Professional Documents
Culture Documents
OS - Key Points by Danesh PDF
OS - Key Points by Danesh PDF
Uploaded by
Noor Haider0 ratings0% found this document useful (0 votes)
84 views16 pagesThis document provides key points related to oral surgery. It includes definitions of various oral surgery terms and procedures. Some key points include:
- Radiotherapy can cause delayed healing and less vascularity in the oral mucosa.
- Trigeminal neuralgia causes sharp, lancinating pain on one side of the face not relieved by analgesics.
- Common side effects of cancer chemotherapy include anemia and thrombocytopenia due to myelosuppression.
- Pan sinusitis is inflammation of all para nasal sinuses simultaneously.
Original Description:
Original Title
OS-- Key Points by Danesh (1).pdf
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThis document provides key points related to oral surgery. It includes definitions of various oral surgery terms and procedures. Some key points include:
- Radiotherapy can cause delayed healing and less vascularity in the oral mucosa.
- Trigeminal neuralgia causes sharp, lancinating pain on one side of the face not relieved by analgesics.
- Common side effects of cancer chemotherapy include anemia and thrombocytopenia due to myelosuppression.
- Pan sinusitis is inflammation of all para nasal sinuses simultaneously.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
84 views16 pagesOS - Key Points by Danesh PDF
OS - Key Points by Danesh PDF
Uploaded by
Noor HaiderThis document provides key points related to oral surgery. It includes definitions of various oral surgery terms and procedures. Some key points include:
- Radiotherapy can cause delayed healing and less vascularity in the oral mucosa.
- Trigeminal neuralgia causes sharp, lancinating pain on one side of the face not relieved by analgesics.
- Common side effects of cancer chemotherapy include anemia and thrombocytopenia due to myelosuppression.
- Pan sinusitis is inflammation of all para nasal sinuses simultaneously.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 16
Oral Surgery Key Points
Compiled by Danesh Kumar-SIOHS/ Jinnah Sindh Medical University
• Long term effect of radiotherapy to oral mucosa is characterized by---Break down & delayed healing,
sub mucosa less vascular.
• Sharp, lancinating pain on right side of face, not relieved by anaelgesics---Trigeminal neuralgia.
• Common sequela after cancer chemotherapy is myelosuppression, which is characterized by--
Anemia& thrombocytopenia.
• Inflammation of most or all of the Para nasal sinuses simultaneously is---Pan sinusitis.
• Maxillary sinus infection of odontogenic origin is most commonly caused by--Anaerobic bacteria.
• Major duct of submandibular gland is--- Wharton’s duct.
• In WINTER’S classification, white line tells us----Angulation of the impacted tooth
• Complication may result from injury to auriculotemporal nerve during removal of parotid tumor---
Gustatory sweating.
• Maxillary sinus is usually involved in fractures—Lefort 1
• Stenson’s duct opens opposite the—upper 2nd molar
• Aspirin--- increase bleeding time
• Cross bar elevator works on mechanical principle of—wheel & axle
• While removing an impacted wisdom tooth, if we have to do the apicoectomy of 2nd molar also,
incision to be given---Extended ward’s.
• Size of suture used commonly in oral cavity is----3/0.
• Lip switch procedure is also called---Transpositional flap vestibuloplasty.
• Incidence of sialolithesis is very high in--- sub Mandibular gland
• Most commonly needle used for aspiration biopsy is---18 gauge.
• Removal of tissue from living individual for diagnostic purpose is called—biopsy
• The basic surgical goal for management of oral pathological lesion is,--- Eradication of lesion,
Functional rehabilitation of pt, Aesthetic improvement, Diagnostic purpose.
• Enucleation means----Removal of entire lesion without rupture.
• Marginal resection means---Resection of tumor without disruption of continuity of bone.
• If stones are present in salivary duct there are chances of-- Metaplasia of lining of salivary duct.
• Surgical blade used for drainage of abcess is---Blade no.11.
• Dean’s technique is also called--Intra septal alveoloplasty
• Effects of heparin can be reversed by---Protamine sulfate.
• Cyclosporine-A, its side effect in oral cavity—gingival hyperplasia
• If a fracture of jaw bone is communicated to external environment, it is called--- compound fracture
• Le fort 3 fracture is also called--- transverse fracture
• Extracted teeth should be preserved in---10% formalin.
• Treatment for patient of cherubism is---Cosmetic surgery.
• Vasoconstrictor in local anesthetics (LA) solution---Reduces toxic effects of LA solution.
• Reducing agent in LA solution is---Sodium metabisulphite.
• Needle used for infilteration is---30 gauge
• When injecting LA solution in maxilla on buccal side, the technique is---Supra periosteal.
• Most common complication of posterior Superior alveolar nerve block is--- hematoma
• Disto buccal root of upper 1st molar is supplied by---Posterior superior alveolar nerve.
• 2 nerves blocked when injection is given in pterygomandibular space--Lingual & inferior alveolar
nerve.
• One of the common side effects of Dilantin sodium therapy seen in oral cavity is---Gingival
hyperplasia
• Blanching at the site of injection is caused by---Increased tissue tension.
• Most common complication after tooth extraction is--Alveolar osteitis.
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 1
• Technique of anesthesia in which local anesthetic solution is injected into the vein is--Intra venous
regional anesthesia.
• Most common complication of rheumatoid arthritis involving TMJ is--Ankylosis.
• Local anesthetic solution with highest tissue irritancy is--Bupivacaine.
• In case of multiple extractions, teeth that should be removed last are--1st molar& canine
• Vazirani akinosis technique--- for limited mouth opening
• least desirable media for transporting an avulsed tooth—water
• It is difficult to obtain anesthesia by infiltration technique in the presence of inflammation because
of—decrease pH
• Sharp surgical instruments should not be sterilized by --- boiling
• The” WINTER’S” classification for impacted third molar is done on the basis of inclination of long axes
of---Third molar to second molar
• Recognized approach for an apicectomy--- Semilunar incision
• In facial trauma, lingual or sublingual haematoma are typically associated with--Mandibular fracture
• Battle’s sign” is associated with displaced fracture of ----Condyle of mandible
• Mouth remain closed with Maxilomandibular fixation (MMF)--- 5 weeks
• Acute Mandibular dislocation typically---treated /corrected manually under local anaesthesia
• The most common complication seen after the administration of local anesthetic agent is ---Trismus
• Most likely the cause of trismus is injury to-- Medial pterygoid muscle
• Cause of Pseudo-ankylosis of temporomandibular joint can be---Mechanical obstruction or extra-
articular fibrosis
• Preferred local anesthetic technique for hemophilic patient---Intraligamentory.
• For diagnosis of zygomatic arch fracture, best view is---Submental vertex view
• Heavy blow to the mandible sustaining a fracture of the right body of mandible. The 2nd most likely
fracture may be present could be---Left sub-condylar region
• Loss of sensation in the lower lip may be caused by---Mandibular body fracture
• Signs and symptoms that commonly suggest cardiac failure---Ankle edema and dyspnea
• Oro-antral fistula treated by---Excision of the fistula and surgical closure
• The roots of 3rd, 2nd & 1st molar are all below the level of the mylohyoid. Infection in these teeth can
pass through----space to reach the lateral pharyngeal space---Submandibular space
• The most common pathognomic sign of mandibular fracture --- malocclusion
• Closed reduction is best used in the treatment of--Favorable, non-displaced fractures
• What determines whether muscle will displace fractured segments from their original position,---
Line of fracture
• While extracting a mandibular 3rd molar, you notice that the distal root tip is displaced from socket.
