Professional Documents
Culture Documents
Comparison of Different Drug Regimens For The Treatment of Loiasis-A TropNet Retrospective Study
Comparison of Different Drug Regimens For The Treatment of Loiasis-A TropNet Retrospective Study
Uploaded by
Lucchéri Ndong AkomezogheCopyright:
Available Formats
You might also like
- Sociological Odyssey Contemporary Readings in Introductory Sociology 4th Edition Adler Test BankDocument142 pagesSociological Odyssey Contemporary Readings in Introductory Sociology 4th Edition Adler Test BankAlexandraMaldonadotzcgn100% (14)
- Guest Speaker Lesson PlanDocument2 pagesGuest Speaker Lesson PlanKelley Thompson NeumannNo ratings yet
- Haze and Luminous Transmittance of Transparent Plastics: Standard Test Method ForDocument7 pagesHaze and Luminous Transmittance of Transparent Plastics: Standard Test Method ForFernando Da RosNo ratings yet
- Drama ScriptDocument3 pagesDrama ScriptDiana Zaibi57% (7)
- Legionnaires' DiseaseDocument14 pagesLegionnaires' Diseaselakshminivas PingaliNo ratings yet
- The Global Distribution and Transmission Limits of Lymphatic Filariasis: Past and PresentDocument20 pagesThe Global Distribution and Transmission Limits of Lymphatic Filariasis: Past and PresentNanda AzzahraNo ratings yet
- European Consensus Statement On Leptospirosis in Dogs and CatsDocument21 pagesEuropean Consensus Statement On Leptospirosis in Dogs and Catsnashfitriyah hidayatNo ratings yet
- LEPTOSPIROSIS ReviewDocument10 pagesLEPTOSPIROSIS ReviewwaktoleNo ratings yet
- Jurnal Kel. 2 FilariasisDocument9 pagesJurnal Kel. 2 FilariasisEka Saptaria NusantiNo ratings yet
- Immunomodulatory Therapy For The Management of Loiasis PDFDocument5 pagesImmunomodulatory Therapy For The Management of Loiasis PDFLucchéri Ndong AkomezogheNo ratings yet
- Covid19 PDFDocument6 pagesCovid19 PDFJeremy Kartika SoeryonoNo ratings yet
- Loa Loa-Does It Deserve To Be NeglectedDocument5 pagesLoa Loa-Does It Deserve To Be NeglectedLucchéri Ndong AkomezogheNo ratings yet
- Naegleria ReviewDocument61 pagesNaegleria ReviewKʀɪsʜɴᴀ ϟNo ratings yet
- Universa MedicaDocument11 pagesUniversa Medicarido eledNo ratings yet
- A Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in Nigeria: Kabuga and El ZowalatyDocument9 pagesA Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in Nigeria: Kabuga and El ZowalatyNers LollipopNo ratings yet
- Clinical Epidemiological and Spatial Features of HDocument15 pagesClinical Epidemiological and Spatial Features of HNealNo ratings yet
- Original ArticleDocument11 pagesOriginal ArticleLisamoni 786No ratings yet
- 1 s2.0 S1201971214015732 MainDocument18 pages1 s2.0 S1201971214015732 MainMichael JonesNo ratings yet
- Positive Francisella Tularensis Meningitis Outcome Despite Delayed Identification A Case ReportDocument5 pagesPositive Francisella Tularensis Meningitis Outcome Despite Delayed Identification A Case Reportd4rkgr455No ratings yet
- Reservoirs and Transmission Routes of Leprosy A SyDocument27 pagesReservoirs and Transmission Routes of Leprosy A SyPUSPA RUSUNAWANo ratings yet
- Lymphatic Filariasis PDFDocument12 pagesLymphatic Filariasis PDFBai Marifah LucasNo ratings yet
- Epidemiology of Elephantiasis With Special Emphasis On Podoconiosis Inethiopia: A Literature ReviewDocument6 pagesEpidemiology of Elephantiasis With Special Emphasis On Podoconiosis Inethiopia: A Literature ReviewSneha VaishnavNo ratings yet
- Faggionvinholo2020 Q1Document5 pagesFaggionvinholo2020 Q1NasriNo ratings yet
- MH 2 PDFDocument13 pagesMH 2 PDFNurul FajriNo ratings yet
- Pone. EbolaDocument12 pagesPone. EbolaJuan MoralesNo ratings yet
- LeptospirosisDocument14 pagesLeptospirosisClement ThansNo ratings yet
- Malaria Vs DBDDocument9 pagesMalaria Vs DBDade hajizah br ritongaNo ratings yet
- Najam 2021Document15 pagesNajam 2021Evelin YanaNo ratings yet
- Insecticide ResistanceDocument3 pagesInsecticide ResistanceGenniNo ratings yet
- A Five-Year Survey of Dematiaceous Fungi in A Tropical Hospital.Document11 pagesA Five-Year Survey of Dematiaceous Fungi in A Tropical Hospital.Anonymous argZ1ZNo ratings yet
- Journal of Pulmonary & Respiratory MedicineDocument5 pagesJournal of Pulmonary & Respiratory Medicinetitan dheaNo ratings yet
- pntd.0005941 BOMDocument16 pagespntd.0005941 BOMhenriquesbimbeNo ratings yet
- A Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in NigeriaDocument9 pagesA Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in NigeriaNadia Desanti RachmatikaNo ratings yet
- Laboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFDocument7 pagesLaboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFLucchéri Ndong AkomezogheNo ratings yet
- DNA Based Mothods For Diognosis of LFDocument10 pagesDNA Based Mothods For Diognosis of LFsenathilakenhks7068No ratings yet
- Journal PNTD 0010076Document19 pagesJournal PNTD 0010076yves.cosnuauNo ratings yet
- RRTM 12 153Document20 pagesRRTM 12 153pramitpatelphotographyNo ratings yet
- Jir 409Document10 pagesJir 409utkarsh PromotiomNo ratings yet
- John 2003Document8 pagesJohn 2003Ibtissam BelehssenNo ratings yet
- 62 Greenwood JCI 08Document11 pages62 Greenwood JCI 08Verlyanita SeptiariniNo ratings yet
- Natural Products As Soruce of Dengue AntiviralsDocument26 pagesNatural Products As Soruce of Dengue AntiviralsKaren SánchezNo ratings yet
- Complex Epidemiology of A Zoonotic Disease in A Culturally Diverse Region: Phylogeography of Rabies Virus in The Middle EastDocument17 pagesComplex Epidemiology of A Zoonotic Disease in A Culturally Diverse Region: Phylogeography of Rabies Virus in The Middle Eastwulan sitorusNo ratings yet
- Pone 0169324Document17 pagesPone 0169324data lmleNo ratings yet
- In Tech OpenDocument16 pagesIn Tech OpenZeo LeoNo ratings yet
- Epidemiology of Visceral LeishmaniasisDocument9 pagesEpidemiology of Visceral LeishmaniasismclimacoNo ratings yet
- A Century of Clinical Use of Phages A Literature RDocument23 pagesA Century of Clinical Use of Phages A Literature RIsidora NikolicNo ratings yet
- The Management of Patients With Severe Malaria: AbstractDocument7 pagesThe Management of Patients With Severe Malaria: AbstractHervi LaksariNo ratings yet
- Viruses 11 00018Document21 pagesViruses 11 00018ismah ibtihaNo ratings yet
- Time For A Farewell To Soap in The Eye?Document4 pagesTime For A Farewell To Soap in The Eye?yazzNo ratings yet
- A Systematic Review On Leptospirosis in Cattle A European PerspectiveDocument11 pagesA Systematic Review On Leptospirosis in Cattle A European PerspectiveTORRES GUTIERREZ JOYNY RAQUEL catedraticoNo ratings yet
- Current Status of Leprosy: Epidemiology, Basic Science and Clinical PerspectivesDocument9 pagesCurrent Status of Leprosy: Epidemiology, Basic Science and Clinical PerspectivesYolan Sentika NovaldiNo ratings yet
- World Allergy OrganizationDocument25 pagesWorld Allergy OrganizationHusnul HanifaNo ratings yet
- Pone 0285900Document11 pagesPone 0285900Walter Huamani AlvitesNo ratings yet
