Professional Documents
Culture Documents
Approach To Ecgs: Rhythm Check Rate
Approach To Ecgs: Rhythm Check Rate
Uploaded by
Ananda NadaradjaneOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Approach To Ecgs: Rhythm Check Rate
Approach To Ecgs: Rhythm Check Rate
Uploaded by
Ananda NadaradjaneCopyright:
Available Formats
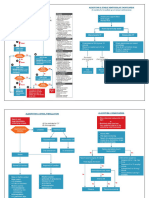
Approach to ECGs tachy/brady algorithm
Check Rate Rhythm
- Age, gender, name - 300 / big squares - RR only (1) P for every QRS and vv
- 25mm/s; 10mm/mV - #QRS in 10s x 6 (2) P +ve in I, II
- 1mm = 40ms; 0.1mV - 2 dots = 3s; #QRS in 6s x 10 (3) 60-100 bpm
Axis
- QRS +ve in I, II LAD
LAD: Inf MI, WPW, LVH, LBBB, LAFB
RAD
RAD: AntLat MI, WPW, RVH, RBBB,
LPFB, dextrocardia, normal
Intervals
- PR = 120-200ms (3-5 small boxes)
- HiPR: AV block (1,2,3)
- LoPR: WPW, ectopic atrial pacemaker
- QRS = <100-120ms (<2.5-3 small boxes)
- WideQRS: RBBB (V1/V2 rsr’; lat leads slurred S), LBBB(V5/V6 rS, qS; lat
leads rsr’), V-pacemaker, ↑K, ICD/pacer
- QTc <1/2 RR or M<420ms, F<440ms, no safe #, but >500 DANGER PR
- Short QT <300-360 ms: ↑Ca
QRS
- Long QT: “antis and hypos” - ABx, antipsychotics, antidepressants, TCA,
QT
antihistamines, antiarhythmics, hypo K, hypo Mg, congenital, MI, high ICP
Hypertrophy
- LAE = II - P wave >100ms (2.5 small boxes) OR V1 - P wave diphasic p mitrale
- RAE = II - P wave > 2.5 small boxes tall
Alternatively,
> 35mm if > 40yo R in V6 >26mm
- LVH = sum of R in V5 + S in V1 > 40mm if fit or 30-40yo R in I + S in III > 25mm
> 45mm if <30yo *R in avL > 11mm
- DDx: HTN, hypertrophic obstructive cardiomyopathy, aortic stenosis
- RVH = R>S or > 7mm in V1, R<S in V5/V6, RAD
- DDx: pulm HTN, mitral stenosis, pulmonic stenosis
- DDx +R in V1: RVH, RBBB, post MI, WPW, Duchenne musclar dystrophy, leads wrong
Mike Wong, uOttawa EM
Approach to ECGs - Ischemia *Always r/o STEMI first*
MI = BIomarkers + ECG or echo/angiogram findings
Pathologic Q - 1/3 height of QRS in 2 leads or 1 small box wide, can be new/old infarct
STEMI - J point STE >0.1mV in any 2 contiguous leads, except
V2-V3: ≥0.25mV men <40; ≥0.2mV men ≥40; ≥0.15mV women
DDx: Acute STEMI, Aortic dissection, PE, peri/myocarditis (diffuse STE, diffuse PR dep),
Takotsubo cardiomyopathy, Prinzmetal/vasospasm, LV aneurysm, LVH,
Pacer, LBBB, Brugada, hyperK, hyperCa, hypothermia
Differentiate STEMI > Classic STEMI localization:
Benign Early Repol (BER):
(1) II, III, avF inferior marginal R coronary
“Q2-R-ST4”
(2) V1, V2 septal proximal LAD
- Q waves, new
(3) V3, V4 anterior distal LAD
- QR-T complex ( sign)
(4) I, aVL, V5, V6 lateral circumflex
- Reciprocal change
(5) STD in V1-V3 posterior
- Straight/Convex STE
- III > II STE or T in V1>V6 Ischemia without acute occlusion (i.e. NSTEMI/UA)
- STE >25% of T in V6 does not localize!