The most likely area it can be found is---- sub Mandibular space
• Termination of vertical incision at gingival crest must be---At the line angle of tooth
• While administering first aid to a trauma patient with facial injury, priority must be given to---
Maintaining the patency of airway
• Denture is ill fitting, generalized inflammation with whitish patches of oral cavity and poor oral
hygiene; indicates--- Candidosis infection
• Sub condylar fracture on the left ---- inability to deviate mandible to the right
• oblique facial clefts occur due to failure of fusion of-- maxillary process with lateral nasal proces
• Sudden drooping of right corner of the mouth--- affected nerve= facial nerve
• Direction of initial force with forceps placed on a tooth for a successful extraction—APICAL
• The most difficult mandibular third molar impaction position--- Distoangular, maxillary= mesio
angular
• Dental elevators are used for --- engage the tooth apical to the cemento enamel junction
• manage a diabetic patient who loses consciousness before tooth extraction should be administration
of--- IV glucose immediately
• Ameloblastoma in anterior mandible with size of 4X3cm--- Follicular type
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 2
• A pregnant woman in 3rd trimester falls into syncope during extraction of upper molar, she should be
kept in--- Left lateral position
• Salivary gland tumor common in children--- Mucoepidermoid Tumor
• Local anaesthesia acts on nerve membrane by:--- Blocking conduction of sodium from exterior to
interior
• Tuberosity fractured and extracted along with molar, management= Smooth the sharpen edges of
the remaining bone & suture the remaining soft tissues.
• Ideal time to remove impacted 3rd molar is--- When the root is approx. 1/3rd formed
• The root of which Maxillary tooth is most often dislodged into the maxillary sinus---- Palatal root of
maxillary 1st molar
• Sutures placed intra orally are normally removed after--- 5 – 7 days postoperatively
• Dislocation of mandible is reduced in which direction---- Downward & backward & upward
• Regarding principles of suturing technique---- Tissue should not be closed under tension.
• Non resorbable suture material= poly propylene
• Resorbable suture= plain cat gut, chromic catgut & polyglycolic acid
• HIV positive patient, flat, slightly blue patch with proliferation on plate-- Kaposi’s sarcoma
Condition Failure of fusion between
Midline upper lip cleft 02 median nasal process
Uni/ bilateral cleft lip Maxillary & median nasal process
Oblique face cleft Maxillary & lateral nasal process
Isolated cleft lip 02 palatine shelves
Lip clefting Median & lateral nasal process
• Hyperventilation syndrome management→ terminate dental treatment, patients in upright position,
diazepam, monitor vitals.
• shortness of breath/ wheezing—full sitting posture, adrenal insufficiency patient—supine position.
• Remove blood & other fluids from field---High volume suctioning with a relatively small tip
Principle of Incision Description
First Principle Usage of sharp blades with proper size & shape
2nd principle Firm, continuous stroke is used.
3rd Principle Avoid accidentally cutting important structures
4th Principle Incision through epithelial surfaces that surgeon plan to re approximate
should be made with blade held at 90° to epithelial surface.
th
5 principle Incisions in oral cavity should be properly placed.
• Prevention of flap necrosis by → 1) Height of flap should NEVER be greater than base unless a major
artery in base. 2) Height of flap should be no more than twice the width of base (length shouldn’t
exceed width). 3) Axial blood supply should be included in base of flap. 4) Base shouldn’t be twisted,
stretch or grasped.
• Prevention of flap dehiscence→ by approximating edges pf flap over healthy bone by gently
handling the edges of flap, & not by placing edges of flap under tension.
• Prevention of flap tearing→ flap should be large enough, if it’s not providing sufficient space, then it
should be lengthened & releasing incision is made.
• Hematomas ----place pressure on wounds, decreasing vascularity; they increase tension on the
wound edges; and they act as culture media.
• Healing by 1° intension→good scar, use of suture, no tissue loss, less infection, same anatomic
position e.g well-repaired lacerations or incisions & well-reduced bone fractures.
• Healing by 2° intension→ tissue loss, no suture is used, poor scar, gap between edges,slower
healing,e.g extraction socket, poorly reduced fracture, deep ulcers, Large avulsive injury.
• Healing by 3° intension→ delayed primary intension, healing via graft.
• Healing of extraction socket→ 1st week= inflammatory phase, fibroplasia,osteoclastic accumulation.
2nd week= large amount of Granulation tissue.
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 3
Phase of wound healing Features
Inflammatory phase/ lagphase For 3-5 days, vascular & cellular events, initial vasoconstriction, histamine, E1 & E2
cause vasodilation, edema, cardinal sign ( redness, swelling, warm, pain), diapedesis,
degranulation, no gain in wound strength, fibrin hold wound together.
Fibroblast/ proliferative phase For 2-3 weeks, criss cross of blood coagulation derived fibrin strands, laying down
of ground substance (mucopolysaccharide) + tropo collagen, increase in wound
strength(70-80%), stiff & erythromatous wound/ angiogenesis, Granulation tissue
into type 3 collagen.
Remolding / maturation phase For months, replacement of randomly laid collagen fibers, increased strength (80-
85%), decrease in vascularity, loss of elasticity, wound contractions, type 3 to type 1
collagen
• The surface of pure titanium implants is completely covered by---- a 2000-Å-thick layer of TiO.
• Nerve healing by degeneration----- ( segmental demyelination & wallerian degeneration)&
regeneration( Rate= 1-1.5 mm/day).
• Mostly injured nerves→ inferior alveolar nerve & lingual nerve.
• Wallerian degeneration→occurs after trauma, Axon of nerve distal to site of nerve trunk undergoes
disintegration.
• Least severe nerve injury= neuroprexia ( by blunt injury or traction) & most severe
type=neurotmesis(complete loss & by displaced fracture, bullets, knife, iatrogenic)
• Axonotomesis = axon disturbance but not sheath, by severe blunt trauma, nerve crushing, extreme
traction.
Paresthesia Spontaneous & subjective altered sensation that a
patient doesn’t find painful.
Dysthesia Spontaneous & subjective altered sensation that a
patient finds uncomfortable.
Hyperesthesia Excessive sensitivity of a nerve to stimulation
• Most infectious hepatic disease--- by Hepatitis A, B, C, and D viruses
• Most serious risk of transmission for unvaccinated dentists--- hepatitis B
• Hepatitis A is spread primarily by --- feces,. Hepatitis C-- feces / blood, Hepatitis B and D viruses are
spread by contact with any human secretion.
• All patients infected with HIV who have CD4+ T lymphocyte counts of ---less than 200/µL.
• Asepsis ----breakdown of living tissues, 02 types , medical & surgical asepsis.
• Antiseptic ---- substances that prevent multiplication of organisms to living tissues.
• Disinfectant--- substances that prevent multiplication of organisms to objects.
• Sanitization---- reduction of the number of viable microorganisms to levels judged safe by public
health standards.
• Decontamination--- similar to sanitization, except that it is not connected with public health
standards.
Sterilization Method/ Usage
disinfectant
Chlorhexidine, iodophors Dis infecting surgeon’s hand prior to surgery
70% ethanol Dis infecting skin prior to veni puncture
Ethylene oxide Surgical instrument, Endo scope etc
Autoclave Non heat sensitive, gown, drapes, bulky items
Filtration IV solution
UV light Dis infecting air in operation room
Sliver sulfadiazine Clean burn wound
• Test the reliability of heat sterilization----spore of Bacillus stearothermophilus
• Moist heat/ autoclaving is more efficient than heat, because it’s effective at---- low temperature &
require less time.
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 4
• Autoclave--at a pressure = 15 lb/in , temperature =121°C for 15 to 20 minutes.
• Intermediate disinfectants are effective against all microbes except---- bacterial spores
• LA→MOA= block sensory nerve function, raise membrane firing threshold, the nerve membrane
remains in polarized state unable to conduct impulses.
• LA work best at---- neutral pH, LA pH without Vasoconstrictor is ----6.5.
• LA less effective at---- inflammatory site
• Acidification of LA produce---- burning syndrome.
• Short acting (< 60 min) --> procaine
• Medium acting (60-120 min)--> lidocaine, articaine mepivacaine, prilocaine, trimecaine.
• Long acting(> 120 min)-->bupivacaine, tetracaine, etidocaine, ropivacaine.
• Esters-->procaine, tetracaine, benzocaine
• Amides-->lidocaine, trimecaine, articaine, mepivacaine, prilocaine, bupivacaine,ropivacaine,,
etidocaine.
• Vasoconstrictors are added to LA to -----prolonging the drug duration.