- Ebola - Virus - Disease - DINA01-dikonversiDocument13 pagesEbola - Virus - Disease - DINA01-dikonversidina amalikaNo ratings yet
- The Clinical and Immunological Features of Leprosy: S. L. Walker and D. N. J. LockwoodDocument19 pagesThe Clinical and Immunological Features of Leprosy: S. L. Walker and D. N. J. LockwoodMariana MarquesNo ratings yet
- Adult Interstitial Lung Diseases and Their Epidemiology 2019Document46 pagesAdult Interstitial Lung Diseases and Their Epidemiology 2019Mary CogolloNo ratings yet
- Antimalarial Drug Mefloquine Is A Possible CureDocument8 pagesAntimalarial Drug Mefloquine Is A Possible Curehuma javeriaNo ratings yet
- Filaria TerbaruDocument6 pagesFilaria TerbaruAbdul GhofurNo ratings yet
- Pathogenesis and PathologyDocument12 pagesPathogenesis and Pathologydies100% (1)
- LeprosyDocument3 pagesLeprosyNadim DinaniNo ratings yet
- Tropical Fevers: C. Important Human Parasitic Fevers of The TropicsDocument25 pagesTropical Fevers: C. Important Human Parasitic Fevers of The TropicsMohammad Jofa Rachman PNo ratings yet
- Childhood Leptospirosis in An Industrialized Country: Population-Based Study in Okinawa, JapanDocument10 pagesChildhood Leptospirosis in An Industrialized Country: Population-Based Study in Okinawa, JapansabrinaNo ratings yet
- Ebola Virus Disease: A Manual for EVD ManagementFrom EverandEbola Virus Disease: A Manual for EVD ManagementMarta LadoNo ratings yet
- IL-10 and Its Related Superfamily Members IL-19 and IL-24 Provide Parallel Redundant Immune-Modulation in Loa Loa Infection PDFDocument9 pagesIL-10 and Its Related Superfamily Members IL-19 and IL-24 Provide Parallel Redundant Immune-Modulation in Loa Loa Infection PDFLucchéri Ndong AkomezogheNo ratings yet
- Laboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFDocument7 pagesLaboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFLucchéri Ndong AkomezogheNo ratings yet
- Ivermectin Inhibits Extracellular Vesicle Secretion From Parasitic Nematodes PDFDocument15 pagesIvermectin Inhibits Extracellular Vesicle Secretion From Parasitic Nematodes PDFLucchéri Ndong AkomezogheNo ratings yet
- Human Loiasis in A Cameroonian Village A Double-Blind, Placebo-Controlled, Crossover Clinical Trial of Athree-Day Albendazole RegimenDocument5 pagesHuman Loiasis in A Cameroonian Village A Double-Blind, Placebo-Controlled, Crossover Clinical Trial of Athree-Day Albendazole RegimenLucchéri Ndong AkomezogheNo ratings yet
- Immunomodulatory Therapy For The Management of Loiasis PDFDocument5 pagesImmunomodulatory Therapy For The Management of Loiasis PDFLucchéri Ndong AkomezogheNo ratings yet
- Albendazole-Related Loa Loa EncephalopathyDocument2 pagesAlbendazole-Related Loa Loa EncephalopathyLucchéri Ndong AkomezogheNo ratings yet
- Loa Loa-Does It Deserve To Be NeglectedDocument5 pagesLoa Loa-Does It Deserve To Be NeglectedLucchéri Ndong AkomezogheNo ratings yet
- The Population Biology and Transmission Dynamics of Loa Loa: ReviewDocument16 pagesThe Population Biology and Transmission Dynamics of Loa Loa: ReviewLucchéri Ndong AkomezogheNo ratings yet
- Cause and Effect EssayDocument2 pagesCause and Effect EssayRida ShakilNo ratings yet
- BJT PDFDocument14 pagesBJT PDFRaka Satria PradanaNo ratings yet
- Examination Pattern - Docx MAPC 1 Cognitive Psychology, Learning and MemoryDocument8 pagesExamination Pattern - Docx MAPC 1 Cognitive Psychology, Learning and MemoryakileshaiyerNo ratings yet
- Job Description For Hse AdvisorDocument2 pagesJob Description For Hse AdvisorSam JoseNo ratings yet
- Lecture Notes: Manila Cavite Laguna Cebu Cagayan de Oro DavaoDocument5 pagesLecture Notes: Manila Cavite Laguna Cebu Cagayan de Oro DavaoDenny June CraususNo ratings yet
- Intensive Care NursesDocument15 pagesIntensive Care NursesUlysses GamayonNo ratings yet
- Sara Ahmed - Happiness and Queer PoliticsDocument20 pagesSara Ahmed - Happiness and Queer Politicsferwerdasma100% (1)
- Test Unit 1: Listening Answer KeyDocument2 pagesTest Unit 1: Listening Answer KeyLaty86No ratings yet
- 4Ms of Production ManagementDocument84 pages4Ms of Production ManagementVincent L. SantiagoNo ratings yet
- For Tuesday, Mar 21 : Venture Capital Problem SetDocument3 pagesFor Tuesday, Mar 21 : Venture Capital Problem SetJerry Chang0% (1)
- In Loco Parentis or As Substitute Parents, As Expressly Provided UnderDocument4 pagesIn Loco Parentis or As Substitute Parents, As Expressly Provided UnderGESELLEENDICO06No ratings yet
- Millimeter Wave Therapy-Disease and PointsDocument31 pagesMillimeter Wave Therapy-Disease and Pointsalfredo.bioxinNo ratings yet
- Six-Sided SagasDocument14 pagesSix-Sided SagasJames Hargrove50% (2)
- Leadership and Management ProjectDocument12 pagesLeadership and Management Projectshian ramdialNo ratings yet
- Bioprogressive Therapy As An AnswerDocument39 pagesBioprogressive Therapy As An Answerelenaelena2011No ratings yet
- The Kelingai Motif' in Iban's Tattoo Motif A Case Study of Kampung Gayau Ulu Pantu, Sri Aman SarawakDocument10 pagesThe Kelingai Motif' in Iban's Tattoo Motif A Case Study of Kampung Gayau Ulu Pantu, Sri Aman SarawaktimartiNo ratings yet
- Managing Markets Strategically: Professor Noel CaponDocument53 pagesManaging Markets Strategically: Professor Noel CaponMoidin AfsanNo ratings yet
- Homophobic Transphobic Bullying Pe Focus1Document2 pagesHomophobic Transphobic Bullying Pe Focus1api-440470277No ratings yet
- Social StructureDocument11 pagesSocial StructureabbiecdefgNo ratings yet
- Match Fixing by Judges & PoliceDocument193 pagesMatch Fixing by Judges & PoliceNagaraja Mysuru RaghupathiNo ratings yet
- Action Plan in MathDocument4 pagesAction Plan in Mathjoanna marie limNo ratings yet
- Rmullinsresume 2019Document2 pagesRmullinsresume 2019api-448247344No ratings yet
- 1 Mirrors PDFDocument30 pages1 Mirrors PDFKevin MaylowNo ratings yet
- Liste Jeux PS Vita Boites PALDocument1 pageListe Jeux PS Vita Boites PALDenis Alibor MajhenNo ratings yet
- MRP Report Chapterwise - 2 PDFDocument95 pagesMRP Report Chapterwise - 2 PDFAfnanParkerNo ratings yet
- LAW - ON - SALES CH 4 Sec 3Document4 pagesLAW - ON - SALES CH 4 Sec 3MaricrisNo ratings yet
Comparison of Different Drug Regimens For The Treatment of Loiasis-A TropNet Retrospective Study
Comparison of Different Drug Regimens For The Treatment of Loiasis-A TropNet Retrospective Study
Uploaded by
Lucchéri Ndong AkomezogheOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Comparison of Different Drug Regimens For The Treatment of Loiasis-A TropNet Retrospective Study
Comparison of Different Drug Regimens For The Treatment of Loiasis-A TropNet Retrospective Study
Uploaded by
Lucchéri Ndong AkomezogheCopyright:
Available Formats
RESEARCH ARTICLE
Comparison of different drug regimens for
the treatment of loiasis—A TropNet
retrospective study
Federico Gobbi ID1*, Emmanuel Bottieau2, Olivier Bouchaud3, Dora Buonfrate ID1,
Fernando Salvador ID4, Gerardo Rojo-Marcos ID5, Paola Rodari1, Jan Clerinx2,
