Professional Documents
Culture Documents
Revised NCP (Baiae)
Revised NCP (Baiae)
Uploaded by
Jennifer BactatOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Revised NCP (Baiae)
Revised NCP (Baiae)
Uploaded by
Jennifer BactatCopyright:
Available Formats
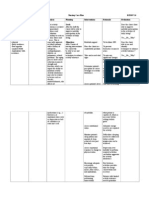
ASSESSMENT
NURSING DIAGNOSIS
Ineffective airway clearance related to bronchospasm and increase production of mucus secretions
PLANNING
NURSING INTERVENTION
y INDEPENDENT: 1. Auscultate breath sounds. Note adventitious breath sounds.
RATIONALE
EVALUATION
SUBJECTIVE: Medyo inuubo pa po ako as verbalized by the patient OBJECTIVE:
After nursing intervention, the patient will improve airway clearance and can demonstrate behaviors to improve her condition.
1. Some degree of bronchospasms present with obstructions in airway and may/may not be manifested in adventitious breath sounds. 2. To serve as s baseline data.
-wheezing upon expiration -V/S:
BP100/70mmHg T- 36 c PR- 71bpm RR- 18 bpm
2. Assess/Monitor respiratory rate. Note respiratory/expiratory ratio. 3. Advise high or semi fowlers position
After nursing intervention, the patient can improve airway clearance and can demonstrate coughing effectively and expectorating secretions.
3. Elevation of the head of the bed facilitates respiratory function by use of gravity and for optimum lung expansion. 4. Precipitators of allergic type of respiratory reactions that can trigger/exacerbate onset of acute episodes. 5. Provide patient with some means
4. Keep environmental pollution to a minimum.
5. Encourage/assist with pursed-lip
breathing exercises.
to cope with control dyspnea and reduce airtrapping. 6. Cough can be persistent but ineffective. Especially if patient coughing is most effective in an upright or in a head-down position after chest percussion. 7. Hydration helps decrease the viscosity of secretions, facilitating expectorations. Using warm liquids may decrease bronchospasm. fluids during meals can increase gastric distention and pressure on the diaphragm.
6. Observe characteristics of cough. Assist with measures to improve effectiveness of cough effort.
7. Increase fluid intake within cardiac tolerance. Provide warm liquids. Recommend intake of fluids between, instead during, meals.
y DEPENDENT:
1. Administer medications as ordered by the doctor.
1. Antibiotics may be prescribed to treat the infection.
y COLLABORATIVE:
1. Assist in
administering nebulizer, as indicated.
1. This ensures adequate delivery of medications to the airways.
ASSESSMENT
NURSING DIAGNOSIS Ineffective breathing pattern related to constricted bronchial walls secondary to bronchospasm as evidenced by presence of mucus secretion
PLANNING
NURSING INTERVENTION
y INDEPENDENT: 1. Establish rapport.
RATIONALE
EVALUATION
OBJECTIVE: -wheezing upon expiration -fatigue -V/S:
BP100/70mmHg T- 36 c PR- 71bpm RR- 18 bpm
After nursing intervention, the patient will demonstrate breathing exercises.
1. To gain patient trust. 2. To obtain baseline Data 3. Serve to track important changes
2. Assess patients condition.
After nursing intervention, the patient can demonstrate breathing exercises.
3. Vital signs monitored and recorded.
4. Auscultate breath sounds and assess airway pattern
4. To check for the presence of adventitious breath sounds 5. To minimize difficulty in breathing
5. Elevate head of the bed and change the position of the pt. every 2 hours. 6. Encourage deep breathing and coughing exercises. 7. Demonstrate pursed-lip breathing.
6. To maximize effort for expectoration. 7. To decrease air
trapping and for efficient breathing. 8. Encourage increase in fluid intake 9. Encourage opportunities for rest and limit physical activities. 8. To prevent fatigue.
9. To prevent situations that will aggravate the condition
ASSESSMENT
NURSING DIAGNOSIS Infection related to inadequate primary defenses (stasis of secretions)
PLANNING
NURSING INTERVENTION
y INDEPENDENT: 1. Review importance of breathing exercises, effective cough, frequent position changes, and adequate fluid intake.
RATIONALE
EVALUATION
OBJECTIVE: -with mucus secretion - Lab. Test: WBC13,800 (8,00010,000)
After nursing intervention, the patient will expectorate the sputum
1. These activities promote mobilization and expectoration of secretions to reduce risks of developing pulmonary infection. 2. Odorous, yellow, or greenish secretions suggest the presence of pulmonary infection. 3. Prevents spread of fluid-borne pathogens.
After nursing intervention, the patient can expectorate the sputum
2. Observe color, character and odor of sputum.
3. Demonstrate and assist patient in disposal of tissues and sputums. Also proper handwashing and use gloves when handling/disposing of tissues, sputum containers. 4. Encourage balance between activity and rest.