• Local Anesthesia Composition
Parts Function
Lignocaine Hcl Anesthetic
Adrenaline Vasoconstrictor
Sodium metabisulphite Reducing agent
Thymol Fungicide
Salts (NaCI) lsotonicity & minimize discomfort during injection
Distilled Water Vehicle
Methyl Preservative
parahydroxybenzoate
• Lidocaine 2% with 1:100000 EN→ maximum amount= 5mg/kg, cartridge for 70kg adult= 10 & for 20 kg
child.
• Procaine→ highest irritability & anesthetic agent in pregnancy→ Xiylocine
• LA affect all types of nerve & may cause hypotension, convulsions & myocardial depression.
• Lingual soft tissue of all teeth by ---lingual nerve, all Mandibular teeth --- inferior alveolar nerve,
• Lingual soft tissues of molar & PM by---- greater palatine & lingual tissues of incisor & canine by ----
nasopalatine nerve.
• Maxillary PM& portion of 1st molar innervated by → middle superior alveolar nerve
• Dialysis—after 24 hours
• Most common impacted teeth= Max & Mand 3rd molar→ Maxillary canine→ Mandibular Pre molar
• Most common cause of lower 3rd molar impaction—failure of rotation from mesio angular to vertical
direction.
• Indications for removal of impacted tooth--- prevention of periodontal disease, caries, pericoronitis,
& root resorption, tooth under prosthesis, prevention of cyst & jaw fracture.
• Contraindications for removal of impacted teeth—extreme age, compromised health, damage to
adjacent structure, treatment planning.
Mandibular Angulation % Description
Mesioangular impaction 43% Common and easiest, proximity of 2nd molar
Horizontal impaction 3% Uncommon and more difficult, immediately adjacent to the root
of 2nd molar—90°
Vertical Impaction 38% Covered posterior aspect with bone of the anterior ramus—O°
Distoangular impaction 6% Uncommon, most difficult, Occlusal surface in ramus
• Easy--- 1, A, mesio angular, difficult--- 3, C, disto angular impaction.
• Maxillary angulation—vertical= 63%, disto angular= 25%, mesio angular—12%( most difficult).
• Most common Incision for reflect soft tissue for removal of impacted 3 rd molar--- envelope incision
• Bur to remove the bone underlying impacted tooth—No-08
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 5
Pell & Gregory Classification
Class 1 The mandibular 3rd molar has sufficient anteroposterior room (i.e anterior-to-anterior border
of ramus) to erupt.
Class 2 Approximately half is covered by the anterior portion of the ramus of the mandible.
Class 3 The impacted third molar is completely embedded in the bone of the ramus of the mandible.
Class A The occlusal plane of impacted tooth is at the same level as the occlusal plane of the 2nd molar.
Class B The occlusal plane of impacted tooth is between the occlusal plane & cervical line of 2nd molar.
Class C The impacted tooth is below the cervical line of the second molar.
• Factors making impaction surgery difficult→ Distoangular position, class 2 or 3 ramus, class B or C
depth, Long, thin ,Divergent, curved roots, Narrow periodontal ligament, Thin, dense, in elastic
follicle, Contact with 2nd molar, Close to inferior alveolar canal, Complete bony impactions.
• Most common factor that causes difficulty with maxillary 3rd molar removal is ----a thin, nonfused
root with erratic curvature.
• Austin & Minnesota retractors ---most commonly used for flap retraction when removing
mandibular third molars.
• Steps—reflecting flap→ removing underlying bone→ selecting tooth→ delivery of sectioned tooth
with elevator→ preparing for wound closure.
• The closure of incision made for an impacted third molar is usually –-- primary closure
• Post operative pain control--- dexamethasone- 0.75-1.25 mg twice a day after impaction surgery.
• Dry socket/ osteitis sicca--- Rx= minocycline
• Impaction surgery--edema in the area of the surgery for 3 to 4 days, with swelling completely
dissipating by about 5 to 7 days.
• Analgesics for post extraction pain—mild pain= ibuprofen (400-800mg), acetaminophen (325-500mg)
• Moderate pain—codeine& hydrocodone, severe pain= oxycodone & tramadol.
• Blood in sub mucosal & sub Mucous tissue--- ecchymosis
• Sutures removal—after one week
• Root most commonly displaced into unfavorable space—Maxillary molar root
• Removal of root tip via—caldwell luc or endo scopic approach
• Lingual cortical bone over root of Molars become thinner as it progress—posteriorly
• Avoid fracture to adjacent structure—avoid excessive torsional force
• The most likely places for bone fractures during exodontia are--- buccal cortical plate over
maxillary canine & 1st molar, portions of floor of maxillary sinus & maxillary tuberosity, & labial bone
over mandibular incisors.
• Confirmation of oro antral communication--- by nose blowing test
Oro antral communication Management
< 2mm Non surgical Rx, avoid blowing & violent sneeze, smoking
2-6( moderate) Additional measure, gelatin sponge, antibiotics- amoxicillin,
cephalexin, Clindamycin- for 05 days, decongestant nasal spray
>7mm( large) Repair with flap procedure
• Prevention of oro antral communication---X ray pre operatively, early surgical extraction, root
sectioning, less apical pressure on maxillary posterior.
• Normal INR--- 2-3 , perform extraction on patients having INR of 2.5 or less without reducing
anticoagulant dose.
• Occurance of dry socket( high fibrinolytic activity)--- 2% of extraction
Distance Implant placement
1mm Inferior to floor of max & nasal sinus
5mm Anterior to mental foramen
2mm Superior to Mandibular canal
3mm Adjacent implant
1.5mm From roots of Adjacent structure
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 6
• Implants need 1.5 mm of space from the outer surface of implant to the adjacent root surface and 3
mm of space between adjacent implants.
• Maintain bone temperature at implant site—below 47°C
• Bone for implant—D2
• Probing depths in a healthy implant--- 1 to 2 mm < total measured dimension from crest of sulcus to
alveolar bone crest.
• Minimum bone need for implant—1mm
• Scribing technique—wash hands & arms
• Double dose—corticosteroids day before & on day of surgery
• 1st dose of LA symptoms— black arm, artery infection
• Pallor—vaso vagal syncope—Rx= ammonia
• Lingual spilt technique—chisel
• Bulbous root extraction—remove bone up to furcation area
• Primary force for exodontia--- towards apical
• Rule of 10--- 10 week, 10 g, 10lb
• Palatal tori--- Y incision
• Labial frenectomy—RX= localized vestibulo plasty with secondary epithelialization
• Optional time for removal of 3 rd Molar in pericoronitis—root 2/3 rd formed
• Thick tuberosity—difficulty in Removal of 3rd molar
• Impacted canine—palataly placed—SLOBE rule—tube distally
• Wheel & axles elevator—4.6 times
• ASA-1--- Hb-14, normal X ray
• Parasymphysis fracture---geniohyoid & genioglossus muscle affected
• Condyle fracture, overlap>5mm—angulation>37°-- open reduction with IMF
• Through & through laceration of Lower lip--- 03 layered suture
• Brusing, battle sign— condylar fracture
• Edentulous, para symphysis fracture, no denture--- Gunning type splint
• High severity infection--- compression of airway
• Swelling in right maxillary posterior region--- space= infra temporal
• Labial alveolar mucosa--- supply by mental nerve
• Bony expansile swelling at body of Mandible, multi locular radiolucency—do aspiration cytology
• Calcifying epithelial odontogenic tumor--- at body with lingual expansion, radiopaque flecks
• Gold standard for predicting malignant potential for pre cancerous lesion—degree of dysplasia
• Carcinoma spread by local infiltration, peri neural invasion, hematogenous spread & less commonly
through lymph—basal cell carcinoma
• Malignancy involving lymph nodes—do FNAC
• Multiple neuro fibroma, with café au lait spots—Von Recklinghausen disease of skin
• TCA--- In TMJ—decrease nocturnal bruxism
• Buccal spcae infection—maxillary due to—molar infection
• Trismus, carious 3rd molar, swelling at anterior tonsillar pillar--- pterygomandibular space
• Most common used for drain of intra oral spce—1/4 inch sterile penrose drain
• 1st choice for prophylaxis before surgery--- amoxicillin
• Prophylaxis for endocarditis – 2g amoxicillin orally- 1 hour before surgery
• MPDS--- nocturnal bruxism, masticatory pain
• Most common cause of ankylosis--- macro trauma
• Condyle fracture—reverse town view
• Ear bleeding, peri auricular pain on one side—unilateral Condyle fracture
• Herefordt syndrome--- uveitis, facial pasly, Parotid gland enlargement
• Bone Resorption near sinus angulation for implant--- sinus lift & grafting
• Smoking history, stabbing pain, runny nose, lacrimation—cluster headache
• Cold air trigger, sharp lancinating pain, like current—trigeminal neurologia
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 7
• Mandibular prognathic—surgery= BSSO
• Sulphur granules—actinomyces
• Soft palate closure—8-18 months
• Midline cyst—dermoid cyst
• Smooth, child, increased swelling in midline—thyroglossal cyst
• Denture patients for evolution for aveloplasty—palpation
• SSC—treatment based on – staging
• Betal nut habit, limited mouth opening, fibrous band—OSF—buccal mucosa
• White lesion, 2mm, Incisional biopsy—by border of ulcer
• Dry socket-- saline , analgesics packing
• Complication of radiotherapy on bone—compromise vascularity
• Most common bone involved in orbital blow out fracture--- ethmoid
• Abrasion on angle of mouth during extraction—no Rx
• Displaced tooth in sinus—OPG
• Caldwell technique—canine fossa
• GCS—level of consciousness
• Faint , patient position—Trendelenburg position
• Reverse status epileptic—by LA overdose,-- diazepam
• Slow growing, gradually enlarging, non tendoe Mandible—ameloblastoma
• Peri Coronal infection of maxillary 3rd molar—infra temporal space
• Salivary glands ingrowth appear in 8th week of gestation.
