Professional Documents
Culture Documents
Intro Parasitology
Intro Parasitology
Uploaded by
KaoriMarieSembrano0 ratings0% found this document useful (0 votes)
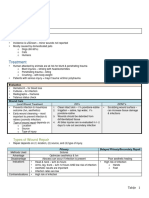
17 views4 pages1. This document provides information on parasitism, including definitions of key terms like host, vector, parasite types, and pathways of infection.
2. It describes the incubation period and clinical signs of parasitism, noting that blood pictures and symptoms can vary depending on the parasite and stage of infection.
3. Diagnosis of parasitism is discussed, including the two main methods of clinical diagnosis by a physician and laboratory examination of samples.
Original Description:
Parasitology review
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. This document provides information on parasitism, including definitions of key terms like host, vector, parasite types, and pathways of infection.
2. It describes the incubation period and clinical signs of parasitism, noting that blood pictures and symptoms can vary depending on the parasite and stage of infection.
3. Diagnosis of parasitism is discussed, including the two main methods of clinical diagnosis by a physician and laboratory examination of samples.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
0 ratings0% found this document useful (0 votes)
17 views4 pagesIntro Parasitology
Intro Parasitology
Uploaded by
KaoriMarieSembrano1. This document provides information on parasitism, including definitions of key terms like host, vector, parasite types, and pathways of infection.
2. It describes the incubation period and clinical signs of parasitism, noting that blood pictures and symptoms can vary depending on the parasite and stage of infection.
3. Diagnosis of parasitism is discussed, including the two main methods of clinical diagnosis by a physician and laboratory examination of samples.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
Download as pdf or txt
You are on page 1of 4
Parasite – can live on (Exopara) or in host (Endopara) 5. Another person’s clothing, beddings or his immediate envi. 5.
eddings or his immediate envi. 5. Open pathways for secondary invaders
Host: (pinworm → enterobiasis → egg is infective) • Ground itch – penetration of hookworm larva
A. Definite – harbors sexual stages/ mature forms of para 6. Oneself • Amoebic colitis – hole in colon → bacteria
B. Intermediate – harbors asexual/immature stages Portals of entry • Balantidiasis – ulcer
a) 1st I.H. – harbors very early larval stages 1. Mouth – protozoa exc. Plasmodium • 1st 4 – Immunocompromised for bacteria
b) 2nd I.H. – harbors late stages 2. Skin – hookworm & threadworm; direct or percutaneous (blood ❖ Oncogenic Para:
Predator – attack living; not necessarily killing them sucking; carried by I.H.) ✓ Gongylonema neoplasticum – gastric tumors
Prey – victim 3. Nose – acantamoeba, enterobius ✓ Cysticereus fasciolaris – larva of threadworm
Scavenger – devouring dead; taking leavings of predator 4. Placenta – toxoplasma, plasmodium (RBC’s para → probably in Immunity - rarely solid
HP relationship – obtain food thru close association: circulation) • Exception: Cutaneous Leishmaniasis
a. Continuous – once inside, mature inside 5. Genitalia – Trichomonas vaginalis (STD) • Trichinosis (Trichinella spirasis) – light exposure in
b. Intervals – part intermediate, part definite Incubation period animals prevent clinical infection (large amt. given)
Symbiosis – give & take; protection a. Biologic – exposure → time demonstrate para thru excretion or • Hookworm (belief)
a. Commensalism – eating at same table; beneficial to one, not secretion (ascaris – 1 month)
• Blood fluke infection (Schistosoma japonicum)
disadvantageous to one b. Clinical – exposure → manifestation of symptoms
• Condylobia (C.anthrophaga): fly maggot infestation
a) Mutualism – beneficial to both Nomenclature: Binomial Scientific Name
Clinical evidence of Parasitism:
b) Parasitism – host is injured thru para’s activities • Kingdom – Phylum – Order – Class – Family – Genus - Species
• Not pathognomonic (diagnostically specific); dependent on:
Vectors – transmit para • Threadworm – US: S. stercoralis; England: E. vermicularis
o Scientific knowledge & clinical experience
a. Biologic – essential to life cycle (plasmodium in malaria) H-P relationship:
o Acute or chronic infection
b. Mechanical / Phoretic – infection can go on w/o it (fly in a. Carrier – para present no damage to host; no symptoms,
• Blood picture: (depenends on para & patient)
Amoebiasis) damage immediately repaired
➢ No dyscrasia (manifestation) in early amoebic colitis – normal
Zoonosis – susceptibility of host to a para b. Pathogen – damage
(bleed → anemia)
a. Euzoonosis – man & reservoir host (maintain para in envi; not Pathogenesis – start / dynamics of infection; types of damage:
➢ Moderate neutrophilic leucocytosis – bacterial invasion of colonic
necessarily infectious) 1. Traumatic damage – external / internal; manifestations:
lesion in hepatic / extraintestinal amoebiasis
b. Parazoonosis – man is incidental host (dog flea) a. Slight – harmonious w/ para
➢ Monocytosis, neutropenia, erythropenia – Visceral Leishmaniasis
c. Anthropozoonosis – acquired by man from other vertebrates b. Moderate
➢ Anemia (moderate – severe) – malaria (plasmodium RBC)
(trichinosis) c. Severe – toxemia, ascaris, pinworm in appendix
➢ Polymorphonuclear leucocytosis, monocytosis, leucopenia
d. Zooanthroponosis – acquired by other vertebrates from man • Lesion – localized (manifestation at site) or generalized (diff.
