Professional Documents
Culture Documents
HYPERTHYROIDISM
HYPERTHYROIDISM
Uploaded by
Philip Gene II MalacasOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
HYPERTHYROIDISM
HYPERTHYROIDISM
Uploaded by
Philip Gene II MalacasCopyright:
Available Formats
THE CLIENT WITH ENDOCRINE HEALTH PROBLEMS THYROID GLAND DISORDER
HYPERTHYROIDISM
(GRAVE’S DISEASE or THYROTOXICOSIS)
Data Base
A. General information: Etiology and Pathophysiology
1. Excessive concentration of thyroid hormones in the blood as a result of thyroid disease or increased TSH; leads to
hypermetabolic state
2. Etiology of Grave’s disease is mediated by immunoglobulin G (IgG) antibody that activates TSH receptors on the surface of
the thyroid cells
3. Etiology of Grave’s disease is unknown but may also believed to be involved with an autoimmune process of impaired
regulation; associated with to other autoimmune disorders
4. The gland may also enlarge (goiter) as a result of decreased iodine intake; no increase in secretion of thyroid is present
5. Most seen in women between ages 30-50 years of age
B. Clinical findings
1. Subjective: polyphagia; emotional liability; apprehension; heat intolerance
2. Objective
a. Weight loss despite of appetite and adequate caloric intake; loose stools; tremors, hyperactive reflexes; diaphoresis;
diarrhea; insomnia; exophthalmos (protrusion of the eyeballs), corneal ulceration; increased systolic blood pressure,
temperature, pulse, and respiration; warm, smooth skin; fine, soft hair; pliable nails, hypertension and tachycardia; mood
problem (irritability)
b. In women, there are changes in the menstrual interval, diminished menstrual flow (oligomenorrhea), or even the absence
of menstruation (amenorrhea) may result from hormonal imbalances of thyrotoxicosis
c. Decreased libido and impotence in men are common features of thyrotoxicosis
d. Decreased TSH levels if thyroid disorder; increased TSH levels if secondary to a pituitary disorder
e. Grave’s disease generally involves hyperthyroidism, goiter, and exophthalmos
f. Thyrotoxic crisis (thyroid storm): a state of hypermetabolism (raising the pulse and temperature) that may lead to heart
failure; usually precipitated by a period of severe physiologic or psychologic stress, thyroid surgery, or radioactive
iodine therapy
3. Diagnostic tests
a. Blood chemistry shows increased serum triiodothyronine (T 3), thyroxine (T4), free T4 levels, protein-bound iodine (PBI);
Long-acting thyroid simulator (LATS), elevated serum concentrations of thyroid hormones and suppressed serum TSH.
b. Radioactive iodine uptake is increased
c. Thyroid scan shows nodules
C. Medical management
1. Drug therapy
a. Antithyroid drugs (Propylthiouracil [PTU] and Methimazole [Tapazole]): block synthesis of thyroid hormone; toxic
effects include agranulocytosis and leucopenia which usually occur within the 3 months of treatment; the client should
be taught to promptly report to the health care provider any signs and symptoms of infection, such as a sore throat and
fever; any client complaining of a sore throat and fever should have an immediate white blood cell (WBC) count and
differential performed, and the drug must be held until the results are obtained
b. Adrenergic blocking agents (commonly propanolol [Inderal]): used to decrease sympathetic activity and alleviate
symptoms such as tachycardia
2. Radioactive iodine (RAI) therapy
a. Radioactive isotope of iodine (e.g., in the form of sodium iodide 131I) given to destroy the thyroid gland, thereby
decreasing production of thyroid hormone; the patient should remain in the outpatient department for about 2 hours to be
monitored for vomiting
b. Used in middle-aged or older clients who are resistant to, or develop toxicity from, drug therapy
c. Permanent hypothyroidism is a potential major complication. At that time, the client will need to be able to recognize
symptoms hypothyroidism, not hyperthyroidism
d. The clients need to be educated about the need for lifelong thyroid hormone replacement; lifelong medical follow-up and
thyroid replacement are warranted
e. The client does not need to be immobilized after RAI treatment
3. Surgery: thyroidectomy performed in younger clients for whom drug therapy has not been effective
D. Treatment
1. High-protein, high-carbohydrate, high-calorie diet, restricting stimulants, such as coffee and caffeine
2. Radiation therapy
3. Thyroidectomy
E. Therapeutic intervention
1. Antithyroid medications such as prophylthiouracil (PTU) and methimazole (Tapazole) to block the synthesis of thyroid
hormone
HTTP://WWW.SMCIC.EDU.PH 1 ST. MICHAEL’S COLLEGE, INC. – ILIGAN CITY
THE CLIENT WITH ENDOCRINE HEALTH PROBLEMS THYROID GLAND DISORDER
2. Antithyroid medications such as iodine (saturated solution of potassium iodide, SSKI) to reduce the Vascularity of the
thyroid gland; frequently prescribed preoperatively for the client; should be diluted well in milk, water, juice, or a carbonated
beverage before administration to help disguise the strong, bitter taste. Also, this drug is irritating to mucosa if taken
undiluted. The client should sip the diluted preparation through a drinking straw to help prevent staining of the teeth.