• Acinus→ collecting cell→ intercalated duct→ striated duct→ excretory duct
• Minor salivary glands → develop fortieth day in utero, larger major glands develop slightly earlier @
thirty-fifth day in utero & acini→ 7/8 months
• Sublingual→ mucus (thick & more viscous saliva) , parotid→ serous & minor salivary glands& sub
mandibular → MIXED
• Number of minor salivary glands- 800-1000, present throughout oral cavity except anterior third of
hard palate, the attached gingiva & the dorsal surface of the anterior third of the tongue.
• Locations of the minor salivary glands are ----as labial, buccal, palatine, tonsillar (Weber glands),
retromolar(Carmalt glands) & lingual glands.
• The lingual glands are divided into 03 groups of glands--: (1) inferior apical glands (of Blandin and
Nuhn), (2) taste buds (Ebner glands), and (3) posterior lubricating gland.
• Serous cells --- cuboidal cells with eosinophilic secretory granules and produce thin, watery
secretions with a low viscosity (1.5pa).
• Mucous cells---- clear low columnar cells with nuclei polarized away from the lumen of acini &
produce a thick secretion with high viscosity(13.4 pa).
• Submandibular gland→ intermediate secretion= 3.4 pa
• Submandibular gland providing 70%, the parotid gland 25%, the sublingual gland 3% to 4%, minor
salivary glands -- trace amounts of saliva.
• Parotid gland concentrations---higher than submandibular gland, except for submandibular gland Ca
concentration, twice concentration of parotid calcium levels.
• Highest viscosity saliva→ sublingual glands, 2nd= sub Mandibular , LOWEST viscosity= Parotid
• Saliva begins to decrease gradually after the age of 20 years because of--- increased
intraparenchymal fibrosis & decreased neural secretory stimulation.
• Sympathetic innervation→ superior cervical ganglion nerve via vast arterial vascular plexus.
• Parasympathetic of Parotid gland→ tympanic branch of the glossopharyngeal nerve (IX)
• Parasympathetic of sub Mandibular & sublingual→ superior salivatory nucleus,which travels via
facial nerve (chorda tympani branch) to submandibular ganglion.
• Plain-Film Radiographs →identify salivary stones, 80% to 85% of all stones → radiopaque,
mandibular occlusal radiograph is most useful for detecting sublingual& submandibular gland calculi.
• PA can show calculi in each salivary gland or duct, including minor salivary glands
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 8
Salivary Gland Anatomical Features
PAROTID GLAND 1.Lie superficial to posterior aspect of the masseter muscles & ascending rami of mandible,in
“inverted triangular” shape below zygomatic arch.
2. Peripheral portions may extend to the mastoid process, along anterior aspect of SCM
muscle & around posterior border of mandible into pterygomandibular space.
3. The facial nerve branches divide gland into superficial & deep lobes.
4. The Stensen duct( diameter= 1-3 mm & L= 6cm) courses superficial to masseter muscle then
curves sharply at anterior edge of masseter muscle to pierce buccinator muscle &enter oral
cavity @ Maxillary 2nd Molar.
5. Structure passing through parotid gland→ facial nerve & it’s branches, retro mandibular vein
& external carotid artery, auriculotemporal nerve parts, superficial & deep parotid lymph
nodes.
6. The parotid gland receives neural innervation from 9th CN (glossopharyngeal) nerve via
auriculo-temporal nerve from the otic ganglion.
SUB MANDIBULAR 1. Located in “submandibular triangle” , formed by anterior & posterior belly of the digastric &
GLAND inferior border of mandible superiorly.
2. Wharton duct(length= 5cm & diameter= 2-4mm) passes forward along superior surface of
mylohyoid muscle in sublingual space, adjacent to lingual nerve.
3. Glossopharyngeal → posterior 1/3rd of tongue, & chorda tympani branch of the facial nerve
provides taste sensation to anterior 2/3rd of tongue.
4. In a medial position, Wharton duct is vulnerable to injury in the third molar region.
5. The Wharton duct opens into floor of mouth via a muscular punctum located close to
mandibular incisors at most anterior aspect of junction of lingual frenum & floor of mouth.
6. The punctum is a constricted portion of the duct, & it functions to limit retrograde flow of
bacteria-laden oral fluids into the ductal system.
SUB LINGUAL 1. Located on superior surface of mylohyoid muscle, in sublingual space, & separated from oral
GLAND cavity by a thin layer of oral mucosa in anterior floor of the mouth.
2. The main acinar ducts of sublingual glands are called Bartholin ducts and in most instances
coalesce to form 8 to 20 ducts of Rivinus which open on plica sublingualis.
3. The sublingual & submandibular glands are innervated by facial (VII) nerve through
submandibular ganglion via chorda tympani nerve.
• Head tilt process—to ensure patent airway
• Amide biotransformation—by liver
• Spontaneous bleeding post extraction—because of fracture of max Tuberosity
• Most common cause of removal of 3 rd molar—recurrent pericoronitis
• Direction Of chisel during cutting--- towards bone to scarified
• During removing pleomorphic adenoma—complication because of injury to auriculotemporal nerve—
gastatory sweating
• Condition of contraindicated to LA—hypersensitivity to drug
• LA suitable for hypertensive patient--- without adrenaline
• Allergy by amide LA--- by methylperaben
• Small, oval, multiple ulcers--- aphthous ulcer
• Highest malignancy rate—erythroplakia
• Unilateral, angled displaced fracture, distal to last standing molar—Rx= ORIF
• Decreased mouth opening—may Also because of 3rd molar
• Extraction of Distoangular impaction of mand 3 rd molar—cause fracture of ramus of Mandible
• Fracture tuberosity, but attached—Rx= if intact blood supply—reposition& stabilize suture
• Odontogenic infection—by s- milleri
• Hard ,tender, red, deep tissue infection--- cellulitis
• Odontogenic deep facial infection--- sub Mandibular infection
• Anterior open bite--- displaced bilateral Condyle fracture
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 9
Fracture Features
Lefort-1 Mobility at ANS, Mobility of alveolus, involve lower 1/3rd & upper 2/3rd of pterygoid
plate, palate, naso maxillary, epistaxis, Buccal ecchymosis, malocclusion, Maxillary
crepitus & mobility, Upper lip swelling, Positive guerin sign.