Begoña Treviño ID6, Juan Paulo Herrera-Ávila5, Andreas Neumayr7, Guido Calleri8,
Andrea Angheben1, Camilla Rothe9,10, Lorenzo Zammarchi11, Massimo Guerriero12,
Zeno Bisoffi1
1 IRCCS Center for Tropical Diseases, Ospedale Sacro Cuore Don Calabria, Negrar, Verona, Italy,
2 Department of Clinical Sciences, Institute of Tropical Medicine, Antwerp, Belgium, 3 Service des Maladies
Infectieuses et Tropicales, CHU Avicenne, Assistance Publique Hôpitaux de Paris, Paris, France,
a1111111111 4 Infectious Diseases Department, Vall d’Hebron University Hospital, PROSICS Barcelona, Barcelona,
a1111111111 Spain, 5 Hospital Universitario Prı́ncipe de Asturias, Alcalá de Henares, Madrid, Spain, 6 International Health
Unit Vall d’Hebron-Drassanes, PROSICS Barcelona, Barcelona, Spain, 7 Swiss Tropical and Public Health
a1111111111
Institute, Basel, Switzerland, 8 Unit A of Infectious and Tropical Diseases, Amedeo di Savoia Hospital, Turin,
a1111111111 Italy, 9 University Hospital Medical Centre, Hamburg, Germany, 10 LMU Medical Centre, Munich, Germany,
a1111111111 11 Dipartimento di Medicina Sperimentale e Clinica, Università di Firenze; SOD Malattie Infettive e Tropicali,
Azienda Ospedaliero Universitaria Careggi, Florence, Italy, 12 Department of Computer Science, University
of Verona, Verona, Italy
* federico.gobbi@sacrocuore.it
OPEN ACCESS
Citation: Gobbi F, Bottieau E, Bouchaud O,
Buonfrate D, Salvador F, Rojo-Marcos G, et al. Abstract
(2018) Comparison of different drug regimens for
the treatment of loiasis—A TropNet retrospective Background
study. PLoS Negl Trop Dis 12(11): e0006917. Loa loa infection is endemic in limited areas of West-Central Africa. Loiasis has been associ-
https://doi.org/10.1371/journal.pntd.0006917
ated with excess mortality, but clinical studies on its treatment are scant, particularly outside
Editor: Timothy G. Geary, McGill University, endemic areas, due to the rarity of cases diagnosed.
CANADA
Received: May 5, 2018 Methodology/Principal findings
Accepted: October 11, 2018 With this retrospective TropNet (European Network for Tropical Medicine and Travel Health)
Published: November 1, 2018 study, we aimed at outlining the treatment schedules followed by different reference centers
Copyright: © 2018 Gobbi et al. This is an open
for tropical medicine across Europe. We gathered information about 238 cases of loiasis,
access article distributed under the terms of the 165 of which had follow up data. The regimens followed by the different centers were hetero-
Creative Commons Attribution License, which geneous. The drugs most frequently administered were: diethylcarbamazine alone (74/165,
permits unrestricted use, distribution, and
45.1%), ivermectin alone (41/165, 25%), albendazole + ivermectin (21/164, 11.6%), iver-
reproduction in any medium, provided the original
author and source are credited. mectin + diethylcarbamazine (16/165, 9.7%).
Data Availability Statement: The dataset has been
uploaded in Zenodo repository with the DOI 10.
Conclusions/Significance
5281/zenodo.1470141. The management of loiasis substantially differs across specialized travel clinics in Europe.
Funding: The authors received no specific funding These discrepancies could be due to different local protocols as well as to (un)availability of
for this work. the drugs. An harmonization of clinical protocols for the treatment of loiasis would be sug-
Competing interests: The authors have declared gested across reference centers for tropical medicine in Europe.
that no competing interests exist.
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 1 / 11
Different regimens for the treatment of loiasis
Author summary
Loa loa is a worm which infects millions of people living in wide forested areas of central
Africa. The infection is rarely diagnosed outside Africa, and cases are mainly referred to
referral centers on tropical medicine. Aim of this study was to describe the treatment and
management of patients diagnosed with loiasis in some referral centers for tropical medi-
cine in Europe. The results showed that different health centers treat the patients with dif-
ferent drugs/drug combinations. On the basis of the availability of the drugs and on the
data observed, common protocols might be recommended for the participating centers.
Introduction
Loa loa is a filarial worm transmitted to the human hosts by the tabanid flies of the genus Chry-
sops. Human loiasis occurs only in Africa, where the transmission is confined to the rainforests
areas from south-eastern Benin in the west, South Sudan and Uganda in the east, North
Angola in the south[1]. Adult worms moving in subcutaneous tissues can live for more than
15 years: moreover, after a prepatent period of a minimum of six months, they can produce
microfilariae (mff), circulating in peripheral blood with a diurnal periodicity[2]. The most
common clinical manifestations due to adult worms and/or mff are "Calabar swelling" (tran-
sient angioedema of allergic nature) and pruritus. Moreover, adult worms may be noticed
when they pass under the conjunctiva of the eye ("eyeworm"). Albeit rarely, loiasis can cause
damage to other organs[2]. Loiasis had been considered as a benign disease until a retrospec-
tive study recently demonstrated an excess of mortality in patients with high microfilaremia
[3], and advocated more studies on this disease[4]. Currently three drugs may be used for the
treatment of loiasis: diethylcarbamazine (DEC), ivermectin (IVM) and albendazole (ALB).
DEC is the drug of choice because of its macro- and microfilaricidal activity, that causes a
rapid decrease in the Loa loa microfilaremia, although sometimes multiple courses of DEC are
required to achieve clinical and parasitological cure[5]. DEC is considered as contra-indicated
in patients with a high microfilarial density (>8.000 mff/ml), because of the risk of encepha-
lopathy[6]. Moreover, this drug is not currently available in Europe[7]. In fact, in an inquiry
involving 69 TropNet (European Network for Tropical Medicine and Travel Health) centers
in Europe, DEC was immediately available in 25 centers, available within a few days in 11, and
not available in 33[8]. Ivermectin has a marked microfilaricidal effect (Loa microfilaremia
decreases by 70–80% within the first 3 days after a single dose of 150 μg/kg)[9], but is probably
not active on macrofilariae[6]. Besides this, this drug should be administered with caution in
case of microfilaremia > 8,000/ml and can also induce an encephalopathy in people with very
high microfilarial densities (>30,000/ml), contra-indicating its use above that level[6,10].
Short courses of ALB have little effect on Loa loa[11,12], but when given at a dose of 200 mg
twice a day for 21 days, the drug has probably an embryotoxic effect (i.e., it interrupts embryo-
genesis in the uterus of the adult female worm), and possibly also a macrofilaricidal effect[13].