(chronic) – Helminthiasis (infected w/ all roundworms)
e. Amphixenosis – man and animals areas)
➢ Hypereosinophilia (90%; normal eosinophil – 1%:
Types of para accdg. to host: • Inapparent infection – no symptoms, but infected; can be long Trematode, Stronglyoides, Visceral larval migrans, arthropod
a. Obligate – can’t exist w/o host; most infectious or short periods → not all para are excreted → low immunity ➢ Microcytic hypochromic anemia – hookworm infection
b. Facultative – free living or parasitic (Strongyloides stercoralis / → relapse → dormant remain
• Delusional Parasitosis – obsessive complusive neurosis
threadworm) 2. Lytic necrosis – para has lytic enzymes → lyse tissues &
Types of para: • Diagnosis (2 methods):
incorporate them to their cytoplasm → bloody stool
a. Amphizoic – free living amoeba – invade brain & other sites 1. Clinical – by physician
a. Plasmodium
(Genus Naegleria & Acanthamoeba) • In endemic – familiar w/ manifestations
b. E. histolytica
b. Spurious – free living para accidentally ingested; not equipped • Uncommon disease – difficult diagnosis
c. Toxoplasma gondii (reticuloendothelial cells)
to live in humans; recovered in human feces 2. Laboratory – by MT’s; one should know:
d. Trypanosoms cruzi (WBC) & Leishmania
Infection vs Infestation a. Type of specimen to be obtained for lab analysis
• Peritonitis – intestine has holes due to enzymes
└ endopara └ ectopara; external manifestation b. How & when specimen is to be obtained
• Amoebiasis
Parasitosis – state of infection & infestation • Plasmodium – at height of fever – RBC rupturing
3. Stimulation of H-Tissue reaxn.
Super infection Autoinfection • Ascaris – wait 1 month before collection
• Para stimulation – beneficial: shows symptoms
You - own source of infection • Elephantiasis (filariasis) – young forms eliminated to blood
• Cellular infiltration at para’s site (hyperplasia – flukes)
Parasitized w/ diff. types of para Pinworm at 10 pm – 2 am
• Systematic inc. in cell types, esp. those in blood
Triumberates (hoowkworm, ascaris, – Enterobius vermicularis c. Precautions to be taken
• Eosinophilia
trichiuris trichuria) - peculiarity: pregnant female d. Specimen - processed by skilled & experienced technician
• Inc. erythropoiesis (infections w/c cause RBC loss or Subkingdom or Phylum Protozoa
- migrate to perianal at nyt
destruction) (hookworm, plasmodium)
• Unicellular
• Host walls off para by fibrous encapsulation
Sources of exposure to infection: • Some free living flagellated protozoa – have green plastids –
• Amoebic granuloma – lesion by E. histolytica synthesize CHO from inorganic substances – Plant Kingdom
1. Contaminated soil & H2O – Hookworm & threadworm
o Amoeboma – tumor (Polypoid or Ulcerative)
Skin (larva) → venous circulation → right <3 → lungs • Morphology:
• Uncomplicated amoebic colitis – ONLY w/o H-T reaxn ➢ Remarkable range in size & form (Biggest: Balantidium coli)
→ rupture alveoli → bronchi → trachea → esophagus →
4. Toxic and allergic phenomena – due to venom-producing ➢ Spherical, ovoidal or bizarre
stomach (not destroyed by gastric juice) → intestine (adult
arthropods ➢ Radial symmetry, bilateral symmetry or longitudinal torsion
stage)
• Spiders & ticks – mouth ➢ Some free living – develop into colonial aggregates
2. Food containing para’s immature infective stage (80%)
3. Blood sucking insect – I.H. (filariasis & elephantism; • Scorpions, bees, wasp, ants – caudal end ➢ Common organelles:
plasmodium) • Caterpillars – base of hollow hairs 1. Nucleus – contain chromosome
4. Domestic or wild animals harboring para (flea) • Helminth larva: o Karyosome (endosome, nucleolus) – vesicular nucleus,
o Echinococcus larva cyst – allergy aggregates of nucleus surrounded by chromatin
o Ascaris - Ascarase
o Compact nucleus - ↑ chromatin, ↓ nucleoplasm • T. hominis – intestine - Short , posterior flagella don’t pass mouth
o Nuclear membrane • T. vaginalis – prostate gland & vagina - Definite body torsion, ellipsoidal, double-
o G. lamblia & D. fragilis – 2 common nuclei at trophozoite Haemosporidia , B&T flagell. – hematophagous invertebrate host wall
o Balantidium coli – 2 dissimilar nuclei 3. Factors of Encystation: B. Family: Chilomastigidae (GIT)
2. Cytoplasm a. Deficiency or overabundance of food a. Genus: Chilomastix
a. Endoplasm – around nucleus b. Excess of catabolic products 1. Chilomastix mesnili / Cercomonas intestinalis
- Dense, granular c. pH change • Diarrheic stool – troph
- Food vacuoles – contain undigested food d. Desiccation of medium • Semi-formed stool – troph & cyst
- Materials inside: e. Depletion or excess O2 supply • Formed - cyst
a) Chromatoidal bodies – stored food; f. Overpopulation a) Troph – asymmetric pyriform (safty-pin) due to spiral groove
glycogen or protein ❖ E. coli cyst wall is more resistant to E. hisolytica - 6-20 x 3-10 microns
b) Mitochondria 4. 2 types of encystment: - 1 spherical nucleus anterior, w/ central karyosome