Lefort -2 Pyramidal , nose + palate, mobility at infra orbital margin, crepitus of midface,
facial lengthening, Bilateral epistaxis, infraorbital nerve paresthesia, buccal,
periorbital & sub conjunctival ecchymosis, widening of inter canthal space, cerebral
fluid rhinorrhea, dish face, ballooning/ moon shaped, middle 3rd of pterygoid plate
Lefort-3 Craniofacial disjunction, transverse fracture, bilateral epistaxis, lateral orbit rim
defect, Peri orbital & sub conjunctival ecchymosis, mobility at fronto zygomatic
suture, no posterior limit , Hooding of eye, ponda face & raccoon eye, @ root origin
of pterygoid plate
• Bilateral un displaced Condylar fracture--- max & mand fixation, with eric arch bar
• Gun shot & committed fracture—close reduction with gunning splint
• Lateral & retro pharyngeal space—direct threat to airway
• Basic management of odontogenic infection—support medically, Surgical, antibiotics
• Most common treatment of ranula—Marsupialization
• Lip switch process--- Temporal flap vestibulo plasty
• Dean technique—intra septal aveloplasty
• Complication of RA--- involving TMJ—ankylosis
• Facial palsy, vertigo, deafness, herpes, vesicular rash -- ramshy hunt syndrome
• Throbbing, temporal pain, increase ESR—gaint cell arthritis
• Complication of posterior sup alveolar nerve block--- hematoma
• Go gets Mandibular nerve block—corner of mouth & tragus of ear
• Redness, swelling of face, shallow breathing—anaphylatic reaction
• Normal face growth--- down ward & forward
• Parasymphysis fracture, occlusal distrubance—IMF for 03 days
• Unfavorable fracture of Mandibular angle--- distraction of fracture segment by muscle pull
Type of fracture Technique
Condyle fracture Reverse town view
Zygomatic fracture Sub mantovertex view
Orbital blow out Occipitomental view
Step deformity in molar Lateral oblique view
Body + angle fracture & type of displacement Posterio anterior
Fracture between symphysis & canine Rotational posterio anterior
Relationship to teeth to line of fracture Peri apical
Relation of tooth root to the fracture Occlusal
Fracture of body proximal to canine,condyl & L & R oblique lateral
ramus fracture
• Fibrin—holding wound together during inflammatory stage
• Malignant tumor of minor salivary glands—muco epidermoid carcinoma & polymorphous low grade
adenocarcinoma.
• Sialolithiasis—meal time pain
• Hyperventilation—CO2 enriched gas is given
• Chest tightness, suffocating, tachycardia, light headache--- hyper ventilation
• Aprire tooth--- helminths maneuver
• Weight loss—hyperthyroidism
• Prevent dead space by pressure dressing until bounded by fibrin—12-18 hour’s
• Leafless fruit laden tree/ cherry Blossom appearance—sjogren syndrome
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 10
• Retrograde filling in right maxillary CI--- sub marginal incision, in 2nd Molar—extended ward
• Common indication for peri apical surgery—horizontal root fracture
• Squamous cell carcinoma—marjolin ulcer – at lower lip mostly
• T 1- < 2mm, T2- = 2-4 cm, T3- > 4, M1- distant metastasis
Indication/ type Suture
Natural suture Silk, categut
Synthetic Vicryl, prolene
Absorbable Categut, vicryl
Non absorbable Silk, prolene
Mono filament Prolene
Polyfilament Categut, silk
Suture material for intraoral incisions Absorbable – Vicryl 3-0
Non-absorbable – Silk 3-0
Inter suture distance 3-5 mm
Distance from the skin edge 2-3 mm
After removal of Mandibular tori, Simple continuous suture
pediatrics, bone grafting, non esthetic,
tight suture.
Peri apical surgery Sling suture
Small area, after extraction, laceration Simple interrupted suture
closure, after enucleation
Hemostasis, esthetic Figure of 08
• Suture is pulled through tissue until short tail of suture approximately 2 inches remains.
• Sutures not placed a cross empty socket.
• Needle enter surface at –90°
Flap Design Indication
03 corner flap Surgical extraction, greater excess, 3rd molar impaction
surgery, for cyst removal, enucleation of radicular cyst
Semi lunar flap Peri apical surgery, avoid Trauma to papilla
Envelope flap Impacted 3rd molar
Sub marginal flap Esthetic
• Anti coagulation therapy--- PT time is seen.
Blade number Indication
10 For large skin Incision
11 For Incising an abscess
12 Muco gingival procedure
15 For intra oral surgery
• ASA3--- not incapacitated patients
• For working surface—hypo chlorite
• Propofol--- IV- LA for neonate
• Flap tear—prevention of lengthening incisions
• Abrasion—no treatment
• 2-6 mm oro antral fistula--- figure of 08
• Sinus pathology—OPG
• Naso palatine duct cyst—occlusal view
• Immobilization for jaw fracture—2-3 week
• Most effective method for TMJ disorders—arthroscopy
• Anterior disc displacement, not respond to surgery—disc reposition surgery
• Rx of disc displacement with/ without reduction--- Modified condylotomy
• Rx for anterior disc displacement without reduction--- Arthrocentesis
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 11
• Diagnosis—SSC – invasion, Rx on staging
• Rolled edges--- basal cell carcinoma
• Dis continue anti coagulation--- INR> 3
• CPR—100 compression: 2 rescue breathing
• Puetz jeghers syndrome—intestinal polyps
• Multiple Mandible fracture--- 05 eyelets in each jaw
• Gold standard—autogenic bone
• Class 3—SSO
• Multiple pre malignant lesion—field cancerization
• Dentigerous cyst & radicular cyst--- Rx Enucleation+ IMF
• OKC—currettage
Instrument Indication/ uses
Austin retractor Right-angle retractor that can be used to retract the cheek, tongue, or flaps.
Allis tissue forceps useful for grasping and holding tissue that will be excised
Rongeurs bone-cutting forceps that have spring-loaded handles
mallet and chisel For removing bone
needle holde To hold needle, grasps the curved needle two-thirds of the
distance from the tip of the needle. Have locking handle and a short, blunt beak.
Iris scissors small, sharp-pointed scissors.
Molt, mouth prop used to open the patient’s mouth when the patient is unable to cooperate
Triangular elevators Pairs of instruments & are therefore used for mesial or distal roots.
Cryer)
Crane pick used to elevate whole roots or even teeth after the purchase point has been prepared
with a burr.
root-tip pick used to tease root tip fragments from the socket
Forceps used to remove maxillary teeth are held with the palm under the handle.
• Semi rigid fixation—healing by secondary intension, callus formation
• Body—Quick healing & symphysis- late healing.
• 5% Infection rate—after Mandibular fracture
• Closed reduction—simple, comminuted, favorable fracture
• Open reduction—unfavorable fracture, basal triangle fracture, periodontal compromised, edentulous
• Diameter pf suture for oral mucosa--- 3-0
• Spontaneous sockets wound, as barrier—figure of 08
• Antidote for heparin—protamine sulfate
• All level of sedation—Inhalation
• % of NO—20%
• Conscious sedation with IV benzodiapine--- pupillary reaction
• Intra capsular fracture—complication= TMJ ankylosis
• Fracture at zygomatic temporal suture—Gillis temporal approach
• Pull, displacing fracture segment—unfavorable fracture
• Marble appearance, limited mouth opening, white bends—OSF
• Easily managed SCC—lower lip
• Malignant lymph nodes—FNAC
• T1, N2, M0--- Stage 4
• Substernal pain, facial pallor—angina pectoris
• Propofol--- day care surgery
• 50 kg—LA- 10 dose
• Burning pain, surgical tooth extraction, boring pain—atypical odontolygia
• Maximum dose of lignocaine without adrenaline—4mG/kg
• Socket post extraction healing time—2-3 weeks
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 12
Fracture Features
Direct impact to TMJ Condyle fracture, comminuted
Lateral impact on body Same side body fracture, opposite side- condyl fracture
Impact from below on chin Symphysis/ para symphysis with bilateral Condyle fracture
From anterior Mandible Bilateral body fracture along with bilateral Condyle fracture
Unilateral Condyle fracture Chin & mandibular midline deviation towards affected side, posterior teeth
gagging affected side, posterior Open bite on opposite side, unable to perform
lateral movement associated with opposite side body fracture.