3. Radioactive iodine 131I to destroy thyroid gland cells, thereby decreasing the production of thyroid hormone (atomic cocktail)
4. Medications to relieve the symptoms related to the increased metabolic rate such as adrenergic blocking agents
5. Well-balanced, high-calorie diet with vitamin and mineral supplements
6. Surgical intervention involves a subtotal or total thyroidectomy
Nursing Care of Clients with Hyperthyroidism
A. ASSESSMENT
1. History of weight loss, diarrhea, insomnia, emotional lability, palpitations, and heat intolerance
2. Eyes for exophthalmos, tearing, and sensitivity to light
3. Neck palpation for enlarged thyroid gland
4. Weight and vital signs to establish baseline
B. ANALYSIS/NURSING DIAGNOSES
1. Ineffective coping related to emotional lability
2. Risk for Ineffective Therapeutic Regimen Management R/T lack of knowledge about disease
3. Imbalanced nutrition: less than body requirements related to increased metabolic needs
C. PLANNING/IMPLEMENTATION
1. Monitor vital signs, daily weights
2. Use measure such as decreased stimulation, medications, and back rub to establish a climate for uninterrupted rest
3. Protect the client from stress-producing situations
4. Keep the room cool
5. DIET: Provide foods high in calories, proteins, and carbohydrates with supplemental feedings between meals and at bedtime;
vitamin and mineral supplements should be given as prescribed; avoid beverages containing caffeine, which may increase
thyroid activity; high-fiber foods should be avoided as it increases peristalsis
6. Understand that the client is upset by lability of mood and exaggerated response to environmental stimuli; take time to
explain disease process involved
7. Provide eye drops or patches as needed; teach the client to prevent corneal irritation from mild exophthalmos by wearing
dark-colored glasses; treatment of ophthalmopathy should be performed in consultation with an ophthalmologist
8. Care for the client before a thyroidectomy
a. Administer prescribed antithyroid medications to achieve euthyroid state
b. Teach deep breathing exercises and use of hands to support neck and to avoid strain ion suture line
9. Care for the client following a thyroidectomy
a. Observe for signs of respiratory distress and laryngeal stridor caused by tracheal edema (keep tracheotomy set available)
b. Provide humidity with cold steam nebulizer to keep secretions moist when at home
c. Keep the bed in a semi-Fowler’s position
d. Observe dressings at the operative site and back of the neck and shoulders for signs of hemorrhage
e. Observe for signs of thyroid storm such as high fever, tachycardia, irritability, delirium, coma; may result from
manipulation of the gland during surgery, which releases thyroid hormone into bloodstream
f. Notify the physician immediately if signs of thyroid storm occur; administer propanolol (Inderal), iodides,
propylthiouracil, and steroids as ordered
g. Observe for signs of tetany such as numbness or twitching of extremities, spasm of the glottis;
h. Hypocalcemia can occur after accidental trauma or removal of the parathyroid glands; if tetany occurs, give calcium
gluconate or calcium chloride (IV) as prescribed
i. Assess for hoarseness; may result from endotracheal intubation or laryngeal nerve damage; laryngeal nerve damage is a
potential complication of thyroid surgery because of the proximity of the thyroid gland to the recurrent laryngeal nerve.