c) Golgi apparatus a. Protective (flagellates, amoeba, ciliates) – outside host body; no - 6 minute blepharoplast anterior to nucleus → give rise
d) Microsomes morphologic change in cyst to 3 anterior free flagella (2 on each nucleus’ side, 1
e) ER b. Reproductive (amoeba, flagellates)–amoeba produce into the cytostome)
b. Ectoplasm – less granular, around endoplasm; functions: amoebiates: - See food vacuoles
✓ Locomotor apparatus • E. coli – 16; E. histolytica – 8; Amoeba – 8 b) Cyst – lemon shaped, 7-10 x 4.5-6 microns
✓ Procurement of food • Nuclei divide during cystic stage → ↑ troph. no. ff. Excystation - 1 vesicular nucleus & cytostome w/ flagella inside
✓ Food ingestion (under favorable - Nipple-like projection
✓ Respiration conditions) - Troph. Characteristics maintained
✓ Metabolic waste discharge • Contain glycogen reserves, condensed C. Family Tetramitidae (GIT)
✓ protection • Dedifferentiation of protoplasm • 3 anterior flagella w/ 4 th trailing (posterior)
3. Food vacuoles 5. Factors involved in Excystation: • Pyriform, no axostyle, anterior nucleus w/ karyosome
4. Contractile vacuoles (pulsating) a. Osmotic changes in medium a. Genus: Enteromonas
- Osmoregulators b. Enzymatic action of org. on inner surface of cyst wall 1. Enteromonas hominis / Tricercomonas intestinalis
- In Protozoa c. In parasitic – favorable pH & enzymatic action of host tissue a) Troph – 4-10 x 3-6 microns
- Not in Sarcodina & Mastigophora 6. Sexual stages in life cycle: (book) - Hyaline pear, jerky forward movement
- Not developed in Sporozoa • Ciliates – conjugation - Ovoidal nucleus (anterior), no mouth,
5. Plasma membrane - Blepharoplast in front of nucleus
• Sporozoa – alteration of sexual & asexual; Sporogony
- Amoeba – no constant shape, changes form by extending b) Cyst – 6-8 x 4-6 microns
• Coccidian
& retracting of temporary pseudopodia - 2 nuclei, one on each end (binary fission)
2 Grps of Flagellates:
- Heliozoa & Radiolaria – ectoplasm secreted nonliving - 2 nuclei after encystation
1. Atrial – intestinal/GIT, oral, genital
calcareous & siliceous shell w/c has - Ovoidal, well defined cyst wall
2. Blood & tissue flagellates
perforations where pseudopodia are projected D. F: Hexamitidae
6. Cyst wall – secreted by ectoplasm • 2 nuclei side by side
FLAGELLATES OF GIT
7. Cytostome – cell mouth • 6 or 8 flagella, paired axonemes, bilateral symmetry
Subphylum: Mastigophora
8. Cytopyge – cell anus
Class: Zoomastigophorea • 5 genera – only GL is pathogenic
If no pyge – Excretory vacuoles at aboral end
• No chromatophores – dependent on manufactured food a. Genus: Giardia
➢ Locomotion:
• Nutrition: parasitic / holozoic 1. Giardia lamblia / Cercomonas intestinalis / Lamblia intestinalis
1. Amoeba – free flowing → Pseudopodia
• 1 nucleus or neuromotor apparatus (axoneme w/ or w/o flagella) a) Troph – rounded anteriorly, pointed posteriorly
2. Flagellates – flagella → arise from kinetoplast
• Some have cytostome - Ventral: w/ sucking disc (attachment)
3. Ciliates – cilia → arise from basal granules (B. coli)
• Reproduction: longitudinal binary fission - 9.5–21 x 5-15 microns
➢ Primitive nervous system (flagellate)
- 1 pair of ovoidal nuclei, one on each side of midline
- Kinetoplast → parabasal body & blepharoplast • Life cycle: simple exc. Trypanosomes (di- or polymorphic)
w/ central karyosome
➢ Energizing part A. Family: Bodonidae (GIT & genital)
- 2 Parabasal bodies – sausage shaped, obliquely
➢ Connected w/ axoneme → intracytoplasmic • 2 flagella (1 anterior, 1 posterior)
posterior to sucking disc
portion of flagellum; motor component • Flagella arise from blepharoplast in front of anterior nucleus
- Habitat: crypts at duodenum of small intestine
Life Cycle among Protozoa a. Genus: Retortamonas – parasitic to man, harmless commensal
- 4 pairs of flagella from 4 pairs of blepharoplast:
1. Asexual – binary fission → nucleus of parent divides mitotically → 1. Retortamonas intestinalis
i. 2 bleph → 2 axonemes → lateral crossed flagella
cytoplasmic separation a) Troph – small, 4-9 x 3-4 microns; bigger nucleus
ii. Median bleph → thicker axoneme (axostyle) →
• Amoeba – no axial gradient & plane of division - Pyriform, vacuolated cytoplasm
posterior flagella
• Flagellate – along longitudinal axis - Anterior end has cleft cytostome (shallower),
iii. Bleph near sucking disc → v. short axoneme →
• Ciliate – in transverse plane - Vesicular nucleus w/ central karyosome
central / ventral flagella
• Sporozoa / Malarial parasite (plasmodium) – trophozoite - 2 minute blepharoplast w/c give rise to flagellum
iv. Lateral uncrossed flagella
→schizont → young schizont → mature schizont → inc. - Longer flagella anterior; shorter passes thru mouth
b) Cyst – double walled, football shaped, 8-12 long, 7-10 breadth
→rupture & release merozoites b) Cyst – transfer stage, non-flagellated
- Young: 2 nuclei; mature: 4 nuclei & crossed fibrils
2. Host to host transfer (troph, cyst, sexual) - Small, 4-7 x 3-4 microns
- Excystation: at duodenum, 5-30 mins.