Bilateral Condyle fracture Posterior teeth gagging on both sides, anterior open bite, no protusion,
symphysis fracture
Clinical features of Pain, swelling, tenderness, characteristics hollow ( after subside edema),
Condyle fracture hematoma- Battle sign, Ear bleeding, Reverse town view.
Right Mandibular angle Colman’s sign
fracture
Impact from anterior Bilateral body fracture with bilateral Condyle fracture
Mandible
Angle fracture Tenderness, swelling at angle, hematoma at angle, step defrormity at last molar,
lower lip paresthesia, de arranged occlusion, painful mandibular movements
Symphysis & Para Soft tissue injury on chin & lip, lingual hematoma, bone tenderness, associated
symphysis fracture with Condyle fracture
Dento alveolar injuy Avulsion, sub luxation, fracture of Teeth, laceration of upper & Lower teeth,
alveolar fracture.
Body fracture Swelling, tenderness, step defrormity, anesthesia & paresthesia of lip & intra oral
hemorrhage
• Ulceration because of instruments—abrasion
• Reactive—Plain & chronic gut
• 20-40% NO—symptoms--. Euphoria
• IANB--- muscle pierce—buccinator
• Most alarming respiratory condition—apnea
• IANB--- absolutely contraindicated in hemophilic patient
• Leg screw for—oblique mandibular fracture
• IMF – eyelet in each jaw—05 eyelets
• Elevator & retrusive of Mandible—Temporalis
• Masseter—elevation of Mandible
• Lateral pterygoid—protusion& depression of Mandible
• Medial pterygoid—elevation& protusion of Mandible
• Pregnant lady fall in syncope—sit in lateral left position
• Syncope—hypoxia
• ASA-3 – not incapacitated patients
• Ineffective against spore forming clostridium—ethylene oxide
• Unresponsive, choking—start CPR( cardio pulmonary resuscitation).
• Plugging Rannula—perforate mylohyoid muscles.
• Sub lingual & minor salivary glands—90% tumor malignant
• Sub Mandibular & Parotid gland—Majority benign tumors
• At junction of upper 3rd & middle 3rd of Anterior border of SCM muscles--- bronchial cyst
• Neonate—cystic hygroma
• move up on swelling—thyroglossal duct cyst—Rx = Sisternuk operation
• Non specific ulcer= shelving edge ulcer
• TB= undermined edges
• Squamous cell carcinoma= Everted, heaped up—marjolin ulcers
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 13
• Syphilis+ Arterial disease= punched out
• Warfarin- PT
• Heparin-- aPTT
• Basal cell carcinoma= rolled edge—rodent ulcer
• Corney solution—60% ethanol, 30% chloroform, 10% acetic acid—decrease reoccurrence of OKC
• Chin laceration—symphysis fracture
• Abscess complication--- cavernous sinus thrombosis
• LA on buccal side--- supra periosteal technique
• AVPU— alertness, voice, pain & unconscious
• TMJ internal de arrangements— analysis by MRI
• Injured structure in excision of ranula—sub mandibular duct
• AED—for arrhythmia
• Hyper baric oxygen—for osteocardio necrosis
Moth eating appearance Osteomyelitis, osteosarcoma
Honey comb appearance Odontogenic cyst, ameloblastoma
Cotton wool appearance Peget disease
Egg shell crackling Radicular cyst & ameloblastoma
Ruston bodies Radicular cyst
Crocodile tear Bells palsy
Tennis ricket appearance Odontogenic myxoma
Speckled appearance Heterogeneous leukoplakia
Rippled appearance Homogeneous leukoplakia
Cobble stone appearance Crohn’s disease
Snow storm & cherry blossom Sjogren syndrome
Floating teeth HED
Crumb like appearance Alveolar osteitis
Hanging drop sign Oribital blow out
Ground glass appearance Fibrous dysplasia
Wickam straie, saw tooth Lichen planus
appearance
Snow cap appearance Amelogenesis imperfecta
Swiss disease pattern Adenoid cystic carcinoma
Radicular type Peri apical cyst
Follicle type Dentigerous cyst
Extra radicular/ primordial OKC
Episton Pearl Gingival cyst—in neonate
Bunch of grape Lateral periodontal cyst
Heart shape Naso palatine cyst
Saucer shaped Stephen idiopathic cyst
Bag of Teeth, denticles Compound odontome
Sun brust appearance Complex odontome- in mandible
• RADICULAR CYST—non keratinized epithelium, unilocular,straw color fluid.
• DENTIGEROUS CYST—unilocular, Mandibular 3rd molar, root Resorption, associated with
supernumerary tooth, yellow fluid
• OKC—uni/ multilocular cyst, white cheesy fluid, associated with garlin syndrome.
• Excisional Biopsy—< 1mm – For lump,, mucocele, pigmentation—removal of whole part, for
confirmation, lesion not at risky location.
• Incisional Biopsy-- > 1mm, removal of part, for diagnosis, risky site, at great suspicion of malignancy.
• Most common malignant salivary— Muco epidermoid carcinoma- 2nd = polymorphous low grade
adenocarcinoma ( at junction of hard & soft palate)—3rf = adenoid cystic carcinoma
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 14
• Warthin tumor/ papillary cystadenoma lymphomatosum—almost exclusively affect Parotid glands
• Most common salivary glands—benign- Pleo morphic adenoma
• Facial paralysis by adenoid cystic carcinoma, as a result of neurotropism—basaloid cell arrange in
Cribriform/ swiss cheese pattern.
MANDIBULAR FRACTURE KEY POINTS
CLASSIFICATION OF FRACTURE:
• Type of fracture ( simple, compound, comminuted, pathological).
• Site of fracture – most used classification/ linear fracture( dento alveolar, condyle, coronoid, ramus,
angle, body, para symphysis & symphysis.
• Causes of fracture ( direct violence, indirect violence & excessive muscular contraction).
• Fracture with gross communication- extensive loss
• Fracture without gross communication- no extensive loss
• Most common overall mandibular fracture is---- condylar fracture.
• Simple fracture (closed fracture)→ linear fracture
• Compound fracture (Open)→ fracture is communicating intra or extra orally. Via the periodontal
membrane involving socket.
• Comminuted fracture→ shattering of bone into multiple pieces.
• Pathological fracture→ results from minimal Trauma already weakened by osteomyelitis, neoplasm
• Greenstick fracture: only in children, Only one cortex broken.
• Mandibular fracture more common than middle 3rd fracture.
• Order of common facial fracture: mandible> maxilla> zygoma> nasal bones.
• Unilateral fracture: by direct violence, one or more than one fracture.
• Bilateral fracture: by direct and indirect violence, commonly involving angle & oppositecondylar neck
or canine region.
• Multiple fracture: direct with indirect violence, common symphysis fracture & both condyle. Seen
also in epileptic patients & guardsman’s fracture.
• Condyle is commonest site for mandibular fracture & angle fracture is the most frequent site, when
only one fracture is present.
• Fracture of tooth bearing areas--- compound fracture
• Compound fractures complicated by bone & soft tissue loss→ comminuted
• In lamellar type fracture, osteosynthesis by 02 plates is done.
• Impacted fracture which is driven into another portion of bone.
• Indirect : a fracture at a point distant from the site of injury.
• Complicated/complex fracture: damage to adjacent soft tissue, can be simple or compound.
• Dentition Classification of fractures:
• Developed by Kazanjian and Converse:
1) Class I: teeth are present on both sides of the fracture line.
2) Class II: Teeth present only on one side of the fracture line.
3) Class III: Patient is edentulous
• Maxilla tolerance level--- 140lb, Mandible: 425lb & symphysis fracture—800-900lb
•
Coronoid process--- Temporalis
Ramus--- Masseter
Condylar Neck---- lateral pterygoid
Rami near angle--- medial pterygoid
Symphysis---- mylohyoid & geniohyoid
Parasymphysis--- geniogloss
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 15
• Favorable fracture--- fracture line & muscle pull resist displacement.