- STE I and II is not STEMI
Repeat ECG r/o dynamic Δ
STEMI Equivalents / Don’t Miss Signs of Ischemia
- hyperacute T waves - broad, prominent asymmetrical, similar or bigger than QRS
- deWinter T waves - starts below isoelectric line; upsloping ST dep and peaked T in
precordial leads with STE in avR
- Wellen’s T - biphasic/deep-symmetric inverted T V2-4 can have no pain - LAD stenosis
- U wave inversion
- STE avR with diffuse depression - left main, prox LAD, 3VD, or general ischemia
- ST depression or T wave inversion in avL - early inferior MI
- R/S >1 or ST depression in V1-V2 - posterior infarct, get a 15 lead
- STE V1 > V2 or STE/isoelectric in V1 with depression in V2 - RV infarct
- New tall T wave in V1 - normal T is inverted in V1, unless LBBB/LVH/high voltage
Modified Sgarbossa’s Criteria for LBBB - any of:
≥ 1 lead with ≥1 mm of concordant ST elevation
≥ 1 lead of V1-V3 with ≥ 1 mm of concordant ST depression
≥ 1 lead with ≥ 1 mm STE and discordant STE ≥ 25% of the depth of S-wave.
DDx inverted T - Acute/old ischemia, HyperK, LVH, RVH, strain (PE, HOCM, etc.), BBB,
high voltage, Normal finding in children / persistent juvenile T wave, raised ICP
Mike Wong, uOttawa EM
Approach to ECGs - Tachy/Bradyarrhythmias
Arrhythmias
Brady < 60 Tachy >100 Wide
(1) VT - DANGER
(2) Sinus Tachy w/ BBB
(3) SVT w/ abberancy
Narrow N.B Afib + WPW - DANGER
(4) Vfib/flutter - DANGER
Regular Irregular
(1) Sinus tachycardia (1) A fib - absent P
(2) Atrial flutter (2) A flutter - w/ variable block
(3) SVTs - atrial/junctional (3) Multifocal atrial tachycardia (MAT)
tachy not from SA node - 3 different P waves in lead II
- treat with beta-agonist despite tachy
(1) Sinus bradycardia
(2) Sick Sinus Syndrome (runs of tachy/brady)
(3) SA node block - escaped beats
(4) SA node arrest - escape rhythms
(5) AV block
1° - long PR intervals >120-200ms from longer pause
2° - Mobitz I / Wenkebach - successively longer PR intervals (2:1, 3:2, 4:3, etc.)
2° - Mobitz II / Mobitz - 2:1, 3:1, 4:1, etc. - DANGER
3° - P running through QRS - DANGER
Narrow QRS - Proximal AV block (lower AV cells can function)
Wide QRS - Distal AV block - ventricular pacemaker
Mike Wong, uOttawa EM
Approach to ECGs - Syncope Syndromes
Electrolytes
↑K - brady, peak T, wide QRS, no P,
Rule out relevant tachy/brady- sine wave, “the great imitator”
arrhythmias, and consider ↓K - STdep, T inv, U wave, long P
these 8 syndromes ↑Ca - short QT, Osborn J (see below)
Brugada 1 - Coved ↓Ca - long QT via long ST
BE WHAT QT PiE STE >2mm in >1 of ↑Mg - assoc with ↑K, AV block
V1-V3 + negative T ↓Mg - long QT, assoc with↓K
ε Trifascicular block - RBBB,
LAFB/LPFB (see below), 1st
δ degree heart block
Long QT (>480-500ms)
Short QT (<360ms)
WPW - delta wave HOCM- dagger Q ARVD - epsilon wave, T
and short PR lat>inf leads, LVH, wave inversion, QRS PE: RBBB, S1Q3T3, tall R in V1,
LAE, giant T inversion widening/prolonged S RAE, RV strain (neg T V1-V4)
precordial wave V1-V3
associated
Appendix:
I / lat II / inf I / lat II / inf
Osborn J waves
DDx - ↑ Ca, hypothermia,
meds, SAH L Ant Fascicular Block (LAFB) L Post Fascicular Block (LPFB)
Left axis and lat qR, inf rS Right axis and lat rS, inf qR
*The above ECGs are sampled from litfl.com
Mike Wong, uOttawa EM
Approach to ECGs - VT vs. SVT - Wide Tachycardias
DDx = VT vs. SVT with BBB
All of the below are specific but not sensitive for VT:
- No RS complexes (i.e. entirely positive or negative) in V1-V6
- Absence of typical RBBB or LBBB morphology
- Extreme axis deviation (“northwest axis”) — QRS positive in aVR and negative in I + aVF.
- Very broad complexes (>160ms)
- AV dissociation (P and QRS complexes at different rates)
- Capture beats - a QRS complex of normal duration.