- Pyriform, double walled, single nucleus
• E. gingivalis, D. fragilis,Trichomonas – troph; droplet sray Life Cycle:
2. Retortamonas sinensis – bigger than a) w/ smaller nucleus
• T. tenax – mouth Mature cyst
- More cavernous cytostome
↓ ingested thru food - Anterior cytostome opposite UM - Nonspecific urethritis – flagellate in 10% - 20% of subjects &
Stomach - D Female Male 20 – 30% on those who had trichomonas vaginitis
↓ unchanged rSedimented urine Urine - US – most common acquired STInfection
Duodenum oVaginal secretions Prostatic secretions - Diagnosis:
↓ excystation pVaginal scrapings ff. massage of prostate gland a) found in:
Trophozoite (binary fission) l
↓ feed and grow et spray (mouth) or use of contaminated utensils
Large intestine (dehydration of feces) - Harmless commensal
↓ encystation - Recover troph from: b)
2-nucleated cyst ✓ Tartar between teeth b) in wet films – 60% recovery
↓ ✓ Gingival margins of gums ✓ Best specimen: thru vaginal speculum (applicator stick)
4-nucleated cyst (mature) ✓ Tonsillar crypts ✓ Phase contrast microscopy – observe flagella & UM
↓ 2. Trichomonas hominis ▪ Female urethral discharge – (+) when no bacteria; if
Passed out together w/ feces - 2nd most common flagellate from GIT (cecum of L. intestine) w/ → difficult
Epidemiology: - Pyriform, 5-14 x 7-10 microns (bigger than tenax) ▪ Male - ↑ ID
- Transmission: viable cyst swallowed (H2O or food) - w/ free trailing posterior end (flagella at margin of UM) c) Culture methods – for best ID
- Intimate contact w/ infected - Semi-rigid axostyle, thick costa ✓ Modified diamond med. – 93% effective
- More prevalent in children (in large families, crowded) - Cytostomal cleft opposite UM d) Serology
- Sx max. frequency: childhood or puberty - Single ovoidal nucleus w/ conspicuous karyosome ✓ Gel Diffusion (GD)
- Higher in warm - No parabasal body ✓ Indirect Hemagglutination Test (IHA) – glycogen w/ para
- Giardasis (STD) – homosexual anal/oral sexual practices - Diarrheic stool – pseudopodial extension at side of UM as antigen; more sensitive than GD
- Contagious - Filth flies – mechanical vector (in food) ✓ Monoclonal Fluorescent Antibody (FA) – 86% of 88
Diagnosis: - Presence – indicate unnatural condition; commensal ✓ Pap smear – 56% → not so efficient
- Not pathogenic, just opportunists - Troph in fresh, unformed stools F. F. Monocercomonadidae
- Fluoroscopy – hypermotility at duodenum & jejunum 3. Trichomonas vaginalis a. Genus: Dientamoeba
- X-ray – mucuosal defects - Like tenax except: 1. Dientamoeba fragilis
- Diarrheic stool – no proper absorption – Steatorrheic stools ▪ Larger (7-23 microns): ave: 13 microns - Link bet. Flagellates & amoeba
- Zinc SO4 – few cyst ▪ Shorter UM - Binucleate, only troph
- 3 patterns of excretion: ▪ Anterior of axostyle may be split into fibrils - Amoeba-like flagellate w/c doesn’t have flagellum
1. High – para in nearly all samples ▪ Uniformly distributed nuclear chromatin - Order: Trichomonadida
2. Low – para in 40% of specimen ▪ Siderophil granules around delicate costa & axostyle - Small: 3-10 micron
3. Mixed pattern – 1-3 weeks high, laternating w/ short ▪ Less conspicuous cytostome - w/ hyaline pseudopodia (leaf-like)
- Sting test / Enterotest – identifying troph in duodenal fluid ▪ Pos. flagella about ½ - food vacuoles w/ bacteria
by intubation - In human vagina & prostate gland - NM – no peripheral chromatin karyosome (large & central;
- ELISA or Immunofluorescent (IF) – detect cyst & troph - Female host: mucosal surface of vagina ingesting bacteria & tetrad like discrete granules)
- Normal blood picture – uncomplicated Giardasis WBC & phagocytosed by macrophage - 1 or 2 nuclei
- Flatulence, fatty stool - Slight alkaline medium or more acid than healthy vagina - In large intestine (cecum & upper colon)
Treatment: - Peak incidence: 16-35 y.o (greatest sexual activity) - Unknown MoT
- Quinacrine / Atabrine (adult: 0.1g 3x a day for 5 days) - In pop. w/ ↑ risk for venereal dis. (Gonorrea & Trichomoniasis) - Carried inside egg of nematode like Histomonas meleagridis
- Metronidazole – 2nd choice: carcinogenic on rats; - 100% of female partners of men w/ Trichomoniasis – infected (causes turkey’s blackhead)
mutagenic on bacteria; not used on pregnant women; w/ - Metronidazole on woman alone → 60 – 80% cure; but w/ male - In eggs of E. vermicularis
alcohol → Disufiram effect partner → 95% cure - Not pathogenic, doesn’t produce organic lesions in intestine,
E. F. Trichomonadidae - Die in not more than 35-40 mins in H2O, or outside body > only irritation in intestinal mucosa → mucous diarrhea
• Cytostome 40° - Examine stool
• 3-5 free flagella, additional 1 at margin of undulating membrane - Survive in wet sponges (sev. hrs) & in urine (more than 24 hrs)
• Axostyle protrudes thru posterior - Occur in communal bathing or sharing douche equipment BLOOD & TISSUE FLAGELLATES (HAEMOFLAGELLATES)
• No cystic stage, non-transplantable - Most commonly acquired STInfection • Biological vector: blood sucking insect
a. Genus: Trichomonas - 2.5 M cases/ yr (asymptomatic fem - 3-15%; prosti – 50-75%) • Family: Trypanosomatidae
• Troph: - WBC & Trichoonads – present in vaginal secretions (liquid, • Genera:
o Have costa at base of undulating membrane greenish/yellow) & cover mucosa to urethral orifice & clitoris 1. Leishmania (tropica, braziliensis, donovani)
o ALL are parasitic - Gram (+) cocci & Gram (-) rods may be seen → 2° infection 2. Trypanosoma (gambiense, rhodesiense, cruzi)
1. Trichomonas tenax (T. elongata, T. buccalis) - I.P.: 4-28 days 3. Leptomonas
- Pyriform, 5-12 microns (smaller, more slender than vaginalis) - Vulvar pruritus, vaginal pruritus, vaginal discharge → acute 4. Crethedia
- 5th flagella doesn’t reach pos. end w/ no free pos. extension (after menstruation – inc. vaginal acidity) 5. Herpetomonas
- Costa-chromatic basal rod same length as UM - Dysuria (difficult, painful urination) – 20% of fem. 6. Phytomonas
- 1 bleph. - 90% - have cervical erosions → predisposition to cervical • Stages: (old name)
- Parabasal body – 1 fibril & shorter thicker body carcinoma (AIDS) 1. Amastigote (Leishmania)
- Thick axostyle – start near bleph, extend behind body - Cause prostatis & rarely reversible sterility 2. Promastigote (Leptomonas)
- Ovoidal, vesicular, anterior nucleus w/ chromatin - Male: latent, irritating persistent or recurring urethritis 3. Epimastigote (Crethedia) - UM
4. Trypomastigote (Trypanosoma) – more elongated - L. braziliensis peruviana – UTA (self-limiting lesions that don’t lymphocytes, proliferation of EC, neuroglial cells bet.