• Unfavorable fracture--- muscle pull results in displacement of fracture portion.
• Frequent direction of dislocation of condylar neck—Medial & forward
• Angle fracture---- If vertical fracture—lingual pull & horizontal fracture— upward
• Most edentulous mandibular fracture @ Body near posterior attachment of mylohyoid.
• Bucket handle displacement: downward & backward angulation of Mandible because
of digastric & mylohyoid muscles.
• Mandible blood supply by 1) periosteum (centripetal) & 2) inferior dental artery
(centrifugal).
• Facial palsy--- lower motor neuron injury, TMJ---- traumatic arthritis, synovial effusion,
fibrous/ bony ankylosis.
~ Compiled by Danesh Kumar-SIOHS/ JSMU (03312415069)
~Errors & Omission are accepted
~ Feedback is welcomed
BEST OF LUCK
Oral Surgery Key Points By Danesh Kumar-SIOHS/ JSMU (03312415069) 16
You might also like
- VICTIMDocument4 pagesVICTIMt7uyuytu100% (4)
- Pressure UlcerDocument35 pagesPressure Ulcerenam professor100% (1)
- Liceo de Cagayan University: WorksheetDocument7 pagesLiceo de Cagayan University: WorksheetLol lolNo ratings yet
- Management of Deep Carious Lesions in ChildrenDocument46 pagesManagement of Deep Carious Lesions in ChildrenSahil Gagnani100% (1)
- Orthodontics Key Points by DaneshDocument16 pagesOrthodontics Key Points by DaneshSyedfaizan AliNo ratings yet
- TMJ Part 3Document86 pagesTMJ Part 3Gaurav SharmaNo ratings yet
- TraumaDocument65 pagesTraumamuhabaw abebeNo ratings yet
- Nasal Fractures: Trauma To NoseDocument38 pagesNasal Fractures: Trauma To NoseSindhura ManjunathNo ratings yet
- CSOM TreatmentDocument21 pagesCSOM TreatmentSarwinder SinghNo ratings yet
- Presented By:-Shalini Thakur Guided By: - Dr. T. RamakrishnaDocument41 pagesPresented By:-Shalini Thakur Guided By: - Dr. T. RamakrishnaShalini Thakur DubeyNo ratings yet
- Gingival Tissue ManagementDocument19 pagesGingival Tissue Managementtaruntj19No ratings yet
- Dentistry For General Medicine: - Part 2 - Dental SurgeryDocument52 pagesDentistry For General Medicine: - Part 2 - Dental SurgeryDimitrios PapadopoulosNo ratings yet
- Fraktur Maksila Dea EditDocument139 pagesFraktur Maksila Dea Editdea putri audinaNo ratings yet
- Surgical Complications of Minor Oral SurgeryDocument53 pagesSurgical Complications of Minor Oral SurgeryDrNagendra Dutt Sharma100% (1)
- EmergeDocument24 pagesEmergeili_izyanNo ratings yet
- Al-Assaf NOTES 02Document9 pagesAl-Assaf NOTES 02alidyab128No ratings yet
- Lefort FractureDocument90 pagesLefort FractureRiya CorreaNo ratings yet
- Oral Surgery 7Document10 pagesOral Surgery 7youssefkamal838No ratings yet
- 0 Tooth ExtractionDocument22 pages0 Tooth ExtractionDrashti ChudasamaNo ratings yet
- Symphysis FractureDocument31 pagesSymphysis FractureParijat Chakraborty PJNo ratings yet
- Head and Neck SurgeryDocument15 pagesHead and Neck SurgeryMedisina101100% (1)
- Fraktur Maksila Dea EditDocument139 pagesFraktur Maksila Dea Editdyas modestyNo ratings yet
- VSR 421 Regional Vet SurgeryDocument233 pagesVSR 421 Regional Vet SurgeryPavan S N PavanNo ratings yet
- Surgical TreatmentDocument4 pagesSurgical TreatmentRobertRaduNo ratings yet
- Oral Surgery Lec. 8Document11 pagesOral Surgery Lec. 8Maysaa AbbasNo ratings yet
- (ENT SGT) Myringotomy, Myringoplasty 25.05.2023Document21 pages(ENT SGT) Myringotomy, Myringoplasty 25.05.2023Devidutta Dash 21PMB055No ratings yet
- Accidental Displacement of Impacted Maxillary Third Molar JC 2Document22 pagesAccidental Displacement of Impacted Maxillary Third Molar JC 2Amna AzharNo ratings yet
- PowerPoint Maxillofacial Trauma EnglishDocument67 pagesPowerPoint Maxillofacial Trauma EnglishRizki Octo Kurniawan100% (1)
- OSCE GuideDocument184 pagesOSCE GuideKesavaa VasuthavenNo ratings yet
- Fractures MidfaceDocument130 pagesFractures MidfaceLAIBA WAHABNo ratings yet
- Notesssss Just MemorizeDocument54 pagesNotesssss Just Memorizedhiraj.2367No ratings yet
- Impacted Maxillary CanineDocument8 pagesImpacted Maxillary CanineMatin Ahmad Khan100% (1)
- Maxillary sinus ppt- jamal lect- 2018-19 -للطلبهDocument153 pagesMaxillary sinus ppt- jamal lect- 2018-19 -للطلبهMurtdha ArifNo ratings yet
- Interceptiveorthodontics 111013083234 Phpapp02Document62 pagesInterceptiveorthodontics 111013083234 Phpapp02Bunga Erlita RosaliaNo ratings yet
- 2012 - EDT-Oral-Surgery-II-Midterm-Questions-2012Document8 pages2012 - EDT-Oral-Surgery-II-Midterm-Questions-2012Laith Al-jarrahNo ratings yet
- 7 Complications of Tooth Extraction PDFDocument10 pages7 Complications of Tooth Extraction PDFlyli Star AngeloNo ratings yet
- Tympanoplasty: Manal Al Quaimi 207000989 2011Document39 pagesTympanoplasty: Manal Al Quaimi 207000989 2011Manal AlQuaimiNo ratings yet
- Midface FracturesDocument31 pagesMidface FracturesJoyabrata SarkarNo ratings yet
- Endo Don TicsDocument32 pagesEndo Don TicsGolbarani HomeNo ratings yet
- Complications of Teeth ExtractionDocument13 pagesComplications of Teeth Extractionfbbqbcht6yNo ratings yet
- Periodontal SurgeryDocument4 pagesPeriodontal SurgeryRinisha SinhaNo ratings yet
- Omr Seminar CystDocument51 pagesOmr Seminar CystJohann GeorgeNo ratings yet
- Complications of Teeth ExtractionDocument13 pagesComplications of Teeth Extractionit's EimyNo ratings yet
- Deviated Nasal SeptumDocument45 pagesDeviated Nasal Septumdrtpk100% (3)
- Complications of Extraction: Prsenting By: Rahul TiwariDocument75 pagesComplications of Extraction: Prsenting By: Rahul TiwariIrfan AliNo ratings yet
- Endodontic MishapsDocument34 pagesEndodontic MishapsSimpy Jindal100% (1)
- Omar SDLE NOTES 3 (1)Document13 pagesOmar SDLE NOTES 3 (1)mohamedalawy1979No ratings yet
- RevisionDocument59 pagesRevisionKeval SutharNo ratings yet
- 4.the Periodontal FlapDocument45 pages4.the Periodontal FlapSamwel EmadNo ratings yet
- Diseases of The Ear PinnaDocument25 pagesDiseases of The Ear PinnaisaacmoggamingakijuNo ratings yet
- Presentation of Le Fort - III Fractures and Its ManagementDocument74 pagesPresentation of Le Fort - III Fractures and Its ManagementmustahsinNo ratings yet
- Ijss Jan Oa10 - 2017Document7 pagesIjss Jan Oa10 - 2017Benedetta GuarinoNo ratings yet
- Preprosthetic SurgeryDocument4 pagesPreprosthetic SurgeryDentist HereNo ratings yet