- Fusion beats - a sinus and ventricular beat coincides to produce a hybrid complex.
- Brugada’s sign – distance from onset of QRS complex to the nadir of the S-wave is > 100ms
- Josephson’s sign – Notching near the nadir of the S-wave
RSR’ complexes with a taller left rabbit ear. This is the most specific finding in favour of VT.
VT should be minimum120-130 bpm
Consider metabolic tachycardia if really wide (i.e. hyperkalemia, acidosis, etc.)
Lead II
Brugada sign (red) “Ultrasimple Brugada Criteria”
Big Left Rabbit Ear R wave to Peak Time (RWPT)
Josephson’s sign (blue)
>50ms specific for VT
*The above ECGs are sampled from litfl.com
Mike Wong, uOttawa EM
You might also like
- EKG Pocket GuideDocument2 pagesEKG Pocket GuideFabian Ramirez HincapiéNo ratings yet
- Relxation Meditation Script PDFDocument3 pagesRelxation Meditation Script PDFzainabNo ratings yet
- TH4-127 KreuzDocument113 pagesTH4-127 Kreuzakp892818No ratings yet
- ElectrocardiogramDocument11 pagesElectrocardiogramAbby BhevNo ratings yet
- Pharmacokinetic Exercises ListDocument5 pagesPharmacokinetic Exercises ListVijendra R100% (1)
- 2015 Acute and Chronic DiarrheaDocument25 pages2015 Acute and Chronic DiarrheaamirthaNo ratings yet
- 67 Success StoriesDocument72 pages67 Success StoriesPoorna Kalandhar100% (1)
- The PH Miracle DietDocument186 pagesThe PH Miracle DietAndre Smith90% (10)
- ECG Brief NotesDocument5 pagesECG Brief NotesKalpani Malsha UdawelagedaraNo ratings yet
- A Simplified ECG GuideDocument4 pagesA Simplified ECG Guidejalan_z96% (28)
- Waves and Intervals Heart Activity Normal/Abnormal (1 Small Box 0.04sec) (1 Big (5 Small) 0.2sec)Document6 pagesWaves and Intervals Heart Activity Normal/Abnormal (1 Small Box 0.04sec) (1 Big (5 Small) 0.2sec)Eben Ezar Dela CruzNo ratings yet
- A Simplified ECG GuideDocument4 pagesA Simplified ECG GuidekaelenNo ratings yet
- Ecg enDocument12 pagesEcg enKeep smileNo ratings yet
- Ekg Panum or OsceDocument69 pagesEkg Panum or OsceGladish RindraNo ratings yet
- This Document For Adult Patients Only. EKG Freq. 0.05-100 HZDocument1 pageThis Document For Adult Patients Only. EKG Freq. 0.05-100 HZLocke Helvet Laurie Kaicer100% (1)
- EKG Interpretation: UNS Cardiovascular Dept Medical Student Lecture SeriesDocument85 pagesEKG Interpretation: UNS Cardiovascular Dept Medical Student Lecture Seriesandina rosmalianti100% (1)
- Ecg For AnkiDocument3 pagesEcg For AnkijNo ratings yet
- ECGDocument33 pagesECGTamia PutriNo ratings yet
- ElectrocardiogramDocument169 pagesElectrocardiogramjitendra magarNo ratings yet
- 11 Steps of ECG - Ali Alnahari PDFDocument16 pages11 Steps of ECG - Ali Alnahari PDFBìnhNo ratings yet
- The Normal Adult ECGDocument84 pagesThe Normal Adult ECGkimiastroNo ratings yet
- 2 Februari 2018 EKGDocument24 pages2 Februari 2018 EKGDarren WilliamNo ratings yet
- EKG Interpretation: DR K P Tripathy Kims, BhubaneswarDocument58 pagesEKG Interpretation: DR K P Tripathy Kims, BhubaneswarAbhilash MohantyNo ratings yet
- EKG Interpretation 1Document56 pagesEKG Interpretation 1usmleusmle86No ratings yet
- ECG TutorialDocument40 pagesECG TutorialAnonymous HAbhRTs2TfNo ratings yet
- Kuliah EKG II Unswagati 2016Document77 pagesKuliah EKG II Unswagati 2016iikNo ratings yet
- CardiologyDocument149 pagesCardiologyMuhammad SyafiqNo ratings yet