a. Metacyclic metastasize), involve nasopharynx Blood vessels & perivascular sheath
b. Typical • Cultivation: NNN medium - 2 forms of trypanosomiasis in Africa:
A Leishmania • LC: same except Genera of sandflies: 1. by rhodesiense → short, end fatally w/in 1 yr
• 2 stages: ✓ Hertigla 2. by gambiense → longer, milder, ends w/in 1 ½ yr (CNS)
✓ Amastigote – vertebrate host ✓ Wareleya - Culture in Weimann’s medium (also rhodesiense)
✓ Promastigote – invertebrate host (Phlebotomiae / sandflies) ✓ Brumptomyia 2 T. rhodesiense – Rhodesian trypanosomiasis
• Reservoir host: domesticated & wild animals ✓ Lutzomyia – 310 species - East African Sleeping Sickness
• Life Cycle: • Sporadic zoonosis 3 T. cruzi – South American Trypanosomiasis
❖ Vertebrate: • Dx: demonstrate amastigote: - Chagas disease
Bite of infected sandfy → promastigote on skin → engulfed by ➢ Culture in NNN - Vertebrate – all stages exc. Metacyclic trypo.
RES cells (macrophage) → amastigote → binary fission → ➢ Serology: o Typ. Tryp – blood
parasitized cell ruptures → Free Amastigote taken by sandflies ✓ Modified Montenegro intradermal rxn. o Amast., promast., epimast – REC & tissue
OR taken by macrophage ✓ Pellegrino test cells
❖ Invertebrate: • Chiclero – no Rx - Invertebrate: epimast – gut
Amastigote ingested in gut of sandfly → promastigote (8-20 3 L. donovani – Visceral Leishmaniasis or Kala-azar Meta. Tryp. – rectum
days) → migrate to pharynx → buccal cavity & mouth → - In viscera (liver, spleen, BM, lymph nodes) - Bite of infected Reduviid bug (defecate) → rubbed into punctured
promastigote in salivary gland transmitted to vertebrate - IP: 10 days – more than 1 yr. wound introducing Meta. Tryp. → blood as Tryp. → RES & tissue
1 L. tropica B Trypanosoma cells as Amast. →divide → promast. → epimast. → typical tryp. In
a Minor – dry or urban type cutaneous leishmaniasis • Has typical trypomastigote peripheral blood → bug eats →typ. Tryp. Taken out from man→
- Oriental sore (wright stain) • Vertebrate & invertebrate host ingested → intestinal tract → short epimast → multiply → long
- On skin (RES), lymph nodes, neutrophil epimast → in hindgut before meta. Tryp in 8-10 days → rectum →
• Transmission from insect vector:
- Not found in peripheral blood unless vicinity of ulcer feces of bug (no defecation – no infection)
✓ Anterior station – thru bite of blood sucking fly
- Cultivation: NNN (Novy, Mc Neal, Nicolle) medium - Insect vectors:
o Tse-Tse fly: T. gambiense – Glossina palpalis
- Anthroponosis - common to man o Reduviid or Triatomid bugs
T. rhodesiense – Glossina morsitans
- Sandfly vectors: ✓ Panstrongylus megistus
o Stages:
➢ Phlebotomus papatasii – India, Pakistan, Afghan, ✓ Rhodnius prolixus
▪ Epimastigote
Mediterranean ✓ Triatoma infestans
▪ Trypomastigote Metacyclic
➢ P. sergentii – Iran, Iraq, Crete, Portugal, Israel, - Other MoT:
▪ Trypomastigote Typical
Leban. ✓ Thru placenta
✓ Posterior station: fecal contamination of bite of arthropod vector
➢ P. perfilievi – Italy & Sicily ✓ Thru mother’s milk
o T. cruzi
➢ P. pernicrosus – Spain ✓ Sexual contact
o Stages:
- I.P.: 6 months ✓ Blood transfusion
▪ Complete 5
- Good prognosis ✓ Accidental ingestion of parasitized bug
▪ T. typical – vertebrates
- Life-long immunity - 3 forms: Acute, Subacute & Chronic
▪ T. metacyclic - invertebrates
b Major – rural or we Cutaneous Leishmaniasis - Initial lesion: Chagoma
• Infection of man of 2 types:
- Spherical amastigote w/ 1 nucleus - C-shaped tryp in peripheral blood
✓ African trypanosomiasis (gambiense & rhodosiense)
- Zoonosis – human infections occuring sporadically - Culture in NNN medium
✓ American trypanosomiasis (cruzi)
- P. papatasii & P. caucasicus - Biopsy of chagoma
1 T. gambiense – Gambian trypanosomiasis
- Good prognosis - MID or West African Sleeping Sickness
- High degree of immunity for wt & dry types - LC (also for rhodesiense)
- Shorter IP (6 days) Metacyclic trypomastigote (infective stage) → bite of Tse-
2 L. mexicana & L. braziliensis complex – New World Cutaneous / Tse fly → trypomastigote invades bloodstream → binary
Mucocutaneous Leishmaniasis division → reticular interstices of lymph nodes & spleen →
a L. mexicana complex – fast growing CSF → typical trypomastigote → taken up by fly → go into