This being said, the treatment strategy depends firstly on the risk of adverse events, which is
related to the patient’s Loa microfilarial density. In fact, given the risk of serious adverse events
after DEC or IVM treatment, Boussinesq proposed the following strategy: ALB for microfilar-
ial loads higher than 8,000/mL, followed by IVM when microfilarial density is between 2,000
and 8,000/mL, DEC when microfilarial density is below 2,000/mL[6]. Two series published in
1986[14] and in 1996[15], reported that a single course of treatment with DEC for 21 days
achieves a cure rate of 55% and 66%, respectively. Four recent papers, a case series of 47
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 2 / 11
Different regimens for the treatment of loiasis
imported cases in France[16], a review of 101 cases reported in non-endemic countries[17], a
case series of 100 cases in a single centre in Italy[18], and a case series of 50 cases in London
[19], revealed a wide heterogeneity of treatment regimens and follow -up patterns over the last
three decades across Europe, highlighting that the management of imported loiasis needs stan-
dardization. A randomized controlled trial (RCT) comparing different drugs in non-endemic
countries, is problematic, due to the relatively small number of cases diagnosed per travel clinic
and the differences in drug availability between countries. The primary objective of this study
was to describe the different drugs regimens used for imported loiasis in different TropNet
sites. Secondary objectives include the description of the treatment outcome and tolerability of
the drugs used.
Methods
This is an observational, retrospective study, analyzing data collected between 1996 and 2015
at TropNet centers participating in this study.
Ethical issues
The study protocol was submitted to the Ethics committee of the coordinating centre (Comi-
tato Etico per la Sperimentazione Clinica delle Province di Verona e Rovigo), and obtained a
waiver of informed consent on the 13th July 2016.
Inclusion criteria
All individuals who had been traveling or living in an endemic country AND were diagnosed
with loiasis (according to the case definition given below) AND were treated with either DEC
alone, IVM alone, ALB alone, ALB + DEC, IVM + DEC or ALB + IVM (at the dosages speci-
fied below) AND had at least one follow up visit � 1 month after treatment AND had not trav-
eled to any endemic country before the last follow up evaluation. Eligible drug regimens for
patient inclusion: DEC, 6 mg/kg/day for 21 days; IVM, 150–200 μg/kg as a single dose; ALB,
200–400 mg twice a day for 21–28 days.
Exclusion criteria
All patients treated with any other drug regimen. Patients retreated after first treatment
failure.
Definitions
A case of loiasis was defined in this study as the presence -or history (in the last two months)—
of eyeworm OR the demonstration of Loa loa microfilaremia OR the presence -or history (in
the last two months)- of a Calabar swelling associated with eosinophilia (defined as > 450
eosinophils/μL).
Clearance of symptoms was defined as the lack of re-occurrence of the clinical signs/symp-
toms present at inclusion (Calabar swellings, eyeworm) in the time frame going from treat-
ment to the last available follow up visit. Parasitological outcome was assessed on the basis of
values of microfilaremia and eosinophil count at the last available follow up visit. Circulating
microfilariae were detected in 9 mL of peripheral blood collected on daytime using a modified
Knott technique followed by Giemsa staining for species identification.
For each patient, information on clinical history, laboratory examinations, and treatment
was extracted from the medical records, and entered into a Google Drive case report form
(CRF). An anonymous code was assigned to each patient.
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 3 / 11
Different regimens for the treatment of loiasis
Primary outcome
1. Frequency of drug regimens used to treat imported loiasis.
Secondary outcomes
1. Proportion of patients with negativization of microfilaremia and normal eosinophil count
at the last available follow-up for each treatment, over the total number of patients who
received that treatment.
2. Proportion of patients presenting clearance of symptoms for each treatment strategy, over
the total number of patients receiving that treatment.
3. Trend in residual microfilaremia for patients who did not cleared it. In this analysis were
excluded patients with negative microfilaremia at baseline and patients with positive mff
but missing value (both at baseline and at the last follow up).
4. Rates of adverse events (AE) in each treatment group.
Statistical analysis
The analyses were performed using Epi Info version 3.5.1 (Centers for Disease Control and
Prevention, Atlanta, GA, USA) and Stata vers. 15 (StataCorp. 2017. Stata Statistical Software:
Release 15. College Station, TX: StataCorp LLC). Categorical variables were reported as fre-
quencies and percentages whilst discrete or continuous variables as medians and interquartile
ranges (IQR).
Results
Eleven TropNet centers from seven countries [Belgium(1 center), Finland(1), France(1), Ger-
many(1), Italy(3), Spain(3), and Switzerland(1)] participated in the study. Initially, 293 cases
were evaluated for inclusion (Fig 1), but 55 of them did not meet the inclusion criteria for loia-
sis. The main results of the 238 cases of loiasis included in the study are reported in Table 1.
The different regimens were administered according to the schedules indicated in methods.
Complete treatment and follow-up data were available for 165 cases, who were therefore
included in the outcome analysis (Table 2).
The treatment most frequent administered was DEC (74/165, 45.1%), followed by IVM
(41/165, 25%), and ALB (5/165, 3.7%). Combination therapies were: ALB + IVM in 21 out of
164 (11.6%) cases, IVM + DEC in 16 of 165 (9.7%) cases, and ALB + DEC in 8 of 165 (4.9%)
cases. Baseline characteristics per administered treatment are reported in Table 3.
Migrants accounted for 42.9% in the ALB + IVM group, 43.7% in the IVM + DEC group,
54.0% in the DEC group, and 72.5% in the IVM group. Median baseline values of eosinophilia
ranged between 1,406/ml and 1,620/ml in all groups, but the IVM + DEC group, in which the
median eosinophilia was 4,700/ml (IQR 1,920; 8,045). Microfilaremic patients accounted for
9.8% in the IVM group, 37.5% in the IVM + DEC group, 60.8% in the DEC group, and 71.4%
in the ALB + IVM group. The median values of microfilaremia were 172 mff/ml in the ALB +
IVM group, 309/ml in the DEC group, 4,820/ml in the IVM group (only 4 patients), 8,107/ml
in the IVM + DEC group. The median time from treatment completion to the last follow up
visit was 4.5 months (IQR 2.5; 10.5). Clinical outcome is reported in Table 4.
Clearance of parasitemia and normal eosinophil count were observed in 67% of patients
treated with ALB+IVM, in half of the patients in the DEC group, 44% in the DEC+IVM
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 4 / 11
Different regimens for the treatment of loiasis
group, 38% in DEC+ALB group, 18% in the patients treated with IVM alone, in none of the 5
patients treated with ALB alone.
For two patients treated with IVM, the parasitological follow up data were unavailable. The
information on clinical outcome was lacking in 58 out of 165 (35.1%). Re-occurrence of symp-
toms was observed in 1/15 (7%) of ALB + IVM treated cases, compared with 4/14 (29%) of
IVM + DEC, 15/48 (31%) of DEC and 12/25 (48%) of IVM.
We then analyzed the trend of microfilaremia in patients who did not clear parasitemia.
This analysis was performed for the whole sample and for patients who were treated with
either DEC or ALB+IVM, as the latter two groups were the ones that presented a sufficient
number of cases permitting this analysis (excluding IVM alone as clearly ineffective). The
results are shown in Fig 2: all the three groups considered demonstrated a consistent reduction
in the median values of microfilaremia.
Side effects
No serious AE was registered. Patients treated with I and A alone had no AE. Two patients in
the AI group (2/21, 9.5%) reported itching; other two patients in the DA group reported
Fig 1. Flow chart of selection of patients with loiasis.
https://doi.org/10.1371/journal.pntd.0006917.g001
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 5 / 11
Different regimens for the treatment of loiasis
Table 1. Characteristics of the 238 patients with loiasis.