- EKG Interpretation: UNC Emergency Medicine Medical Student Lecture SeriesDocument58 pagesEKG Interpretation: UNC Emergency Medicine Medical Student Lecture SeriesNathalia ValdesNo ratings yet
- EKG Interpretation Lecture 1 - Identifying The Squiggles, Developing A System For ReadingDocument6 pagesEKG Interpretation Lecture 1 - Identifying The Squiggles, Developing A System For Readingkcargen100% (1)
- Elektrokardiografi Dasar: Hendra ZufryDocument38 pagesElektrokardiografi Dasar: Hendra ZufryAndiNo ratings yet
- Elektro Kardio Grafi - Dasar - : DR Eka Ginanjar, SPPDDocument105 pagesElektro Kardio Grafi - Dasar - : DR Eka Ginanjar, SPPDalmiraerickaiNo ratings yet
- Kuliah Ekg UnswagatiDocument75 pagesKuliah Ekg UnswagatiiikNo ratings yet
- Pakya ECG BasicsDocument5 pagesPakya ECG BasicsFrederick CokroNo ratings yet
- EKG InterpretationDocument58 pagesEKG InterpretationHasnahdurrNo ratings yet
- EKG Interpretation: UNC Emergency Medicine Medical Student Lecture SeriesDocument58 pagesEKG Interpretation: UNC Emergency Medicine Medical Student Lecture SeriesanisaNo ratings yet
- EKG Interpretation: UNC Emergency Medicine Medical Student Lecture SeriesDocument58 pagesEKG Interpretation: UNC Emergency Medicine Medical Student Lecture SeriesHasnahdurrNo ratings yet
- EKG InterpretationDocument58 pagesEKG InterpretationIman Sama-aliNo ratings yet
- Basic Ecg Reading - McuDocument63 pagesBasic Ecg Reading - McuJofandAndrea MendozaNo ratings yet
- Ecg 6Document17 pagesEcg 6api-3757039No ratings yet
- Suatu Alat Laboratoris Alat Bantu DiagnosisDocument78 pagesSuatu Alat Laboratoris Alat Bantu DiagnosisAnonymous 3LwVkUsdNo ratings yet
- ECG, EEG &, EMG: 45 Notes To PGDocument6 pagesECG, EEG &, EMG: 45 Notes To PGskycall28No ratings yet
- Joseph Brian L. Costiniano, MD, DPCPDocument70 pagesJoseph Brian L. Costiniano, MD, DPCPcarmsNo ratings yet
- Suatu Alat LaboratorisDocument78 pagesSuatu Alat LaboratorisHematology 2016No ratings yet
- Hendra - EKGDocument34 pagesHendra - EKGRINANo ratings yet
- 5 ECG Interpretation With AnswersDocument48 pages5 ECG Interpretation With AnswersQusai Ibraheem100% (1)
- EKG Interpretation: Amir Aziz AlkatiriDocument51 pagesEKG Interpretation: Amir Aziz AlkatiriShabrina Sari MedinaNo ratings yet
- 16-Handout - ECG Interpretation (Study This)Document38 pages16-Handout - ECG Interpretation (Study This)Sa GhNo ratings yet
- I. Systematic Approach To ECG InterpretationDocument11 pagesI. Systematic Approach To ECG Interpretationkilladim992No ratings yet
- ECG InterpretationDocument83 pagesECG InterpretationJuana Maria Garcia Espinoza100% (2)
- Suatu Alat Laboratoris Alat Bantu DiagnosisDocument78 pagesSuatu Alat Laboratoris Alat Bantu DiagnosisMohammad AlmuhaiminNo ratings yet
- Kursus Ekg DR Ismi-1Document78 pagesKursus Ekg DR Ismi-1Sekar Ayu WulandariNo ratings yet
- 5hypertrophy and MIDocument116 pages5hypertrophy and MIsamooanatenaNo ratings yet
- All EcgDocument143 pagesAll EcgYenza FaheraNo ratings yet
- ELECTROCARDIOGRAPHYDocument75 pagesELECTROCARDIOGRAPHYMeliaNo ratings yet
- ECG TutorialDocument102 pagesECG Tutorialepic sound everNo ratings yet
- Materi Dasar EkgDocument52 pagesMateri Dasar EkgFirsandiPrasastyaFikryGozali100% (2)
- Interpretasi ElektrokardiogramDocument36 pagesInterpretasi ElektrokardiogramendahNo ratings yet
- How To: Read ECG?Document63 pagesHow To: Read ECG?Let BNo ratings yet