- L. mexicana mexicana – Chiclero ulcer (face & ears) (Chicle fly’s gut → divide → metamorphosed to epimastigote →
ulcerative lesions on gum harvesting from sapodilla tress) multiply → metacyclic trypomastigote
- L. mexicana amazonensis – rarely infects human - Entire cycle in fly: 20 days
- L. mexicana pifanoi – dessiminated cutaneous leishmaniasis - IP: 2-23 days
- L. mexicana enrietti – in lab animals - Chronic disease w/ 3 progressive stages:
b L. braziliensis complex – slow growing 1. Acute – trypomastigote in bloodstream → local
- L. braziliensis braziliensis – Espundia (most notorious of inflammatory rxn. (subside in 1-2 weeks) → enter
American Leish. → mutilation, treatment resistance, bloodstream → multiply → PARASITEMIA
persistent) 2. Subacute – Tryp in lymph node → produce injurious
- L. braziliensis guyanenis – Pian Bois (Forest yaws) – single effects on every tissue & organ of body (1st: lymph) →
ulcerative lesions that metastasize over torso & extremities proliferation of Endotheliel cells lining sinuses
- L. braziliensis panamanensis – rare nasopharyngeal 3. Chronic – CNS invasion → enter subarachnoid space
involvement, doesn’t metastasize then brain substance → infiltration of plasma cells &
You might also like
- (English) MEGACITIES of The World (Season 1 - Complete)Document58 pages(English) MEGACITIES of The World (Season 1 - Complete)Sveta EnglishNo ratings yet
- Aqwa Theory ManualDocument168 pagesAqwa Theory ManualWeb Logueando100% (3)
- Tanabe Air Compressor ManualDocument4 pagesTanabe Air Compressor ManualMeta Beta50% (2)
- DX MSS Architecture - DocDocument48 pagesDX MSS Architecture - DocLuca Siddhartha100% (3)
- Module 6.4 ParasitesDocument6 pagesModule 6.4 ParasitesPNo ratings yet
- Communicablediseases 130202222928 Phpapp01Document4 pagesCommunicablediseases 130202222928 Phpapp01Adlyn Bea Albesa-BernaldezNo ratings yet
- Aureus C. Diphteriae (Man) : Classification Based On HaemolysisDocument4 pagesAureus C. Diphteriae (Man) : Classification Based On HaemolysisJulia IshakNo ratings yet
- Intoduction and NematodesDocument3 pagesIntoduction and NematodesENRIKA ROSE B. ALBISNo ratings yet
- Nematodes - TranscribedDocument12 pagesNematodes - TranscribedDenver CarbonNo ratings yet
- Disease Detectives Cheat SheetDocument2 pagesDisease Detectives Cheat SheetBereket LakiNo ratings yet
- SGD 2Document1 pageSGD 2Thea PepitoNo ratings yet
- 2023.pedia - Trans26.BacteriaI-Infections-Gram Negative (Part3)Document14 pages2023.pedia - Trans26.BacteriaI-Infections-Gram Negative (Part3)Adrian CaballesNo ratings yet
- Parasitology LectureDocument13 pagesParasitology LectureSophia Elinor MenesesNo ratings yet
- Communicable Diseases 2.4-5.22Document9 pagesCommunicable Diseases 2.4-5.22Vhince PiscoNo ratings yet
- Parasitology SummaryDocument9 pagesParasitology SummaryVanessa RamosNo ratings yet
- Parasitology NotesDocument5 pagesParasitology NotesAyaAlforque100% (1)
- Nematodes For Quiz 1 RevisedDocument6 pagesNematodes For Quiz 1 RevisedAra NuesaNo ratings yet
- Clinical Bacteriology MidtermDocument32 pagesClinical Bacteriology MidtermRazmine RicardoNo ratings yet
- Module 1 - TransDocument8 pagesModule 1 - TransJohanna Kate DiestroNo ratings yet
- Lecture NotesDocument61 pagesLecture NotesTom Anthony Tonguia100% (1)
- Parasitology Review On FlagellatesDocument2 pagesParasitology Review On FlagellatesKaoriMarieSembranoNo ratings yet
- LESSON 1B Introduction To ParasitologyDocument11 pagesLESSON 1B Introduction To ParasitologyKrixie LagundiNo ratings yet
- PARASITOSES and MYCOSESDocument7 pagesPARASITOSES and MYCOSESGeriel QuidesNo ratings yet
- Microbiology - 20Document6 pagesMicrobiology - 20karmylle andradeNo ratings yet
- 1 2 Prelim Introduction To ParasitologyDocument27 pages1 2 Prelim Introduction To ParasitologyHersey MiayoNo ratings yet
- Systemic and Opportunistic MycosesDocument5 pagesSystemic and Opportunistic Mycosesmiguel cuevasNo ratings yet
- Parasitology NematodesDocument26 pagesParasitology Nematodes8dxf5bqv6gNo ratings yet
- Body's Normal Flora:: ScavengersDocument4 pagesBody's Normal Flora:: ScavengersNatnaelNo ratings yet
- Micp211 (Lec) Final ReviewerDocument20 pagesMicp211 (Lec) Final ReviewerMAV TAJNo ratings yet
- Emerging Parasitic InfectionDocument6 pagesEmerging Parasitic Infectionmiguel gaquitNo ratings yet