Characteristic Number (%) Median (Q1;Q3)
Age 37 (27.5; 55)
Male gender 129 (54.2)
Patient classification (n = 231)
Migrants 149 (64.5)
Travelers 28 (12.1)
Expatriates > 6 months 54 (23.4)
Country of diagnosis
France 108 (45.4)
Belgium 71 (29.8)
Spain 30 (12.6)
Italy 23 (9.6)
Germany 3 (1.3)
Switzerland 3 (1.3)
Country of infection (n = 234)
Cameroon 133 (56.8)
Equatorial Guinea 28 (12.0)
Gabon 22 (9.4)
Democratic Republic of Congo 22 (9.4)
Congo 19 (8.2)
Central African Republic 4 (1.7)
Nigeria 3 (1.3)
South Sudan 1 (0.4)
Chad 1 (0.4)
Angola 1 (0.4)
Presence of symptoms of loiasis 234/238 (98.3)
Calabar swellings 106 (45.3)
Eyeworm 57 (24.2)
Eyeworm and Calabar swelling 24 (10.3)
Presence of eosinophilia (>450 eos / mL) 209 (87.8)
Median value of eosinophilia (mmf/mL) 1,480 (925; 3,180)
Presence of mf/ mL 105 (44.3)
Median value of mmf 311 (52; 1,782)
IQR = Interquartile range.
https://doi.org/10.1371/journal.pntd.0006917.t001
itching (2/8, 25%), and one patient in the same group reported dizziness. Itching was also
reported by three patients of 16 in the DI group (3/16, 18.7%), and one patient in the same
group reported dyspnea. The number of AE registered for patients in the D group was 19 (19/
74, 25.7%): 8 patients reported itching (8/74, 10.8%), 5 fever (5/74, 6.7%), 2 had a syncope (2/
74, 2.7%), and single patients reported one of the following symptoms: thoracic pain, abdomi-
nal pain, dizziness, skin rash. None of the patients had to stop the treatment due to AE.
Discussion
To our knowledge, this is the largest case series of loiasis treatment of imported cases ever pub-
lished in non-endemic settings, where the observation of treatment response is not hampered
by possible re-infections. The first striking observation was that the management of loiasis sub-
stantially differs even across specialized travel clinics of TropNet network sites. Not only six
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 6 / 11
Different regimens for the treatment of loiasis
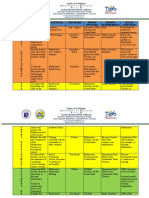
Table 2. Number and type of patients, drug regimen for each TropNet center.
TropNet N. of patients Exp. Mig. Trav. DEC IVM ALB IVM + DEC DEC + ALB ALB + IVM
Center
Antwerp 69 30 28 11 53 1 15
Paris 43 3 31 8 4 38 1
(for France)
Negrar Verona 19 8 8 3 19
Barcelona 14 14 10 1 3
(Vall d’Hebron)
Madrid (Alcalà de Henares) 11 11 4 1 1 1 4
Basel 3 1 2 1 2
Turin 3 2 1 1 1 1
Hamburg 2 1 1 1 1
Florence 1 1 1
https://doi.org/10.1371/journal.pntd.0006917.t002
different therapeutic regimens were used, but also the timing and lab approach for follow up
differed. These discrepancies could be due to different local protocols as well as to (un)avail-
ability of the drugs (IVM is not registered in the majority of the European countries, DEC is
not registered and often very difficult to find) and peculiarities of the patients. Indeed, 85.4%
of the patients were either migrants or expatriates, who are not sedentary and could be more
difficult to follow up at regular time points.
In terms of outcome, we found that only 50% of patients treated with DEC alone achieved a
parasitological cure. This drug showed a cure rate of 73% in a work by Saito et al[19], while in
the only study reporting a long-term follow up after DEC treatment in non-endemic countries
the efficacy after a single treatment course resulted of only 38%[5]. Taken all together, these
results suggest that DEC monotherapy is often unsuccessful, despite its micro and macrofilari-
cidal activity[19]. The combination of DEC with IVM or ALB did not improve the proportion
of parasitological cure. On the other hand, the combination ALB + IVM provided a high pro-
portion of parasitological cure. Although this observation should be taken with caution, given
the small number on patients in this group, exploring the efficacy of this combination deserves
further research, considering: 1) the synergy of the mode of action of the two drugs (ALB prob-
able macrofilaricidal and IVM microfilaricidal); 2) safety issues: given as the first drug, ALB
would reduce the levels of mmf and overcome the possibility of severe adverse events due to a
massive death of mff, caused by IVM; 3) the serious threaten to the availability of DEC. Indeed,
this treatment option also fits with the treatment strategy previously proposed by Boussinesq
[6]. However, larger prospective studies to explore whether this regimen could represent a
Table 3. Baseline characteristics of the patients according to the treatment group.
DEC IVM ALB IVM + DEC DEC + ALB ALB + IVM
Migrants 40/74 29/40 5/5 7/16 7/8 9/21
(54%) (72.5%) (100%) (43.7%) (87.5%) (42.9%)
Patients with microfilaremia 45/74 4/41 5/5 6/16 8/8 15/21
(60.8%) (9.8%) (100%) (37.5%) (100%) (71.4%)
Microfilaremia 309 4,820 2 8,107 556 172
(per ml)–median(Q1;Q3) (48–2016) (800–7,760) (1–505) (682–16,773) (145–1,300) (26–791)
Eosinophilia (per ml)–median (Q1;Q3) 1,410 1,406 1,450 4,700 1,600 1,620
(860–2940) (995–2,746) (1,011–1,603) (1,920–8,045) (850–3,745) (790–4,100)
DEC = Diethylcarbamazine, IVM = ivermectin, ALB = albendazole, IQR = Interquartile range
https://doi.org/10.1371/journal.pntd.0006917.t003
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 7 / 11
Different regimens for the treatment of loiasis
Table 4. Parasitological and clinical outcome of 165 patients with follow-up.
PARASITOLOGICAL OUTCOME DEC IVM ALB IVM + DEC DEC + ALB ALB + IVM
Clearance of mmf + normal eosinophil count 37/74 (50.0%) 7/39 (17.9%) 0/5 7/16 (43.7%) 3/8 (37.5%) 14/21
(0%) (66.7%)
Persisting mmf and/or eosinophilia 37/74 (50.0%) 32/39 (82.1%) 5/5 9/16 (56.3%) 5/8 (62.5%) 7/21
(100%) (33.3%)
CLINICAL OUTCOME
Clearance of symptoms 33/48 (68.7%) 13/25 (52.0%) 1/2 10/14 (71.4%) 2/2 (100%) 14/15
(50.0%) (93.3%)
Re-occurrence of symptoms 15/48 (31.3%) 12/25 (48.0%) 1/2 4/14 (28.6%) 0/2 1/15
(50.0%) (0%) (6.7%)
DEC = Diethylcarbamazine, IVM = ivermectin, ALB = albendazole
https://doi.org/10.1371/journal.pntd.0006917.t004
valid alternative to DEC are needed. In addition, it must be taken into account that in our
work almost all patients (20/21) treated with this regimen received ALB at the dose of 400 mg
twice a day for 28 days, which is a higher dose given for a longer period compared with what
has been previously reported[13]. IVM alone showed poor efficacy (parasitological cure 18%),
which is not surprising as its action seems to be purely microfilaricidal. Although the drug is
Fig 2. Box plots showing the trend of microfilaremia in patients who did not clear parasitemia. Due to a strong asymmetry of mmf count,
variable data were transformed by zero-skewness log transformation.
https://doi.org/10.1371/journal.pntd.0006917.g002
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 8 / 11
Different regimens for the treatment of loiasis
not capable of clearing the infection, it can contribute to reduce transmission in endemic
countries by reducing microfilaremia in affected populations.
Study limitations
The main limitation of this study is represented by its retrospective design and the substantial pro-
portion of missing data. Also, different drug dosages and durations were used in the study sites,
thus limiting the comparison among the regimens. A statistical inference on the different out-
comes after each regimen was not performed, as the recruitment was not random and the groups
differed markedly before treatment. Indeed, clearance of symptoms, reduction of microfilaremia
and eosinophilia are the parameters usually considered to follow up patients with Loa loa infec-
tion, but there are no clear indications for the timing of follow-up and the cut-off values defining
cure. Finally, the clinical outcome may be difficult to assess, for example in case of persistence of
symptoms not clearly attributable to loiasis (such as edemas reported by the patients, but not
observed by the health staff). Despite these limitations, we were able to provide useful clinical
information on a neglected disease for which complete follow up data are hardly available[16–19].