4. Reduces oxygen consumption/demand imbalance, and improve patients resistance to infection, promoting healing. 5. Malnutrition can affect general wellbeing and lower-
5. Discuss need for adequate nutritional intake.
resistance to infection. 6. Recommend rinsing mouth with water and spitting, not swallowing. 6. Reduces localized immunosuppressive effect of drug and risk of oral candidiasis.
y DEPENDENT: 1. Administer antimicrobials as indicated.
1. May be given for specific organisms identified by culture sensitivity because of high risk.
ASSESSMENT
NURSING DIAGNOSIS Risk for imbalanced nutrition, less than body requirements related to decrease appetite due to present condition
PLANNING
NURSING INTERVENTION
y INDEPENDENT: 1. Assess dietary habits, recent food intake.
RATIONALE
EVALUATION
After nursing intervention, the patient will ingest daily nutritional requirements in accordance with her activity level and metabolic needs and will demonstrate behaviors changes to regain weight.
1. Patient in acute respiratory distress is often anorectic because of dyspnea, sputum production and medication. 2. To not aggravate the patients condition.
2. Instruct the diet indicated for her condition.
3. Give frequent oral care, remove expectorated secretions promptly, provide specific container for disposal of secretions. 4. Encourage a rest period of 1hr. before and after meals. Provide frequent small feedings. 5. Avoid gas-producing foods and carbonated beverages.
3. Noxious tastes, smells, and sights are prime deterrents to appetite and can produce N&V with increased respiratory difficulty. 4. Helps reduce fatigue during mealtime, and provide opportunity to increase total caloric intake. 5. Can produce abdominal distension, which hampers abdominal breathing and diaphragmatic
After nursing intervention, the patient can able to ingest her nutritional requirements in accordance with her activity level and metabolic needs and can demonstrate behaviors changes to regain weight
movement and can increase dyspnea. 6. Avoid very hot or very cold foods. 6. Extremes in temp. can precipitate/aggravate coughing spasms. 7. Useful in setting weight goal and evaluating adequacy of nutritional plan.
7. Weight as indicated.
You might also like
- NCP BronchopneumoniaDocument8 pagesNCP BronchopneumoniaCrisantaCasliNo ratings yet
- Medical Management For PneumoniaDocument2 pagesMedical Management For PneumoniaSue Elaine100% (1)
- Dengue Fever Health TeachingDocument3 pagesDengue Fever Health TeachingDante Sales100% (3)
- Nursing Theory: Asthma (Presentation)Document13 pagesNursing Theory: Asthma (Presentation)vinda astri permatasari100% (1)
- NCP BaiaeDocument7 pagesNCP BaiaeJonathan Delos ReyesNo ratings yet
- Acute Pain Related To Body Response To An Infective AgentDocument2 pagesAcute Pain Related To Body Response To An Infective AgentSheril Sularte CasanesNo ratings yet
- Assignment For Oxy. Online BasedDocument5 pagesAssignment For Oxy. Online BasedNurhassem Nor AkangNo ratings yet
- NCP Micu Hascvd Cad - RioDocument5 pagesNCP Micu Hascvd Cad - RioRio BonifacioNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care Planapi-309251523No ratings yet
- Asthma Nursing Care Plan NCP Ineffective Airway Clearance CompressDocument2 pagesAsthma Nursing Care Plan NCP Ineffective Airway Clearance CompressMargarette GeresNo ratings yet
- Baiae NCPDocument1 pageBaiae NCPreignyfayeNo ratings yet
- Nursing History and Gordon'sDocument2 pagesNursing History and Gordon'sCarlo bersamiraNo ratings yet
- Simple Schematic Diagram of PneumoniaDocument1 pageSimple Schematic Diagram of PneumoniaJason A. AdoyoganNo ratings yet
- NCP Ineffective Airway ClearanceDocument1 pageNCP Ineffective Airway Clearancejae_007No ratings yet
- Peritonsillar AbscessDocument2 pagesPeritonsillar AbscessKevin Leo Lucero AragonesNo ratings yet
- CARE PLAN For BRONCHIECTASISDocument8 pagesCARE PLAN For BRONCHIECTASISCecil MonteroNo ratings yet
- Module 12Document12 pagesModule 12mirai desuNo ratings yet
- 3 NCP AsthmaDocument6 pages3 NCP AsthmajaninenicoleNo ratings yet
- Anatomy and Physiology PneumoniaDocument4 pagesAnatomy and Physiology PneumoniaJohnson MallibagoNo ratings yet