Asking the client to speak helps assess for signs of laryngeal nerve damage; persistent or worsening hoarseness and
weak voice are signs of laryngeal nerve damage and should be reported to the physician immediately; laryngeal nerve
damage can result in vocal cord spasm and respiratory obstruction
10. Provide teaching regarding radioactive iodine therapy
a. Following therapy client returns to the community
b. Hospitalization in isolation may be required for several days if larger doses are used
c. Symptoms of hyperthyroidism may take 3 to 4 weeks to subside
11. Teach client signs and symptoms of:
a. Hypothyroidism as a result of treatment
b. Hyperthyroidism as a result of thyroid storm or overmedication with thyroid hormone replacement therapy
12. Teach the importance of taking antithyroid medications regularly and to observe for adverse effects.
D. EVALUATION/OUTCOMES
1. The client’s weight and vital signs are within normal limits
2. The client verbalizes understanding and follows the recommended treatment
3. Establishes regular routine of activity and rest
HTTP://WWW.SMCIC.EDU.PH 2 ST. MICHAEL’S COLLEGE, INC. – ILIGAN CITY
You might also like
- A Practical Guide To Chemical Peels, Microdermabrasion and TopicalDocument230 pagesA Practical Guide To Chemical Peels, Microdermabrasion and TopicalApple Blue100% (3)
- Graves DiseaseDocument35 pagesGraves DiseaseMarianGadugdug75% (4)
- Therapeutic CommunicationDocument3 pagesTherapeutic CommunicationPhilip Gene II Malacas100% (1)
- Hashimoto ThyroiditisDocument6 pagesHashimoto Thyroiditismananginsiang100% (1)
- RNSG 1533 Raising The Bar For Success Concept: Metabolism: Diabetes Type 1/diabetes Type 2Document4 pagesRNSG 1533 Raising The Bar For Success Concept: Metabolism: Diabetes Type 1/diabetes Type 2katrinasdNo ratings yet
- Case 1 EndocrineDocument5 pagesCase 1 EndocrineRegine Mae EncinadaNo ratings yet
- Physiology Behind Contraceptive MethodsDocument26 pagesPhysiology Behind Contraceptive Methodsnirilib100% (2)
- KMB II Sistem Endokrin PT IIDocument68 pagesKMB II Sistem Endokrin PT IIAngel ChrisNo ratings yet
- 20 Items QaDocument19 pages20 Items QaRegiever SalvanteNo ratings yet
- Child With EndocrineDocument4 pagesChild With EndocrineSanthosh.S.UNo ratings yet
- N245 Endocrine PPT NotesDocument9 pagesN245 Endocrine PPT NotesAANo ratings yet
- Resume Hyperthyroidism And: Diabetic KetoacidosisDocument9 pagesResume Hyperthyroidism And: Diabetic KetoacidosisYopy OctavianaNo ratings yet
- Review Ped SobDocument44 pagesReview Ped SobRandyNo ratings yet
- Disorders of The Thyroid and Parathyroid Glands: Ms TeamDocument36 pagesDisorders of The Thyroid and Parathyroid Glands: Ms TeamShy Dela PuertaNo ratings yet
- Thyroid ParathyroidDocument79 pagesThyroid Parathyroid2M SANCHEZ, CYLESNo ratings yet
- Competency Appraisal 1 Disturbance in Metabolism EndocrineDocument46 pagesCompetency Appraisal 1 Disturbance in Metabolism EndocrineJohn Paul M. TagapanNo ratings yet
- Thyroid StormDocument1 pageThyroid StormPhilip Gene II MalacasNo ratings yet
- Thyroid Emergencies: Siddharth N ShahDocument1 pageThyroid Emergencies: Siddharth N ShahSubramanian MurugesanNo ratings yet
- HyperthyroidismDocument4 pagesHyperthyroidismavinash dhameriyaNo ratings yet
- Endocrine Disorders - NotesDocument8 pagesEndocrine Disorders - NotesLLLJJJNo ratings yet
- Endocrine System Prepared By: Prof. Mike Chavez RN, USRNDocument7 pagesEndocrine System Prepared By: Prof. Mike Chavez RN, USRNMeiJoyFlamianoIINo ratings yet