Conclusions
This paper shows that, in absence of specific guidelines, different reference centers for tropical
diseases in Europe use different treatment schedules for loiasis. Our study suggests that some
alternative recommendations may be possible for the treatment of loiasis in non-endemic
areas, also in consideration of the unavailability of some drugs (namely, DEC). Ideally, a ran-
domized clinical trial would provide a much more robust base of evidence to support manage-
ment guidelines, but its feasibility in non-endemic countries is questionable. Nevertheless, an
observational, prospective study, with well-defined criteria for inclusion and for definition of
cure, would be a valuable option in order to evaluate the proposed management indications.
Supporting information
S1 Checklist. STROBE checklist.
(DOCX)
Acknowledgments
We wish to acknowledge Seedley Charles, Alexandra Sophia Affricot, Joaquin Salas-Coronas,
Heli Siikamaki and the French study group on loiasis for their kind support in this study.
Author Contributions
Conceptualization: Federico Gobbi.
Data curation: Federico Gobbi, Emmanuel Bottieau, Olivier Bouchaud, Fernando Salvador,
Gerardo Rojo-Marcos, Paola Rodari, Jan Clerinx, Begoña Treviño, Juan Paulo Herrera-
Ávila, Andreas Neumayr, Guido Calleri, Andrea Angheben, Camilla Rothe, Lorenzo Zam-
marchi, Massimo Guerriero.
Formal analysis: Federico Gobbi, Dora Buonfrate, Massimo Guerriero.
Funding acquisition: Federico Gobbi.
Investigation: Federico Gobbi, Emmanuel Bottieau, Olivier Bouchaud, Fernando Salvador,
Gerardo Rojo-Marcos, Paola Rodari, Jan Clerinx, Begoña Treviño, Juan Paulo Herrera-
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 9 / 11
Different regimens for the treatment of loiasis
Ávila, Andreas Neumayr, Guido Calleri, Andrea Angheben, Camilla Rothe, Lorenzo
Zammarchi.
Methodology: Dora Buonfrate, Massimo Guerriero, Zeno Bisoffi.
Software: Massimo Guerriero.
Supervision: Federico Gobbi, Zeno Bisoffi.
Visualization: Zeno Bisoffi.
Writing – original draft: Federico Gobbi, Dora Buonfrate.
Writing – review & editing: Federico Gobbi, Emmanuel Bottieau, Olivier Bouchaud, Fer-
nando Salvador, Gerardo Rojo-Marcos, Paola Rodari, Jan Clerinx, Begoña Treviño, Juan
Paulo Herrera-Ávila, Andreas Neumayr, Guido Calleri, Andrea Angheben, Camilla Rothe,
Lorenzo Zammarchi, Zeno Bisoffi.
References
1. Zoure HG, Wanji S, Noma M, Amazigo UV, Diggle PJ, et al. (2011) The geographic distribution of Loa loa
in Africa: results of large-scale implementation of the Rapid Assessment Procedure for Loiasis (RAPLOA).
PLoS Negl Trop Dis 5: e1210. https://doi.org/10.1371/journal.pntd.0001210 PMID: 21738809
2. Boussinesq M (2006) Loiasis. Ann Trop Med Parasitol 100: 715–731. https://doi.org/10.1179/
136485906X112194 PMID: 17227650
3. Chesnais CB, Takougang I, Paguele M, Pion SD, Boussinesq M (2017) Excess mortality associated
with loiasis: a retrospective population-based cohort study. Lancet Infect Dis 17: 108–116. https://doi.
org/10.1016/S1473-3099(16)30405-4 PMID: 27777031
4. Metzger WG, Mordmuller B (2013) Loa loa-does it deserve to be neglected? Lancet Infect Dis.
5. Klion AD, Ottesen EA, Nutman TB (1994) Effectiveness of diethylcarbamazine in treating loiasis
acquired by expatriate visitors to endemic regions: long-term follow-up. J Infect Dis 169: 604–610.
PMID: 8158033
6. Boussinesq M (2012) Loiasis: new epidemiologic insights and proposed treatment strategy. J Travel
Med 19: 140–143. https://doi.org/10.1111/j.1708-8305.2012.00605.x PMID: 22530819
7. Buonfrate D, Gobbi F, Bisoffi Z (2017) Helminths in organ transplantation. Lancet Infect Dis 17: 581–582.
8. http://www.tropnet.eu/indexphp?id=200&fsize=2%27A%3D0
9. Gardon J, Kamgno J, Folefack G, Gardon-Wendel N, Bouchite B, et al. (1997) Marked decrease in Loa
loa microfilaraemia six and twelve months after a single dose of ivermectin. Trans R Soc Trop Med Hyg
91: 593–594. PMID: 9463678
10. Gardon J, Gardon-Wendel N, Demanga N, Kamgno J, Chippaux JP, et al. (1997) Serious reactions
after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet
350: 18–22. https://doi.org/10.1016/S0140-6736(96)11094-1 PMID: 9217715
11. Tabi TE, Befidi-Mengue R, Nutman TB, Horton J, Folefack A, et al. (2004) Human loiasis in a Cameroo-
nian village: a double-blind, placebo-controlled, crossover clinical trial of a three-day albendazole regi-
men. Am J Trop Med Hyg 71: 211–215. PMID: 15306713
12. Kamgno J, Nguipdop-Djomo P, Gounoue R, Tejiokem M, Kuesel AC (2016) Effect of Two or Six Doses
800 mg of Albendazole Every Two Months on Loa loa Microfilaraemia: A Double Blind, Randomized,
Placebo-Controlled Trial. PLoS Negl Trop Dis 10: e0004492. https://doi.org/10.1371/journal.pntd.
0004492 PMID: 26967331
13. Klion AD, Horton J, Nutman TB (1999) Albendazole therapy for loiasis refractory to diethylcarbamazine
treatment. Clin Infect Dis 29: 680–682. PMID: 10530467
14. Nutman TB, Miller KD, Mulligan M, Ottesen EA (1986) Loa loa infection in temporary residents of
endemic regions: recognition of a hyperresponsive syndrome with characteristic clinical manifestations.
J Infect Dis 154: 10–18. PMID: 3458832
15. Churchill DR, Morris C, Fakoya A, Wright SG, Davidson RN (1996) Clinical and laboratory features of
patients with loiasis (Loa loa filariasis) in the U.K. J Infect 33: 103–109. PMID: 8889997
16. Gantois N, Rapp C, Gautret P, Ficko C, Savini H, et al. (2013) Imported loiasis in France: a retrospective
analysis of 47 cases. Travel Med Infect Dis 11: 366–373. https://doi.org/10.1016/j.tmaid.2013.08.005
PMID: 24035648
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 10 / 11
Different regimens for the treatment of loiasis
17. Antinori S, Schifanella L, Million M, Galimberti L, Ferraris L, et al. (2012) Imported Loa loa filariasis:
three cases and a review of cases reported in non-endemic countries in the past 25 years. Int J Infect
Dis 16: e649–662. https://doi.org/10.1016/j.ijid.2012.05.1023 PMID: 22784545
18. Gobbi F, Postiglione C, Angheben A, Marocco S, Monteiro G, et al. (2014) Imported loiasis in Italy: an
analysis of 100 cases. Travel Med Infect Dis 12: 713–717. https://doi.org/10.1016/j.tmaid.2014.07.004
PMID: 25131142
19. Saito M, Armstrong M, Boadi S, Lowe P, Chiodini PL, et al. (2015) Clinical Features of Imported Loiasis:
A Case Series from the Hospital for Tropical Diseases, London. Am J Trop Med Hyg 93: 607–611.