- Micro-Para Practical Exam ReviewerDocument8 pagesMicro-Para Practical Exam ReviewerRA TranceNo ratings yet
- Microbiology 19 PDFDocument6 pagesMicrobiology 19 PDFLyka Villagracia AsiloNo ratings yet
- MODULE 6 Supplement APRIL 2018 PDFDocument3 pagesMODULE 6 Supplement APRIL 2018 PDFEryll Paolo AleaNo ratings yet
- Clinical Parasitology TransesDocument73 pagesClinical Parasitology TransesNikoh Anthony EwayanNo ratings yet
- Viruses of Medical Importance and Their DistributionDocument9 pagesViruses of Medical Importance and Their DistributionYIKI ISAACNo ratings yet
- PostTest Parasitology IDocument4 pagesPostTest Parasitology Iasa mutia0% (1)
- Para01 - Lab Parasitology 2 (1/1) Finals: RemindersDocument2 pagesPara01 - Lab Parasitology 2 (1/1) Finals: Remindersrenato renatoNo ratings yet
- 3.1 Bites Stings TabijeDocument7 pages3.1 Bites Stings TabijeEduardo Marco Villarama DayritNo ratings yet
- Communicable Disease HandoutsDocument8 pagesCommunicable Disease HandoutsMeryville JacildoNo ratings yet
- Bacteria-Borne Diseases Handout 2022Document3 pagesBacteria-Borne Diseases Handout 2022Anna CrisNo ratings yet
- MICP211 LEC - CombinedDocument40 pagesMICP211 LEC - CombinedJULIANA NICOLE TUIBUENNo ratings yet
- PATH InfectionDocument9 pagesPATH InfectionDavid DvoskineNo ratings yet
- Parasitology ReviewerDocument7 pagesParasitology ReviewerSandra Mhay RodilloNo ratings yet
- Medical Technology Assessment Program: Parasitology Review NotesDocument8 pagesMedical Technology Assessment Program: Parasitology Review NotesMoira Pauline LibroraniaNo ratings yet
- ParasitologyDocument4 pagesParasitologyJuan Miguel TevesNo ratings yet
- YersiniosisDocument2 pagesYersiniosisMaisarah RepinNo ratings yet
- Intro To para 2015Document3 pagesIntro To para 2015Ivy FlorentinoNo ratings yet
- Chapter 41 - 42 - Anaerobic OrganimsDocument4 pagesChapter 41 - 42 - Anaerobic OrganimsKoarie Frae ZuleNo ratings yet
- Zoonosis Parasiter (Protozoa) Penyakit Etiologi Hospes Distribusi Penularan Ke Manusia Gejala Klinik PD ManusiaDocument8 pagesZoonosis Parasiter (Protozoa) Penyakit Etiologi Hospes Distribusi Penularan Ke Manusia Gejala Klinik PD ManusiaAdil Bin IbrahimNo ratings yet
- (IM) 1.4b Malaria - Dra. CondeDocument14 pages(IM) 1.4b Malaria - Dra. CondeReggie Lyn BaricanNo ratings yet
- Parasitic DiseaseDocument21 pagesParasitic DiseaseRakib HossainNo ratings yet
- Intro To ParasitologyDocument4 pagesIntro To ParasitologyFaten BuenaventuraNo ratings yet
- Vector Borne Diseases: Malaria (Ague)Document20 pagesVector Borne Diseases: Malaria (Ague)Nina OaipNo ratings yet
- Specimen Collection LabDocument5 pagesSpecimen Collection LabENRIKA ROSE B. ALBISNo ratings yet
- Communicable Disease Nursing Part I IntroductionDocument5 pagesCommunicable Disease Nursing Part I Introductionchelljynxie100% (4)
- Parasitology: Basic Terminologies Major Groups of Medically Important ParasitesDocument4 pagesParasitology: Basic Terminologies Major Groups of Medically Important ParasitesHannah Grace CorveraNo ratings yet
- MIC 211 Papillomavirus Polyomavirus and Parvovirus IBD MergedDocument14 pagesMIC 211 Papillomavirus Polyomavirus and Parvovirus IBD MergedJack Ortega PuruggananNo ratings yet
- Micropara MidtermDocument30 pagesMicropara MidtermAmalyn OmarNo ratings yet
- Prelim Myco Trans PPT BasedDocument98 pagesPrelim Myco Trans PPT BasedJohn Vincent TacalNo ratings yet
- Arenavirus Bunyavirus FilovirusDocument5 pagesArenavirus Bunyavirus FilovirusRue VargasNo ratings yet
- Microbiology: Parvovirus, Papillomavirus, and PolyomavirusDocument3 pagesMicrobiology: Parvovirus, Papillomavirus, and PolyomavirusJustin TayabanNo ratings yet
- Balantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansDocument2 pagesBalantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansMichael Vincent P.No ratings yet
- Rickettsia ProwazekiiDocument3 pagesRickettsia ProwazekiinabdeepNo ratings yet
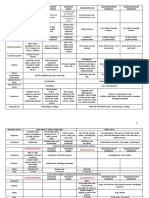
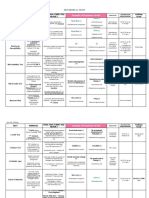
- DRUGS2Document1 pageDRUGS2KaoriMarieSembranoNo ratings yet
- Para - AmoebaDocument2 pagesPara - AmoebaKaoriMarieSembranoNo ratings yet
- Para - Amoeba TabulatedDocument1 pagePara - Amoeba TabulatedKaoriMarieSembranoNo ratings yet
- Parasitology Review On FlagellatesDocument2 pagesParasitology Review On FlagellatesKaoriMarieSembranoNo ratings yet