- A. Brief Definition of The Specific Disease Condition: Mechanism CauseDocument6 pagesA. Brief Definition of The Specific Disease Condition: Mechanism CauseEuniceNo ratings yet
- Hesi RN Med Surg 2020 Study Guide Review and Test BankDocument5 pagesHesi RN Med Surg 2020 Study Guide Review and Test BankJoseph Post100% (33)
- Hormonal RegulationDocument20 pagesHormonal Regulationel shilohNo ratings yet
- Thyroid StormDocument4 pagesThyroid Stormbhaskaracharya dontabhaktuniNo ratings yet
- Hyperthyroidism: Sudiarto, MNDocument21 pagesHyperthyroidism: Sudiarto, MNerikaNo ratings yet
- Radioactive Iodine Therapy (Rai) : GoalsDocument6 pagesRadioactive Iodine Therapy (Rai) : GoalsFirras SalsabilaNo ratings yet
- Thyroid Storm and Hyperthyroidism - CorePendiumDocument17 pagesThyroid Storm and Hyperthyroidism - CorePendiumSajeewanieNo ratings yet
- Specific Disorders of The Thyroid GlandDocument8 pagesSpecific Disorders of The Thyroid Glandgiselle chloeNo ratings yet
- Legend - Answer - Rationale Hypothyroidism Vs Hyperthyroidism NCLEX QuizDocument8 pagesLegend - Answer - Rationale Hypothyroidism Vs Hyperthyroidism NCLEX QuizSherilNo ratings yet
- Endocrine MedicationsDocument13 pagesEndocrine MedicationsAlexis de los Santos100% (1)
- Common Autoimmune Disorders and Its Nursing InterventionsDocument7 pagesCommon Autoimmune Disorders and Its Nursing InterventionsIan Mizzel A. DulfinaNo ratings yet
- Chapter 128 - Thyroid and Adrenal Disorders: Episode OverviewDocument15 pagesChapter 128 - Thyroid and Adrenal Disorders: Episode OverviewIkenna EzeiloNo ratings yet
- Thyroid Disease Anesthetic ConsiderationsDocument30 pagesThyroid Disease Anesthetic Considerationssachin10dulkarNo ratings yet
- Pituitary &thyroid NotesDocument7 pagesPituitary &thyroid NotesAli salimNo ratings yet
- U World Endocrine FinalDocument12 pagesU World Endocrine Finalsean blazeNo ratings yet
- HYPOTHYROIDISMDocument2 pagesHYPOTHYROIDISMPhilip Gene II MalacasNo ratings yet
- Hyperthyroidism, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHyperthyroidism, A Simple Guide To The Condition, Treatment And Related ConditionsRating: 2 out of 5 stars2/5 (2)
- LO&WO - Endokrin.week4 (Michael G)Document6 pagesLO&WO - Endokrin.week4 (Michael G)Michael GNo ratings yet
- Thyroid CrisisDocument34 pagesThyroid CrisisRidyah Ning TyasNo ratings yet
- Endocrine: Common Lab Tests For Endocrine and Hormonal DisordersDocument19 pagesEndocrine: Common Lab Tests For Endocrine and Hormonal DisordersPhilip SimanganNo ratings yet
- Ms-Endocrine Sample QuestionsDocument28 pagesMs-Endocrine Sample QuestionsDanica Alan QuemanNo ratings yet
- ESSAYDocument2 pagesESSAYBokNo ratings yet
- Endocrine NursingDocument8 pagesEndocrine NursingBunny Bonny100% (5)
- HypothyroidismDocument26 pagesHypothyroidismSirpa MhrznNo ratings yet
- Lect 5Document26 pagesLect 5eslambasuony98No ratings yet
- Drug Use DisorderDocument10 pagesDrug Use Disordergeng gengNo ratings yet
- Thyroid Colloid Nodular GoiterDocument23 pagesThyroid Colloid Nodular Goitervahn025No ratings yet
- HyperthyroidismDocument73 pagesHyperthyroidismZNEROL100% (1)
- HypothyroidismDocument7 pagesHypothyroidismavinash dhameriyaNo ratings yet
- Kuliah HyperthyroidDocument18 pagesKuliah HyperthyroidFreddyNo ratings yet
- Hesi Study GuidDocument44 pagesHesi Study GuidJazzmyne T.No ratings yet
- Management of Thyroid Emergencies: Sunita Tarsarya SonavaneDocument2 pagesManagement of Thyroid Emergencies: Sunita Tarsarya Sonavanekevok7No ratings yet
- 1 PDFDocument8 pages1 PDFDianne NuñalNo ratings yet