- Caldwell Luc MiercolesDocument16 pagesCaldwell Luc MiercolesSERVICIOS MINEROSNo ratings yet
- 11月book readingDocument31 pages11月book reading新手冒險家No ratings yet
- Oral SurgeryDocument52 pagesOral Surgerykhaled alahmadNo ratings yet
- Treatment Planing and SeminarsDocument15 pagesTreatment Planing and Seminarsalsakar26No ratings yet
- 3 (Fractures of The Middle Third)Document84 pages3 (Fractures of The Middle Third)sara.kattan22No ratings yet
- TympanoplastyDocument34 pagesTympanoplastymanu100% (1)
- Prosthodontics Key Points by DANESHDocument21 pagesProsthodontics Key Points by DANESHNoor HaiderNo ratings yet
- Endodontic SurgeryDocument8 pagesEndodontic SurgeryjoseNo ratings yet
- Oral Medicine & Pathology from A-ZFrom EverandOral Medicine & Pathology from A-ZRating: 5 out of 5 stars5/5 (9)
- Altamash Oral Surgery Preproff PapersDocument96 pagesAltamash Oral Surgery Preproff PapersNoor HaiderNo ratings yet
- Oral Surgery Preproff LCMD PapersDocument54 pagesOral Surgery Preproff LCMD PapersNoor HaiderNo ratings yet
- Prostho Pre Prof-22 JSMUDocument2 pagesProstho Pre Prof-22 JSMUNoor HaiderNo ratings yet
- Oral Surgery JMDC Preproff PaperDocument58 pagesOral Surgery JMDC Preproff PaperNoor HaiderNo ratings yet
- Cast Analysis and Space SupervisionDocument36 pagesCast Analysis and Space SupervisionNoor HaiderNo ratings yet
- FJDC Operative PREPROFF PAPERSDocument154 pagesFJDC Operative PREPROFF PAPERSNoor HaiderNo ratings yet
- Prosthodontics Key Points by DANESHDocument21 pagesProsthodontics Key Points by DANESHNoor HaiderNo ratings yet
- Resin Bonded Bridge09Document8 pagesResin Bonded Bridge09Noor HaiderNo ratings yet
- Key Points ProsthoDocument45 pagesKey Points ProsthoNoor HaiderNo ratings yet
- Types of Crowns and BridgesDocument40 pagesTypes of Crowns and BridgesNoor HaiderNo ratings yet
- Principles of Tooth PreparationDocument7 pagesPrinciples of Tooth PreparationNoor HaiderNo ratings yet
- Partial Veneer Crown N' BioDocument6 pagesPartial Veneer Crown N' BioNoor HaiderNo ratings yet
- Crowns 1Document5 pagesCrowns 1Noor HaiderNo ratings yet
- MecamylanimeDocument15 pagesMecamylanimeNoor HaiderNo ratings yet
- Endodontics Key Points by DaneshDocument16 pagesEndodontics Key Points by DaneshNoor HaiderNo ratings yet
- Surgery 2020 Fjdc.Document101 pagesSurgery 2020 Fjdc.Noor HaiderNo ratings yet
- Qunoot Lakhani - Pharma Ospe FJDCDocument11 pagesQunoot Lakhani - Pharma Ospe FJDCNoor HaiderNo ratings yet
- Amalgam-Notes by DaneshDocument12 pagesAmalgam-Notes by DaneshNoor HaiderNo ratings yet
- Oral Surgery LCMD 2020 DR Ehsan LecturesDocument36 pagesOral Surgery LCMD 2020 DR Ehsan LecturesNoor HaiderNo ratings yet
- LCMD VK Prostho'20Document46 pagesLCMD VK Prostho'20Noor HaiderNo ratings yet
- OS JMDC Preproff 2022 PDFDocument15 pagesOS JMDC Preproff 2022 PDFNoor HaiderNo ratings yet
- Pharma JSMU Preproff 2019 by Jeetendar HaraniDocument3 pagesPharma JSMU Preproff 2019 by Jeetendar HaraniNoor HaiderNo ratings yet
- SOVED Patho 19Document20 pagesSOVED Patho 19Noor HaiderNo ratings yet
- Radiographic Positioning SummaryDocument13 pagesRadiographic Positioning SummaryRadoi Sandina Rodica100% (1)
- Musculoskeletal SystemDocument4 pagesMusculoskeletal SystemJm AshiiNo ratings yet
- Treatment of A Lisfranc Injury in A 7-Year-Old BoyDocument5 pagesTreatment of A Lisfranc Injury in A 7-Year-Old BoyDaniel AguilarNo ratings yet
- Type of Joints: Group MembersDocument21 pagesType of Joints: Group MembersBeni Ram RawalNo ratings yet
- Anatomy Ii: by Dr. Ziyad M. Al Zeer Orthopedic Surgeon Assistant Professor MD - PHDDocument64 pagesAnatomy Ii: by Dr. Ziyad M. Al Zeer Orthopedic Surgeon Assistant Professor MD - PHDMOHAMMAD ALSWEITYNo ratings yet
- Pudendal Nerve BlockDocument2 pagesPudendal Nerve BlockLauraNo ratings yet
- Forensic Science 2Document20 pagesForensic Science 2Paramjit Singh100% (1)
- 01 Respiratory SystemDocument15 pages01 Respiratory Systemnaseer alfahdNo ratings yet
- 6 Series - Notes Need To WriteDocument9 pages6 Series - Notes Need To WriteVijay UNo ratings yet
- Davasia Yohannan Vs State 05021958 KERHCk580076COM535534Document7 pagesDavasia Yohannan Vs State 05021958 KERHCk580076COM535534Aadhitya NarayananNo ratings yet
- EP1010Document53 pagesEP1010cacollins1965No ratings yet
- Body MechanicsDocument26 pagesBody MechanicsSandeepNo ratings yet
- Screenshot 2023-06-18 at 10.34.34 PMDocument1 pageScreenshot 2023-06-18 at 10.34.34 PMNandan BethinaNo ratings yet
- Sistema Venoso ProfundoDocument12 pagesSistema Venoso ProfundoEngie VersabethNo ratings yet
- Pelvis and Perinium 2019Document59 pagesPelvis and Perinium 2019Vuluwa George100% (1)
- Mclarty 2012Document7 pagesMclarty 2012Gisele CanelaNo ratings yet
- Spinal Cord Epidural Stimulation For Lower Limb Motor Function Recovery in Individuals With Motor Complete Spinal Cord InjuryDocument18 pagesSpinal Cord Epidural Stimulation For Lower Limb Motor Function Recovery in Individuals With Motor Complete Spinal Cord InjurynorazmiNo ratings yet
- 20 Questions Abdominal PainDocument3 pages20 Questions Abdominal Painsumiti_kumarNo ratings yet
- Basic Lower Limb Assessment Flow SheetDocument2 pagesBasic Lower Limb Assessment Flow Sheetمحمد نعمة جياد100% (1)
- CVP Insertion Close Tube Thoracostomy RDocument6 pagesCVP Insertion Close Tube Thoracostomy RFaye Nadine T. CABURALNo ratings yet
- Week 3 Lectorial SlidesDocument56 pagesWeek 3 Lectorial SlidesTrần Đức AnhNo ratings yet
- Ascending & Descending Tracts: Dr. Aneela JamilDocument20 pagesAscending & Descending Tracts: Dr. Aneela JamilSidra FarooqNo ratings yet
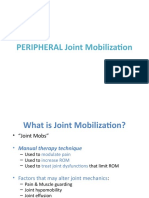
- PERIPHERAL Joint MobilizationDocument53 pagesPERIPHERAL Joint MobilizationRaghu NadhNo ratings yet
- DHP482 Makita PDFDocument72 pagesDHP482 Makita PDFatorresh090675No ratings yet
- Head and Neck QuestionsDocument3 pagesHead and Neck QuestionsVeriteNo ratings yet
- First Aid and Basic Life Support Training CourseDocument3 pagesFirst Aid and Basic Life Support Training CourseBfp Riva Morong RizalNo ratings yet
- First Aid Sports InjuriesDocument11 pagesFirst Aid Sports Injuriesjlemmon1979No ratings yet