- Scribd 020922 Case Study-Oncology A&kDocument2 pagesScribd 020922 Case Study-Oncology A&kKellie DNo ratings yet
- HTP of AsthmaDocument1 pageHTP of AsthmaMarland Faith Dela CruzNo ratings yet
- Cholecystectomy Nursing Care Plan: Intraoperative Problem: Risk For AspirationDocument1 pageCholecystectomy Nursing Care Plan: Intraoperative Problem: Risk For AspirationJess GoNo ratings yet
- Fistula NCPDocument1 pageFistula NCPHasna LisnaNo ratings yet
- Impaired Gas Exchange PneumoniaDocument2 pagesImpaired Gas Exchange PneumoniaShanice BedecirNo ratings yet
- Transcultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodDocument5 pagesTranscultural Perspective in The Nursing Care of Adults Physiologic Development During AdulthoodeuLa-mayzellNo ratings yet
- Diet: Bath: ActivityDocument2 pagesDiet: Bath: ActivityKristian Karl Bautista Kiw-isNo ratings yet
- Discharge PlanDocument1 pageDischarge PlanBernalene SyNo ratings yet
- This Study Resource Was Shared Via: Nursing Care Plan FormDocument3 pagesThis Study Resource Was Shared Via: Nursing Care Plan FormissaiahnicolleNo ratings yet
- FINALS ReviewerDocument14 pagesFINALS ReviewerJustine Simeon lagunzadNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care Planusama_salaymehNo ratings yet
- RRLDocument4 pagesRRLAnnalyn MantillaNo ratings yet
- Ineffective Airway ClearanceDocument6 pagesIneffective Airway ClearanceBenly Grace Rebuyon MosquedaNo ratings yet
- Occurs Most Often In:: Muscular DystrophyDocument4 pagesOccurs Most Often In:: Muscular DystrophyJiezl Abellano AfinidadNo ratings yet
- NCP BMDocument1 pageNCP BMSourabh MehraNo ratings yet
- Drug Studies and Health Teaching PlanDocument28 pagesDrug Studies and Health Teaching PlansfkjalkhsafgNo ratings yet
- NCP For CAP TB.Document5 pagesNCP For CAP TB.Cherry Ann BalagotNo ratings yet
- Pulmonary Tuberculosis: A Case Study ofDocument28 pagesPulmonary Tuberculosis: A Case Study ofDyanne BautistaNo ratings yet
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasNo ratings yet
- Health Teaching Plan For CKDDocument1 pageHealth Teaching Plan For CKDInah Floresta Besas100% (1)
- Ineffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaDocument3 pagesIneffective Breathing Pattern As Evidenced by Use of Accessory Muscles and Episodes of DyspneaNiel MinatozakiNo ratings yet
- NCPDocument5 pagesNCPMcmc Ryan Ferdinand GutierrezNo ratings yet
- Drug Study of TBDocument7 pagesDrug Study of TBMarc AntonioNo ratings yet
- Im Case Study 04Document49 pagesIm Case Study 04Shaine BalverdeNo ratings yet
- NCP (Risk of Infection Related To Episiotomy)Document3 pagesNCP (Risk of Infection Related To Episiotomy)Paolo UyNo ratings yet
- NCP - ERDocument5 pagesNCP - ERAnnelore ArcayNo ratings yet
- Impaired Gas ExchangeDocument10 pagesImpaired Gas ExchangeWardinatul ImanNo ratings yet
- Developmental HistoryDocument2 pagesDevelopmental HistoryShulamaye VelascoNo ratings yet
- CHN Journal ReadingDocument4 pagesCHN Journal ReadingKrizle AdazaNo ratings yet
- ANATOMY AND PHYSIOLOGY of RabiesDocument5 pagesANATOMY AND PHYSIOLOGY of RabiesDavid CalaloNo ratings yet
- NCP PTBDocument6 pagesNCP PTBJay Dela VegaNo ratings yet
- Nursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy MalaiseDocument1 pageNursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy Malaise06eltianNo ratings yet
- Case Study AppendicitisDocument6 pagesCase Study AppendicitisPrincess Camille ArceoNo ratings yet
- NCP #2Document4 pagesNCP #2Nutz TolentinoNo ratings yet
- NCP For AsthmaDocument2 pagesNCP For AsthmawaadNo ratings yet
- Pneumonia NCPDocument10 pagesPneumonia NCPDIAZ Candy AliahNo ratings yet
- The Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeFrom EverandThe Ride of Your Life: What I Learned about God, Love, and Adventure by Teaching My Son to Ride a BikeRating: 4.5 out of 5 stars4.5/5 (2)
- Ncp'sDocument8 pagesNcp'sDuchess Kleine RafananNo ratings yet
- NCPDocument4 pagesNCPAbegail Abaygar100% (1)
- NCP Kochs2Document2 pagesNCP Kochs2Ava VierNo ratings yet
- Drug Study and NCP!Document8 pagesDrug Study and NCP!Abegail Abaygar100% (1)