- Thyrotoxicosis: By: DR Mukesh Kumar Samota PG (M.D. Medicine) Medical College Jhalawar (RajasthanDocument40 pagesThyrotoxicosis: By: DR Mukesh Kumar Samota PG (M.D. Medicine) Medical College Jhalawar (RajasthanShravani ShagapuramNo ratings yet
- Pathophysiology of HyperthyroidismDocument97 pagesPathophysiology of HyperthyroidismMarie Joyce SablanNo ratings yet
- Endocrine SystemDocument59 pagesEndocrine Systemayesharajput5110No ratings yet
- Thyroid and Parathyroid GlandsDocument133 pagesThyroid and Parathyroid GlandsmunafalmahdiNo ratings yet
- Activity 1Document2 pagesActivity 1Jan Cyrel ColomaNo ratings yet
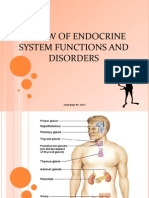
- Review of Endocrine System Functions and Disorders: Arnel Ipapo RN, MANDocument51 pagesReview of Endocrine System Functions and Disorders: Arnel Ipapo RN, MANcha_cha_magistradoNo ratings yet
- Causes of Hyperthyroidism2Document73 pagesCauses of Hyperthyroidism2Kompari EvansNo ratings yet
- Thyroid Diet: How to Improve Thyroid Disorders, Manage Thyroid Symptoms, Lose Weight, and Improve Your Metabolism through Diet!From EverandThyroid Diet: How to Improve Thyroid Disorders, Manage Thyroid Symptoms, Lose Weight, and Improve Your Metabolism through Diet!No ratings yet
- HYPOTHYROIDISMDocument2 pagesHYPOTHYROIDISMPhilip Gene II MalacasNo ratings yet
- Specific Disorders of The PancreasDocument6 pagesSpecific Disorders of The PancreasPhilip Gene II MalacasNo ratings yet
- Thyroid ProblemDocument8 pagesThyroid ProblemPhilip Gene II MalacasNo ratings yet
- The Endocrine System (Instructor Guide)Document8 pagesThe Endocrine System (Instructor Guide)Philip Gene II MalacasNo ratings yet
- ThyroidectomyDocument1 pageThyroidectomyPhilip Gene II MalacasNo ratings yet
- HYPOPITUITARISMDocument1 pageHYPOPITUITARISMPhilip Gene II MalacasNo ratings yet
- Thyroid StormDocument1 pageThyroid StormPhilip Gene II MalacasNo ratings yet
- HYPERPARATHYROIDISMDocument1 pageHYPERPARATHYROIDISMPhilip Gene II MalacasNo ratings yet
- HYPOPHYSECTOMYDocument1 pageHYPOPHYSECTOMYPhilip Gene II MalacasNo ratings yet
- HYPERPITUITARISMDocument1 pageHYPERPITUITARISMPhilip Gene II MalacasNo ratings yet
- HYPOPARATHYROIDISMDocument1 pageHYPOPARATHYROIDISMPhilip Gene II MalacasNo ratings yet
- Cushing's SyndromeDocument2 pagesCushing's SyndromePhilip Gene II MalacasNo ratings yet
- CONNDocument1 pageCONNPhilip Gene II MalacasNo ratings yet
- Surgical ProceduresDocument355 pagesSurgical ProceduresPhilip Gene II MalacasNo ratings yet
- CRETENISMDocument2 pagesCRETENISMPhilip Gene II MalacasNo ratings yet
- ADDISONIANDocument2 pagesADDISONIANPhilip Gene II MalacasNo ratings yet
- ADRENALECTOMYDocument1 pageADRENALECTOMYPhilip Gene II MalacasNo ratings yet
- Psych Notes FGPDocument74 pagesPsych Notes FGPPhilip Gene II MalacasNo ratings yet
- Surgical Instruments-2Document55 pagesSurgical Instruments-2Philip Gene II MalacasNo ratings yet
- PRC FormsDocument5 pagesPRC FormsPhilip Gene II MalacasNo ratings yet
- The Patient in SurgeryDocument6 pagesThe Patient in SurgeryPhilip Gene II MalacasNo ratings yet
- OncologyDocument26 pagesOncologyPhilip Gene II MalacasNo ratings yet
- Oncology TestDocument32 pagesOncology TestPhilip Gene II MalacasNo ratings yet
- Maternal & Newborn 1Document133 pagesMaternal & Newborn 1Philip Gene II MalacasNo ratings yet
- Histo - Pituitary GlandDocument22 pagesHisto - Pituitary GlandRessam Nazir100% (1)
- KB HormonalDocument8 pagesKB Hormonalf4rh4t1No ratings yet
