynamic therapy in dentistry. 19. Maisch T, Szeimies RM, Jori G, Abels C. Antibacterial
J Dent Res 2007;86:694‑707. photodynamic therapy in dermatology. Photochem Photobiol Sci
8. von Tappeiner H, Jodlbauer A. About the effect of photodynamic 2004;3:907‑17.
substances on Protozoa and enzymes. Dtsches Arch Small Med 20. Sharman WM, Allen CM, van Lier JE. Photodynamic
1904;39:427‑87. therapeutics: Basic principles and clinical applications. Drug
9. Lamont RJ. In or out: The invasiveness of oral bacteria. Discov Today 1999;4:507‑17.
Periodontol 2000 2002;30:61‑9. 21. Wainwright M. Photodynamic antimicrobial chemotherapy
10. Mishima E, Sharma A. Tannerella forsythia invasion in oral (PACT). J Antimicrob Chemother 1998;42:13‑28.
epithelial cells requires phosphoinositide 3‑kinase activation and 22. Foote CS. Definition of type I and type II photosensitized
clathrin‑mediated endocytosis. Microbiology 2011;157):2382‑91. oxidation. Photochem Photobiol 1991;54:659.
11. Tribble GD, Lamont RJ. Bacterial invasion of epithelial cells and 23. Soukos NS, Goodson JM. Photodynamic therapy in the control
spreading in periodontal tissue. Periodontol 2000 2010;52:68‑83. of oral biofilms. Periodontol 2000 2011;55:143‑66.
12. Giannelli M, Formigli L, Lorenzini L, Bani D. Combined 24. Usacheva MN, Teichert MC, Biel MA. The interaction of
photoablative and photodynamic diode laser therapy as an lipopolysaccharides with phenothiazine dyes. Lasers Surg Med
adjunct to non‑surgical periodontal treatment: A randomized 2003;33:311‑9.
split‑mouth clinical trial. J Clin Periodontol 2012;39:962‑70. 25. Ge LH, Shu R, Shen MH. Effect of photodynamic therapy on
13. Ardila CM, Granada MI, Guzmán IC. Antibiotic resistance IL‑1beta and MMP‑8 in gingival crevicular fluid of chronic
of subgingival species in chronic periodontitis patients. periodontitis. Shanghai Kou Qiang Yi Xue 2008;17:10‑4.
J Periodontal Res 2010;45:557‑63. 26. Berakdar M, Callaway A, Eddin MF, Ross A, Willershausen B.
14. Bascones A, Noronha S, Gómez M, Mota P, Gónzalez Moles MA, Comparison between scaling‑root‑planing (SRP) and
Villarroel Dorrego M. Tissue destruction in periodontitis: SRP/photodynamic therapy: Six‑month study. Head Face Med
Bacteria or cytokines fault? Quintessence Int 2005;36:299‑306. 2012;8:12.
15. Giannobile WV. Host‑response therapeutics for periodontal 27. Meqa K, Disha M, Dragidella M, Sllamniku‑Dalipi Z. Evaluation
diseases. J Periodontol 2008;79 8 Suppl:1592‑600. of photodynamic therapy in the treatment of periodontitis. Open
16. Mombelli A, Cionca N, Almaghlouth A. Does adjunctive J Stomatol 2016;6:145‑54.
antimicrobial therapy reduce the perceived need for periodontal 28. de Oliveira RR, Schwartz‑Filho HO, Novaes AB Jr.,
surgery? Periodontol 2000 2011;55:205‑16. Taba M Jr. Antimicrobial photodynamic therapy in
17. Tester AM, Cox JH, Connor AR, Starr AE, Dean RA, Puente XS, the non‑surgical treatment of aggressive periodontitis:
et al. LPS responsiveness and neutrophil chemotaxis in vivo A preliminary randomized controlled clinical study.
require PMN MMP‑8 activity. PLoS One 2007;2:e312. J Periodontol 2007;78:965‑73.