https://doi.org/10.4269/ajtmh.15-0214 PMID: 26101271
PLOS Neglected Tropical Diseases | https://doi.org/10.1371/journal.pntd.0006917 November 1, 2018 11 / 11
You might also like
- Sociological Odyssey Contemporary Readings in Introductory Sociology 4th Edition Adler Test BankDocument142 pagesSociological Odyssey Contemporary Readings in Introductory Sociology 4th Edition Adler Test BankAlexandraMaldonadotzcgn100% (14)
- Guest Speaker Lesson PlanDocument2 pagesGuest Speaker Lesson PlanKelley Thompson NeumannNo ratings yet
- Haze and Luminous Transmittance of Transparent Plastics: Standard Test Method ForDocument7 pagesHaze and Luminous Transmittance of Transparent Plastics: Standard Test Method ForFernando Da RosNo ratings yet
- Drama ScriptDocument3 pagesDrama ScriptDiana Zaibi57% (7)
- Legionnaires' DiseaseDocument14 pagesLegionnaires' Diseaselakshminivas PingaliNo ratings yet
- The Global Distribution and Transmission Limits of Lymphatic Filariasis: Past and PresentDocument20 pagesThe Global Distribution and Transmission Limits of Lymphatic Filariasis: Past and PresentNanda AzzahraNo ratings yet
- European Consensus Statement On Leptospirosis in Dogs and CatsDocument21 pagesEuropean Consensus Statement On Leptospirosis in Dogs and Catsnashfitriyah hidayatNo ratings yet
- LEPTOSPIROSIS ReviewDocument10 pagesLEPTOSPIROSIS ReviewwaktoleNo ratings yet
- Jurnal Kel. 2 FilariasisDocument9 pagesJurnal Kel. 2 FilariasisEka Saptaria NusantiNo ratings yet
- Immunomodulatory Therapy For The Management of Loiasis PDFDocument5 pagesImmunomodulatory Therapy For The Management of Loiasis PDFLucchéri Ndong AkomezogheNo ratings yet
- Covid19 PDFDocument6 pagesCovid19 PDFJeremy Kartika SoeryonoNo ratings yet
- Loa Loa-Does It Deserve To Be NeglectedDocument5 pagesLoa Loa-Does It Deserve To Be NeglectedLucchéri Ndong AkomezogheNo ratings yet
- Naegleria ReviewDocument61 pagesNaegleria ReviewKʀɪsʜɴᴀ ϟNo ratings yet
- Universa MedicaDocument11 pagesUniversa Medicarido eledNo ratings yet
- A Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in Nigeria: Kabuga and El ZowalatyDocument9 pagesA Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in Nigeria: Kabuga and El ZowalatyNers LollipopNo ratings yet
- Clinical Epidemiological and Spatial Features of HDocument15 pagesClinical Epidemiological and Spatial Features of HNealNo ratings yet
- Original ArticleDocument11 pagesOriginal ArticleLisamoni 786No ratings yet
- 1 s2.0 S1201971214015732 MainDocument18 pages1 s2.0 S1201971214015732 MainMichael JonesNo ratings yet
- Positive Francisella Tularensis Meningitis Outcome Despite Delayed Identification A Case ReportDocument5 pagesPositive Francisella Tularensis Meningitis Outcome Despite Delayed Identification A Case Reportd4rkgr455No ratings yet
- Reservoirs and Transmission Routes of Leprosy A SyDocument27 pagesReservoirs and Transmission Routes of Leprosy A SyPUSPA RUSUNAWANo ratings yet
- Lymphatic Filariasis PDFDocument12 pagesLymphatic Filariasis PDFBai Marifah LucasNo ratings yet
- Epidemiology of Elephantiasis With Special Emphasis On Podoconiosis Inethiopia: A Literature ReviewDocument6 pagesEpidemiology of Elephantiasis With Special Emphasis On Podoconiosis Inethiopia: A Literature ReviewSneha VaishnavNo ratings yet
- Faggionvinholo2020 Q1Document5 pagesFaggionvinholo2020 Q1NasriNo ratings yet
- MH 2 PDFDocument13 pagesMH 2 PDFNurul FajriNo ratings yet
- Pone. EbolaDocument12 pagesPone. EbolaJuan MoralesNo ratings yet
- LeptospirosisDocument14 pagesLeptospirosisClement ThansNo ratings yet
- Malaria Vs DBDDocument9 pagesMalaria Vs DBDade hajizah br ritongaNo ratings yet
- Najam 2021Document15 pagesNajam 2021Evelin YanaNo ratings yet
- Insecticide ResistanceDocument3 pagesInsecticide ResistanceGenniNo ratings yet
- A Five-Year Survey of Dematiaceous Fungi in A Tropical Hospital.Document11 pagesA Five-Year Survey of Dematiaceous Fungi in A Tropical Hospital.Anonymous argZ1ZNo ratings yet
- Journal of Pulmonary & Respiratory MedicineDocument5 pagesJournal of Pulmonary & Respiratory Medicinetitan dheaNo ratings yet
- pntd.0005941 BOMDocument16 pagespntd.0005941 BOMhenriquesbimbeNo ratings yet
- A Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in NigeriaDocument9 pagesA Review of The Monkeypox Virus and A Recent Outbreak of Skin Rash Disease in NigeriaNadia Desanti RachmatikaNo ratings yet
- Laboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFDocument7 pagesLaboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFLucchéri Ndong AkomezogheNo ratings yet
- DNA Based Mothods For Diognosis of LFDocument10 pagesDNA Based Mothods For Diognosis of LFsenathilakenhks7068No ratings yet
- Journal PNTD 0010076Document19 pagesJournal PNTD 0010076yves.cosnuauNo ratings yet
- RRTM 12 153Document20 pagesRRTM 12 153pramitpatelphotographyNo ratings yet
- Jir 409Document10 pagesJir 409utkarsh PromotiomNo ratings yet
- John 2003Document8 pagesJohn 2003Ibtissam BelehssenNo ratings yet
- 62 Greenwood JCI 08Document11 pages62 Greenwood JCI 08Verlyanita SeptiariniNo ratings yet
- Natural Products As Soruce of Dengue AntiviralsDocument26 pagesNatural Products As Soruce of Dengue AntiviralsKaren SánchezNo ratings yet
- Complex Epidemiology of A Zoonotic Disease in A Culturally Diverse Region: Phylogeography of Rabies Virus in The Middle EastDocument17 pagesComplex Epidemiology of A Zoonotic Disease in A Culturally Diverse Region: Phylogeography of Rabies Virus in The Middle Eastwulan sitorusNo ratings yet
- Pone 0169324Document17 pagesPone 0169324data lmleNo ratings yet
- In Tech OpenDocument16 pagesIn Tech OpenZeo LeoNo ratings yet
- Epidemiology of Visceral LeishmaniasisDocument9 pagesEpidemiology of Visceral LeishmaniasismclimacoNo ratings yet
- A Century of Clinical Use of Phages A Literature RDocument23 pagesA Century of Clinical Use of Phages A Literature RIsidora NikolicNo ratings yet
- The Management of Patients With Severe Malaria: AbstractDocument7 pagesThe Management of Patients With Severe Malaria: AbstractHervi LaksariNo ratings yet
- Viruses 11 00018Document21 pagesViruses 11 00018ismah ibtihaNo ratings yet
- Time For A Farewell To Soap in The Eye?Document4 pagesTime For A Farewell To Soap in The Eye?yazzNo ratings yet
- A Systematic Review On Leptospirosis in Cattle A European PerspectiveDocument11 pagesA Systematic Review On Leptospirosis in Cattle A European PerspectiveTORRES GUTIERREZ JOYNY RAQUEL catedraticoNo ratings yet