- Endometriosis: Aetiology, Pathogenesis and TreatmentDocument16 pagesEndometriosis: Aetiology, Pathogenesis and Treatmentyuyu tuptupNo ratings yet
- Credentialing and PrivilegingDocument113 pagesCredentialing and PrivilegingRobert Montuya100% (2)
- Brands and Types of Insulin - Rapid-Acting, Long-Acting, and MoreDocument4 pagesBrands and Types of Insulin - Rapid-Acting, Long-Acting, and MoreRaul Fernando Vasquez WoddensonNo ratings yet
- ADIL BSN - 1C Manual Endocrine SystemDocument3 pagesADIL BSN - 1C Manual Endocrine Systembernadil01No ratings yet
- Quiz 9 Human Reproduction Pregnancy Menstruation GraphsDocument4 pagesQuiz 9 Human Reproduction Pregnancy Menstruation GraphsCamille FrancoNo ratings yet
- Blood Sugar Blood Pressure Log 12012017Document2 pagesBlood Sugar Blood Pressure Log 12012017Mahbub RahmanNo ratings yet
- Thyroid Gland Function in Ovariectomized Ewes Exposed To PhytoestrogensDocument7 pagesThyroid Gland Function in Ovariectomized Ewes Exposed To PhytoestrogensAhmad Daud OmNo ratings yet
- Remedial QUIZDocument2 pagesRemedial QUIZsinunuc nhsNo ratings yet
- Estrogenic Activity of Alcoholic Extract of Lemon Seeds (Citrus Limonum) On Immature Albino RatsDocument5 pagesEstrogenic Activity of Alcoholic Extract of Lemon Seeds (Citrus Limonum) On Immature Albino RatsKocyd Dyck OkooNo ratings yet
- Pex 09 04Document4 pagesPex 09 04DominiqueLovesAmaurionnaSmith33% (9)
- Diabetes Mellitus An OverviewDocument4 pagesDiabetes Mellitus An OverviewALNo ratings yet
- Mary Keeper's Aching Head: Part I-Trouble Sleeping Prompts An Urgent Doctors AppointmentDocument4 pagesMary Keeper's Aching Head: Part I-Trouble Sleeping Prompts An Urgent Doctors AppointmentJeelNo ratings yet
- DynaMed Plus - Thyroid NoduleDocument85 pagesDynaMed Plus - Thyroid NoduleGamer MadaNo ratings yet
- 11 Biology Notes ch22 Chemical Coordination and Integration PDFDocument6 pages11 Biology Notes ch22 Chemical Coordination and Integration PDFAarav VarshneyNo ratings yet
- Prof. DR. Dr. Ketut Suastika, SP - PD-KEMD - Management of Growth Hormone Deficiency in AdultDocument31 pagesProf. DR. Dr. Ketut Suastika, SP - PD-KEMD - Management of Growth Hormone Deficiency in AdultvillnachintyaNo ratings yet
- Endocrine-System Important-Qs Important-QuestionsDocument4 pagesEndocrine-System Important-Qs Important-Questionssshashvat810No ratings yet
- Primary Empty Sella A Comprehensive Review 2017Document11 pagesPrimary Empty Sella A Comprehensive Review 2017Paúl Otañez MolinaNo ratings yet
- 9th - Cystic OvariesDocument25 pages9th - Cystic Ovariesnoor aineNo ratings yet
- Congestive Heart Failure in Type 2 Diabetes: Prevalence, Incidence, and Risk FactorsDocument6 pagesCongestive Heart Failure in Type 2 Diabetes: Prevalence, Incidence, and Risk FactorsFini Riski Aulia SagalaNo ratings yet
- Preboards 2 - NP3 (Printable)Document10 pagesPreboards 2 - NP3 (Printable)Joana Marie DomingoNo ratings yet
- The Phases of Menstrual CycleDocument5 pagesThe Phases of Menstrual CycleKristine AlejandroNo ratings yet
- Activity Sheets in Science 5 Quarter 2, Week 1: Parts of The Reproductive System and Their FunctionsDocument6 pagesActivity Sheets in Science 5 Quarter 2, Week 1: Parts of The Reproductive System and Their Functionsricardo salayonNo ratings yet
- Dr. Sony - PKB3 - CKD Dan Komplikasi-FinalDocument75 pagesDr. Sony - PKB3 - CKD Dan Komplikasi-FinalIzka P RahmaniaNo ratings yet
- Tugas Remedial PaperDocument7 pagesTugas Remedial PaperFujiNo ratings yet
- Calcium MetabolismDocument28 pagesCalcium MetabolismAhmedkhaed100% (1)