22 Journal of Interdisciplinary Dentistry ¦ Volume 7 ¦ Issue 1 ¦ January-April 2017
You might also like
- Sample CPJE: Finasteride 1 MG Tablets #30 1 Tab P.O. Daily For Benign Prostatic HyperplasiaDocument12 pagesSample CPJE: Finasteride 1 MG Tablets #30 1 Tab P.O. Daily For Benign Prostatic HyperplasiaHerne Balberde78% (9)
- Case Study On Pre EclampsiaDocument21 pagesCase Study On Pre EclampsiaKavi rajput96% (24)
- Antimicrobial Photodynamic Therapy With Diode Laser and Methylene Blue As An Adjunct To Scaling and Root Planning A Clinical TrialDocument5 pagesAntimicrobial Photodynamic Therapy With Diode Laser and Methylene Blue As An Adjunct To Scaling and Root Planning A Clinical TrialFelipe AraujoNo ratings yet
- The Clinical Effect of Diode Laser in The Treatment of The Periodontal Pockets in Comparison With The Use of Photodynamic TherapyDocument18 pagesThe Clinical Effect of Diode Laser in The Treatment of The Periodontal Pockets in Comparison With The Use of Photodynamic TherapyAthenaeum Scientific PublishersNo ratings yet
- Yutaro Kitanaka Article PDFDocument23 pagesYutaro Kitanaka Article PDFNay AungNo ratings yet
- Effectiveness of Antimicrobial Photodynamic Therapy in The Periodontis Systematic ReviewDocument42 pagesEffectiveness of Antimicrobial Photodynamic Therapy in The Periodontis Systematic ReviewreizkayNo ratings yet
- 2 PDFDocument6 pages2 PDFEmaNo ratings yet
- JR PERIO Evaluation of The ReactiveDocument7 pagesJR PERIO Evaluation of The ReactivemediyantiNo ratings yet
- J PDPDT 2017 11 018Document15 pagesJ PDPDT 2017 11 018Yusuf DiansyahNo ratings yet
- Microorganisms 09 00713 v2Document15 pagesMicroorganisms 09 00713 v2Delia Guadalupe Gardea ContrerasNo ratings yet
- 9548 67097 1 PB PDFDocument7 pages9548 67097 1 PB PDFKarim KhedimNo ratings yet
- Periodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisDocument6 pagesPeriodontal Tray Application of Chlorine Dioxide Gel As An Adjunct To Scaling and Root Planing in The Treatment of Chronic PeriodontitisPhuong ThaoNo ratings yet
- Life 12 00370Document10 pagesLife 12 00370Mind Mapping Dept of Cons & EndoNo ratings yet
- Analyze The Clinical Effect of YAG Laser CombinedDocument9 pagesAnalyze The Clinical Effect of YAG Laser CombinedJose Luis AnayaNo ratings yet
- Javed 2013Document7 pagesJaved 2013Peter von TanNo ratings yet
- 10835-Article Text-51780-1-10-20220425Document9 pages10835-Article Text-51780-1-10-20220425Wilma Nurul AzizahNo ratings yet
- The Effect of Injectable Platelet-Rich Fibrin Use in TheDocument6 pagesThe Effect of Injectable Platelet-Rich Fibrin Use in TheNurul Fajriah YunitaNo ratings yet
- Comparison Between Antimicrobial Photodynamic Therapy and Low-Level Laser Therapy On Non-Surgical Periodontal Treatment A Clinical StudyDocument6 pagesComparison Between Antimicrobial Photodynamic Therapy and Low-Level Laser Therapy On Non-Surgical Periodontal Treatment A Clinical StudyFelipe AraujoNo ratings yet
- Photodiagnosis and Photodynamic Therapy: ReviewDocument7 pagesPhotodiagnosis and Photodynamic Therapy: ReviewCristian AndriescuNo ratings yet
- Comparison of Efficacy of Probiotics Versus.9Document6 pagesComparison of Efficacy of Probiotics Versus.9samanvi badriNo ratings yet