- Basic EKGDocument76 pagesBasic EKGradiologoa1aprilNo ratings yet
- 37 7-PDF EcDocument1 page37 7-PDF EcLwin Maung Maung ThikeNo ratings yet
- Basics of ECG: By-Pallavi ChicholikarDocument115 pagesBasics of ECG: By-Pallavi ChicholikarBhakti WashilkarNo ratings yet
- Paeds ECG InterpretationDocument28 pagesPaeds ECG InterpretationMuhammad Moazzam GulzarNo ratings yet
- Essential Cardiac Electrophysiology: The Self-Assessment ApproachFrom EverandEssential Cardiac Electrophysiology: The Self-Assessment ApproachNo ratings yet
- Blood Pressure: Protocol About Blood PDocument2 pagesBlood Pressure: Protocol About Blood PconheoconNo ratings yet
- Pathogenic Effects of Twelve Signs of The ZodiacDocument6 pagesPathogenic Effects of Twelve Signs of The ZodiacParamNo ratings yet
- PFAMCDocument12 pagesPFAMCDESTYANNo ratings yet
- Motor Assessment ScaleDocument20 pagesMotor Assessment ScaleSyeda WaniyaNo ratings yet
- Essential Medicines List: 2007 Cook IslandsDocument34 pagesEssential Medicines List: 2007 Cook IslandsportosinNo ratings yet
- Shock TypesDocument25 pagesShock TypesMuqeet76No ratings yet
- Report Employee Training IPCDocument11 pagesReport Employee Training IPCDandi RawhideNo ratings yet
- Azimor - 250 TabletsDocument1 pageAzimor - 250 TabletsRakesh PalNo ratings yet
- Pityriasis AlbaDocument7 pagesPityriasis AlbaAri Kurniawan100% (1)
- Calendario InsanityDocument2 pagesCalendario InsanityyujoeyNo ratings yet
- ST Johns Tel DirectoryDocument1 pageST Johns Tel DirectoryeshariffNo ratings yet
- Alpha and Beta ThalassemiaDocument6 pagesAlpha and Beta ThalassemiaSi vis pacem...100% (1)
- DR AZAM Penyimpanan UbatanDocument11 pagesDR AZAM Penyimpanan UbatanZakaria YahayaNo ratings yet
- Zoology Notes: 011 Chapter 7Document4 pagesZoology Notes: 011 Chapter 7humanupgradeNo ratings yet
- HTB-14 Product Sheet - U-87 MGDocument6 pagesHTB-14 Product Sheet - U-87 MGBiopharma GuruNo ratings yet
- Ld-Anoop Full Moth Rehab / Orthodontic Courses by Indian Dental AcademyDocument279 pagesLd-Anoop Full Moth Rehab / Orthodontic Courses by Indian Dental Academyindian dental academyNo ratings yet
- Growth Hormone Responses To Sub-Maximal and Sprint Exercise: Keith StokesDocument14 pagesGrowth Hormone Responses To Sub-Maximal and Sprint Exercise: Keith StokesganduaffNo ratings yet
- OJOLNS-10 - II - Interlay Myringoplasty PDFDocument7 pagesOJOLNS-10 - II - Interlay Myringoplasty PDFAnonymous ST1Ot2GAHx100% (1)
- Hematology ReviewDocument4 pagesHematology ReviewAlfred ChowNo ratings yet
- Flowchart - Medical Pathways 2014Document2 pagesFlowchart - Medical Pathways 2014Hillaryy K JongNo ratings yet
- E-PrepTalk Aug 2009Document73 pagesE-PrepTalk Aug 2009tharkibudhauNo ratings yet
- Injuries Around Leg: DR Abhishek Pathak Asst. Prof Deptt of Orthopaedics & Traumatology Gandhi Medical College BhopalDocument43 pagesInjuries Around Leg: DR Abhishek Pathak Asst. Prof Deptt of Orthopaedics & Traumatology Gandhi Medical College BhopaldrabhishekorthoNo ratings yet
- Tackling FatigueDocument7 pagesTackling FatigueAnurrag KumarNo ratings yet
- Claims - Evidence - Reasoning (C-E-R) Writing Graphic Organizer / 7thDocument4 pagesClaims - Evidence - Reasoning (C-E-R) Writing Graphic Organizer / 7thToot ScootNo ratings yet
- Nutrition Analysis ProjectDocument10 pagesNutrition Analysis Projectapi-268293649No ratings yet