- Tabulated Review On AmoebaDocument1 pageTabulated Review On AmoebaKaoriMarieSembranoNo ratings yet
- Parasitology On AmoebaDocument2 pagesParasitology On AmoebaKaoriMarieSembranoNo ratings yet
- TrophozoitesDocument4 pagesTrophozoitesKaoriMarieSembranoNo ratings yet
- Anti-Epileptic DrugsDocument2 pagesAnti-Epileptic DrugsKaoriMarieSembranoNo ratings yet
- Table Review of ParasitesDocument6 pagesTable Review of ParasitesKaoriMarieSembranoNo ratings yet
- Micro Lab EnterobacteriaceaeDocument5 pagesMicro Lab EnterobacteriaceaeKaoriMarieSembranoNo ratings yet
- Biochemical Tests in MicrobiologyDocument7 pagesBiochemical Tests in MicrobiologyKaoriMarieSembrano100% (1)
- Psychoactive and AntibioticsDocument2 pagesPsychoactive and AntibioticsKaoriMarieSembranoNo ratings yet
- General Organic ChemistryDocument5 pagesGeneral Organic ChemistryG RNo ratings yet
- Urban Development - 2Document3 pagesUrban Development - 2APSDPS17 OFFICENo ratings yet
- Inductive Deductive QuizDocument1 pageInductive Deductive Quizkimbeerlyn doromasNo ratings yet
- CSF XanthochromiaDocument3 pagesCSF XanthochromiaShaikh Ghassan AbidNo ratings yet
- Horizontal Well Drill String DesignDocument23 pagesHorizontal Well Drill String DesignTarek HassanNo ratings yet
- Download full ebook of Google Cloud Platform Gcp Professional Cloud Network Engineer Certification Companion Learn And Apply Network Design Concepts To Prepare For The Exam 1St Edition Dario Cabianca online pdf all chapter docxDocument70 pagesDownload full ebook of Google Cloud Platform Gcp Professional Cloud Network Engineer Certification Companion Learn And Apply Network Design Concepts To Prepare For The Exam 1St Edition Dario Cabianca online pdf all chapter docxoufireny100% (11)
- Truth and Falsehood in IslamDocument3 pagesTruth and Falsehood in IslamZiad Cassim (anti-Sufi)No ratings yet
- Daily Lesson Plan: Understand and Use The Concept of Sine Rule To Solve ProblemsDocument4 pagesDaily Lesson Plan: Understand and Use The Concept of Sine Rule To Solve ProblemsRaj'z KingzterNo ratings yet
- Developmental Reading 1Document17 pagesDevelopmental Reading 1api-310357012100% (1)
- ReproDocument14 pagesRepro41umeshcha41No ratings yet
- WEG cfw500 Manual Do Usuario 10001278006 Manual Portugues BR PDFDocument134 pagesWEG cfw500 Manual Do Usuario 10001278006 Manual Portugues BR PDFLeandroNo ratings yet
- Impact of Leadership Styles On Employee Performance Case Study of A Non Profit Organization NGO in CambodiaDocument7 pagesImpact of Leadership Styles On Employee Performance Case Study of A Non Profit Organization NGO in CambodiaEditor IJTSRDNo ratings yet
- A Feminist Reading of Selected Poems of Kishwar Naheed: Huzaifa PanditDocument15 pagesA Feminist Reading of Selected Poems of Kishwar Naheed: Huzaifa PanditShivangi DubeyNo ratings yet
- Budesonide (Drug Study)Document3 pagesBudesonide (Drug Study)Franz.thenurse6888No ratings yet
- Science 2010Document77 pagesScience 2010roxtrNo ratings yet
- The Solitary Reaper - William Words WorthDocument8 pagesThe Solitary Reaper - William Words WorthLinio_92No ratings yet
- Cambridge Large1 Template Aog and JogDocument3 pagesCambridge Large1 Template Aog and JogFresh Prince Of NigeriaNo ratings yet
- Sonic Marketing Plan - Nguyen Thi Hong Diep, Truong Minh Hoang, Vu Quynh NgaDocument44 pagesSonic Marketing Plan - Nguyen Thi Hong Diep, Truong Minh Hoang, Vu Quynh NgaTruong Minh Hoang100% (1)
- Quarter 4 - Week 1 Daily Lesson PlanDocument3 pagesQuarter 4 - Week 1 Daily Lesson PlanAvegail Montemayor Orladan-MacanlalayNo ratings yet
- Interfacing Arduino With LinxDocument17 pagesInterfacing Arduino With LinxWinarno SurahmadNo ratings yet
- Rules25 50Document98 pagesRules25 50anandrv86No ratings yet
- 07363769410070872Document15 pages07363769410070872Palak AgarwalNo ratings yet
- MODUL 3 SPK - LF1S - CompleteDocument12 pagesMODUL 3 SPK - LF1S - CompleteKhovivatul qolbyNo ratings yet
- Chapter 6 - Job Order CostingDocument63 pagesChapter 6 - Job Order CostingXyne FernandezNo ratings yet
- WWW TSZ Com NP 2021 09 The-Bull-Exercise-Questions-And-Answers HTMLDocument11 pagesWWW TSZ Com NP 2021 09 The-Bull-Exercise-Questions-And-Answers HTMLAbhay PantNo ratings yet
- 555 Timer IcDocument23 pages555 Timer IcCircuits BazaarNo ratings yet