- Photo-Biomodulation in EndodonticsDocument7 pagesPhoto-Biomodulation in EndodonticsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Багрила концентрацииDocument12 pagesБагрила концентрацииМихаил ТаневNo ratings yet
- Comparative Evaluation of Locally Delivered.12Document7 pagesComparative Evaluation of Locally Delivered.12samanvi badriNo ratings yet
- ParoDocument8 pagesParoOctavian BoaruNo ratings yet
- J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineDocument57 pagesJ Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineKeHuyDietNo ratings yet
- Efficacy of Xanthan Based Chlorhexidine Gel As AnDocument5 pagesEfficacy of Xanthan Based Chlorhexidine Gel As AnMai ThúyNo ratings yet
- Chiniforush2016 PDT PDFDocument10 pagesChiniforush2016 PDT PDFShriya ShahuNo ratings yet
- Clinical Effectiveness of Diode Laser Therapy As An Adjunct To Non-Surgical Periodontal Treatment: A Randomized Clinical StudyDocument7 pagesClinical Effectiveness of Diode Laser Therapy As An Adjunct To Non-Surgical Periodontal Treatment: A Randomized Clinical StudyAnea MlinarNo ratings yet
- 1 s2.0 S1572100021003562 MainDocument6 pages1 s2.0 S1572100021003562 MainEduardo FernandezNo ratings yet
- Grzech-Leśniak2018 Article LaserReductionOfSpecificMicrooDocument10 pagesGrzech-Leśniak2018 Article LaserReductionOfSpecificMicrooeliasNo ratings yet
- Photobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureDocument18 pagesPhotobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureAbhishek NaikNo ratings yet
- Photobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureDocument18 pagesPhotobiomodulation in Endodontic, Restorative, and Prosthetic Dentistry: A Review of The LiteratureAbhishek NaikNo ratings yet
- OzonearticleDocument9 pagesOzonearticleسامر مضحيNo ratings yet
- Antibacterial Efficacy PH EWN Periodontal TreatmentDocument5 pagesAntibacterial Efficacy PH EWN Periodontal TreatmentSayabil AvendañoNo ratings yet
- Jurnal 2Document6 pagesJurnal 2Endy TiasNo ratings yet
- Wjoud 11 221Document5 pagesWjoud 11 221ReshmaaRajendranNo ratings yet
- Recent Advances in Clinical Periodontal DiagnosisDocument6 pagesRecent Advances in Clinical Periodontal DiagnosisSharmika SavanthNo ratings yet
- Toledano 2021 - Efficacy of Local Antibiotic Therapy in The Treatment of Peri-Implantitis A Systematic Review and Meta-AnalysisDocument9 pagesToledano 2021 - Efficacy of Local Antibiotic Therapy in The Treatment of Peri-Implantitis A Systematic Review and Meta-Analysissamusm.smNo ratings yet
- (PDF) Piperacillin-Tazobactam As An Adjuvant in The Mechanical Treatment of Patients With Periodontitis - A Randomized Clinical StudyDocument12 pages(PDF) Piperacillin-Tazobactam As An Adjuvant in The Mechanical Treatment of Patients With Periodontitis - A Randomized Clinical StudyAmruta MahajanNo ratings yet
- 5232 ArticleText 16212 2 10 201909291 PDFDocument5 pages5232 ArticleText 16212 2 10 201909291 PDFPutiNo ratings yet
- 2023 Efficacy of Adjunctive Measures in The Non-Surgical Treatment of Peri-Implantitis A Systematic ReviewDocument20 pages2023 Efficacy of Adjunctive Measures in The Non-Surgical Treatment of Peri-Implantitis A Systematic Reviewmatias cofreNo ratings yet
- Comparative Evaluation PF 1 Curcumin Solution and o 2 Chlorhexidine IrrigationDocument7 pagesComparative Evaluation PF 1 Curcumin Solution and o 2 Chlorhexidine Irrigationsamanvi badriNo ratings yet