- Current Status of Leprosy: Epidemiology, Basic Science and Clinical PerspectivesDocument9 pagesCurrent Status of Leprosy: Epidemiology, Basic Science and Clinical PerspectivesYolan Sentika NovaldiNo ratings yet
- World Allergy OrganizationDocument25 pagesWorld Allergy OrganizationHusnul HanifaNo ratings yet
- Pone 0285900Document11 pagesPone 0285900Walter Huamani AlvitesNo ratings yet
- Ebola - Virus - Disease - DINA01-dikonversiDocument13 pagesEbola - Virus - Disease - DINA01-dikonversidina amalikaNo ratings yet
- The Clinical and Immunological Features of Leprosy: S. L. Walker and D. N. J. LockwoodDocument19 pagesThe Clinical and Immunological Features of Leprosy: S. L. Walker and D. N. J. LockwoodMariana MarquesNo ratings yet
- Adult Interstitial Lung Diseases and Their Epidemiology 2019Document46 pagesAdult Interstitial Lung Diseases and Their Epidemiology 2019Mary CogolloNo ratings yet
- Antimalarial Drug Mefloquine Is A Possible CureDocument8 pagesAntimalarial Drug Mefloquine Is A Possible Curehuma javeriaNo ratings yet
- Filaria TerbaruDocument6 pagesFilaria TerbaruAbdul GhofurNo ratings yet
- Pathogenesis and PathologyDocument12 pagesPathogenesis and Pathologydies100% (1)
- LeprosyDocument3 pagesLeprosyNadim DinaniNo ratings yet
- Tropical Fevers: C. Important Human Parasitic Fevers of The TropicsDocument25 pagesTropical Fevers: C. Important Human Parasitic Fevers of The TropicsMohammad Jofa Rachman PNo ratings yet
- Childhood Leptospirosis in An Industrialized Country: Population-Based Study in Okinawa, JapanDocument10 pagesChildhood Leptospirosis in An Industrialized Country: Population-Based Study in Okinawa, JapansabrinaNo ratings yet
- Ebola Virus Disease: A Manual for EVD ManagementFrom EverandEbola Virus Disease: A Manual for EVD ManagementMarta LadoNo ratings yet
- IL-10 and Its Related Superfamily Members IL-19 and IL-24 Provide Parallel Redundant Immune-Modulation in Loa Loa Infection PDFDocument9 pagesIL-10 and Its Related Superfamily Members IL-19 and IL-24 Provide Parallel Redundant Immune-Modulation in Loa Loa Infection PDFLucchéri Ndong AkomezogheNo ratings yet
- Laboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFDocument7 pagesLaboratory Parameters After Treatment For Loa Loa and Mansonella Perstans The Experience of A Single Referral Center For Tropical Diseases in A Non-Endemic Area PDFLucchéri Ndong AkomezogheNo ratings yet
- Ivermectin Inhibits Extracellular Vesicle Secretion From Parasitic Nematodes PDFDocument15 pagesIvermectin Inhibits Extracellular Vesicle Secretion From Parasitic Nematodes PDFLucchéri Ndong AkomezogheNo ratings yet
- Human Loiasis in A Cameroonian Village A Double-Blind, Placebo-Controlled, Crossover Clinical Trial of Athree-Day Albendazole RegimenDocument5 pagesHuman Loiasis in A Cameroonian Village A Double-Blind, Placebo-Controlled, Crossover Clinical Trial of Athree-Day Albendazole RegimenLucchéri Ndong AkomezogheNo ratings yet
- Immunomodulatory Therapy For The Management of Loiasis PDFDocument5 pagesImmunomodulatory Therapy For The Management of Loiasis PDFLucchéri Ndong AkomezogheNo ratings yet
- Albendazole-Related Loa Loa EncephalopathyDocument2 pagesAlbendazole-Related Loa Loa EncephalopathyLucchéri Ndong AkomezogheNo ratings yet
- Loa Loa-Does It Deserve To Be NeglectedDocument5 pagesLoa Loa-Does It Deserve To Be NeglectedLucchéri Ndong AkomezogheNo ratings yet
- The Population Biology and Transmission Dynamics of Loa Loa: ReviewDocument16 pagesThe Population Biology and Transmission Dynamics of Loa Loa: ReviewLucchéri Ndong AkomezogheNo ratings yet
- Cause and Effect EssayDocument2 pagesCause and Effect EssayRida ShakilNo ratings yet
- BJT PDFDocument14 pagesBJT PDFRaka Satria PradanaNo ratings yet
- Examination Pattern - Docx MAPC 1 Cognitive Psychology, Learning and MemoryDocument8 pagesExamination Pattern - Docx MAPC 1 Cognitive Psychology, Learning and MemoryakileshaiyerNo ratings yet
- Job Description For Hse AdvisorDocument2 pagesJob Description For Hse AdvisorSam JoseNo ratings yet
- Lecture Notes: Manila Cavite Laguna Cebu Cagayan de Oro DavaoDocument5 pagesLecture Notes: Manila Cavite Laguna Cebu Cagayan de Oro DavaoDenny June CraususNo ratings yet
- Intensive Care NursesDocument15 pagesIntensive Care NursesUlysses GamayonNo ratings yet
- Sara Ahmed - Happiness and Queer PoliticsDocument20 pagesSara Ahmed - Happiness and Queer Politicsferwerdasma100% (1)
- Test Unit 1: Listening Answer KeyDocument2 pagesTest Unit 1: Listening Answer KeyLaty86No ratings yet
- 4Ms of Production ManagementDocument84 pages4Ms of Production ManagementVincent L. SantiagoNo ratings yet
- For Tuesday, Mar 21 : Venture Capital Problem SetDocument3 pagesFor Tuesday, Mar 21 : Venture Capital Problem SetJerry Chang0% (1)
- In Loco Parentis or As Substitute Parents, As Expressly Provided UnderDocument4 pagesIn Loco Parentis or As Substitute Parents, As Expressly Provided UnderGESELLEENDICO06No ratings yet
- Millimeter Wave Therapy-Disease and PointsDocument31 pagesMillimeter Wave Therapy-Disease and Pointsalfredo.bioxinNo ratings yet
- Six-Sided SagasDocument14 pagesSix-Sided SagasJames Hargrove50% (2)
- Leadership and Management ProjectDocument12 pagesLeadership and Management Projectshian ramdialNo ratings yet
- Bioprogressive Therapy As An AnswerDocument39 pagesBioprogressive Therapy As An Answerelenaelena2011No ratings yet
- The Kelingai Motif' in Iban's Tattoo Motif A Case Study of Kampung Gayau Ulu Pantu, Sri Aman SarawakDocument10 pagesThe Kelingai Motif' in Iban's Tattoo Motif A Case Study of Kampung Gayau Ulu Pantu, Sri Aman SarawaktimartiNo ratings yet
- Managing Markets Strategically: Professor Noel CaponDocument53 pagesManaging Markets Strategically: Professor Noel CaponMoidin AfsanNo ratings yet
- Homophobic Transphobic Bullying Pe Focus1Document2 pagesHomophobic Transphobic Bullying Pe Focus1api-440470277No ratings yet
- Social StructureDocument11 pagesSocial StructureabbiecdefgNo ratings yet
- Match Fixing by Judges & PoliceDocument193 pagesMatch Fixing by Judges & PoliceNagaraja Mysuru RaghupathiNo ratings yet
- Action Plan in MathDocument4 pagesAction Plan in Mathjoanna marie limNo ratings yet
- Rmullinsresume 2019Document2 pagesRmullinsresume 2019api-448247344No ratings yet
- 1 Mirrors PDFDocument30 pages1 Mirrors PDFKevin MaylowNo ratings yet
- Liste Jeux PS Vita Boites PALDocument1 pageListe Jeux PS Vita Boites PALDenis Alibor MajhenNo ratings yet
- MRP Report Chapterwise - 2 PDFDocument95 pagesMRP Report Chapterwise - 2 PDFAfnanParkerNo ratings yet
- LAW - ON - SALES CH 4 Sec 3Document4 pagesLAW - ON - SALES CH 4 Sec 3MaricrisNo ratings yet