- 2 ND JC PDF - SindhuDocument8 pages2 ND JC PDF - SindhuDadi SindhuNo ratings yet
- Probing Pocket Depth Reduction After Non Surgical Periodontal TherapyDocument11 pagesProbing Pocket Depth Reduction After Non Surgical Periodontal Therapymartesebastian081No ratings yet
- Impact of Periodontal Pocket Depth On The EfficienDocument7 pagesImpact of Periodontal Pocket Depth On The EfficienRonaldo PutraNo ratings yet
- Treatment Stage I-Iii J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineDocument57 pagesTreatment Stage I-Iii J Clinic Periodontology - 2020 - Sanz - Treatment of Stage I III Periodontitis The EFP S3 Level Clinical Practice GuidelineSofia Zaematul ArifahNo ratings yet
- Supportive Periodontal Therapy: July 2018Document8 pagesSupportive Periodontal Therapy: July 2018Alaghen VespanathanNo ratings yet
- Journal Homepage: - : IntroductionDocument9 pagesJournal Homepage: - : IntroductionIJAR JOURNALNo ratings yet
- Reconstructive Surgical Therapy of Peri-Implantitis: A Multicenter Randomized Controlled Clinical TrialDocument24 pagesReconstructive Surgical Therapy of Peri-Implantitis: A Multicenter Randomized Controlled Clinical Trialrmartins76No ratings yet
- Locally Administered Probiotic, RCT-articleDocument7 pagesLocally Administered Probiotic, RCT-articleDebjyoti DebnathNo ratings yet
- Jctres07202105003 EpubDocument18 pagesJctres07202105003 Epubسامر مضحيNo ratings yet
- Treatment of Stage I-III Periodontitis-The EFP S3 Level Clinical Practice GuidelineDocument57 pagesTreatment of Stage I-III Periodontitis-The EFP S3 Level Clinical Practice GuidelinePaulina Müller100% (1)
- 2794Document11 pages2794RodolfoDamásioNunesNo ratings yet
- Regeneration in Chronicperiodontitis-Casereports of OurdifferentproceduresDocument9 pagesRegeneration in Chronicperiodontitis-Casereports of Ourdifferentproceduresvishrutha purushothamNo ratings yet
- Cap 5Document22 pagesCap 5Elena DimitriuNo ratings yet
- Journal of Periodontology - 2022 - Andere - Open Flap Debridement Compared To Repeated Applications of Photodynamic TherapyDocument11 pagesJournal of Periodontology - 2022 - Andere - Open Flap Debridement Compared To Repeated Applications of Photodynamic TherapySalma HelmyNo ratings yet
- Chlorhexidine Oral Rinse Vs Povidone IodineDocument9 pagesChlorhexidine Oral Rinse Vs Povidone Iodineapi-733087623No ratings yet
- Systematic Review of Orthodontic Treatment ManagementDocument7 pagesSystematic Review of Orthodontic Treatment ManagementJuan AndradeNo ratings yet
- 1 s2.0 S0020653922001708 MainDocument11 pages1 s2.0 S0020653922001708 MainHONG JIN TANNo ratings yet
- Article MetaDocument13 pagesArticle MetaAkanksha SinghNo ratings yet
- Clinical Applications of Nuclear Medicine Targeted TherapyFrom EverandClinical Applications of Nuclear Medicine Targeted TherapyEmilio BombardieriNo ratings yet
- 978 613 4 99100 1Document69 pages978 613 4 99100 1salman khawarNo ratings yet
- Stain1 PDFDocument6 pagesStain1 PDFsalman khawarNo ratings yet
- Stain 2Document4 pagesStain 2salman khawarNo ratings yet
- New Doc 2019-02-08 10.51.43Document11 pagesNew Doc 2019-02-08 10.51.43salman khawarNo ratings yet
- Ijpi 2 (4) 136-140Document5 pagesIjpi 2 (4) 136-140salman khawarNo ratings yet
- Nsaids in PeriodontologyDocument7 pagesNsaids in Periodontologysalman khawarNo ratings yet
- Pengaruh Terapi Akupresur Dan Pijat Oksitosin Terhadap Peningkatan Produksi Asi Pada Ibu Postpartum Di Rsud JombangDocument10 pagesPengaruh Terapi Akupresur Dan Pijat Oksitosin Terhadap Peningkatan Produksi Asi Pada Ibu Postpartum Di Rsud Jombangriska yuniartiNo ratings yet
- Emergency Evacuation Plan For CradleDocument5 pagesEmergency Evacuation Plan For CradleAbraar AhmedhNo ratings yet
- Intermediate UveitisDocument33 pagesIntermediate UveitismitaamayNo ratings yet
- Parent Ver SCH 0 6yrsDocument2 pagesParent Ver SCH 0 6yrsSrinivasamurthy KamarthiNo ratings yet
- Anm 10102023Document53 pagesAnm 10102023MANISHNo ratings yet
- LeprosyDocument34 pagesLeprosySubhashish DasNo ratings yet
- Attending Physicians Statement-Death ClaimDocument2 pagesAttending Physicians Statement-Death ClaimKen CelesteNo ratings yet
- FddfsDocument3 pagesFddfshlkuy tiutytyNo ratings yet
- NHMSFAP As Post Anesthesia CareDocument11 pagesNHMSFAP As Post Anesthesia CareOktavia PutriNo ratings yet
- Essay About ObesityDocument1 pageEssay About ObesityNgọc Thảo0% (1)
- Potential Conflicts of Interest. All Authors:: Clinical Infectious Diseases 2018 66 (8) :1316-7Document2 pagesPotential Conflicts of Interest. All Authors:: Clinical Infectious Diseases 2018 66 (8) :1316-7Chikondi TemboNo ratings yet
- Tuberculous Mastitis A Case ReportDocument4 pagesTuberculous Mastitis A Case ReportLmao DNo ratings yet
- Chakra - Factors Associated With Complications of C DiffDocument8 pagesChakra - Factors Associated With Complications of C DiffCherry SmileNo ratings yet
- Letter To EditorDocument1 pageLetter To EditorPARIJAT CHAKRABORTYNo ratings yet
- ACHONDROPLASIADocument18 pagesACHONDROPLASIAJennie Mayaute AllcaNo ratings yet
- Standard Operating Procedure (SOP) Niacin TestDocument5 pagesStandard Operating Procedure (SOP) Niacin TestSuci IrianiNo ratings yet
- Medical Home: Care Coordination: The Patient-CenteredDocument23 pagesMedical Home: Care Coordination: The Patient-CenteredDwi Suranto100% (1)
- CefepimeDocument1 pageCefepimeTracy Megan RusillonNo ratings yet
- Electrocardiographic Monitoring 2017Document72 pagesElectrocardiographic Monitoring 2017Mirela Marina BlajNo ratings yet
- Smoking CessationDocument4 pagesSmoking CessationAimee GutierrezNo ratings yet
- Emotion Release ChiroDocument12 pagesEmotion Release ChiroEurico GonçalvesNo ratings yet
- 3 Date of Accreditation: January 1, 2014 Bataan General Hospital, Balanga City, BataanDocument3 pages3 Date of Accreditation: January 1, 2014 Bataan General Hospital, Balanga City, BataanArra BeatrizNo ratings yet
- Dental Students' Motivations and Perceptions of Dental Professional Career in IndiaDocument8 pagesDental Students' Motivations and Perceptions of Dental Professional Career in IndiaNiel Robert UyNo ratings yet
- Teks PidatoDocument5 pagesTeks Pidatorezpector9100% (1)
- 5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryDocument2 pages5 Minute Spotlight - Vacuum Extraction and Forceps DeliveryMikeNo ratings yet
- 58-File Utama Naskah-62-1-10-20200928Document8 pages58-File Utama Naskah-62-1-10-20200928Alfaera Rahma FarestyNo ratings yet
- Case 6 Abnormal PsychologyDocument4 pagesCase 6 Abnormal PsychologyPrincess Hannah Nicole LATNo ratings yet
- 664 8537 1 PBDocument5 pages664 8537 1 PBMICHAEL NUGROHONo ratings yet